Presence of sarcopenia identifies a special group of lean NAFLD in middle-aged and older people (original) (raw)
Abstract
Background
Sarcopenia, the age-related loss of muscle mass and function, is closely associated and frequently concomitant with non-alcoholic fatty liver disease (NAFLD). We aimed to investigate the clinical features of the sarcopenic NAFLD patients from middle-aged and older people.
Methods
A total of 1305 patients with NAFLD from the Shanghai Changfeng Study were included for analysis. Sarcopenia was diagnosed based on the height-adjusted appendicular skeletal muscle mass (ASM/height2). We comprehensively analyzed the metabolic phenotype, carotid artery condition, liver fibrosis score, and serum metabolomic profile of each participant.
Results
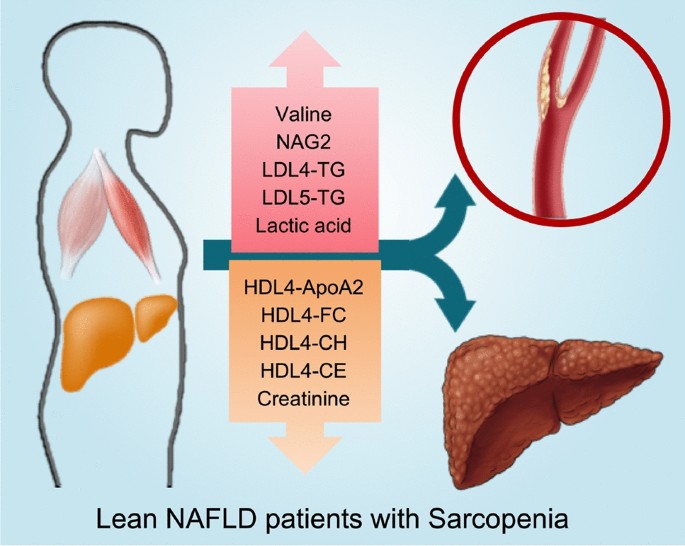
Among the middle-aged and older population, 68.1% of patients with sarcopenia and NAFLD were lean. Sarcopenia was independently associated with increased risk of carotid plaque (OR, 2.22; 95%CI 1.23–4.02) and liver fibrosis (OR, 2.07; 95%CI 1.24–3.44), and the sarcopenic lean NAFLD patients were characterized by a higher risk of carotid plaque (p = 0.008) and liver fibrosis (p = 0.001) than the non-sarcopenic lean NAFLD patients, despite their lower BMI and similar prevalence of metabolic syndrome and diabetes. Further serum metabolomic examination indicated that the sarcopenic lean NAFLD patients presented a distinct metabolomic profile prone to carotid plaque and liver fibrosis, with upregulated serum valine, N-acetylneuraminyl-glycoproteins, lactic acid, small LDL triglycerides and VLDL5 components, and reduced components of HDL4. A sarcopenic characterization score based on above metabolites was established and could also predict increased risk of carotid plaque and liver fibrosis.
Conclusion
The presence of sarcopenia identifies a special subgroup of lean NAFLD with increased risk of cardiovascular disease and liver fibrosis clinically.
Graphical abstract
Access this article
Subscribe and save
- Starting from 10 chapters or articles per month
- Access and download chapters and articles from more than 300k books and 2,500 journals
- Cancel anytime View plans
Buy Now
Price excludes VAT (USA)
Tax calculation will be finalised during checkout.
Instant access to the full article PDF.
