Weight Loss after Roux-en-Y Gastric Bypass in Obese Patients Heterozygous for MC4R Mutations (original) (raw)
Abstract
Background
Heterozygous mutations in melanocortin-4 receptor (MC4R) are the most frequent genetic cause of obesity. Bariatric surgery is a successful treatment for severe obesity. The mechanisms of weight loss after bariatric surgery are not well understood.
Methods
Ninety-two patients who had Roux-en-Y gastric bypass (RYGB) surgery were screened for MC4R mutations. We compared percent excess weight loss (%EWL) in the four MC4R mutation carriers with that of two control groups: 8 matched controls and with the remaining 80 patients who underwent RYGB.
Results
Four patients were heterozygous for functionally significant MC4R mutations_._ In patients with MC4R mutations, the %EWL after RYGB (66% EWL) was not significantly different compared to matched controls (70% EWL) and non-matched controls (60% EWL) after 1 year of follow-up.
Conclusions
This study suggests that patients with heterozygous MC4R mutations also benefit from RYGB and that weight loss may be independent of the presence of such mutations.
Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.
Introduction
Lifestyle modification, such as diet and exercise, is not effective in maintaining long-term weight loss in patients with class III (BMI > 40 kg/m2) obesity. Bariatric surgery is currently the most effective therapy for these patients. Outcomes after different types of bariatric surgery are variable and the mechanisms of resultant weight loss are poorly understood [1]. It has been suggested that the outcome of these procedures could be influenced by genetic variations implicated in the predisposition to obesity [2].
Genetic factors account for 40% to 70% of an individual’s predisposition to obesity [3]. Several known obesity-associated mutations involve genes of the hypothalamic leptin–melanocortin system. These include mutations in leptin, the leptin receptor, proopiomelanocortin, prohormone convertase 1/3, and melanocortin-4 receptor (MC4R) [3–5]. Specifically, heterozygous MC4R mutations are the most common genetic form of obesity, and mutations in this gene account for approximately 2.5% of severely obese individuals [6, 7].
MC4R is expressed at low levels and is found in hypothalamic nuclei involved in the regulation of food intake and in particular neurons of the paraventricular nucleus [8]. The physiological role of MC4R in food intake and body weight regulation is best demonstrated by the phenotype of the MC4R knockout mice [9]. Mice lacking both alleles of MC4R (MC4R−/− mice) develop a maturity-onset hyperphagic obesity syndrome by 10 weeks of age. Mice heterozygous for an MC4R deletion (MC4R+/− mice) show an average weight that is intermediate between that of wild-type and MC4R−/− mice. This suggests that haplo-insufficiency at the MC4R locus is sufficient to cause an alteration in the regulation of body weight in rodents. MC4R regulates food intake and maintains long-term energy homeostasis by integrating signals provided by its agonist α-melanocyte stimulating hormone and antagonist agouti-related peptide from leptin-sensitive neurons in the arcuate nucleus [10]. An important argument for showing that non-synonymous mutations are responsible for a disease is the demonstration of the functional relevance of these mutations (i.e., the demonstration that the mutated product behaves differently in a functional assay). Functional studies of MC4R mutations associated with obesity indicate that multiple functional alterations contribute to their pathogenicity and that more severely impaired receptor function in vitro correlates with earlier age of obesity onset and higher BMI [6].
Lifestyle interventions based on exercise, behavior, and nutrition therapy in children with MC4R mutations are not effective in providing long-term weight loss in contrast to children without MC4R mutations [11]. In addition, a controversial report suggested that carriers of non-obesity-associated genetic variations at the MC4R locus might have poorer weight loss outcomes after gastric banding [2, 12].
Here, we compare the weight loss outcome after Roux-en-Y gastric bypass (RYGB) in patients who are heterozygous carriers of rare functionally relevant obesity-associated MC4R mutations with that of control patients who do not carry such mutations.
Patients and Methods
Patients
Ninety-two patients who were considered appropriate candidates for RYGB were screened for MC4R mutations. Criteria used at the University of California San Francisco Bariatric Surgery Program for the selection of patients for a RYGB has been described in detail previously [13]. Briefly, all patients met the 1991 NIH Consensus Development Conference guidelines, including: BMI (weight in kilograms divided by height in meters squared) >40 or BMI between 35 and 40 with obesity-related comorbidities for at least 5 years and a documented attempt of medically supervised therapy for weight loss for at least 6 months [14]. All patients also underwent preoperative psychological, nutritional, and medical evaluations. Active binge eating disorder is considered a contraindication for bariatric surgery at the UCSF Bariatric Program_._ Procedure selection was determined by patient preference and occurred after participation in a 1-h educational and screening session with a dietician and a bariatric surgeon and after medical and psychological clearances.
