Medication Review and Enhanced Information Transfer at Discharge of Older Patients with Polypharmacy: a Cluster-Randomized Controlled Trial in Swiss Hospitals (original) (raw)
Abstract
Background
Medication safety in patients with polypharmacy at transitions of care is a focus of the current Third WHO Global Patient Safety Challenge. Medication review and communication between health care professionals are key targets to reduce medication-related harm.
Objective
To study whether a hospital discharge intervention combining medication review with enhanced information transfer between hospital and primary care physicians can delay hospital readmission and impact health care utilization or other health-related outcomes of older inpatients with polypharmacy.
Design
Cluster-randomized controlled trial in 21 Swiss hospitals between January 2019 and September 2020, with 6 months follow-up.
Participants
Sixty-eight senior physicians and their blinded junior physicians included 609 patients ≥ 60 years taking ≥ 5 drugs.
Interventions
Participating hospitals were randomized to either integrate a checklist-guided medication review and communication stimulus into their discharge processes, or follow usual discharge routines.
Main Measures
Primary outcome was time-to-first-readmission to any hospital within 6 months, analyzed using a shared frailty model. Secondary outcomes covered readmission rates, emergency department visits, other medical consultations, mortality, drug numbers, proportions of patients with potentially inappropriate medication, and the patients’ quality of life.
Key Results
At admission, 609 patients (mean age 77.5 (SD 8.6) years, 49.4% female) took a mean of 9.6 (4.2) drugs per patient. Time-to-first-readmission did not differ significantly between study arms (adjusted hazard ratio 1.14 (intervention vs. control arm), 95% CI [0.75–1.71], p = 0.54), nor did the 30-day hospital readmission rates (6.7% [3.3–10.1%] vs. 7.0% [3.6–10.3%]). Overall, there were no clinically relevant differences between study arms at 1, 3, and 6 months after discharge.
Conclusions
The combination of a structured medication review with enhanced information transfer neither delayed hospital readmission nor improved other health-related outcomes of older inpatients with polypharmacy. Our results may help researchers in balancing practicality versus stringency of similar hospital discharge interventions.
Study Registration
ISRCTN18427377, https://doi.org/10.1186/ISRCTN18427377
Similar content being viewed by others
INTRODUCTION
Polypharmacy and inappropriate medication prescribing are major risk factors for adverse drug events, drug interactions, intake errors, and low medication adherence,[1](#ref-CR1 "Chiatti C, Bustacchini S, Furneri G, et al. The economic burden of inappropriate drug prescribing, lack of adherence and compliance, adverse drug events in older people: a systematic review. Drug Saf. 2012;35 Suppl 1:73-87. https://doi.org/10.1007/BF03319105
."),[2](#ref-CR2 "Field TS, Mazor KM, Briesacher B, Debellis KR, Gurwitz JH. Adverse drug events resulting from patient errors in older adults. J Am Geriatr Soc. 2007;55(2):271-6.
https://doi.org/10.1111/j.1532-5415.2007.01047.x
."),[3](/article/10.1007/s11606-022-07728-6#ref-CR3 "Maher RL, Hanlon J, Hajjar ER. Clinical consequences of polypharmacy in elderly. Expert Opin Drug Saf. 2014;13(1):57-65.
https://doi.org/10.1517/14740338.2013.827660
.") thereby increasing morbidity, hospitalization rates, costs, and mortality in multimorbid older patients.[1](/article/10.1007/s11606-022-07728-6#ref-CR1 "Chiatti C, Bustacchini S, Furneri G, et al. The economic burden of inappropriate drug prescribing, lack of adherence and compliance, adverse drug events in older people: a systematic review. Drug Saf. 2012;35 Suppl 1:73-87.
https://doi.org/10.1007/BF03319105
."),[4](/article/10.1007/s11606-022-07728-6#ref-CR4 "Frazier SC. Health outcomes and polypharmacy in elderly individuals: an integrated literature review. J Gerontol Nurs. 2005;31(9):4-11."),[5](/article/10.1007/s11606-022-07728-6#ref-CR5 "Lau DT, Kasper JD, Potter DE, Lyles A, Bennett RG. Hospitalization and death associated with potentially inappropriate medication prescriptions among elderly nursing home residents. Arch Intern Med. 2005;165(1):68-74.
https://doi.org/10.1001/archinte.165.1.68
.") Recognizing the rising prevalence of polypharmacy,[6](/article/10.1007/s11606-022-07728-6#ref-CR6 "Guthrie B, Makubate B, Hernandez-Santiago V, Dreischulte T. The rising tide of polypharmacy and drug-drug interactions: population database analysis 1995-2010. BMC Med. 2015;13:74.
https://doi.org/10.1186/s12916-015-0322-7
.") national authorities and the WHO advocate deprescribing of inappropriate medications to reduce medication-related harm.[7](#ref-CR7 "Clyne W, Alison B, Seal R. A Guide to Medication Review 2008. The National Prescribing Centre; 2008."),[8](#ref-CR8 "Donaldson LJ, Kelley ET, Dhingra-Kumar N, Kieny MP, Sheikh A. Medication without harm: WHO’s third global patient safety challenge. Lancet. 2017;389(10080):1680-1.
https://doi.org/10.1016/s0140-6736(17)31047-4
."),[9](#ref-CR9 "Leitliniengruppe Hessen. Hausärztliche Leitlinie Multimedikation. 1.09 ed: Deutsche Gesellschaft für Allgemeinmedizin und Familienmedizin DEGAM; 2013."),[10](#ref-CR10 "National Institute for Health and Care Excellence. Medicines Optimisation: the safe and effective use of medicines to enable the best possible outcomes (NICE guideline NG5); 2015.
https://www.nice.org.uk/guidance/ng5
."),[11](/article/10.1007/s11606-022-07728-6#ref-CR11 "Scottish Government Model of Care Polypharmacy Working Group. Polypharmacy Guidance. 2nd Edition ed: Scottish Government; 2015.")Medication errors frequently occur at the interface between hospital-based and primary care,[12](/article/10.1007/s11606-022-07728-6#ref-CR12 "Parekh N, Ali K, Page A, Roper T, Rajkumar C. Incidence of medication-related harm in older adults after hospital discharge: a systematic review. J Am Geriatr Soc. 2018;66(9):1812-22. https://doi.org/10.1111/jgs.15419
."),[13](/article/10.1007/s11606-022-07728-6#ref-CR13 "Pérez T, Moriarty F, Wallace E, McDowell R, Redmond P, Fahey T. Prevalence of potentially inappropriate prescribing in older people in primary care and its association with hospital admission: longitudinal study. BMJ. 2018;363:k4524.
https://doi.org/10.1136/bmj.k4524
.") due to increased polypharmacy during hospitalization[14](/article/10.1007/s11606-022-07728-6#ref-CR14 "Nobili A, Licata G, Salerno F, et al. Polypharmacy, length of hospital stay, and in-hospital mortality among elderly patients in internal medicine wards. The REPOSI study. Eur J Clin Pharmacol. 2011;67(5):507-19.
https://doi.org/10.1007/s00228-010-0977-0
.") and communication deficits between hospital physicians (HPs) and primary care physicians (PCPs). In Switzerland, PCPs do not retain responsibility for the treatment of their hospitalized patients. Even when hospital treatment is delivered by independent specialists, and also in rehabilitation hospitals, general care is provided by HPs. When PCPs resume care after discharge, they are usually provided with a provisional discharge letter without reasons for medication changes, in which case they may tend to revert to the preadmission medication.[15](/article/10.1007/s11606-022-07728-6#ref-CR15 "Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007a;297(8):831-41.
