Eosinophilic Fasciitis: Practice Essentials, Pathophysiology, Etiology (original) (raw)
Practice Essentials
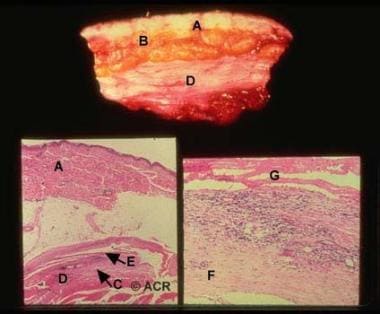
Eosinophilic fasciitis (EF), also called Shulman syndrome, is a rare, localized fibrosing disorder of the fascia. [1] (See image below.) The etiology and pathophysiology are unclear.
Eosinophilic fasciitis. Top: In this gross specimen, the dermis (A), subcutaneous adipose tissue (B), and skeletal muscle do not appear unusual. However, the fascia (D) is markedly thickened. Bottom left: The gross findings are recapitulated in this low-power photomicrograph. The epidermis, dermis (A), and subcutaneous adipose tissue are not remarkable in this case. The fascia (D) is markedly thickened and focally infiltrated by inflammatory cells (E). The small amount of skeletal muscle (C) appears normal (hematoxylin and eosin stain at low power). Bottom right: A close-up photograph of a portion of the fascia showing mostly edematous cellular connective tissue (F). It is focally infiltrated by inflammatory cells, including lymphocytes, plasma cells, and histiocytes. The more intensely stained hypocellular pink bands across the top of the field (G) are part of an interstitial exudate of fibrin (hematoxylin and eosin stain at medium power).
In 1974, Shulman provided an early description of a disorder characterized by peripheral eosinophilia and fasciitis that could be differentiated from scleroderma by the distinctive pattern of skin involvement that spares the digits, involves fascia rather than dermis, and is not accompanied by Raynaud phenomenon. [2] In 1975, Rodnan et al proposed the term eosinophilic fasciitis for the disorder. [3] Eosinophilic fasciitis is relatively rare, with only about 300 cases reported; the literature consists of a relatively few large case series and multiple case reports. Therefore, the understanding of key aspects of the disease continues to evolve. [1]
The etiology of eosinophilic fasciitis remains unknown, although many possible triggers (in particular, sustained intense physical exercise) and disease associations have been suggested. Some aspects of pathophysiology have been elucidated; however, a more complete understanding has yet to develop.
The available literature has generated a broader clinical image of the condition, but fascial thickening in the setting of eosinophilia, elevated erythrocyte sedimentation rate, and hypergammaglobulinemia remain critical elements of the syndrome. Visceral involvement in eosinophilic fasciitis is generally absent, a finding that helps differentiate eosinophilic fasciitis from systemic sclerosis and other differential considerations. However, an association with several hematologic diseases is recognized and frequently carries a grave prognosis.
The diagnosis of eosinophilic fasciitis is suspected in a patient presenting with characteristic skin changes and consistent laboratory findings. It is confirmed with full-thickness biopsy or characteristic MRI findings. See Presentation and Workup.
Eosinophilic fasciitis is generally corticosteroid-responsive, and initial treatment regimens are based on this therapy. Multiple additional agents have been used in steroid-refractory disease. The evidence for many of these agents is anecdotal, and there is no general consensus regarding the best agent for treatment of steroid-resistant disease or cases refractory to steroid withdrawal. See Treatment and Medication.

Pathophysiology
Although the etiology of eosinophilic fasciitis is unknown, studies have shed light on some of the mechanisms involved in its pathogenesis.
In general, the pathophysiology underlying eosinophilic fasciitis is postulated to involve an inflammatory response resulting in an activated inflammatory cell infiltrate of affected tissues and subsequent dysregulation of extracellular matrix production by lesional fibroblasts.
