MERS transmission and risk factors: a systematic review (original) (raw)
- Research article
- Open access
- Published: 02 May 2018
- Soyoung Jung2,
- Aeran Kim2 &
- …
- Ji-Eun Park3,4
BMC Public Health volume 18, Article number: 574 (2018)Cite this article
- 16k Accesses
- 88 Altmetric
- Metrics details
Abstract
Background
Since Middle East respiratory syndrome (MERS) infection was first reported in 2012, many studies have analysed its transmissibility and severity. However, the methodology and results of these studies have varied, and there has been no systematic review of MERS. This study reviews the characteristics and associated risk factors of MERS.
Method
We searched international (PubMed, ScienceDirect, Cochrane) and Korean databases (DBpia, KISS) for English- or Korean-language articles using the terms “MERS” and “Middle East respiratory syndrome”. Only human studies with > 20 participants were analysed to exclude studies with low representation. Epidemiologic studies with information on transmissibility and severity of MERS as well as studies containing MERS risk factors were included.
Result
A total of 59 studies were included. Most studies from Saudi Arabia reported higher mortality (22–69.2%) than those from South Korea (20.4%). While the R0 value in Saudi Arabia was < 1 in all but one study, in South Korea, the R0 value was 2.5–8.09 in the early stage and decreased to < 1 in the later stage. The incubation period was 4.5–5.2 days in Saudi Arabia and 6–7.8 days in South Korea. Duration from onset was 4–10 days to confirmation, 2.9–5.3 days to hospitalization, 11–17 days to death, and 14–20 days to discharge. Older age and concomitant disease were the most common factors related to MERS infection, severity, and mortality.
Conclusion
The transmissibility and severity of MERS differed by outbreak region and patient characteristics. Further studies assessing the risk of MERS should consider these factors.
Background
Middle East respiratory syndrome (MERS) was first reported in 2012 in Saudi Arabia [1]. Although most patients are linked to the Arabian Peninsula geographically, MERS has been detected in many other parts of the world [[2](/articles/10.1186/s12889-018-5484-8#ref-CR2 "World Health Organization; WHO MERS-CoV global summary and risk assessment. 2016. http://www.who.int/emergencies/mers-cov/mers-summary-2016.pdf?ua=1&ua=1
. Accessed 20 Oct 2017.")\]. A large MERS cluster was also observed in 2015 in South Korea \[[3](/articles/10.1186/s12889-018-5484-8#ref-CR3 "Ki M. 2015 MERS outbreak in Korea: hospital-to-hospital transmission. Epidemiol Health. 2015;
https://doi.org/10.4178/epih/e2015033
.")\].MERS causes sporadic infection and intrafamilial and healthcare-associated infection. Its symptoms can vary from asymptomatic infection to death. Despite the infection’s association with high mortality, specified antiviral therapy is lacking, especially for patients with concomitant diseases [[2](/articles/10.1186/s12889-018-5484-8#ref-CR2 "World Health Organization; WHO MERS-CoV global summary and risk assessment. 2016. http://www.who.int/emergencies/mers-cov/mers-summary-2016.pdf?ua=1&ua=1
. Accessed 20 Oct 2017.")\].Many previous studies have assessed the risks of MERS, such as factors dictating severity or an infection risk, yet the indices they present vary. For example, the case fatality rate was found to be 25.9% in the Middle East area, but 20.4% in South Korea [4]. The incubation period was reported to be 6.83–7 days in South Korea [4, 5], but 5.5 in a study using data from multiple areas [6] and 5.2 in Saudi Arabia [7]. Accurate assessment of the risk of MERS is essential for predicting and preventing infection.
A systematic review of the risk of MERS, as covered in previous studies, is potentially helpful for predicting this spread, and its future impact. This study aimed at reviewing the risk of MERS, focusing on indices related to infectivity and severity.
Methods
We searched international (PubMed, ScienceDirect, Cochrane) and Korean databases (DBpia, KISS) using the term “MERS” or “Middle East respiratory syndrome”, encompassing articles published after 2000. The search process was conducted in October 2017. We also manually searched the reference lists of the included studies.
Human studies were included, while animal studies and reviews were excluded. Only articles in English or Korean were included. Even if a study collected data on humans, such as collecting specimens from religious pilgrims, it was excluded if there were no MERS patients in the study sample. Additionally, case studies including fewer than 20 MERS patients were excluded as they were considered as having insufficient MERS patient numbers and representative information.
The included studies were classified as epidemiologic studies and those covering risk factors of MERS. In the epidemiologic category, indices related to the risk of MERS were divided into two categories; related to infectivity and related to severity. The index related to infectivity included the reproduction number (R), attack rate, incubation period, serial interval, and days from onset to confirmation. The index related to severity included the case fatality rate (CFR), days from onset to hospitalization, days from onset to discharge, days from onset to death, and days from hospitalization to death.
In the risk factor category, factors related to infection, transmission, severity, and mortality of MERS were analysed. Even if the included studies investigated factors that were related to mortality, when they did not analyse risk factors of severity or mortality using appropriate statistical methods (e.g., regression analysis, Cox proportional hazards model) or only compared prevalence factors, we excluded them from the risk factor category. In all categories, we extracted the study period, number of participants, and geographical region where the data were collected using a data extraction form confirmed after pilot assessment.
Results
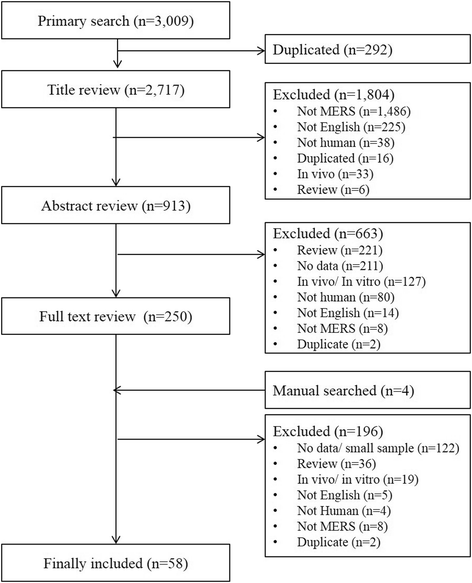
A total of 3009 studies were searched, and 2717 were reviewed, excluding 292 duplicate studies. After the title and abstract review, a further 1804 and 663 were excluded, respectively. Another four studies were included via a manual search, which left a total of 58 studies for analysis (Fig. 1).
Fig. 1
Flow of the systematic review in this study
Epidemiologic studies
The 38 of total 58 included studies were classified as epidemiologic studies (Table 1).
Table 1 Epidemiologic studies of MERS, 2012–2017
R value
R value, representing the reproduction number, indicates the average number of secondary cases generated by infectious individuals. Thirteen studies reported R value of MERS. Four studies that used data from multiple areas had R < 1.0 [6, 8,9,10]. Studies using Saudi Arabia or Middle East area data reported R < 1, at 0.45–0.98 [11,12,13,14], though one reported 1.9–3.9 [[15](/articles/10.1186/s12889-018-5484-8#ref-CR15 "Choi S, Jung E, Choi BY, Hur YJ, Ki M. High reproduction number of Middle East respiratory syndrome coronavirus in nosocomial outbreaks: mathematical modelling in Saudi Arabia and South Korea. J Hosp Infect. 2017; https://doi.org/10.1016/j.jhin.2017.09.017
.")\]. Studies using South Korea data showed higher values, at 2.5–8.09 \[[16](#ref-CR16 "Kim Y, Lee S, Chu C, Choe S, Hong S, Shin Y. The characteristics of middle eastern respiratory syndrome coronavirus transmission dynamics in South Korea. Osong Public Health Res Perspect. 2016;7(1):49–55."),[17](#ref-CR17 "Zhang XS, Pebody R, Charlett A, de Angelis D, Birrell P, Kang H, et al. Estimating and modelling the transmissibility of Middle East respiratory syndrome CoronaVirus during the 2015 outbreak in the Republic of Korea. Influenza Other Respir Viruses. 2017;11(5):434–44."),[18](#ref-CR18 "Chang HJ. Estimation of basic reproduction number of the Middle East respiratory syndrome coronavirus (MERS-CoV) during the outbreak in South Korea, 2015. Biomed Eng Online. 2017;16(1):79."),[19](/articles/10.1186/s12889-018-5484-8#ref-CR19 "Xia ZQ, Zhang J, Xue YK, Sun GQ, Jin Z. Modeling the transmission of Middle East respirator syndrome corona virus in the Republic of Korea. PLoS One. 2015;10(12):e0144778.")\], in the early stage, and < 1 in the later period \[[20](/articles/10.1186/s12889-018-5484-8#ref-CR20 "Kim CJ, Choi WS, Jung Y, Kiem S, Seol HY, Woo HJ, et al. Surveillance of the Middle East respiratory syndrome (MERS) coronavirus (CoV) infection in healthcare workers after contact with confirmed MERS patients: incidence and risk factors of MERS-CoV seropositivity. Biomed Res Int. 2016;22(10):880–6.")\] or with control intervention \[[19](/articles/10.1186/s12889-018-5484-8#ref-CR19 "Xia ZQ, Zhang J, Xue YK, Sun GQ, Jin Z. Modeling the transmission of Middle East respirator syndrome corona virus in the Republic of Korea. PLoS One. 2015;10(12):e0144778.")\].Attack rate
A total of eight studies reported the attack rate. Four reported the overall or secondary attack rate, and the other four reported the attack rate of specific participant groups. Two studies conducted in Saudi Arabia showed 0.42% [21] and 4% [22] secondary attack rates. Studies in South Korea showed secondary attack rates of 3.7% in one study [23] and 14.3–15.8% in another [24].
