Kruppel-like factor 2 regulates thymocyte and T-cell migration (original) (raw)
Kruppel-like factors (KLFs) are a family of zinc-finger transcription factors including at least 15 mammalian family members2. KLFs have critical roles in the development of specific cell lineages, as demonstrated by the profound phenotypes that result from gene-targeting KLF family members1,2. Several KLFs have an important role in cell maturation—a feature exemplified by erythroid KLF (KLF1), which is essential for erythrocyte production of adult-form haemoglobin1,2,3.
KLF2 is expressed in lung, endothelial cells and lymphocytes4,8,9,10,11, and is essential for normal blood-vessel integrity and lung development4,9,10,11. Although _Klf2_-/- thymocyte development is grossly normal, few KLF2-deficient T cells are found in peripheral lymphoid tissues4,6. Moreover, the few _Klf2_-/- T cells that are present in peripheral tissues show signs of activation and induction of cell death, suggesting KLF2 may have a critical role in T-cell quiescence and survival4,6. KLF2 is normally expressed in mature thymocytes, naive T cells and memory T cells, but its expression is dramatically downregulated with T-cell receptor activation4,12,13,14. Overexpression of KLF2 in the Jurkat T cell line leads to inhibition of cell-cycle progression, an effect that may involve KLF2 repression of c-myc transcription and/or induction of p21 WAF1/CIP1 (refs 6, 15, 16). Taken together, these features have lead to the proposal that KLF2 functions to prevent spontaneous activation and subsequent death of mature T cells4,5,6,7.
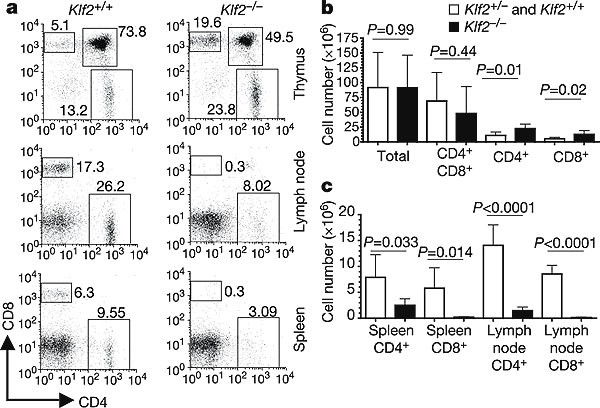
To test this model, we studied maintenance of _Klf2_-/- T cells in vivo. Because murine KLF2 deficiency is embryonic lethal9,11, we generated fetal liver chimaeras (FLCs) using embryonic day 12.5 fetal livers from _Klf2_-/- or Klf2+/- donors injected into irradiated _Rag2_-/- hosts (see Methods). After allowing haematopoietic reconstitution, we studied the T-cell pool in the thymus and peripheral lymphoid tissues of the chimaeras. Consistent with previous reports, which involved a distinct targeted allele of KLF2 (ref. 4), we found that thymic development of _Klf2_-/- T cells was grossly normal (Fig. 1a, b), but that there was a massive deficit of peripheral T cells (Fig. 1a, c). Notably, we also observed an increase in the representation of _Klf2_-/- mature CD4+CD8- (CD4 single-positive; CD4 SP) and CD4-CD8+ (CD8 single-positive; CD8 SP) thymocytes compared with controls (Fig. 1b). Similar results were obtained using FLCs generated in lethally irradiated C57BL/6 (rather than _Rag2_-/-) hosts (data not shown).
Figure 1: Klf2 -/- T cells develop but do not populate the periphery in fetal liver chimaeras.