Viallard et al demonstrated that, when stimulated, peripheral blood mononuclear cells of eosinophilic fasciitis patients produce significantly higher amounts of five cytokines, including interleukin (IL)–5 and interferon (IFN)–gamma. [4] IL-5 is known to activate mature eosinophils and to stimulate eosinophil chemotaxis, growth, and differentiation. IFN-gamma activates tissue macrophages and T cells. The findings of Dziadzio et al support increased levels of IL-5 in eosinophilic fasciitis, in addition to increased levels of transforming growth factor (TGF)–beta, another fibrogenic cytokine. [5]
Toquet et al investigated the phenotype of the lesional inflammatory cell infiltrate in patients with eosinophilic fasciitis and demonstrated a predominance of macrophages, CD8+ lymphocytes, and few eosinophils. [6] Pathologic specimens from patients with eosinophilic fasciitis demonstrate increased numbers of eosinophils, especially early in the disease course.
Taken together, the findings of these studies suggest a mechanistic framework marked by a proinflammatory and fibrogenic cytokine response with resultant tissue inflammatory cell infiltration.
In the tissues, the end effector cell of fibrosis is the fibroblast. Fibroblasts from lesional tissue of patients with eosinophilic fasciitis produce excess collagen in vitro and display elevated TGF-beta and type 1 collagen mRNA levels when examined via in situ hybridization with specific cDNA. [7, 8] Therefore, the pathogenesis appears to involve the concomitant increase in the expression of genes for TGF-beta and extracellular matrix proteins in fibroblasts in the affected tissues.
Mori et al suggested that an autocrine stimulatory loop involving major basic protein, a product of eosinophil degranulation, IL-6, which enhances collagen production and is induced by major basic protein, and TGF-beta could account for the progressive fibrosis seen in several eosinophil-prominent disorders. [9]
Other studies showed elevated levels of serum manganese superoxide dismutase and tissue metalloproteinase 1 (TIMP-1) in eosinophilic fasciitis, suggesting a role in pathogenesis and providing a possible marker of disease activity. [10]
Fasciitis may be a common manifestation of various pathophysiologic processes associated with eosinophilia. Understanding the mechanisms involved in the development of fascial inflammation and fibrosis in these conditions may yield insights into the pathogenesis of other fibrotic skin diseases.

Etiology
The etiology of eosinophilic fasciitis is unknown. Its clinical manifestations are the result of an inflammatory response in the affected tissues. As noted above, the current understanding of eosinophilic fasciitis relies on a relatively few case series and case reports. As such, many etiologic factors have been suggested with varying degrees of supporting evidence. Any of these factors, alone or in combination, may possibly initiate this inflammatory response.
Several possible triggers have been reported with some consistency. A preceding history of vigorous exercise or trauma has been reported in 30%-50% of patients. [11, 12] Multiple drugs have also been implicated, including simvastatin, atorvastatin, and phenytoin. [13, 14, 15] In addition, cases of eosinophilic fascitis following treatment with immunne checkpoint inhibitors atezolizumab, nivolumab and pembrolizumab have been reported. [16, 17] One report described eosinophilic fasciitis in association with cemiplimab. [18]
In several cases, patients have demonstrated positive Borrelia serologies. The significance of this finding continues to be debated. Spirochetes were visualized by silver stain in 4 patients in one study. [19] These findings have not been repeated. It has been suggested that positive serology for Borrelia represents an epiphenomenon among cases from _Borrelia_-endemic areas and is insufficient evidence of infection and therefore does not support a causal association. [20]
Eosinophilic fasciitis shares clinical similarities, as well as key differences, with eosinophilia-myalgia syndrome. Some studies have suggested an association between L-tryptophan ingestion and eosinophilic fasciitis. [21, 22] Despite this, no consistent association has been found between L-tryptophan or other dietary exposure and eosinophilic fasciitis. As evidence, l-tryptophan use was significantly associated with dyspnea, an uncommon finding in eosinophilic fasciitis cases. In another instance, a patient with eosinophilic fasciitis had used L-tryptophan for several years but had started a formal exercise program 2 weeks prior to disease onset. [23]
Multiple additional etiologic triggers have been suggested by single or infrequent case reports.