Two studies reported the attack rate among healthcare workers (HCWs). One study in South Korea reported a MERS incidence of 1.5% among HCWs [20], and another study using multiple area data reported a 13.4–13.5% infection rate among HCWs [8]. The attack rate among hospital patients was 4% in one study [5] and 22% in the early and 1% in the later period in another [16].
Incubation period
The incubation period is the period between infection and appearance of signs of a disease. A total of 12 studies reported the incubation period of MERS. Nine used data from South Korea and showed a 6–7.8 day incubation period [[3](#ref-CR3 "Ki M. 2015 MERS outbreak in Korea: hospital-to-hospital transmission. Epidemiol Health. 2015; https://doi.org/10.4178/epih/e2015033
."),[4](#ref-CR4 "Korea Centers for Disease Control & Prevention. Middle East respiratory syndrome coronavirus outbreak in the Republic of Korea, 2015. Osong Public Health Res Perspect. 2015;6(4):269–78."),[5](/articles/10.1186/s12889-018-5484-8#ref-CR5 "Cho SY, Kang JM, Ha YE, Park GE, Lee JY, Ko JH, et al. MERS-CoV outbreak following a single patient exposure in an emergency room in South Korea: an epidemiological outbreak study. Lancet. 2016;388(10048):994–1001."), [23](#ref-CR23 "Park JW, Lee KJ, Lee KH, Lee SH, Cho JR, Mo JW, et al. Hospital outbreaks of Middle East respiratory syndrome, Daejeon, South Korea, 2015. Emerg Infect Dis. 2017;23(6):898–905."),[24](#ref-CR24 "Park SH, Kim YS, Jung Y, Choi SY, Cho NH, Jeong HW, et al. Outbreaks of Middle East respiratory syndrome in two hospitals initiated by a single patient in Daejeon, South Korea. Infect Chemother. 2016;48(2):99–107."),[25](#ref-CR25 "Virlogeux V, Park M, Wu JT, Cowling BJ. Association between severity of MERS-CoV infection and incubation period. Emerg Infect Dis. 2016;22(3):526–8."),[26](#ref-CR26 "Cowling BJ, Park M, Fang VJ, Wu P, Leung GM, Wu JT. Preliminary epidemiological assessment of MERS-CoV outbreak in South Korea, May to June 2015. Euro Surveill. 2015;20(25):7–13."),[27](#ref-CR27 "Ministry of Health and Welfare, Republic of Korea. MERS white book. 2016.
http://www.cdc.go.kr/CDC/intro/CdcKrIntro0101.jsp?menuIds=HOME001-MNU1154-MNU0005-MNU0010&cid=70039
. Accessed 10 Oct 2017."),[28](/articles/10.1186/s12889-018-5484-8#ref-CR28 "Park HY, Lee EJ, Ryu YW, Kim Y, Kim H, Lee H, et al. Epidemiological investigation of MERS-CoV spread in a single hospital in South Korea, May to June 2015. Euro Surveill. 2015;20(25):1–6.")\]. One study using data from Saudi Arabia reported a 5.2 day incubation period \[[7](/articles/10.1186/s12889-018-5484-8#ref-CR7 "Assiri A, Al-Tawfiq JA, Al-Rabeeah AA, Al-Rabiah FA, Al-Hajjar S, Al-Barrak A, et al. Epidemiological, demographic, and clinical characteristics of 47 cases of Middle East respiratory syndrome coronavirus disease from Saudi Arabia: a descriptive study. Lancet Infect Dis. 2013;13(9):752–61.")\], and another using data from multiple areas reported a 5.5 day incubation period \[[6](/articles/10.1186/s12889-018-5484-8#ref-CR6 "Cauchemez S, Fraser C, Van Kerkhove MD, Donnelly CA, Riley S, Rambaut A, et al. Middle East respiratory syndrome coronavirus: quantification of the extent of the epidemic, surveillance biases, and transmissibility. Lancet Infect Dis. 2014;14(1):50–6.")\]. Sha et al. compared the incubation periods between the Middle East area and South Korea and reported 4.5–5 and 6 days, respectively \[[29](/articles/10.1186/s12889-018-5484-8#ref-CR29 "Sha J, Li Y, Chen X, Hu Y, Ren Y, Geng X, et al. Fatality risks for nosocomial outbreaks of Middle East respiratory syndrome coronavirus in the Middle East and South Korea. Arch Virol. 2017;162(1):33–44.")\].Serial interval
The serial interval of an infectious disease represents the duration between symptom onset of a primary case and of its secondary cases. Two studies used South Korea data, reporting serial intervals of MERS of 12.6 and 14.6 days, respectively [24, 26].
Days from onset to confirmation
Among five studies reporting days from onset to confirmation, three studies used data from South Korea. One study analysing all South Korea cases reported 5 days from onset to confirmation [[3](/articles/10.1186/s12889-018-5484-8#ref-CR3 "Ki M. 2015 MERS outbreak in Korea: hospital-to-hospital transmission. Epidemiol Health. 2015; https://doi.org/10.4178/epih/e2015033
.")\]. Park et al. reported 6.5 days for all cases, 9 for second generation and 4 for third generation \[[28](/articles/10.1186/s12889-018-5484-8#ref-CR28 "Park HY, Lee EJ, Ryu YW, Kim Y, Kim H, Lee H, et al. Epidemiological investigation of MERS-CoV spread in a single hospital in South Korea, May to June 2015. Euro Surveill. 2015;20(25):1–6.")\]. One study from Taiwan reported 6 days for HCWs and 10 for non-HCWs \[[30](/articles/10.1186/s12889-018-5484-8#ref-CR30 "Liu M, Jiang C, Donovan C, Wen Y, Sun W. Middle East respiratory syndrome and medical students: letter from China. Int J Environ Res Public Health. 2015;12(10):13289–94.")\]. A study from Saudi Arabia reported 4 days from onset to confirmation \[[31](/articles/10.1186/s12889-018-5484-8#ref-CR31 "Ahmed AE. Diagnostic delays in 537 symptomatic cases of Middle East respiratory syndrome coronavirus infection in Saudi Arabia. Int J Infect Dis. 2017;62:47–51.")\]. Sha et al. compared the data from Middle East and South Korea areas and reported 4–8 and 4–5 days, respectively \[[29](/articles/10.1186/s12889-018-5484-8#ref-CR29 "Sha J, Li Y, Chen X, Hu Y, Ren Y, Geng X, et al. Fatality risks for nosocomial outbreaks of Middle East respiratory syndrome coronavirus in the Middle East and South Korea. Arch Virol. 2017;162(1):33–44.")\].Days from onset to hospitalization
Two studies from Saudi Arabia reported days from onset to hospitalization. One reported 2.9–5 days [32], and the other reported 5.3 days [33].
