Body size perception and weight control in youth: 9-year international trends from 24 countries (original) (raw)
Introduction
Adolescents have a tendency to misperceive their weight status.1,2 Among non-overweight and overweight adolescents, both overestimation and underestimation of weight status are associated with adverse outcomes such as depressive symptoms and other psychological problems,3, 4, 5 and subsequently may influence weight management behaviors.6,7 In particular, non-overweight adolescents who overestimate their body size may experience body dissatisfaction leading to greater risk for disordered eating and eating disorders.2 Conversely, overweight adolescents who underestimate their body size may be less motivated to reduce body fat, thus increasing chronic disease risk.8
Before the international increase in obesity prevalence, researchers were primarily concerned about perceived overweight in non-overweight adolescents, which increased their risk for body dissatisfaction and eating disorders.9,10 Body dissatisfaction continues to be highly prevalent among girls (24–46%) and boys (12–26%) and is increasing worldwide.11, 12, 13, 14, 15 A recent international report from the Health Behaviour in School-aged Children study of 43 countries found that at age 15 years, 40% of girls and 22% of boys were dissatisfied with their bodies.16 Additionally, 22% of 15-year-old girls reported being on a diet to lose weight, even though only 10% were classified as being overweight, whereas 9% of 15-year-old boys reported being on a diet, but 18% were classified as being overweight.16 In the United States, adolescents with body dissatisfaction are more likely to take active steps to lose weight, including dieting or use of more extreme methods to change their body weight and shape that can lead to adverse physical and psychological consequences.17 As many as one-third to half of US girls report experimenting with or regularly engaging in unhealthy weight control methods such as fasting, vomiting or laxative use.18
In the past three decades, attention has turned to the international rise in body weights and the tendency for persons not to recognize they are overweight.6,19, 20, 21 This raises concerns because individuals who do not recognize that they are overweight are unlikely to take steps to reduce their weight. On the other hand, non-overweight adolescents may be protected from body dissatisfaction and engagement in unhealthy weight control behaviors in an environment with heavier people. In social comparison processes, an individual bases perceptions of his or her own body’s appearance and abilities by comparing him- or herself to others.22 In populations with high obesity prevalence, social body weight comparisons may underlie a shift in perceptions of ‘normal weight’,21,23 such that overweight may now be perceived as ‘normal’.24 However, little attention has been given to how the rise in obesity prevalence may influence both underestimation and overestimation of body size in adolescents.
The purpose of this study was to examine 9-year trends and relationships regarding misperceptions of body size and dieting for weight loss among adolescent girls and boys from 24 countries. Although there may be intercountry variation in cultural-specific body ideals,25 previous research does not show any clear geographical patterns with attempts for dieting for weight loss.1 Therefore, data from all countries were combined for analysis, and country-level overweight prevalence was examined to assess whether social comparison processes may underlie changes in body size misperceptions and dieting behaviors. Analyses were stratified by adolescent weight status and sex, and controlled for family and country-level indicators of affluence. It was hypothesized that over time, overweight adolescents would be more likely to underestimate their body size and less likely to diet for weight loss, whereas non-overweight adolescents would be less likely to overestimate their body size and diet for weight loss, and that these trends would be attenuated after taking into account country-level overweight prevalence. Because self-perception of overweight status is associated with increased likelihood of performing weight control behaviors,26,27 it was also hypothesized that perceptions of being overweight would be positively associated with dieting for weight loss and this relationship would weaken over time as overestimating body size decreased over time.
Materials and methods
Participants
Data were obtained from three waves (2001/2002, 2005/2006 and 2009/2010) of the Health Behaviour in School-Aged Children cross-sectional survey (HBSC), a World Health Organization collaborative study that is conducted every 4 years in nationally representative, school-based samples. Over 40 countries and regions participate in the study. HBSC examines a number of health behaviors and lifestyles and their context in young people. A standardized international research protocol was followed within each country to ensure consistency in survey instruments, data collection and processing procedures.28 Sociodemographics, weight control and body size perception were mandatory items for all participating countries. The surveys were administered in school classrooms by trained personnel, teachers or school nurses, and took about one school period for participants to complete.
