Metabolic associated fatty liver disease better identifying patients at risk of liver and cardiovascular complications (original) (raw)
Abstract
Background/purpose
A nomenclature of “metabolic associated fatty liver disease” (MAFLD) with a new definition was proposed in 2020 instead of the previous “non-alcoholic fatty liver disease” (NAFLD). Whether it better coheres with the clinical demand remains controversial.
Methods
The participants with fatty liver on ultrasonography in Taiwan bio-bank cohorts were included. MAFLD is defined as the presence of fatty liver, plus any of the following three conditions: overweight/obesity, type 2 diabetes mellitus (DM), or metabolic dysfunction. The severity of liver fibrosis was determined using fibrosis-4 (FIB-4) index and NAFLD fibrosis score (NFS). The risk of atherosclerotic cardiovascular disease was assessed using intima–media thickness (IMT) or plaques of carotid duplex ultrasound.
Results
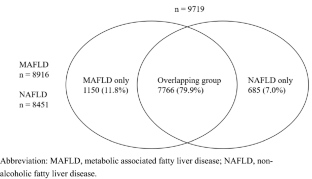
A total of 9,719 subjects (ages 55.9 ± 10.8; males 42.6%) were distributed among 4 groups: “overlapping group”, “MAFLD only”, “NAFLD only”, and “neither fatty liver disease (FLD)” with the percentages of 79.7, 12, 7.1, and 1.2%, respectively. Compared with NAFLD patients, MAFLD patients had a greater percentage of males, higher levels of BMI, waist circumference, HbA1c, and triglyceride. In addition, they had higher levels of serum ALT, AST, GGT, fatty liver index (FLI), NFS, and IMT, but no difference in FIB-4 index and the percentage of carotid plaques. To note, “MAFLD only group” had greater levels of AST, ALT, GGT, FLI, FIB-4, NFS, IMT and a higher percentage of carotid plaques than the “NAFLD only group”.
Conclusion
The grand, population-based study showed MAFLD with new diagnostic criteria to aid in identifying a greater number of high-risk patients of metabolic, liver, and cardiovascular complications, suggesting MAFLD may be a better nomenclature than NAFLD in clinical practice.
Access this article
Subscribe and save
- Starting from 10 chapters or articles per month
- Access and download chapters and articles from more than 300k books and 2,500 journals
- Cancel anytime View plans
Buy Now
Price excludes VAT (USA)
Tax calculation will be finalised during checkout.
Instant access to the full article PDF.
Fig. 1
Similar content being viewed by others
References
- Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73–84
Article PubMed Google Scholar - Farrell GC, Larter CZ. Nonalcoholic fatty liver disease: from steatosis to cirrhosis. Hepatology (Baltimore, MD). 2006;43:S99–S112
Article CAS PubMed Google Scholar - Starley BQ, Calcagno CJ, Harrison SA. Nonalcoholic fatty liver disease and hepatocellular carcinoma: a weighty connection. Hepatology. 2010;51(5):1820–1832
Article PubMed Google Scholar - Asrih M, Jornayvaz FR. Metabolic syndrome and nonalcoholic fatty liver disease: is insulin resistance the link? Mol Cell Endocrinol. 2015;418(Pt 1):55–65
Article CAS PubMed Google Scholar - Dharmalingam M, Yamasandhi PG. Nonalcoholic Fatty Liver Disease and Type 2 Diabetes Mellitus. Indian J Endocrinol Metab. 2018;22:421–428
Article CAS PubMed PubMed Central Google Scholar - Brunner KT, Pedley A, Massaro JM, Hoffmann U, Benjamin EJ, Long MT. Increasing liver fat is associated with progression of cardiovascular risk factors. Liver Int. 2020;40:1339–1343
Article CAS PubMed PubMed Central Google Scholar - Brea A, Puzo J. Non-alcoholic fatty liver disease and cardiovascular risk. Int J Cardiol. 2013;167:1109–1117
Article PubMed Google Scholar - Paik JM, Golabi P, Younossi Y, Mishra A, Younossi ZM. Changes in the global burden of chronic liver diseases from 2012 to 2017: the growing impact of NAFLD. Hepatology. 2020;72(5):1605–1616
Article PubMed Google Scholar - Pal P, Palui R, Ray S. Heterogeneity of non-alcoholic fatty liver disease: Implications for clinical practice and research activity. World J Hepatol. 2021;13(11):1584–1610
Article PubMed PubMed Central Google Scholar - Eslam M, Sanyal AJ, George J. International Consensus Panel MAFLD a consensus-driven proposed nomenclature for metabolic associated fatty liver disease. Gastroenterology. 2020;158:1999-2014.e1