https://doi.org/10.1001/jama.297.8.831
.")Recent studies have shown that in-hospital medication reconciliation and review have the potential to reduce inappropriate prescribing and medication-related harm, but they alone seem insufficient to lastingly reduce polypharmacy and affect hard clinical outcomes.[16](#ref-CR16 "Christensen M, Lundh A. Medication review in hospitalised patients to reduce morbidity and mortality. Cochrane Database Syst Rev. 2016;2(2):Cd008986. https://doi.org/10.1002/14651858.CD008986.pub3
."),[17](#ref-CR17 "Gillespie U, Alassaad A, Henrohn D, et al. A comprehensive pharmacist intervention to reduce morbidity in patients 80 years or older: a randomized controlled trial. Arch Intern Med. 2009;169(9):894-900.
https://doi.org/10.1001/archinternmed.2009.71
."),[18](#ref-CR18 "Ravn-Nielsen LV, Duckert ML, Lund ML, et al. Effect of an in-hospital multifaceted clinical pharmacist intervention on the risk of readmission: a randomized clinical trial. JAMA Intern Med. 2018;178(3):375-82.
https://doi.org/10.1001/jamainternmed.2017.8274
."),[19](#ref-CR19 "Kempen TGH, Bertilsson M, Hadziosmanovic N, et al. Effects of hospital-based comprehensive medication reviews including postdischarge follow-up on older patients’ use of health care: a cluster randomized clinical trial. JAMA Netw Open. 2021;4(4):e216303.
https://doi.org/10.1001/jamanetworkopen.2021.6303
."),[20](#ref-CR20 "Graabaek T, Kjeldsen LJ. Medication reviews by clinical pharmacists at hospitals lead to improved patient outcomes: a systematic review. Basic Clin Pharmacol Toxicol. 2013;112(6):359-73.
https://doi.org/10.1111/bcpt.12062
."),[21](/article/10.1007/s11606-022-07728-6#ref-CR21 "Silva ROS, Macêdo LA, Santos GADJ, Aguiar PM, de Lyra DPJ. Pharmacist-participated medication review in different practice settings: Service or intervention? An overview of systematic reviews. PLoS ONE. 2019;14(1):e0210312.
https://doi.org/10.1371/journal.pone.0210312
.") Although some complex, multi-component interventions that included discharge planning and outpatient follow-up resulted in lower readmission rates,[17](/article/10.1007/s11606-022-07728-6#ref-CR17 "Gillespie U, Alassaad A, Henrohn D, et al. A comprehensive pharmacist intervention to reduce morbidity in patients 80 years or older: a randomized controlled trial. Arch Intern Med. 2009;169(9):894-900.
https://doi.org/10.1001/archinternmed.2009.71
."),[18](/article/10.1007/s11606-022-07728-6#ref-CR18 "Ravn-Nielsen LV, Duckert ML, Lund ML, et al. Effect of an in-hospital multifaceted clinical pharmacist intervention on the risk of readmission: a randomized clinical trial. JAMA Intern Med. 2018;178(3):375-82.
https://doi.org/10.1001/jamainternmed.2017.8274
.") others did not,[19](#ref-CR19 "Kempen TGH, Bertilsson M, Hadziosmanovic N, et al. Effects of hospital-based comprehensive medication reviews including postdischarge follow-up on older patients’ use of health care: a cluster randomized clinical trial. JAMA Netw Open. 2021;4(4):e216303.
https://doi.org/10.1001/jamanetworkopen.2021.6303
."),[20](#ref-CR20 "Graabaek T, Kjeldsen LJ. Medication reviews by clinical pharmacists at hospitals lead to improved patient outcomes: a systematic review. Basic Clin Pharmacol Toxicol. 2013;112(6):359-73.
https://doi.org/10.1111/bcpt.12062
."),[21](/article/10.1007/s11606-022-07728-6#ref-CR21 "Silva ROS, Macêdo LA, Santos GADJ, Aguiar PM, de Lyra DPJ. Pharmacist-participated medication review in different practice settings: Service or intervention? An overview of systematic reviews. PLoS ONE. 2019;14(1):e0210312.
https://doi.org/10.1371/journal.pone.0210312
.") and it remains unclear how to design an optimal discharge process aimed at minimizing readmission rates or emergency department (ED) visits.[22](/article/10.1007/s11606-022-07728-6#ref-CR22 "Kripalani S, Theobald CN, Anctil B, Vasilevskis EE. Reducing hospital readmission rates: current strategies and future directions. Annu Rev Med. 2014;65:471-85.
https://doi.org/10.1146/annurev-med-022613-090415
."),[23](/article/10.1007/s11606-022-07728-6#ref-CR23 "O’Mahony D. Optimization of medication by pharmacists in older people with multimorbidity for improved outcomes-mirage or reality? JAMA Netw Open. 2021;4(4):e216392.
https://doi.org/10.1001/jamanetworkopen.2021.6392
.")In this pragmatic study, we combined medication deprescribing at discharge with a communication stimulus between HPs and the patients’ PCPs. Our intent was to synthesize a minimal but sufficient subset of core components of existing discharge frameworks and best practice recommendations[24](#ref-CR24 "Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150(3):178-87. https://doi.org/10.7326/0003-4819-150-3-200902030-00007
."),[25](#ref-CR25 "Kripalani S, Jackson AT, Schnipper JL, Coleman EA. Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. 2007b;2(5):314-23.
https://doi.org/10.1002/jhm.228
."),[26](/article/10.1007/s11606-022-07728-6#ref-CR26 "Soong C, Daub S, Lee J, et al. Development of a checklist of safe discharge practices for hospital patients. J Hosp Med. 2013;8(8):444-9.
https://doi.org/10.1002/jhm.2032
.") into a discharge procedure that could be flexibly adopted by different hospitals. Medication safety and communication were identified as a promising tandem, based on the rationale that better HP-PCP communication would foster consensus on appropriate discharge medication, and thereby lead to better anchored and longer-lasting maintenance of the optimized medication.[27](/article/10.1007/s11606-022-07728-6#ref-CR27 "Anthierens S, Tansens A, Petrovic M, Christiaens T. Qualitative insights into general practitioners views on polypharmacy. BMC Fam Pract. 2010;11:65.
