Plasma activity of Thioredoxin Reductase as a Novel Biomarker in Gastric Cancer (original) (raw)
Introduction
Gastric cancer (GC) is the fifth most common cancer worldwide, the fourth most commonly occurring cancer in men and the seventh most commonly occurring cancer in women[1](/articles/s41598-019-55641-6#ref-CR1 "Bray, F. et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a cancer journal for clinicians 68, 394–424, https://doi.org/10.3322/caac.21492
(2018)."). There were over 1 million new cases in 2018, and the highest incidence rates of countries are mostly located in Asia including South Korea, Mongolia, Japan and China[1](/articles/s41598-019-55641-6#ref-CR1 "Bray, F. et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a cancer journal for clinicians 68, 394–424, https://doi.org/10.3322/caac.21492
(2018)."),[2](/articles/s41598-019-55641-6#ref-CR2 "Ferlay, J. et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. International journal of cancer 144, 1941–1953, https://doi.org/10.1002/ijc.31937
(2019)."). In China, GC rank the second highest tumor incidence rates (10.26%) and the third highest tumor mortality rates (10.74%)[3](#ref-CR3 "Zheng Rongshou et al. Analysis of the prevalence of malignant tumors in China, 2015. Chinese Journal of Oncology 41, 19–28, https://doi.org/10.3760/cma.j.issn.0253-3766.2019.01.005
(2019)."),4,[5](/articles/s41598-019-55641-6#ref-CR5 "Chen Wanqing et al. Analysis of the incidence and mortality of malignant tumors in China, 2014. Chinese Journal of Oncology 27, 1–14, https://doi.org/10.11735/j.issn.1004-0242.2018.01.A001
(2018)."). Approximately 85% of GC cases are diagnosed as adenocarcinoma based on histologic classification. Compared with other carcinomas, GC carries a far worse prognosis and high recurrence (around 30%); while the overall 5-year survival rate after diagnosis remains around 27%[6](/articles/s41598-019-55641-6#ref-CR6 "Rota, M. et al. Education and gastric cancer risk-An individual participant data meta-analysis in the StoP project consortium. International journal of cancer, https://doi.org/10.1002/ijc.32298
(2019)."),[7](/articles/s41598-019-55641-6#ref-CR7 "DeSantis, C. E. et al. Cancer treatment and survivorship statistics, 2014. CA: a cancer journal for clinicians 64, 252–271, https://doi.org/10.3322/caac.21235
(2014)."). Early clinical interventions are essential to improve the 5-year survival rates and reduce GC recurrence, and largely depend on the early and accurate diagnosis of GC. However, delays and omission commonly occur in the clinical diagnosis of GC.
Currently, invasive diagnostic strategies such as gastroscope are widely applied in the clinical diagnosis of GC. However, these tests usually fail to uncover the hidden or subclinical lesions and lead to high false-positive rates especially in early-stage GC[8](/articles/s41598-019-55641-6#ref-CR8 "Miki, K. et al. Clinical application of serum pepsinogen I and II levels for mass screening to detect gastric cancer. Japanese journal of cancer research: Gann 84, 1086–1090, https://doi.org/10.1111/j.1349-7006.1993.tb02805.x
(1993)."). Additionally, pain and inconvenience led by gastroscope and needle biopsy always make it unfeasible for some patients. Recently, several tumor-specific proteins have been identified as GC biomarkers in the clinical diagnosis, such as carcinoembryonic antigen (CEA), cancer antigen 72-4 (CA72-4) and cancer antigen 19-9 (CA19-9)9,[10](#ref-CR10 "Yu, J., Zhang, S. & Zhao, B. Differences and correlation of serum CEA, CA19-9 and CA72-4 in gastric cancer. Molecular and clinical oncology 4, 441–449, https://doi.org/10.3892/mco.2015.712
(2016)."),[11](/articles/s41598-019-55641-6#ref-CR11 "Liang, Y. et al. Clinical significance and diagnostic value of serum CEA, CA19-9 and CA72-4 in patients with gastric cancer. Oncotarget 7, 49565–49573, https://doi.org/10.18632/oncotarget.10391
(2016)."). However, the appliance of these biomarkers has limited application owing to their low sensitivity not only in the diagnosis of early-stage GC, but also in the monitoring of GC therapeutic efficiencies in response to chemotherapy[12](/articles/s41598-019-55641-6#ref-CR12 "Feng, F. et al. Diagnostic and prognostic value of CEA, CA19-9, AFP and CA125 for early gastric cancer. BMC Cancer 17, 737, https://doi.org/10.1186/s12885-017-3738-y
(2017)."),[13](/articles/s41598-019-55641-6#ref-CR13 "Zhou, Y. C., Zhao, H. J. & Shen, L. Z. Preoperative serum CEA and CA19-9 in gastric cancer–a single tertiary hospital study of 1,075 cases. Asian Pac J Cancer Prev 16, 2685–2691, https://doi.org/10.7314/apjcp.2015.16.7.2685
(2015)."). Therefore, it is a top priority to identify a novel GC biomarker with high sensitivity and specificity to improve the clinical GC diagnosis.
Mammalian thioredoxin reductase (TrxR) is a selenium-containing oxidoreductase that is responsible for catalyzing the NADPH-dependent reduction reaction of thioredoxin (Trx) disulfide[14](#ref-CR14 "Arner, E. S. Focus on mammalian thioredoxin reductases–important selenoproteins with versatile functions. Biochimica et biophysica acta 1790, 495–526, https://doi.org/10.1016/j.bbagen.2009.01.014
(2009)."),[15](#ref-CR15 "Sun, Q. A. et al. Redox regulation of cell signaling by selenocysteine in mammalian thioredoxin reductases. The Journal of biological chemistry 274, 24522–24530, https://doi.org/10.1074/jbc.274.35.24522
(1999)."),[16](#ref-CR16 "Lu, J. & Holmgren, A. Thioredoxin system in cell death progression. Antioxidants & redox signaling 17, 1738–1747, https://doi.org/10.1089/ars.2012.4650
(2012)."),[17](#ref-CR17 "Holmgren, A. & Lu, J. Thioredoxin and thioredoxin reductase: current research with special reference to human disease. Biochemical and biophysical research communications 396, 120–124, https://doi.org/10.1016/j.bbrc.2010.03.083
(2010)."),[18](#ref-CR18 "Gromer, S., Urig, S. & Becker, K. The thioredoxin system–from science to clinic. Medicinal research reviews 24, 40–89, https://doi.org/10.1002/med.10051
(2004)."),[19](#ref-CR19 "Lu, J. & Holmgren, A. The thioredoxin antioxidant system. Free Radic Biol Med 66, 75–87, https://doi.org/10.1016/j.freeradbiomed.2013.07.036
(2014)."),[20](/articles/s41598-019-55641-6#ref-CR20 "Zhang, J. et al. Small molecule inhibitors of mammalian thioredoxin reductase as potential anticancer agents: An update. Medicinal research reviews 39, 5–39, https://doi.org/10.1002/med.21507
(2019)."). TrxR is also known to participate in several redox-sensitive signaling cascades that mediate numerous physiological processes, especially cell survival, proliferation, growth and apoptosis[20](#ref-CR20 "Zhang, J. et al. Small molecule inhibitors of mammalian thioredoxin reductase as potential anticancer agents: An update. Medicinal research reviews 39, 5–39, https://doi.org/10.1002/med.21507
(2019)."),21,22,[23](#ref-CR23 "Jakupoglu, C. et al. Cytoplasmic thioredoxin reductase is essential for embryogenesis but dispensable for cardiac development. Molecular and cellular biology 25, 1980–1988, https://doi.org/10.1128/mcb.25.5.1980-1988.2005
(2005)."),[24](#ref-CR24 "Conrad, M. et al. Essential role for mitochondrial thioredoxin reductase in hematopoiesis, heart development, and heart function. Molecular and cellular biology 24, 9414–9423, https://doi.org/10.1128/mcb.24.21.9414-9423.2004
(2004)."),[25](#ref-CR25 "Arner, E. S. & Holmgren, A. The thioredoxin system in cancer. Seminars in cancer biology 16, 420–426, https://doi.org/10.1016/j.semcancer.2006.10.009
(2006)."),[26](#ref-CR26 "Bahn, Y. S., Hicks, J. K., Giles, S. S., Cox, G. M. & Heitman, J. Adenylyl cyclase-associated protein Aca1 regulates virulence and differentiation of Cryptococcus neoformans via the cyclic AMP-protein kinase A cascade. Eukaryotic cell 3, 1476–1491, https://doi.org/10.1128/ec.3.6.1476-1491.2004
(2004)."),[27](#ref-CR27 "Arner, E. S. J. Targeting the Selenoprotein Thioredoxin Reductase 1 for Anticancer Therapy. Advances in cancer research 136, 139–151, https://doi.org/10.1016/bs.acr.2017.07.005
(2017)."),[28](#ref-CR28 "Bhatia, M. et al. The thioredoxin system in breast cancer cell invasion and migration. Redox biology 8, 68–78, https://doi.org/10.1016/j.redox.2015.12.004
(2016)."),[29](#ref-CR29 "Gopalakrishna, R., Gundimeda, U., Zhou, S., Bui, H. & Holmgren, A. Redox regulation of protein kinase C by selenometabolites and selenoprotein thioredoxin reductase limits cancer prevention by selenium. Free Radic Biol Med 127, 55–61, https://doi.org/10.1016/j.freeradbiomed.2018.05.062
(2018)."),[30](#ref-CR30 "Zhang, J., Li, X., Han, X., Liu, R. & Fang, J. Targeting the Thioredoxin System for Cancer Therapy. Trends Pharmacol Sci 38, 794–808, https://doi.org/10.1016/j.tips.2017.06.001
(2017)."),[31](#ref-CR31 "Mohammadi, F., Soltani, A., Ghahremanloo, A., Javid, H. & Hashemy, S. I. The thioredoxin system and cancer therapy: a review. Cancer Chemother Pharmacol 84, 925–935, https://doi.org/10.1007/s00280-019-03912-4
(2019)."),[32](/articles/s41598-019-55641-6#ref-CR32 "Jia, J. J., Geng, W. S., Wang, Z. Q., Chen, L. & Zeng, X. S. The role of thioredoxin system in cancer: strategy for cancer therapy. Cancer Chemother Pharmacol 84, 453–470, https://doi.org/10.1007/s00280-019-03869-4
(2019)."). TrxR1, the major isoform of TrxR in the cytoplasm, has been observed to be highly expressed in various malignancies including non-small cell lung carcinoma (NSCLC), breast cancer and hepatocellular carcinoma[33](#ref-CR33 "Chen, G. et al. The serum activity of thioredoxin reductases 1 (TrxR1) is correlated with the poor prognosis in EGFR wild-type and ALK negative non-small cell lung cancer. Oncotarget 8, 115270–115279, https://doi.org/10.18632/oncotarget.23252
(2017)."),34,[35](/articles/s41598-019-55641-6#ref-CR35 "Li, C., Peng, Y., Mao, B. & Qian, K. Thioredoxin reductase: a novel, independent prognostic marker in patients with hepatocellular carcinoma. Oncotarget 6, 17792–17804, https://doi.org/10.18632/oncotarget.3785
(2015)."). Previous studies have suggested TrxR as a potential and effective clinical biomarker of early-stage diagnosis and prognosis after chemotherapy in NSCLC, breast cancer, prostate cancer and liver cancer[35](#ref-CR35 "Li, C., Peng, Y., Mao, B. & Qian, K. Thioredoxin reductase: a novel, independent prognostic marker in patients with hepatocellular carcinoma. Oncotarget 6, 17792–17804, https://doi.org/10.18632/oncotarget.3785
(2015)."),[36](#ref-CR36 "Dong, C. et al. Role of thioredoxin reductase 1 in dysplastic transformation of human breast epithelial cells triggered by chronic oxidative stress. Sci Rep 6, 36860, https://doi.org/10.1038/srep36860
(2016)."),37,[38](/articles/s41598-019-55641-6#ref-CR38 "Ye, S. et al. Thioredoxin Reductase as a Novel and Efficient Plasma Biomarker for the Detection of Non-Small Cell Lung Cancer: a Large-scale, Multicenter study. Sci Rep 9, 2652, https://doi.org/10.1038/s41598-018-38153-7
(2019)."). Moreover, TrxR was also reported to be overexpressed in BGC823 GC cell line, and the inhibition of TrxR activity by the TrxR-specific inhibitor resulted in a robust antitumor effect in BGC823 cell line as well as in vivo in GC xenograft mice, suggesting that TrxR may be a potential biomarker involved in the GC diagnosis and evaluation of therapeutic efficiency39,[40](/articles/s41598-019-55641-6#ref-CR40 "Zhao, F. et al. A thioredoxin reductase inhibitor induces growth inhibition and apoptosis in five cultured human carcinoma cell lines. Cancer letters 236, 46–53, https://doi.org/10.1016/j.canlet.2005.05.010
(2006).").