Mortality
Twenty-six studies reported on MERS-related mortality. Ten reported the mortality rate in South Korea as 14.5–47.8% [[3](/articles/10.1186/s12889-018-5484-8#ref-CR3 "Ki M. 2015 MERS outbreak in Korea: hospital-to-hospital transmission. Epidemiol Health. 2015; https://doi.org/10.4178/epih/e2015033
."), [4](/articles/10.1186/s12889-018-5484-8#ref-CR4 "Korea Centers for Disease Control & Prevention. Middle East respiratory syndrome coronavirus outbreak in the Republic of Korea, 2015. Osong Public Health Res Perspect. 2015;6(4):269–78."), [23](#ref-CR23 "Park JW, Lee KJ, Lee KH, Lee SH, Cho JR, Mo JW, et al. Hospital outbreaks of Middle East respiratory syndrome, Daejeon, South Korea, 2015. Emerg Infect Dis. 2017;23(6):898–905."),[24](#ref-CR24 "Park SH, Kim YS, Jung Y, Choi SY, Cho NH, Jeong HW, et al. Outbreaks of Middle East respiratory syndrome in two hospitals initiated by a single patient in Daejeon, South Korea. Infect Chemother. 2016;48(2):99–107."),[25](#ref-CR25 "Virlogeux V, Park M, Wu JT, Cowling BJ. Association between severity of MERS-CoV infection and incubation period. Emerg Infect Dis. 2016;22(3):526–8."),[26](/articles/10.1186/s12889-018-5484-8#ref-CR26 "Cowling BJ, Park M, Fang VJ, Wu P, Leung GM, Wu JT. Preliminary epidemiological assessment of MERS-CoV outbreak in South Korea, May to June 2015. Euro Surveill. 2015;20(25):7–13."), [28](/articles/10.1186/s12889-018-5484-8#ref-CR28 "Park HY, Lee EJ, Ryu YW, Kim Y, Kim H, Lee H, et al. Epidemiological investigation of MERS-CoV spread in a single hospital in South Korea, May to June 2015. Euro Surveill. 2015;20(25):1–6."), [29](/articles/10.1186/s12889-018-5484-8#ref-CR29 "Sha J, Li Y, Chen X, Hu Y, Ren Y, Geng X, et al. Fatality risks for nosocomial outbreaks of Middle East respiratory syndrome coronavirus in the Middle East and South Korea. Arch Virol. 2017;162(1):33–44."), [34](/articles/10.1186/s12889-018-5484-8#ref-CR34 "Kim SW, Park JW, Jung HD, Yang JS, Park YS, Lee C, et al. Risk factors for transmission of Middle East respiratory syndrome coronavirus infection during the 2015 outbreak in South Korea. Clin Infect Dis. 2017;64(5):551–7."), [35](/articles/10.1186/s12889-018-5484-8#ref-CR35 "Mizumoto K, Saitoh M, Chowell G, Miyamatsu Y, Nishiura H. Estimating the risk of Middle East respiratory syndrome (MERS) death during the course of the outbreak in the Republic of Korea, 2015. Int J Infect Dis. 2015;39:7–9.")\]; one of which, including all MERS patients in South Korea, reported a mortality rate of 20.4% \[[27](/articles/10.1186/s12889-018-5484-8#ref-CR27 "Ministry of Health and Welfare, Republic of Korea. MERS white book. 2016.
http://www.cdc.go.kr/CDC/intro/CdcKrIntro0101.jsp?menuIds=HOME001-MNU1154-MNU0005-MNU0010&cid=70039
. Accessed 10 Oct 2017.")\]. Ten studies analysing data from Saudi Arabia reported higher mortality rates, of 22–69.2% \[[7](/articles/10.1186/s12889-018-5484-8#ref-CR7 "Assiri A, Al-Tawfiq JA, Al-Rabeeah AA, Al-Rabiah FA, Al-Hajjar S, Al-Barrak A, et al. Epidemiological, demographic, and clinical characteristics of 47 cases of Middle East respiratory syndrome coronavirus disease from Saudi Arabia: a descriptive study. Lancet Infect Dis. 2013;13(9):752–61."), [12](/articles/10.1186/s12889-018-5484-8#ref-CR12 "Alenazi TH, Al Arbash H, El-Saed A, Alshamrani MM, Baffoe-Bonnie H, Arabi YM, et al. Identified transmission dynamics of Middle East respiratory syndrome coronavirus infection during an outbreak: implications of an overcrowded emergency department. Clin Infect Dis. 2017;65(4):675–9."), [22](/articles/10.1186/s12889-018-5484-8#ref-CR22 "Drosten C, Meyer B, Muller MA, Corman VM, Al-Masri M, Hossain R, et al. Transmission of MERS-coronavirus in household contacts. N Engl J Med. 2014;371(9):828–35."), [31](#ref-CR31 "Ahmed AE. Diagnostic delays in 537 symptomatic cases of Middle East respiratory syndrome coronavirus infection in Saudi Arabia. Int J Infect Dis. 2017;62:47–51."),[32](#ref-CR32 "Sherbini N, Iskandrani A, Kharaba A, Khalid G, Abduljawad M, Al-Jahdali H. Middle East respiratory syndrome coronavirus in Al-Madinah City, Saudi Arabia: demographic, clinical and survival data. J Epidemiolo Glob Health. 2017;7(1):29–36."),[33](/articles/10.1186/s12889-018-5484-8#ref-CR33 "Halim AA, Alsayed B, Embarak S, Yaseen T, Dabbous S. Clinical characteristics and outcome of ICU admitted MERS corona virus infected patients. Egypt J Chest Dis Tuberc. 2016;65(1):81–7."), [36](#ref-CR36 "Assiri A, Abedi GR, Bin Saeed AA, Abdalla MA, al-Masry M, Choudhry AJ, et al. Multifacility outbreak of Middle East respiratory syndrome in Taif, Saudi Arabia. Emerg Infect Dis. 2016;22(1):32–40."),[37](#ref-CR37 "Noorwali AA, Turkistani AM, Asiri SI, Trabulsi FA, Alwafi OM, Alzahrani SH, et al. Descriptive epidemiology and characteristics of confirmed cases of Middle East respiratory syndrome coronavirus infection in the Makkah Region of Saudi Arabia, March to June 2014. Ann Saudi Med. 2015;35(3):203–9."),[38](#ref-CR38 "Oboho IK, Tomczyk SM, Al-Asmari AM, Banjar AA, Al-Mugti H, Aloraini MS, et al. 2014 MERS-CoV outbreak in Jeddah--a link to health care facilities. N Engl J Med. 2015;372(9):846–54."),[39](/articles/10.1186/s12889-018-5484-8#ref-CR39 "Lessler J, Salje H, Van Kerkhove MD, Ferguson NM, Cauchemez S, Rodriquez-Barraquer I, et al. Estimating the severity and subclinical burden of Middle East respiratory syndrome coronavirus infection in the Kingdom of Saudi Arabia. Am J Epidemiol. 2016;183(7):657–63.")\], although others reported mortality rates 10% \[[40](/articles/10.1186/s12889-018-5484-8#ref-CR40 "Mohd HA, Memish ZA, Alfaraj SH, McClish D, Altuwaijri T, Alanazi MS, et al. Predictors of MERS-CoV infection: a large case control study of patients presenting with ILI at a MERS-CoV referral hospital in Saudi Arabia. Travel Med Infect Dis. 2016;14(5):464–70.")\] and 19.9% \[[21](/articles/10.1186/s12889-018-5484-8#ref-CR21 "El Bushra HE, Al Arbash HA, Mohammed M, Abdalla O, Abdallah MN, Al-Mayahi ZK, et al. Outcome of strict implementation of infection prevention control measures during an outbreak of Middle East respiratory syndrome. Am J Infect Control. 2017;45(5):502–7.")\]. A Taiwanese study reported a mortality rate of 35.6% \[[30](/articles/10.1186/s12889-018-5484-8#ref-CR30 "Liu M, Jiang C, Donovan C, Wen Y, Sun W. Middle East respiratory syndrome and medical students: letter from China. Int J Environ Res Public Health. 2015;12(10):13289–94.")\]. Studies using data from multiple areas reported mortality rates ranging from 26.6% \[[29](/articles/10.1186/s12889-018-5484-8#ref-CR29 "Sha J, Li Y, Chen X, Hu Y, Ren Y, Geng X, et al. Fatality risks for nosocomial outbreaks of Middle East respiratory syndrome coronavirus in the Middle East and South Korea. Arch Virol. 2017;162(1):33–44.")\] to 59.4% \[[9](/articles/10.1186/s12889-018-5484-8#ref-CR9 "Breban R, Riou J, Fontanet A. Interhuman transmissibility of Middle East respiratory syndrome coronavirus: estimation of pandemic risk. Lancet. 2013;382(9893):694–9."), [41](/articles/10.1186/s12889-018-5484-8#ref-CR41 "Penttinen PM, Kaasik-Aaslav K, Friaux A, Donachie A, Sudre B, Amato-Gauci AJ, et al. Taking stock of the first 133 MERS coronavirus cases globally--is the epidemic changing? Euro Surveill. 2013;18(39)")\].Days from onset to discharge
Three studies reported days from MERS onset to discharge. Sha et al. reported 14 days in the Middle East area and 17 in South Korea [29]. One study from Saudi Arabia reported 17 days [36], and another in South Korea reported 20 [[3](/articles/10.1186/s12889-018-5484-8#ref-CR3 "Ki M. 2015 MERS outbreak in Korea: hospital-to-hospital transmission. Epidemiol Health. 2015; https://doi.org/10.4178/epih/e2015033
.")\].Days from onset to death
Two Korean studies reported similar periods of 11–13 days from onset to death: 11–12.5 in Park et al. [24] and 13 in Ki et al. [[3](/articles/10.1186/s12889-018-5484-8#ref-CR3 "Ki M. 2015 MERS outbreak in Korea: hospital-to-hospital transmission. Epidemiol Health. 2015; https://doi.org/10.4178/epih/e2015033
.")\]. Although one study from Saudi Arabia reported longer than 17 days from onset to death \[[36](/articles/10.1186/s12889-018-5484-8#ref-CR36 "Assiri A, Abedi GR, Bin Saeed AA, Abdalla MA, al-Masry M, Choudhry AJ, et al. Multifacility outbreak of Middle East respiratory syndrome in Taif, Saudi Arabia. Emerg Infect Dis. 2016;22(1):32–40.")\], Sha et al., comparing data between the Middle East and South Korea, reported similar periods of 11.5 and 11 days, respectively \[[29](/articles/10.1186/s12889-018-5484-8#ref-CR29 "Sha J, Li Y, Chen X, Hu Y, Ren Y, Geng X, et al. Fatality risks for nosocomial outbreaks of Middle East respiratory syndrome coronavirus in the Middle East and South Korea. Arch Virol. 2017;162(1):33–44.")\]. One Taiwanese study also reported a similar period of 12–13 days \[[30](/articles/10.1186/s12889-018-5484-8#ref-CR30 "Liu M, Jiang C, Donovan C, Wen Y, Sun W. Middle East respiratory syndrome and medical students: letter from China. Int J Environ Res Public Health. 2015;12(10):13289–94.")\].Days from hospitalization to death
Two studies reported a similar length of hospitalization: 15 [33] and 15.2 days [19].
