Quality of life after acute respiratory distress syndrome: a meta-analysis (original) (raw)
Abstract
Objective
To summarize long-term quality of life (QOL) and the degree of variation in QOL estimates across studies of acute respiratory distress (ARDS) survivors.
Design
A systematic review of studies evaluating QOL in ARDS survivors was conducted. Medline, EMBASE, CINAHL, pre-CINAHL, and the Cochrane Library were searched, and reference lists from relevant articles were evaluated. Two authors independently selected studies reporting QOL in adult survivors of ARDS or acute lung injury at least 30 days after intensive care unit discharge and extracted data on study design, patient characteristics, methods, and results.
Measurements and results
Thirteen independent observational studies (557 patients) met inclusion criteria. Eight of these studies used eight different QOL instruments, allowing only qualitative synthesis of results. The five remaining studies (330 patients) measured QOL using the Medical Outcomes Study 36-Item Short Form survey (SF-36). Mean QOL scores were similar across these studies, falling within a range of 20 points for all domains. Pooled domain-specific QOL scores in ARDS survivors 6 months or later after discharge ranged from 45 (role physical) to 66 (social functioning), or 15–26 points lower than population norms, in all domains except mental health (11 points) and role physical (39 points). Corresponding confidence intervals were no wider than ± 9 points. Six studies all found stable or improved QOL over time, but only one found significant improvement beyond 6 months after discharge.
Conclusions
ARDS survivors in different clinical settings experience similar decrements in QOL. The precise magnitude of these decrements helps clarify the long-term prognosis for ARDS survivors.
Similar content being viewed by others
Introduction
The acute respiratory distress syndrome (ARDS) is an important cause of morbidity and mortality in the intensive care unit (ICU) [1, 2]. As the short-term mortality after ARDS has fallen in recent years [3, 4, 5, 6], the long-term quality of life (QOL) experienced by ARDS survivors has become a research priority [7, 8]. While recent studies have measured QOL following ARDS, they have been unable to precisely characterize this outcome due to factors such as small sample size, extensive losses to follow-up, and differences in study design [9]. Furthermore, important clinical variation exists between ARDS patients at different centers [10, 11]. Consequently it is unclear whether QOL findings in ARDS survivors can be generalized across different studies [12]. Thus the objective of this review is to synthesize results from studies that measured long-term QOL in survivors of ARDS or acute lung injury to assess the variability of QOL estimates across studies and to provide more precise estimates of QOL outcomes in this patient population.
Materials and methods
Search strategy
To identify studies that measured QOL after hospital discharge in adult survivors of ARDS or acute lung injury we searched Medline (1966–2005), EMBASE (1974–2005), CINAHL (1982–2005), pre-CINAHL, and the Cochrane Library (2005, Issue 1) as of 31 March 2005. The following search strategy was used, with all terms mapped to the appropriate MeSH/EMTREE subject headings and “exploded”: (“quality of life” or “health status indicators”) and (“intensive care units” or “critical care” OR “critical illness” or “adult respiratory distress syndrome”). The terms “ARDS,” “acute lung injury,” and “ALI” were also searched as text words. No limits regarding language or publication type were applied. In addition, we hand-searched personal files and the reference lists of narrative reviews and of all articles included in the final review.
Study selection, data extraction, and quality assessment
Two authors (D.W.D., M.P.E.) independently reviewed citations, abstracts, and full articles to select eligible studies. Any disagreement regarding eligibility of a full article was resolved by a third author (D.M.N.). Agreement between the two reviewers was calculated by percentage agreement and the κ statistic [13]. For foreign language articles English translations of abstracts were reviewed to determine eligibility. Eligible full-text articles written in Spanish or German were reviewed by a single author (D.W.D.); one potentially eligible article written in Czech [14] was excluded without full-text review. Original research studies were selected for review if they met three eligibility criteria: (a) study of adults (≥ 14 years old) [15] with ARDS or acute lung injury, (b) use of a previously validated QOL instrument (see earlier reviews [8, 16] for a more complete description of these instruments), and (c) quantitative reporting of QOL for at least 30 days after ICU discharge. Studies of other patient populations (e.g., mechanically ventilated patients with pneumonia [17]) were eligible only if they separately reported QOL in ARDS survivors.
For each eligible study two authors (D.W.D., M.P.E.) independently abstracted data on study design, patient baseline characteristics, QOL instrument and method of administration, QOL results, and study quality. Abstraction was not masked to author or publication [18], and differences were resolved by a third author (D.M.N.). Study quality was assessed using three criteria adapted from the United States Preventive Services Task Force [19]: (a) assessment of an inception cohort with longitudinal follow-up, (b) loss to follow-up of less than 25% over 1 year, and (c) adjustment for confounders by randomization, statistical adjustment, or comparison to a matched population. No study was excluded from the synthesis based on study quality [20].