Article CAS PubMed Google Scholar - Eslam M, Newsome PN, Sarin SK, Anstee QM, Targher G, Romero-Gomez M, et al. A new definition for metabolic dysfunction associated fatty liver disease: an international expert consensus statement. J Hepatol. 2020;73:202–209
Article PubMed Google Scholar - Eslam M, Ahmed A, Després JP, Jha V, Halford JCG, Wei Chieh JT, et al. Incorporating fatty liver disease in multidisciplinary care and novel clinical trial designs for patients with metabolic diseases. Lancet Gastroenterol Hepatol. 2021;6(9):743–753
Article PubMed Google Scholar - Sarin SK, Eslam M, Fan JG, Lin HC, George J, Omata M. MAFLD, patient-centred care, and APASL. Hepatol Int. 2022;16:1032–1034 (Published online ahead of print, 2022 Sep 7)
Article PubMed Google Scholar - Alharthi J, Gastaldelli A, Cua IH, Ghazinian H, Eslam M. Metabolic dysfunction-associated fatty liver disease: a year in review. Curr Opin Gastroenterol. 2022;38(3):251–260
Article CAS PubMed Google Scholar - Ciardullo S, Perseghin G. Prevalence of NAFLD, MAFLD and associated advanced fibrosis in the contemporary United States population. Liver Int. 2021;41:1290–1293
Article PubMed Google Scholar - Fan CT, Lin JC, Lee CH. Taiwan biobank: A project aiming to aid Taiwan’s transition into a biomedical island. Pharmacogenomics. 2008;9:235–246
Article PubMed Google Scholar - Lin JC, Fan CT, Liao CC, Chen YS. Taiwan biobank: Making cross-database convergence possible in the big data era. Gigascience. 2018;7:1–4
Article PubMed Google Scholar - Wang CC, Liu CH, Lin CL, Wang PC, Tseng TC, Lin HH, et al. Fibrosis index based on four factors better predicts advanced fibrosis or cirrhosis than aspartate aminotransferase/platelet ratio index in chronic hepatitis C patients. J Formos Med Assoc. 2015;114:923–928
Article PubMed Google Scholar - Angulo P, Hui JM, Marchesini G, et al. The NAFLD fibrosis score: A noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology. 2007;45(4):846–854
Article CAS PubMed Google Scholar - Bedogni G, Bellentani S, Miglioli L, et al. The Fatty Liver Index: a simple and accurate predictor of hepatic steatosis in the general population. BMC Gastroenterol. 2006;6:33
Article PubMed PubMed Central Google Scholar - Kabłak-Ziembicka A, Przewłocki T. Clinical significance of carotid intima-media complex and carotid plaque assessment by ultrasound for the prediction of adverse cardiovascular events in primary and secondary care patients. J Clin Med. 2021;10(20):4628
Article PubMed PubMed Central Google Scholar - Méndez-Sánchez N, Bugianesi E, Gish RG, Lammert F, Tilg H, Nguyen MH, et al. Global multi-stakeholder consensus on the redefinition of fatty liver disease. Global multi-stakeholder endorsement of the MAFLD definition. Lancet Gastroenterol Hepatol. 2022;7:388–390
Article PubMed Google Scholar - Eslam M, Sarin SK, Wong VW, Fan JG, Kawaguchi T, Ahn SH, et al. The Asian pacific association for the study of the liver clinical practice guidelines for the diagnosis and management of metabolic associated fatty liver disease. Hepatol Int. 2020;14(6):889–919
Article PubMed Google Scholar - Yu C, Wang M, Zheng S, Xia M, Yang H, Zhang D, et al. Comparing the diagnostic criteria of MAFLD and NAFLD in the Chinese population: a population-based prospective cohort study. J Clin Transl Hepatol. 2022;10(1):6–16
Article PubMed Google Scholar - Wong VW, Wong GL, Woo J, Abrigo JM, Chan CK, Shu SS, et al. Impact of the new definition of metabolic associated fatty liver disease on the epidemiology of the disease. Clin Gastroenterol Hepatol. 2021;19(10):2161-2171.e5
Article CAS PubMed Google Scholar - Lin S, Huang J, Wang M, Kumar R, Liu Y, Liu S, et al. Comparison of MAFLD and NAFLD diagnostic criteria in real world. Liver Int. 2020;40:2082–2089
Article PubMed Google Scholar - Dhar D, Baglieri J, Kisseleva T, Brenner DA. Mechanisms of liver fibrosis and its role in liver cancer. Exp Biol Med (Maywood). 2020;245(2):96–108