Risk factors related to mortality
Of the 20 studies included in the risk factor category, four were duplicates of studies in the epidemiologic category as they had information regarding the epidemiologic index and risk factors (Table 2).
Table 2 Factors related to infection, transmission, severity, and mortality of MERS
Factors related to MERS infection
Two studies reported on the risk factors of MERS infection. Alraddadi et al. [42] analysed the effect of non-human contact, including travel history, animal-related exposure, food exposure, health condition, and behaviour and reported direct dromedary exposure, diabetes or heart disease, and smoking as risk factors of MERS infection. Another study reported older age, outbreak week, and nationality as risk factors [43].
Factors related to MERS transmission
Three studies analysed factors associated with spreaders. Non-isolated in-hospital days, hospitalization or emergency room visits before isolation, deceased patients, and clinical symptoms, including fever, chest X-ray abnormality in more than three lung zones, and the cycle threshold value, were related to spreaders [34, 44, 45].
Factors related to MERS severity
Four studies reported risk factors of MERS severity. The included studies showed that the PRNT50 and CD4 T cell response [46] as well as a high MERS virus load [47] were associated with the severity of MERS. Additionally, male sex; older age; concomitant disease, including hypertension; and symptoms, including fever, thrombocytopenia, lymphopenia, and low albumin concentration, were related to MERS severity or secondary disease [47,48,49].
Factors related to MERS mortality
Fifteen studies reported risk factors of mortality in MERS patients. Older age [4, 25, 32, 49,50,51,52,53,54,55] and comorbidity [29, 50,51,52, 54], including diabetes [32, 55], chronic kidney disease [32], respiratory disease [4, 55], pneumonia [56], cardiac disease, and cancer [53], were the most prevalent in the included studies. Male sex was reported as a risk factor in one study [56]. Smoking [32, 56] and location of acquisition [51, 53] were also reported. While one study noted that HCW, as a profession, was associated with mortality [53], non-HCWs were reported to be related to mortality in two other studies [50, 51].
Additionally, a shorter incubation period [25, 56], longer duration of symptoms [32], more days from onset to confirmation [29], later epidemic period [52], and longer hospitalized days [29] were reported as mortality risk factors.
Symptoms at diagnosis, including abnormal renal function [56], respiratory symptoms [56], gastrointestinal symptoms [32], lower blood pressure [32, 55], and leucocytosis [55, 56], were also found to be associated with mortality in MERS patients.
Severity of illness, [50, 51] such as need for vasopressors [57], chest radiographic score [58], health condition [59], use of mechanical ventilation [55], and occurrence of dyspnoea [55] were also found to increase the mortality risk.
Epidemiological index of MERS between the Middle East area and South Korea
The characteristics of MERS differ between South Korea and the Middle East area. The R value of MERS was reported to be below 1 in the Middle East area, except in one study [[15](/articles/10.1186/s12889-018-5484-8#ref-CR15 "Choi S, Jung E, Choi BY, Hur YJ, Ki M. High reproduction number of Middle East respiratory syndrome coronavirus in nosocomial outbreaks: mathematical modelling in Saudi Arabia and South Korea. J Hosp Infect. 2017; https://doi.org/10.1016/j.jhin.2017.09.017
.")\], but was from 2.5–8.1 in South Korea \[[15](#ref-CR15 "Choi S, Jung E, Choi BY, Hur YJ, Ki M. High reproduction number of Middle East respiratory syndrome coronavirus in nosocomial outbreaks: mathematical modelling in Saudi Arabia and South Korea. J Hosp Infect. 2017;
https://doi.org/10.1016/j.jhin.2017.09.017
."),[16](#ref-CR16 "Kim Y, Lee S, Chu C, Choe S, Hong S, Shin Y. The characteristics of middle eastern respiratory syndrome coronavirus transmission dynamics in South Korea. Osong Public Health Res Perspect. 2016;7(1):49–55."),[17](#ref-CR17 "Zhang XS, Pebody R, Charlett A, de Angelis D, Birrell P, Kang H, et al. Estimating and modelling the transmissibility of Middle East respiratory syndrome CoronaVirus during the 2015 outbreak in the Republic of Korea. Influenza Other Respir Viruses. 2017;11(5):434–44."),[18](#ref-CR18 "Chang HJ. Estimation of basic reproduction number of the Middle East respiratory syndrome coronavirus (MERS-CoV) during the outbreak in South Korea, 2015. Biomed Eng Online. 2017;16(1):79."),[19](/articles/10.1186/s12889-018-5484-8#ref-CR19 "Xia ZQ, Zhang J, Xue YK, Sun GQ, Jin Z. Modeling the transmission of Middle East respirator syndrome corona virus in the Republic of Korea. PLoS One. 2015;10(12):e0144778.")\]. Although studies using data from the Middle East area reported 0.42–4% secondary attack rates, studies in South Korea reported 4–6% secondary attack rates for patients or hospital visitors \[[5](/articles/10.1186/s12889-018-5484-8#ref-CR5 "Cho SY, Kang JM, Ha YE, Park GE, Lee JY, Ko JH, et al. MERS-CoV outbreak following a single patient exposure in an emergency room in South Korea: an epidemiological outbreak study. Lancet. 2016;388(10048):994–1001.")\], and 3.7–15.8% for the overall attack rate \[[23](/articles/10.1186/s12889-018-5484-8#ref-CR23 "Park JW, Lee KJ, Lee KH, Lee SH, Cho JR, Mo JW, et al. Hospital outbreaks of Middle East respiratory syndrome, Daejeon, South Korea, 2015. Emerg Infect Dis. 2017;23(6):898–905."), [24](/articles/10.1186/s12889-018-5484-8#ref-CR24 "Park SH, Kim YS, Jung Y, Choi SY, Cho NH, Jeong HW, et al. Outbreaks of Middle East respiratory syndrome in two hospitals initiated by a single patient in Daejeon, South Korea. Infect Chemother. 2016;48(2):99–107.")\]. The MERS incubation period was reported to be 4.5–5.2 days in the Middle East area \[[7](/articles/10.1186/s12889-018-5484-8#ref-CR7 "Assiri A, Al-Tawfiq JA, Al-Rabeeah AA, Al-Rabiah FA, Al-Hajjar S, Al-Barrak A, et al. Epidemiological, demographic, and clinical characteristics of 47 cases of Middle East respiratory syndrome coronavirus disease from Saudi Arabia: a descriptive study. Lancet Infect Dis. 2013;13(9):752–61."), [29](/articles/10.1186/s12889-018-5484-8#ref-CR29 "Sha J, Li Y, Chen X, Hu Y, Ren Y, Geng X, et al. Fatality risks for nosocomial outbreaks of Middle East respiratory syndrome coronavirus in the Middle East and South Korea. Arch Virol. 2017;162(1):33–44.")\], but this period was found to be slightly longer in South Korea \[[3](#ref-CR3 "Ki M. 2015 MERS outbreak in Korea: hospital-to-hospital transmission. Epidemiol Health. 2015;
https://doi.org/10.4178/epih/e2015033
."),[4](#ref-CR4 "Korea Centers for Disease Control & Prevention. Middle East respiratory syndrome coronavirus outbreak in the Republic of Korea, 2015. Osong Public Health Res Perspect. 2015;6(4):269–78."),[5](/articles/10.1186/s12889-018-5484-8#ref-CR5 "Cho SY, Kang JM, Ha YE, Park GE, Lee JY, Ko JH, et al. MERS-CoV outbreak following a single patient exposure in an emergency room in South Korea: an epidemiological outbreak study. Lancet. 2016;388(10048):994–1001."), [23](#ref-CR23 "Park JW, Lee KJ, Lee KH, Lee SH, Cho JR, Mo JW, et al. Hospital outbreaks of Middle East respiratory syndrome, Daejeon, South Korea, 2015. Emerg Infect Dis. 2017;23(6):898–905."),[24](#ref-CR24 "Park SH, Kim YS, Jung Y, Choi SY, Cho NH, Jeong HW, et al. Outbreaks of Middle East respiratory syndrome in two hospitals initiated by a single patient in Daejeon, South Korea. Infect Chemother. 2016;48(2):99–107."),[25](#ref-CR25 "Virlogeux V, Park M, Wu JT, Cowling BJ. Association between severity of MERS-CoV infection and incubation period. Emerg Infect Dis. 2016;22(3):526–8."),[26](#ref-CR26 "Cowling BJ, Park M, Fang VJ, Wu P, Leung GM, Wu JT. Preliminary epidemiological assessment of MERS-CoV outbreak in South Korea, May to June 2015. Euro Surveill. 2015;20(25):7–13."),[27](#ref-CR27 "Ministry of Health and Welfare, Republic of Korea. MERS white book. 2016.