Statistical analysis
The Medical Outcomes Study Short Form 36-Item Health Survey (SF-36) measures QOL in eight domains; each is scored from 0 (worst QOL) to 100 (best QOL). For studies using SF-36 to measure QOL we abstracted two measures: (a) mean score for each QOL domain and (b) mean difference in domain-specific QOL score vs. population norms (matched on age, gender, and country). When published data were insufficient, authors of the original studies were contacted to provide these measures. When QOL was measured at multiple time points, the measurement taken closest to 24 months after hospital discharge was used in the quantitative synthesis. Study results were summarized by calculating (a) the median and range of QOL measurements across studies and (b) pooled estimates from a random-effects model with inverse variance-weighted averages [21]. Between-study heterogeneity was assessed using the Q statistic [22]. The number of studies was too small to reliably assess publication bias. A sensitivity analysis assessed the impact on pooled estimates of removing individual studies. All analyses were conducted using STATA 9.0 (Stata, College Station, Tex., USA).
Results
Search results and study characteristics
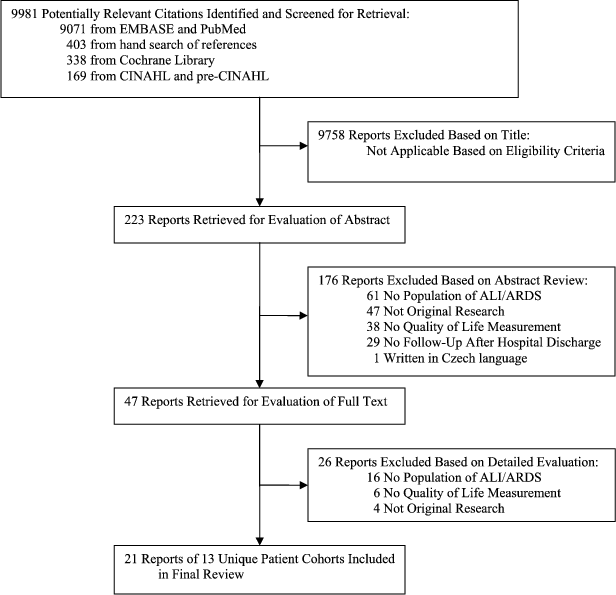
We identified 9,981 citations, of which 223 abstracts and 47 full-text publications were reviewed (Fig. 1). A total of 21 articles [10, 15, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41] describing 13 unique patient cohorts (n = 557) were eligible for the review (Table 1). Reviewer agreement on selection of abstracts for full-text evaluation was 93% (κ = 0.77) and for inclusion of articles in the final review was 100%.
Fig. 1
Flow diagram of literature search results. ARDS Acute respiratory distress syndrome; ALI acute lung injury
Table 1 Characteristics of studies reporting quality of life in adult ARDS survivors; values reported refer to ARDS patients only (QOL quality of Life, MV mechanical ventilation, SF-36 Medical Outcomes Study Short Form 36-Item Health Survey, LTVV low tidal volume ventilation, ARDS acute respiratory distress syndrome, CHF congestive heart failure, psych psychiatric, neuro neurological, CPR cardiopulmonary resuscitation, ALI acute lung injury, CRQ Chronic Respiratory Questionnaire, SIP Sickness Impact Profile, NHP Nottingham Health Profile, SGRQ St. George's Respiratory Questionnaire, EQ-5D EuroQol-5D, PQOL Patrick's Perceived Quality of Life, QWB Quality of Well-Being, MOD multiple organ dysfunction)
Of 13 independent studies reviewed six were conducted in the United States [15, 23, 25, 28, 29, 33], four in Europe [30, 31, 32, 39], two in Canada [10, 27], and one in South Korea [26]. Eleven studies were restricted to survivors of ARDS (n = 513), whereas two small studies [25, 27] (n < 25 in each) also included acute lung injury patients who did not fulfill ARDS criteria. All studies included both medical and surgical patients, except for one study [26] from a medical ICU. The most common exclusion criteria were head trauma [15, 23, 24, 33] and preexisting psychiatric or neurological disease [10, 23, 24]. Two studies had mean patient ages of 58 and 59 years [27, 32], but otherwise mean or median age ranged from 36 to 46 years. Five studies, including the four largest [10, 15, 23, 39], used SF-36 to measure QOL; these studies accounted for 59% of all patients included in the review. No other QOL instrument was used in more than two studies. The QOL instruments were administered in three ways: six studies used personal interview [10, 23, 27, 29, 31, 32], five used self-administered questionnaire [25, 26, 28, 30, 39], and two used telephone interview [15, 33]. Only two studies [10, 23], both using SF-36, met all three quality criteria. Five studies [10, 15, 23, 24, 25, 39] reported a comparison of domain-specific QOL against population norms or healthy controls; all used SF-36.