Fetal liver chimaeras (FLCs) were generated from _Klf2_-/- and Klf2+ (Klf2+/- or Klf2+/+) donors in _Rag2_-/- hosts. a, Representative CD4/CD8 staining of the indicated tissues from _Klf2_-/- and Klf2+ FLCs. Values represent the percentage of cells in each boxed region. b, c, Cell numbers for the indicated populations from thymus (b) and peripheral lymphoid tissues (c). Graphs show the average recovery from multiple experiments (n > 6 for b; n > 4 for c), with error bars representing standard deviation. Statistical comparisons between _Klf2_-/- and Klf2+ groups are indicated.
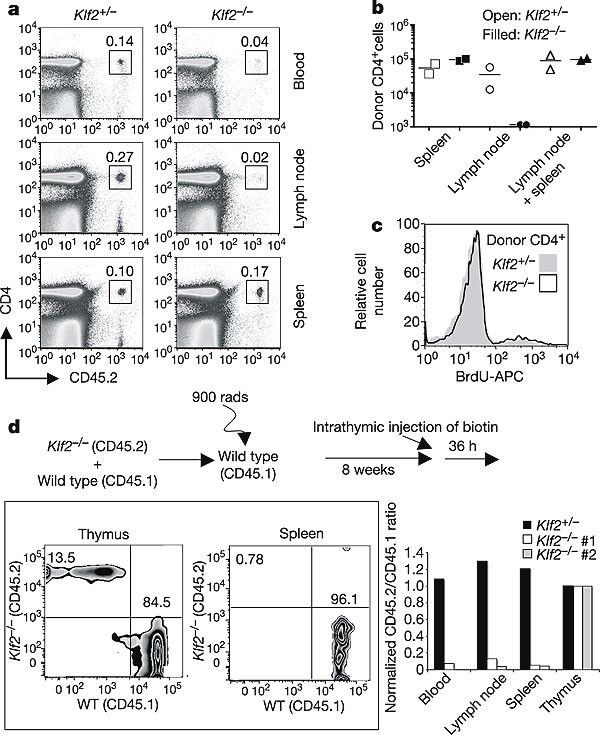
To study the proposed demise of mature _Klf2_-/- T cells, we performed adoptive transfer of _Klf2_-/- versus Klf2+/- thymocytes into congenic hosts and tracked maintenance of the donor population. Unexpectedly, donor _Klf2_-/- CD4 SP cells were recovered at similar total numbers compared to Klf2+/- CD4 SP cells 14 days following adoptive transfer (Fig. 2a, b), and even at later time points (30 days post-transfer; data not shown)—results that seemed to conflict with the model that KLF2 was required for mature T-cell survival in the periphery. We considered that KLF2 deficiency might deregulate T-cell cytokine dependence, such that the normal survival cytokines were superfluous for _Klf2_-/- T-cell persistence. However, in vitro culture of _Klf2_-/- and Klf2+/- T cells showed very similar survival characteristics, including dependence on interleukin (IL)-7 for maintenance (Supplementary Fig. S1). As KLF2 deficiency has also been proposed to induce a loss in T-cell quiescence4,6, it was possible that _Klf2_-/- T cells underwent spontaneous proliferation in vivo, balancing an increased rate of cell death. To explore this, we labelled proliferating cells in vivo with BrdU (5-bromodeoxyuridine). Both _Klf2_-/- and Klf2+/- T cells showed similar BrdU incorporation following adoptive transfer, arguing against differential proliferation of these populations (Fig. 2c). Although these data suggested _Klf2_-/- CD4 SP thymocytes were competent for short-term survival, we noted marked abnormalities in their tissue distribution: Whereas Klf2+/- donor T cells were found in blood, lymph nodes and spleen, _Klf2_-/- T cells segregated almost exclusively to the spleen (Fig. 2a, b), a pattern that was also seen at three and seven days following adoptive transfer (Supplementary Fig. S2a; data not shown). Recovery of both CD4+ and CD8+ donor _Klf2_-/- T cells was similar to controls soon after adoptive transfer (Supplementary Fig. S2a), but we did observe reduced recovery of _Klf2_-/- CD8+ (but not CD4+) T cells at later times (days 14 and 30; data not shown). However, it is currently unclear whether KLF2 has a direct role in long-term CD8+ T-cell survival, or if this gradual decline is secondary to altered T-cell trafficking.