Currently, we conducted a retrospective study aiming to analyze the efficiency of TrxR activity as a plasma biomarker in the GC diagnosis and evaluation of therapeutic efficiency. Furthermore, we compared the levels of TrxR activity with CEA, CA72-4, CA19-9 and combinations thereof in a large clinical population. Our results revealed that TrxR could be a valuable biomarker of GC diagnosis and therapeutic evaluation for future clinical application.
Materials and Methods
Patients
Patients with pathologically diagnosed gastric cancer and sex- and age-matched healthy controls, as shown in Supplemental Table S1, were continuously recruited from Jiangsu Cancer Hospital (Jiangsu, China), from 2017 to 2019. All healthy controls were in normal conditions based on their complete blood test, liver/kidney functions and chest X-ray examination. Gastric cancer was defined based on computed tomography (CT) results and confirmed by histopathology according to the World Health Organization Classification of Tumors41. Tumor stage was defined according to the 8th IASLC/AJCC staging system42.
Specimen characteristics
Sample collection was performed as described in previous publication[38](/articles/s41598-019-55641-6#ref-CR38 "Ye, S. et al. Thioredoxin Reductase as a Novel and Efficient Plasma Biomarker for the Detection of Non-Small Cell Lung Cancer: a Large-scale, Multicenter study. Sci Rep 9, 2652, https://doi.org/10.1038/s41598-018-38153-7
(2019)."). EDTA or anticoagulant-free tubes were used to collect 5 mL samples of preoperative peripheral blood. Samples were then centrifuged at 3,500 rpm at room temperature for 5 minutes within 2 hours of collection. Supernatants were collected immediately to measure the levels of GC biomarkers.
Analysis of tumor markers
Levels of GC-related tumor markers CEA, CA19-9 and CA72-4 in patients were measured at the indicated time of their visit to the hospital. As described in previous literature[12](/articles/s41598-019-55641-6#ref-CR12 "Feng, F. et al. Diagnostic and prognostic value of CEA, CA19-9, AFP and CA125 for early gastric cancer. BMC Cancer 17, 737, https://doi.org/10.1186/s12885-017-3738-y
(2017)."),[38](/articles/s41598-019-55641-6#ref-CR38 "Ye, S. et al. Thioredoxin Reductase as a Novel and Efficient Plasma Biomarker for the Detection of Non-Small Cell Lung Cancer: a Large-scale, Multicenter study. Sci Rep 9, 2652, https://doi.org/10.1038/s41598-018-38153-7
(2019)."), CEA, CA19-9 and CA72-4 were analyzed based on electrochemiluminescence immunoassay (ECLIA) using Cobas analyzer (Roche Diagnostics, Mannheim, Germany), and performed according to the manufacturer’s instruction. According to the standard clinical guideline from Chinese society of clinical oncology (CSCO), the cut-off value for the tumor markers were set at 3.5 ng/mL for CEA, 39 U/mL for CA19-9, and 6.9 U/mL for CA72-4[43](/articles/s41598-019-55641-6#ref-CR43 "Locker, G. Y. et al. ASCO 2006 update of recommendations for the use of tumor markers in gastrointestinal cancer. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 24, 5313–5327, https://doi.org/10.1200/jco.2006.08.2644
(2006)."),44.
Analysis of TrxR activity
According to the previous publication[33](/articles/s41598-019-55641-6#ref-CR33 "Chen, G. et al. The serum activity of thioredoxin reductases 1 (TrxR1) is correlated with the poor prognosis in EGFR wild-type and ALK negative non-small cell lung cancer. Oncotarget 8, 115270–115279, https://doi.org/10.18632/oncotarget.23252
(2017)."),[36](#ref-CR36 "Dong, C. et al. Role of thioredoxin reductase 1 in dysplastic transformation of human breast epithelial cells triggered by chronic oxidative stress. Sci Rep 6, 36860, https://doi.org/10.1038/srep36860
(2016)."),37,[38](/articles/s41598-019-55641-6#ref-CR38 "Ye, S. et al. Thioredoxin Reductase as a Novel and Efficient Plasma Biomarker for the Detection of Non-Small Cell Lung Cancer: a Large-scale, Multicenter study. Sci Rep 9, 2652, https://doi.org/10.1038/s41598-018-38153-7
(2019)."), 5, 5′-dithiobis (2-nitrobenzoic) acid (DTNB) reduction assay was widely applied to measure the TrxR activity in vitro, especially in biological samples. Basically, TrxR activity was measured by the enzymatic activity of TrxR to catalyze the reduction of DTNB with NADPH to 5-thio-2-nitrobenzoic acid (TNB2-), which generates a strong yellow color with maximum absorbance at 412 nm[45](#ref-CR45 "Wang, L. et al. Ethaselen: a potent mammalian thioredoxin reductase 1 inhibitor and novel organoselenium anticancer agent. Free Radic Biol Med 52, 898–908, https://doi.org/10.1016/j.freeradbiomed.2011.11.034
(2012)."),[46](#ref-CR46 "Luthman, M. & Holmgren, A. Rat liver thioredoxin and thioredoxin reductase: purification and characterization. Biochemistry 21, 6628–6633, https://doi.org/10.1021/bi00269a003
(1982)."),47. In the current study, a specific TrxR inhibitor is used to deduct the background in plasma and determine the reduction of DTNB due only to TrxR activity. TrxR activity was measured by commercially available colorimetric assay kits (Clairvoyance Health Technology, China), and performed according to the manufacturer’s instruction[36](#ref-CR36 "Dong, C. et al. Role of thioredoxin reductase 1 in dysplastic transformation of human breast epithelial cells triggered by chronic oxidative stress. Sci Rep 6, 36860, https://doi.org/10.1038/srep36860
(2016)."),37,[38](/articles/s41598-019-55641-6#ref-CR38 "Ye, S. et al. Thioredoxin Reductase as a Novel and Efficient Plasma Biomarker for the Detection of Non-Small Cell Lung Cancer: a Large-scale, Multicenter study. Sci Rep 9, 2652, https://doi.org/10.1038/s41598-018-38153-7
(2019)."). Full details are provided in Supplemental experimental procedures.
Immunohistochemical analysis
The immunohistochemical analysis of normal gastric mucosa and adenocarcinoma tissues was performed as described previously[48](/articles/s41598-019-55641-6#ref-CR48 "Zhou, M. et al. Plasma thioredoxin reductase activity, a diagnostic biomarker, is up-regulated in resectable non-small cell lung cancers. Translational Cancer Research 6, 383–392, https://doi.org/10.21037/tcr.2017.03.39
(2017)."),49. Briefly, the tissues were dewaxed in xylene (twice for 5 min) and rehydrated in a series of ethanol solutions. Antigen retrieval was performed in sodium citrate buffer in a boiling water bath for 10 min. After cooling, three times washing with PBS (5 min each time) and blocking using a hydrogen peroxide solution, the tissue sections were incubated with the primary antibody (1:500) to TrxR1 (Abcam, USA, 16840) for 8 hours. Secondary anti-rabbit IgG (Maxim, China) was then used to incubate for 30 min[48](/articles/s41598-019-55641-6#ref-CR48 "Zhou, M. et al. Plasma thioredoxin reductase activity, a diagnostic biomarker, is up-regulated in resectable non-small cell lung cancers. Translational Cancer Research 6, 383–392, https://doi.org/10.21037/tcr.2017.03.39
(2017)."). Staining was performed using 3,3′-diaminobenzidine. TrxR expression was scored based on the area and staining intensity according to the previous literature[48](/articles/s41598-019-55641-6#ref-CR48 "Zhou, M. et al. Plasma thioredoxin reductase activity, a diagnostic biomarker, is up-regulated in resectable non-small cell lung cancers. Translational Cancer Research 6, 383–392, https://doi.org/10.21037/tcr.2017.03.39
(2017).").
