Impact of obesity in elderly patients with postural instability (original) (raw)
Abstract
Objective
The aim of the study is to assess whether obesity affects balance in elderly patients with postural instability.
Study design
It is a case–control study, with cases defined by BMI ≥30 kg/m2, and developed in a third level university hospital.
Methods
We included 135 patients aged 65 years old or more who presented postural instability. Balance assessment was through the sensory organisation test (SOT), limits of stability (LOS) and rhythmic weight shift (RWS) of computerised dynamic posturography (CDP) and the modified timed up-and-go (TUG) test. The patients also completed the Dizziness Handicap Inventory and short Falls Efficacy Scale-International questionnaire.
Results
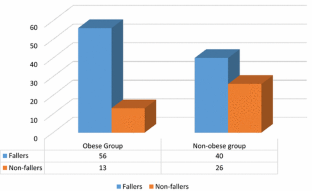
Patients with obesity took longer to perform the modified TUG and required more steps. Also these patients had poorer scores in the subjective tests. In the CDP there were no significant differences in the SOT nor the LOS, and only there was a statistical significant difference in the anterior-posterior directional control of the RWS. Obese patients have a higher risk of fallings compared to non-obese patients.
Conclusion
In essence, our results indicate that obesity interferes in the balance of elderly patients with postural instability, putting them at a greater risk of fallings, performing worse dynamic tasks and feeling more disabled. Although continued education on training balance may be useful in older population, since the obese group shows more rate of fallers, rehabilitation programmes focus on dynamic tasks in these patients could be useful to reduce their fall risk and improve their quality of life.
Access this article
Subscribe and save
- Starting from 10 chapters or articles per month
- Access and download chapters and articles from more than 300k books and 2,500 journals
- Cancel anytime View plans
Buy Now
Price excludes VAT (USA)
Tax calculation will be finalised during checkout.
Instant access to the full article PDF.
Fig. 1
Similar content being viewed by others
References
- Boult C, Murphy J, Sloane P et al (1991) The relation of dizziness to functional decline. J Am Geriatr Soc 39:858–861
Article CAS PubMed Google Scholar - Hale HE, Perkins LL, May FE et al (1986) Sympton prevalence in the elderly. An evaluation of age, sex, disease and medication use. J Am Geriatr Soc 34(5):333–341
Article CAS PubMed Google Scholar - Lin HW, Bhattacharyya N (2012) Balance disorders in the elderly: epidemiology and functional impact. Laryngoscope 122(8):1858–1861
Article PubMed Google Scholar - Arellano B, Camacho RR (2003) Patología vestibular en el anciano. In: Camacho RR (ed) Trastornos del equilibrio. Un abordaje multidisciplinario. McGraw-Hill Interamericana, Madrid, pp 307–310
Google Scholar - Neuhauser HK, von Brevern M, Radtke A et al (2005) Epidemiology of vestibular vertigo. A neurotologic survey of the general population. Neurology 65(6):898–904
Article CAS PubMed Google Scholar - Padilla Ruiz F, Bueno Cavanillas A, Peinado Alonso C et al (1998) Frecuencia, características y consecuencias de las caídas en una cohorte de ancianos institucionalizados. Aten Primaria 21(7):437–445
CAS PubMed Google Scholar - Lord SR, McLean D, Strathers G (1992) Physiological factors associated with injorius falls in older people living in the community. Gerontology 38:338–346
Article CAS PubMed Google Scholar - Faraldo-García A, Santos-Pérez S, Crujeiras-Casais R et al (2012) Influence of age and gender in the sensory analysis of balance control. Eur Arch Otorhinolaryngol 269(2):673–677
Article PubMed Google Scholar - Basta D, Rossi-Izquierdo M, Soto-Varela A et al (2013) Mobile posturography: posturographic analysis of daily-life mobility. Otol Neurotol 34(2):288–297
Article PubMed Google Scholar - Faraldo-García A, Santos-Pérez S, Labella-Caballero T et al (2011) Influence of gender on the sensory organisation test and the limits of stability in healthy subjects. Acta Otorrinolaringol Esp 62(5):333–338
Article PubMed Google Scholar - Hue O, Simoneau M, Marcotte J et al (2007) Body weight is a strong predictor of postural stability. Gait Posture 26(1):32–38
Article PubMed Google Scholar - Błaszczyk JW, Cieślinska-Swider J, Plewa M et al (2009) Effects of excessive body weight on postural control. J Biomech 42(9):1295–1300
Article PubMed Google Scholar - Young Y, Myers AH, Provenzano G (2001) Factors associated with time to first hip fracture. J Aging Health 13:511–526
Article CAS PubMed Google Scholar - Mitchell RJ, Lord SR, Harvey LA et al (2015) Obesity and falls in older people: mediating effects of disease, sedentary behavior, mood, pain and medication use. Arch Gerontol Geriatr 60(1):52–58