Surgical Technique for RYGB
The technique for RYGB has been described previously [15]. In brief, it was performed laparoscopically using staplers (US Surgical Corporation, Norwalk, CT) to create a 15- to 30-mL gastric pouch, the antecolic gastrojejunostomy, the100-cm Roux limb, and the side-to-side jejunojejunostomy.
Postoperative Care
Patients were given clear liquids on the first postoperative day and then advanced to a full liquid diet on the second postoperative day. Patients were seen in clinic 2 weeks postoperatively, then every 3 months for the first year. After the operation, patients received prenatal vitamins, calcium supplements, vitamin D, and acid suppression medication. Nutritional supplements were prescribed as needed for documented deficiencies. All weight measurements were obtained at the UCSF Bariatric Surgery Center. Calculation of excess weight loss was based on Metropolitan Life Insurance height and weight tables to determine ideal body weight (IBW) [16]. We defined excess weight as the weight above the patient’s IBW. We calculated the total weight loss (kg) on each follow-up time and the percent excess weight loss (%EWL) after surgery, which was weight loss divided by excess weight multiplied by 100 on each follow-up point.
Control Group Matching
Controls were matched for gender and the presence of diabetes. In addition, controls were matched within one standard deviation for baseline BMI before surgery and for age. The UCSF Committee on Human Research approved the protocols, and informed written consent was obtained from all patients.
Gene Analysis
Genomic DNA was extracted from white blood cells using standard methods. Our group previously described DNA sequencing and in vitro analysis of blood samples from patients with MC4R mutations [7].
Statistical Analyses and Power Calculation
The comparison of %EWL at each follow-up time point (1, 3, 6, 9, and 12 months) between cases (n = 4) and matched controls (n = 8) was performed using a paired, two-tailed t test. Additionally, the comparison between the four cases and the 88 controls (8 matched controls and 80 non-matched controls) was performed using linear regression while adjusting for age, gender, self-reported race, and baseline BMI.
Results
Identification of MC4R Mutations
Ninety-two patients were screened for MC4R mutations. The mean ± SD of BMI and age prior to surgery was 55 ± 8.5 kg/m2 and 45 ± 10.4 years, respectively.
Four patients carried heterozygous MC4R mutations. One patient carried the Cys271Phe (812G>T) mutation, one patient carried the nonsense mutation Gln307stop (919C>T), and two patients carried the Arg236Cys (706C>T) mutation. All these mutations cause functional alteration in vitro [7].
Weight Loss After RYGB
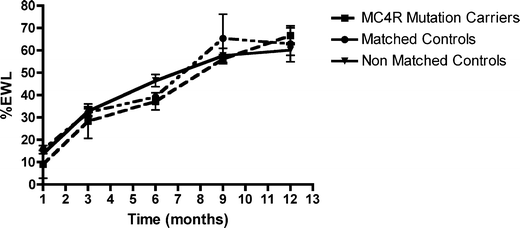
Subjects who were heterozygous for known MC4R non-synonymous mutations, defined as cases, were matched to subjects who lacked any non-synonymous MC4R mutations, defined as controls, based on age, sex, BMI, and type 2 diabetes mellitus (see “Patients and Methods”). Four cases were matched to eight controls (Table 1). We compared %EWL between MC4R mutation carriers and the entire cohort of 88 patients without MC4R mutations (4 matched controls and 80 non-matched controls) with a starting BMI > 40 kg/m2 at all time points (1, 3, 6, 9, and 12 months). There was no statistically significant difference in %EWL between cases and controls at any time point (Fig. 1).
Table 1 Clinical data from patients heterozygous for MC4R mutations and eight matched non-carrier for MC4R mutations controls
Fig. 1
%EWL curves of MC4R mutation carriers (n = 4), matched controls for gender, age, race, BMI, and presence of diabetes (n = 8) and non-matched controls (n = 80) from 1 to 12 months post-RYGB
Linear regression controlling for age, sex, self-reported race, and baseline BMI was used to compare %EWL between cases and all 88 controls patients (8 matched controls and 80 non-matched controls) without MC4R mutations in the cohort at the 9- and 12-month follow-up time points. After controlling for all the above variables, MC4R mutation carriers did not have a significantly different %EWL at 9 or 12 months. At 9 months of follow-up, the mutation carriers had less %EWL compared to controls; however, at 12 months, the mutation carriers had more %EWL compared to controls. Thus, neither the rate nor the absolute amount of weight loss was related to the presence of MC4R variants. In fact, the only predictor that was significant was baseline BMI. For every 10 points greater in BMI, patients lost 10% less EWL at a follow-up time of 9 months (effect size ± SE, 1 ± 0.38, p = 0.006) and 7% less EWL at a follow-up time of 12 months (effect size ± SE, −0.7 ± 0.3, p = 0.026). The combination of analysis of matched pairs and linear regression analysis provides better statistical analyses with the available cohort.