http://www.cdc.go.kr/CDC/intro/CdcKrIntro0101.jsp?menuIds=HOME001-MNU1154-MNU0005-MNU0010&cid=70039
. Accessed 10 Oct 2017."),[28](/articles/10.1186/s12889-018-5484-8#ref-CR28 "Park HY, Lee EJ, Ryu YW, Kim Y, Kim H, Lee H, et al. Epidemiological investigation of MERS-CoV spread in a single hospital in South Korea, May to June 2015. Euro Surveill. 2015;20(25):1–6.")\].The severity of MERS also differed between the Middle East area and South Korea. Mortality of MERS patients was found to be 20.4% in South Korea based on a report including all cases [[27](/articles/10.1186/s12889-018-5484-8#ref-CR27 "Ministry of Health and Welfare, Republic of Korea. MERS white book. 2016. http://www.cdc.go.kr/CDC/intro/CdcKrIntro0101.jsp?menuIds=HOME001-MNU1154-MNU0005-MNU0010&cid=70039
. Accessed 10 Oct 2017.")\], but most studies from Saudi Arabia reported higher rates, from 22 to 69.2% \[[7](/articles/10.1186/s12889-018-5484-8#ref-CR7 "Assiri A, Al-Tawfiq JA, Al-Rabeeah AA, Al-Rabiah FA, Al-Hajjar S, Al-Barrak A, et al. Epidemiological, demographic, and clinical characteristics of 47 cases of Middle East respiratory syndrome coronavirus disease from Saudi Arabia: a descriptive study. Lancet Infect Dis. 2013;13(9):752–61."), [22](/articles/10.1186/s12889-018-5484-8#ref-CR22 "Drosten C, Meyer B, Muller MA, Corman VM, Al-Masri M, Hossain R, et al. Transmission of MERS-coronavirus in household contacts. N Engl J Med. 2014;371(9):828–35."), [33](/articles/10.1186/s12889-018-5484-8#ref-CR33 "Halim AA, Alsayed B, Embarak S, Yaseen T, Dabbous S. Clinical characteristics and outcome of ICU admitted MERS corona virus infected patients. Egypt J Chest Dis Tuberc. 2016;65(1):81–7."), [37](#ref-CR37 "Noorwali AA, Turkistani AM, Asiri SI, Trabulsi FA, Alwafi OM, Alzahrani SH, et al. Descriptive epidemiology and characteristics of confirmed cases of Middle East respiratory syndrome coronavirus infection in the Makkah Region of Saudi Arabia, March to June 2014. Ann Saudi Med. 2015;35(3):203–9."),[38](#ref-CR38 "Oboho IK, Tomczyk SM, Al-Asmari AM, Banjar AA, Al-Mugti H, Aloraini MS, et al. 2014 MERS-CoV outbreak in Jeddah--a link to health care facilities. N Engl J Med. 2015;372(9):846–54."),[39](/articles/10.1186/s12889-018-5484-8#ref-CR39 "Lessler J, Salje H, Van Kerkhove MD, Ferguson NM, Cauchemez S, Rodriquez-Barraquer I, et al. Estimating the severity and subclinical burden of Middle East respiratory syndrome coronavirus infection in the Kingdom of Saudi Arabia. Am J Epidemiol. 2016;183(7):657–63.")\]. Days from onset to confirmation were similar, 4–8 days in the Middle East area \[[29](/articles/10.1186/s12889-018-5484-8#ref-CR29 "Sha J, Li Y, Chen X, Hu Y, Ren Y, Geng X, et al. Fatality risks for nosocomial outbreaks of Middle East respiratory syndrome coronavirus in the Middle East and South Korea. Arch Virol. 2017;162(1):33–44."), [31](/articles/10.1186/s12889-018-5484-8#ref-CR31 "Ahmed AE. Diagnostic delays in 537 symptomatic cases of Middle East respiratory syndrome coronavirus infection in Saudi Arabia. Int J Infect Dis. 2017;62:47–51.")\] and 4–6.5 days in South Korea \[[3](/articles/10.1186/s12889-018-5484-8#ref-CR3 "Ki M. 2015 MERS outbreak in Korea: hospital-to-hospital transmission. Epidemiol Health. 2015;
https://doi.org/10.4178/epih/e2015033
."), [28](/articles/10.1186/s12889-018-5484-8#ref-CR28 "Park HY, Lee EJ, Ryu YW, Kim Y, Kim H, Lee H, et al. Epidemiological investigation of MERS-CoV spread in a single hospital in South Korea, May to June 2015. Euro Surveill. 2015;20(25):1–6."), [29](/articles/10.1186/s12889-018-5484-8#ref-CR29 "Sha J, Li Y, Chen X, Hu Y, Ren Y, Geng X, et al. Fatality risks for nosocomial outbreaks of Middle East respiratory syndrome coronavirus in the Middle East and South Korea. Arch Virol. 2017;162(1):33–44.")\]. Days from onset to discharge were slightly longer in South Korea, 14–17 days in the Middle East area \[[29](/articles/10.1186/s12889-018-5484-8#ref-CR29 "Sha J, Li Y, Chen X, Hu Y, Ren Y, Geng X, et al. Fatality risks for nosocomial outbreaks of Middle East respiratory syndrome coronavirus in the Middle East and South Korea. Arch Virol. 2017;162(1):33–44."), [36](/articles/10.1186/s12889-018-5484-8#ref-CR36 "Assiri A, Abedi GR, Bin Saeed AA, Abdalla MA, al-Masry M, Choudhry AJ, et al. Multifacility outbreak of Middle East respiratory syndrome in Taif, Saudi Arabia. Emerg Infect Dis. 2016;22(1):32–40.")\] and 17–20 days in South Korea \[[3](/articles/10.1186/s12889-018-5484-8#ref-CR3 "Ki M. 2015 MERS outbreak in Korea: hospital-to-hospital transmission. Epidemiol Health. 2015;
https://doi.org/10.4178/epih/e2015033
."), [29](/articles/10.1186/s12889-018-5484-8#ref-CR29 "Sha J, Li Y, Chen X, Hu Y, Ren Y, Geng X, et al. Fatality risks for nosocomial outbreaks of Middle East respiratory syndrome coronavirus in the Middle East and South Korea. Arch Virol. 2017;162(1):33–44.")\] (Table [3](/articles/10.1186/s12889-018-5484-8#Tab3)).Table 3 Epidemiologic index of MERS between the Middle East area and South Korea
Discussion
The transmissibility and severity of MERS were different by outbreak countries, especially between the Middle East area and South Korea. The virus, host, and environmental factors may be the causes of the MERS outbreak-related differences between the two regions. From the standpoint of viral factors, there was a mutation of the MERS coronavirus (MERS-CoV) in the South Korea outbreak. Kim et al. [60] reported a point mutation in the receptor-binding domain of the viral spike protein in MERS-CoV, and another study showed that MERS-CoV in South Korea had higher genetic variability and mutation rates [61]. Individual characteristics can also affect MERS transmission. As previous studies showed, there is an association between older age and MERS infection [43], severity [48], and mortality [4, 50], and the population structure may be related to transmission and severity. Additionally, individuals aware of MERS were found to be more likely to practice preventive behaviour [[62](/articles/10.1186/s12889-018-5484-8#ref-CR62 "Alqahtani AS, Wiley KE, Mushta SM, Yamazaki K, BinDhim NF, Heywood AE, et al. Association between Australian Hajj Pilgrims' awareness of MERS-CoV, and their compliance with preventive measures and exposure to camels. J Travel Med. 2016;23(5). https://doi.org/10.1093/jtm/taw046
.")\], which differed by demographic characteristics \[[63](/articles/10.1186/s12889-018-5484-8#ref-CR63 "Choi J-S, Kim J-S. Factors influencing preventive behavior against Middle East respiratory syndrome-coronavirus among nursing students in South Korea. Nurse Educ Today. 2016;40:168–72."), [64](/articles/10.1186/s12889-018-5484-8#ref-CR64 "Kim JS, Choi JS. Middle East respiratory syndrome-related knowledge, preventive behaviours and risk perception among nursing students during outbreak. J Clin Nurs. 2016;25(17–18):2542–9.")\]. The transmission environment may also contribute to the difference. While many MERS cases were contracted through exposure to camels in Saudi Arabia \[[42](/articles/10.1186/s12889-018-5484-8#ref-CR42 "Alraddadi BM, Watson JT, Almarashi A, Abedi GR, Turkistani A, Sadran M, et al. Risk factors for primary Middle East respiratory syndrome coronavirus illness in humans, Saudi Arabia, 2014. Emerg Infect Dis. 2016;22(1):49–55.")\], the South Korea outbreak involved multiple generations of secondary infections caused by intra-hospital and hospital-to-hospital transmission \[[3](/articles/10.1186/s12889-018-5484-8#ref-CR3 "Ki M. 2015 MERS outbreak in Korea: hospital-to-hospital transmission. Epidemiol Health. 2015;
https://doi.org/10.4178/epih/e2015033
."), [65](/articles/10.1186/s12889-018-5484-8#ref-CR65 "Lee SS, Wong NS. Probable transmission chains of Middle East respiratory syndrome coronavirus and the multiple generations of secondary infection in South Korea. Int J Infect Dis. 2015;38:65–7.")\]. Strategies considering various factors are therefore needed to assess the impact of MERS and to better control its spread.Although several studies have reported the overall R value [9, 10, 14, 19], others have shown that this value this can be variable based on the generation or a control intervention [11, 16, 19]. Especially in the South Korea epidemic, the R value was particularly high in the early stage or first generation, at 4.42–5.4, though it later decreased to 0.14–0.39 [16, 19]. Further studies should consider and analyse the variation of the R value depending on the period or control intervention.