Figure 2: Klf2 -/- T cells survive but show deregulated trafficking following adoptive transfer.
a, b, Thymocytes from Klf2+/- or _Klf2_-/- FLCs were transferred into C57BL/6.SJL hosts and labelled with BrdU for 14 days. The percentage (a) and absolute numbers (b) of donor CD4+ T cells in the indicated tissues was determined (representative of n > 4 experiments). c, Representative BrdU incorporation in donor-derived CD4+ splenocytes. An allophycocyanin (APC)-conjugated anti-BrdU antibody was used to detect BrdU in cells. d, The schematic describes the generation and intrathymic injection of mixed bone-marrow chimaeras. Fluorescence-activated cell sorting (FACS) plots show _Klf2_-/- and wild-type biotinylated CD4+ cells from a representative mixed chimaera. The bar graph indicates the ratio of FLC-derived:normal donor cells in indicated tissues, normalized against the thymic ratio.
These results suggested KLF2 regulates T-cell trafficking, raising the possibility that the absence of _Klf2_-/- peripheral T cells might arise from defective thymocyte emigration. To test this model directly, _Klf2_-/- or Klf2+/- FLCs were used to generate secondary radiation bone-marrow chimaeras, in which donor FLC cells were placed in competition with congenic wild-type cells (Fig. 2d). Biotin was then administered by intrathymic injection and, 36 h later, the export of biotin-labelled thymocytes into peripheral lymphoid tissues was determined. Klf2+/- recent thymic emigrants were detected in blood, spleen and lymph nodes in the ratios expected from thymocyte labelling (Fig. 2d). In contrast, _Klf2_-/- recent thymic emigrants were very rare, despite efficient labelling of these cells in the thymus (Fig. 2d). These data contrast with those expected if KLF2 deficiency caused T-cell death following thymic egress, in which case most peripheral _Klf2_-/- T cells would presumably be thymic emigrants. Hence, these results argue for impaired thymic emigration of _Klf2_-/- T cells.
To understand the basis for these altered trafficking patterns, we analysed the phenotype of _Klf2_-/- T cells. CD4+CD8+ (double-positive; DP) thymocytes from _Klf2_-/- and Klf2+/- chimaeras had very similar phenotypes (Fig. 3a), consistent with the fact that KLF2 is upregulated only after positive selection in the thymus4,17. Single-positive (SP) thymocytes from _Klf2_-/- and Klf2+/- chimaeras showed similar expression of some markers, including T-cell receptor β (TCRβ), CD25 and CD5 (Fig. 3a; data not shown), but other molecules were altered in KLF2-deficient cells. _Klf2_-/- SP thymocytes were CD69high and CD62Llow (Fig. 3a), suggestive of a ‘semi-mature’ phenotype18,19,20; yet these cells were also CD24low and Qa2high (Fig. 3a; data not shown), a phenotype consistent with full maturity18,19,20. Despite their CD69 expression, the CD24lowCD25low phenotype of _Klf2_-/- T cells argues against them being activated. Furthermore, expression levels of the activation/memory marker CD44 were similar on _Klf2_-/- and Klf2+/- thymocytes, although there was considerable variability in CD44 expression in individual FLCs (data not shown). With regard to trafficking, the expression of CD62L, CCR7 and β7 integrin—all of which are involved in the entry of T cells into peripheral lymphoid tissues21,22,23,24—was decreased on _Klf2_-/- T cells (Fig. 3a). Furthermore, CD69 expression by _Klf2_-/- SP thymocytes is potentially relevant, as CD69 can impair T-cell migration19,25,26. The rare peripheral _Klf2_-/- T cells were phenotypically similar to SP thymocytes (Fig. 3a; data not shown), and the CD69hiCD62Llo phenotype of _Klf2_-/- SP thymocytes was maintained at 6 (Supplementary Fig. S2b), 14 or 30 (data not shown) days after adoptive transfer, indicating that the deregulated expression of these markers by _Klf2_-/- T cells is stable.