Search results and study characteristics
Five studies (n = 330) measured QOL in ARDS survivors using SF-36. Across these studies mean SF-36 scores fell within ranges of 12 points or less for six domains and 20 points or less for the role physical and social functioning domains. Domain-specific pooled scores ranged from 45 (role physical) to 66 (social functioning), with confidence intervals no larger than ± 9 points in any domain (Table 2). Statistical heterogeneity (p < 0.1) was detected in only two of the eight SF-36 domains: role physical and social functioning.
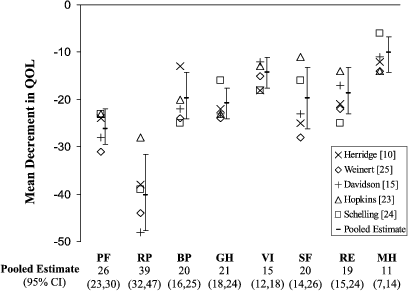
ARDS survivors had significantly lower QOL vs. matched population norms in all SF-36 domains. Mean QOL decrements, defined as the differences in SF-36 scores between ARDS survivors and population norms, were similar across the five studies, falling within ranges of 11 points or less for six QOL domains and 20 points or less for role physical and social functioning (Fig. 2). These decrements were greater in the four physical domains (physical functioning, role physical, bodily pain, general health perceptions) than in the four mental domains (vitality, social functioning, role emotional, mental health). Pooled estimates of the mean QOL decrements ranged between 15 and 26 points for all domains except for mental health (11 points) and role physical (39 points), with confidence intervals no larger than ± 8 points for any domain. Median vs. pooled scores did not differ by more than three points for any domain, suggesting that results were similar regardless of whether formal meta-analysis or a simpler methodology was used to summarize the data. Statistical heterogeneity in QOL decrements was again detected only in the role physical and social functioning domains. Sensitivity analysis by sequential exclusion of each individual study did not result in any important change in the pooled results.
Fig. 2
SF-36 quality of life decrements in adult ARDS survivors. The difference in SF-36 scores between ARDS survivors and healthy population norms is shown. The time points at which quality of life was measured are: 12 months [10], 15 months [25], 23 months [15], 24 months [23], and 48 months [24]. Pooled estimates were calculated using a random-effects model with associated 95% confidence intervals (95% CI) represented by error bars around the estimate. ARDS Acute respiratory distress syndrome; QOL quality of life; PF physical functioning; RP role physical; BP bodily pain; GH general health perceptions; VI vitality; SF social functioning; RE role emotional; MH mental health
Three studies reported longitudinal SF-36 findings. Two studies [10, 23] followed ARDS survivors prospectively from ICU discharge. Both studies noted improvement in all QOL domains between the first two QOL evaluations, which occurred at 0 and 12 months postdischarge in one study [23] and at 3 and 6 months in the other [10] (Table 2). Both studies showed pronounced (> 15 points) improvements in the physical functioning, role physical, and social functioning domains, while one study each showed similar improvement in vitality [23] and role emotional [10]. Both studies reported stable QOL beyond the second evaluation in all domains except role physical, which continued to improve during subsequent follow-up. The third longitudinal study [24] retrospectively identified a cohort of patients discharged over a 10-year period and administered the SF-36 at two points in calendar time (median 4.0 and 5.5 years after ICU discharge). Comparison of these two QOL measurements shows significant (p > 0.05) improvement in vitality (14 points) and a significant decline in both social functioning (27 points) and role emotional (8 points). No other QOL domain showed significant change, although in patients completing both measurements, the authors reported a significant increase in overall QOL, as assessed by the median SF-36 physical and mental component summary scores.
Table 2 SF-36 Quality of life scores in adult ARDS survivors (SF-36 Medical Outcomes Study Short Form 36-Item Health Survey, ALI, acute lung injury ARDS acute respiratory distress syndrome, QOL quality of life, CI confidence interval)
QOL results: studies using instruments other than SF-36
Eight studies (n = 227) used instruments other than SF-36 to measure QOL in ARDS survivors (Table 3). Studies differed markedly with respect to research question, patient population, comparison group, and type of QOL results reported. Among two studies that followed patients longitudinally after discharge, losses to follow-up were reported as 62% between discharge and 12 months postdischarge [29], and 65% between 28 days and 1 year after ARDS diagnosis. Compared against healthy populations, one study [26] found similar and another study [33] found worse, QOL scores in ARDS survivors. Compared to other critically ill populations, two studies found similar [28, 31], and one worse [30], QOL among ARDS survivors. Individual studies found no difference in global QOL measures by ventilation strategy [27] or ARDS etiology [26]. Three studies found no significant change in QOL beyond 6 months after discharge [29, 30, 33].