Statistical analysis
The value of TrxR activity and other tumor biomarkers in human samples did follow the skewed distribution instead of the normal distribution; and therefore, results are described as percentages for categorical variables and as medians (interquartile ranges, IQRs) for the continuous variables. As suggested by previous publications[36](/articles/s41598-019-55641-6#ref-CR36 "Dong, C. et al. Role of thioredoxin reductase 1 in dysplastic transformation of human breast epithelial cells triggered by chronic oxidative stress. Sci Rep 6, 36860, https://doi.org/10.1038/srep36860
(2016)."),[38](/articles/s41598-019-55641-6#ref-CR38 "Ye, S. et al. Thioredoxin Reductase as a Novel and Efficient Plasma Biomarker for the Detection of Non-Small Cell Lung Cancer: a Large-scale, Multicenter study. Sci Rep 9, 2652, https://doi.org/10.1038/s41598-018-38153-7
(2019)."), Chi-squared test were used to calculate and compare the proportions, while non-parametric Mann-Whitney test were applied to compare the continuous variables between groups with a Bonferroni correction. The diagnostic efficacy of biomarkers was evaluated based on the receiver operating characteristic (ROC) curves, the area under the curve (AUC) values and the 95% confidence interval (CI). Logistic regression analysis was used to evaluate the correlations between plasma TrxR activity and other tumor biomarkers by the Spearman test[38](/articles/s41598-019-55641-6#ref-CR38 "Ye, S. et al. Thioredoxin Reductase as a Novel and Efficient Plasma Biomarker for the Detection of Non-Small Cell Lung Cancer: a Large-scale, Multicenter study. Sci Rep 9, 2652, https://doi.org/10.1038/s41598-018-38153-7
(2019)."). All statistical analyses were performed using GraphPad Prism 7 (version 7.0; Graphpad, La Jolla, CA, USA) and SPSS version 19.0 (SPSS Inc., Chicago, IL, USA). P values were calculated by using the non-parametric Mann-Whitney U-test. P values less than 0.05 were considered statistically significant.
Ethics statement
This study was approved by the Ethics Committee of Jiangsu Cancer Hospital (Jiangsu, China). The methods were applied in accordance with the approved guidelines. Informed consent was obtained from all patients.
Results
A total of 923 specimens were recruited in the current study, including 131 specimens from patients with GC before clinical intervention, 662 specimens from patients with GC after chemical drug treatment, and 130 healthy controls.
Plasma TrxR activity in patients with gastric cancer and healthy controls before clinical intervention
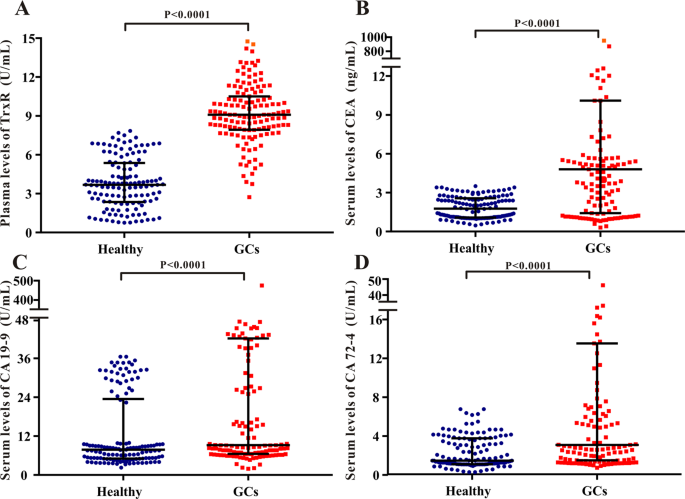
The levels of plasma TrxR activity, serum CEA, serum CA19-9, and serum CA72-4 [median (IQR)] in patients with GC and healthy controls before clinical interventions were detected and analyzed. As shown in Fig. 1A, the plasma levels of TrxR activity in patients with GC [9.09 (7.96, 10.45) U/mL] were significantly higher (P < 0.0001, Mann-Whitney U test) than that in healthy controls [3.69 (2.38, 5.32) U/mL]. Similarly, levels of serum CEA, CA19-9, and CA72-4 in patients with GC were also significantly higher relative to healthy controls, suggesting plasma TrxR activity, as well as CEA, CA19-9, and CA72-4 are sensitive biomarkers elevated in GC before clinical intervention (Fig. 1B—D). Meanwhile, these findings were further strengthened by the overexpression of TrxR protein in GC tissues in comparison with normal gastric mucosa tissues. As shown in Supplemental Fig. S1, TrxR expression was determined to be positive in 60% of the GC tissues. However, its expression in normal gastric mucosa tissue was rarely seen (3/20).
Figure 1
Scatter plot of the distribution of plasma TrxR (A), serum CEA (B), serum CA19-9 (C), and serum CA72-4 (D) levels in GC patients and healthy controls. The black horizontal lines are median values and interquartile ranges. P values were determined by the Mann–Whitney U test.
The efficacy of TrxR activity as a diagnostic biomarker of gastric cancer
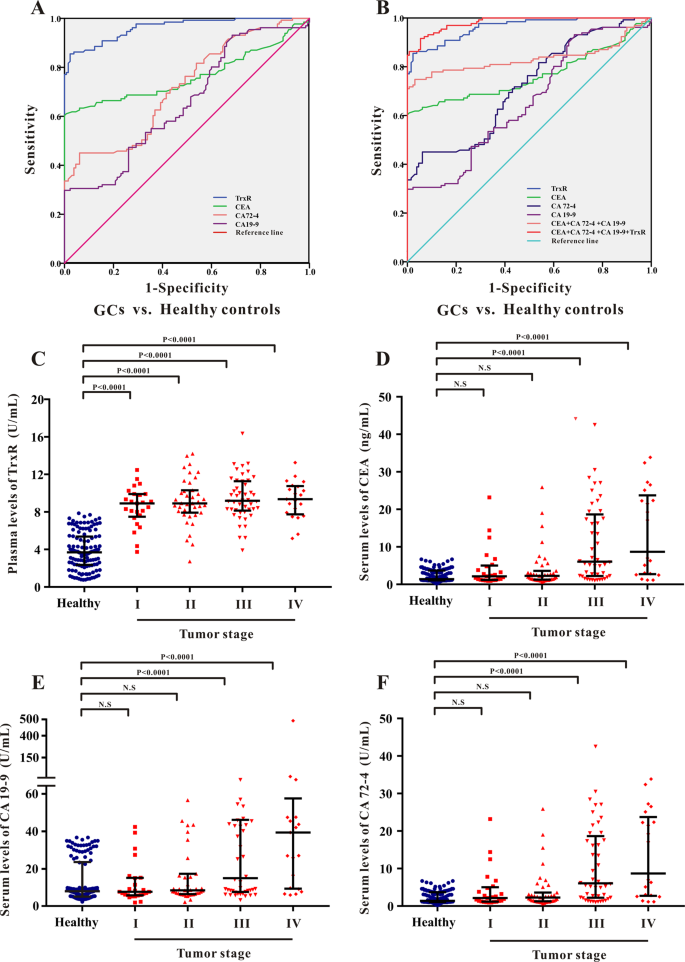
ROC curve analysis was performed to evaluate the efficacy of TrxR plasma activity as a diagnostic biomarker for GC. The maximal Youden Index (sensitivity + specificity-1) was used to calculated the optimal cut-off value of TrxR activity to distinguish between GC patients with healthy controls. As shown in Fig. 2A and Table 1, the critical value of TrxR activity for GC diagnosis was set at 7.34 U/mL based on the ROC curve (AUC 0.963; 95% CI, 0.943-0.983) with a sensitivity of 85.50% and a specificity of 97.69%. As a comparison, CEA displayed the second highest AUC in differentiating GC patients from healthy controls (Fig. 2A and Table 1; 0.764; 95% CI, 0.701–0.826). Meanwhile, CA19-9 and CA72-4 also exhibited moderate capacities for differentiating GC patients from healthy controls with AUCs of 0.657(95% CI, 0.591–0.723) and 0.719 (95% CI, 0.658–0.780), respectively. However, the sensitivities of both CA19-9 and CA72-4 were blow 50%, suggesting the high risk of false-negative rate using CA19-9 and CA72-4 in GC diagnosis. These results indicated that the diagnostic efficacy of plasma TrxR activity in GC was greater than that of CEA, CA19-9 and CA72-4.
Figure 2
(A,B) ROC curve analyses of TrxR, CEA, CA19-9, CA72-4 (A), and the combinations thereof (B) for the differentiation of GCs and healthy controls. (C–F) Scatter plot of the distribution of plasma TrxR (C), serum CEA (D), serum CA19-9 (E), and serum CA72-4 (F) levels in GC patients with various pathological TNM stages. The black horizontal lines are median values and interquartile ranges. P values were determined by the Mann–Whitney U test. N.S: no statistical significance.
Table 1 The diagnostic efficiency of TrxR, CEA, CA72-4, CA19-9 and combinations thereof in differentiating between GC patients and healthy controls.
Furthermore, a binary logistic regression analysis was applied to explore the diagnostic efficacy of the combination of these tumor biomarkers in GC diagnosis. As shown in Fig. 2B and Table 2, the combination panel of CEA, CA19-9 and CA72-4 exhibited an improved diagnostic efficacy for GCs (AUC 0.834; 95% CI, 0.778-0.891) relative to any individual biomarker (P < 0.05). Notably, when adding TrxR into this combination panel, diagnostic efficiency for GC was further elevated (AUC 0.982; 95% CI, 0.970–0.993) relative to the combination of only CEA, CA19-9 and CA72-4 (P < 0.01). These results offered a novel diagnostic panel of 4 biomarkers (TrxR, CEA, CA19-9, CA72-4) in GC diagnosis for future clinical application.