https://doi.org/10.1186/1471-2296-11-65
.")The aim of this study was to evaluate whether such an approach reduces readmission rates of older inpatients with polypharmacy, compared to usual care, and whether it improves other health-related outcomes. Additional objectives addressed implementation issues, and related results have been published.[28](/article/10.1007/s11606-022-07728-6#ref-CR28 "Rachamin Y, Grischott T, Neuner-Jehle S. Implementation of a complex intervention to improve hospital discharge: process evaluation of a cluster randomised controlled trial. BMJ Open. 2021;11(5):e049872. https://doi.org/10.1136/bmjopen-2021-049872
.")METHODS
The study was designed as an effectiveness-implementation hybrid trial set in hospitals in German-speaking Switzerland.[29](/article/10.1007/s11606-022-07728-6#ref-CR29 "Grischott T, Zechmann S, Rachamin Y, et al. Improving inappropriate medication and information transfer at hospital discharge: study protocol for a cluster RCT. Implement Sci. 2018;13(1):155. https://doi.org/10.1186/s13012-018-0839-1
.") Ethics approval was granted by the Ethics Committees Zurich and Bern, Switzerland (BASEC2018-00215). Here we present the effectiveness outcomes of this prospective, double-blind, cluster-randomized parallel-controlled trial following up hospitalized older patients with polypharmacy for 6 months after discharge.Recruitment, Allocation, and Patient Inclusion
In three waves (July 2018–October 2019), 165 medical decision-makers of all 141 non-psychiatric and non-pediatric hospitals in German-speaking Switzerland were contacted by postal mail. Ultimately, 21 hospitals chose to participate (with their internal medicine and/or geriatric wards) of which two were allocated as pilot hospitals to the intervention arm. Using blockwise covariate-constrained randomization[30](/article/10.1007/s11606-022-07728-6#ref-CR30 "Grischott T. The Shiny Balancer - Software and imbalance criteria for optimally balanced treatment allocation in small RCTs and cRCTs. BMC Med Res Methodol. 2018;18(108). https://doi.org/10.1186/s12874-018-0551-5
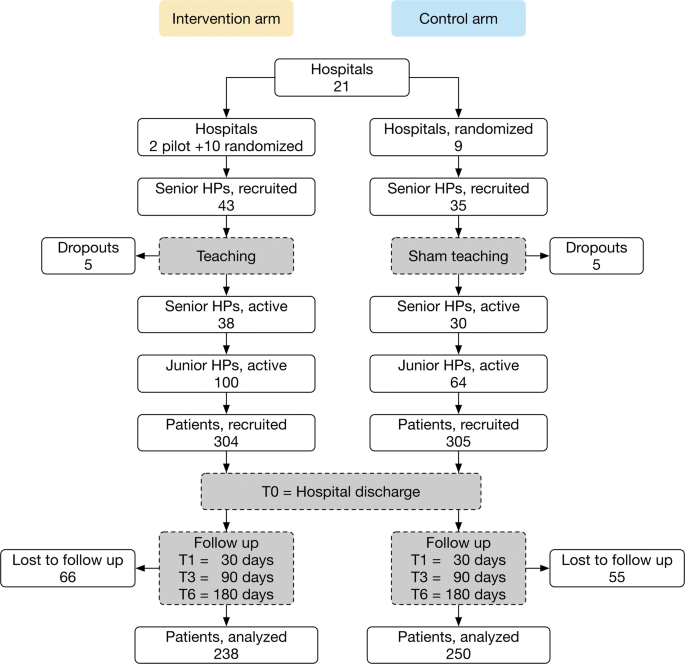
.") (eMethods 1), the remaining 19 were 1:1 randomized to either intervention or control arm (February–November 2019).January 2019–June 2020, 78 senior HPs (attending physicians), appointed by their superiors and consenting in writing to participate (without remuneration), were either instructed about the study intervention and data collection (intervention arm) or data collection alone (control arm). Several senior HPs withdrew from participation when the COVID-19 pandemic delayed the study in spring 2020. Finally, 38 senior HPs actively participated in the intervention and 30 in the control arm (Fig. 1). Their junior HPs (residents) were informed that their hospitals aimed to evaluate and improve discharge procedures, and thus remained blinded to treatment allocation. All participating junior HPs entered a raffle with a 1/10 chance of winning CHF 500 (USD 520).
Figure 1
CONSORT diagram of the study design and participant flow. Abbreviation: HP, hospital physician.
January 2019–September 2020, both junior and senior HPs recruited patients. To minimize selection bias, HPs were asked to approach all eligible patients whenever feasible. Inclusion criteria were (1) in-hospital patient at the time of inclusion, (2) aged ≥ 60 years with ≥ 5 drugs prescribed (including “as needed” medication), and (3) written informed consent or consent from a legal representative. Patients were excluded in case of (1) end-stage disease with life expectancy < 3 months, or (2) cognitive inability to follow study procedures even with assistance. Patients were secondarily excluded when later transferred to another hospital or where medical care was otherwise not provided by a PCP. Readmitted study patients were acceptable as new index patients; however, this situation never occurred.
Soon after patient recruitment started, it became obvious that COVID-19 would drastically impact HP workload and recruitment success in virtually all participating hospitals. An ad hoc interim analysis revealed smaller-than expected clusters, a very low within-cluster correlation, and a relatively high fraction of censored data due to unexpectedly low baseline readmission rates, suggesting that our study would achieve 50–60% power with one-third of the target sample size. We also expected secondary outcomes to confirm a possible null result and thus mitigate this loss of power.
Intervention
The intervention consisted of the instruction of a structured discharge procedure with two core components, namely (a) medication review performed by HPs and involving patients, and (b) measures to encourage medication-related information transfer between HPs and the referring PCPs:
- (a)
To optimize medication and deprescribe inappropriate drugs, each drug was subjected to questions about whether (i) the patient took it as prescribed, (ii) the drug’s indication was correct, (iii) the risk of side effects was lower than the expected benefit, (iv) the dose was correct given age and comorbidities, and (v) there was an alternative drug with a better benefit-to-risk ratio. - (b)
To anchor medication changes with the follow-up PCPs, the discharge letters were customized. Depending on technical feasibility, they should contain (in order of preference) (i) a table of all medication changes with reasons (so implemented in n = 1 hospital), (ii) separate tables of admission and discharge medications, adjacent or in immediate sequence and again with reasons for changes (n = 8), or (iii) a table with the discharge medication only, and changes explained in the letter body (n = 3). Additionally, the discharge letters were supplemented by invitations to the PCPs to discuss the discharge medication with the responsible HPs (in bold print, with phone numbers of the discharging HPs).
In the 2-h instructions of the senior HPs by a member of the study team with extensive practical and research experience in polypharmacy and deprescribing in the primary care setting, they were first given background information on polypharmacy in multimorbid patients and then demonstrated the medication review using a hypothetical model patient. Subsequently, data collection was explained, and a discussion concluded the instructions.
Similar training of the junior HPs was entrusted to their seniors because of frequent personnel changes among the former. Both then participated in discharging study participants according to the study’s specifications. Proper implementation was guided by and recorded in a checklist by the discharging HPs (eFigure 1).
The senior HPs in the control arm were given a 2-h “sham” instruction by the same study team member, focusing on the significance of multimorbidity and polypharmacy, and on data collection. The untrained HPs in the control arm then discharged their patients as per the established local routines.