Figure 3: KLF2 is required for thymocyte expression of critical trafficking molecules.
a, Phenotype of thymocytes and CD4+ splenocytes from _Klf2_-/- and Klf2+/- FLCs (representative of n > 4 experiments). b, S1P1, CD62L, β7 integrin and BCL2 mRNA abundance was assessed by real-time RT–PCR analysis of sorted DP and CD4 SP thymocytes from _Klf2_-/- and Klf2+/- FLCs. Bar graphs show the average signal from _n_≧3 experiments, with error bars representing standard deviation. _P_-values from comparisons between _Klf2_-/- and Klf2+/- CD4 SP samples are indicated.
In order to further explore the maturation state and trafficking potential of _Klf2_-/- SP thymocytes, we sorted _Klf2_-/- and Klf2+/- DP and CD4 SP thymocytes and performed real-time polymerase chain reaction following reverse transcription (RT–PCR) on genes known to change in expression during thymocyte maturation (Supplementary Fig. S3). Most genes showed a similar pattern of expression in Klf2+/- and _Klf2_-/- thymocyte populations, consistent with normal thymocyte maturation in the absence of KLF2 (Supplementary Fig. S3). Real-time RT–PCR analysis did, however, demonstrate a dramatic decrease in the expression of mRNA encoding CD62L in _Klf2_-/- SP thymocytes (Fig. 3b and Supplementary Fig. S3) and a more modest impairment in the expression of β7 integrin mRNA (Fig. 3b and Supplementary Fig. S3). Notably, loss of KLF2 had no substantial effect on the expression of CCR7 mRNA, although expression of the CCR7 protein was reproducibly reduced on _Klf2_-/- SP thymocytes (Fig. 3a). Also of note, two molecules involved in the regulation of apoptosis—Bcl2 and Ian1—were unaffected at the mRNA level by KLF2 loss (Fig. 3b and Supplementary Fig. S3). Although these assays focused on CD4 SP thymocytes, preliminary data indicate similar gene expression patterns in _Klf2_-/- CD8 SP cells (data not shown).
Reduced expression of CD62L, CCR7 and β7 integrin immediately suggested a basis for the altered trafficking of _Klf2_-/- thymocytes: CD62L and CCR7 are essential for trafficking into peripheral lymph nodes; β7 integrin for entry into Peyer's patches; and access to mesenteric lymph nodes requires either CD62L or β7 integrin21,22,23,24. However, although the loss of these molecules could explain aspects of altered _Klf2_-/- T-cell trafficking in the adoptive transfer experiments (Fig. 2a, b), they were insufficient to account for the defect in _Klf2_-/- thymocyte emigration (Fig. 2d). Recently, reports have demonstrated that the sphingosine-1-phosphate receptor S1P1 (also known as Edg1) is critical for thymocyte emigration and T-cell recirculation26,27,28. Hence, we examined the expression of S1P1 in _Klf2_-/- thymocytes. Real-time RT–PCR analysis demonstrated the expected upregulation of S1P1 mRNA expression between the DP and CD4 SP stages in control thymocytes, but S1P1 expression was not upregulated in _Klf2_-/- CD4 SP thymocytes (Fig. 3b), nor in _Klf2_-/- CD8 SP thymocytes (data not shown). On the basis of previous studies27,28,29, defective S1P1 expression could explain the crippled _Klf2_-/- thymocyte egress observed (Fig. 2d), as well as the absence of _Klf2_-/- T cells in peripheral blood following adoptive transfer (Fig. 2a, b).