Table 3 Key findings for quality of life studies using instruments other than SF-36 (ALI acute lung injury, ARDS acute respiratory distress syndrome, SF-36 Medical Outcomes Study Short Form 36-Item Health Survey, QOL quality of life, CRQ Chronic Respiratory Questionnaire, LTVV low tidal volume ventilation, SIP Sickness Impact Profile, NHP Nottingham Health Profile, SGRQ St. George's Respiratory Questionnaire, EQ-5D EuroQol-5D, PQOL Patrick's Perceived Quality of Life, QWB Quality of Well-Being)
Discussion
This meta-analysis of quality of life in 557 ARDS survivors has three major findings. First, the five studies that used SF-36 reported similar QOL scores. This finding suggests that QOL may depend more strongly on factors common to ARDS survivors in different settings than on elements that differ between study populations. These common factors may include the impact of critical illness, an ARDS-specific effect, or the outcomes of ICU interventions used in treatment. Alternatively, similar long-term QOL among ARDS survivors may reflect lower baseline health status. At present, the mechanisms and relative importance of these and other factors have not been fully elucidated. Earlier studies [42, 43, 44] have shown that general ICU survivors have significantly lower SF-36 scores at baseline prior to admission (using retrospective patient or proxy responses) than population norms. However, no study in this review reported preadmission QOL specifically in ARDS survivors. As a result, this meta-analysis is unable to distinguish whether the observed QOL decrements reflect prior disability or the long-term effects of critical illness or ARDS. Furthermore, we are unable to comment on the specific effects of any interventions during hospitalization, as only two of the reviewed studies [27, 37] investigated the long-term impact of a specific ICU intervention, both finding no difference in QOL between patients receiving low tidal volume vs. standard ventilation. Further research is needed to fully understand the observed consistency of QOL scores among ARDS survivors across different settings.
Second, QOL recovery in ARDS survivors is both domain- and time-specific. In certain domains (i.e., physical functioning, role physical, and social functioning) QOL improves rapidly during the first 6 months after discharge. In other domains this initial QOL improvement is less pronounced. Beyond 6 months after discharge QOL remains stable or improves slightly, although substantial improvement in the role physical domain may continue [10, 23, 24, 29, 33]. However, the longitudinal studies [10, 23, 24, 28, 29, 33] reviewed here used different QOL instruments and had modest sample sizes (37–83 patients). Furthermore, follow-up times in four of these six studies ranged from 0 to 2 years after discharge, with one small study [28] measuring QOL at 3 years and one [24] assessing QOL at 5.5 years postdischarge (Tables 2, 3). Thus although ARDS survivors likely experience the majority of their QOL recovery in the first 6 months after discharge, it remains uncertain whether true and clinically meaningful QOL improvements occur beyond this time.
Third, ARDS survivors experience persistent and important QOL decrements compared to the general population. The magnitude of this decrement, measured using SF-36, is generally 15–26 points, although this decrement may be more pronounced for physical role limitations and less pronounced for mental health. To illustrate the magnitude of these findings a 25-point decrement in physical functioning corresponds to moderate limitation (decrease by one of three response levels) in half of tested physical activities (e.g., “lifting or carrying groceries”), and a 10-point decrement in mental health corresponds to mild impairment (increase by one of six response levels), in two of five mental states (e.g., feeling depressed). Thus, compared to population norms, ARDS survivors experience important and persistent QOL decrements after ICU discharge. The magnitude and precision of the pooled estimates in Fig. 2 may help clinicians better understand the long-term prognosis for ARDS patients and serve as a reference point for future research studying the impact of specific interventions on QOL in this patient population.