Eosinophilic fasciitis has been associated with several diseases. [24] Hematologic diseases have been consistently reported and are supported by large case series and case reports. [11, 12, 25] The spectrum of associated hematologic disease is broad and includes aplastic and hemolytic anemia, thrombocytopenia, myeloproliferative disorders, myelodysplastic disorders, lymphoma, leukemia, monoclonal gammopathy of undetermined significance (MGUS), and multiple myeloma. [25, 26, 27]
An association with thyroid disease has been reported in several cases. [28] Eosinophilic fasciitis has rarely been linked to solid-organ tumors and primary biliary cholangitis, in addition to several other diseases. These disease associations may suggest a shared pathophysiology of cellular dysregulation and/or autoimmunity.

Epidemiology
Frequency
Eosinophilic fasciitis is very rare.
Mortality/Morbidity
No data are available on morbidity or mortality rates associated with eosinophilic fasciitis. Morbidity may result from joint contractures or carpal tunnel syndrome associated with fascial fibrosis. Rarely, a fatal aplastic anemia may develop.
Race-, sex-, and age-related demographics
Eosinophilic fasciitis affects Whites more often than it affects other races. It has been reported in African Americans, Africans, and Asians. [29, 30, 31, 32, 33]
In adults, eosinophilic fasciitis affects women more often than men. [11, 34, 12]
The age range in eosinophilic fasciitis is 1-88 years, although most patients present during the third to sixth decades of life. [34] The average age of onset in two case series was 54.4 and 49.8 years. [34, 12]

Prognosis
A retrospective review found that clinical factors associated with persistent fibrosis included the following [35] :
- Younger age at onset
- Morphealike skin lesions
- Truncal involvement
- Dermal fibrosclerosis on histopathologic specimen
Loss of edema is usually the first clinical sign of improvement and can occur within 4 weeks of commencing treatment. Concurrently, the skin becomes softer, but 3-6 months may elapse before maximal reduction in induration and contractures is achieved. [11, 12]
While total resolution of the clinical signs can occur, some degree of induration remaining even after many months of corticosteroid therapy is not unusual.
A direct correlation does not always exist between clinical disease activity and laboratory findings. The eosinophil count and erythrocyte sedimentation rate (ESR) usually return to reference ranges within 6-8 weeks, although ESR prolongation and hypergammaglobulinemia may persist for up to 12 months. [11, 12]
Eventually, corticosteroid therapy can be withdrawn in many patients, without relapse occurring.
The development of aplastic anemia is a rare but grave complication. [36] One study reported on 4 patients with eosinophilic fasciitis and severe aplastic anemia. In 3 cases, the aplastic anemia was refractory to conventional immunosuppressive therapy with antithymocyte globulin and cyclosporine. However, in 1 patient, rituximab had significant efficacy for both the skin and hematologic symptoms. In an additional 19 cases of eosinophilic fasciitis and aplastic anemia, corticosteroid regimens improved skin symptoms in 5 of 12 cases but were ineffective in the treatment of aplastic anemia in all but 1 case. Aplastic anemia was profound in 13 cases and was the cause of death in 8 cases. Only 5 patients achieved long-term remission. [37]

- Mazilu D, Boltașiu Tătaru LA, Mardale DA, Bijă MS, Ismail S, Zanfir V, et al. Eosinophilic Fasciitis: Current and Remaining Challenges. Int J Mol Sci. 2023 Jan 19. 24 (3):74. [QxMD MEDLINE Link]. [Full Text].
- Shulman LE. Diffuse fasciitis with eosinophilia: a new syndrome?. Trans Assoc Am Physicians. 1975. 88:70-86. [QxMD MEDLINE Link].
- Blackmond N, Kanke J, Brown K, Weitzman R. Eosinophilic Fasciitis: A Rare and Challenging Diagnosis in a Free Clinic Setting. Cureus. 2022 Jun. 14 (6):e25668. [QxMD MEDLINE Link]. [Full Text].
- Viallard JF, Taupin JL, Ranchin V, Leng B, Pellegrin JL, Moreau JF. Analysis of leukemia inhibitory factor, type 1 and type 2 cytokine production in patients with eosinophilic fasciitis. J Rheumatol. 2001 Jan. 28(1):75-80. [QxMD MEDLINE Link].
- Dziadzio L, Kelly EA, Panzer SE, Jarjour N, Huttenlocher A. Cytokine abnormalities in a patient with eosinophilic fasciitis. Ann Allergy Asthma Immunol. 2003 Apr. 90(4):452-5. [QxMD MEDLINE Link].