Table 2 The diagnostic efficiency of CEA, CA72-4, CA19-9, and TrxR in discriminating GC patients with various pathological TNM stages from healthy controls.
Plasma TrxR activity in gastric cancer patients with different pathological TNM stage
Previous literature has reported that the existing GC biomarkers, such as CEA, exhibited limited clinical application due to their low sensitivity in patients with early-stage GC[12](/articles/s41598-019-55641-6#ref-CR12 "Feng, F. et al. Diagnostic and prognostic value of CEA, CA19-9, AFP and CA125 for early gastric cancer. BMC Cancer 17, 737, https://doi.org/10.1186/s12885-017-3738-y
(2017)."),[13](/articles/s41598-019-55641-6#ref-CR13 "Zhou, Y. C., Zhao, H. J. & Shen, L. Z. Preoperative serum CEA and CA19-9 in gastric cancer–a single tertiary hospital study of 1,075 cases. Asian Pac J Cancer Prev 16, 2685–2691, https://doi.org/10.7314/apjcp.2015.16.7.2685
(2015)."). In the present study, levels of TrxR, CEA, CA19-9 and CA72-4 were measured in GC patients with different TNM stage and compared with those in healthy controls (Fig. 2 and Supplemental Fig. S2). Consistent with previous publication, levels of CEA, CA72-4 and CA19-9 remained slightly altered in phase I/II GC patients compared with those in healthy controls (Fig. 2D–F and Table 2); however, plasma TrxR activity in phase I/II GC patients were significantly higher than that in healthy controls (P < 0.0001), suggesting its high sensitivity and diagnostic efficiency (AUC > 0.900) in early-stage GC diagnosis (Fig. 2C). Levels of CEA, CA72-4 and CA19-9 displayed strong elevation in phase III/IV GC patients compared with those in phase I/II GC patients (Fig. 2D–F), suggesting the diagnostic efficiency of CEA, CA19-9 and CA72-4 was remarkably improved in late-stage GC.
Plasma TrxR activity in gastric cancer patients after chemotherapy
To further explore the efficacy of TrxR activity in evaluating the clinical outcome of GC patients after chemotherapy, a total of 662 GC patients were divided into two groups according to the clinical outcome: Clinical Responsive Patients (CRP, 456 cases) or Clinical Unresponsive Patients (CUP, 206 cases) based on their CT results. Patients with complete response (CR), partial response (PR) or stable disease (SD) mostly benefited from the chemotherapy and were included into CRP group. On the contrary, patients with progressive disease (PD) or uncontrolled condition after chemotherapy were included into CUP group. Plasma TrxR activity of both CRP and CUP groups were measured for further statistical analyses.
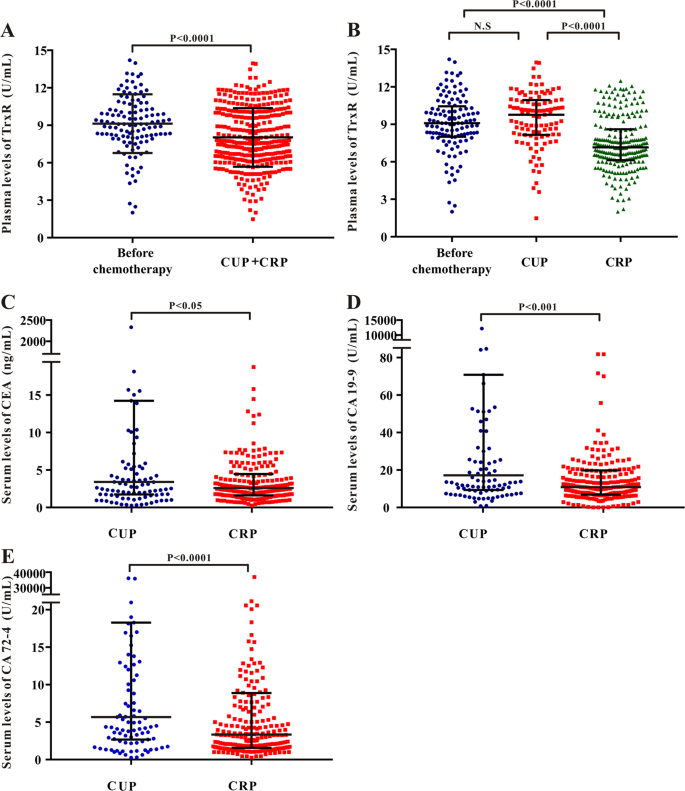
As shown in Fig. 3A, overall levels of TrxR activity in GC patients after chemotherapy [7.58 (6.26, 10.00) U/mL] was relatively lower than that in patients before clinical interventions [9.09 (7.96, 10.45) U/mL]. Notably, among the GC patients after chemotherapy, TrxR activity in CRP group [7.12 (6.08, 8.37) U/mL] was significantly lower than that in CUP group [10.07 (8.19, 11.02) U/mL], suggesting that TrxR activity was markedly reduced when patients benefit from chemotherapy (Fig. 3B). However, TrxR levels remain unaltered in CUP group in comparison with the patients before clinical interventions (P > 0.05). In consistent with TrxR activity, levels of CEA, CA72-4, and CA19-9 were also decreased in CRP group compared with CUP group (Fig. 3C–E).
Figure 3
(A) Scatter plot of the distribution of plasma TR activity levels between GC patients before clinical interventions and GC patients after chemotherapy. (B–E) Scatter plot of the distribution of plasma TrxR (B), serum CEA (C), serum CA19-9 (D), and serum CA72-4 (E) among GC patients with different clinical outcome after chemotherapy (CUP vs. CRP). CUP: clinical unresponsive patient; CRP: clinical responsive patient. The black horizontal lines are median values and interquartile ranges. P values were determined by the Mann–Whitney U test. N.S: no statistical significance.
ROC analysis and cut-off value of TrxR, CEA, CA72-4, and CA19-9 in the evaluation of therapeutic efficiencies of GC after chemotherapy
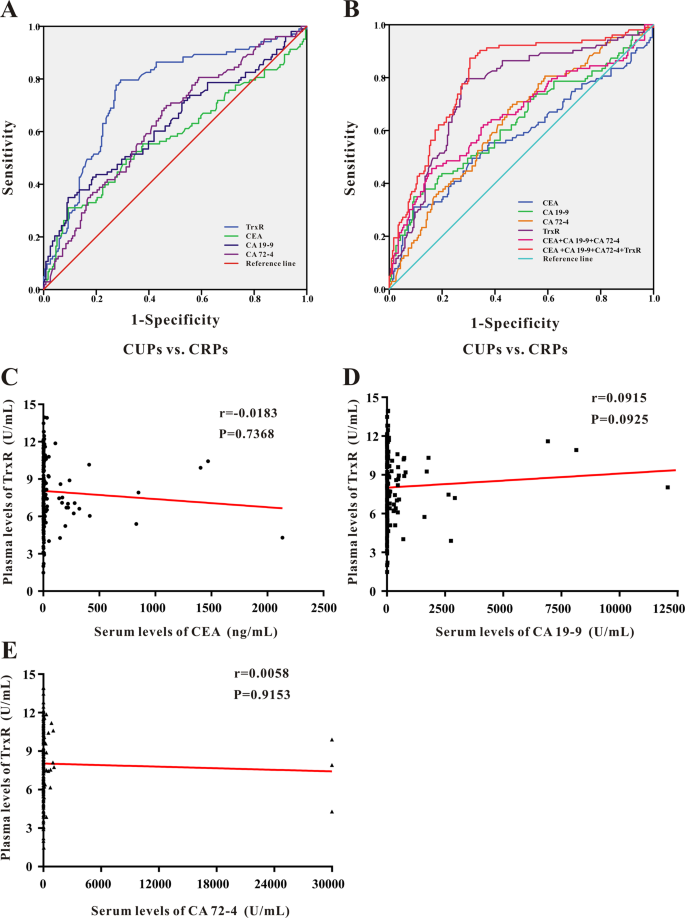
ROC analysis was further applied to evaluate the therapeutic efficiencies of TrxR activity as well as existing GC tumor biomarkers CEA, CA72-4, CA19-9 to differentiate between CRP and CUP group (Fig. 4). The sensitivity, specificity, predictive value, and likelihood ratios of each marker are summarized in Table 3.
Figure 4
(A,B) ROC curve analyses of TrxR, CEA, CA19-9, CA72-4 (A), and the combinations thereof (B) for the differentiation of GCs with different clinical outcome after chemotherapy (CUPs vs. CRPs). (C–E) Pearson correlation analyses between TrxR activity with CEA (C), CA19-9 (D), CA72-4 (E) levels in GC patients after chemotherapy. P values were determined by the Spearman test.
Table 3 The diagnostic efficiency of TrxR, CEA, CA72-4, CA19-9 and combinations thereof in differentiating between CUPs and CRPs in GC patients after chemotherapy.
Among four GC biomarkers, plasma TrxR activity exhibited the highest efficiency to distinguish CRPs from CUPs (AUC 0.751; 95% CI, 0.693–0.808) with a sensitivity of 79.61% and a specificity of 70.06% (Fig. 4A and Table 3). The optimal cut-off value of TrxR activity based on ROC analysis was set at 7.85 U/mL. Meanwhile, CEA, CA19-9 and CA72-4 exhibited similar capacities for differentiating CRPs from CUPs with AUCs of 0.578 (95%CI, 0.506–0.650), 0.628 (95% CI, 0.560–0.697), 0.633 (95% CI, 0.569–0.697), respectively (Fig. 4A and Table 3). These results collectively suggested TrxR as a better biomarker to evaluate the therapeutic efficiencies of GC after chemotherapy in comparison with CEA, CA19-9, and CA72-4.