While earlier studies on infectious diseases assumed a homogeneous infection ability of a population, recent studies have shown the existence of so-called super spreaders, individuals with a high potential to infect others in many infectious diseases, including Ebola and severe acute respiratory syndrome (SARS) [66]. The role of the super spreader is also important in the spread of MERS. In South Korea, 83.2% of MERS patients were associated with five super-spreading events [[27](/articles/10.1186/s12889-018-5484-8#ref-CR27 "Ministry of Health and Welfare, Republic of Korea. MERS white book. 2016. http://www.cdc.go.kr/CDC/intro/CdcKrIntro0101.jsp?menuIds=HOME001-MNU1154-MNU0005-MNU0010&cid=70039
. Accessed 10 Oct 2017.")\]. Stein et al. \[[67](/articles/10.1186/s12889-018-5484-8#ref-CR67 "Stein RA. Super-spreaders in infectious diseases. Int J Infect Dis. 2011;15(8):e510–3.")\] asserted that super spreaders were related with the host, pathogen, and environmental factors, and Wong et al. \[[66](/articles/10.1186/s12889-018-5484-8#ref-CR66 "Wong G, Liu W, Liu Y, Zhou B, Bi Y, Gao GF. MERS, SARS, and Ebola: the role of super-spreaders in infectious disease. Cell Host Microbe. 2015;18(4):398–401.")\] reported that individual behaviours could also contribute to disease spread.There are variations in the mortality and attack rates among studies using South Korea data. For example, Park et al. [24] reported a 47.8% MERS mortality, while reports from the Korean Ministry of Health and Welfare showed 20.4% MERS mortality. This disparity may, in part, be due to small sample sizes. Park et al. [24] included only 23 patients because the study was conducted in an early phase of a MERS outbreak. We excluded studies that included cases with < 20 subjects, which were mostly case series, to reduce those types of biases.
The present review found that older age and concomitant disease were risk factors of MERS infection and mortality. These results are consistent with a recent systematic review that reported older age, male, and an underlying medical condition as predictors of death related to MERS [68]; therefore, these factors should be prioritized in protection and treatment procedures.
One limitation of this study was the possibility of subject duplication. Especially in South Korea, the Korean government publishes MERS reports that include all patients. The epidemiologic index in other studies might be biased since they included partial Korean patients and were analysed in the middle of an outbreak. However, we included those studies because they showed the characteristics of MERS in different situations and different stages.
We did not conduct a meta-analysis because of the small number of studies for each index, which might be another limitation of this study. Although this study reviewed the risk factors of MERS and their impact, assessing the effect size of each risk factor is important. More studies investigating the effect of risk factors on MERS need to be constantly conducted.
Conclusion
Most studies on the transmissibility and severity of MERS have originated from Saudi Arabia and South Korea. Even though the R0 value in South Korea was higher than that in Saudi Arabia, mortality was higher in Saudi Arabia. The most common factors behind MERS infection and mortality were older age and concomitant disease. Future studies should consider the risk of MERS based on the outbreak region and patient characteristics. The results of the present study are valuable for informing further studies and health policy in preparation for MERS outbreaks.
Abbreviations
CD4:
Cluster of differentiation 4
CFR:
Case fatality rate
MERS:
Middle East respiratory syndrome
PRNT:
Plaque reduction neutralization test
SARS:
Severe acute respiratory syndrome
References
- Zaki AM, van Boheemen S, Bestebroer TM, Osterhaus AD, Fouchier RA. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Engl J Med. 2012;367(19):1814–20.
Article CAS PubMed Google Scholar - World Health Organization; WHO MERS-CoV global summary and risk assessment. 2016. http://www.who.int/emergencies/mers-cov/mers-summary-2016.pdf?ua=1&ua=1. Accessed 20 Oct 2017.
Google Scholar - Ki M. 2015 MERS outbreak in Korea: hospital-to-hospital transmission. Epidemiol Health. 2015; https://doi.org/10.4178/epih/e2015033.
- Korea Centers for Disease Control & Prevention. Middle East respiratory syndrome coronavirus outbreak in the Republic of Korea, 2015. Osong Public Health Res Perspect. 2015;6(4):269–78.
Article Google Scholar - Cho SY, Kang JM, Ha YE, Park GE, Lee JY, Ko JH, et al. MERS-CoV outbreak following a single patient exposure in an emergency room in South Korea: an epidemiological outbreak study. Lancet. 2016;388(10048):994–1001.
Article PubMed Google Scholar - Cauchemez S, Fraser C, Van Kerkhove MD, Donnelly CA, Riley S, Rambaut A, et al. Middle East respiratory syndrome coronavirus: quantification of the extent of the epidemic, surveillance biases, and transmissibility. Lancet Infect Dis. 2014;14(1):50–6.
Article PubMed PubMed Central Google Scholar - Assiri A, Al-Tawfiq JA, Al-Rabeeah AA, Al-Rabiah FA, Al-Hajjar S, Al-Barrak A, et al. Epidemiological, demographic, and clinical characteristics of 47 cases of Middle East respiratory syndrome coronavirus disease from Saudi Arabia: a descriptive study. Lancet Infect Dis. 2013;13(9):752–61.
Article PubMed Google Scholar - Chowell G, Abdirizak F, Lee S, Lee J, Jung E, Nishiura H, et al. Transmission characteristics of MERS and SARS in the healthcare setting: a comparative study. BMC Med. 2015;13:210.
Article PubMed PubMed Central Google Scholar - Breban R, Riou J, Fontanet A. Interhuman transmissibility of Middle East respiratory syndrome coronavirus: estimation of pandemic risk. Lancet. 2013;382(9893):694–9.
Article PubMed Google Scholar - Kucharski AJ, Althaus CL. The role of superspreading in Middle East respiratory syndrome coronavirus (MERS-CoV) transmission. Euro Surveill. 2015;20(25):14–8.
Article CAS PubMed Google Scholar - Chowell G, Blumberg S, Simonsen L, Miller MA, Viboud C. Synthesizing data and models for the spread of MERS-CoV, 2013: key role of index cases and hospital transmission. Epidemics. 2014;9:40–51.
Article PubMed Google Scholar - Alenazi TH, Al Arbash H, El-Saed A, Alshamrani MM, Baffoe-Bonnie H, Arabi YM, et al. Identified transmission dynamics of Middle East respiratory syndrome coronavirus infection during an outbreak: implications of an overcrowded emergency department. Clin Infect Dis. 2017;65(4):675–9.
Article PubMed Google Scholar - Eifan SA, Nour I, Hanif A, Zamzam AMM, AlJohani SM. A pandemic risk assessment of Middle East respiratory syndrome coronavirus (MERS-CoV) in Saudi Arabia. Saudi J Biol Sci. 2017;24(7):1631–8.
