Pressure Injuries (Pressure Ulcers) and Wound Care Clinical Presentation: History, Physical Examination, Complications (original) (raw)
History
The clinical presentation of pressure injuries (pressure ulcers) can be deceiving to the inexperienced observer. Soft tissue, muscle, and skin resist pressure to differing degrees. Generally, muscle is the least resistant and will become necrotic before skin breaks down. Also, pressure is not equally distributed from the bony surface to the overlying skin; it is greatest at the bony prominence, decreasing gradually toward the periphery. A small area of skin breakdown may represent only the tip of the iceberg, with a large cavity and extensive undermining of skin edges beneath.
In the initial evaluation of a patient with pressure injury, the following important information should be obtained from the history:
- Overall physical and mental health, including life expectancy
- Previous hospitalizations, operations, or ulcerations
- Diet and recent weight changes
- Bowel habits and continence status
- Presence of spasticity or flexion contractures
- Medications and allergies to medications
- Tobacco, alcohol, and recreational drug use
- Place of residence and the support surface used in bed or while sitting
- level of independence, mobility, and ability to comprehend and cooperate with care
- Underlying social and financial support structure
- Presence of specific cultural, religious, or ethnic issues
- Presence of advanced directives, power of attorney, or specific preferences regarding care
Information related to the current pressure injury should also be obtained, particularly with regard to the following:
- Pain - Although pain may be present at the injury site, it is more commonly absent because the patient either is paraplegic is in critical condition and unable to acknowledge pain
- Foul odor or discharge - This could be a sign of a more serious infection at the injury site
- Natural history of the present pressure injury - This would include the length of time the injury has been present, the circumstances under which the ulcer developed, and any local treatments currently or previously employed
- Associated medical cause for the injury (eg, paraplegia, quadriplegia, spina bifida, immobilization in hospital, or multiple sclerosis)
A complete review of systems, including the presence of fevers, night sweats, rigors, weight loss, weakness, or loss of appetite, should be carried out.

Physical Examination
A thorough physical examination is necessary to evaluate the patient’s overall state of health, comorbidities, nutritional status, and mental status. The patient’s level of comprehension and extent of cooperation dictate the intensity of nursing care that will be required. The presence of contractures or spasticity is important to note and may help identify additional areas at risk for pressure ulceration.
After the general physical examination, attention should be turned to the pressure injury. Adequate examination of the wound may necessitate the administration of intravenous (IV) or oral pain medications to ensure patient comfort. Chronic pain may be present among these patients and may be exacerbated by examination ulcer.
Many classification schemes have been developed to define the severity of pressure ulcers. [46] For a considerable period, the most widely accepted approach was that of Shea, which was modified and subsequently refined by the National Pressure Ulcer Advisory Panel (NPUAP). [47] In April 2016, the NPUAP (known as the National Pressure Injury Advisory Panel [NPIAP] since November 2019) announced an updated version of its staging system, along with a change in preferred terminology from pressure ulcer to pressure injury. [1, 2]
The NPIAP system consists of four main stages of pressure injury but is not intended to imply that all pressure injuries follow a standard progression from stage 1 to stage 4 or that healing pressure injuries follow a standard regression from stage 4 to stage 1 to a healed wound. Rather, the system is designed to describe the degree of tissue damage observed at a specific time of examination and is meant to facilitate communication among the various disciplines involved in the study and care of patients with these lesions.
The categories specified in the current NPIAP staging system are as follows [2] :
- Stage 1 pressure injury - Intact skin with a localized area of nonblanchable erythema, which may appear differently in darkly pigmented skin; presence of blanchable erythema or changes in sensation, temperature, or firmness may precede visual changes; color changes do not include purple or maroon discoloration, which may indicate deep tissue pressure injury
- Stage 2 pressure injury - Partial-thickness skin loss with exposed dermis; the wound bed is viable, pink or red, moist, and may also present as an intact or ruptured serum-filled blister; adipose (fat) and deeper tissues are not visible, and granulation tissue, slough and eschar are not present; these injuries commonly result from adverse microclimate and shear in the skin over the pelvis and shear in the heel
- Stage 3 pressure injury - Full-thickness skin loss, in which adipose (fat) is visible in the ulcer and granulation tissue and epibole (rolled wound edges) are often present; slough or eschar may be visible; the depth of tissue damage varies by anatomic location; areas of significant adiposity can develop deep wounds; undermining and tunneling may occur; fascia, muscle, tendon, ligament, cartilage, and bone are not exposed
- Stage 4 pressure injury - Full-thickness skin and tissue loss with exposed or directly palpable fascia, muscle, tendon, ligament, cartilage or bone in the ulcer; slough or eschar may be visible; epibole (rolled edges), undermining, and tunneling often occur; depth varies by anatomic location
- Unstageable pressure injury - Full-thickness skin and tissue loss in which the extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar; if slough or eschar is removed, a stage 3 or 4 pressure injury will be revealed
- Deep tissue pressure injury - Intact or nonintact skin with localized area of persistent nonblanchable deep red, maroon, purple discoloration or epidermal separation revealing a dark wound bed or blood-filled blister; pain and temperature change often precede skin color changes; discoloration may appear differently in darkly pigmented skin; the injury results from intense and/or prolonged pressure and shear forces at the bone-muscle interface
Such staging is only a small part of the initial assessment. The injury location, the size of the skin opening (if present), and the presence of any surrounding maceration or induration must be accurately recorded. The presence of multiple pressure injuries prompts a search for interconnecting tracts with overlying skin bridging that may not be readily apparent. The presence or absence of foul odors, wound drainage, and soiling from urinary or fecal incontinence provides information about bacterial contamination and the need for debridement or diversionary procedures.