It is noteworthy that the optimal cut-off values of these GC biomarkers based on ROC analyses were distinct from the thresholds recommended by the CSCO clinical guideline. According to the previous publication and CSCO clinical guideline[43](/articles/s41598-019-55641-6#ref-CR43 "Locker, G. Y. et al. ASCO 2006 update of recommendations for the use of tumor markers in gastrointestinal cancer. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 24, 5313–5327, https://doi.org/10.1200/jco.2006.08.2644
(2006)."),44,[50](#ref-CR50 "Mackenzie, M., Spithoff, K. & Jonker, D. Systemic therapy for advanced gastric cancer: a clinical practice guideline. Current oncology (Toronto, Ont.) 18, e202–209, https://doi.org/10.3747/co.v18i4.737
(2011)."),[51](#ref-CR51 "Wang, F. H. et al. The Chinese Society of Clinical Oncology (CSCO): clinical guidelines for the diagnosis and treatment of gastric cancer. Cancer communications (London, England) 39, 10, https://doi.org/10.1186/s40880-019-0349-9
(2019)."),[52](/articles/s41598-019-55641-6#ref-CR52 "Ye, S. et al. Prospective Clinical Application of Thioredoxin Reductase as a Novel Diagnostic Tumor Marker. Journal of Biosciences and Medicines 02, 44–53, https://doi.org/10.4236/jbm.2014.24008
(2014)."), the cut-off value for these GC markers were recommended at 8 U/mL for TrxR, 3.5 ng/mL for CEA, 39 U/mL for CA19-9, and 6.9 U/mL for CA72-4. Therefore, the sensitivity and specificity of these tumor markers based on the recommended cut-off values were also analyzed to evaluate the therapeutic efficiencies in GC after chemotherapy. As shown in Supplemental Fig. S3, among the four GC biomarkers, TrxR activity displayed the highest sensitivity (81.6%), and effectively distinguish CRP group from CUP group. Nevertheless, CEA, CA72-4 and CA19-9 only exhibited moderate capacities with <52% sensitivity (Supplemental Fig. S3). All these findings suggest TrxR activity as a better biomarker to monitor the therapeutic efficiencies in GC.
Combination of TrxR, CEA, CA19-9, and CA72-4 increase the value of therapeutic evaluation in GC after chemotherapy
Levels of CEA, CA19-9 and CA72-4 are considered as important biomarkers associated with GC and commonly used in the clinical diagnosis9,[10](#ref-CR10 "Yu, J., Zhang, S. & Zhao, B. Differences and correlation of serum CEA, CA19-9 and CA72-4 in gastric cancer. Molecular and clinical oncology 4, 441–449, https://doi.org/10.3892/mco.2015.712
(2016)."),[11](/articles/s41598-019-55641-6#ref-CR11 "Liang, Y. et al. Clinical significance and diagnostic value of serum CEA, CA19-9 and CA72-4 in patients with gastric cancer. Oncotarget 7, 49565–49573, https://doi.org/10.18632/oncotarget.10391
(2016)."). Therefore, it is of great significance to investigate the value of combined detection of TrxR, CEA, CA19-9 and CA72-4 in the evaluation of therapeutic efficiencies in GC after chemotherapy. Through a binary logistic regression, the combination of CEA, CA19-9, and CA72-4 was found to exhibit an improved evaluation of therapeutic efficiency for GC patients (AUC 0.655; 95% CI, 0.587–0.723) relative to any individual biomarker (Fig. 4B and Table 3). In addition, when adding TrxR into this combined group, value of therapeutic evaluation was further strengthened for GC patients (AUC 0.802; 95% CI, 0.750–0.853) relative to TrxR alone or to the combination of other three biomarkers (Table 3). These results offered an excellent modality to evaluate the therapeutic efficiency in GC after chemotherapy.
TrxR as an independent indicator for therapeutic efficiencies in GC after chemotherapy
To further demonstrate the clinical significance of TrxR activity in GC, we investigated the association between TrxR activity and other tumor biomarkers in GC patients after chemotherapy. As displayed in Fig. 4C–E, Pearson correlation analysis indicated no significant correlation between TrxR activity and CEA, CA19-9, or CA72-4 in GC patients. Similarly, no correlation was observed between TrxR activity with other GC biomarkers in CRP or CUP group (Supplemental Fig. S4). These results indicated plasma TrxR activity as an independent indicator for therapeutic efficiencies in GC, and TrxR level was not affected by other tumor biomarkers.
Discussion
Numerous studies have demonstrated the crucial role of TrxR involved in the pathology of carcinomas[17](/articles/s41598-019-55641-6#ref-CR17 "Holmgren, A. & Lu, J. Thioredoxin and thioredoxin reductase: current research with special reference to human disease. Biochemical and biophysical research communications 396, 120–124, https://doi.org/10.1016/j.bbrc.2010.03.083
(2010)."),[20](/articles/s41598-019-55641-6#ref-CR20 "Zhang, J. et al. Small molecule inhibitors of mammalian thioredoxin reductase as potential anticancer agents: An update. Medicinal research reviews 39, 5–39, https://doi.org/10.1002/med.21507
(2019)."),[27](#ref-CR27 "Arner, E. S. J. Targeting the Selenoprotein Thioredoxin Reductase 1 for Anticancer Therapy. Advances in cancer research 136, 139–151, https://doi.org/10.1016/bs.acr.2017.07.005
(2017)."),[28](#ref-CR28 "Bhatia, M. et al. The thioredoxin system in breast cancer cell invasion and migration. Redox biology 8, 68–78, https://doi.org/10.1016/j.redox.2015.12.004
(2016)."),[29](#ref-CR29 "Gopalakrishna, R., Gundimeda, U., Zhou, S., Bui, H. & Holmgren, A. Redox regulation of protein kinase C by selenometabolites and selenoprotein thioredoxin reductase limits cancer prevention by selenium. Free Radic Biol Med 127, 55–61, https://doi.org/10.1016/j.freeradbiomed.2018.05.062
(2018)."),[30](#ref-CR30 "Zhang, J., Li, X., Han, X., Liu, R. & Fang, J. Targeting the Thioredoxin System for Cancer Therapy. Trends Pharmacol Sci 38, 794–808, https://doi.org/10.1016/j.tips.2017.06.001
(2017)."),[31](#ref-CR31 "Mohammadi, F., Soltani, A., Ghahremanloo, A., Javid, H. & Hashemy, S. I. The thioredoxin system and cancer therapy: a review. Cancer Chemother Pharmacol 84, 925–935, https://doi.org/10.1007/s00280-019-03912-4
(2019)."),[32](/articles/s41598-019-55641-6#ref-CR32 "Jia, J. J., Geng, W. S., Wang, Z. Q., Chen, L. & Zeng, X. S. The role of thioredoxin system in cancer: strategy for cancer therapy. Cancer Chemother Pharmacol 84, 453–470, https://doi.org/10.1007/s00280-019-03869-4
(2019)."),[53](/articles/s41598-019-55641-6#ref-CR53 "Lu, J., Chew, E. H. & Holmgren, A. Targeting thioredoxin reductase is a basis for cancer therapy by arsenic trioxide. Proceedings of the National Academy of Sciences of the United States of America 104, 12288–12293, https://doi.org/10.1073/pnas.0701549104
(2007)."),[54](/articles/s41598-019-55641-6#ref-CR54 "Carlson, B. A. et al. Thioredoxin reductase 1 protects against chemically induced hepatocarcinogenesis via control of cellular redox homeostasis. Carcinogenesis 33, 1806–1813, https://doi.org/10.1093/carcin/bgs230
(2012)."). Overexpression of TrxR has been observed in multiple types of tumor, including lung, kidney, breast, stomach and prostate, suggesting TrxR as a pan-cancer biomarker[35](/articles/s41598-019-55641-6#ref-CR35 "Li, C., Peng, Y., Mao, B. & Qian, K. Thioredoxin reductase: a novel, independent prognostic marker in patients with hepatocellular carcinoma. Oncotarget 6, 17792–17804, https://doi.org/10.18632/oncotarget.3785
(2015)."),[36](/articles/s41598-019-55641-6#ref-CR36 "Dong, C. et al. Role of thioredoxin reductase 1 in dysplastic transformation of human breast epithelial cells triggered by chronic oxidative stress. Sci Rep 6, 36860, https://doi.org/10.1038/srep36860
(2016)."),[48](/articles/s41598-019-55641-6#ref-CR48 "Zhou, M. et al. Plasma thioredoxin reductase activity, a diagnostic biomarker, is up-regulated in resectable non-small cell lung cancers. Translational Cancer Research 6, 383–392, https://doi.org/10.21037/tcr.2017.03.39
(2017)."),[52](/articles/s41598-019-55641-6#ref-CR52 "Ye, S. et al. Prospective Clinical Application of Thioredoxin Reductase as a Novel Diagnostic Tumor Marker. Journal of Biosciences and Medicines 02, 44–53, https://doi.org/10.4236/jbm.2014.24008
(2014)."),[55](/articles/s41598-019-55641-6#ref-CR55 "Sobhani, M., Taheri, A. R., Jafarian, A. H. & Hashemy, S. I. The activity and tissue distribution of thioredoxin reductase in basal cell carcinoma. Journal of cancer research and clinical oncology 142, 2303–2307, https://doi.org/10.1007/s00432-016-2242-0
(2016)."). Further studies have confirmed the overexpression of TrxR in GC both in vitro and in vivo39,[40](/articles/s41598-019-55641-6#ref-CR40 "Zhao, F. et al. A thioredoxin reductase inhibitor induces growth inhibition and apoptosis in five cultured human carcinoma cell lines. Cancer letters 236, 46–53, https://doi.org/10.1016/j.canlet.2005.05.010
(2006)."),56. More importantly for diagnostic purposes, the secretion of TrxR into the peripheral blood has been observed and this secreted TrxR has proven to maintain remarkably higher levels in cancer patients compared with in healthy controls57. Additionally, the robust elevation of TrxR level was validated to drive the tumor growth, anti-apoptosis and activation of transcription factors in GC; while the inhibition of TrxR activity by the TrxR-specific inhibitor resulted in a strong antitumor effect in GC both i_n vitro_ and in vivo39,[40](/articles/s41598-019-55641-6#ref-CR40 "Zhao, F. et al. A thioredoxin reductase inhibitor induces growth inhibition and apoptosis in five cultured human carcinoma cell lines. Cancer letters 236, 46–53, https://doi.org/10.1016/j.canlet.2005.05.010
(2006)."). All these evidences suggest that TrxR may be a novel biomarker involved in the pathology of GC.
