Evaluation of Antibody-Dependent Enhancement of SARS-CoV Infection in Rhesus Macaques Immunized with an Inactivated SARS-CoV Vaccine (original) (raw)
Dear Editor,
In 2003, severe acute respiratory syndrome coronavirus (SARS-CoV) emerged in Guangdong Province, China, infected more than 8000 individuals, and resulted in a 10% mortality rate (Rota et al. 2003). Later, in 2012, a novel CoV, Middle East respiratory syndrome coronavirus (MERS-CoV), was isolated from the sputum of a man in Saudi Arabia (Perl et al. 2014). Notably, MERS-CoV recently reemerged in the Republic of Korea, and killed 36 out of 186 confirmed cases (Korea Centers for Disease Control and Prevention 2015). Therefore, SARS-CoV still carries the potential for resurgence; efforts are being made to prevent the recurrence of an epidemic.
Currently, effective antiviral strategies to control SARS-CoV infections are lacking; vaccination is still regarded as the major approach for preventing SARS and related diseases. Generally, virus-specific antibodies play important roles in the control of viral infections. However, the presence of specific antibodies can be beneficial for infection in case of some viruses including flaviviruses, CoVs, and retroviruses (de Alwis et al. 2014; Jolly and Weiss 2000; Takano et al. 2008). Vaccine-induced enhancement of susceptibility to SARS-CoV has been documented. One study showed that the antibody against SARS-CoV spikes protein potentiated infection of both monocytic and lymphoid cell lines, which do not express the virus receptor, and reported antibody-dependent enhancement (ADE)-mediated vaccine-induced infection aggravation (Yip et al. 2014). We previously reported that an inactivated SARS-CoV Z-1 vaccine effectively elicits a neutralizing and protective antibody response in rhesus macaques (Luo et al. 2007; Zhou et al. 2005). Thus, to ensure the safety of the vaccine in clinical use, the present study examined whether the vaccine can trigger ADE.
It has been demonstrated that higher concentrations of anti-sera against SARS-CoV neutralized the SARS-CoV infection, while highly diluted anti-sera significantly increased the SARS-CoV infection and triggered ADE effects (Wang et al. 2014). Moreover, the low levels of neutralizing antibodies are more consistent in the context of vaccination of the general population. The findings from the low neutralizing antibody stage challenges were promising. Therefore, to determine the ADE of the inactivated SARS-CoV vaccine, we first established the model with low levels of neutralizing antibodies. Sixteen adult Chinese rhesus macaques (No. 1–16, 8 male and 8 female, 3.5–4.5 kg, 2–4-year-old) were individually housed in isolator cages at the Animal Biosafety Level (ABSL)-III laboratory of Wuhan University (Wuhan, China). The monkeys were randomized into 3 groups (8 monkeys in the immunized group, 4 monkeys in the virus control group, and 4 monkeys in the negative control group; male and female monkeys were equally assigned to each group), and immunized intramuscularly with 2.5 μg beta-propiolactone-inactivated whole SARS-CoV Z-1 vaccine or PBS as control, and boosted on day 7. The blood was collected at 0, 4, 6, 7, 8, 9 weeks post-immunization. The neutralizing antibodies were tested by a 50% plaque reduction neutralization test. Following the immunization, each animal was monitored daily for clinical signs such as changes in activity, rectal temperature, appetite, frequency of defecation, and stool consistency. Hematological examination was tested on pocH-100i (SYSMEX, Kobe, Japan). Serum alanine aminotransferase (ALT), aspartate aminotranferase (AST), total bilirubin (TBiL), total protein (TP), urea, creatinine (Crea), and alkaline phosphatase (ALP) levels were detected on the semi-automatic biochemical analyzer RT-1904C (Rayto Corporation, Shenzhen) to evaluate the liver and kidney functions. We observed that the clinical signs of all animals were normal (data not shown). No systemic complications were observed and none of the monkeys showed a skin rash at the vaccine injection site. Hematological assay results were in the normal range (Supplementary Table S1). No elevation of biochemical indices was observed after immunization (Supplementary Table S2). As shown in Fig. 1A, the neutralizing antibody titers of monkeys were below 10 at 9 weeks after the first immunization, which was consistent with the study requirement (Woo et al. 2005). The results suggested that the inactivated vaccine was safe and the immunized rhesus macaques could be used as the model for testing ADE of the candidate vaccine.