ARDS is an archetype for severe critical illness, representing a multifactorial syndrome experienced by many patients with long-term ICU stays [45]. Few studies have compared QOL in ARDS survivors vs. ICU survivors without ARDS in order to understand the unique contribution of ARDS to patient outcomes. Davidson et al. [15] found ARDS survivors to have lower QOL than general ICU survivors, whereas three other studies [28, 30, 31] found no widespread differences in QOL. An earlier systematic review [8] examined QOL in general populations of ICU survivors. The largest study (n = 298) in that review [46] reported SF-36 QOL scores at 12 months after discharge that were within five points of the pooled estimates for ARDS survivors in our study, except that general ICU survivors reported significantly less bodily pain (mean 67, 95% confidence interval 64–70 vs. pooled estimate 58, 95% confidence interval 54–63), but more emotional role limitations (50, 45–55 vs. 65, 60–70) than ARDS survivors. Thus ARDS survivors appear to have similar long-term QOL to other ICU survivors, suggesting that ARDS (vs. general critical illness) may not exert a specific effect on long-term QOL, or that any ARDS-specific effect is balanced by a difference in the baseline QOL of survivors.
This analysis has certain limitations. First, the studies included in the meta-analysis had differing observational designs, eligibility criteria, QOL instruments, and techniques of administration; furthermore, the clinical definition of ARDS is inherently imprecise [10, 11]. Despite this clinical heterogeneity, our estimates of the mean scores and decrements in six of eight QOL domains fell within narrow ranges (≤ 12 points) across all studies and showed no evidence of statistical heterogeneity. The pooled estimates for the two potentially heterogeneous QOL domains (social functioning and role physical) should be interpreted with caution. Second, we were unable to quantitatively synthesize QOL results from instruments other than SF-36. Thus our pooled estimates of QOL rely on the validity of SF-36 in ARDS patients. To our knowledge, SF-36 has not been validated specifically in ARDS patients. However, it has been validated in ICU patients [47], recommended for use in studying the long-term outcomes of ICU survivors [7], and used more widely than any other instrument for that purpose [8]. Furthermore, the two highest-quality studies, and all five studies comparing domain-specific QOL to healthy population norms, used SF-36. Third, the number of studies and patients included in this review is small. Consequently the pooled estimates for certain SF-36 domains (e.g., role physical and social function) are relatively imprecise. Furthermore, certain findings (e.g., longitudinal SF-36 changes, reported by only three studies) rely on particularly small samples. Thus our conclusions should be considered preliminary and encourage larger, confirmatory longitudinal studies. Finally, the reviewed study populations suffer from the high mortality rates and losses to follow-up that are typical of critically ill populations [9]. At 1–4 years after hospital discharge the five SF-36 studies achieved follow-up rates of 65% [25] to 89% [23] among eligible patients who survived to hospital discharge; however, hospital mortality rates ranged from 38% [23, 24] to 46% [25]. Thus the study populations and related findings may not be representative of ARDS patients as a whole.
Further studies of long-term QOL outcomes in ARDS survivors are needed to better characterize the trajectory of QOL decline and recovery in these patients. Especially needed are validated methods for measuring baseline QOL prior to hospital admission (i.e., proxy or retrospective patient assessments). In addition to measuring baseline QOL, future studies of QOL in ARDS survivors should evaluate larger patient samples and extend longitudinal assessments over longer follow-up periods. To facilitate comparison with prior research future studies should consider using the SF-36 QOL instrument and reporting domain-specific means, standard deviations, and comparisons to population norms matched on age, gender, and country. When SF-36 is not feasible, the EQ-5D [48] is a brief, five-question QOL instrument that is also recommended for use in ICU patients [7]. In order to more fully understand the impact of existing and novel ICU therapies, future studies of those therapies should explicitly assess long-term QOL as an outcome.
In conclusion, this meta-analysis suggests that, despite early improvement in some domains, quality of life in ARDS survivors remains persistently lower than in healthy populations. The magnitude of this decrement is consistent across different populations of ARDS survivors and may be more pronounced in physical domains than in mental health. Additional research is needed to further characterize QOL recovery in ARDS survivors, to help understand the mechanisms responsible for QOL decline and recovery, and to assess the impact of ICU interventions on these patients' long-term quality of life. These findings may help clinicians more accurately understand the long-term prognosis for ARDS survivors and help researchers effectively plan future studies in this field.