- Toquet C, Hamidou MA, Renaudin K, Jarry A, Foulc P, Barbarot S. In situ immunophenotype of the inflammatory infiltrate in eosinophilic fasciitis. J Rheumatol. 2003 Aug. 30(8):1811-5. [QxMD MEDLINE Link].
- Kahari VM, Heino J, Niskanen L, et al. Eosinophilic fasciitis. Increased collagen production and type I procollagen messenger RNA levels in fibroblasts cultured from involved skin. Arch Dermatol. 1990 May. 126(5):613-7. [QxMD MEDLINE Link].
- Peltonen J, Kahari L, Jaakkola S, et al. Evaluation of transforming growth factor beta and type I procollagen gene expression in fibrotic skin diseases by in situ hybridization. J Invest Dermatol. 1990 Mar. 94(3):365-71. [QxMD MEDLINE Link].
- Mori Y, Kahari VM, Varga J. Scleroderma-like cutaneous syndromes. Curr Rheumatol Rep. 2002 Apr. 4(2):113-22. [QxMD MEDLINE Link].
- Jinnin M, Ihn H, Yamane K, Asano Y, Yazawa N, Tamaki K. Serum levels of tissue inhibitor of metalloproteinase-1 and 2 in patients with eosinophilic fasciitis. Br J Dermatol. 2004 Aug. 151(2):407-12. [QxMD MEDLINE Link].
- Lakhanpal S, Ginsburg WW, Michet CJ, et al. Eosinophilic fasciitis: clinical spectrum and therapeutic response in 52 cases. Semin Arthritis Rheum. 1988 May. 17(4):221-31. [QxMD MEDLINE Link].
- Bischoff L, Derk CT. Eosinophilic fasciitis: demographics, disease pattern and response to treatment: report of 12 cases and review of the literature. Int J Dermatol. 2008 Jan. 47(1):29-35. [QxMD MEDLINE Link].
- Choquet-Kastylevsky G, Kanitakis J, Dumas V, Descotes J, Faure M, Claudy A. Eosinophilic fasciitis and simvastatin. Arch Intern Med. 2001 Jun 11. 161(11):1456-7. [QxMD MEDLINE Link].
- DeGiovanni C, Chard M, Woollons A. Eosinophilic fasciitis secondary to treatment with atorvastatin. Clin Exp Dermatol. 2006 Jan. 31(1):131-2. [QxMD MEDLINE Link].
- Buchanan RR, Gordon DA, Muckle TJ, McKenna F, Kraag G. The eosinophilic fasciitis syndrome after phenytoin (dilantin) therapy. J Rheumatol. 1980 Sep-Oct. 7(5):733-6. [QxMD MEDLINE Link].
- Chan KK, Magro C, Shoushtari A, Rudin C, Rotemberg V, Rossi A, et al. Eosinophilic Fasciitis Following Checkpoint Inhibitor Therapy: Four Cases and a Review of Literature. Oncologist. 2020 Feb. 25 (2):140-149. [QxMD MEDLINE Link].
- Le Tallec E, Ricordel C, Triquet L, Deniel A, Marcorelles P, Lena H, et al. An Original Case of an Association of Eosinophilic Fasciitis with Cholangitis Induced by Nivolumab. J Thorac Oncol. 2019 Jan. 14 (1):e13-e15. [QxMD MEDLINE Link].
- Boppana SH, Dulla NR, Beutler BD, Gullapalli N, Kaur R. Drug-Associated Eosinophilic Fasciitis: A Case of Eosinophilic Fasciitis Secondary to Cemiplimab Therapy. Am J Case Rep. 2021 Aug 17. 22:e932888. [QxMD MEDLINE Link]. [Full Text].
- Granter SR, Barnhill RL, Duray PH. Borrelial fasciitis: diffuse fasciitis and peripheral eosinophilia associated with Borrelia infection. Am J Dermatopathol. 1996 Oct. 18(5):465-73. [QxMD MEDLINE Link].
- Antón E. Failure to demonstrate Borrelia burgdorferi-specific DNA in lesions of eosinophilic fasciitis. Histopathology. 2006 Jul. 49(1):88-90. [QxMD MEDLINE Link].