Fig. 1
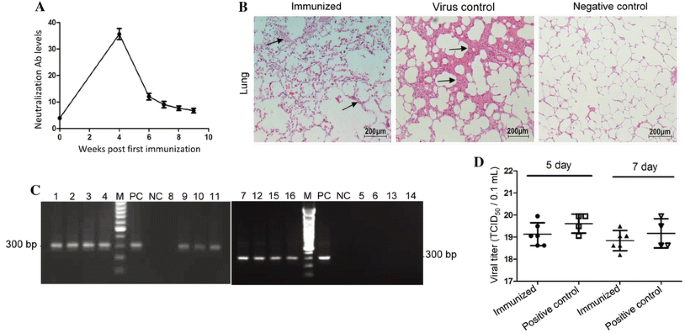
Low levels of neutralizing antibodies induced by the inactivated vaccine SARS-CoV Z-1 do not trigger ADE following the challenge. A Rhesus macaques were immunized intramuscularly with 2.5 μg beta-propiolactone-inactivated whole SARS-CoV Z-1 vaccine or PBS as control, and boosted on day 7. The blood was collected at 0, 4, 6, 7, 8, 9 weeks post-immunization. Titers were expressed as the reciprocal of the dilution at which 50% of the plaques reduced completely in the virus-wells. Data were presented as the mean ± S.E. for each group. B On day 10 or 14 post-infection, the surviving monkeys from the three groups were euthanized and necropsied; the lungs were collected and fixed using 4% formaldehyde, sectioned, and subjected to hematoxylin and eosin staining. Magnification, ×200. The arrows refer to the widening of alveolar septa and the infiltration of inflammatory cells. C The nasopharyngeal swabs were collected on day 2 post-challenge. The presence of SARS-CoV polymerase gene in the swabs was confirmed by RT-PCR. No. 1, 2, 3, 4, 8, 9, 10, and 11 lanes are from immunized group; No. 7, 12, 15, and 16 lanes are from virus control group; No. 5, 6, 13, 14 lanes are the swabs from negative control group; M, molecular size marker; PC, purified virus as positive control; NC, without cDNA template. D The virus titers of the sera from the monkeys whose samples showed positive results in virus isolation were detected on days 5 and 7 post-challenge by TCID50. The values of the titer were expressed directly by the calculated number.
Next, we used the above-established model to evaluate the correlation between the vaccine and the infection severity. At week 9 post-immunization, 8 immunized monkeys (No. 1–4 and 8–11) and 4 virus control monkeys (No. 7, 12, 15, 16) were intratracheally challenged with the SARS-CoV NS-1 at 5 × 106.7 50% tissue culture infectious doses (TCID50) per animal. Four negative control monkeys (No. 5, 6, 13, 14) were challenged with PBS as control. The blood and nasopharyngeal secretions were collected on days 2, 5, 7, 9, and 11 post-challenge for virological evaluation. The animals were provided with full supportive care and humanely killed on day 10 (No. 1, 3, 5, 7, 9, 11, 13, and 15) and 14 (No. 2, 4, 6, 8, 10, 12, 14, and 16) post-infection. The lung tissues were fixed in formalin, embedded, sectioned, and stained with hematoxylin and eosin for pathological observation. The homogenates of the lung lobes were prepared for the RT-PCR assay of SARS-CoV and virus isolation.
Following the virus challenge, no remarkable rectal temperature changes were noted in all the vaccine-immunized animals. Other clinical symptoms such as coughing, lethargy, and rash were not observed in the vaccinated animals. Likewise, normal body weight gain was observed in all the vaccinated animals. All the infected or non-infected monkeys remained alive before being sacrificed.
As shown in Fig. 1B, histopathological observations indicated that monkeys in the virus control group had obvious interstitial pneumonia, including thickening of the alveolar wall and infiltration of mononuclear cells and lymphocytes. Interstitial pneumonia was also observed in the immunized group, but fewer pathological changes were observed. According to the degree of the histopathological changes, among the virus control group, one monkey presented the most severe interstitial pneumonia, two monkeys displayed moderate interstitial pneumonia, and one monkey had slight interstitial pneumonia. Meanwhile, in the immunized group, four monkeys developed moderate interstitial pneumonia and four other monkeys had mild interstitial pneumonia.