Complications
Complications fall into one of two categories: complications of chronic pressure injury (see below) and complications of reconstruction (see Treatment).
Complications of chronic injury include the following:
- Malignant transformation
- Autonomic dysreflexia
- Osteomyelitis
- Pyarthrosis
- Urethral fistula
Malignant transformation
The most serious complication of chronic ulceration is malignant transformation or degeneration (see the images below), also referred to as Marjolin ulceration. Although Marjolin initially described malignant transformation of a chronic scar from a burn wound, the term Marjolin ulcer has been commonly applied to the malignant transformation of any chronic wound, including pressure injuries, osteomyelitis, venous stasis ulcers, urethral fistulas, anal fistulas, and other traumatic wounds. [48]
Heaps of verrucous white tissue around the ulcer suggest malignant transformation, as observed with Marjolin ulcers.
Close-up view of area with heaps of verrucous white tissue around the ulcer, the presence of which suggests malignant transformation (as observed with Marjolin ulcers).
Histologically, this malignant transformation is a well-differentiated squamous cell carcinoma; however, its behavior is very aggressive in pressure injuries, considerably more so than in burns or osteomyelitis. [48] There is a high likelihood of nodal metastasis at the time of diagnosis. Any long-standing, nonhealing wound should alert the examiner to the need for biopsy.
Marjolin ulcers arising from burns or osteomyelitis have been treated with wide local excision, amputation, and lymph node dissection. Because pressure injury carcinoma is substantially more aggressive, more radical treatment (eg, hemicorporectomy and regional node dissection) is required if a cure is to be effected. [48]
The actual rate for malignant transformation of a pressure injury is not known but can be assumed to be low, in that only 18 cases have been described in the literature to date. Although apparently rare, pressure ulcer carcinoma is highly lethal: 12 of the 18 known patients died within 2 years.
Autonomic dysreflexia
Autonomic dysreflexia is a disordered autonomic response to specific stimuli. It includes sweating and flushing proximal to the injury, nasal congestion, headache, intermittent hypertension, piloerection, and bradytachycardia. Patients with midthoracic spinal cord lesions are most prone to this response. When autonomic dysreflexia is suggested, the patient is first positioned with the head up and monitored for changes in heart rate and blood pressure. Then, the precipitating stimulus must be removed.
The most common precipitating cause of autonomic dysreflexia is bladder distention, which is treated by inserting a Foley catheter or irrigating an already placed Foley catheter to remove blockage. Rectal examination to evaluate for fecal impaction should be considered. Nifedipine, hydralazine, or topical nitroglycerin may be administered to stabilize blood pressure. If autonomic dysreflexia does not respond to these measures, spinal anesthesia may be required.
Osteomyelitis
Foremost in the treatment of osteomyelitis is the removal of all nonviable bone, down to bone that bleeds bright red. In the reconstruction of reconstructing pressure injuries associated with osteomyelitis, it is important to use bone that is in the base flaps and has a muscle component. The muscle is placed over this bone after appropriate bone debridement. The flap reconstruction can be performed at the same time as the bone debridement. A 6-week course of IV antibiotics is then administered.
Pyarthrosis
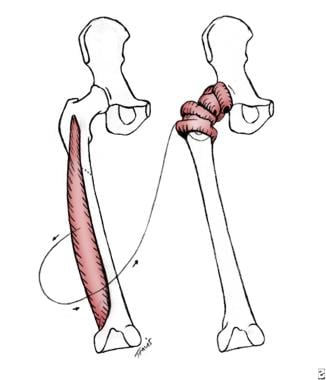
Pyarthrosis of the hip joint can occur with communication of ischial or trochanteric ulcers. Often, the femoral head contains osteomyelitis, which necessitates its removal. The Girdlestone arthroplasty procedure has been employed in this situation (ie, hip pyarthrosis), including removal of the femoral head and reconstruction of this space with the vastus lateralis muscle flap (see the image below).
Illustrated is Girdlestone arthroplasty for femoral head osteomyelitis pyarthrosis of hip joint. Femoral head is removed, and hip joint space is reconstructed with vastus lateralis muscle flap.
Sepsis
Pressure injuries do not cause sepsis. In patients who present with sepsis and pressure injuries, the sepsis is usually caused by a urinary tract infection. These wounds are almost always open to drain and therefore do not constitute debridement emergencies. Only on rare occasions are these injuries entirely occluded by a thick leathery eschar that prevents open drainage. In these cases, debridement is required to facilitate drainage and prevent systemic infection. In general, patients do not die of pressure injuries, but they can die with them.