- Blauvelt A, Falanga V. Idiopathic and L-tryptophan-associated eosinophilic fasciitis before and after L-tryptophan contamination. Arch Dermatol. 1991 Aug. 127(8):1159-66. [QxMD MEDLINE Link].
- Hibbs JR, Mittleman B, Hill P, Medsger TA Jr. L-tryptophan-associated eosinophilic fasciitis prior to the 1989 eosinophilia-myalgia syndrome outbreak. Arthritis Rheum. 1992 Mar. 35(3):299-303. [QxMD MEDLINE Link].
- Hamilton ME. Eosinophilic fasciitis associated with L-tryptophan ingestion. Ann Rheum Dis. 1991 Jan. 50 (1):55-6. [QxMD MEDLINE Link]. [Full Text].
- Lee P. Eosinophilic fasciitis: new associations and current perspectives [editorial]. J Rheumatol. 1981 Jan-Feb. 8(1):6-8. [QxMD MEDLINE Link].
- Doyle JA, Connolly SM, Hoagland HC. Hematologic disease in scleroderma syndromes. Acta Derm Venereol. 1985. 65(6):521-5. [QxMD MEDLINE Link].
- Masuoka H, Kikuchi K, Takahashi S, Kakinuma T, Hayashi N, Furue M. Eosinophilic fasciitis associated with low-grade T-cell lymphoma. Br J Dermatol. 1998 Nov. 139(5):928-30. [QxMD MEDLINE Link].
- Garcia VP, de Quiros JF, Caminal L. Autoimmune hemolytic anemia associated with eosinophilic fasciitis. J Rheumatol. 1998 Sep. 25(9):1864-5. [QxMD MEDLINE Link].
- Hur JW, Lee HS, Uhm WS, et al. Eosinophilic fasciitis associated with autoimmune thyroiditis. Korean J Intern Med. 2005 Jun. 20(2):180-2. [QxMD MEDLINE Link].
- Moutsopoulos HM, Webber BL, Pavlidis NA, Fostiropoulos G, Goules D, Shulman LE. Diffuse fasciitis with eosinophilia. A clinicopathologic study. Am J Med. 1980 May. 68(5):701-9. [QxMD MEDLINE Link].
- Barnes L, Rodnan GP, Medsger TA, Short D. Eosinophilic fasciitis. A pathologic study of twenty cases. Am J Pathol. 1979 Aug. 96(2):493-518. [QxMD MEDLINE Link].
- Brent LH, Abruzzo JL. Localized eosinophilic fasciitis in a patient with rheumatoid arthritis. J Rheumatol. 1985 Oct. 12(5):987-9. [QxMD MEDLINE Link].
- Allen SC. Eosinophilic fasciitis in an African--possible benefit of chloroquine treatment. Postgrad Med J. 1984 Oct. 60(708):685-6. [QxMD MEDLINE Link]. [Full Text].
- Nawata Y, Sueishi M, Koike T, Tomioka H. Eosinophilic fasciitis with autoimmune features. Arthritis Rheum. 1983 May. 26(5):688. [QxMD MEDLINE Link].
- Antic M, Lautenschlager S, Itin PH. Eosinophilic fasciitis 30 years after - what do we really know? Report of 11 patients and review of the literature. Dermatology. 2006. 213(2):93-101. [QxMD MEDLINE Link].
- Endo Y, Tamura A, Matsushima Y, Iwasaki T, Hasegawa M, Nagai Y. Eosinophilic fasciitis: report of two cases and a systematic review of the literature dealing with clinical variables that predict outcome. Clin Rheumatol. 2007 Sep. 26(9):1445-51. [QxMD MEDLINE Link].
- Kim SW, Rice L, Champlin R, Udden MM. Aplastic anemia in eosinophilic fasciitis: responses to immunosuppression and marrow transplantation. Haematologia (Budap). 1997. 28(3):131-7. [QxMD MEDLINE Link].
- de Masson A, Bouaziz JD, Peffault de Latour R, Benhamou Y, Moluçon-Chabrot C, Bay JO, et al. Severe aplastic anemia associated with eosinophilic fasciitis: report of 4 cases and review of the literature. Medicine (Baltimore). 2013 Mar. 92(2):69-81. [QxMD MEDLINE Link].