To the best of our knowledge, it is the first study to investigate the role of TrxR in GC diagnosis and evaluation of therapeutic efficiency using clinical specimen. In this study, the detection of plasma TrxR activity in 131 GC patients before clinical intervention and 130 health controls was conducted, indicating that TrxR activity in patients [9.09 (7.96, 10.45) U/mL] was significantly higher than in health controls [3.69 (2.38, 5.32) U/mL], probably due to the elevated level of TrxR secretion under tumor growth conditions (Fig. 1A). Moreover, a ROC analysis has revealed that the diagnostic efficiency of TrxR activity in distinguishing GCs with health controls is 0.963 for AUC (95% CI, 0.943–0.983) (Fig. 2A and Table 1). Hence, the critical cut-off value of TrxR activity was set at 7.34 U/mL for GC diagnosis (SEN: 85.50%, SPE: 97.69%) based on the maximal Youden Index, which is similar to the cut-off value of plasma TrxR activity (8.0 U/mL) recommended by manufacturer and China Food and Drug Administration (CFDA). Previous studies have also reported the critical cut-off value of plasma TrxR activity in the diagnosis of multiple types of tumor, including NSCLC with 10.18 U/mL and prostate cancer with 8.20 U/mL37,[38](/articles/s41598-019-55641-6#ref-CR38 "Ye, S. et al. Thioredoxin Reductase as a Novel and Efficient Plasma Biomarker for the Detection of Non-Small Cell Lung Cancer: a Large-scale, Multicenter study. Sci Rep 9, 2652, https://doi.org/10.1038/s41598-018-38153-7
(2019)."). All these results suggest that the threshold of TrxR activity was distinctive in the diagnosis of different tumor types.
Several tumor-specific proteins have been previously used in the clinical diagnosis of GC, such as CEA, CA72-4, and CA19-99,[10](#ref-CR10 "Yu, J., Zhang, S. & Zhao, B. Differences and correlation of serum CEA, CA19-9 and CA72-4 in gastric cancer. Molecular and clinical oncology 4, 441–449, https://doi.org/10.3892/mco.2015.712
(2016)."),[11](/articles/s41598-019-55641-6#ref-CR11 "Liang, Y. et al. Clinical significance and diagnostic value of serum CEA, CA19-9 and CA72-4 in patients with gastric cancer. Oncotarget 7, 49565–49573, https://doi.org/10.18632/oncotarget.10391
(2016)."),[58](/articles/s41598-019-55641-6#ref-CR58 "Yin, L. K., Sun, X. Q. & Mou, D. Z. Value of Combined Detection of Serum CEA, CA72-4, CA19-9 and TSGF in the Diagnosis of Gastric Cancer. Asian Pacific journal of cancer prevention: APJCP 16, 3867–3870, https://doi.org/10.7314/apjcp.2015.16.9.3867
(2015)."). Indeed, these proteins have been applied as biomarkers to the diagnosis and prognosis of several cancer types, including as a means of monitoring recurrence and evaluating therapeutic efficiencies in GC[59](/articles/s41598-019-55641-6#ref-CR59 "Jiexian, J. et al. Clinical assessment and prognostic evaluation of tumor markers in patients with gastric cancer. The International journal of biological markers 28, 192–200, https://doi.org/10.5301/jbm.5000023
(2013)."). However, these biomarkers have exhibited limited clinical application due to their low sensitivity and diagnostic capability in patients with GC, especially in early-stage GC. Feng et al. have reported the low sensitivity of CEA (4.3%), CA19-9 (4.8%), AFP (1.5%), and CA125 (1.9%) in 587 cases of phase I GC patients[12](/articles/s41598-019-55641-6#ref-CR12 "Feng, F. et al. Diagnostic and prognostic value of CEA, CA19-9, AFP and CA125 for early gastric cancer. BMC Cancer 17, 737, https://doi.org/10.1186/s12885-017-3738-y
(2017)."). Another study performed by Zhou et al. found that the sensitivity of CEA (22.4%) and CA19-9 (12.3%) was not sufficient for the diagnosis of phase I/II GC patients (1075 cases)[13](/articles/s41598-019-55641-6#ref-CR13 "Zhou, Y. C., Zhao, H. J. & Shen, L. Z. Preoperative serum CEA and CA19-9 in gastric cancer–a single tertiary hospital study of 1,075 cases. Asian Pac J Cancer Prev 16, 2685–2691, https://doi.org/10.7314/apjcp.2015.16.7.2685
(2015)."). In the present study, CEA, CA72-4, and CA19-9 only performed moderately well in GC diagnosis, and their diagnostic sensitivities (61.07% for CEA, 45.04% for CA72-4, and 29.77% for CA19-9) were relatively lower than that of plasma TrxR activity (SEN: 85.50%) (Table 1). All these findings suggest that TrxR activity appear to be a more sensitive and effective biomarker for GC diagnosis. Furthermore, we compared the diagnostic efficiency of these GC biomarkers in different stages of GC (Fig. 2C–F and Supplemental Fig. S2). Levels of CEA, CA72-4, and CA19-9 remained unchanged in phase I/II GC patients compared with those in healthy controls. On the contrary, plasma TrxR activity in phase I/II GC patients were remarkably higher than that in healthy controls, suggesting its higher sensitivity in early-stage GC diagnosis (Table 2). Interestingly, no significant change of TrxR levels was observed among different stage of GC; while levels of CEA, CA72-4 and CA19-9 displayed robust elevation in phase III/IV GC patients, indicating that the routine biomarker such as CEA may be more effective in late-stage GC diagnosis. In addition, we established a joint detection model for GC diagnosis, and incorporated CEA, CA72-4, CA19-9 and TrxR into our panel. Combination of CEA, CA72-4, and CA19-9 displayed the diagnostic sensitivity of 78.41% for GC diagnosis (Fig. 2B and Table 1). After adding TrxR into the diagnostic panel, the sensitivity greatly increased to 91.60%. Therefore, TrxR activity was well validated as an effective and efficient biomarker for GC diagnosis.
The next step was to evaluate the efficacy of TrxR activity to monitor the therapeutic efficiencies of GC patients after chemotherapy. 662 GC patients after chemotherapy were divided into CRP (Clinical Responsive Patients) and CUP (Clinical Unresponsive Patients) group according to their different clinical outcomes. Patients with complete response, partial response or stable disease mostly benefited from the chemotherapy and were included into CRP group. On the contrary, patients with progressive disease or uncontrolled condition after chemotherapy were included into CUP group. Plasma TrxR level in CRP group [7.12 (6.08, 8.37) U/mL] was remarkably decreased when compared with TrxR levels in CUP group [10.07 (8.19, 11.02) U/mL] or in GC patients before clinical interventions [9.09 (7.96, 10.45) U/mL], providing a possibility that TrxR level may be a potential indicator to monitor the therapeutic efficiencies of GC patients (Fig. 3B). Plasma TrxR level was inclined to decrease when GC patients benefited from chemotherapy, while it remained unaltered if GC patients still suffered from progressive disease after chemotherapy. Similar evidence has been previously reported in NSCLC and hepatocellular carcinoma[33](/articles/s41598-019-55641-6#ref-CR33 "Chen, G. et al. The serum activity of thioredoxin reductases 1 (TrxR1) is correlated with the poor prognosis in EGFR wild-type and ALK negative non-small cell lung cancer. Oncotarget 8, 115270–115279, https://doi.org/10.18632/oncotarget.23252
(2017)."),[35](/articles/s41598-019-55641-6#ref-CR35 "Li, C., Peng, Y., Mao, B. & Qian, K. Thioredoxin reductase: a novel, independent prognostic marker in patients with hepatocellular carcinoma. Oncotarget 6, 17792–17804, https://doi.org/10.18632/oncotarget.3785
(2015)."),[48](/articles/s41598-019-55641-6#ref-CR48 "Zhou, M. et al. Plasma thioredoxin reductase activity, a diagnostic biomarker, is up-regulated in resectable non-small cell lung cancers. Translational Cancer Research 6, 383–392, https://doi.org/10.21037/tcr.2017.03.39
(2017)."). For example, Zhou et al. demonstrated that almost 90% of NSCLCs patients (138/149) have shown a significant decrease of TrxR level after surgery, suggesting TrxR activity as a promising biomarker during surgery or clinical treatment[48](/articles/s41598-019-55641-6#ref-CR48 "Zhou, M. et al. Plasma thioredoxin reductase activity, a diagnostic biomarker, is up-regulated in resectable non-small cell lung cancers. Translational Cancer Research 6, 383–392, https://doi.org/10.21037/tcr.2017.03.39
(2017).").
We also investigated the role of CEA, CA72-4, and CA19-9 in monitoring the therapeutic efficiencies of GC patients after chemotherapy. Although the levels of CEA, CA72-4 and CA19-9 were decreased in CRP group compared with CUP group (Fig. 3C–E), the sensitivity of these biomarkers to discriminate between CRP and CUP was still lower than that of plasma TrxR level (Fig. 4A and Table 3). Notably, using the CSCO recommended thresholds of biomarkers instead of the critical cut-off values calculated by ROC analyses, the sensitivities of CEA, CA72-4 and CA19-9 in monitoring the therapeutic efficiencies of GC patients were even declined to 51.4%, 44.6%, and 34.9%, respectively (Supplemental Fig. S3). However, TrxR level still maintained relatively high efficiency with a sensitivity of 81.6% and specificity of 66.1% (Supplemental Fig. S3A). Moreover, the combination detection panel of biomarkers was applied to evaluate the GC therapeutic efficiency. The combination of CEA, CA72-4 and CA19-9 was found to exhibit an improved evaluation of therapeutic efficiency for GC patients relative to any individual biomarker (Fig. 4B and Table 3). When adding TrxR into this combined group, diagnostic efficacy was further strengthened for GC patients relative to TrxR alone or to the combination of routine biomarker screening (Table 3). According to a Pearson correlation analysis results, no significant correlation between TrxR activity and CEA, CA19-9, or CA72-4 was identified, suggesting plasma TrxR activity as an independent indicator for therapeutic efficiencies in GC (Fig. 4C–E and Supplemental Fig. S4). Together, in the present study, all evidences indicate TrxR as a promising biomarker to monitor the therapeutic efficiency of GC patients in future clinical application.