The infectious virus was isolated from various samples that were collected from the monkeys at different time points post-challenge. Filtered nasopharyngeal washings, serum, or 10% lung tissue homogenates were inoculated onto Vero-E6 cell monolayer in 6-well plates (Costar, Corning, Inc., USA). The culture plates were observed for 7 days and blindly passaged two times if no SARS-CoV-specific cytopathogenic effects (CPE) were exhibited. The positive rate of virus isolation in the nasopharyngeal swabs and sera from immunized monkeys was lower than that of virus control in general. However, the positive rate of virus isolation was consistent among the lung specimens (as shown in Table 1).
Table 1 Detection of SARS-CoV in various specimens from the three groups on different days post-challenge.
RT-PCR was used to test the presence of the polymerase gene of SARS-CoV in the nasopharyngeal secretions, sera, and lungs of monkeys from the three groups. The forward and reverse primers were 5′-CACCGTTTCTACAGGTTAGCTAACGA-3′ and 5′-AAATGTTTACGCAGGTAACGTAAAA-3′, respectively. The rate of viral RNA detection in nasopharyngeal secretions and sera taken from the immunized group was lower than that in the virus control group on days 2 and 5 post-challenge; the lungs of the monkeys in the immunized group and the virus control group were positive on days 10 and 14 post-challenge, respectively; the positive rate was consistent, which correlated with the virus isolation results (Table 1). The nasopharyngeal secretions obtained from the immunized group and the virus control group on day 2 post-challenge were positive for SARS-CoV RNA (Fig. 1C).
The viral titers of the monkey sera that were positive for virus were determined on days 5 and 7 post-challenge. The virus titer was calculated by the Reed-Muench formula and expressed as TCID50/0.1 mL (Reed and Muench 1938). As shown in Fig. 1d, although the virus titer of the immunized group was slightly lower than that of the virus control group universally, this difference was not statistically significant. Altogether, the results indicated that SARS-CoV replication in the immunized group was not enhanced.
Until now, several SARS-CoV vaccines have been developed using different vaccine platforms, including whole inactivated, DNA, subunit, and vectored vaccines (Enjuanes et al. 2008; Roberts et al. 2008). The immunogenicity and efficacy of these experimental vaccines have been evaluated in animal models such as mice, ferrets, hamsters, and non-human primates (Roberts et al. 2008). The monkey is the most widely studied animal model in SARS research. Similar to another study (Qin et al. 2006) on inactivated SARS vaccine in monkeys, in our previous study, the inactivated SARS-CoV Z-1 vaccine that elicits a robust serum-neutralizing antibody response in rhesus macaque provides protection from challenge with virus. Nevertheless, at least one report has indicated that a SARS-CoV vaccine candidate based on recombinant full-length SARS-CoV spikes protein triggered infection of human B cell lines in vitro despite eliciting a neutralizing and protective immune response in rodents (Kam et al. 2007). Additionally, at least two studies have shown that anti-SARS-CoV-spiked immune serum potentiates infection of immune cell lines by SARS-CoV because of antibody-mediated ADE (Jaume et al. 2011; Wang et al. 2014). Meanwhile, another research group performed the ADE assays using sera from patients positive for SARS-CoV. The research data showed that treatment of human promonocyte with more diluted anti-sera collected from patients positive for SARS-CoV resulted in increased virus infectivity and cytopathic effect (Wang et al. 2014). Therefore, in our present study, although the clinical and histopathological observations, and viral assays indicated that the virus infection was not enhanced, we believe that an in vitro ADE assay should also be performed to examine whether the immune sera induced by inactivated vaccine can mediate ADE in some cell lines such as K562, THP-1 cells, and monkey’s peripheral blood mononuclear cells. Moreover, we need to investigate the molecular mechanisms and responses to antibody-mediated infection in vitro.