Similar content being viewed by others
Abbreviations
ALT:
Alanine transaminase
ApoA1:
Apolipoprotein A1
ApoA2:
Apolipoprotein A2
ApoB:
Apolipoprotein B100
ASM/height2 :
Height-adjusted appendicular skeletal muscle mass
AST:
Aspartate transaminase
AWGS:
Asian working group for sarcopenia
BMI:
Body mass index
CE:
Cholesterol esters
DBP:
Diastolic blood pressure
DXA:
Dual-energy X-ray absorptiometry
FC:
Free cholesterol
FDR:
False discovery rate
FIB-4:
Fibrosis 4 score
FPG:
Fasting plasma glucose
HDL:
High-density lipoprotein
HOMA-IR:
Homeostasis model assessment for insulin resistance
hs-CRP:
High-sensitivity C-reactive protein
HR:
Hazard ratio
ICD-10:
The 10th revision of international classification of diseases
IDL:
Intermediate density lipoprotein
LDL:
Low-density lipoprotein
LFC:
Liver fat content
NAFLD:
Non-alcoholic fatty liver disease
NAG:
N-acetyl-glycoproteins
NAG1:
N-acetylglucosamine/galactosamine-glycoproteins
NAG2:
N-acetylneuraminyl-glycoproteins
NASH:
Non-alcoholic steatohepatitis
NHANES III.:
Third National Health and Nutrition Examination Survey
OGTT:
Oral glucose tolerance test
OR:
Odds ratio
PPG:
Post-load plasma glucose
PL:
Phospholipids
SBP:
Systolic blood pressure
TC:
Total cholesterol
TG:
Triglycerides
VLDL:
Very low-density lipoprotein
1H-NMR:
1-H nuclear magnetic resonance spectroscopy
95%CI:
95% Confidence interval
References
- Younossi ZM. Non-alcoholic fatty liver disease—a global public health perspective. J Hepatol. 2019;70(3):531–544
Article PubMed Google Scholar - Yki-Järvinen H. Non-alcoholic fatty liver disease as a cause and a consequence of metabolic syndrome. Lancet Diabetes Endocrinol. 2014;2(11):901–910
Article PubMed Google Scholar - Younossi ZM, Stepanova M, Younossi Y, Golabi P, Mishra A, Rafiq N, et al. Epidemiology of chronic liver diseases in the USA in the past three decades. Gut. 2020;69:564–568
Article PubMed Google Scholar - Estes C, Anstee QM, Arias-Loste MT, Bantel H, Bellentani S, Caballeria J, et al. Modeling NAFLD disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom, and United States for the period 2016–2030. J Hepatol. 2018;69(4):896–904
Article PubMed Google Scholar - Wong VW, Chu WC, Wong GL, Chan RS, Chim AM, Ong A, et al. Prevalence of non-alcoholic fatty liver disease and advanced fibrosis in Hong Kong Chinese: a population study using proton-magnetic resonance spectroscopy and transient elastography. Gut. 2012;61(3):409–415
Article PubMed Google Scholar - Younossi ZM, Blissett D, Blissett R, Henry L, Stepanova M, Younossi Y, et al. The economic and clinical burden of nonalcoholic fatty liver disease in the United States and Europe. Hepatology. 2016;64(5):1577–1586
Article PubMed Google Scholar - Zou B, Yeo YH, Nguyen VH, Cheung R, Ingelsson E, Nguyen MH. Prevalence, characteristics and mortality outcomes of obese, nonobese and lean NAFLD in the United States, 1999–2016. J Intern Med. 2020;288(1):139–151
Article CAS PubMed Google Scholar - Shi Y, Wang Q, Sun Y, Zhao X, Kong Y, Ou X, et al. The prevalence of lean/nonobese nonalcoholic fatty liver disease: a systematic review and meta-analysis. J Clin Gastroenterol. 2020;54(4):378–387
Article PubMed Google Scholar - Sookoian S, Pirola CJ. Systematic review with meta-analysis: risk factors for non-alcoholic fatty liver disease suggest a shared altered metabolic and cardiovascular profile between lean and obese patients. Aliment Pharmacol Ther. 2017;46(2):85–95
Article CAS PubMed Google Scholar - Ye Q, Zou B, Yeo YH, Li J, Huang DQ, Wu Y, et al. Global prevalence, incidence, and outcomes of non-obese or lean non-alcoholic fatty liver disease: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020;5(8):739–752
Article PubMed Google Scholar - Xia MF, Chen LY, Wu L, Ma H, Li Q, Aleteng Q, et al. The PNPLA3 rs738409 C>G variant influences the association between low skeletal muscle mass and NAFLD: the Shanghai Changfeng Study. Aliment Pharmacol Ther. 2019;50(6):684–695
Article CAS PubMed Google Scholar - Hong HC, Hwang SY, Choi HY, Yoo HJ, Seo JA, Kim SG, et al. Relationship between sarcopenia and nonalcoholic fatty liver disease: the Korean sarcopenic obesity study. Hepatology. 2014;59:1772–1778
Article CAS PubMed Google Scholar - Koo BK, Kim D, Joo SK, Kim JH, Chang MS, Kim BG, et al. Sarcopenia is an independent risk factor for non-alcoholic steatohepatitis and significant fibrosis. J Hepatol. 2017;66:123–131
Article PubMed Google Scholar - Petta S, Ciminnisi S, Di Marco V, Cabibi D, Cammà C, Licata A, et al. Sarcopenia is associated with severe liver fibrosis in patients with non-alcoholic fatty liver disease. Aliment Pharmacol Ther. 2017;45:510–518
Article CAS PubMed Google Scholar - Xia M, Zeng H, Wang S, Tang H, Gao X. Insights into contribution of genetic variants towards the susceptibility of MAFLD revealed by the NMR-based lipoprotein profiling. J Hepatol. 2021;74(4):974–977