Urethral fistula
Pressure injuries can also erode into the urethra (see the images below). Treatment of this complication (ie, urethral fistula) involves urinary diversion. Pressure injury reconstruction can be considered once the fistula has healed.
Patient has urethral fistula within his pressure ulcer. When he performs Valsalva maneuver, urine leaks through this opening.
Close-up view in patient who has urethral fistula within his pressure ulcer. When he performs Valsalva maneuver, urine leaks through this opening.

- Edsberg LE, Black JM, Goldberg M, McNichol L, Moore L, Sieggreen M. Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System: Revised Pressure Injury Staging System. J Wound Ostomy Continence Nurs. 2016 Nov/Dec. 43 (6):585-597. [QxMD MEDLINE Link]. [Full Text].
- NPIAP pressure injury stages. National Pressure Injury Advisory Panel. Available at https://cdn.ymaws.com/npiap.com/resource/resmgr/online_store/npiap_pressure_injury_stages.pdf. Accessed: January 31, 2024.
- Schweinberger MH, Roukis TS. Effectiveness of instituting a specific bed protocol in reducing complications associated with bed rest. J Foot Ankle Surg. 2010 Jul-Aug. 49(4):340-7. [QxMD MEDLINE Link].
- Zhao G, Hiltabidel E, Liu Y, Chen L, Liao Y. A cross-sectional descriptive study of pressure ulcer prevalence in a teaching hospital in China. Ostomy Wound Manage. 2010 Feb 1. 56(2):38-42. [QxMD MEDLINE Link].
- Pham B, Stern A, Chen W, Sander B, John-Baptiste A, Thein HH, et al. Preventing pressure ulcers in long-term care: a cost-effectiveness analysis. Arch Intern Med. 2011 Nov 14. 171(20):1839-47. [QxMD MEDLINE Link].
- Pham B, Teague L, Mahoney J, Goodman L, Paulden M, Poss J, et al. Early prevention of pressure ulcers among elderly patients admitted through emergency departments: a cost-effectiveness analysis. Ann Emerg Med. 2011 Nov. 58(5):468-78.e3. [QxMD MEDLINE Link].
- Pieper B, ed. Pressure Ulcers: Prevalence, Incidence, and Implications for the Future. Washington, DC: National Pressure Ulcer Advisory Panel; 2013.
- Leblebici B, Turhan N, Adam M, Akman MN. Clinical and epidemiologic evaluation of pressure ulcers in patients at a university hospital in Turkey. J Wound Ostomy Continence Nurs. 2007 Jul-Aug. 34(4):407-11. [QxMD MEDLINE Link].
- Daniel RK, Faibisoff B. Muscle coverage of pressure points--the role of myocutaneous flaps. Ann Plast Surg. 1982 Jun. 8(6):446-52. [QxMD MEDLINE Link].
- Gefen A. Reswick and Rogers pressure-time curve for pressure ulcer risk. Part 1. Nurs Stand. 2009 Jul 15-21. 23(45):64, 66, 68 passim. [QxMD MEDLINE Link].
- Gefen A. Reswick and Rogers pressure-time curve for pressure ulcer risk. Part 2. Nurs Stand. 2009 Jul 22-28. 23(46):40-4. [QxMD MEDLINE Link].
- LINDAN O, GREENWAY RM, PIAZZA JM. PRESSURE DISTRIBUTION ON THE SURFACE OF THE HUMAN BODY. I. EVALUATION IN LYING AND SITTING POSITIONS USING A "BED OF SPRINGS AND NAILS". Arch Phys Med Rehabil. 1965 May. 46:378-85. [QxMD MEDLINE Link].
- Fogerty M, Guy J, Barbul A, Nanney LB, Abumrad NN. African Americans show increased risk for pressure ulcers: a retrospective analysis of acute care hospitals in America. Wound Repair Regen. 2009 Sep-Oct. 17(5):678-84. [QxMD MEDLINE Link].
- Manley MT. Incidence, contributory factors and costs of pressure sores. S Afr Med J. 1978 Feb 11. 53(6):217-22. [QxMD MEDLINE Link].
- Gerson LW. The incidence of pressure sores in active treatment hospitals. Int J Nurs Stud. 1975. 12(4):201-4. [QxMD MEDLINE Link].
- Shannon ML, Skorga P. Pressure ulcer prevalence in two general hospitals. Decubitus. 1989 Nov. 2(4):38-43. [QxMD MEDLINE Link].
- Meehan M. Multisite pressure ulcer prevalence survey. Decubitus. 1990 Nov. 3(4):14-7. [QxMD MEDLINE Link].
- Bergstrom N, Demuth PJ, Braden BJ. A clinical trial of the Braden Scale for Predicting Pressure Sore Risk. Nurs Clin North Am. 1987 Jun. 22 (2):417-28. [QxMD MEDLINE Link].
