Potentially resistant microorganisms in intubated patients with hospital-acquired pneumonia: the interaction of ecology, shock and risk factors (original) (raw)
Abstract
Purpose
As per 2005 American Thoracic Society and Infectious Disease Society of America (ATS/IDSA) guidelines for managing hospital-acquired pneumonia, patients with early-onset pneumonia and without risk factors do not need to be treated for potentially resistant microorganisms (PRM).
Methods
This was a secondary analysis of a prospective, observational, cohort, multicentre study conducted in 27 ICUs from nine European countries.
Results
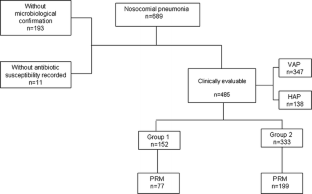
From a total of 689 patients with nosocomial pneumonia who required mechanical ventilation, 485 patients with confirmed etiology and antibiotic susceptibility were further analysed. Of these patients, 152 (31.3 %) were allocated to group 1 with early-onset pneumonia and no risk factors for PRM acquisition, and 333 (68.7 %) were classified into group 2 with early-onset pneumonia with risk factors for PRM or late-onset pneumonia. Group 2 patients were older and had more chronic renal failure and more severe illness (SAPS II score, 44.6 ± 16.5 vs. 47.4 ± 17.8, p = 0.04) than group 1 patients. Trauma patients were more frequent and surgical patients less frequent in group 1 than in group 2 (p < 0.01). In group 1, 77 patients (50.7 %) had PRM in spite of the absence of classic risk factors recognised by the current guidelines. A logistic regression analysis identified that presence of severe sepsis/septic shock (OR = 3.7, 95 % CI 1.5–8.9) and pneumonia developed in centres with greater than 25 % prevalence of PRM (OR = 11.3, 95 % CI 2.1–59.3) were independently associated with PRM in group 1 patients.
Conclusions
In patients admitted to ICUs with a prevalence of PRM greater than 25 % or with severe sepsis/septic shock, empiric therapy for group 1 nosocomial pneumonia requiring mechanical ventilation should also include agents likely to be effective for PRM pathogens.
Access this article
Subscribe and save
- Starting from 10 chapters or articles per month
- Access and download chapters and articles from more than 300k books and 2,500 journals
- Cancel anytime View plans
Buy Now
Price excludes VAT (USA)
Tax calculation will be finalised during checkout.
Instant access to the full article PDF.
Fig. 1
Similar content being viewed by others
References
- American Thoracic Society (2005) Guidelines for the management of adults with hospital-acquired pneumonia, ventilator-associated pneumonia, and healthcare-associated pneumonia. Am J Respir Crit Care Med 17:388–416
Google Scholar - Rello J, Gallego M, Mariscal D, Soñora R, Valles J (1997) The value of routine microbial investigation in ventilator-associated pneumonia. Am J Respir Crit Care Med 156:196–200
PubMed CAS Google Scholar - Alvarez-Lerma F, ICU-Acquired Pneumonia Study Group (1996) Modification of empiric antibiotic treatment in patients with pneumonia acquired in the intensive care unit. Intensive Care Med 22:387–394
Article PubMed CAS Google Scholar - Luna CM, Vujacich P, Niederman MS, Vay C, Gherardi C, Matera J, Jolly EC (1997) Impact of BAL data on the therapy and outcome of ventilator-associated pneumonia. Chest 111:676–685
Article PubMed CAS Google Scholar - Vincent JL, Rello J, Marshall J, Silva E, Anzueto A, Martin CD, Moreno R, Lipman J, Gomersall C, Sakr Y, Reinhart K, EPIC II Group of Investigators (2009) International study of the prevalence and outcomes of infection in intensive care units. JAMA 302:2323–2329
Article PubMed CAS Google Scholar - Koulenti D, Lisboa T, Brun-Buisson C, Krueger W, Macor A, Sole-Violan J, Diaz E, Topeli A, DeWaele J, Carneiro A, Martin-Loeches I, Armaganidis A, Rello J, EU-VAP/CAP Study Group (2009) Spectrum of practice in the diagnosis of nosocomial pneumonia in patients requiring mechanical ventilation in European intensive care units. Crit Care Med 37:2360–2368