For each country, cluster sampling was used where the cluster was the school class (or school in the absence of a sampling frame of classes). These samples were selected to be nationally representative for 11-, 13- and 15-year-old school children. The youngest age group was excluded from the present study because questions concerning weight control were not presented to them. For each country, the recommended sample size for each age group was approximately 1500 students, assuming a 95% confidence interval of ±3% around a proportion of 50% and allowing for the clustered nature of the samples. Each participating country obtained approval to conduct the survey from the relevant ethics review board or equivalent regulatory institution. More detailed information about the study design and procedures can be found elsewhere.29, 30, 31, 32
Twenty-five countries had data at all three time points (2001/2002, 2005/2006 and 2009/2010); however, Greenland was excluded from this analyses due to missing data on their level of development, a covariate in the analyses, leaving a total of 24 countries. Participating countries in the study sample included Croatia, Latvia, Lithuania, Poland, Portugal, Russia, Austria, Belgium, Czech Rebublic, Denmark, Finland, Ireland, Netherlands, Norway, Sweden, Switzerland, United Kingdom, United States of America, Canada, Italy, France, Spain, Slovenia and Macedonia. Participants aged 13 years or older with missing height or weight (_n_=13 204, 5.4%), or missing values for body size perception (_n_=2236, 0.9%) or dieting for weight loss (_n_=1233, 0.5%) were also excluded from the total analytic sample (_n_=229 614).
Measures
BMI measurement and overweight classification
Self-report data on height and weight were used to calculate body mass index (BMI) (kg m−2). Weight status was categorized by means of age- and sex-specific BMI international cut-points recommended for use in international comparisons.33,34 Specifically, sex- and age-adjusted cutoff values for overweight status were based on percentiles passing through BMI 25 kg m−2 at age 18 years. In the present study, the group of overweight adolescents includes obese, and the group of non-overweight includes normal weight and underweight adolescents.
Body size misperception
Body size perception was assessed by asking participants, ‘Do you think your body is…?’ with the response options of ‘much too thin’, ‘a bit too thin’, ‘about the right size’, ‘a bit too fat’ and ‘much too fat’, which were combined into perceived underweight, normal weight and overweight, respectively. To classify body size distortion, self-reported weight status (0=underweight, 1=non-overweight, 2=overweight/obese) as determined by adolescents’ self-reported height and weight and perceived weight status (0=perceived underweight, 1=perceived normal weight, 2=perceived overweight) were first coded numerically. The difference between values of perceived and self-reported weight status was then calculated; scores deviating from 0 indicate body size distortion. Participants were categorized as either no distortion (concordant perceived and reported weight status), underestimation (perceived weight status lower than reported weight status) or overestimation (perceived weight status higher than reported weight status). In non-overweight adolescents, body size distortion was dichotomized into overestimators and non-overestimators (i.e., includes ‘no distortion’ and ‘underestimation’ participants) of body size. Overweight adolescents were dichotomized as underestimators and non-underestimators (i.e., includes ‘no distortion’ and ‘overestimation’ participants) of body size.
Weight control
Dieting for weight control was assessed by asking, ‘At present are you on a diet or doing something else to lose weight?’ with the response options of ‘No, my weight is fine’, ‘No, but I should lose some weight’ and ‘No, because I need to put on weight’ and ‘Yes’. As the focus of this analysis was on dieting behavior rather than reasons for non-dieting, this variable was dichotomized into yes/no dieting for weight loss.
Sociodemographic characteristics
Individual-level sociodemographic characteristics included sex, age and family affluence (a proxy for socioeconomic status). The family affluence scale, which has demonstrated good content and external validity,35 was constructed from questions about family wealth and categorized into tertiles.