- Robnett MK. The incidence of skin breakdown in a surgical intensive care unit. J Nurs Qual Assur. 1986 Nov. 1(1):77-81. [QxMD MEDLINE Link].
- Amlung SR, Miller WL, Bosley LM. The 1999 National Pressure Ulcer Prevalence Survey: a benchmarking approach. Adv Skin Wound Care. 2001 Nov-Dec. 14 (6):297-301. [QxMD MEDLINE Link].
- Roberts BV, Goldstone LA. A survey of pressure sores in the over sixties on two orthopaedic wards. Int J Nurs Stud. 1979. 16(4):355-64. [QxMD MEDLINE Link].
- Versluysen M. How elderly patients with femoral fracture develop pressure sores in hospital. Br Med J (Clin Res Ed). 1986 May 17. 292(6531):1311-3. [QxMD MEDLINE Link]. [Full Text].
- Baumgarten M, Margolis DJ, Orwig DL, Shardell MD, Hawkes WG, Langenberg P, et al. Pressure ulcers in elderly patients with hip fracture across the continuum of care. J Am Geriatr Soc. 2009 May. 57(5):863-70. [QxMD MEDLINE Link]. [Full Text].
- Reed JW. Pressure ulcers in the elderly: prevention and treatment utilizing the team approach. Md State Med J. 1981 Nov. 30(11):45-50. [QxMD MEDLINE Link].
- Barbenel JC, Jordan MM, Nicol SM, Clark MO. Incidence of pressure-sores in the Greater Glasgow Health Board area. Lancet. 1977 Sep 10. 2(8037):548-50. [QxMD MEDLINE Link].
- Schols JM, Heyman H, Meijer EP. Nutritional support in the treatment and prevention of pressure ulcers: an overview of studies with an arginine enriched oral nutritional supplement. J Tissue Viability. 2009 Aug. 18(3):72-9. [QxMD MEDLINE Link].
- Berlowitz DR, Wilking SV. Risk factors for pressure sores. A comparison of cross-sectional and cohort-derived data. J Am Geriatr Soc. 1989 Nov. 37(11):1043-50. [QxMD MEDLINE Link].
- Kenkel JM. Pressure Sores (overview). Kenkel JM. Selected Read Plast Surg. Texas: Baylor University Medical Center; 1998. Vol 8, No 39: 1-29.
- Klitzman B, Kalinowski C, Glasofer SL, Rugani L. Pressure ulcers and pressure relief surfaces. Clin Plast Surg. 1998 Jul. 25(3):443-50. [QxMD MEDLINE Link].
- Evans GR, Dufresne CR, Manson PN. Surgical correction of pressure ulcers in an urban center: is it efficacious?. Adv Wound Care. 1994 Jan. 7 (1):40-6. [QxMD MEDLINE Link].
- Fuhrer MJ, Garber SL, Rintala DH, Clearman R, Hart KA. Pressure ulcers in community-resident persons with spinal cord injury: prevalence and risk factors. Arch Phys Med Rehabil. 1993 Nov. 74(11):1172-7. [QxMD MEDLINE Link].
- Basson MD, Burney RE. Defective wound healing in patients with paraplegia and quadriplegia. Surg Gynecol Obstet. 1982 Jul. 155(1):9-12. [QxMD MEDLINE Link].
- Regan MA, Teasell RW, Wolfe DL, Keast D, Mortenson WB, Aubut JA. A systematic review of therapeutic interventions for pressure ulcers after spinal cord injury. Arch Phys Med Rehabil. 2009 Feb. 90(2):213-31. [QxMD MEDLINE Link]. [Full Text].
- Okamoto GA, Lamers JV, Shurtleff DB. Skin breakdown in patients with myelomeningocele. Arch Phys Med Rehabil. 1983 Jan. 64(1):20-3. [QxMD MEDLINE Link].
- Basset A, Liautaud B, Ndiaye B. Dermatology of Black Skin. Oxford: Oxford University Press; 1986.
- Lahmann NA, Dassen T, Poehler A, Kottner J. Pressure ulcer prevalence rates from 2002 to 2008 in German long-term care facilities. Aging Clin Exp Res. 2010 Apr. 22(2):152-6. [QxMD MEDLINE Link].
- Fogerty MD, Abumrad NN, Nanney L, Arbogast PG, Poulose B, Barbul A. Risk factors for pressure ulcers in acute care hospitals. Wound Repair Regen. 2008 Jan-Feb. 16(1):11-8. [QxMD MEDLINE Link].
- Howard DL, Taylor YJ. Racial and gender differences in pressure ulcer development among nursing home residents in the Southeastern United States. J Women Aging. 2009. 21(4):266-78. [QxMD MEDLINE Link].
- Dinsdale SM. Decubitus ulcers: role of pressure and friction in causation. Arch Phys Med Rehabil. 1974 Apr. 55(4):147-52. [QxMD MEDLINE Link].
- Allman RM. Pressure ulcers among the elderly. N Engl J Med. 1989 Mar 30. 320(13):850-3. [QxMD MEDLINE Link].