Article PubMed Google Scholar - Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP et al (2007) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Epidemiology 18:800–804
Article Google Scholar - McCabe JR, Jackson GG (1962) Gram-negative bacteraemia I: etiology and ecology. Arch Intern Med 110:847–855
Article Google Scholar - Le-Gall JR, Lemeshow S, Saulnier F (1993) A new simplified physiology score (SAPS II) based on a European/North American multicentre study. JAMA 270:2957–296314
Article PubMed CAS Google Scholar - American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 20:864–874
Article Google Scholar - Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, Reinhart CK, Suter PM, Thijs LG (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. Intensive Care Med 22:707–710
Article PubMed CAS Google Scholar - Pugin J, Auckenthaler R, Mili N, Janssens JP, Lew PD, Suter PM (1991) Diagnosis of ventilator–associated pneumonia by bacteriologic analysis of bronchoscopic and non bronchoscopic ‘blind’ bronchoalveolar lavage fluid. Am Rev Respi Dis 143:1121–1129
CAS Google Scholar - American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 20:864–874
Article Google Scholar - Chastre J, Fagon JY (2002) Ventilator-associated pneumonia. Am J Respir Crit Care Med 165:867–903
PubMed Google Scholar - Ferrer M, Liapikou A, Valencia M, Esperatti M, Theessen A, Antonio Martinez J, Mensa J, Torres A (2010) Validation of the American Thoracic Society-Infectious Diseases Society of America guidelines for hospital-acquired pneumonia in the intensive care unit. Clin Infect Dis 50:945–952
Article PubMed Google Scholar - Heyland DK, Dodek P, Muscedere J, Day A, Cook D, Canadian Critical Care Trials Group (2008) Randomized trial of combination versus monotherapy for the empiric treatment of suspected ventilator-associated pneumonia. Crit Care Med 36:737–744
Article PubMed Google Scholar - Rello J, Torres A (1996) Microbial causes of ventilator-associated pneumonia. Semin Respir Infect 11:24–31
PubMed CAS Google Scholar - Rello J, Ausina V, Ricart M, Puzo C, Quintana E, Net A, Prats G (1994) Risk factors for infection by Pseudomonas aeruginosa in patients with ventilator-associated pneumonia. Intensive Care Med 20:193–198
Article PubMed CAS Google Scholar - Sirvent JM, Torres A, El-Ebiary M, Castro P, de Batlle J, Bonet A (1997) Protective effect of intravenously administered cefuroxime against nosocomial pneumonia in patients with structural coma. Am J Respir Crit Care Med 155:1729–1734
PubMed CAS Google Scholar - Nseir S, Blazejewski C, Lubret R, Wallet F, Courcol R, Durocher A (2011) Risk of acquiring multidrug-resistant Gram-negative bacilli from prior room occupants in the intensive care unit. Clin Microbiol Infect 17:1201–1208
Article PubMed CAS Google Scholar - Grundmann H, Bärwolff S, Tami A, Behnke M, Schwab F, Geffers C, Halle E, Göbel UB, Schiller R, Jonas D, Klare I, Weist K, Witte W, Beck-Beilecke K, Schumacher M, Rüden H, Gastmeier P (2005) How many infections are caused by patient-to-patient transmission in intensive care units? Crit Care Med 33:946–951
Article PubMed Google Scholar - Rello J, Sa-Borges M, Correa H, Leal SR, Baraibar J (1999) Variations in etiology of ventilator-associated pneumonia across four treatment sites: implications for antimicrobial prescribing practices. Am J Respir Crit Care Med 160:608–613
PubMed CAS Google Scholar - Namias N, Samiian L, Nino D, Shirazi E, O’Neill K, Kett DH, Ginzburg E, McKenney MG, Sleeman D, Cohn SM (2000) Incidence and susceptibility of pathogenic bacteria vary between ICU within a single hospital: implications for empiric antibiotic strategies. J Trauma 49:638–645