- Inel TY. A clue for eosinophilic fasciitis: groove sign. Rheumatology (Oxford). 2021 Mar 2. 60 (3):1113. [QxMD MEDLINE Link]. [Full Text].
- Wollheim FA, Lindstrom CG, Eiken O. Eosinophilic fasciitis complicated by carpal tunnel syndrome. J Rheumatol. 1981 Sep-Oct. 8(5):856-60. [QxMD MEDLINE Link].
- Caspi D, Fishel R, Varon M, et al. Multisystem presentation of eosinophilic fasciitis. Rheumatol Rehabil. 1982 Nov. 21(4):218-21. [QxMD MEDLINE Link].
- Pinal-Fernandez I, Selva-O' Callaghan A, Grau JM. Diagnosis and classification of eosinophilic fasciitis. Autoimmun Rev. 2014 Apr-May. 13 (4-5):379-82. [QxMD MEDLINE Link].
- Jinnin M, Yamamoto T, Asano Y, Ishikawa O, Sato S, Takehara K, et al. Diagnostic criteria, severity classification and guidelines of eosinophilic fasciitis. J Dermatol. 2018 Aug. 45 (8):881-890. [QxMD MEDLINE Link].
- Wlodek C, Korendowych E, McHugh N, Lovell CR. Morphoea profunda and its relationship to eosinophilic fasciitis. Clin Exp Dermatol. 2018 Apr. 43 (3):306-310. [QxMD MEDLINE Link].
- Chan WH, Lewis DJ, Kim EJ, Aung PP, Duvic M. Generalized morphea/eosinophilic fasciitis overlap after epoxy exposure. JAAD Case Rep. 2018 Mar. 4 (2):175-178. [QxMD MEDLINE Link]. [Full Text].
- Katz JD, Wakem CJ, Parke AL. L-tryptophan associated eosinophilia-myalgia syndrome. J Rheumatol. 1990 Nov. 17(11):1559-61. [QxMD MEDLINE Link].
- Shulman LE. The eosinophilia-myalgia syndrome associated with ingestion of L- tryptophan. Arthritis Rheum. 1990 Jul. 33(7):913-7. [QxMD MEDLINE Link].
- Kaufman LD, Krupp LB. Eosinophilia-myalgia syndrome, toxic-oil syndrome, and diffuse fasciitis with eosinophilia. Curr Opin Rheumatol. 1995 Nov. 7(6):560-7. [QxMD MEDLINE Link].
- Varga J, Kähäri VM. Eosinophilia-myalgia syndrome, eosinophilic fasciitis, and related fibrosing disorders. Curr Opin Rheumatol. 1997 Nov. 9(6):562-70. [QxMD MEDLINE Link].
- Abeles M, Belin DC, Zurier RB. Eosinophilic fasciitis: a clinicopathologic study. Arch Intern Med. 1979 May. 139(5):586-8. [QxMD MEDLINE Link].
- Falanga V, Medsger TA Jr. Frequency, levels, and significance of blood eosinophilia in systemic sclerosis, localized scleroderma, and eosinophilic fasciitis. J Am Acad Dermatol. 1987 Oct. 17(4):648-56. [QxMD MEDLINE Link].
- Naschitz JE, Yeshurun D, Zuckerman E, Rosenbaum M, Misselevitch I, Shajrawi I. Cancer-associated fasciitis panniculitis. Cancer. 1994 Jan 1. 73(1):231-5. [QxMD MEDLINE Link].
- Sugimoto T, Nitta N, Kashiwagi A. Usefulness of magnetic resonance imaging in eosinophilic fasciitis. Rheumatol Int. 2007 Jun. 27(8):791-2. [QxMD MEDLINE Link].
- Moulton SJ, Kransdorf MJ, Ginsburg WW, Abril A, Persellin S. Eosinophilic fasciitis: spectrum of MRI findings. AJR Am J Roentgenol. 2005 Mar. 184(3):975-8. [QxMD MEDLINE Link].