Article CAS PubMed Google Scholar - Xia MF, Yan HM, He WY, Li XM, Li CL, Yao XZ, et al. Standardized ultrasound hepatic/renal ratio and hepatic attenuation rate to quantify liver fat content: an improvement method. Obesity (Silver Spring). 2012;20:444–452
Article CAS PubMed Google Scholar - Stein JH, Korcarz CE, Hurst RT, Lonn E, Kendall CB, Mohler ER, et al. Use of carotid ultrasound to identify subclinical vascular disease and evaluate cardiovascular disease risk: a consensus statement from the American society of echocardiography carotid intima-media thickness task force. Endorsed by the society for vascular medicine. J Am Soc Echocardiogr. 2008;21(2):93–111
Article PubMed Google Scholar - Jiménez B, Holmes E, Heude C, Tolson RF, Harvey N, Lodge SL, et al. Quantitative lipoprotein subclass and low molecular weight metabolite analysis in human serum and plasma by 1 H NMR spectroscopy in a multilaboratory trial. Anal Chem. 2018;90(20):11962–11971
Article PubMed Google Scholar - Xia MF, Ma S, Huang QX, Zeng HL, Ge JY, Xu WJ, et al. NAFLD-related gene polymorphisms and all-cause and cause-specific mortality in an Asian population: the Shanghai Changfeng Study. Aliment Pharmacol Ther. 2022;55(6):705–721
Article CAS PubMed Google Scholar - European Association for the Study of the Liver (EASL), European Association for the Study of Diabetes (EASD), European Association for the Study of Obesity. EASL-EASD-EASO clinical practice guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016;64(6):1388–402
Article Google Scholar - Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, et al. Sarcopenia in Asia: consensus report of the Asian working group for sarcopenia. J Am Med Dir Assoc. 2014;15(2):95–101
Article PubMed Google Scholar - Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet. 2019;393(10191):2636–2646
Article PubMed Google Scholar - Bhanji RA, Narayanan P, Allen AM, Malhi H, Watt KD. Sarcopenia in hiding: the risk and consequence of underestimating muscle dysfunction in nonalcoholic steatohepatitis. Hepatology. 2017;66(6):2055–2065
Article CAS PubMed Google Scholar - Kim JA, Choi KM. Sarcopenia and fatty liver disease. Hepatol Int. 2019;13(6):674–687
Article CAS PubMed Google Scholar - Han YH, Onufer EJ, Huang LH, Sprung RW, Davidson WS, Czepielewski RS, et al. Enterically derived high-density lipoprotein restrains liver injury through the portal vein. Science. 2021;373(6553):eabe6729
Article CAS PubMed PubMed Central Google Scholar - Xie G, Wang X, Wei R, Wang J, Zhao A, Chen T, et al. Serum metabolite profiles are associated with the presence of advanced liver fibrosis in Chinese patients with chronic hepatitis B viral infection. BMC Med. 2020;18(1):144
Article CAS PubMed PubMed Central Google Scholar - Yu D, Richardson NE, Green CL, Spicer AB, Murphy ME, Flores V, et al. The adverse metabolic effects of branched-chain amino acids are mediated by isoleucine and valine. Cell Metab. 2021;33(5):905-922.e6
Article CAS PubMed PubMed Central Google Scholar - Xia MF, Chen LY, Wu L, Ma H, Li XM, Li Q, et al. Sarcopenia, sarcopenic overweight/obesity and risk of cardiovascular disease and cardiac arrhythmia: a cross-sectional study. Clin Nutr. 2021;40(2):571–580
Article PubMed Google Scholar - Ko BJ, Chang Y, Jung HS, Yun KE, Kim CW, Park HS, et al. Relationship between low relative muscle mass and coronary artery calcification in healthy adults. Arterioscler Thromb Vasc Biol. 2016;36(5):1016–1021
Article CAS PubMed Google Scholar - Brown JC, Harhay MO, Harhay MN. Sarcopenia and mortality among a population-based sample of community-dwelling older adults. J Cachexia Sarcopenia Muscle. 2016;7(3):290–298
Article PubMed Google Scholar - Xu Y, Jiang H, Li L, Chen F, Liu Y, Zhou M, et al. Branched-chain amino acid catabolism promotes thrombosis risk by enhancing tropomodulin-3 propionylation in platelets. Circulation. 2020;142(1):49–64
Article CAS PubMed Google Scholar - Yeung S, Zhu Z, Kwok T, Woo J. Serum amino acids patterns and 4-year sarcopenia risk in community-dwelling chinese older adults. Gerontology. 2022;68:736–745
Article CAS PubMed Google Scholar - Ma S, Xia M, Gao X. Biomarker discovery in atherosclerotic diseases using quantitative nuclear magnetic resonance metabolomics. Front Cardiovasc Med. 2021;8:681444
Article CAS PubMed PubMed Central Google Scholar - Gong H, Liu Y, Lyu X, Dong L, Zhang X. Lipoprotein subfractions in patients with sarcopenia and their relevance to skeletal muscle mass and function. Exp Gerontol. 2022;159:111668
Article CAS PubMed Google Scholar
Funding
We have obtained financial supports from the Ministry of Science and Technology of China (2018YFE0201603, 2020YFE0201600), the Shanghai Pujiang Talent Project (20PJ1402300), the Shanghai Municipal Science and Technology Major Project (2017SHZDZX01), the Science and Technology Commission of Shanghai Municipality (16JC1400500, 16411954800), the National Natural Science Foundation of China (81873660, 31821002 and 82100849), and Foundations from Zhongshan Hospital, Fudan University (2020ZSLC58, 2021ZSQN07).