- Allman RM, Walker JM, Hart MK, Laprade CA, Noel LB, Smith CR. Air-fluidized beds or conventional therapy for pressure sores. A randomized trial. Ann Intern Med. 1987 Nov. 107(5):641-8. [QxMD MEDLINE Link].
- Maklebust J. Pressure ulcers: etiology and prevention. Nurs Clin North Am. 1987 Jun. 22(2):359-77. [QxMD MEDLINE Link].
- Doughty D. The process of wound healing: a nursing perspective. Prog Develop Ostomy Wound Care. 1990. 2:3-12.
- Peromet M, Labbe M, Yourassowsky E, Schoutens E. Anaerobic bacteria isolated from decubitus ulcers. Infection. 1973. 1(4):205-7. [QxMD MEDLINE Link].
- Deloach ED, DiBenedetto RJ, Womble L, Gilley JD. The treatment of osteomyelitis underlying pressure ulcers. Decubitus. 1992 Nov. 5(6):32-41. [QxMD MEDLINE Link].
- Stausberg J, Kiefer E. Classification of pressure ulcers: a systematic literature review. Stud Health Technol Inform. 2009. 146:511-5. [QxMD MEDLINE Link].
- Black J, Baharestani M, Cuddigan J, Dorner B, Edsberg L, Langemo D, et al. National Pressure Ulcer Advisory Panel's updated pressure ulcer staging system. Dermatol Nurs. 2007 Aug. 19(4):343-9; quiz 350. [QxMD MEDLINE Link].
- Copcu E. Marjolin's ulcer: a preventable complication of burns?. Plast Reconstr Surg. 2009 Jul. 124(1):156e-64e. [QxMD MEDLINE Link].
- James GA, Swogger E, Wolcott R, Pulcini Ed, Secor P, Sestrich J, et al. Biofilms in chronic wounds. Wound Repair Regen. 2008 Jan-Feb. 16(1):37-44. [QxMD MEDLINE Link].
- Kirker KR, Secor PR, James GA, Fleckman P, Olerud JE, Stewart PS. Loss of viability and induction of apoptosis in human keratinocytes exposed to Staphylococcus aureus biofilms in vitro. Wound Repair Regen. 2009 Sep-Oct. 17(5):690-9. [QxMD MEDLINE Link]. [Full Text].
- Schierle CF, De la Garza M, Mustoe TA, Galiano RD. Staphylococcal biofilms impair wound healing by delaying reepithelialization in a murine cutaneous wound model. Wound Repair Regen. 2009 May-Jun. 17(3):354-9. [QxMD MEDLINE Link].
- Rhoads DD, Wolcott RD, Percival SL. Biofilms in wounds: management strategies. J Wound Care. 2008 Nov. 17 (11):502-8. [QxMD MEDLINE Link].
- Woolsey RM, McGarry JD. The cause, prevention, and treatment of pressure sores. Neurol Clin. 1991 Aug. 9 (3):797-808. [QxMD MEDLINE Link].
- Gorecki C, Nixon J, Madill A, Firth J, Brown JM. What influences the impact of pressure ulcers on health-related quality of life? A qualitative patient-focused exploration of contributory factors. J Tissue Viability. 2012 Feb. 21(1):3-12. [QxMD MEDLINE Link].
- [Guideline] Qaseem A, Mir TP, Starkey M, Denberg TD. Risk assessment and prevention of pressure ulcers: a clinical practice guideline from the american college of physicians. Ann Intern Med. 2015 Mar 3. 162(5):359-69. [QxMD MEDLINE Link].
- [Guideline] Qaseem A, Humphrey LL, Forciea MA, Starkey M, Denberg TD. Treatment of pressure ulcers: a clinical practice guideline from the american college of physicians. Ann Intern Med. 2015 Mar 3. 162(5):370-9. [QxMD MEDLINE Link].
- Banks MD, Graves N, Bauer JD, Ash S. Cost effectiveness of nutrition support in the prevention of pressure ulcer in hospitals. Eur J Clin Nutr. 2013 Jan. 67(1):42-6. [QxMD MEDLINE Link].
- Cereda E, Gini A, Pedrolli C, Vanotti A. Disease-specific, versus standard, nutritional support for the treatment of pressure ulcers in institutionalized older adults: a randomized controlled trial. J Am Geriatr Soc. 2009 Aug. 57(8):1395-402. [QxMD MEDLINE Link].
- Benbow M, Bateman S. Working towards clinical excellence Pressure ulcer prevention and management in primary and secondary care. J Wound Care. 2012 Sep. 21(9):S25-40. [QxMD MEDLINE Link].
- Heyneman A, Vanderwee K, Grypdonck M, Defloor T. Effectiveness of two cushions in the prevention of heel pressure ulcers. Worldviews Evid Based Nurs. 2009. 6(2):114-20. [QxMD MEDLINE Link].