Country-level sociodemographic characteristics included development status and overweight prevalence. Development status was based on the human development index (HDI) scores created by the United Nations Global Development Network as a way to measure social and economic development of countries.[36](/articles/ijo201462#ref-CR36 "United Nations Global Development Network. Human Development Index. Available at: http://hdr.undp.org/en/humandev/
(accessed 30 January 2013).") The HDI score for each country includes an algorithm of life expectancy, educational attainment and income that form a composite score ranging from 0 to 1\. A country with an HDI score ⩾0.80 indicates a developed country.[36](/articles/ijo201462#ref-CR36 "United Nations Global Development Network. Human Development Index. Available at:
http://hdr.undp.org/en/humandev/
(accessed 30 January 2013).") For the country-level overweight prevalence variable, the percent adolescent overweight (BMI international cut-point ⩾25) was calculated using the sample of participants for each country and time period.Data analysis
Sociodemographic characteristics of participants at each wave of data collection (i.e., 2001/2002, 2005/2006, 2009/2010) were cross-tabulated for girls and boys, and country-level overweight prevalence and mean HDI scores were cross-tabulated for all participants. The unadjusted trend over time was tested using Kendall’s tau statistic for categorical variables and analysis of variance for continuous variables. All analyses were stratified by weight status and sex because non-overweight and overweight adolescents are likely to have different perceptions of their weight and dieting attempts,16 and girls have greater body dissatisfaction compared with boys.37 Logistic regression models were fitted to evaluate change over time relative to Time 1 in body size overestimation among non-overweight adolescents, body size underestimation among overweight adolescents and dieting for weight loss (in non-overweight and overweight adolescents). Family affluence and country-level development were included as covariates in all models, and BMI was a covariate only in models estimating dieting for weight loss. Models were estimated with and without adjustment for country-level overweight prevalence. A multiplicative interaction term between time and body size perception was used to examine time trends in the relationship between body size perception (perceived overweight) and dieting for weight loss. Odds ratios (ORs), 95% confidence intervals and standard errors are reported for all logistic regression models. Statistical significance was set at P<0.05. All analyses were performed using SPSS version 21.0 (Chicago, IL, USA).
Results
Among all participants, the country-level overweight prevalence increased significantly over time (11.6–14.7%, P<0.001), whereas mean HDI scores from the 24 countries remained constant (0.82–0.85). Sociodemographics, body size perception and dieting by sex and weight status (overweight and non-overweight) at each wave of data collection are shown in Table 1.
Table 1 Sociodemographic, body size perception and dieting characteristics in overweight and non-overweight adolescents over time
Unadjusted analyses: change over time in body size perception and dieting in overweight and non-overweight adolescents
Among overweight girls, perceptions of being ‘much too fat/a bit fat’ and dieting for weight loss decreased across the three time periods from 87% to 81% and 44% to 40%, respectively (Table 1). Overweight girls were also more likely to underestimate their body size over time (from 13 to 19%). Among non-overweight girls over time, 35–33% perceived themselves as ‘much too fat/a bit fat’ and around 17% were dieting for weight loss at each time period. Over one-third of non-overweight girls overestimated their body size at each time period; however, body size overestimation among non-overweight girls decreased over time (from 45 to 42%).
Among overweight boys, perceptions of being ‘much too fat/a bit fat’ decreased (from 66 to 64%), whereas dieting for weight loss increased (from 23 to 25%) across the three time periods (see Table 1). Overweight adolescent boys were also more likely to underestimate their body size over time (from 34 to 36%). Among non-overweight boys, 14% perceived themselves as ‘much too fat/a bit fat’ and 21% perceived themselves as ‘much too thin/a bit thin’ at each time period. Body size overestimation and dieting for weight loss remained relatively constant over time among non-overweight boys.
Adjusted analyses: body size underestimation among overweight adolescents
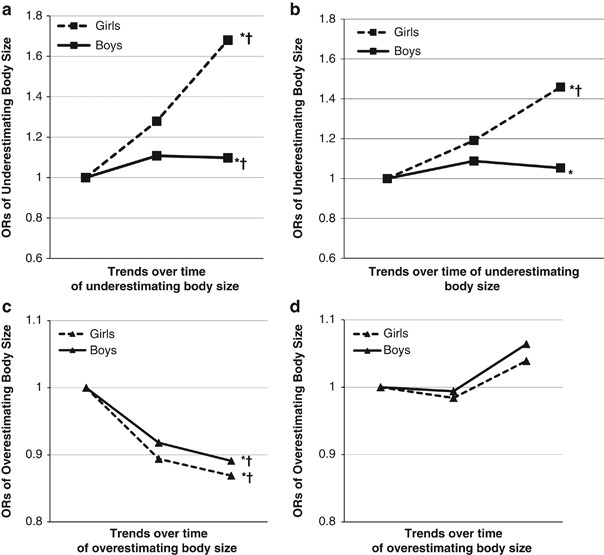
In models adjusting only for individual-level covariates and country level of development, the odds of underestimating body size increased over time for overweight girls and boys (Figure 1a and Supplementary Appendix S1). Specifically, compared with Time 1 (2001/2002), overweight girls and boys were 1.3 and 1.1 times more likely to underestimate their body size at Time 2 (2005/2006) and 1.7 and 1.1 times more likely to underestimate their body size at Time 3 (2009/2010).