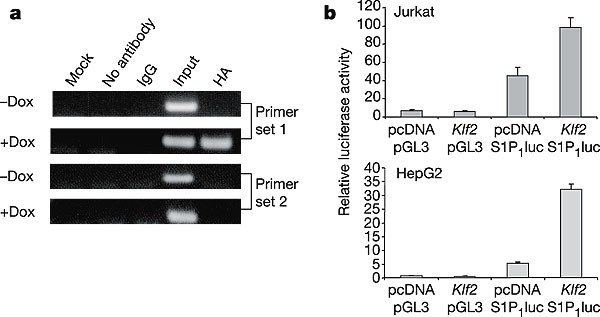
These effects on gene transcription might indicate direct regulation by KLF2 or an indirect consequence of KLF2 deficiency altering thymocyte maturation. Given the primacy of S1P1 in directing thymocyte egress, we focused on the ability of KLF2 to interact with the S1P1 promoter. Chromatin immunoprecipitation (ChIP) assays were performed using an inducible KLF2 expression system6,15 as described previously14, and resulted in co-immunoprecipitation of KLF2 with the proximal S1P1 promoter region (Fig. 4a). Furthermore, reporter assays demonstrated transactivation of the S1P1 promoter by KLF2 (Fig. 4b), arguing that KLF2 positively regulates S1P1 expression. These findings are consistent with previous reports showing upregulation of S1P1 mRNA with KLF2 overexpression16. Interestingly, a consensus KLF family binding-site motif (CACCC) is found just upstream of the S1P1 transcriptional start site (Supplementary Fig. S4), although KLF2 could also be acting through neighbouring SP1 sites, as demonstrated previously15. Together with our analysis of thymocyte gene expression, these findings suggest KLF2 directly induces S1P1 expression in developing thymocytes.
Figure 4: KLF2 transactivates the S1P 1 promoter.
a, Jurkat T cells were induced (“ + Dox”) or not (“ - Dox”) to express HA-tagged KLF2 and chromatin immunoprecipitation (ChIP) performed. PCR for S1P1 promoter fragments was conducted on chromosomal DNA (“Input”), DNA co-precipitated with KLF2 (“HA”), and control immunoprecipitations, as indicated. Primer set 1 amplifies a region immediately upstream of the S1P1 transcriptional start site (Supplementary Fig. S4), whereas primer set 2 amplifies a region about 300 bp further upstream. b, KLF2 transactivation of the S1P1 promoter was assessed by reporter assay14,15. Jurkat (T) and HepG2 (liver) cells were co-transfected with either Klf2 cDNA (“_Klf2_”) or empty vector (“pcDNA”), plus either the S1P1 promoter luciferase reporter (“S1P1luc”) or control plasmid (“pGL3”). Data are representative of n = 3 experiments. Error bars represent s.d.
In summary, our data suggest a radically different model of the role of KLF2: rather than primarily influencing T-cell survival, KLF2 regulates thymocyte and T-cell trafficking. Loss of KLF2 results in defective expression of S1P1, CD62L, β7 integrin and CCR7, and KLF2 seems to have a direct role in induction of S1P1 expression. KLF2 and S1P1 show similar expression patterns in T cells, both being upregulated on thymocyte maturation, downregulated after T-cell activation and re-expressed in the late effector/memory pool4,12,13,27. Furthermore, KLF2-null and S1P1-null mice die at similar stages in gestation because of widespread haemorrhaging, probably owing to defective tunica media integrity9,11,27,30. It is interesting to speculate that KLF2 may be required for promoting S1P1 expression in endothelial cells, explaining the early embryonic lethality of KLF2-deficient mice.
Our data do not exclude additional roles for KLF2, potentially including long-term effects on T-cell quiescence or survival. Indeed, forced KLF2 expression can clearly promote cell-cycle withdrawal in tumour cell lines6,15,16. However, our findings suggest KLF2 is critical to license mature thymocytes for trafficking competence. Such a role is consistent with the action of other KLF family members, which are essential for terminal differentiation of various cell types1,2,3.