- Agnew KL, Blunt D, Francis ND, Bunker CB. Magnetic resonance imaging in eosinophilic fasciitis. Clin Exp Dermatol. 2005 Jul. 30(4):435-6. [QxMD MEDLINE Link].
- Baumann F, Bruhlmann P, Andreisek G, et al. MRI for diagnosis and monitoring of patients with eosinophilic fasciitis. AJR Am J Roentgenol. 2005 Jan. 184(1):169-74. [QxMD MEDLINE Link].
- Dybowski F, Neuen-Jacob E, Braun J. Eosinophilic fasciitis and myositis: use of imaging modalities for diagnosis and monitoring. Ann Rheum Dis. 2008 Apr. 67(4):572-4. [QxMD MEDLINE Link].
- Verenes M, Stone SL, Hobson-Webb LD, Mhoon JT, Guidon AC, De Jesus-Acosta C, et al. Neuromuscular ultrasound findings in eosinophilic fasciitis: A case series and literature review. Muscle Nerve. 2018 Aug. 58 (2):E15-E18. [QxMD MEDLINE Link]. [Full Text].
- Kissin EY, Garg A, Grayson PC, Dubreuil M, Vradii D, York M, et al. Ultrasound assessment of subcutaneous compressibility: a potential adjunctive diagnostic tool in eosinophilic fasciitis. J Clin Rheumatol. 2013 Oct. 19(7):382-5. [QxMD MEDLINE Link].
- Au Eong DTM, Cronin O, Biswas A, McKay ND. Ultrasound in the diagnosis and monitoring of eosinophilic fasciitis. Rheumatology (Oxford). 2021 Mar 2. 60 (3):e107-e108. [QxMD MEDLINE Link]. [Full Text].
- Bertken R, Shaller D. Chronic progressive eosinophilic fasciitis: report of a 20-year failure to attain remission. Ann Rheum Dis. 1983 Feb. 42(1):103-5. [QxMD MEDLINE Link].
- Carneiro S, Brotas A, Lamy F, et al. Eosinophilic fasciitis (Shulman syndrome). Cutis. 2005 Apr. 75(4):228-32. [QxMD MEDLINE Link].
- Daniel RS, Brown AN. Case report of unilateral eosinophilic fasciitis in a Vietnamese woman. Am J Med Sci. 2009 Feb. 337(2):153-4. [QxMD MEDLINE Link].
- Cramer SF, Kent L, Abramowsky C, Moskowitz RW. Eosinophilic fasciitis. Immunopathology, ultrastructure, literature review,a nd consideration of its pathogenesis and relation to scleroderma. Arch Pathol Lab Med. 1982 Feb. 106(2):85-91. [QxMD MEDLINE Link].
- Kähäri VM, Heino J, Niskanen L, Fräki J, Uitto J. Eosinophilic fasciitis. Increased collagen production and type I procollagen messenger RNA levels in fibroblasts cultured from involved skin. Arch Dermatol. 1990 May. 126(5):613-7. [QxMD MEDLINE Link].
- Wright NA, Mazori DR, Patel M, Merola JF, Femia AN, Vleugels RA. Epidemiology and Treatment of Eosinophilic Fasciitis: An Analysis of 63 Patients From 3 Tertiary Care Centers. JAMA Dermatol. 2016 Jan 1. 152 (1):97-9. [QxMD MEDLINE Link].
- Manzini C, Sebastiani M, Giuggioli D, Manfredi A, Colaci M, Cesinaro A, et al. D-penicillamine in the treatment of eosinophilic fasciitis: case reports and review of the literature. Clin Rheumatol. 2011 Oct 12. [QxMD MEDLINE Link].
- Suzuki G, Itoh Y, Horiuchi Y. Surgical management of eosinophilic fasciitis of the upper extremity. J Hand Surg Br. 1997 Jun. 22(3):405-7. [QxMD MEDLINE Link].
- Tzaribachev N, Holzer U, Schedel J, Maier V, Klein R, Kuemmerle-Deschner J. Infliximab effective in steroid-dependent juvenile eosinophilic fasciitis. Rheumatology (Oxford). 2008 Jun. 47(6):930-2. [QxMD MEDLINE Link].