Figure 1
(a) Overweight youth: ORs of underestimating body size over time by sex adjusted for individual-level and country level of development covariates. *Significant (P<0.05) difference from Time 1 to Time 2. †Significant (P<0.05) difference from Time 1 to Time 3. (b) Overweight youth: ORs of underestimating body size over time by sex adjusted for individual-level and country level of development covariates and country-level overweight prevalence. *Significant (P<0.05) difference from Time 1 to Time 2. †Significant (P<0.05) difference from Time 1 to Time 3. (c) Non-overweight youth: ORs of overestimating body size over time by sex adjusted for individual-level and country level of development covariates. *Significant (P<0.05) difference from Time 1 to Time 2. †Significant (P<0.05) difference from Time 1 to Time 3. (d) Non-overweight youth: ORs of overestimating body size over time by sex adjusted for individual-level and country level of development covariates and country-level overweight prevalence.
Controlling for country-level overweight prevalence attenuated these relationships (Figure 1b and Supplementary Appendix S1). The increasing odds of underestimating body size over time remained significant in overweight girls, but became nonsignificant at Time 3 for overweight boys.
Adjusted analyses: body size overestimation among non-overweight adolescents
In models adjusting only for individual-level covariates and country level of development, the odds of overestimating body size decreased over time for non-overweight girls and boys (Figure 1c and Supplementary Appendix S1). Specifically, compared with Time 1 (2001/2002), non-overweight girls and boys were 0.89 and 0.92 times, respectively, less likely to overestimate their body size at Time 2 (2005/2006) and 0.87 and 0.89 times, respectively, less likely to overestimate their body size at Time 3 (2009/2010).
Controlling for country-level overweight prevalence attenuated these relationships (Figure 1d and Supplementary Appendix S1) such that among non-overweight girls and boys, the decreasing odds of overestimating body size over time became nonsignificant.
Adjusted analyses: dieting for weight loss among overweight and non-overweight adolescents
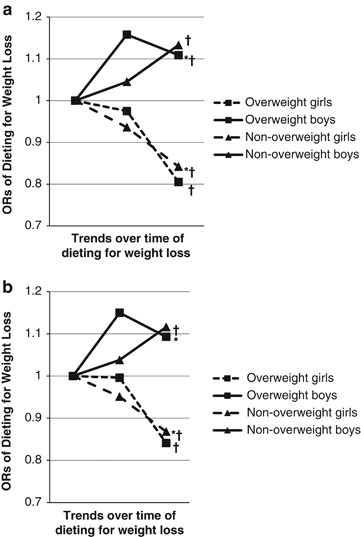
In models adjusting only for individual-level covariates and country level of development, compared with Time 1, overweight and non-overweight boys were 1.1 times more likely to diet at Time 3 (Figure 2a and Supplementary Appendix S2). Conversely, overweight and non-overweight girls were 0.81 and 0.84 times, respectively, less likely to diet at Time 3 compared with Time 1.
Figure 2
(a) ORs of dieting over time by sex and weight status adjusted for individual-level and country level of development covariates. *Significant (P<0.05) difference from Time 1 to Time 2. †Significant (P<0.05) difference from Time 1 to Time 3. (b) ORs of dieting over time by sex and weight status adjusted for individual-level and country level of development covariates and country-level overweight prevalence. *Significant (P<0.05) difference from Time 1 to Time 2. †Significant (P<0.05) difference from Time 1 to Time 3.
After controlling for country-level overweight prevalence, the trends and associations of dieting for weight loss were essentially unchanged (Figure 2b and Supplementary Appendix S2). Significant interactions of year and country-level overweight prevalence were found among overweight and non-overweight girls at Time 2 and among overweight and non-overweight boys at each time period, except at Time 2 for overweight boys.
Adjusted analyses: relationships between perceived overweight and dieting for weight loss among overweight and non-overweight adolescents
In models adjusting for individual-level covariates and country level of development, the odds of dieting were strongly associated with perceptions of being overweight, regardless of weight status (Table 2). Results from the interactions between year and perceived overweight reveal the odds of dieting among adolescents has weakened or remained relatively stable (i.e., non-overweight girls) over time.