In conclusion, the clinical, virological, and pathological findings presented in this study revealed no exacerbation of infection in the rhesus macaques immunized with the inactivated SARS-CoV Z-1 vaccine following challenge with SARS-CoV NS-1. Therefore, these results preliminarily indicated that low levels of antibodies induced by the inactivated SARS-CoV Z-1 vaccine may not induce ADE in rhesus macaques, and the vaccine could be a good candidate for clinical trials.
References
- de Alwis R, Williams KL, Schmid MA, Lai CY, Patel B, Smith SA, Crowe JE, Wang WK, Harris E, de Silva AM (2014) Dengue viruses are enhanced by distinct populations of serotype cross-reactive antibodies in human immune sera. PLoS Pathog 10:e1004386
Article PubMed PubMed Central Google Scholar - Enjuanes L, Dediego ML, Alvarez E, Deming D, Sheahan T, Baric R (2008) Vaccines to prevent severe acute respiratory syndrome coronavirus-induced disease. Virus Res 133:45–62
Article CAS PubMed Google Scholar - Jaume M, Yip MS, Cheung CY, Leung HL, Li PH, Kien F, Dutry I, Callendret B, Escriou N, Altmeyer R, Nal B, Daëron M, Bruzzone R, Peiris JS (2011) Anti-severe acute respiratory syndrome coronavirus spike antibodies trigger infection of human immune cells via a pH- and cysteine protease-independent FcgammaR pathway. J Virol 85:10582–10597
Article CAS PubMed PubMed Central Google Scholar - Jolly PE, Weiss HL (2000) Neutralization and enhancement of HIV-1 infection by Sera from HIV-1 infected individuals who progress to disease at different rates. Virology 273:52–59
Article CAS PubMed Google Scholar - Kam YW, Kien F, Roberts A, Cheung YC, Lamirande EW, Vogel L, Chu SL, Tse J, Guarner J, Zaki SR, Subbarao K, Peiris M, Nal B, Altmeyer R (2007) Antibodies against trimeric S glycoprotein protect hamsters against SARS-CoV challenge despite their capacity to mediate FcgammaRII-dependent entry into B cells in vitro. Vaccine 25:729–740
Article CAS PubMed Google Scholar - Korea Centers for Disease Control and Prevention (2015) Middle east respiratory syndrome coronavirus outbreak in the Republic of Korea, 2015. Osong Public Health Res Perspect 6:269–278
Article PubMed Central Google Scholar - Luo F, Hou W, Yang ZQ, Tang ZJ, Wang Y, Xian QY, Sun LH (2007) Intratracheal inoculation of severe acute respiratory syndrome coronavirus in monkeys Macaca rhesus. Acta Virol 51:171–177
CAS PubMed Google Scholar - Perl TM, McGeer A, Price CS (2014) Medusa’s ugly head again: from SARS to MERS-CoV. Ann Intern Med 160:432–433
Article PubMed Google Scholar - Qin E, Shi H, Tang L, Wang C, Chang G, Ding Z, Zhao K, Wang J, Chen Z, Yu M, Si B, Liu J, Wu D, Cheng X, Yang B, Peng W, Meng Q, Liu B, Han W, Yin X, Duan H, Zhan D, Tian L, Li S, Wu J, Tan G, Li Y, Li Y, Liu Y, Liu H, Lv F, Zhang Y, Kong X, Fan B, Jiang T, Xu S, Wang X, Li C, Wu X, Deng Y, Zhao M, Zhu Q (2006) Immunogenicity and protective efficacy in monkeys of purified inactivated Vero-cell SARS vaccine. Vaccine 24:1028–1034
Article CAS PubMed Google Scholar - Reed LJ, Muench H (1938) A simple method of estimating fifty percent endpoints. Am J Hyg 27:493–497
Google Scholar - Roberts A, Lamirande EW, Vogel L, Jackson JP, Paddock CD, Guarner J, Zaki SR, Sheahan T, Baric R, Subbarao K (2008) Animal models and vaccines for SARS-CoV infection. Virus Res 133:20–32
Article CAS PubMed Google Scholar - Rota PA, Oberste MS, Monroe SS, Nix WA, Campagnoli R, Icenogle JP, Peñaranda S, Bankamp B, Maher K, Chen MH, Tong S, Tamin A, Lowe L, Frace M, DeRisi JL, Chen Q, Wang D, Erdman DD, Peret TC, Burns C, Ksiazek TG, Rollin PE, Sanchez A, Liffick S, Holloway B, Limor J, McCaustland K, Olsen-Rasmussen M, Fouchier R, Günther S, Osterhaus AD, Drosten C, Pallansch MA, Anderson LJ, Bellini WJ (2003) Characterization of a novel coronavirus associated with severe acute respiratory syndrome. Science 300:1394–1399