- McInnes E, Dumville JC, Jammali-Blasi A, Bell-Syer SE. Support surfaces for treating pressure ulcers. Cochrane Database Syst Rev. 2011 Dec 7. CD009490. [QxMD MEDLINE Link].
- Cullum N, McInnes E, Bell-Syer SE, Legood R. Support surfaces for pressure ulcer prevention. Cochrane Database Syst Rev. 2004. CD001735:
- McInnes E, Jammali-Blasi A, Bell-Syer SE, Dumville JC, Cullum N. Support surfaces for pressure ulcer prevention. Cochrane Database Syst Rev. 2011 Apr 13. CD001735. [QxMD MEDLINE Link].
- McInnes E, Jammali-Blasi A, Bell-Syer SE, Dumville JC, Middleton V, Cullum N. Support surfaces for pressure ulcer prevention. Cochrane Database Syst Rev. 2015 Sep 3. CD001735. [QxMD MEDLINE Link]. [Full Text].
- Clark M, Hiskett G, Russell L. Evidence-based practice and support surfaces: are we throwing the baby out with the bath water?. J Wound Care. 2005 Nov. 14(10):455-8. [QxMD MEDLINE Link].
- Bruce TA, Shever LL, Tschannen D, Gombert J. Reliability of pressure ulcer staging: a review of literature and 1 institution's strategy. Crit Care Nurs Q. 2012 Jan-Mar. 35(1):85-101. [QxMD MEDLINE Link].
- Bergstrom N, Bennett MA, Carlson CE, et al. Treatment of Pressure Ulcers. Clinical Practice Guideline Number 14. Agency for Health Care Policy and Research, Public Health Service. Rockville, MD: US Department of Health and Human Services; 1994. AHCPR Publication No. 95-0642.:
- Ho CH, Bensitel T, Wang X, Bogie KM. Pulsatile lavage for the enhancement of pressure ulcer healing: a randomized controlled trial. Phys Ther. 2012 Jan. 92(1):38-48. [QxMD MEDLINE Link].
- Werdin F, Tennenhaus M, Schaller HE, Rennekampff HO. Evidence-based management strategies for treatment of chronic wounds. Eplasty. 2009 Jun 4. 9:e19. [QxMD MEDLINE Link]. [Full Text].
- Flemming K, Cullum N. Electromagnetic therapy for the treatment of pressure sores. Cochrane Database Syst Rev. 2001. CD002930. [QxMD MEDLINE Link].
- Landi F, Aloe L, Russo A, Cesari M, Onder G, Bonini S, et al. Topical treatment of pressure ulcers with nerve growth factor: a randomized clinical trial. Ann Intern Med. 2003 Oct 21. 139 (8):635-41. [QxMD MEDLINE Link].
- Salcido R, Carney J, Fisher S, et al. A reliable animal model of pressure sore development: The role of free radicals. J Am Paraplegia Soc. 1993. 16:61.
- Salcido R, Fisher SB, Donofrio JC, Bieschke M, Knapp C, Liang R, et al. An animal model and computer-controlled surface pressure delivery system for the production of pressure ulcers. J Rehabil Res Dev. 1995 May. 32(2):149-61. [QxMD MEDLINE Link].
- Ford CN, Reinhard ER, Yeh D, Syrek D, De Las Morenas A, Bergman SB, et al. Interim analysis of a prospective, randomized trial of vacuum-assisted closure versus the healthpoint system in the management of pressure ulcers. Ann Plast Surg. 2002 Jul. 49(1):55-61; discussion 61. [QxMD MEDLINE Link].
- Evans D, Land L. Topical negative pressure for treating chronic wounds. Cochrane Database Syst Rev. 2001. CD001898. [QxMD MEDLINE Link].
- Gupta S, Baharestani M, Baranoski S, de Leon J, Engel SJ, Mendez-Eastman S, et al. Guidelines for managing pressure ulcers with negative pressure wound therapy. Adv Skin Wound Care. 2004 Nov-Dec. 17 Suppl 2:1-16. [QxMD MEDLINE Link].
- Niezgoda JA. Combining negative pressure wound therapy with other wound management modalities. Ostomy Wound Manage. 2005 Feb. 51 (2A Suppl):36S-38S. [QxMD MEDLINE Link].
- Mendez-Eastman S. Guidelines for using negative pressure wound therapy. Adv Skin Wound Care. 2001 Nov-Dec. 14(6):314-22; quiz 324-5. [QxMD MEDLINE Link].
- He J, Xu H, Wang T, Ma S, Dong J. Treatment of complex ischial pressure sores with free partial lateral latissimus dorsi musculocutaneous flaps in paraplegic patients. J Plast Reconstr Aesthet Surg. 2012 May. 65(5):634-9. [QxMD MEDLINE Link].
- Lin H, Hou C, Chen A, Xu Z. Treatment of ischial pressure sores using a modified gracilis myofasciocutaneous flap. J Reconstr Microsurg. 2010 Apr. 26(3):153-7. [QxMD MEDLINE Link].
- Wound, Ostomy and Continence Nurses Society. Guideline for Prevention and Management of Pressure Ulcers (Injuries). Mt Laurel, NJ: Wound, Ostomy and Continence Nurses Society; 2016.