- Tahara K, Yukawa S, Shoji A, Hayashi H, Tsuboi N. Long-term remission by cyclosporine in a patient with eosinophilic fasciitis associated with primary biliary cirrhosis. Clin Rheumatol. 2008 Sep. 27(9):1199-201. [QxMD MEDLINE Link].
- Herson S, Brechignac S, Godeau P. Cimetidine in eosinophilic fasciitis. Ann Intern Med. 1990 Sep 1. 113(5):412-3. [QxMD MEDLINE Link].
- Bukiej A, Dropinski J, Dyduch G, Szczeklik A. Eosinophilic fasciitis successfully treated with cyclosporine. Clin Rheumatol. 2005 Nov. 24(6):634-6. [QxMD MEDLINE Link].
- Sehgal R, Ernste FC, Eckloff S. Successful Treatment With Baricitinib in a Patient With Refractory Eosinophilic Fasciitis. J Rheumatol. 2021 Jun. 48 (6):948-949. [QxMD MEDLINE Link]. [Full Text].
- Lebeaux D, Francès C, Barete S, Wechsler B, Dubourg O, Renoux J, et al. Eosinophilic fasciitis (Shulman disease): new insights into the therapeutic management from a series of 34 patients. Rheumatology (Oxford). 2012 Mar. 51(3):557-61. [QxMD MEDLINE Link].
- Tkachenko E, Steuer AB, Lo K, LaChance A, Merola JF, Femia AN, et al. Mycophenolate Mofetil for Eosinophilic Fasciitis: A Retrospective Analysis From 3 Tertiary Care Centers. JAMA Dermatol. 2020 May 1. 156 (5):595-597. [QxMD MEDLINE Link].
- El Iskandarani S, Khasho M, Merashli M. Tocilizumab in the Treatment of Eosinophilic Fasciitis: A Case Study and Review of Literature. Mediterr J Rheumatol. 2023 Mar. 34 (1):78-85. [QxMD MEDLINE Link]. [Full Text].
- Tognetti L, Marrocco C, Carraro A, Conticini E, Habougit C, Mariotti G, et al. UVA-1 phototherapy as adjuvant treatment for eosinophilic fasciitis: in vitro and in vivo functional characterization. Int J Dermatol. 2022 Jun. 61 (6):718-726. [QxMD MEDLINE Link].
Author
Peter M Henning, DO MAJ, US Marine Corps; Rheumatology Clinic, Madigan Army Medical Center
Peter M Henning, DO is a member of the following medical societies: American College of Physicians
Disclosure: Nothing to disclose.
Coauthor(s)
George R Mount, MD MAJ USA MC, Assistant Professor of Medicine, Uniformed Services University of the Health Sciences; Attending Physician, Department of Rheumatology, Madigan Army Medical Center, Tacoma, WA
George R Mount, MD is a member of the following medical societies: Alpha Omega Alpha, American College of Physicians, American College of Rheumatology, Phi Beta Kappa
Disclosure: Nothing to disclose.
Kristine M Lohr, MD, MS Professor, Department of Internal Medicine, Interim Chief, Division of Rheumatology, Director, Rheumatology Training Program, University of Kentucky College of Medicine
Kristine M Lohr, MD, MS is a member of the following medical societies: American College of Physicians, American College of Rheumatology
Disclosure: Nothing to disclose.
Specialty Editor Board
Francisco Talavera, PharmD, PhD Adjunct Assistant Professor, University of Nebraska Medical Center College of Pharmacy; Editor-in-Chief, Medscape Drug Reference
Disclosure: Received salary from Medscape for employment. for: Medscape.
Lawrence H Brent, MD Associate Professor of Medicine, Sidney Kimmel Medical College of Thomas Jefferson University; Chair, Program Director, Department of Medicine, Division of Rheumatology, Albert Einstein Medical Center
Lawrence H Brent, MD is a member of the following medical societies: American Association for the Advancement of Science, American Association of Immunologists, American College of Physicians, American College of Rheumatology
Disclosure: Stock ownership for: Johnson & Johnson.
Additional Contributors
Acknowledgements
The opinions or assertions contained here are the private views of the authors and are not to be construed as official or as reflecting the views of the Department of the Army or the Department of Defense.