Table 2 Logistic regression models examining the relationship between body size perception and dieting for weight loss over time by weight statusa
Discussion
This study documents 9-year trends from 2001 to 2010 in overestimation and underestimation of body size and dieting for weight loss among adolescent girls and boys from 24 countries. Findings demonstrate a decrease over time in body size overestimation among non-overweight girls and boys and an increase in body size underestimation in overweight girls and boys. Controlling for country-level overweight prevalence partially attenuated these findings for overweight adolescents, and fully attenuated them among non-overweight adolescents, consistent with the hypothesized effect of social comparison on body size perceptions. However, controlling for country-level overweight prevalence did not impact findings regarding trends in dieting behaviors, suggesting a potentially stronger impact of social comparison on weight-related perceptions than behavior. Findings also indicate that self-perceptions of being overweight increase the likelihood of dieting, but the strength of this relationship has diminished over time.
These study findings are consistent with previous work indicating that self-perceived appropriateness of weight status likely reflects differences in the normative evaluation of bodily weight standards,38,39 consistent with social comparison theory.22 In this study, adolescent body weights increased over time (2001–2010). However, overweight adolescents were more likely to underestimate and non-overweight adolescents were less likely to overestimate their body size over time. Controlling for country-level overweight prevalence attenuated these relationships, suggesting that social comparisons of body weights may be taking place whereby adolescents’ perceptions of ‘normal’ weight may be shifting. This difference in perception of weight appropriateness between public health and normative cultural standards may be problematic if this misperception prevents individuals from engaging in healthy behaviors to reduce adiposity.
As evidenced by others26,27 and further supported by our findings, self-perception of overweight status is associated with increased odds of dieting for weight loss, and the strength of this relationship has diminished over time. Given these findings, it may be anticipated that over time dieting for weight loss would decrease as body size overestimation decreased among non-overweight adolescents and body size underestimation increased among overweight adolescents. When controlling for country-level overweight prevalence, girls were less likely to diet over time while boys were more likely to diet over time, regardless of weight status. However, the percentage of girls dieting for weight loss was higher than the percentage of girls overweight, indicating that a proportion of dieters are normal weight. Although there was an increasing trend in dieting among boys, a higher percentage of boys were overweight by medical standards than were actually dieting for weight loss. The prevalence of dieting among boys remains lower than that for girls, suggesting that boys continue to be less concerned about their weight than girls. These findings are consistent with those from an international study among university students from 22 countries demonstrating that men were less aware they were overweight and less likely to diet to lose weight than women.40 The decreasing trend in dieting among non-overweight girls in this study is encouraging in terms of potentially leading to a lower incidence of disordered eating behaviors, but body dissatisfaction remains a common problem that could potentially spawn disordered eating and eating disorders.8
At the same time, findings indicate that overweight adolescents are underestimating their weight status and are less often taking steps toward achieving a healthy body weight by dieting. This suggests that over time overweight adolescents have shifted their perceptions of what is considered a normal body weight potentially through social comparison processes, and are less likely to diet to lose weight.21 This misperception among overweight adolescents may limit the effectiveness of public health campaigns and interventions aimed at weight reduction and improved health outcomes. However, underestimating body size may be associated with improved body image, and potentially, a decline in the incidence of disordered eating and eating disorders. Thus, the costs and benefits of underestimating body size among overweight adolescents who are still growing physically and emotionally poses a challenge for the development of obesity interventions. Including family and peers in weight management and obesity interventions may be important to consider given the role social comparison theory may have in adolescent weight perception.
Study limitations should be considered when interpreting these findings. Biases in self-reported height and weight are a common limitation in survey data. However, previous research has considered self-report height and weight adequate for estimating objective height and weight measurements.8,41,42 In some countries, there were a number of adolescents with missing height or weight data, but previous research has found that weight loss practices among adolescents are similar in those with and without reported height and weight data.43 Data were collected from a repeated cross-national sample and from a selected number of countries, limiting causal inference from the findings. However, this large cross-national sample provides generalizability in both US and European adolescents. A drawback to using survey data that assesses a number of health-related behaviors such as the HBSC is the use of single-item measures to assess perceptions of body weight and dieting for weight loss. However, the large sample size may have mitigated the effect of this limitation. Additionally, our measure did not distinguish between dieting owing to health concerns versus dieting for appearance concerns; it may be informative for future research to examine differences in weight management behaviors by these differing motivations.