Outcomes
The primary outcome was time-to-first-hospital-readmission within 6 months after discharge, and secondary outcomes covered readmission rates, numbers of ED visits, and other medical consultations (including with PCPs), all collected at 1, 3, and 6 months after discharge, as well as numbers and Anatomical Therapeutic Chemical (ATC) classes[31](/article/10.1007/s11606-022-07728-6#ref-CR31 "Anatomical Therapeutic Chemical Classification System - Structure and Principles. WHO Collaboration Centre for Drug Statistics Methodology, Oslo. https://www.whocc.no/atc/structure_and_principles/
.") of drugs prescribed, proportions of patients with potentially inappropriate medications (PIMs), and the patients’ QoL, all collected at discharge and after 1, 3, and 6 months. Medications were classified as PIMs if they figured among the 2012 PRISCUS list[32](/article/10.1007/s11606-022-07728-6#ref-CR32 "Holt S, Schmiedl S, Thürmann PA. Potentially inappropriate medications in the elderly: the PRISCUS list. Dtsch Arztebl Int. 2010;107(31-32):543-51.
https://doi.org/10.3238/arztebl.2010.0543
.") or the updated 2019 Beers list of “unconditional PIMs”.[33](/article/10.1007/s11606-022-07728-6#ref-CR33 "American Geriatrics Society 2019 Updated AGS Beers Criteria® for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc. 2019;67(4):674-94.
https://doi.org/10.1111/jgs.15767
.") QoL was assessed with the EQ-5D-3L instrument and evaluated using the French TTO value set.[34](/article/10.1007/s11606-022-07728-6#ref-CR34 "Foundation ER. EQ-5D-3L User Guide. Version 6.0 ed. Rotterdam; 2018.") Additionally, baseline characteristics of hospitals, HPs, and patients were recorded (Table [1](/article/10.1007/s11606-022-07728-6#Tab1)).Table 1 Hospital, Participating HP, and Patient Characteristics
Data Collection
Consent forms and copies of the discharge letters were sent to the study center in weekly batches, along with filled quality of life (QoL) questionnaires and, in the intervention arm, the checklists. During the study period and for 10 days beyond in each hospital, all contacts between PCPs and HPs were recorded by the discharging HP, other HPs, or administrative staff, with dates and duration. Six newsletters repeatedly reminded senior HPs to ensure that all PCP-HP contacts were recorded.
One (T1 = 30 days), 3 (T3 = 90 days), and 6 months (T6 = 180 days) after their discharge (T0), patients were requested by postal mail from the study center to report any hospital readmissions (for at least one night), ED visits, and other medical consultations (with reasons, if applicable) since their index discharge in paper-based case report forms (CRFs). The patients were also asked to provide their current medication plans and filled QoL forms. To improve data quality, a study nurse contacted patients or relatives in writing and/or by phone (up to three attempts) and also inquired with the patients’ PCPs for verifying patient reports and completing missing data.
Implementation outcomes were collected in parallel to the core study and evaluated according to an adapted framework[28](/article/10.1007/s11606-022-07728-6#ref-CR28 "Rachamin Y, Grischott T, Neuner-Jehle S. Implementation of a complex intervention to improve hospital discharge: process evaluation of a cluster randomised controlled trial. BMJ Open. 2021;11(5):e049872. https://doi.org/10.1136/bmjopen-2021-049872
.") for process evaluation studies.[35](/article/10.1007/s11606-022-07728-6#ref-CR35 "Grant A, Treweek S, Dreischulte T, Foy R, Guthrie B. Process evaluations for cluster-randomised trials of complex interventions: a proposed framework for design and reporting. Trials. 2013;14:15.
https://doi.org/10.1186/1745-6215-14-15
.")Statistical Analysis
Hospital and patient characteristics and outcome baselines were presented as counts and proportions or means with standard deviations, with standardized mean differences and fractions of missing data.
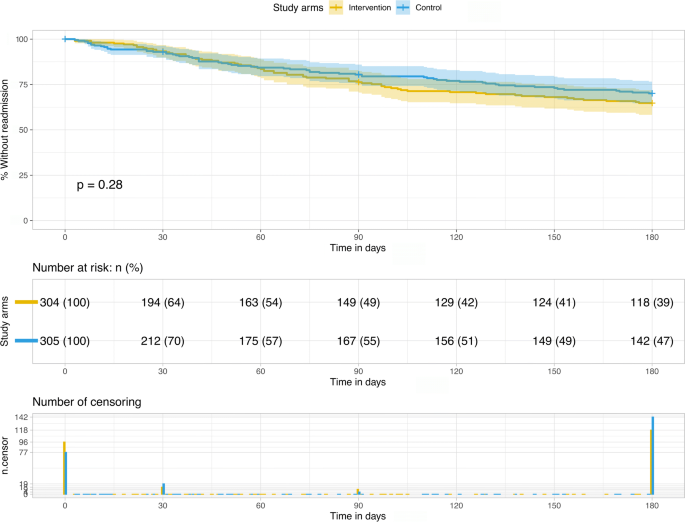
Kaplan-Meier curves[36](/article/10.1007/s11606-022-07728-6#ref-CR36 "Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53(282):457-81. https://doi.org/10.1080/01621459.1958.10501452
.") and the log rank test[37](/article/10.1007/s11606-022-07728-6#ref-CR37 "Mantel N. Evaluation of survival data and two new rank order statistics arising in its consideration. Cancer ChemoTherapy Reports. 1966;50(3):163-70.") were used to compare the primary outcome (time-to-first-hospital-readmission) between study arms. The analysis was adjusted for hospital and patient characteristics using a shared frailty model[38](/article/10.1007/s11606-022-07728-6#ref-CR38 "Austin PC. A tutorial on multilevel survival analysis: methods, models and applications. international statistical review = Revue internationale de statistique. 2017;85(2):185-203.
https://doi.org/10.1111/insr.12214
.") with normally distributed cluster-specific random effects to account for within-hospital homogeneity.Similar models were fitted for ED visits and other medical consultations. The competing risk death was treated as censor in the shared frailty models. Missing values (numbers of drugs at admission) were multiply imputed using R’s mice package,39 and for comparison, we also analyzed time-to-first-readmission on complete cases.
Additional secondary outcomes were presented with 95% confidence intervals (CIs) and/or compared between study arms using Fisher’s exact or Mann-Whitney U tests as appropriate. Sensitivity analyses as well as longitudinal analyses (numbers of drugs, QoL scores) using (generalized) linear mixed models are explained and presented with results in Online Supplement 1.
To quantify how multiple non-significant outcomes jointly speak against a true intervention effect, we calculated an approximate “aggregate power,” i.e., the probability of observing a hypothetic effect in at least one or two of n outcomes (eMethods 3).
All analyses of primary and secondary outcomes followed a modified intention-to-treat principle (Fig. 1) and were carried out using R, version 4.0.3.40
RESULTS
In 21 participating hospitals, 68 senior and 164 junior HPs included 609 patients (intervention arm: 328 initial inclusions - 24 secondary exclusions; control arm: 317 - 12; p = 0.06). No patient dropped out before discharge, but 121 provided no follow-up data (intervention arm: 66; control arm: 55; p = 0.27) (Fig. 1). There were no significant differences in sex and age between those who did or did not complete follow-up.
On admission, the patients’ mean age was 77.5 years, they took a mean of 9.64 drugs, and 49.4% were female. Randomization covariates (hospital type, care level, number of beds in participating wards) and patient baseline characteristics were similar in both study arms (Table 1; eTable 1).
Primary Outcome
Time-to-first-readmission to any hospital within 6 months after discharge did not differ between study arms (Fig. 2; log rank test p = 0.28). The adjusted shared frailty model showed no significant discrepancy in hazard rates either (hazard ratio (HR) = 1.14 (intervention vs. control arm), 95% CI = [0.75-1.71], p = 0.54; eTable 2). Covariates reaching significance in the adjusted model were sex (HR = 1.50 (male vs. female), 95% CI = [1.05–2.13], p = 0.03), age (HR = 0.98 (per 5 year increase), 95% CI = [0.96–1.00], p = 0.03), and the number of drugs at admission (HR = 1.06 (per one additional drug), 95% CI = [1.01–1.12], p = 0.03).