References
- Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Legall JR, Morris A, Spragg R (1994) The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 149:818–824
PubMed CAS Google Scholar - Rubenfeld GD, Caldwell E, Peabody E, Weaver J, Martin DP, Neff M, Stern EJ, Hudson LD (2005) Incidence and outcomes of acute lung injury. N Engl J Med 353:1685–1693
Article PubMed CAS Google Scholar - Bersten AD, Edibam C, Hunt T, Moran J (2002) Incidence and mortality of acute lung injury and the acute respiratory distress syndrome in three Australian States. Am J Respir Crit Care Med 165:443–448
PubMed Google Scholar - Milberg JA, Davis DR, Steinberg KP, Hudson LD (1995) Improved survival of patients with acute respiratory distress syndrome (ARDS): 1983–1993. JAMA 273:306–309
Article PubMed CAS Google Scholar - Abel SJ, Finney SJ, Brett SJ, Keogh BF, Morgan CJ, Evans TW (1998) Reduced mortality in association with the acute respiratory distress syndrome (ARDS). Thorax 53:292–294
Article PubMed CAS Google Scholar - Carone M, Donner CF (2005) Impact of long-term ventilation on patients' health status. Chronic Respir Dis 2:29–33
Article CAS Google Scholar - Angus DC, Carlet J (2003) Surviving intensive care: a report from the 2002 Brussels Roundtable. Intensive Care Med 29:368–377
PubMed Google Scholar - Dowdy DW, Eid MP, Sedrakyan A, Mendez-Tellez PA, Pronovost PJ, Herridge MS, Needham DM (2005) Quality of life in adult survivors of critical illness: a systematic review of the literature. Intensive Care Med 31:611–620
Article PubMed Google Scholar - Needham DM, Dowdy DW, Mendez-Tellez PA, Herridge MS, Pronovost PJ (2005) Studying outcomes of intensive care unit survivors: measuring exposures and outcomes. Intensive Care Med 31:1153–1160
Article PubMed Google Scholar - Herridge MS, Cheung AM, Tansey CM, Matte-Martyn A, Diaz-Granados N, Al-Saidi F, Cooper AB, Guest CB, Mazer CD, Mehta S, Stewart TE, Barr A, Cook D, Slutsky AS (2003) One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med 348:683–693
Article PubMed Google Scholar - Esteban A, Fernandez-Segoviano P, Frutos-Vivar F, Aramburu JA, Najera L, Ferguson ND, Alia I, Gordo F, Rios F (2004) Comparison of clinical criteria for the acute respiratory distress syndrome with autopsy findings. Ann Intern Med 141:440–445
PubMed Google Scholar - Fan E, Needham DM, Stewart TE (2005) Ventilatory management of acute lung injury and acute respiratory distress syndrome. JAMA 294:2889–2896
Article PubMed CAS Google Scholar - Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Article PubMed CAS Google Scholar - Parizkova R, Cerny V, Dostal P, Vasatko L, Hora P, Herold I, Novak I, Nalos D (2001) Monitoring quality of life in critically ill patients: a multicenter study. Anesteziol Neodkladna Pece 12:240–251
Google Scholar - Davidson TA, Caldwell ES, Curtis JR, Hudson LD, Steinberg KP (1999) Reduced quality of life in survivors of acute respiratory distress syndrome compared with critically ill control patients. JAMA 281:354–360
Article PubMed CAS Google Scholar - Hayes JA, Black NA, Jenkinson C, Young D, Rowan KM, Daly K, Ridley S (2000) Outcome measures for adult critical care: a systematic review. Health Technol Assess 4:1–111
PubMed CAS Google Scholar - Hamel MB, Phillips RS, Davis RB, Teno J, Connors AF, Desbiens N, Lynn J, Dawson NV, Fulkerson W, Tsevat J (2000) Outcomes and cost-effectiveness of ventilator support and aggressive care for patients with acute respiratory failure due to pneumonia or acute respiratory distress syndrome. Am J Med 109:614–620
Article PubMed CAS Google Scholar - Berlin J (1996) A. Randomized trial comparing masked/unmasked meta-analyses. AHCPR-97–20. Agency for Health Care Policy and Research, Rockville
- Harris RP, Helfand M, Woolf SH, Lohr KN, Mulrow CD, Teutsch SM, Atkins D; Methods Work Group, Third US Preventive Services Task Force (2001) Current methods of the US Preventive Services Task Force: a review of the process. Am J Prev Med 20:21–35
Article PubMed CAS Google Scholar - Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283:2008–2012
Article PubMed CAS Google Scholar - Berlin JA, Laird NM, Sacks HS, Chalmers TC (1989) A comparison of statistical methods for combining event rates from clinical trials. Stat Med 8:141–151