Despite these limitations, this study provides novel findings regarding perceptions of body size and dieting for weight loss across three study waves (2001/2002, 2005/2006 and 2009/2010). A major strength of this study is the large population-representative sample on adolescents in 24 countries over a 9-year time span. Findings highlight contributions of country-level overweight prevalence to adolescents’ perceptions of body weight and dieting for weight loss. However, further research is needed to examine the implications of these findings. For example, there may be other factors within countries that could mediate or moderate perceptions of body weight and dieting to lose weight such as the amount and types of media viewed by adolescents.44 The influence of advertising and the mass media on how the public views dieting and body image should be examined in future research to determine the strength of this association. These findings demonstrate that body size perceptions and dieting among adolescents have changed over time, potentially due to a shifting of body weight norms. Regardless of weight status, adolescents who misperceive their weight status may be at risk for negative health risk behaviors,45 weight gain/obesity46,47 and psychological problems.17,48,49 Therefore, there is a need for continued awareness and development of obesity interventions that prevent body dissatisfaction and incorporate healthy weight management behaviors for all adolescents.
References
- Brener N, Eaton D, Lowry R, McManus T . The association between weight perception and BMI among high school students. Obes Res 2004; 12: 1866–1874.
Article Google Scholar - Talamayan K, Springer A, Kelder S, Gorospe E, Joye K . Prevalence of overweight misperception and weight control behaviors among normal weight adolescents in the United States. Scientific World J 2006; 6: 365–373.
Article Google Scholar - Al Mamun A, Cramb S, McDermott B, O'Callaghan M, Najman J, Williams G . Adolescents' perceived weight associated with depression in young adulthood: a longitudinal study. Obesity 2007; 15: 3097–3105.
Article Google Scholar - Daniels J . Weight and weight concerns: are they associated with reported depressive symptoms in adolescents? J Pediatr Health Care 2005; 19: 33–41.
Google Scholar - Pesa J, Syre T, Jones E . Psychosocial differences associated with body weight among female adolescents: the importance of body image. J Adolesc Health 2000; 26: 330–337.
Article CAS Google Scholar - Johnson-Taylor W, Fisher R, Hubbard V, Starke-Reed P, Eggers P . The change in weight perception of weight status among the overweight: comparison of NHANES III (1988–1994) and 1999–2004 NHANES. Int J Behav Nutr Phys Act 2008; 5: 9.
Article Google Scholar - Gee L, Peebles R, Storfer-Isser A, Golden N, Horwitz S . Underestimation of weight status in Californian adolescents. Child Obes 2013; 9: 132–136.
Article Google Scholar - Ojala K, Vereecken C, Valimaa R, Currie C, Villberg J, Tynjala J, et al. Attempts to lose weight among overweight and non-overweight adolescents: a cross-national survey. Int J Behav Nutr Phys Act 2007; 4: 1–10.
Article Google Scholar - Wardle J, Marsland L . Adolescent concerns about weight and eating: a social development perspective. J Psychosom Res 1990; 34: 377–391.
Article CAS Google Scholar - Casper R, Offer D . Weight and dieting concerns in adolescents, fashion or symptom? Pediatrics 1990; 86: 384–390.
CAS PubMed Google Scholar - Stice E, Whitenton K . Risk factors for body dissatisfaction in adolescent girls: a longitudinal investigation. Dev Psychol 2002; 38: 669–678.
Article Google Scholar - Presnell K, Bearman SK, Stice E . Risk factors for body dissatisfaction in adolescent boys and girls: a prospective study. Int J Eat Disord 2004; 36: 389–401.
Article Google Scholar - Neumark-Sztainer D, Story M, Hannan PJ, Perry C, Irving LM . Weight-related concerns and behaviors among overweight and non-overweight adolescents: implications for preventing weight-related disorders. Arch Pediatr Adolesc Med 2002; 156: 171–178.
Article Google Scholar - Eisenberg M, Neumark-Sztainer D, Paxton S . Five-year change in body dissatisfaction among adolescents. J Psychosom Res 2006; 61: 521–527.
Article Google Scholar - Sabbah H, Verecken C, Elgar F, Nansel T, Aasvee K, Abdeen Z, et al. Body weight dissatisfaction and communication with parents among adolescent in 24 countries: International cross-sectional survey. BMC Public Health 2009; 9: 52.
Article Google Scholar - Currie C, Zanotti C, Morgan A, Currie D, de Looze M, Roberts C, et al. Social Determinants of Health and Well-being Among Young People. Health Behaviour in School-aged Children (HBSC) Study: International Report From 2009/2010 Survey, 2012, Copenhagen, Denmark: WHO Regional Office for Europe.