Figure 2
Time-to-first-readmission to any hospital within 180 days of the index discharge. Kaplan-Meier curve with log-rank test.
Secondary Outcomes
Table 2 presents rates of readmissions, ED visits (eFigure 2), and other medical consultations (eFigure 3) for each follow-up stage. All rates were within the CIs of the respective other study arm. Shared frailty models for time-to-ED visits and time-to-other medical consultations showed no significant differences between study arms (HR = 1.14, 95% CI = [0.63–2.09], p = 0.66; and HR = 1.11, 95% CI = [0.86–1.43], p = 0.42; eTables 4 and 5), and no consistent pattern regarding covariate influence.
Table 2 Rates (%) of Readmissions, ED Visits, and Other Medical Consultations, by Study Stage
Any-cause mortality rates were 1.6% within 30 and 7.6% within 180 days after discharge and did not differ between study arms (eTable 6).
Table 3 summarizes the patients’ medications (eFigures 4 and 5), with total numbers and numbers of drugs per patient, proportions of patients with (at least one) PIM and of the drug classes oral antidiabetics, antihypertensives, statins, and acetylsalicylic acid, which were explicitly addressed as frequent candidates of inappropriate prescribing in the teaching sessions. Inspection of the CIs revealed neither differences between study arms nor temporal trends. In particular, a longitudinal mixed model confirmed the absence of a time trend in the number of drugs per patient (p = 0.07, 0.55, 0.63, and 0.29 for discharge and 1, 3, and 6 months later, each compared to admission; eTable 7).
Table 3 Medication, by Study Stage
eTables 8 and 9 in Online Supplement 1 analogously present proportions of all ATC anatomical main groups and of the three most frequently prescribed medications.
Regarding QoL, the raw data showed a slight increase over time, with some significant study arm differences (in favor of the control arm) at later time points (eTable 10). Imputation based on a plausible missing at random (MAR) assumption followed by fitting a longitudinal mixed model exposed raw p values < 0.05 as likely to be false positives due to attrition bias (eTable 11).
DISCUSSION
In this pragmatic study, we combined medication review with a HP-PCP communication stimulus into a checklist-guided discharge procedure. This dual intervention did not decrease time-to-hospital-readmission of older inpatients with polypharmacy, compared with established discharge procedures, and showed no effect on secondary outcomes (apart from a slightly slower increase in QoL, likely due to attrition bias, and clinically irrelevant).
Previous research on the effectiveness of medication-related interventions at hospital discharge is inconclusive:[16](/article/10.1007/s11606-022-07728-6#ref-CR16 "Christensen M, Lundh A. Medication review in hospitalised patients to reduce morbidity and mortality. Cochrane Database Syst Rev. 2016;2(2):Cd008986. https://doi.org/10.1002/14651858.CD008986.pub3
."),[23](/article/10.1007/s11606-022-07728-6#ref-CR23 "O’Mahony D. Optimization of medication by pharmacists in older people with multimorbidity for improved outcomes-mirage or reality? JAMA Netw Open. 2021;4(4):e216392.
https://doi.org/10.1001/jamanetworkopen.2021.6392
.") Medication review alone was shown to reduce drug-related problems, but not readmission rates or mortality.[41](#ref-CR41 "Huiskes VJ, Burger DM, van den Ende CH, van den Bemt BJ. Effectiveness of medication review: a systematic review and meta-analysis of randomized controlled trials. BMC Fam Pract. 2017;18(1):5.
https://doi.org/10.1186/s12875-016-0577-x
."),[42](#ref-CR42 "Mistiaen P, Poot E. Telephone follow-up, initiated by a hospital-based health professional, for postdischarge problems in patients discharged from hospital to home. Cochrane Database Syst Rev. 2006;2006(4):Cd004510.
https://doi.org/10.1002/14651858.CD004510.pub3
."),[43](/article/10.1007/s11606-022-07728-6#ref-CR43 "Redmond P, Grimes TC, McDonnell R, Boland F, Hughes C, Fahey T. Impact of medication reconciliation for improving transitions of care. Cochrane Database Syst Rev. 2018;8(8):Cd010791.
https://doi.org/10.1002/14651858.CD010791.pub2
.") In contrast, such effects were achieved in trials that involved patients beyond their discharge.[44](#ref-CR44 "Braet A, Weltens C, Sermeus W. Effectiveness of discharge interventions from hospital to home on hospital readmissions: a systematic review. JBI database of systematic reviews and implementation reports. 2016;14(2):106-73.
https://doi.org/10.11124/jbisrir-2016-2381
."),[45](#ref-CR45 "Dautzenberg L, Bretagne L, Koek HL, et al. Medication review interventions to reduce hospital readmissions in older people. J Am Geriatr Soc. 2021;69(6):1646-58.
https://doi.org/10.1111/jgs.17041
."),[46](#ref-CR46 "Leppin AL, Gionfriddo MR, Kessler M, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174(7):1095-107.
https://doi.org/10.1001/jamainternmed.2014.1608
."),[47](#ref-CR47 "Mizokami F, Mizuno T, Kanamori K, et al. Clinical medication review type III of polypharmacy reduced unplanned hospitalizations in older adults: A meta-analysis of randomized clinical trials. Geriatr Gerontol Int. 2019;19(12):1275-81.
https://doi.org/10.1111/ggi.13796
."),[48](/article/10.1007/s11606-022-07728-6#ref-CR48 "Tomlinson J, Cheong VL, Fylan B, et al. Successful care transitions for older people: a systematic review and meta-analysis of the effects of interventions that support medication continuity. Age Ageing. 2020;49(4):558-69.
https://doi.org/10.1093/ageing/afaa002
.") Notably, a Swedish RCT with patients aged ≥ 80 years reported a 16% reduction of hospitalizations in the year following discharge,[17](/article/10.1007/s11606-022-07728-6#ref-CR17 "Gillespie U, Alassaad A, Henrohn D, et al. A comprehensive pharmacist intervention to reduce morbidity in patients 80 years or older: a randomized controlled trial. Arch Intern Med. 2009;169(9):894-900.
https://doi.org/10.1001/archinternmed.2009.71
.") and in a Danish multicenter RCT, medication review plus individual follow-up by hospital pharmacists reduced readmissions within 6 months by 25%.[18](/article/10.1007/s11606-022-07728-6#ref-CR18 "Ravn-Nielsen LV, Duckert ML, Lund ML, et al. Effect of an in-hospital multifaceted clinical pharmacist intervention on the risk of readmission: a randomized clinical trial. JAMA Intern Med. 2018;178(3):375-82.
https://doi.org/10.1001/jamainternmed.2017.8274
.") Conversely, our study confirms the results of a recent crossover trial with 2644 patients from 4 Swedish hospitals that found no beneficial effects of medication review plus postdischarge patient follow-up on the incidence of unplanned hospital visits within 12 months, nor on health care utilization or mortality.[19](/article/10.1007/s11606-022-07728-6#ref-CR19 "Kempen TGH, Bertilsson M, Hadziosmanovic N, et al. Effects of hospital-based comprehensive medication reviews including postdischarge follow-up on older patients’ use of health care: a cluster randomized clinical trial. JAMA Netw Open. 2021;4(4):e216303.
https://doi.org/10.1001/jamanetworkopen.2021.6303
.")Multiple reasons may account for this null result. Firstly, the baseline readmission rate in our sample (7.0% within 1 month; Table 2) was unexpectedly low, thus impeding further improvements. For example, US sources reported 30-day all-cause readmission rates of 13.9% in 2016,49 and in Swiss acute care hospitals, they were 11% across all ages in 2009–2016.50 A slight overrepresentation of smaller and rehabilitation hospitals in our sample may have resulted in a more favorable case mix with lower readmission risk.