Article CAS PubMed Google Scholar - Takano T, Kawakami C, Yamada S, Satoh R, Hohdatsu T (2008) Antibody-dependent enhancement occurs upon re-infection with the identical serotype virus in feline infectious peritonitis virus infection. J Vet Med Sci 70:1315–1321
Article PubMed Google Scholar - Wang SF, Tseng SP, Yen CH, Yang JY, Tsao CH, Shen CW, Chen KH, Liu FT, Liu WT, Chen YM, Huang JC (2014) Antibody-dependent SARS coronavirus infection is mediated by antibodies against spike proteins. Biochem Biophys Res Commun 451:208–214
Article CAS PubMed Google Scholar - Woo PC, Lau SK, Tsoi HW, Chen ZW, Wong BH, Zhang L, Chan JK, Wong LP, He W, Ma C, Chan KH, Ho DD, Yuen KY (2005) SARS coronavirus spike polypeptide DNA vaccine priming with recombinant spike polypeptide from Escherichia coli as booster induces high titer of neutralizing antibody against SARS coronavirus. Vaccine 23:4959–4968
Article CAS PubMed Google Scholar - Yip MS, Leung NH, Cheung CY, Li PH, Lee HH, Daëron M, Peiris JS, Bruzzone R, Jaume M (2014) Antibody-dependent infection of human macrophages by severe acute respiratory syndrome coronavirus. Virol J 11:82
Article PubMed PubMed Central Google Scholar - Zhou J, Wang W, Zhong Q, Hou W, Yang Z, Xiao SY, Zhu R, Tang Z, Wang Y, Xian Q, Tang H, Wen L (2005) Immunogenicity, safety, and protective efficacy of an inactivated SARS-associated coronavirus vaccine in rhesus monkeys. Vaccine 23:3202–3209
Article CAS PubMed Google Scholar
Acknowledgements
This work was supported by the Chinese Medicine Foundation and Opening Foundation of State Key Laboratory of Virology, Wuhan University (No. 2016KF010).
Author information
Author notes
- Fan Luo and Fan-Lu Liao have contributed equally to this work.
Authors and Affiliations
- State Key Laboratory of Virology/Hubei Province Key Laboratory of Allergy and Immunology/Institute of Medical Virology, School of Basic Medical Sciences, Wuhan University, Wuhan, 430071, China
Fan Luo, Hui Wang, Zhan-Qiu Yang & Wei Hou - Department of Clinical Laboratory, Zhongnan Hospital, Wuhan University, Wuhan, 430071, China
Fan-Lu Liao - Center for Animal Experiment/Animal Biosafety Level-III Laboratory, Wuhan University, Wuhan, 430071, China
Hong-Bin Tang
Authors
- Fan Luo
You can also search for this author inPubMed Google Scholar - Fan-Lu Liao
You can also search for this author inPubMed Google Scholar - Hui Wang
You can also search for this author inPubMed Google Scholar - Hong-Bin Tang
You can also search for this author inPubMed Google Scholar - Zhan-Qiu Yang
You can also search for this author inPubMed Google Scholar - Wei Hou
You can also search for this author inPubMed Google Scholar
Corresponding author
Correspondence toWei Hou.
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest to disclose.
Animal and Human Rights Statement
All of the study protocols and procedures were approved by the Institutional Animal Care and Use Committee of Wuhan University.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Luo, F., Liao, FL., Wang, H. et al. Evaluation of Antibody-Dependent Enhancement of SARS-CoV Infection in Rhesus Macaques Immunized with an Inactivated SARS-CoV Vaccine.Virol. Sin. 33, 201–204 (2018). https://doi.org/10.1007/s12250-018-0009-2
- Received: 20 August 2017
- Accepted: 08 January 2018
- Published: 14 March 2018
- Issue Date: April 2018
- DOI: https://doi.org/10.1007/s12250-018-0009-2