Article CAS PubMed Google Scholar - Libby P, Ridker PM, Hansson GK. Progress and challenges in translating the biology of atherosclerosis. Nature. 2011;473:317–325
Article CAS PubMed Google Scholar - Huang SC, Su HJ, Kao JH, Tseng TC, Yang HC, Su TH, et al. Clinical and histologic features of patients with biopsy-proven metabolic dysfunction-associated fatty liver disease. Gut Liver. 2021;15:451–458
Article PubMed PubMed Central Google Scholar - Yamamura S, Eslam M, Kawaguchi T, Tsutsumi T, Nakano D, Yoshinaga S, et al. MAFLD better identifies patients with significant hepatic fibrosis than NAFLD. Liver Int. 2020;40:3018–3030
Article CAS PubMed Google Scholar - Lee H, Lee YH, Kim SU, Kim HC. Metabolic dysfunction-associated fatty liver disease and incident cardiovascular disease risk: a nationwide cohort study. Clin Gastroenterol Hepatol. 2021;19:2138–2147
Article PubMed Google Scholar - Niriella MA, Ediriweera DS, Kasturiratne A, De Silva ST, Dassanayaka AS, De Silva AP, et al. Outcomes of NAFLD and MAFLD: results from a community-based, prospective cohort study. PLoS ONE. 2021;16: e0245762
Article CAS PubMed PubMed Central Google Scholar - Tsutsumi T, Eslam M, Kawaguchi T, Yamamura S, Kawaguchi A, Nakano D, et al. MAFLD better predicts the progression of atherosclerotic cardiovascular risk than NAFLD: Generalized estimating equation approach. Hepatol Res. 2021;51:1115–1128
Article CAS PubMed Google Scholar - Huang J, Kumar R, Wang M, Zhu Y, Lin S. MAFLD criteria overlooks a number of patients with severe steatosis: is it clinically relevant? J Hepatol. 2020;73:1265–1267
Article PubMed Google Scholar - Huang J, Xue W, Wang M, Yinlian Wu, Singh M, et al. MAFLD criteria may overlook a subset of patients with steatohepatitis and significant fibrosis. Diabetes Metab Syndr Obes. 2021;14:3417–3425
Article PubMed PubMed Central Google Scholar - Huang S-C, Kao J-H. Metabolic dysfunction-associated fatty liver disease and chronic hepatitis B. J Formos Med Assoc. 2022;121:2148–2151
Article CAS PubMed Google Scholar
Funding
This work was supported by grants from Taipei Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation (TCRD-TPE-111–09) and the Taiwan Liver Disease Consortium, Ministry of Science and Technology, Taiwan (MOST 109-2314-B-002-091-MY3).
Author information
Authors and Affiliations
- Department of Gastroenterology and Hepatology, Tung’s Taichung MetroHarbor Hospital, Taichung, Taiwan
Yu-Ming Cheng - Department of Gastroenterology, Buddhist Tzu Chi Medical Foundation and School of Medicine, Taipei Tzu Chi Hospital, Tzu Chi University, Hualien, Taiwan
Chia-Chi Wang - Division of Gastroenterology and Hepatology, Department of Internal Medicine, National Taiwan University Hospital, Taipei, Taiwan
Jia-Horng Kao - Graduate Institute of Clinical Medicine, National Taiwan University College of Medicine, Taipei, Taiwan
Jia-Horng Kao - Medical Department, Buddhist Tzu Chi Medical Foundation and School of Medicine, Taipei Tzu Chi Hospital, Tzu Chi University, 289 Jianguo Rd., Xindian Area, New Taipei City, 23142, Taiwan
Chia-Chi Wang
Authors
- Yu-Ming Cheng
- Chia-Chi Wang
- Jia-Horng Kao
Corresponding author
Correspondence toChia-Chi Wang.
Ethics declarations
Conflict of interest
Yu-Ming Cheng, Chia-Chi Wang, and Jia-Horng Kao declare no conflict and interest.
Ethical considerations
This study was performed in accordance with the principles of the 1975 Declaration of Helsinki and approved by the Research Ethics Committee of Taipei Tzu Chi Hospital; Buddhist Tzu Chi Medical Foundation (approval numbers: 10-XD-055 and 11-X-074) with waived informed consent and the Ethics and Governance Council of the TWB (approval numbers: TWBR11102-03).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cheng, YM., Wang, CC. & Kao, JH. Metabolic associated fatty liver disease better identifying patients at risk of liver and cardiovascular complications.Hepatol Int 17, 350–356 (2023). https://doi.org/10.1007/s12072-022-10449-x
- Received: 02 September 2022
- Accepted: 04 November 2022
- Published: 05 December 2022
- Version of record: 05 December 2022
- Issue date: April 2023
- DOI: https://doi.org/10.1007/s12072-022-10449-x