At present, routine biomarker screening (CEA, CA72-4, and CA19-9) is the recommended approach for GC diagnosis and evaluation of therapeutic efficiency, considering the invasive diagnostic strategies such as gastroscope always lead to severe pain and inconvenience[8](/articles/s41598-019-55641-6#ref-CR8 "Miki, K. et al. Clinical application of serum pepsinogen I and II levels for mass screening to detect gastric cancer. Japanese journal of cancer research: Gann 84, 1086–1090, https://doi.org/10.1111/j.1349-7006.1993.tb02805.x
(1993)."),[60](/articles/s41598-019-55641-6#ref-CR60 "Mahar, A. L. et al. Geographic variation in surgical practice patterns and outcomes for resected nonmetastatic gastric cancer in Ontario. Current oncology (Toronto, Ont.) 25, e436–e443, https://doi.org/10.3747/co.25.3953
(2018).") In this study, we proposed plasma TrxR activity as a novel, independent and efficient biomarker for GC diagnosis and therapeutic evaluation. In both cases, TrxR activity displayed higher diagnostic AUC and sensitivity when compared with CEA, CA72-4, and CA19-9. Meanwhile, the combination of TrxR activity with routine biomarkers can further improve the GC diagnostic value and offer a better diagnostic panel for GC patients. However, it is noteworthy that most participants in this retrospective study were from eastern China, and therefore, the presence of common confounding variables and comorbid conditions cannot be ignored. Given the distinct pathogeny of GC existed in different region and ethnicity, future studies are definitely necessary in different cohort of GC patients. Besides, the molecular mechanisms of TrxR activity in GC patients remain to be elucidated, which may further explain the reason of elevated TrxR levels in GC patients.
In summary, this is the first study to investigate the diagnostic relevance of TrxR activity as a plasma biomarker in GCs. Our results indicated that plasma TrxR activity is an effective, efficient and independent biomarker for GC diagnosis and evaluation of therapeutic efficiency, suggesting TrxR activity as a better diagnostic tool in future GC clinical application.
References
- Bray, F. et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a cancer journal for clinicians 68, 394–424, https://doi.org/10.3322/caac.21492 (2018).
Article Google Scholar - Ferlay, J. et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. International journal of cancer 144, 1941–1953, https://doi.org/10.1002/ijc.31937 (2019).
Article CAS PubMed Google Scholar - Zheng Rongshou et al. Analysis of the prevalence of malignant tumors in China, 2015. Chinese Journal of Oncology 41, 19–28, https://doi.org/10.3760/cma.j.issn.0253-3766.2019.01.005 (2019).
Article Google Scholar - Chen, W. et al. Cancer incidence and mortality in China, 2014. Chinese Journal of Cancer Research 30, 1–12 (2018).
Article ADS Google Scholar - Chen Wanqing et al. Analysis of the incidence and mortality of malignant tumors in China, 2014. Chinese Journal of Oncology 27, 1–14, https://doi.org/10.11735/j.issn.1004-0242.2018.01.A001 (2018).
Article Google Scholar - Rota, M. et al. Education and gastric cancer risk-An individual participant data meta-analysis in the StoP project consortium. International journal of cancer, https://doi.org/10.1002/ijc.32298 (2019).
- DeSantis, C. E. et al. Cancer treatment and survivorship statistics, 2014. CA: a cancer journal for clinicians 64, 252–271, https://doi.org/10.3322/caac.21235 (2014).
Article Google Scholar - Miki, K. et al. Clinical application of serum pepsinogen I and II levels for mass screening to detect gastric cancer. Japanese journal of cancer research: Gann 84, 1086–1090, https://doi.org/10.1111/j.1349-7006.1993.tb02805.x (1993).
Article CAS PubMed Google Scholar - Chen, C., Chen, Q., Zhao, Q., Liu, M. & Guo, J. Value of Combined Detection of Serum CEA, CA72-4, CA19-9, CA15-3 and CA12-5 in the Diagnosis of Gastric Cancer. Annals of clinical and laboratory science 47, 260–263 (2017).
CAS PubMed Google Scholar - Yu, J., Zhang, S. & Zhao, B. Differences and correlation of serum CEA, CA19-9 and CA72-4 in gastric cancer. Molecular and clinical oncology 4, 441–449, https://doi.org/10.3892/mco.2015.712 (2016).
Article CAS PubMed Google Scholar - Liang, Y. et al. Clinical significance and diagnostic value of serum CEA, CA19-9 and CA72-4 in patients with gastric cancer. Oncotarget 7, 49565–49573, https://doi.org/10.18632/oncotarget.10391 (2016).
Article PubMed PubMed Central Google Scholar - Feng, F. et al. Diagnostic and prognostic value of CEA, CA19-9, AFP and CA125 for early gastric cancer. BMC Cancer 17, 737, https://doi.org/10.1186/s12885-017-3738-y (2017).
Article CAS PubMed PubMed Central Google Scholar - Zhou, Y. C., Zhao, H. J. & Shen, L. Z. Preoperative serum CEA and CA19-9 in gastric cancer–a single tertiary hospital study of 1,075 cases. Asian Pac J Cancer Prev 16, 2685–2691, https://doi.org/10.7314/apjcp.2015.16.7.2685 (2015).
Article PubMed Google Scholar - Arner, E. S. Focus on mammalian thioredoxin reductases–important selenoproteins with versatile functions. Biochimica et biophysica acta 1790, 495–526, https://doi.org/10.1016/j.bbagen.2009.01.014 (2009).
Article CAS PubMed Google Scholar - Sun, Q. A. et al. Redox regulation of cell signaling by selenocysteine in mammalian thioredoxin reductases. The Journal of biological chemistry 274, 24522–24530, https://doi.org/10.1074/jbc.274.35.24522 (1999).
Article CAS PubMed Google Scholar - Lu, J. & Holmgren, A. Thioredoxin system in cell death progression. Antioxidants & redox signaling 17, 1738–1747, https://doi.org/10.1089/ars.2012.4650 (2012).
Article CAS Google Scholar - Holmgren, A. & Lu, J. Thioredoxin and thioredoxin reductase: current research with special reference to human disease. Biochemical and biophysical research communications 396, 120–124, https://doi.org/10.1016/j.bbrc.2010.03.083 (2010).
Article CAS PubMed Google Scholar - Gromer, S., Urig, S. & Becker, K. The thioredoxin system–from science to clinic. Medicinal research reviews 24, 40–89, https://doi.org/10.1002/med.10051 (2004).
Article CAS PubMed Google Scholar - Lu, J. & Holmgren, A. The thioredoxin antioxidant system. Free Radic Biol Med 66, 75–87, https://doi.org/10.1016/j.freeradbiomed.2013.07.036 (2014).
Article CAS PubMed Google Scholar - Zhang, J. et al. Small molecule inhibitors of mammalian thioredoxin reductase as potential anticancer agents: An update. Medicinal research reviews 39, 5–39, https://doi.org/10.1002/med.21507 (2019).
Article ADS CAS PubMed Google Scholar - Powis, G., Mustacich, D. & Coon, A. The role of the redox protein thioredoxin in cell growth and cancer. Free Radical Biology &. Medicine 29, 312–322 (2000).
CAS Google Scholar - Mustacich, D. & Powis, G. Thioredoxin reductase. The Biochemical journal 346(Pt 1), 1–8 (2000).
Article CAS Google Scholar - Jakupoglu, C. et al. Cytoplasmic thioredoxin reductase is essential for embryogenesis but dispensable for cardiac development. Molecular and cellular biology 25, 1980–1988, https://doi.org/10.1128/mcb.25.5.1980-1988.2005 (2005).
Article CAS PubMed PubMed Central Google Scholar - Conrad, M. et al. Essential role for mitochondrial thioredoxin reductase in hematopoiesis, heart development, and heart function. Molecular and cellular biology 24, 9414–9423, https://doi.org/10.1128/mcb.24.21.9414-9423.2004 (2004).
Article CAS PubMed PubMed Central Google Scholar - Arner, E. S. & Holmgren, A. The thioredoxin system in cancer. Seminars in cancer biology 16, 420–426, https://doi.org/10.1016/j.semcancer.2006.10.009 (2006).
Article CAS PubMed Google Scholar - Bahn, Y. S., Hicks, J. K., Giles, S. S., Cox, G. M. & Heitman, J. Adenylyl cyclase-associated protein Aca1 regulates virulence and differentiation of Cryptococcus neoformans via the cyclic AMP-protein kinase A cascade. Eukaryotic cell 3, 1476–1491, https://doi.org/10.1128/ec.3.6.1476-1491.2004 (2004).
Article CAS PubMed PubMed Central Google Scholar - Arner, E. S. J. Targeting the Selenoprotein Thioredoxin Reductase 1 for Anticancer Therapy. Advances in cancer research 136, 139–151, https://doi.org/10.1016/bs.acr.2017.07.005 (2017).
Article CAS PubMed Google Scholar - Bhatia, M. et al. The thioredoxin system in breast cancer cell invasion and migration. Redox biology 8, 68–78, https://doi.org/10.1016/j.redox.2015.12.004 (2016).
Article CAS PubMed Google Scholar - Gopalakrishna, R., Gundimeda, U., Zhou, S., Bui, H. & Holmgren, A. Redox regulation of protein kinase C by selenometabolites and selenoprotein thioredoxin reductase limits cancer prevention by selenium. Free Radic Biol Med 127, 55–61, https://doi.org/10.1016/j.freeradbiomed.2018.05.062 (2018).
Article CAS PubMed Google Scholar - Zhang, J., Li, X., Han, X., Liu, R. & Fang, J. Targeting the Thioredoxin System for Cancer Therapy. Trends Pharmacol Sci 38, 794–808, https://doi.org/10.1016/j.tips.2017.06.001 (2017).
Article CAS PubMed Google Scholar - Mohammadi, F., Soltani, A., Ghahremanloo, A., Javid, H. & Hashemy, S. I. The thioredoxin system and cancer therapy: a review. Cancer Chemother Pharmacol 84, 925–935, https://doi.org/10.1007/s00280-019-03912-4 (2019).
Article PubMed Google Scholar - Jia, J. J., Geng, W. S., Wang, Z. Q., Chen, L. & Zeng, X. S. The role of thioredoxin system in cancer: strategy for cancer therapy. Cancer Chemother Pharmacol 84, 453–470, https://doi.org/10.1007/s00280-019-03869-4 (2019).