Secondly, high-quality pre-existing discharge procedures and/or high postdischarge standards of care by ambulatory providers may have thwarted our intervention’s effect. Aside from the low baseline readmission rate, this hypothesis is supported by the observation that potential mediators of early readmission did not differ between study arms: (a) Early PCP support, inversely associated with readmission, ED visits, and mortality,51,[52](/article/10.1007/s11606-022-07728-6#ref-CR52 "Costantino ME, Frey B, Hall B, Painter P. The influence of a postdischarge intervention on reducing hospital readmissions in a Medicare population. Popul Health Manag. 2013;16(5):310-6. https://doi.org/10.1089/pop.2012.0084
.") was equally sought in both study arms (Table [2](/article/10.1007/s11606-022-07728-6#Tab2), other medical consultations). (b) Medication numbers increased just slightly (and insignificantly) from admission to discharge, when they were equal in both study arms (Table [3](/article/10.1007/s11606-022-07728-6#Tab3)). (c) Likewise, there was no difference in the—relatively low[53](/article/10.1007/s11606-022-07728-6#ref-CR53 "Huber CA, Scherer M, Rapold R, Blozik E. Evidence-based quality indicators for primary healthcare in association with the risk of hospitalisation: a population-based cohort study in Switzerland. BMJ Open. 2020;10(4):e032700.
https://doi.org/10.1136/bmjopen-2019-032700
.")—fractions of patients with PIM, which is a well-known driver of hospitalization.[53](/article/10.1007/s11606-022-07728-6#ref-CR53 "Huber CA, Scherer M, Rapold R, Blozik E. Evidence-based quality indicators for primary healthcare in association with the risk of hospitalisation: a population-based cohort study in Switzerland. BMJ Open. 2020;10(4):e032700.
https://doi.org/10.1136/bmjopen-2019-032700
.")Thirdly, encouraging PCPs to communicate with HPs—a key component of our intervention—may have failed. Few PCPs contacted HPs in the postdischarge period (4 documented contacts in the intervention and 10 in the control arm; p = 0.17). However, HP-initiated communication had much more frequently taken place during hospitalization (intervention arm: 22.4%, information missing for 36 patients; control arm 22.0%, missing for 30; p = 0.24), which further indicates a relatively high baseline quality of care.
The flexible implementation of our study minimally disrupted hospital routines,[28](/article/10.1007/s11606-022-07728-6#ref-CR28 "Rachamin Y, Grischott T, Neuner-Jehle S. Implementation of a complex intervention to improve hospital discharge: process evaluation of a cluster randomised controlled trial. BMJ Open. 2021;11(5):e049872. https://doi.org/10.1136/bmjopen-2021-049872
.") but possibly at the expense of a weaker intervention[54](/article/10.1007/s11606-022-07728-6#ref-CR54 "Landes SJ, McBain SA, Curran GM. An introduction to effectiveness-implementation hybrid designs. Psychiatry research. 2019;280:112513.
https://doi.org/10.1016/j.psychres.2019.112513
.") that generated no incremental benefit in hospitals with already well-organized discharge procedures including routine HP-PCP communication, critical medication review, and a high awareness of polypharmacy and deprescribing.Limitations
Our study suffered from under-recruitment in most hospitals during the first two waves of the COVID-19 pandemic in Switzerland, resulting in some loss of power. However, we assume a low risk of a false-negative result (Methods, eMethods 3).
The study design with a voluntary hospital sample and cluster-randomization before patient recruitment carried the risk of selection bias. HPs were instructed to invite all eligible patients to participate, but depending on workload, this was surely not always possible, and it is unclear how fluctuations in recruitment intensity may have affected the outcomes. Imperfect blinding (i.e., of junior HPs only), losses to follow-up, incomplete medication data, self-declared outcomes, and subjective measurement tools (e.g., for QoL) were other potential sources of bias.
Although our evaluation of the checklists suggested that the hospitals implemented the study largely as instructed, the COVID-19-related additional workload may at times have favored a somewhat leaner implementation on the HPs’ own initiative (e.g., cursory medication review).
Finally, we must assume that the HP-PCP communication in the postdischarge period, which we could not monitor reliably, was incompletely documented. That being said, follow-up surveys among PCPs confirmed that they often and readily adopted changes to their patients’ long-term medication without further consultation with HPs.[28](/article/10.1007/s11606-022-07728-6#ref-CR28 "Rachamin Y, Grischott T, Neuner-Jehle S. Implementation of a complex intervention to improve hospital discharge: process evaluation of a cluster randomised controlled trial. BMJ Open. 2021;11(5):e049872. https://doi.org/10.1136/bmjopen-2021-049872
.")CONCLUSIONS
Our dual intervention combining a patient-centered medication review with enhanced medication-related information transfer between HPs and PCPs neither delayed hospital readmission nor impacted health care utilization, mortality, polypharmacy, or medication appropriateness among older inpatients after discharge. Given the consistency in all outcomes, we assume a true null result despite the limited sample size. Prioritizing flexibility over implementation rigor may have weakened the intervention. Our data and experience may help to strike an optimal balance between practicality and stringency in future hospital discharge interventions.
Data Availability
The datasets generated and/or analyzed during the current study are available from the last author on reasonable request.
References
- Chiatti C, Bustacchini S, Furneri G, et al. The economic burden of inappropriate drug prescribing, lack of adherence and compliance, adverse drug events in older people: a systematic review. Drug Saf. 2012;35 Suppl 1:73-87. https://doi.org/10.1007/BF03319105.
- Field TS, Mazor KM, Briesacher B, Debellis KR, Gurwitz JH. Adverse drug events resulting from patient errors in older adults. J Am Geriatr Soc. 2007;55(2):271-6. https://doi.org/10.1111/j.1532-5415.2007.01047.x.
- Maher RL, Hanlon J, Hajjar ER. Clinical consequences of polypharmacy in elderly. Expert Opin Drug Saf. 2014;13(1):57-65. https://doi.org/10.1517/14740338.2013.827660.
- Frazier SC. Health outcomes and polypharmacy in elderly individuals: an integrated literature review. J Gerontol Nurs. 2005;31(9):4-11.
- Lau DT, Kasper JD, Potter DE, Lyles A, Bennett RG. Hospitalization and death associated with potentially inappropriate medication prescriptions among elderly nursing home residents. Arch Intern Med. 2005;165(1):68-74. https://doi.org/10.1001/archinte.165.1.68.
- Guthrie B, Makubate B, Hernandez-Santiago V, Dreischulte T. The rising tide of polypharmacy and drug-drug interactions: population database analysis 1995-2010. BMC Med. 2015;13:74. https://doi.org/10.1186/s12916-015-0322-7.
- Clyne W, Alison B, Seal R. A Guide to Medication Review 2008. The National Prescribing Centre; 2008.