Article PubMed Google Scholar - Nashner LM (2011) Computerize dynamic posturography. In: Goebel JA (ed) Practical management of the dizzy patient. Lippincott Williams & Wilkins, Philadelphia, pp 143–170
Google Scholar - Girardi M, Konrad HR, Amin M et al (2001) Predicting fall risks in an elderly population: computer dynamic posturography versus electronystagmography test results. Laryngoscope 111(9):1528–1532
Article CAS PubMed Google Scholar - Podsiadlo D, Richardson S (1991) The timed ‘up and go’ test. J Am Geriatr Soc 39:142–148
Article CAS PubMed Google Scholar - Ashburn A, Stack E, Pickering RM et al (2001) A community-dwelling sample of people with Parkinson’s disease: characteristics of fallers and non-fallers. Age Ageing 30:47–52
Article CAS PubMed Google Scholar - Soto-Varela A, Gayoso-Diz P, Rossi-Izquierdo M et al (2015) Reduction of falls in older people by improving balance with vestibular rehabilitation (ReFOVeRe study): design and methods. Aging Clin Exp Res (In press). doi:10.1007/s40520-015-0362-z
Google Scholar - Rossi M, Soto A, Santos S et al (2009) A prospective study of alteration of balance among patients with Parkinson’s disease: protocol of the postural evaluation. Eur Neurol 61(3):171–176
Article CAS PubMed Google Scholar - Pérez N, Garmendia I, Martín E et al (2000) Adaptación cultural de dos cuestionarios de medida de la salud en pacientes con vértigo. Acta Otorrinolaringol Esp 51(7):572–580
PubMed Google Scholar - Kempen GI, Yardley L, van Haastregt JC et al (2008) The Short FES-I: a shortened version of the falls efficacy scale-international to assess fear of falling. Age Ageing 37(1):45–50
Article PubMed Google Scholar - Lin HW, Bhattacharyya N (2014) Impact of dizziness and obesity on the prevalence of falls and fall-related injuries. Laryngoscope 124:2797–2801
Article PubMed Google Scholar - Himes CL, Reynolds SL (2012) Effect of obesity on falls, injury, and disability. J Am Geriatr Soc 60(1):124–129
Article PubMed Google Scholar - Simoneau M, Teasdale N (2015) Balance control impairment in obese individuals is caused by larger balance motor commands variability. Gait Posture 41(1):203–208
Article PubMed Google Scholar - Corbeil P, Simoneau M, Rancourt D et al (2001) Increased risk of falling associated with obesity: mathematical modeling of postural control. IEEE Trans Neural Syst Rehabil Eng 9:126–136
Article CAS PubMed Google Scholar - Schoene D, Wu SM, Mikolaizak AS et al (2013) Discriminative ability and predictive validity of the timed up and go test in identifying older people who fall: systematic review and meta-analysis. J Am Geriatr Soc 61(2):202–208
Article PubMed Google Scholar - Rossi-Izquierdo M, Basta D, Rubio-Rodríguez JP et al (2014) Is posturography able to identify fallers in patients with Parkinson’s disease? Gait Posture 40(1):53–57
Article PubMed Google Scholar - Tinneti ME (2003) Clinical practice, preventing falls in elderly persons. N Engl J Med 348:42–49
Article Google Scholar
Acknowledgments
This study was supported by a grant of the National Institute of Health Carlos III (National R&D&I Plan, dossier PI11/01328).
Author information
Authors and Affiliations
- Department of Otolaryngology, University Hospital Lucus Augusti, Calle Dr. Ulises Romero, 1, 27003, Lugo, Spain
Marcos Rossi-Izquierdo - Department of Otolaryngology, Complexo Hospitalario, Universitario de Santiago de Compostela, Santiago de Compostela, Spain
Sofía Santos-Pérez, Ana Faraldo-García, Isabel Vaamonde-Sánchez-Andrade, María Del-Río-Valeiras, Antonio Lirola-Delgado & Andrés Soto-Varela - Clinical Epidemiology Unit, Hospital Clínico Universitario, Instituto de Investigación Sanitaria de Santiago (IDIS), Santiago de Compostela, Spain
Pilar Gayoso-Diz
Authors
- Marcos Rossi-Izquierdo
- Sofía Santos-Pérez
- Ana Faraldo-García
- Isabel Vaamonde-Sánchez-Andrade
- Pilar Gayoso-Diz
- María Del-Río-Valeiras
- Antonio Lirola-Delgado
- Andrés Soto-Varela
Corresponding author
Correspondence toMarcos Rossi-Izquierdo.
Ethics declarations
Conflict of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Human and Animal Rights
The experimental protocol was designed in accordance with the Declaration of Helsinki (1964) and was approved by the Independent Ethics Committee of Galicia (protocol 2010/139).
Informed consent
All study participants provided informed consent.
Rights and permissions
About this article
Cite this article
Rossi-Izquierdo, M., Santos-Pérez, S., Faraldo-García, A. et al. Impact of obesity in elderly patients with postural instability.Aging Clin Exp Res 28, 423–428 (2016). https://doi.org/10.1007/s40520-015-0414-4
- Received: 16 May 2015
- Accepted: 03 July 2015
- Published: 18 July 2015
- Issue date: June 2016
- DOI: https://doi.org/10.1007/s40520-015-0414-4