Google Scholar - Neumark-Sztainer D, Wall M, Guo J, Story M, Haines J, Eisenberg M . Obesity, disordered eating, and eating disorders in a longitudinal study of adolescents: how do dieters fare 5 years later? J Am Diet Assoc 2006; 106: 559–568.
Article Google Scholar - Wertheim E, Paxton S . Body image development in adolescent girls. In: Cash T, Smolak L (eds). Body Image: A Handbook of Science, Practice, and Prevention. The Guilford Press: New York, NY, USA, 2011, pp 76–84.
Google Scholar - Jeffery A, Voss L, Metcalf B, Alba S, Wilkin T . Parents' awareness of overweight in themselves and their children: cross sectional study within a cohort. BMJ 2005; 330: 23–24.
Article CAS Google Scholar - Johnson F, Cooke L, Croker H . Changing perceptions of weight in Great Britian: comparison of two population surveys. BMJ 2008; 337: a494.
Article CAS Google Scholar - Burke M, Heiland F, Nadler C . From ‘overweight’ to ‘about right’: evidence of a genernational shift in body weight norms. Obesity (Silver Spring, MD) 2010; 18: 1226–1234.
Article Google Scholar - Festinger L . A theory of social comparison processes. Hum Relat 1954; 7: 117–140.
Article Google Scholar - Burke M, Heiland F . Social dynamics of obesity. Econ Inq 2007; 45: 571–591.
Article Google Scholar - James P, Leach R, Kalamara E, Shayeghi M . The worldwide obesity epidemic. Obes Res 2001; 9: 228S–233S.
Article Google Scholar - McCabe MP, Waga G, Dev A, Cama T, Swinburn BA . The role of cultural values and religion on views of body size and eating practices among adolescents from Fiji, Tona, and Australia. Br J Health Psychol 2013; 18: 383–394.
Article Google Scholar - Crawford D, Campbell K . Lay definitions of ideal weight and overweight. Int J Obes 1999; 23: 738–745.
Article CAS Google Scholar - Strauss R . Self-reported weight status and dieting in a cross-sectional sample of young adolescents: National Health and Nutrition Examination Survey III. Arch Pediactr Adolesc Med 1999; 153: 741–747.
Article CAS Google Scholar - Currie C Samdal O Boyce W (eds)Health Behaviour in School-Aged Children: A World Health Organization Cross-National Study (HBSC). Research Protocol for the 2001/2002 Survey. Child and Adolescent Health Research Unit: Edinburgh, UK, 2001.
Google Scholar - Roberts C, Freeman J, Samdal O, Schnohr C, de Looze M, Gabhainn N, et al. The Health Behaviour in School-aged Children (HBSC) study: methodological developments and current tensions. Int J Public Health 2009; 54: S140–S150.
Article Google Scholar - Roberts C, Currie C, Samdal O, Currie D, Smith R, Maes L . Measuring the health and health behaviours of adolescents through cross national survey research: recent developments in the Health Behaviour in School-aged Children (HBSC) study. J Public Health 2007; 15: 176–186.
Article Google Scholar - Currie C, Gabhainn N, Godeau E, Roberts C, Smith R, Currie D, et al. Inequalities in Young People's Health: HBSC International Report from the 2005/2006 Survey. Health Policy for Children and Adolescents. WHO Regional Office for Europe: Copenhagen, Denmark, 2008.
Google Scholar - Currie C, Gabhainn N, Godeau E . The Health Behaviour in School-Aged Children (HBSC) study: origins, concept, history and development 1982–2008. Int J Public Health 2009; 54: 131–139.
Article Google Scholar - Cole T, Flegal K, Nicholls D, Jackson A . Body mass index cut offs to define thinness in chidlren and adolescents: international survey. BMJ 2007; 335: 194.
Article Google Scholar - Cole T, Bellizzi M, Flegal K, Dietz W . Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 2000; 320: 1240–1243.
Article CAS Google Scholar - Currie C, Molcho M, Boyce W, Holstein B, Thorsheim T, Richter M . Researching health inequalities in adolescence: the development of the HBSC Family Affluence Scale. Soc Sci Med 2008; 66: 1429–1436.
Article Google Scholar - United Nations Global Development Network. Human Development Index. Available at: http://hdr.undp.org/en/humandev/ (accessed 30 January 2013).