- Donaldson LJ, Kelley ET, Dhingra-Kumar N, Kieny MP, Sheikh A. Medication without harm: WHO’s third global patient safety challenge. Lancet. 2017;389(10080):1680-1. https://doi.org/10.1016/s0140-6736(17)31047-4.
- Leitliniengruppe Hessen. Hausärztliche Leitlinie Multimedikation. 1.09 ed: Deutsche Gesellschaft für Allgemeinmedizin und Familienmedizin DEGAM; 2013.
- National Institute for Health and Care Excellence. Medicines Optimisation: the safe and effective use of medicines to enable the best possible outcomes (NICE guideline NG5); 2015. https://www.nice.org.uk/guidance/ng5.
- Scottish Government Model of Care Polypharmacy Working Group. Polypharmacy Guidance. 2nd Edition ed: Scottish Government; 2015.
- Parekh N, Ali K, Page A, Roper T, Rajkumar C. Incidence of medication-related harm in older adults after hospital discharge: a systematic review. J Am Geriatr Soc. 2018;66(9):1812-22. https://doi.org/10.1111/jgs.15419.
- Pérez T, Moriarty F, Wallace E, McDowell R, Redmond P, Fahey T. Prevalence of potentially inappropriate prescribing in older people in primary care and its association with hospital admission: longitudinal study. BMJ. 2018;363:k4524. https://doi.org/10.1136/bmj.k4524.
- Nobili A, Licata G, Salerno F, et al. Polypharmacy, length of hospital stay, and in-hospital mortality among elderly patients in internal medicine wards. The REPOSI study. Eur J Clin Pharmacol. 2011;67(5):507-19. https://doi.org/10.1007/s00228-010-0977-0.
- Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007a;297(8):831-41. https://doi.org/10.1001/jama.297.8.831.
- Christensen M, Lundh A. Medication review in hospitalised patients to reduce morbidity and mortality. Cochrane Database Syst Rev. 2016;2(2):Cd008986. https://doi.org/10.1002/14651858.CD008986.pub3.
- Gillespie U, Alassaad A, Henrohn D, et al. A comprehensive pharmacist intervention to reduce morbidity in patients 80 years or older: a randomized controlled trial. Arch Intern Med. 2009;169(9):894-900. https://doi.org/10.1001/archinternmed.2009.71.
- Ravn-Nielsen LV, Duckert ML, Lund ML, et al. Effect of an in-hospital multifaceted clinical pharmacist intervention on the risk of readmission: a randomized clinical trial. JAMA Intern Med. 2018;178(3):375-82. https://doi.org/10.1001/jamainternmed.2017.8274.
- Kempen TGH, Bertilsson M, Hadziosmanovic N, et al. Effects of hospital-based comprehensive medication reviews including postdischarge follow-up on older patients’ use of health care: a cluster randomized clinical trial. JAMA Netw Open. 2021;4(4):e216303. https://doi.org/10.1001/jamanetworkopen.2021.6303.
- Graabaek T, Kjeldsen LJ. Medication reviews by clinical pharmacists at hospitals lead to improved patient outcomes: a systematic review. Basic Clin Pharmacol Toxicol. 2013;112(6):359-73. https://doi.org/10.1111/bcpt.12062.
- Silva ROS, Macêdo LA, Santos GADJ, Aguiar PM, de Lyra DPJ. Pharmacist-participated medication review in different practice settings: Service or intervention? An overview of systematic reviews. PLoS ONE. 2019;14(1):e0210312. https://doi.org/10.1371/journal.pone.0210312.
- Kripalani S, Theobald CN, Anctil B, Vasilevskis EE. Reducing hospital readmission rates: current strategies and future directions. Annu Rev Med. 2014;65:471-85. https://doi.org/10.1146/annurev-med-022613-090415.
- O’Mahony D. Optimization of medication by pharmacists in older people with multimorbidity for improved outcomes-mirage or reality? JAMA Netw Open. 2021;4(4):e216392. https://doi.org/10.1001/jamanetworkopen.2021.6392.
- Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150(3):178-87. https://doi.org/10.7326/0003-4819-150-3-200902030-00007.
- Kripalani S, Jackson AT, Schnipper JL, Coleman EA. Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. 2007b;2(5):314-23. https://doi.org/10.1002/jhm.228.
- Soong C, Daub S, Lee J, et al. Development of a checklist of safe discharge practices for hospital patients. J Hosp Med. 2013;8(8):444-9. https://doi.org/10.1002/jhm.2032.
- Anthierens S, Tansens A, Petrovic M, Christiaens T. Qualitative insights into general practitioners views on polypharmacy. BMC Fam Pract. 2010;11:65. https://doi.org/10.1186/1471-2296-11-65.
- Rachamin Y, Grischott T, Neuner-Jehle S. Implementation of a complex intervention to improve hospital discharge: process evaluation of a cluster randomised controlled trial. BMJ Open. 2021;11(5):e049872. https://doi.org/10.1136/bmjopen-2021-049872.
- Grischott T, Zechmann S, Rachamin Y, et al. Improving inappropriate medication and information transfer at hospital discharge: study protocol for a cluster RCT. Implement Sci. 2018;13(1):155. https://doi.org/10.1186/s13012-018-0839-1.
- Grischott T. The Shiny Balancer - Software and imbalance criteria for optimally balanced treatment allocation in small RCTs and cRCTs. BMC Med Res Methodol. 2018;18(108). https://doi.org/10.1186/s12874-018-0551-5.
- Anatomical Therapeutic Chemical Classification System - Structure and Principles. WHO Collaboration Centre for Drug Statistics Methodology, Oslo. https://www.whocc.no/atc/structure_and_principles/.
- Holt S, Schmiedl S, Thürmann PA. Potentially inappropriate medications in the elderly: the PRISCUS list. Dtsch Arztebl Int. 2010;107(31-32):543-51. https://doi.org/10.3238/arztebl.2010.0543.
- American Geriatrics Society 2019 Updated AGS Beers Criteria® for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc. 2019;67(4):674-94. https://doi.org/10.1111/jgs.15767.
- Foundation ER. EQ-5D-3L User Guide. Version 6.0 ed. Rotterdam; 2018.
- Grant A, Treweek S, Dreischulte T, Foy R, Guthrie B. Process evaluations for cluster-randomised trials of complex interventions: a proposed framework for design and reporting. Trials. 2013;14:15. https://doi.org/10.1186/1745-6215-14-15.
- Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53(282):457-81. https://doi.org/10.1080/01621459.1958.10501452.
- Mantel N. Evaluation of survival data and two new rank order statistics arising in its consideration. Cancer ChemoTherapy Reports. 1966;50(3):163-70.
- Austin PC. A tutorial on multilevel survival analysis: methods, models and applications. international statistical review = Revue internationale de statistique. 2017;85(2):185-203. https://doi.org/10.1111/insr.12214.
- van Buuren S, Groothuis-Oudshoorn K. mice: multivariate imputation by chained equations in R. J Stat Softw. 2011;45(3):1-67.
- R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2020.
- Huiskes VJ, Burger DM, van den Ende CH, van den Bemt BJ. Effectiveness of medication review: a systematic review and meta-analysis of randomized controlled trials. BMC Fam Pract. 2017;18(1):5. https://doi.org/10.1186/s12875-016-0577-x.
- Mistiaen P, Poot E. Telephone follow-up, initiated by a hospital-based health professional, for postdischarge problems in patients discharged from hospital to home. Cochrane Database Syst Rev. 2006;2006(4):Cd004510. https://doi.org/10.1002/14651858.CD004510.pub3.