Article CAS PubMed Google Scholar - Chen, G. et al. The serum activity of thioredoxin reductases 1 (TrxR1) is correlated with the poor prognosis in EGFR wild-type and ALK negative non-small cell lung cancer. Oncotarget 8, 115270–115279, https://doi.org/10.18632/oncotarget.23252 (2017).
Article PubMed PubMed Central Google Scholar - Fu, Y. et al. Evaluation of thioredoxin reductase as a novel biomarker in the diagnosis and treatment of breast cancer. Journal of Chinese Pharmaceutical Seciences 23, 711–715 (2014).
CAS Google Scholar - Li, C., Peng, Y., Mao, B. & Qian, K. Thioredoxin reductase: a novel, independent prognostic marker in patients with hepatocellular carcinoma. Oncotarget 6, 17792–17804, https://doi.org/10.18632/oncotarget.3785 (2015).
Article PubMed PubMed Central Google Scholar - Dong, C. et al. Role of thioredoxin reductase 1 in dysplastic transformation of human breast epithelial cells triggered by chronic oxidative stress. Sci Rep 6, 36860, https://doi.org/10.1038/srep36860 (2016).
Article ADS CAS PubMed PubMed Central Google Scholar - Zhang, W., Zheng, X. & Wang, X. Oxidative stress measured by thioredoxin reductase level as potential biomarker for prostate cancer. Am J Cancer Res 5, 2788–2798 (2015).
CAS PubMed PubMed Central Google Scholar - Ye, S. et al. Thioredoxin Reductase as a Novel and Efficient Plasma Biomarker for the Detection of Non-Small Cell Lung Cancer: a Large-scale, Multicenter study. Sci Rep 9, 2652, https://doi.org/10.1038/s41598-018-38153-7 (2019).
Article ADS CAS PubMed PubMed Central Google Scholar - Li, J., Fu, J. N. & Tan, Q. Synergistic effect of ethaselen and cisplatin treatment against tumor cell lines. Journal of Chinese Pharmaceutical Seciences 18, 337–341 (2009).
ADS CAS Google Scholar - Zhao, F. et al. A thioredoxin reductase inhibitor induces growth inhibition and apoptosis in five cultured human carcinoma cell lines. Cancer letters 236, 46–53, https://doi.org/10.1016/j.canlet.2005.05.010 (2006).
Article CAS PubMed Google Scholar - Bosman F. T., et al. WHO Classification of Tumours of the Digestive System, Fourth Edition. Lyon, France: IARC Press; 2010.
- Amin M. B. et al. AJCC Cancer Staging Manual. 8th ed. New York: Springer; 2016.
- Locker, G. Y. et al. ASCO 2006 update of recommendations for the use of tumor markers in gastrointestinal cancer. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 24, 5313–5327, https://doi.org/10.1200/jco.2006.08.2644 (2006).
Article CAS Google Scholar - Wang, F. H. et al. Guidelines of Chinese Society of Clinical Oncology gastric cancer. China: PMPH Press; 2019.
- Wang, L. et al. Ethaselen: a potent mammalian thioredoxin reductase 1 inhibitor and novel organoselenium anticancer agent. Free Radic Biol Med 52, 898–908, https://doi.org/10.1016/j.freeradbiomed.2011.11.034 (2012).
Article CAS PubMed Google Scholar - Luthman, M. & Holmgren, A. Rat liver thioredoxin and thioredoxin reductase: purification and characterization. Biochemistry 21, 6628–6633, https://doi.org/10.1021/bi00269a003 (1982).
Article CAS PubMed Google Scholar - Soderberg, A., Sahaf, B. & Rosen, A. Thioredoxin reductase, a redox-active selenoprotein, is secreted by normal and neoplastic cells: presence in human plasma. Cancer research 60, 2281–2289 (2000).
CAS PubMed Google Scholar - Zhou, M. et al. Plasma thioredoxin reductase activity, a diagnostic biomarker, is up-regulated in resectable non-small cell lung cancers. Translational Cancer Research 6, 383–392, https://doi.org/10.21037/tcr.2017.03.39 (2017).
Article CAS Google Scholar - Kakolyris, S. et al. Thioredoxin expression is associated with lymph node status and prognosis in early operable non-small cell lung cancer. Clin Cancer Res 7, 3087–3091 (2001).
CAS PubMed Google Scholar - Mackenzie, M., Spithoff, K. & Jonker, D. Systemic therapy for advanced gastric cancer: a clinical practice guideline. Current oncology (Toronto, Ont.) 18, e202–209, https://doi.org/10.3747/co.v18i4.737 (2011).
Article CAS Google Scholar - Wang, F. H. et al. The Chinese Society of Clinical Oncology (CSCO): clinical guidelines for the diagnosis and treatment of gastric cancer. Cancer communications (London, England) 39, 10, https://doi.org/10.1186/s40880-019-0349-9 (2019).
Article Google Scholar - Ye, S. et al. Prospective Clinical Application of Thioredoxin Reductase as a Novel Diagnostic Tumor Marker. Journal of Biosciences and Medicines 02, 44–53, https://doi.org/10.4236/jbm.2014.24008 (2014).
Article CAS Google Scholar - Lu, J., Chew, E. H. & Holmgren, A. Targeting thioredoxin reductase is a basis for cancer therapy by arsenic trioxide. Proceedings of the National Academy of Sciences of the United States of America 104, 12288–12293, https://doi.org/10.1073/pnas.0701549104 (2007).
Article ADS CAS PubMed PubMed Central Google Scholar - Carlson, B. A. et al. Thioredoxin reductase 1 protects against chemically induced hepatocarcinogenesis via control of cellular redox homeostasis. Carcinogenesis 33, 1806–1813, https://doi.org/10.1093/carcin/bgs230 (2012).
Article CAS PubMed PubMed Central Google Scholar - Sobhani, M., Taheri, A. R., Jafarian, A. H. & Hashemy, S. I. The activity and tissue distribution of thioredoxin reductase in basal cell carcinoma. Journal of cancer research and clinical oncology 142, 2303–2307, https://doi.org/10.1007/s00432-016-2242-0 (2016).
Article CAS PubMed Google Scholar - Lincoln, D. T., Ali Emadi, E. M., Tonissen, K. F. & Clarke, F. M. The thioredoxin-thioredoxin reductase system: over-expression in human cancer. Anticancer research 23, 2425–2433 (2003).
CAS PubMed Google Scholar - Berghella, A. M., Pellegrini, P., Beato, T. D., Ciccone, F. & Contasta, I. The potential role of thioredoxin 1 and CD30 systems as multiple pathway targets and biomarkers in tumor therapy. Cancer Immunology Immunotherapy 60, 1373–1381 (2011).
Article CAS Google Scholar - Yin, L. K., Sun, X. Q. & Mou, D. Z. Value of Combined Detection of Serum CEA, CA72-4, CA19-9 and TSGF in the Diagnosis of Gastric Cancer. Asian Pacific journal of cancer prevention: APJCP 16, 3867–3870, https://doi.org/10.7314/apjcp.2015.16.9.3867 (2015).
Article PubMed Google Scholar - Jiexian, J. et al. Clinical assessment and prognostic evaluation of tumor markers in patients with gastric cancer. The International journal of biological markers 28, 192–200, https://doi.org/10.5301/jbm.5000023 (2013).
Article PubMed Google Scholar - Mahar, A. L. et al. Geographic variation in surgical practice patterns and outcomes for resected nonmetastatic gastric cancer in Ontario. Current oncology (Toronto, Ont.) 25, e436–e443, https://doi.org/10.3747/co.25.3953 (2018).
Article CAS Google Scholar
Author information
Author notes
- These authors contributed equally: Wei Peng and Zhaofei Zhou.
Authors and Affiliations
- Department of Medicine, Jiangsu Cancer Hospital & Jiangsu Institute of Cancer Research & The Affiliated Cancer Hospital of Nanjing Medical University, Nanjing, China
Wei Peng, Zhaofei Zhou, Yuejiao Zhong, Yan Sun, Yajing Wang & Jianwei Lu - Nantong Tumor Hospital, Nantong, China
Zili Zhu - State Key Laboratory of Natural and Biomimetic Drugs, Peking University Health Science Center, Beijing, China
Wenxuan Jiao, Man Bai & Jing Sun - Keaise Center for Clinical Laboratory, Wuhan, China
Hanwei Yin
Authors
- Wei Peng
You can also search for this author inPubMed Google Scholar - Zhaofei Zhou
You can also search for this author inPubMed Google Scholar - Yuejiao Zhong
You can also search for this author inPubMed Google Scholar - Yan Sun
You can also search for this author inPubMed Google Scholar - Yajing Wang
You can also search for this author inPubMed Google Scholar - Zili Zhu
You can also search for this author inPubMed Google Scholar - Wenxuan Jiao
You can also search for this author inPubMed Google Scholar - Man Bai
You can also search for this author inPubMed Google Scholar - Jing Sun
You can also search for this author inPubMed Google Scholar - Jianwei Lu
You can also search for this author inPubMed Google Scholar - Hanwei Yin
You can also search for this author inPubMed Google Scholar
Contributions
J.L. and H.Y. conceived the research plan. W.P., Zh.Z., and H.Y. devised experiments. W.P., Zh.Z., Y.Z., Y.S., and Y.W. conducted experiments as follows: W.P., Zh.Z., and Y.Z. prepared Figures 1/2 and Table 1; W.P., Y.S., and Y.W. prepared Figures 3/4 and Tables 2/3. W.J., M.B., J.S., and H.Y. analyzed data. W.P., H.Y., and J.L. wrote the manuscript text. Zi.Z. and W.J. provided reagents. W.P., Zi.Z., H.Y., and J.L. edited the manuscript.
Corresponding authors
Correspondence toJianwei Lu or Hanwei Yin.
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Peng, W., Zhou, Z., Zhong, Y. et al. Plasma activity of Thioredoxin Reductase as a Novel Biomarker in Gastric Cancer.Sci Rep 9, 19084 (2019). https://doi.org/10.1038/s41598-019-55641-6
- Received: 09 September 2019
- Accepted: 18 November 2019
- Published: 13 December 2019
- DOI: https://doi.org/10.1038/s41598-019-55641-6