Perioperative (30 Days) Complications
Among the MC4R mutation carriers, one patient had aspiration pneumonia and was admitted to the ICU. He was discharged home on postoperative day 8. Out of eight matched control patients, none had perioperative complications.
Discussion
Bariatric surgery is an effective weight loss tool for selected severely obese patients for whom conventional medical and behavioral therapy for obesity has failed. With rising obesity rates, bariatric surgery has become a more common tool to achieve weight control and resolution of comorbidities [17]. Heterozygous MC4R mutations are the most common genetic form of obesity, and mutations in this gene account for approximately 2.5% of severely obese individuals [6, 7]. Our study is the first one to document weight loss after RYGB in patients with heterozygous MC4R mutations, and the results, although preliminary, suggest that patients with these mutations were able to lose as much weight as patients without MC4R mutations after RYGB. It is well established that obese patients can achieve a %EWL of approximately 60% after RYGB [18], and previous studies suggests that the %EWL after RYGB is superior than that obtained with gastric banding [19].
A previous report suggested that carriers of genetic variations at the MC4R locus have poorer outcomes after gastric banding [2]. This study, however, grouped many disparate mutations and polymorphisms together. A large majority of patients in the study carried MC4R variants that were not associated with obesity (i.e., found also in non-obese controls) and with no demonstrated functional effect on the MC4R protein. In addition, patients with binge eating disorders were included, which has been implicated in poorer outcomes after bariatric surgery, making the independent effect of MC4R gene variants in the previous study unclear [12].
Other studies have demonstrated resolution of or marked improvement in type 2 diabetes mellitus (DM) after bariatric surgery [20]. Only one out of the four patients with MC4R mutations had type 2 DM prior to RYGB, which did not resolve after surgery. Due to the small sample size of MC4R mutation carriers, we could not draw conclusions about the benefits of bariatric surgery for the resolution of diabetes in patients with heterozygous MC4R mutations. In a previous cohort of 769 obese adult patients, there was no significant difference in the prevalence of type 2 DM between carriers and non-carriers of MC4R patients. Nineteen patients were found to be MC4R carriers, and the prevalence of type 2 DM was 20% among these patients, similar to our patients with MC4R mutations [6].
The limitations of our study are mostly due to the rarity of patients with MC4R mutations and the lack of power to drawn definitive conclusions. Further research to understand the pathogenic mechanisms underlying obesity caused by MC4R mutations is required for the development of rational and effective treatments. This research is challenging because in addition to the relative small number of patients with MC4R mutations, there is great genetic heterogeneity of the disorder. However, our study is the first one to document weight loss after RYGB in patients with heterozygous MC4R mutations and provide preliminary information of outcomes after RYGB.
In conclusion, and in view of the limitations described above, our study shows that patients with heterozygous MC4R mutations had a similar rate of weight loss and %EWL after RYGB as patients without MC4R mutations. This suggests that heterozygous MC4R mutation status should not influence the decision to perform RYGB as a treatment for severe obesity.
References
- Tadross JA, le Roux CW. The mechanisms of weight loss after bariatric surgery. Int J Obes (Lond). 2009;33 Suppl 1:S28–32.
Article Google Scholar - Potoczna N, Branson R, Kral JG, et al. Gene variants and binge eating as predictors of comorbidity and outcome of treatment in severe obesity. J Gastrointest Surg. 2004;8(8):971–81. discussion 81–2.
Article PubMed Google Scholar - Ranadive SA, Vaisse C. Lessons from extreme human obesity: monogenic disorders. Endocrinol Metab Clin North Am. 2008;37(3):733–51. x.
Article PubMed CAS Google Scholar - Farooqi S, O’Rahilly S. Genetics of obesity in humans. Endocr Rev. 2006;27(7):710–18.
PubMed CAS Google Scholar - Farooqi IS. Genetic and hereditary aspects of childhood obesity. Best Pract Res Clin Endocrinol Metab. 2005;19(3):359–74.
Article PubMed CAS Google Scholar - Lubrano-Berthelier C, Dubern B, Lacorte JM, et al. Melanocortin 4 receptor mutations in a large cohort of severely obese adults: prevalence, functional classification, genotype–phenotype relationship, and lack of association with binge eating. J Clin Endocrinol Metab. 2006;91(5):1811–8.