Article PubMed CAS Google Scholar - Rello J, Ulldemolins M, Lisboa T, Koulenti D, Mañez R, Martin-Loeches I, De Waele JJ, Putensen C, Guven M, Deja M, Diaz E, EU-VAP/CAP Study Group (2011) Determinants of prescription and choice of empirical therapy for hospital-acquired and ventilator-associated pneumonia. Eur Respir J 37:1332–1339
Article PubMed CAS Google Scholar - Depuydt PO, Vandijck DM, Bekaert MA, Decruyenaere JM, Blot SI, Vogelaers DP, Benoit DD (2008) Determinants and impact of multidrug antibiotic resistance in pathogens causing ventilator-associated-pneumonia. Crit Care 12:R142
Article PubMed Google Scholar - Tseng CC, Liu SF, Wang CC, Tu ML, Chung YH, Lin MC, Fang WF (2012) Impact of clinical severity index, infective pathogens, and initial empiric antibiotic use on hospital mortality in patients with ventilator-associated pneumonia. Am J Infect Control 40(7):648–652
Article PubMed Google Scholar - Damas P, Layios N, Seidel L, Nys M, Melin P, Ledoux D (2011) Severity of ICU-acquired pneumonia according to infectious microorganisms. Intensive Care Med 37:1128–1135
Article PubMed Google Scholar - Kumar A, Safdar N, Kethireddy S, Chateau D (2010) A survival benefit of combination antibiotic therapy for serious infections associated with sepsis and septic shock is contingent only on the risk of death: a meta-analytic/meta-regression study. Crit Care Med 38:1651–1664
Article PubMed CAS Google Scholar - Kollef KE, Schramm GE, Wills AR, Reichley RM, Micek ST, Kollef MH (2008) Predictors of 30-day mortality and hospital costs in patients with ventilator-associated pneumonia attributed to potentially antibiotic-resistant gram-negative bacteria. Chest 134:281–287
Article PubMed CAS Google Scholar - Lisboa T, Diaz E, Sa-Borges M, Socias A, Sole-Violan J, Rodríguez A, Rello J (2008) The ventilator-associated pneumonia PIRO score: a tool for predicting ICU mortality and health-care resources use in ventilator-associated pneumonia. Chest 134:1208–1216
Article PubMed Google Scholar - Kumar A, Roberts D, Wood KE, Light B, Parrillo JE, Sharma S, Suppes R, Feinstein D, Zanotti S, Taiberg L, Gurka D, Kumar A, Cheang M (2006) Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med 34:1589–1596
Article PubMed Google Scholar
Acknowledgments
Supported by AGAUR 2005/SGR/920, CibeRes 06/06/0036.
Conflicts of interest
The authors declare no conflict of interest regarding the present manuscript.
Author information
Authors and Affiliations
- Critical Care Centre, Coporació Sanitaria Parc Tauli, Sabadell, Spain
Ignacio Martin-Loeches - Institut Universitari UAB, Barcelona, Spain
Ignacio Martin-Loeches - Critical Care Department, Mater Misericordiae University Hospital, Dublin, Ireland
Ignacio Martin-Loeches & Brian Marsh - Department of Anesthesiology and Critical Care Medicine, Charité Medical Center, Campus Virchow-Clinic, Augustenburger Platz 1, 13353, Berlin, Germany
Maria Deja - Critical Care Department, University Hospital Attikon, Rimini 1, 12462, Haidari, Athens, Greece
Despoina Koulenti - Department of Critical Care Medicine, University Hospital ATTIKON, Medical School, University of Athens, Athens, Greece
George Dimopoulos - Pneumology Department, Hospital Clinic, Barcelona, Spain
Antonio Torres - Department of Medicine, Winthrop-University Hospital, 222 Station Plaza N., Suite 509, Mineola, NY, 11501, USA
Michael S. Niederman - Critical Care Department, Hospital Vall d’Hebron, Barcelona, Spain
Jordi Rello - Vall d’ Hebron Research Institute (VHIR), Barcelona, Spain
Jordi Rello - Universitat Autónoma de Barcelona, Barcelona, Spain
Jordi Rello - CIBERES, Barcelona, Spain
Ignacio Martin-Loeches, Antonio Torres & Jordi Rello
Authors
- Ignacio Martin-Loeches
- Maria Deja
- Despoina Koulenti
- George Dimopoulos
- Brian Marsh
- Antonio Torres
- Michael S. Niederman
- Jordi Rello
Consortia
EU-VAP Study Investigators
Corresponding author
Correspondence toJordi Rello.