Article PubMed CAS Google Scholar - DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Article PubMed CAS Google Scholar - Hopkins RO, Weaver LK, Collingridge D, Parkinson RB, Chan KJ, Orme JF (2005) Two-year cognitive, emotional, and quality-of-life outcomes in acute respiratory distress syndrome. Am J Respir Crit Care Med 171:340–347
Article PubMed Google Scholar - Schelling G, Stoll C, Vogelmeier C, Hummel T, Behr J, Kapfhammer HP, Rothenhausler HB, Haller M, Durst K, Krauseneck T, Briegel J (2000) Pulmonary function and health-related quality of life in a sample of long-term survivors of the acute respiratory distress syndrome. Intensive Care Med 26:1304–1311
Article PubMed CAS Google Scholar - Weinert CR, Gross CR, Kangas JR, Bury CL, Marinelli WA (1997) Health-related quality of life after acute lung injury. Am J Respir Crit Care Med 156:1120–1128
PubMed CAS Google Scholar - Kim SJ, Oh BJ, Lee JS, Lim CM, Shim TS, Lee SD, Kim WS, Kim DS, Kim WD, Koh Y (2004) Recovery from lung injury in survivors of acute respiratory distress syndrome: difference between pulmonary and extrapulmonary subtypes. Intensive Care Med 30:1960–1963
Article PubMed Google Scholar - Cooper AB, Ferguson ND, Hanly PJ, Meade MO, Kachura JR, Granton JT, Slutsky AS, Stewart TE (1999) Long-term follow-up of survivors of acute lung injury: lack of effect of a ventilation strategy to prevent barotrauma. Crit Care Med 27:2616–2621
Article PubMed CAS Google Scholar - Chatila W, Kreimer DT, Criner GJ (2001) Quality of life in survivors of prolonged mechanical ventilatory support. Crit Care Med 29:737–742
Article PubMed CAS Google Scholar - McHugh LG, Milberg JA, Whitcomb ME, Schoene RB, Maunder RJ, Hudson LD (1994) Recovery of function in survivors of the acute respiratory distress syndrome. Am J Respir Crit Care Med 150:90–94
PubMed CAS Google Scholar - Combes A, Costa MA, Trouillet JL, Baudot J, Mokhtari M, Gibert C, Chastre J (2003) Morbidity, mortality, and quality-of-life outcomes of patients requiring > or = 14 days of mechanical ventilation. Crit Care Med 31:1373–1381
Article PubMed Google Scholar - Granja C, Morujao E, Costa-Pereira A (2003) Quality of life in acute respiratory distress syndrome survivors may be no worst than in other ICU survivors. Intensive Care Med 29:1744–1750
Article PubMed Google Scholar - Ortiz CD, Jam Gatell MR (2003) Long term of quality of life and mortality in acute respiratory distress syndrome (ARDS) patients. Enferm Intensiva 14:88–95
Google Scholar - Angus DC, Musthafa AA, Clermont G, Griffin MF, Linde-Zwirble WT, Dremsizov TT, Pinsky MR (2001) Quality-adjusted survival in the first year after the acute respiratory distress syndrome. Am J Respir Crit Care Med 163:1389–1394
PubMed CAS Google Scholar - Hopkins RO, Weaver LK, Pope D, Orme JF, Bigler ED, Larson-Lohr V (1999) Neuropsychological sequelae and impaired health status in survivors of severe acute respiratory distress syndrome. Am J Respir Crit Care Med 160:50–56
PubMed CAS Google Scholar - Hopkins RO, Weaver LK, Chan KJ, Orme J (2004) Quality of life, emotional, and cognitive function following acute respiratory distress syndrome. J Int Neuropsychol Soc 10:1005–1017
PubMed Google Scholar - Kapfhammer HP, Rothenhausler HB, Krauseneck T, Stoll C, Schelling G (2004) Posttraumatic stress disorder and health-related quality of life in long-term survivors of acute respiratory distress syndrome. Am J Psychiatry 161:45–52
Article PubMed Google Scholar - Orme J Jr, Romney JS, Hopkins RO, Pope D, Chan KJ, Thomsen G, Crapo RO, Weaver LK (2003) Pulmonary function and health-related quality of life in survivors of acute respiratory distress syndrome. Am J Respir Crit Care Med 167:690–694
Article PubMed Google Scholar - Rothenhausler HB, Ehrentraut S, Stoll C, Schelling G, Kapfhammer HP (2001) The relationship between cognitive performance and employment and health status in long-term survivors of the acute respiratory distress syndrome: results of an exploratory study. Gen Hosp Psychiatry 23:90–96
Article PubMed CAS Google Scholar - Schelling G, Stoll C, Haller M, Briegel J, Manert W, Hummel T, Lenhart A, Heyduck M, Polasek J, Meier M, Preuss U, Bullinger M, Schuffel W, Peter K (1998) Health-related quality of life and posttraumatic stress disorder in survivors of the acute respiratory distress syndrome. Crit Care Med 26:651–659
Article PubMed CAS Google Scholar - Stoll C, Haller M, Briegel J, Meier M, Manert W, Hummel T, Heyduck M, Lenhart A, Polasek J, Bullinger M, Schelling G (1998) Health-related quality of life. Long-term survival in patients with ARDS following extracorporeal membrane oxygenation (ECMO). Anaesthesist 47:24–29
