Detection of Intestinal Metaplasia After Successful Eradication of Barrett’s Esophagus with Radiofrequency Ablation (original) (raw)
Abstract
Background
Radiofrequency ablation (RFA) is an effective means of eradicating Barrett’s esophagus (BE), both with and without associated dysplasia. Several studies have documented high initial success rates with RFA. However, there is limited data on IM detection rates after eradication.
Aims
To determine the rate of detection of intestinal metaplasia (IM) after successful eradication of Barrett’s esophagus.
Methods
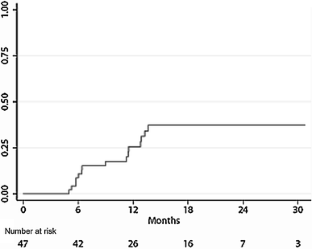
BE patients with and without dysplasia who had undergone RFA were retrospectively identified. Only those who had complete eradication as documented on the initial post-ablation endoscopy, and had minimum two surveillance endoscopies, were included in the analyses. Clinical, demographic, and endoscopic data were collected. Cumulative incidence of IM detection was calculated by the Kaplan–Meier method.
Results
Forty-seven patients underwent RFA and had complete eradication of Barrett’s epithelium. The majority of patients were male (76.6%), and the mean age was 64.2 years. The cumulative incidence of newly detected IM at 1 year was 25.9% (95% CI 15.1–42.1%). Dysplasia was detected at the time of recurrence in four patients, and all cases were detected at the GE junction in the absence of visible BE. Patients with recurrent IM had longer baseline segments of BE (median, 4 cm vs. 2 cm, p = 0.03).
Conclusions
The rate of detection of new IM is high in patients who have undergone successful eradication of BE by RFA. Additionally, dysplasia can recur at the GE junction in the absence of visible BE. Future studies are warranted to identify those patients at increased risk for the development of recurrent intestinal metaplasia.
Access this article
Subscribe and save
- Starting from 10 chapters or articles per month
- Access and download chapters and articles from more than 300k books and 2,500 journals
- Cancel anytime View plans
Buy Now
Price excludes VAT (USA)
Tax calculation will be finalised during checkout.
Instant access to the full article PDF.
Fig. 1
References
- Ronkainen J, Aro P, Storskrubb T, et al. Prevalence of Barrett’s esophagus in the general population: an endoscopic study. Gastroenterology. 2005;129:1825–1831.
Article PubMed Google Scholar - Hayeck TJ, Kong CY, Spechler SJ, Gazelle GS, Hur C. The prevalence of Barrett’s esophagus in the US: estimates from a simulation model confirmed by SEER data. Dis Esophagus. 2010;23:451–457.
Article PubMed CAS Google Scholar - Rex DK, Cummings OW, Shaw M, et al. Screening for Barrett’s esophagus in colonoscopy patients with and without heartburn. Gastroenterology. 2003;125:1670–1677.
Article PubMed Google Scholar - Shaheen NJ, Richter JE. Barrett’s oesophagus. Lancet. 2009;373:850–861.
Article PubMed CAS Google Scholar - Sharma P, Falk GW, Weston AP, Reker D, Johnston M, Sampliner RE. Dysplasia and cancer in a large multicenter cohort of patients with Barrett’s esophagus. Clin Gastroenterol Hepatol. 2006;4:566–572.
Article PubMed Google Scholar - Shaheen NJ, Sharma P, Overholt BF, et al. Radiofrequency ablation in Barrett’s esophagus with dysplasia. N Engl J Med. 2009;360:2277–2288.
Article PubMed CAS Google Scholar - Harrison R, Perry I, Haddadin W, et al. Detection of intestinal metaplasia in Barrett’s esophagus: an observational comparator study suggests the need for a minimum of eight biopsies. Am J Gastroenterol. 2007;102:1154–1161.
Article PubMed Google Scholar - Gondrie JJ, Pouw RE, Sondermeijer CM, et al. Effective treatment of early Barrett’s neoplasia with stepwise circumferential and focal ablation using the HALO system. Endoscopy. 2008;40:370–379.
Article PubMed CAS Google Scholar - Fleischer DE, Overholt BF, Sharma VK, et al. Endoscopic ablation of Barrett’s esophagus: a multicenter study with 2.5-year follow-up. Gastrointest Endosc. 2008;68:867–76.
Google Scholar - Fleischer DE, Overholt BF, Sharma VK, et al. Endoscopic radiofrequency ablation for Barrett’s esophagus: 5-year outcomes from a prospective multicenter trial. Endoscopy. 2010;42:781–789.
Article PubMed CAS Google Scholar - Halsey KD, Chang JW, Greenwald BD. Recurrent disease following endoscopic ablation of Barrett’s neoplasia. Gastroenterology. 2010;138:S17.
Google Scholar - Shaheen NJ, Fleischer DE, Eisen GM, et al. Durability of epithelial reversion after radiofrequency ablation: follow-up of the AIM Dysplasia Trial. Gastroenterology. 2010;138:S16.
Google Scholar - Pech O, Behrens A, May A, et al. Long-term results and risk factor analysis for recurrence after curative endoscopic therapy in 349 patients with high-grade intraepithelial neoplasia and mucosal adenocarcinoma in Barrett’s oesophagus. Gut. 2008;57:1200–1206.
Article PubMed CAS Google Scholar
Acknowledgments
Dr. Abrams is supported in part by a K07 award from the National Cancer Institute (CA132892) and by a Louis V. Gerster, Jr. Scholar Award. Mr. Vaccaro was supported by the Digestive Disease Research Foundation.
Disclosures
Dr. Lightdale has received research support from Barrx Medical, a royalty from Cook, Inc., and consulting fees from Olympus and Oncoscope.
Author information
Authors and Affiliations
- Department of Medicine, Columbia University Medical Center, New York, NY, USA
Benjamin J. Vaccaro, Susana Gonzalez, John M. Poneros, Peter D. Stevens, Kristina M. Capiak, Charles J. Lightdale & Julian A. Abrams - Herbert Irving Comprehensive Cancer Center, Columbia University, New York, NY, USA
Charles J. Lightdale & Julian A. Abrams - 622 W. 168th Street, PH 20-303, New York, NY, 10032, USA
Julian A. Abrams
Authors
- Benjamin J. Vaccaro
- Susana Gonzalez
- John M. Poneros
- Peter D. Stevens
- Kristina M. Capiak
- Charles J. Lightdale
- Julian A. Abrams
Corresponding author
Correspondence toJulian A. Abrams.
Rights and permissions
About this article
Cite this article
Vaccaro, B.J., Gonzalez, S., Poneros, J.M. et al. Detection of Intestinal Metaplasia After Successful Eradication of Barrett’s Esophagus with Radiofrequency Ablation.Dig Dis Sci 56, 1996–2000 (2011). https://doi.org/10.1007/s10620-011-1680-4
- Received: 27 October 2010
- Accepted: 11 March 2011
- Published: 06 April 2011
- Issue date: July 2011
- DOI: https://doi.org/10.1007/s10620-011-1680-4