Article PubMed PubMed Central Google Scholar - Poletto C, Pelat C, Levy-Bruhl D, Yazdanpanah Y, Boelle PY, Colizza V. Assessment of the Middle East respiratory syndrome coronavirus (MERS-CoV) epidemic in the Middle East and risk of international spread using a novel maximum likelihood analysis approach. Euro Surveill. 2014;19(23)
- Choi S, Jung E, Choi BY, Hur YJ, Ki M. High reproduction number of Middle East respiratory syndrome coronavirus in nosocomial outbreaks: mathematical modelling in Saudi Arabia and South Korea. J Hosp Infect. 2017; https://doi.org/10.1016/j.jhin.2017.09.017.
- Kim Y, Lee S, Chu C, Choe S, Hong S, Shin Y. The characteristics of middle eastern respiratory syndrome coronavirus transmission dynamics in South Korea. Osong Public Health Res Perspect. 2016;7(1):49–55.
Article PubMed PubMed Central Google Scholar - Zhang XS, Pebody R, Charlett A, de Angelis D, Birrell P, Kang H, et al. Estimating and modelling the transmissibility of Middle East respiratory syndrome CoronaVirus during the 2015 outbreak in the Republic of Korea. Influenza Other Respir Viruses. 2017;11(5):434–44.
Article PubMed PubMed Central Google Scholar - Chang HJ. Estimation of basic reproduction number of the Middle East respiratory syndrome coronavirus (MERS-CoV) during the outbreak in South Korea, 2015. Biomed Eng Online. 2017;16(1):79.
Article PubMed PubMed Central Google Scholar - Xia ZQ, Zhang J, Xue YK, Sun GQ, Jin Z. Modeling the transmission of Middle East respirator syndrome corona virus in the Republic of Korea. PLoS One. 2015;10(12):e0144778.
Article PubMed PubMed Central Google Scholar - Kim CJ, Choi WS, Jung Y, Kiem S, Seol HY, Woo HJ, et al. Surveillance of the Middle East respiratory syndrome (MERS) coronavirus (CoV) infection in healthcare workers after contact with confirmed MERS patients: incidence and risk factors of MERS-CoV seropositivity. Biomed Res Int. 2016;22(10):880–6.
Google Scholar - El Bushra HE, Al Arbash HA, Mohammed M, Abdalla O, Abdallah MN, Al-Mayahi ZK, et al. Outcome of strict implementation of infection prevention control measures during an outbreak of Middle East respiratory syndrome. Am J Infect Control. 2017;45(5):502–7.
Article PubMed Google Scholar - Drosten C, Meyer B, Muller MA, Corman VM, Al-Masri M, Hossain R, et al. Transmission of MERS-coronavirus in household contacts. N Engl J Med. 2014;371(9):828–35.
Article PubMed Google Scholar - Park JW, Lee KJ, Lee KH, Lee SH, Cho JR, Mo JW, et al. Hospital outbreaks of Middle East respiratory syndrome, Daejeon, South Korea, 2015. Emerg Infect Dis. 2017;23(6):898–905.
Article PubMed PubMed Central Google Scholar - Park SH, Kim YS, Jung Y, Choi SY, Cho NH, Jeong HW, et al. Outbreaks of Middle East respiratory syndrome in two hospitals initiated by a single patient in Daejeon, South Korea. Infect Chemother. 2016;48(2):99–107.
Article CAS PubMed PubMed Central Google Scholar - Virlogeux V, Park M, Wu JT, Cowling BJ. Association between severity of MERS-CoV infection and incubation period. Emerg Infect Dis. 2016;22(3):526–8.
Article CAS PubMed PubMed Central Google Scholar - Cowling BJ, Park M, Fang VJ, Wu P, Leung GM, Wu JT. Preliminary epidemiological assessment of MERS-CoV outbreak in South Korea, May to June 2015. Euro Surveill. 2015;20(25):7–13.
Article CAS PubMed Google Scholar - Ministry of Health and Welfare, Republic of Korea. MERS white book. 2016. http://www.cdc.go.kr/CDC/intro/CdcKrIntro0101.jsp?menuIds=HOME001-MNU1154-MNU0005-MNU0010&cid=70039. Accessed 10 Oct 2017.
Google Scholar - Park HY, Lee EJ, Ryu YW, Kim Y, Kim H, Lee H, et al. Epidemiological investigation of MERS-CoV spread in a single hospital in South Korea, May to June 2015. Euro Surveill. 2015;20(25):1–6.
Article CAS PubMed Google Scholar - Sha J, Li Y, Chen X, Hu Y, Ren Y, Geng X, et al. Fatality risks for nosocomial outbreaks of Middle East respiratory syndrome coronavirus in the Middle East and South Korea. Arch Virol. 2017;162(1):33–44.
Article CAS PubMed Google Scholar - Liu M, Jiang C, Donovan C, Wen Y, Sun W. Middle East respiratory syndrome and medical students: letter from China. Int J Environ Res Public Health. 2015;12(10):13289–94.
Article PubMed PubMed Central Google Scholar - Ahmed AE. Diagnostic delays in 537 symptomatic cases of Middle East respiratory syndrome coronavirus infection in Saudi Arabia. Int J Infect Dis. 2017;62:47–51.
Article PubMed Google Scholar - Sherbini N, Iskandrani A, Kharaba A, Khalid G, Abduljawad M, Al-Jahdali H. Middle East respiratory syndrome coronavirus in Al-Madinah City, Saudi Arabia: demographic, clinical and survival data. J Epidemiolo Glob Health. 2017;7(1):29–36.
Article Google Scholar - Halim AA, Alsayed B, Embarak S, Yaseen T, Dabbous S. Clinical characteristics and outcome of ICU admitted MERS corona virus infected patients. Egypt J Chest Dis Tuberc. 2016;65(1):81–7.
Article Google Scholar - Kim SW, Park JW, Jung HD, Yang JS, Park YS, Lee C, et al. Risk factors for transmission of Middle East respiratory syndrome coronavirus infection during the 2015 outbreak in South Korea. Clin Infect Dis. 2017;64(5):551–7.
PubMed Google Scholar - Mizumoto K, Saitoh M, Chowell G, Miyamatsu Y, Nishiura H. Estimating the risk of Middle East respiratory syndrome (MERS) death during the course of the outbreak in the Republic of Korea, 2015. Int J Infect Dis. 2015;39:7–9.
Article PubMed Google Scholar - Assiri A, Abedi GR, Bin Saeed AA, Abdalla MA, al-Masry M, Choudhry AJ, et al. Multifacility outbreak of Middle East respiratory syndrome in Taif, Saudi Arabia. Emerg Infect Dis. 2016;22(1):32–40.
Article CAS PubMed PubMed Central Google Scholar - Noorwali AA, Turkistani AM, Asiri SI, Trabulsi FA, Alwafi OM, Alzahrani SH, et al. Descriptive epidemiology and characteristics of confirmed cases of Middle East respiratory syndrome coronavirus infection in the Makkah Region of Saudi Arabia, March to June 2014. Ann Saudi Med. 2015;35(3):203–9.
Article PubMed Google Scholar - Oboho IK, Tomczyk SM, Al-Asmari AM, Banjar AA, Al-Mugti H, Aloraini MS, et al. 2014 MERS-CoV outbreak in Jeddah--a link to health care facilities. N Engl J Med. 2015;372(9):846–54.
Article CAS PubMed PubMed Central Google Scholar - Lessler J, Salje H, Van Kerkhove MD, Ferguson NM, Cauchemez S, Rodriquez-Barraquer I, et al. Estimating the severity and subclinical burden of Middle East respiratory syndrome coronavirus infection in the Kingdom of Saudi Arabia. Am J Epidemiol. 2016;183(7):657–63.
Article PubMed PubMed Central Google Scholar - Mohd HA, Memish ZA, Alfaraj SH, McClish D, Altuwaijri T, Alanazi MS, et al. Predictors of MERS-CoV infection: a large case control study of patients presenting with ILI at a MERS-CoV referral hospital in Saudi Arabia. Travel Med Infect Dis. 2016;14(5):464–70.
Article PubMed Google Scholar - Penttinen PM, Kaasik-Aaslav K, Friaux A, Donachie A, Sudre B, Amato-Gauci AJ, et al. Taking stock of the first 133 MERS coronavirus cases globally--is the epidemic changing? Euro Surveill. 2013;18(39)
- Alraddadi BM, Watson JT, Almarashi A, Abedi GR, Turkistani A, Sadran M, et al. Risk factors for primary Middle East respiratory syndrome coronavirus illness in humans, Saudi Arabia, 2014. Emerg Infect Dis. 2016;22(1):49–55.
Article CAS PubMed PubMed Central Google Scholar - Hastings DL, Tokars JI, Abdel Aziz IZ, Alkhaldi KZ, Bensadek AT, Alraddadi BM, et al. Outbreak of Middle East respiratory syndrome at tertiary care hospital, Jeddah, Saudi Arabia, 2014. Emerg Infect Dis. 2016;22(5):794–801.