Author information
Author notes
- Xiaopeng Zhu, Qingxia Huang and Shuai Ma have contributed equally to this work.
Authors and Affiliations
- Department of Endocrinology and Metabolism, Zhongshan Hospital, Fudan Institute for Metabolic Diseases, Fudan University, 180 Fenglin Rd, Shanghai, 200032, China
Xiaopeng Zhu, Shuai Ma, Qi Wu, Li Wu, Xiaoming Li, Qian Li, Qiqige Aleteng, Huandong Lin, Xin Gao & Mingfeng Xia - State Key Laboratory of Genetic Engineering, School of Life Sciences, Metabonomics and Systems Biology Laboratory at Shanghai International Centre for Molecular Phenomics, Human Phenome Institute, Zhongshan Hospital, Fudan University, 825 Zhangheng Rd, Shanghai, 200438, China
Qingxia Huang & Huiru Tang - Department of Geriatrics, Zhongshan Hospital, Fudan University, Shanghai, China
Lingyan Chen, Hui Ma & Yu Hu - Department of Ultrasonography, Zhongshan Hospital, Fudan University, Shanghai, China
Wanyuan He - Department of Nutrition, Center of Clinical Epidemiology and EBM, Zhongshan Hospital, Fudan University, Shanghai, China
Jian Gao
Authors
- Xiaopeng Zhu
- Qingxia Huang
- Shuai Ma
- Lingyan Chen
- Qi Wu
- Li Wu
- Hui Ma
- Xiaoming Li
- Qian Li
- Qiqige Aleteng
- Yu Hu
- Wanyuan He
- Jian Gao
- Huandong Lin
- Huiru Tang
- Xin Gao
- Mingfeng Xia
Contributions
Study concept and design: MX, XG, HT. Acquisition of data: XZ, QH, SM, LC, QW, LW, XL, HM, QL, QA, MX, HL. Analysis of data: XZ, SM, QH, JG, MX. Technic support and data interpretation: QH, WH. Data management: HL. Manuscript drafting: XZ, MX. Manuscript revision: MX, XG, HT, YH. Obtained funding; XG, HT, MX, XZ. MX and XG are the guarantors of this work and, as such, takes responsibility for the integrity of the work as a whole, from inception to published article.
Corresponding authors
Correspondence toHuiru Tang, Xin Gao or Mingfeng Xia.
Ethics declarations
Conflict of interests
Xiaopeng Zhu declares that there is no duality of interest. Qingxia Huang declares that there is no duality of interest. Shuai Ma declares that there is no duality of interest. Lingyan Chen declares that there is no duality of interest. Qi Wu declares that there is no duality of interest. Li Wu declares that there is no duality of interest. Hui Ma declares that there is no duality of interest. Xiaoming Li declares that there is no duality of interest. Qian Li declares that there is no duality of interest. Qiqige Aleteng declares that there is no duality of interest. Yu Hu declares that there is no duality of interest. Wanyuan He declares that there is no duality of interest. Jian Gao declares that there is no duality of interest. Huandong Lin declares that there is no duality of interest. Huiru Tang declares that there is no duality of interest. Xin Gao declares that there is no duality of interest. Mingfeng Xia declares that there is no duality of interest.
Ethical approval
The study was approved by the Research Ethics Committees of Zhongshan Hospital, Fudan University (No. 2008-119 and B2013-132).
Informed consent
Each participant provided written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhu, X., Huang, Q., Ma, S. et al. Presence of sarcopenia identifies a special group of lean NAFLD in middle-aged and older people.Hepatol Int 17, 313–325 (2023). https://doi.org/10.1007/s12072-022-10439-z
- Received: 14 July 2022
- Accepted: 09 October 2022
- Published: 03 November 2022
- Version of record: 03 November 2022
- Issue date: April 2023
- DOI: https://doi.org/10.1007/s12072-022-10439-z