- Schmitt S, Andries MK, Ashmore PM, Brunette G, Judge K, Bonham PA. WOCN Society Position Paper: Avoidable Versus Unavoidable Pressure Ulcers/Injuries. J Wound Ostomy Continence Nurs. 2017 Sep/Oct. 44 (5):458-468. [QxMD MEDLINE Link]. [Full Text].
- Schoonhoven L, Grobbee DE, Donders AR, Algra A, Grypdonck MH, Bousema MT, et al. Prediction of pressure ulcer development in hospitalized patients: a tool for risk assessment. Qual Saf Health Care. 2006 Feb. 15 (1):65-70. [QxMD MEDLINE Link]. [Full Text].
- Walton-Geer PS. Prevention of pressure ulcers in the surgical patient. AORN J. 2009 Mar. 89(3):538-48; quiz 549-51. [QxMD MEDLINE Link].
- Saleh M, Anthony D, Parboteeah S. The impact of pressure ulcer risk assessment on patient outcomes among hospitalised patients. J Clin Nurs. 2009 Jul. 18(13):1923-9. [QxMD MEDLINE Link].
- Bergstrom N. Panel for the Prediction and Prevention of Pressure Ulcers in Adults. Prediction and Prevention Clinical Practice Guideline, Number 3. Agency for Health Care Policy and Research, Public Health Service. AHCPR Publication No. 920047. Rockville, MD: US Department of Health and Human Services; 1992.
- Milne CT, Trigilia D, Houle TL, Delong S, Rosenblum D. Reducing pressure ulcer prevalence rates in the long-term acute care setting. Ostomy Wound Manage. 2009 Apr. 55(4):50-9. [QxMD MEDLINE Link].
- Crewe R. Problems of rubber ring nursing cushions and a clinical survey of alternative cushions for ill patients. Care Sci Pract. 1987. 5:9-11.
- Bergstrom N, Braden BJ, Laguzza A, Holman V. The Braden Scale for Predicting Pressure Sore Risk. Nurs Res. 1987 Jul-Aug. 36(4):205-10. [QxMD MEDLINE Link].
- Norton D. Calculating the risk: reflections on the Norton Scale. Decubitus. 1989 Aug. 2(3):24-31. [QxMD MEDLINE Link].
- Norton D, McLaren R, Exton-Smith A. An Investigation of Geriatric Nursing Problems in Hospital. London: Churchill Livingstone; 1975.
- Watanabe S, Yamada K, Ono S, Ishibashi Y. Skin changes in patients with amyotrophic lateral sclerosis: light and electron microscopic observations. J Am Acad Dermatol. 1987 Dec. 17(6):1006-12. [QxMD MEDLINE Link].
- Conine TA, Daechsel D, Lau MS. The role of alternating air and Silicore overlays in preventing decubitus ulcers. Int J Rehabil Res. 1990. 13(1):57-65. [QxMD MEDLINE Link].
- Warner DJ. A clinical comparison of two pressure-reducing surfaces in the management of pressure ulcers. Decubitus. 1992 May. 5(3):52-5, 58-60, 62-4. [QxMD MEDLINE Link].
- Smoot EC 3rd. Clinitron bed therapy hazards. Plast Reconstr Surg. 1986 Jan. 77(1):165. [QxMD MEDLINE Link].
- Nimit K. Guidelines for home air-fluidized bed therapy, 1989. Health Technol Assess Rep. 1989. 1-11. [QxMD MEDLINE Link].
Author
Chief Editor
John Geibel, MD, MSc, DSc, AGAF Vice Chair and Professor, Department of Surgery, Section of Gastrointestinal Medicine, Professor, Department of Cellular and Molecular Physiology, Yale University School of Medicine; Director of Surgical Research, Department of Surgery, Yale-New Haven Hospital; American Gastroenterological Association Fellow; Fellow of the Royal Society of Medicine
John Geibel, MD, MSc, DSc, AGAF is a member of the following medical societies: American Gastroenterological Association, American Physiological Society, American Society of Nephrology, Association for Academic Surgery, International Society of Nephrology, New York Academy of Sciences, Society for Surgery of the Alimentary Tract
Disclosure: Nothing to disclose.
Acknowledgements
Kat Kolaski, MD Assistant Professor, Departments of Orthopedic Surgery and Pediatrics, Wake Forest University School of Medicine
Kat Kolaski, MD is a member of the following medical societies: American Academy for Cerebral Palsy and Developmental Medicine and American Academy of Physical Medicine and Rehabilitation
Disclosure: Nothing to disclose.
Consuelo T Lorenzo, MD Physiatrist, Department of Physical Medicine and Rehabilitation, Alegent Health Immanuel Rehabilitation Center
Consuelo T Lorenzo, MD is a member of the following medical societies: American Academy of Physical Medicine and Rehabilitation
Disclosure: Nothing to disclose.