- Neumark-Sztainer D, Wall M, Larson N, Eisenberg M, Loth K . Dieting and disordered eating behaviors from adolescence to young adulthood: findings from a 10-year longitudinal study. J Am Diet Assoc 2011; 111: 1004–1011.
Article Google Scholar - Chang V, Christakis N . Self-perceptions of weight appropriateness in the United States. Am J Prev Med 2003; 24: 332–339.
Article Google Scholar - Ali MM, Amialchuk A, Renna F . Social network and weight misperception among adolescents. South Econ J 2011; 77: 827–842.
Article Google Scholar - Wardle J, Haase A, Steptoe A . Body image and weight control in young adults: international comparisons in university students from 22 countries. Int J Obes 2006; 30: 644–651.
Article CAS Google Scholar - Goodman E, Hinden B, Khandelwal S . Accuracy of teen and parental reports of obestiy and body mass index. Pediatr 2000; 106: 52–58.
Article CAS Google Scholar - Dietz W, Bellizzi M . Introduction: the use of body mass index to assess obesity in children. Am J Clin Nutr 1999; 70: 123S–125S.
Article CAS Google Scholar - Janssen I, Katzmarzyk P, Boyce W, Verecken C, Mulvihill C, Roberts C, et al. Comparison of overweight and obesity prevalence in school-aged youth from 34 countries and their relationships with physical activity and dietary patterns. Obes Rev 2005; 6: 123–132.
Article CAS Google Scholar - Field AE, Camargo CA, Taylor CB, Berkey CS, Roberts SB, Colditz GA . Peer, parent, and media influences on the development of weight concerns and frequent dieting among preadolescent and adolescent girls and boys. Pediatrics 2001; 107: 54–60.
Article CAS Google Scholar - Crow S, Eisenberg M, Story M, Neumark-Sztainer D . Suicidal behavior in adolescents: relationship to weight status, weight control behaviors, and body dissatisfaction. Int J Eat Disord 2008; 41: 82–87.
Article Google Scholar - Stice E, Cameron R, Killen J, Hayward C, Taylor C . Naturalistic weight-reduction efforts prospectively predict growth in relative weight and onset of obesity among female adolescents. J Consult Clin Psychol 1999; 67: 967–674.
Article CAS Google Scholar - Field A, Austin S, Taylor C, Malspeic S, Rosner B, Rockett H, et al. Relation between dieting and weight change among preadolescents and adolescents. Pediatrics 2003; 112: 900–906.
Article Google Scholar - Stice E, Bearman S . Body image and eating disturbances prospectively predict increases in depressive symptoms in adolescent girls: a growth curve analysis. Dev Psychol 2001; 37: 597–607.
Article CAS Google Scholar - Neumark-Sztainer D, Wall M, Story M, Perry C . Correlates of unhealthy weight control behaviors among adolescent girls and boys: implications for the primary prevention of disordered eating. Health Psychol 2003; 22: 88–98.
Article Google Scholar
Acknowledgements
HBSC is an international study carried out in collaboration with WHO/EURO. The international coordinator of all three waves of data was Candace Currie, University of St Andrews, Scotland, and the data bank manager was Oddrun Samdal, University of Bergen, Norway. A complete list of the participating researchers can be found on the HBSC website (www.HBSC.org). This research was also supported in part by the intramural research program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development (contract no. N01-HD-5-3401) and by the Maternal and Child Health Bureau of the Health Resources and Services Administration.
Author information
Authors and Affiliations
- Division of Intramural Population Health Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development/NIH, Bethesda, MD, USA
V Quick, T R Nansel, D Liu & L M Lipsky - Child and Adolescent Health Research Programme, The National Institute of Public Health, University of Southern Denmark, Copenhagen, Denmark
P Due - College of Nursing and Health Sciences, University of Massachusettes Boston, Boston, MA, USA
R J Iannotti
Authors
- V Quick
- T R Nansel
- D Liu
- L M Lipsky
- P Due
- R J Iannotti
Corresponding author
Correspondence toV Quick.
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Supplementary information
Rights and permissions
About this article
Cite this article
Quick, V., Nansel, T., Liu, D. et al. Body size perception and weight control in youth: 9-year international trends from 24 countries.Int J Obes 38, 988–994 (2014). https://doi.org/10.1038/ijo.2014.62
- Received: 07 November 2013
- Revised: 13 March 2014
- Accepted: 01 April 2014
- Published: 11 April 2014
- Issue date: July 2014
- DOI: https://doi.org/10.1038/ijo.2014.62