Additional information
EU-VAP Study Investigators working group are listed in the "Appendix".
This article is discussed in the editorial available at: doi:10.1007/s00134-012-2811-x.
EU-VAP/CAP Study was endorsed by the European Critical Care Research Network (ECCRN) of the European Society of Intensive Care Medicine (ESICM).
Appendix: EU-VAP/CAP Study
Appendix: EU-VAP/CAP Study
Principal Investigator: Jordi Rello
Study Co-ordinator: Despoina Koulenti
Βelgium
National Co-ordinator (NC): Jan DeWaele
- Ghent Univ. Hospital, Ghent, Belgium: Jan DeWaele and Stijn Blot
- St Jan Hospital, Brugges, Belgium: Marc Nauwynck
France
NC: Christian Brun-Buisson
- Henri-Mondor Univ. Hospital, Paris, France: Christian Brun-Buisson
- Raymond Poincaré Univ. Hospital, Garches, France: Djilali Annane
- Nord Univ. Hospital, Marseille, France: Claude Martin
- Sainte-Marguerite Univ. Hospital, Marseille, France: Laurent Papazian
- Bichat-Claude-Bernard Univ. Hospital, Paris, France: Bernard Regnier
Germany
NC: Wolfgang Krueger
- Tuebingen Univ. Hospital, Tuebingen, Germany: Wolfgang Krueger
- Bonn Univ. Hospital, Bonn, Germany: Christian Putensen and Hermann Wrigge
- Charite Univ. Hospital, Berlin, Germany: Maria Deja
Greece
NC: Despoina Koulenti and Apostolos Armaganidis
- Attikon Univ. Hospital, Athens, Greece: Apostolos Armaganidis
- Sotiria General Hospital, Athens, Greece: George Dimopoulos
- KAT Hospital, Athens, Greece: Pavlos Myrianthefs
- Larisa General Hospital, Larisa, Greece: Apostolos Komnos
Italy
NC: Antonio Macor (Amedeo di Savoia Hospital, Torino, Italy)
- Maria Vittoria Hospital, Torino, Italy: Emilpaolo Manno
- Cardinal Massaia Hospital, Asti, Italy: Silvano Cardellino
- Mauriziano Umberto I Hospital, Torino, Italy: Giuseppe Spina
Ireland
NC: Ignacio Martin-Loeches
- Mater Misericordiae Univ. Hospital, Dublin, Ireland: Ignacio Martin-Loeches & Brian Marsh
Portugal
NC: Antonio Carneiro
- Santo Antonio Hospital, Porto, Portugal: Antonio Carneiro
Spain
NC: Jordi Rello
- Joan XXIII Univ. Hospital, Tarragona, Spain (UCI1): Jordi Rello
- Joan XXIII Univ. Hospital, Tarragona, Spain (UCI2): Emili Diaz
- Bellvitge Univ. Hospital, Barcelona, Spain: Rafael Mañez
- Dr Negrin Univ. Hospital, Gran Canarias, Spain: Jordi Sole-Violan
- Virgen de Rocio Univ. Hospital, Seville, Spain (ICU1): Jose Garnacho-Montero
- Virgen de Rocio Univ. Hospital, Seville, Spain (ICU2): Rosario Amaya-Villar
Turkey
NC: Arzu Topeli
- Hacettepe Univ. Hospital, Ankara, Turkey: Arzu Topeli
- Erciyes Univ. Hospital, Kayseri, Turkey: Muhammet Guven