Article PubMed CAS Google Scholar - Calton MA, Ersoy BA, Zhang S, et al. Association of functionally significant melanocortin-4 but not melanocortin-3 receptor mutations with severe adult obesity in a large North American case–control study. Hum Mol Genet. 2009;18:1140–7.
Article PubMed CAS Google Scholar - Mountjoy KG, Mortrud MT, Low MJ, et al. Localization of the melanocortin-4 receptor (MC4-R) in neuroendocrine and autonomic control circuits in the brain. Mol Endocrinol. 1994;8(10):1298–308.
Article PubMed CAS Google Scholar - Huszar D, Lynch CA, Fairchild-Huntress V, et al. Targeted disruption of the melanocortin-4 receptor results in obesity in mice. Cell. 1997;88(1):131–41.
Article PubMed CAS Google Scholar - Schwartz MW, Woods SC, Porte Jr D, et al. Central nervous system control of food intake. Nature. 2000;404(6778):661–71.
PubMed CAS Google Scholar - Reinehr T, Hebebrand J, Friedel S, et al. Lifestyle intervention in obese children with variations in the melanocortin 4 receptor gene. Obesity (Silver Spring). 2009;17(2):382–9.
CAS Google Scholar - List JF, Habener JF. Defective melanocortin 4 receptors in hyperphagia and morbid obesity. N Engl J Med. 2003;348(12):1160–3.
Article PubMed Google Scholar - Campos GM, Ciovica R, Rogers SJ, et al. Spectrum and risk factors of complications after gastric bypass. Arch Surg. 2007;142(10):969–75. discussion 76.
Article PubMed Google Scholar - National Institutes of Health. Gastrointestinal surgery for severe obesity: National Institutes of Health Consensus Development Conference Statement. Am J Clin Nutr. 1992 Feb;55(2 Suppl):615S–9S.
- Campos GM, Rabl C, Mulligan K, et al. Factors associated with weight loss after gastric bypass. Arch Surg. 2008;143(9):877–83. discussion 84.
Article PubMed Google Scholar - Deitel M, Gawdat K, Melissas J. Reporting weight loss 2007. Obes Surg. 2007;17(5):565–8.
Article PubMed Google Scholar - Pories WJ. Bariatric surgery: risks and rewards. J Clin Endocrinol Metab. 2008;93(11 Suppl 1):S89–96.
Article PubMed CAS Google Scholar - Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. Jama. 2004;292(14):1724–37.
Article PubMed CAS Google Scholar - Nguyen NT, Slone JA, Nguyen XM, et al. A prospective randomized trial of laparoscopic gastric bypass versus laparoscopic adjustable gastric banding for the treatment of morbid obesity: outcomes, quality of life, and costs. Ann Surg. 2009;250:631–41.
PubMed Google Scholar - Buchwald H, Estok R, Fahrbach K, et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med. 2009;122(3):248–56. e5.
Article PubMed Google Scholar
Acknowledgments
This publication was supported by NIH/NCRR UCSF-CTSI UL1 RR024131. IA was supported by American Heart Association post-doctoral fellowship and Genentech clinical fellowship. DSE is supported by National Institutes of Health training grant T32 DK007418. CV is supported by NIH RO1 DK DK60540 and DK068152 as well as an established investigator award from the American Heart Association: AHA#0740041N. GMC was supported by Grant Number KL2 RR024130 from the National Center for Research Resources (NCRR).
Disclosure Statement
The authors have nothing to disclose.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
- Department of Pediatrics, Division of Endocrinology, University of California San Francisco, San Francisco, CA, 94143, USA
Ivy R. Aslan - Diabetes Center and Department of Medicine, University of California San Francisco, 513 Parnassus Avenue, Room HSW1113, San Francisco, CA, 94143-0573, USA
Melissa A. Calton, Daniel S. Evans & Christian Vaisse - Department of Surgery, University of Wisconsin, Madison, WI, USA
Guilherme M. Campos - Division of Gastroenterology, California Pacific Medical Center, San Francisco, CA, 94115, USA
Raphael B. Merriman
Authors
- Ivy R. Aslan
- Guilherme M. Campos
- Melissa A. Calton
- Daniel S. Evans
- Raphael B. Merriman
- Christian Vaisse
Corresponding author
Correspondence toChristian Vaisse.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Aslan, I.R., Campos, G.M., Calton, M.A. et al. Weight Loss after Roux-en-Y Gastric Bypass in Obese Patients Heterozygous for MC4R Mutations.OBES SURG 21, 930–934 (2011). https://doi.org/10.1007/s11695-010-0295-8
- Published: 19 October 2010
- Issue Date: July 2011
- DOI: https://doi.org/10.1007/s11695-010-0295-8