Article PubMed PubMed Central Google Scholar - Kang CK, Song KH, Choe PG, Park WB, Bang JH, Kim ES, et al. Clinical and epidemiologic characteristics of spreaders of Middle East respiratory syndrome coronavirus during the 2015 outbreak in Korea. J Korean Med Sci. 2017;32(5):744–9.
Article PubMed PubMed Central Google Scholar - Majumder MS, Brownstein JS, Finkelstein SN, Larson RC, Bourouiba L. Nosocomial amplification of MERS-coronavirus in South Korea, 2015. Trans R Soc Trop Med Hyg. 2017;111(6):261–9.
Article PubMed Google Scholar - Zhao J, Alshukairi AN, Baharoon SA, Ahmed WA, Bokhari AA, Nehdi AM, et al. Recovery from the Middle East respiratory syndrome is associated with antibody and T-cell responses. Sci Immunol. 2017;2(14).
- Feikin DR, Alraddadi B, Qutub M, Shabouni O, Curns A, Oboho IK, et al. Association of higher MERS-CoV virus load with severe disease and death, Saudi Arabia, 2014. Emerg Infect Dis. 2015;21(11):2029–35.
Article CAS PubMed PubMed Central Google Scholar - Ko J-H, Park GE, Lee JY, Lee JY, Cho SY, Ha YE, et al. Predictive factors for pneumonia development and progression to respiratory failure in MERS-CoV infected patients. J Inf Secur. 2016;73(5):468–75.
Google Scholar - Saad M, Omrani AS, Baig K, Bahloul A, Elzein F, Matin MA, et al. Clinical aspects and outcomes of 70 patients with Middle East respiratory syndrome coronavirus infection: a single-center experience in Saudi Arabia. Int J Infect Dis. 2014;29:301–6.
Article PubMed Google Scholar - Adegboye OA, Gayawan E, Hanna F. Spatial modelling of contribution of individual level risk factors for mortality from Middle East respiratory syndrome coronavirus in the Arabian Peninsula. PLoS One. 2017;12(7):e0181215.
Article PubMed PubMed Central Google Scholar - Ahmed AE. The predictors of 3- and 30-day mortality in 660 MERS-CoV patients. BMC Infect Dis. 2017;17(1):615.
Article PubMed PubMed Central Google Scholar - Yang YM, Hsu CY, Lai CC, Yen MF, Wikramaratna PS, Chen HH, et al. Impact of comorbidity on fatality rate of patients with Middle East respiratory syndrome. Sci Rep. 2017;7(1):11307.
Article PubMed PubMed Central Google Scholar - Alsahafi AJ, Cheng AC. The epidemiology of Middle East respiratory syndrome coronavirus in the Kingdom of Saudi Arabia, 2012-2015. Int J Infect Dis. 2016;45:1–4.
Article PubMed Google Scholar - Majumder MS, Kluberg SA, Mekaru SR, Brownstein JS. Mortality risk factors for Middle East respiratory syndrome outbreak, South Korea, 2015. Emerg Infect Dis. 2015;21(11):2088–90.
Article PubMed PubMed Central Google Scholar - Choi WS, Kang CI, Kim Y, Choi JP, Joh JS, Shin HS, et al. Clinical presentation and outcomes of Middle East respiratory syndrome in the Republic of Korea. Infect Chemother. 2016;48(2):118–26.
Article CAS PubMed PubMed Central Google Scholar - Nam H-S, Park JW, Ki M, Yeon M-Y, Kim J, Kim SW. High fatality rates and associated factors in two hospital outbreaks of MERS in Daejeon, the Republic of Korea. Int J Infect Dis. 2017;58:37–42.
Article PubMed Google Scholar - Almekhlafi GA, Albarrak MM, Mandourah Y, Hassan S, Alwan A, Abudayah A, et al. Presentation and outcome of Middle East respiratory syndrome in Saudi intensive care unit patients. Crit Care. 2016;20(1):123.
Article PubMed PubMed Central Google Scholar - Das KM, Lee EY, Al Jawder SE, Enani MA, Singh R, Skakni L, et al. Acute Middle East respiratory syndrome coronavirus: temporal lung changes observed on the chest radiographs of 55 patients. AJR Am J Roentgenol. 2015;205(3):W267–74.
Article PubMed Google Scholar - Al Ghamdi M, Alghamdi KM, Ghandoora Y, Alzahrani A, Salah F, Alsulami A, et al. Treatment outcomes for patients with Middle Eastern Respiratory Syndrome Coronavirus (MERS CoV) infection at a coronavirus referral center in the Kingdom of Saudi Arabia. BMC Infect Dis. 2016;16:174.
Article PubMed PubMed Central Google Scholar - Kim Y, Cheon S, Min CK, Sohn KM, Kang YJ, Cha YJ, et al. Spread of mutant Middle East respiratory syndrome coronavirus with reduced affinity to human CD26 during the South Korean outbreak. MBio. 2016;7(2):e00019.
Article CAS PubMed PubMed Central Google Scholar - Kim DW, Kim YJ, Park SH, Yun MR, Yang JS, Kang HJ, et al. Variations in spike glycoprotein gene of MERS-CoV, South Korea, 2015. Emerg Infect Dis. 2016;22(1):100–4.
Article CAS PubMed PubMed Central Google Scholar - Alqahtani AS, Wiley KE, Mushta SM, Yamazaki K, BinDhim NF, Heywood AE, et al. Association between Australian Hajj Pilgrims' awareness of MERS-CoV, and their compliance with preventive measures and exposure to camels. J Travel Med. 2016;23(5). https://doi.org/10.1093/jtm/taw046.
- Choi J-S, Kim J-S. Factors influencing preventive behavior against Middle East respiratory syndrome-coronavirus among nursing students in South Korea. Nurse Educ Today. 2016;40:168–72.
Article PubMed Google Scholar - Kim JS, Choi JS. Middle East respiratory syndrome-related knowledge, preventive behaviours and risk perception among nursing students during outbreak. J Clin Nurs. 2016;25(17–18):2542–9.
Article PubMed Google Scholar - Lee SS, Wong NS. Probable transmission chains of Middle East respiratory syndrome coronavirus and the multiple generations of secondary infection in South Korea. Int J Infect Dis. 2015;38:65–7.
Article PubMed Google Scholar - Wong G, Liu W, Liu Y, Zhou B, Bi Y, Gao GF. MERS, SARS, and Ebola: the role of super-spreaders in infectious disease. Cell Host Microbe. 2015;18(4):398–401.
Article CAS PubMed Google Scholar - Stein RA. Super-spreaders in infectious diseases. Int J Infect Dis. 2011;15(8):e510–3.
Article PubMed Google Scholar - Matsuyama R, Nishiura H, Kutsuna S, Hayakawa K, Ohmagari N. Clinical determinants of the severity of Middle East respiratory syndrome (MERS): a systematic review and meta-analysis. BMC Public Health. 2016;16(1):1203.
Article PubMed PubMed Central Google Scholar
Funding
This work was supported by the National Research Council of Science & Technology (NST) grant by the Korea government (MSIP) (No. CRC-16-01-KRICT) and Korea Institute of Oriental Medicine (G17273).
Author information
Authors and Affiliations
- Research Center for Korean Medicine Policy, Korea Institute of Oriental Medicine, Daejeon, Republic of Korea
Ji-Eun Park - Clinical Research Division, Korea Institute of Oriental Medicine, Daejeon, Republic of Korea
Soyoung Jung & Aeran Kim - Herbal Medicine Research Division, Korea Institute of Oriental Medicine, Daejeon, Republic of Korea
Ji-Eun Park - Center for Convergent Research of Emerging Virus Infection, Korea Research Institute of Chemical Technology, Daejeon, Republic of Korea
Ji-Eun Park
Authors
- Ji-Eun Park
You can also search for this author inPubMed Google Scholar - Soyoung Jung
You can also search for this author inPubMed Google Scholar - Aeran Kim
You can also search for this author inPubMed Google Scholar - Ji-Eun Park
You can also search for this author inPubMed Google Scholar
Contributions
JEP (corresponding author) designed the study, and conducted the data search and the analysis with JEP (1st author). SYJ and ARK participated in the data review. JEP (corresponding) drafted the manuscript, and JEP (1st), SYJ, and ARK revised it. All authors read and approved the final manuscript.
Corresponding author
Correspondence toJi-Eun Park.
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Park, JE., Jung, S., Kim, A. et al. MERS transmission and risk factors: a systematic review.BMC Public Health 18, 574 (2018). https://doi.org/10.1186/s12889-018-5484-8
- Received: 21 November 2017
- Accepted: 19 April 2018
- Published: 02 May 2018
- DOI: https://doi.org/10.1186/s12889-018-5484-8