EU-VAP/CAP Study Group: Djilali Annane (Raymond Poincaré Univ. Hospital, Garches, France), Rosario Amaya-Villar (Virgen de Rocio Univ. Hospital, Seville, Spain), Apostolos Armaganidis (Attikon Univ. Hospital, Athens, Greece), Stijn Blot (Ghent Univ. Hospital, Ghent, Belgium), Christian Brun-Buisson (Henri-Mondor Univ. Hospital, Paris, France), Antonio Carneiro (Santo Antonio Hospital, Porto, Portugal), Maria Deja (Charite Univ. Hospital, Berlin, Germany), Jan DeWaele (Ghent Univ. Hospital, Ghent, Belgium), Emili Diaz (Joan XIII Univ. Hospital, Tarragona, Spain), George Dimopoulos (Attikon Univ. Hospital and Sotiria Hospital, Athens, Greece), Silvano Cardellino (Cardinal Massaia Hospital, Asti, Italy), Jose Garnacho-Montero (Virgen de Rocio Univ. Hospital, Seville, Spain), Muhammet Guven (Erciyes Univ. Hospital, Kayseri, Turkey), Apostolos Komnos (Larisa Hospital, Larisa, Greece), Despona Koulenti (Attikon Univ. Hospital, Athens, Greece and Rovira i Virgili University, Tarragona, Spain), Wolfgang Krueger (Tuebingen Univ. Hospital, Tuebingen, Germany and Constance Hospital, Constance, Germany), Thiago Lisboa (Joan XIII Univ. Hospital, Tarragona, Spain and CIBER Enfermedades Respiratorias), Antonio Macor (Amedeo di Savoia Hospital, Torino, Italy), Emilpaolo Manno (Maria Vittoria Hospital, Torino, Italy), Rafael Mañez (Bellvitge Univ. Hospital, Barcelona, Spain), Brian Marsh (Mater Misericordiae Univ. Hospital, Dublin, Ireland), Claude Martin (Nord Univ. Hospital, Marseille, France), Ignacio Martin-Loeches (Mater Misericordiae Univ. Hospital, Dublin, Ireland and Corporacio Sanitaria Parc Tauli, Sabadell, Spain), Pavlos Myrianthefs (KAT Hospital, Athens, Greece), Marc Nauwynck (St Jan Hospital, Brugges, Belgium), Laurent Papazian (Sainte-Marguerite Univ. Hospital, Marseille, France), Christian Putensen (Bonn Univ. Hospital, Bonn, Germany), Bernard Regnier (Claude Bernard Univ. Hospital, Paris, France), Jordi Rello (Joan XIII Univ. Hospital, Tarragona, Spain and Vall d’Hebron University Hospital, Spain), Jordi Sole-Violan (Dr Negrin Univ. Hospital, Gran Canarias, Spain), Giuseppe Spina (Mauriziano Umberto I Hospital, Torino, Italy), Arzu Topeli (Hacettepe Univ. Hospital, Ankara, Turkey), Hermann Wrigge (Bonn Univ. Hospital, Bonn, Germany).
Rights and permissions
About this article
Cite this article
Martin-Loeches, I., Deja, M., Koulenti, D. et al. Potentially resistant microorganisms in intubated patients with hospital-acquired pneumonia: the interaction of ecology, shock and risk factors.Intensive Care Med 39, 672–681 (2013). https://doi.org/10.1007/s00134-012-2808-5
- Received: 08 June 2012
- Accepted: 22 October 2012
- Published: 29 January 2013
- Issue date: April 2013
- DOI: https://doi.org/10.1007/s00134-012-2808-5