- Redmond P, Grimes TC, McDonnell R, Boland F, Hughes C, Fahey T. Impact of medication reconciliation for improving transitions of care. Cochrane Database Syst Rev. 2018;8(8):Cd010791. https://doi.org/10.1002/14651858.CD010791.pub2.
- Braet A, Weltens C, Sermeus W. Effectiveness of discharge interventions from hospital to home on hospital readmissions: a systematic review. JBI database of systematic reviews and implementation reports. 2016;14(2):106-73. https://doi.org/10.11124/jbisrir-2016-2381.
- Dautzenberg L, Bretagne L, Koek HL, et al. Medication review interventions to reduce hospital readmissions in older people. J Am Geriatr Soc. 2021;69(6):1646-58. https://doi.org/10.1111/jgs.17041.
- Leppin AL, Gionfriddo MR, Kessler M, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174(7):1095-107. https://doi.org/10.1001/jamainternmed.2014.1608.
- Mizokami F, Mizuno T, Kanamori K, et al. Clinical medication review type III of polypharmacy reduced unplanned hospitalizations in older adults: A meta-analysis of randomized clinical trials. Geriatr Gerontol Int. 2019;19(12):1275-81. https://doi.org/10.1111/ggi.13796.
- Tomlinson J, Cheong VL, Fylan B, et al. Successful care transitions for older people: a systematic review and meta-analysis of the effects of interventions that support medication continuity. Age Ageing. 2020;49(4):558-69. https://doi.org/10.1093/ageing/afaa002.
- Bailey MK, Weiss AJ, Barrett ML, Jiang HJ. Characteristics of 30-day all-cause hospital readmissions, 2010–2016: Statistical Brief #248. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD): Agency for Healthcare Research and Quality (US); 2006.
- Tuch A, Jörg R, Hedinger D, Widmer M. Qualität der stationären Leistungen unter der neuen Spitalfinanzierung. Monitoring der Qualitätsindikatoren 2009–2016. Schlussbericht (Obsan Dossier 65). Neuchâtel: Schweizerisches Gesundheitsobservatorium; 2018.
- Effect of Early Follow-Up After Hospital Discharge on Outcomes in Patients With Heart Failure or Chronic Obstructive Pulmonary Disease: A Systematic Review. Ontario health technology assessment series. 2017;17(8):1-37.
- Costantino ME, Frey B, Hall B, Painter P. The influence of a postdischarge intervention on reducing hospital readmissions in a Medicare population. Popul Health Manag. 2013;16(5):310-6. https://doi.org/10.1089/pop.2012.0084.
- Huber CA, Scherer M, Rapold R, Blozik E. Evidence-based quality indicators for primary healthcare in association with the risk of hospitalisation: a population-based cohort study in Switzerland. BMJ Open. 2020;10(4):e032700. https://doi.org/10.1136/bmjopen-2019-032700.
- Landes SJ, McBain SA, Curran GM. An introduction to effectiveness-implementation hybrid designs. Psychiatry research. 2019;280:112513. https://doi.org/10.1016/j.psychres.2019.112513.
Acknowledgements
The authors thank Stefan Zechmann, Stefan Markun, and Corinne Chmiel for their support in early stages; Nicolas Rodondi for providing contacts and formally heading the second study center; our study nurse Susan Groth for managing data collection during follow-up; the patients who participated in our study, in many cases despite severe chronic illnesses; as well as all hospital staff: Marcel Amstutz, Jürg Hans Beer, Thomas Brack, Beate Buchmann, Claude Cao, Christian Clarenbach, Adam Dobrylovsky, Nadine Duthiers, Karim El-Hag, Thomas Fehr, Daniel Franzen, Fiorenza Gautschi, Thomas Gottschalk, Priska Grünig, Andrea Güttler, Martina Heim, Jens Hellermann, Jörg Isenegger, Daniel Joller, Bettina Joos, Thomas Kaeslin, Walter Kistler, Diana Lehmann, Caroline Lenherr, Otto Meyer, Matthias Möhrenschlager, Salih Muminagic, N.N., Sebastian Nowag, Alexander Nydegger, Claudia Pirozzi, Lesek Purek, Luzia Reutemann, Christian Reutlinger, Lauri Röllin, Julia Christin Sanchez, Oliver Schmidlin, Andreas Serra, Marc Spielmanns, Philip Tarr, Mirko Thiene, Alexander Turk, Igor Turkalj, Anders Vetsch, Jan Vontobel, Henning Usadel, Christian Waldthaler, Thomas Wieland, Murat Yilmaz, and all junior HPs.
Funding
Open access funding provided by University of Zurich. The study was funded as part of the National Research Programme “Smarter Health Care” (NRP 74) by research grant 407440_167193 / 1 from the Swiss National Science Foundation.
Author information
Authors and Affiliations
- Institute of Primary Care, University of Zurich & University Hospital Zurich, Zurich, Switzerland
Thomas Grischott MD, Yael Rachamin PhD, Oliver Senn MD, Petra Hug MMed, Thomas Rosemann PhD & Stefan Neuner-Jehle MD
Authors
- Thomas Grischott MD
You can also search for this author inPubMed Google Scholar - Yael Rachamin PhD
You can also search for this author inPubMed Google Scholar - Oliver Senn MD
You can also search for this author inPubMed Google Scholar - Petra Hug MMed
You can also search for this author inPubMed Google Scholar - Thomas Rosemann PhD
You can also search for this author inPubMed Google Scholar - Stefan Neuner-Jehle MD
You can also search for this author inPubMed Google Scholar
Contributions
Concept and Design: Grischott, Senn, Rosemann, Neuner-Jehle; Acquisition, Analysis, or Interpretation of Data: Grischott, Rachamin, Senn, Hug, Neuner-Jehle; Drafting of the Manuscript: Grischott; Critical Revision of the Manuscript for Important Intellectual Content: All authors; Statistical Analysis: Grischott; Obtained Funding: Senn, Rosemann, Neuner-Jehle; Administrative, Technical, or Material Support: Senn, Rosemann; Supervision: Senn, Rosemann, Neuner-Jehle. Mr. Grischott had full access to all deidentified data in the study and takes responsibility for data integrity and the accuracy of the data analysis.
Corresponding author
Correspondence toThomas Grischott MD.
Ethics declarations
Ethics Approval
Ethics Committees Zurich and Bern, Switzerland (BASEC2018-00215).
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Role of the Funder
The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; review or approval of the manuscript; and decision to submit the manuscript for publication.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prior Presentations
Poster presentations at the Programme Conference and the Synthesis Conference of the National Research Programme “Smarter Health Care” (NRP 74) of the Swiss National Science Foundation, 15 November 2021, Zurich, and 11/12 April 2022, Lucerne, Switzerland.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Grischott, T., Rachamin, Y., Senn, O. et al. Medication Review and Enhanced Information Transfer at Discharge of Older Patients with Polypharmacy: a Cluster-Randomized Controlled Trial in Swiss Hospitals.J GEN INTERN MED 38, 610–618 (2023). https://doi.org/10.1007/s11606-022-07728-6
- Received: 11 January 2022
- Accepted: 26 June 2022
- Published: 31 August 2022
- Issue Date: February 2023
- DOI: https://doi.org/10.1007/s11606-022-07728-6