Prophylactic esophagectomy in Barrett esophagus with high-grade dysplasia (original) (raw)
- 87 Accesses
- 14 Citations
- Explore all metrics
Abstract
Objectives
We review the significance of Barrett mucosa with high-grade dysplasia, management options, rationale for prophylactic esophagectomy, and results of surgical treatment.
Patients and methods
The surgical results of prophylactic esophagectomy are presented from two previous studies, involving 60 patients over 1982–2001 at a single institution. These results are compared with nonsurgical treatment options.
Results
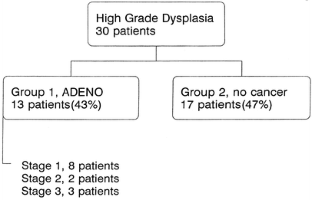
The transhiatal esophagectomy technique was the most commonly used surgical approach (81.7% of patients). Operative mortality was 1.7%. The incidence of occult adenocarcinoma for 1982–1994 and 1994–2001 was 43% and 16.7%, respectively. The overall incidence of occult adenocarcinoma for the entire study period was 30%.
Conclusions
Prophylactic esophagectomy for patients with Barrett esophagus and high-grade dysplasia, performed at a center of high volume and experience, can be accomplished with low mortality and excellent long-term survival. Incidence of occult adenocarcinoma is decreasing, but still 16.7–30%.
Access this article
Subscribe and save
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime Subscribe now
Buy Now
Price excludes VAT (USA)
Tax calculation will be finalised during checkout.
Instant access to the full article PDF.
Fig. 1.
Similar content being viewed by others
Esophagectomy
Chapter © 2024
References
- Bolton JS, Wu TT, Yeo CJ, Cameron JL, Heitmiller RF (2001) Esophagectomy for adenocarcinoma in patients 45 years of age or younger. J Gastrointest Surg 32:447–454
Google Scholar - Miros M, Kerlin P, Walker N (1991) Only patients with dysplasia progress to adenocarcinoma in Barrett's oesophagus. Gut 32:1441
CAS PubMed Google Scholar - Hameeteman W, Tygat GNJ, Houtoff HJ, et al (1989) Barrett's esophagus: development of dysplasia and adenocarcinoma. Gastroenterology 96:1249–1256
CAS PubMed Google Scholar - Weston AP, Badr AS, Hassanein RS (1999) Prospective multivariate analysis of clinical, endoscopic, and histological factors predictive of the development of Barrett's multifocal high-grade dysplasia or adenocarcinoma. Am J Gastroenterol 94:3413–3419
Google Scholar - O'Connor JB, Falk GW, Richter JE (1999) The incidence of adenocarcinoma and dysplasia in Barrett's esophagus: report on the Cleveland Clinic Barrett's Esophagus Registry. Am J Gastroenterol 94:2037–2042
Google Scholar - Tygat GNJ, Hameeteman W (1992) The neoplastic potential of columnar-lined (Barrett's) esophagus. World J Surg 16:308–312
PubMed Google Scholar - Pera M, Trastek VF, Carpenter HA, et al (1992) Barrett's esophagus with high-grade dysplasia: an indication for esophagectomy? Ann Thorac Surg 54:199–204
CAS PubMed Google Scholar - Heitmiller RF (1995) Esophageal tumors. In: Cameron JL (ed.) Current surgical therapy, 5th edn. Mosby, St Louis, p 45
- Moskaluk CA, Heitmiller RF, Zuharhak M, et al (1996) p53 and p21 WAF1/C1P1/SD11 gene products in Barrett esophagus and adenocarcinoma of the esophagus and esophagogastric junction. Hum Pathol 27:1211
CAS PubMed Google Scholar - Wu TT, Watanabe T, Heitmiller RF, et al (1998) Genetic alterations in Barrett esophagus and adenocarcinoma of the esophagus and esophagogastric junction region. Am J Pathol 153:287
CAS PubMed Google Scholar - Hamilton SR, Smith RRL (1987) The relationship between columnar epithelial dysplasia and invasive adenocarcinoma arising in Barrett's esophagus. Am J Clin Pathol 87:301–312
CAS PubMed Google Scholar - Hamilton SR, Smith RRL (1984) Epithelial dysplasia in Barrett esophagus: relationship to invasive carcinoma. Gastroenterology 86:1105
Google Scholar - Reid BJ, Haggitt RC, Rubin CE, et al (1988) Observer variation in the diagnosis of dysplasia in Barrett' esophagus. Hum Pathol 19:166–178
Google Scholar - DeMeester TR (2002) Surgical therapy for Barrett's esophagus: prevention, protection, and excision. Dis Esophagus 15:109–116
Article CAS PubMed Google Scholar - Heitmiller RF (1999) Closed chest esophageal resection. Oper Techn Thorac Cardiovasc Surg 4:252–265
Google Scholar - Stone CD, Heitmiller RF (1994) Simplified, standardized technique for cervical esophagogastric anastomosis. Ann Thorac Surg 58:259–261
CAS PubMed Google Scholar - Zehr KJ, Dawson PB, Yang SC, Heitmiller RF (1998) Implementation of standardized clinical care pathways for major general thoracic cases reduces hospital costs and length of stay. Ann Thorac Surg 66:914–919
CAS PubMed Google Scholar - Heitmiller RF, Redmond M, Hamilton SR (1996) Barrett's esophagus with high-grade dysplasia. An indication for prophylactic esophagectomy. Ann Surg 224:66–71
CAS PubMed Google Scholar - Tseng EE, Wu TT, Yeo CJ, Heitmiller RF (2003) Barrett's esophagus with high grade dysplasia: surgical results and long-term outcome—an update. J Gastrointest Surg (in press)
Google Scholar - Schnell TG, Sontag SJ, Chejfec G, Aranha G, Metz A, O'Connell S, Seidel UJ, Sonnenberg A (2001) Long-term nonsurgical management of Barrett's esophagus with high-grade dysplasia. Gastroenterology 120:1607–1619
CAS PubMed Google Scholar
Author information
Authors and Affiliations
- Department of Surgery, Union Memorial Hospital, 3333 N. Calvert Street, Baltimore, MD 21218, USA
Richard F. Heitmiller
Authors
- Richard F. Heitmiller
You can also search for this author inPubMed Google Scholar
Corresponding author
Correspondence toRichard F. Heitmiller.
Rights and permissions
About this article
Cite this article
Heitmiller, R.F. Prophylactic esophagectomy in Barrett esophagus with high-grade dysplasia.Langenbecks Arch Surg 388, 83–87 (2003). https://doi.org/10.1007/s00423-002-0343-5
- Received: 29 November 2002
- Accepted: 29 November 2002
- Published: 20 February 2003
- Issue Date: April 2003
- DOI: https://doi.org/10.1007/s00423-002-0343-5