Article PubMed CAS Google Scholar - Stoll C, Rothenhausler HB, Kapfhammer HP, Schelling G (2000) Pulmonary function, quality of life, psychosocial and cognitive function after ARDS. J Anasth Intensivbehandl 7:212–215
Google Scholar - Wehler M, Geise A, Hadzionerovic D, Aljukic E, Reulbach U, Hahn EG, Strauss R (2003) Health-related quality of life of patients with multiple organ dysfunction: individual changes and comparison with normative population. Crit Care Med 31:1094–1101
Article PubMed Google Scholar - Ridley SA, Chrispin PS, Scotton H, Rogers J, Lloyd D (1997) Changes in quality of life after intensive care: comparison with normal data. Anaesthesia 52:195–202
Article PubMed CAS Google Scholar - Graf J, Koch M, Dujardin R, Kersten A, Janssens U (2003) Health-related quality of life before, 1 month after, and 9 months after intensive care in medical cardiovascular and pulmonary patients. Crit Care Med 31:2163–2169
Article PubMed Google Scholar - Herridge MS, Angus DC (2005) Acute lung injury—affecting many lives. N Engl J Med 353:1736–1738
Article PubMed CAS Google Scholar - Pettila V, Kaarlola A, Makelainen A (2000) Health-related quality of life of multiple organ dysfunction patients one year after intensive care. Intensive Care Med 26:1473–1479
Article PubMed CAS Google Scholar - Chrispin PS, Scotton H, Rogers J, Lloyd D, Ridley SA (1997) Short Form 36 in the intensive care unit: assessment of acceptability, reliability and validity of the questionnaire. Anaesthesia 52:15–23
Article PubMed CAS Google Scholar - EuroQol Group (1990) EuroQol–a new facility for the measurement of health-related quality of life. Health Policy 16:199–208
Article Google Scholar
Acknowledgements
We thank Ramona Hopkins, PhD, and Gustav Schelling, MD, for providing data for use in this review.
Author information
Authors and Affiliations
- Department of Epidemiology, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, USA
David W. Dowdy & Eliseo Guallar - School of Medicine, Johns Hopkins University, Baltimore, MD, USA
David W. Dowdy & Mark P. Eid - School of Nursing, Johns Hopkins University, Baltimore, MD, USA
Cheryl R. Dennison & Peter J. Pronovost - Department of Anesthesiology/Critical Care Medicine, Johns Hopkins University, Baltimore, MD, USA
Pedro A. Mendez-Tellez & Peter J. Pronovost - Interdepartmental Division of Critical Care Medicine, University of Toronto, Toronto, Canada
Margaret S. Herridge - Department of Surgery, Johns Hopkins University, Baltimore, MD, USA
Peter J. Pronovost - Department of Health Policy and Management, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, USA
Peter J. Pronovost - Division of Pulmonary/Critical Care Medicine, Johns Hopkins University, 1830 E. Monument Street, 21205, Baltimore, MD, USA
Dale M. Needham
Authors
- David W. Dowdy
You can also search for this author inPubMed Google Scholar - Mark P. Eid
You can also search for this author inPubMed Google Scholar - Cheryl R. Dennison
You can also search for this author inPubMed Google Scholar - Pedro A. Mendez-Tellez
You can also search for this author inPubMed Google Scholar - Margaret S. Herridge
You can also search for this author inPubMed Google Scholar - Eliseo Guallar
You can also search for this author inPubMed Google Scholar - Peter J. Pronovost
You can also search for this author inPubMed Google Scholar - Dale M. Needham
You can also search for this author inPubMed Google Scholar
Corresponding author
Correspondence toDale M. Needham.
Additional information
This research is supported by National Institutes of Health (ALI SCCOR Grant # P050 HL 73994). D.W.D. is supported by a Medical Scientist Training Program Grant from the National Institutes of Health (Award # 5 T32 GMO7309). D.M.N. is supported by a Clinician-Scientist Award from the Canadian Institutes of Health Research and a Detweiler Fellowship from the Royal College of Physicians and Surgeons of Canada.
Rights and permissions
About this article
Cite this article
Dowdy, D.W., Eid, M.P., Dennison, C.R. et al. Quality of life after acute respiratory distress syndrome: a meta-analysis.Intensive Care Med 32, 1115–1124 (2006). https://doi.org/10.1007/s00134-006-0217-3
- Received: 13 January 2006
- Accepted: 02 May 2006
- Published: 17 June 2006
- Issue Date: August 2006
- DOI: https://doi.org/10.1007/s00134-006-0217-3