Joseph A Molnar, MD, PhD, FACS Director, Wound Care Center, Associate Director of Burn Unit, Associate Professor, Department of Plastic and Reconstructive Surgery, Wake Forest University School of Medicine
Joseph A Molnar, MD, PhD, FACS is a member of the following medical societies: American Association of Plastic Surgeons, American Burn Association, American College of Surgeons, American Medical Association, American Society for Parenteral and Enteral Nutrition, American Society of Plastic Surgeons, North Carolina Medical Society, Peripheral Nerve Society, Undersea and Hyperbaric Medical Society, and Wound Healing Society
Disclosure: Abbott Laboratories Honoraria Speaking and teaching; Clincal Cell Culture Grant/research funds Co-investigator; KCI, Inc Wake Forest University receives royalties Other
Michael Neumeister, MD, FRCSC, FRCSC, FACS Chairman, Professor, Division of Plastic Surgery, Director of Hand/Microsurgery Fellowship Program, Chief of Microsurgery and Research, Institute of Plastic and Reconstructive Surgery, Southern Illinois University School of Medicine
Michael Neumeister, MD, FRCSC, FRCSC, FACS is a member of the following medical societies: American Association for Hand Surgery, American Association of Plastic Surgeons, American Burn Association, American College of Surgeons, American Medical Association, American Society for Reconstructive Microsurgery, American Society for Surgery of the Hand, American Society of Plastic Surgeons, Association of Academic Chairmen of Plastic Surgery, CanadianSocietyofPlastic Surgeons, Illinois State Medical Society, Illinois State Medical Society, Ontario Medical Association, Plastic Surgery Research Council, Royal College of Physicians and Surgeons of Canada, and Society of University Surgeons
Disclosure: Nothing to disclose.
Adrian Popescu, MD Research Fellow, Department of Physical Medicine and Rehabilitation, University of Pennsylvania School of Medicine
Disclosure: Nothing to disclose.
Patrick J Potter, MD, FRCP(C) Associate Professor, Department of Physical Medicine and Rehabilitation, University of Western Ontario School of Medicine; Consulting Staff, Department of Physical Medicine and Rehabilitation, St Joseph's Health Care Centre
Patrick J Potter, MD, FRCP(C) is a member of the following medical societies: American Paraplegia Society, Canadian Association of Physical Medicine and Rehabilitation, Canadian Medical Association, College of Physicians and Surgeons of Ontario, Ontario Medical Association, and Royal College of Physicians and Surgeons of Canada
Disclosure: Nothing to disclose.
Don R Revis Jr, MD Consulting Staff, Department of Surgery, Division of Plastic and Reconstructive Surgery, University of Florida College of Medicine
Don R Revis Jr, MD is a member of the following medical societies: American College of Surgeons, American Medical Association, American Society for Aesthetic Plastic Surgery, and American Society of Plastic Surgeons
Disclosure: Nothing to disclose.
Richard Salcido, MD Chairman, Erdman Professor of Rehabilitation, Department of Physical Medicine and Rehabilitation, University of Pennsylvania School of Medicine
Richard Salcido, MD is a member of the following medical societies: American Academy of Pain Medicine, American Academy of Physical Medicine and Rehabilitation, American College of Physician Executives, American Medical Association, and American Paraplegia Society
Disclosure: Nothing to disclose.
Wayne Karl Stadelmann, MD Stadelmann Plastic Surgery, PC
Wayne Karl Stadelmann, MD is a member of the following medical societies: Alpha Omega Alpha, American College of Surgeons, American Society of Plastic Surgeons, New Hampshire Medical Society, Northeastern Society of Plastic Surgeons, and Phi Beta Kappa
Disclosure: Nothing to disclose.
Francisco Talavera, PharmD, PhD Adjunct Assistant Professor, University of Nebraska Medical Center College of Pharmacy; Editor-in-Chief, Medscape Drug Reference
Disclosure: Medscape Salary Employment
Bradon J Wilhelmi, MD Professor and Endowed Leonard J Weiner, MD, Chair of Plastic Surgery, Residency Program Director, University of Louisville School of Medicine
Bradon J Wilhelmi, MD is a member of the following medical societies: Alpha Omega Alpha, American Association for Hand Surgery, American Association of Clinical Anatomists, American Association of Plastic Surgeons, American Burn Association, American College of Surgeons, American Society for Aesthetic Plastic Surgery, American Society for Reconstructive Microsurgery, American Society for Surgery of the Hand, American Society of Plastic Surgeons,Association for Surgical Education, Plastic Surgery Research Council, and Wound Healing Society
Disclosure: Nothing to disclose.
Acknowledgments
The authors and editors of Medscape Reference gratefully acknowledge the contributions of Steve Jenkins in the Department of Physical Medicine and Rehabilitation at the University of Kentucky for his significant editorial assistance in preparing this article.
Dr Richard Salcido acknowledges that his studies cited in this article are supported by the National Heart, Lung and Blood Institute, the National Institutes of Health grant P01HL36552-07, the National Center for Medical Rehabilitation Research grant R01HD31426-01, the Paralyzed