Minimally Invasive Esophagectomy: Background, Indications, Contraindications (original) (raw)
Background
Minimally invasive esophagectomy (MIE) is a well-accepted approach to the treatment of benign esophageal diseases. It has not been as widely employed for the treatment of esophageal cancer, largely because it is highly technical and complex, but a number of studies have supported its feasibility in this context, and interest in this application has grown. [1, 2]
The incidence of esophageal cancer has increased over the last several decades, and adenocarcinoma now surpasses the incidence of squamous cell carcinoma. Treatment of esophageal carcinoma has become more aggressive and effective, and the overall morbidity and mortality in those who are surgically treated have declined, approaching 8-11% and 40-50%, respectively. [3, 4]
In the 17th century, the first cervical esophagotomy was reported; in the latter part of the 19th century, the first cervical esophagectomy was performed by Johann Nepomuk Czerny. [5] In 1913, Franz Torek performed the first thoracic esophagectomy for cancer in the German (now Lenox Hill) Hospital in New York City. [6] Over the next several decades, open surgical esophagectomy developed as an acceptable treatment for benign disease as well as esophageal cancer.
In 1989, interest in laparoscopic surgical techniques was sparked, as the first laparoscopic cholecystectomy was performed. [7] This technique was first adapted into the field of esophageal disease in 1991 with laparoscopic fundoplication, performed by Dallemagne et al. [8] With this, the shift toward minimally invasive esophageal surgery began.
Traditional approaches via open transhiatal or transthoracic (Ivor Lewis) resections were first "hybridized" with minimally invasive techniques, where parts of the procedure were performed in a minimally invasive fashion and other parts via standard incisions. [9]
Dallemagne et al performed the first mini-invasive subtotal esophagectomy in 1992, using both thoracoscopy (for dissecting the esophagus) and laparoscopy (for the gastroplasty). [10] The first esophagectomy performed completely via laparoscopy through a transhiatal approach was in 1995 by DePaul et al. [11] In 1999, Watson et al described a completely minimally invasive Ivor Lewis technique. [12] Since then, robotic-assisted approaches have described [13, 14, 15, 16, 17] (see the video below). Single-port approaches have been developed as well. [18]
Advantages of robotic-assisted minimally invasive surgery. Video courtesy of Memorial Sloan-Kettering Cancer Center, featuring Inderpal S Sarkaria, MD.

Indications
Traditionally, esophagectomy has been performed via open transthoracic or transhiatal approaches, with randomized trials showing no significant difference in overall survival or disease-free survival. Outcomes after MIE have compared favorably to the reported series of open esophagectomy. [19]
Minimally invasive approaches to treatment of benign esophageal diseases have been met with widespread acceptance. This includes diseases such as achalasia, paraesophageal hernia, and other complex esophageal disorders. [20, 21, 22, 23]
This has not been the case with malignant disease of the esophagus. Currently, criteria for determining when a minimally invasive procedure should be performed in preference to an open procedure remain to be defined. [24] However, support for the feasibility of employing MIE in esophageal cancer has grown. [25] A multicenter retrospective matched-cohort study by Capovilla et al found that in 160 elderly patients (> 75 y) with esophageal cancer, thoracoscopic/laparoscopic MIE and robot-assisted MIE (RAMIE; n = 58) yielded a better postoperative course than open esophagectomy (n = 102), an improvement comparable to that seen in younger patients. [26]
Many high-volume institutions have increasingly elected to use MIE in the treatment of Barrett disease with high-grade dysplasia and in patients with small resectable lesions that have limited nodal involvement (N0-1). This includes T1 (invasion of the lamina propria or submucosa), T2 (invasion of the muscularis propria), and some instances of T3 lesions (invasion of the adventitia). Neoadjuvant chemoradiation is not a contraindication for MIE. [27, 28] For more information, see Esophageal Cancer Guidelines.

Contraindications
Currently, no standardized contraindications exist for the use of MIE. However, T4 lesions (invasion of surrounding tissues) are generally not amenable to any form of surgical resection. Extensive nodal disease and metastatic disease are also advanced stages that may necessitate an open surgical approach or even endoscopic stenting for palliation instead of an attempt at MIE. [28] Furthermore, any patient with a lesion that bridges the esophagogastric junction (EGJ) may not be considered a candidate for this approach unless the gastric margin can be cleared and an esophagogastrectomy can be done via either an open or a minimally invasive approach.
As with other laparoscopic procedures, patients with extensive adhesions and scar tissue over the abdomen or chest wall, particularly in areas where the thoracoscope or laparoscope would be placed, are at higher risk with MIE. Older patients and those with comorbid conditions are not candidates for surgery, because of the high morbidity with either an MIE or a standard procedure, but they may benefit more from nonsurgical therapy. [29]

Outcomes
Minimally invasive techniques for esophageal resection have been reported to have acceptably reduced procedure-related morbidity without compromising disease-free survival rates. [19]
Luketich et al have reported an extensive experience; their initial series of 222 patients had grown to more than 1000 by 2012. [30] In the initial series, mortality was 1.4% versus 5.5% for an open approach. [29, 31, 32] Furthermore, the survival curve at 19-month follow-up was comparable in the two groups. [29] In their 2012 report of 1011 patients who underwent MIE via either a modified McKeown minimally invasive approach or an Ivor Lewis approach, the authors cited a 0.9% mortality for the Ivor Lewis MIE approach. [30]
In another analysis of 41 elderly patients over the age of 75 years who underwent MIE, no operative deaths occurred, with a survival of 81% at 20 month follow-up. [33] These findings suggest that MIE can be safely performed in selected patients and even in those considered high-risk who might not otherwise be considered for an open surgery.
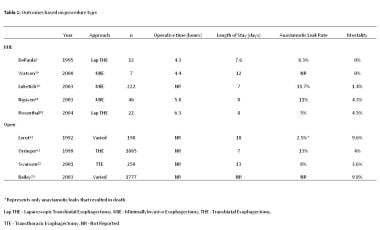
Other outcome improvements seen with MIE include decreased intensive care unit (ICU) and hospital length of stay, reduced blood loss, and shorter operating times. In particular, Luketich et al reported a median ICU stay of 1 day and a total hospital stay of 7 days, compared with the average hospital stay of 16.6 days in the open approach. Operating room times in the same study averaged 306 minutes, whereas the average for an open procedure is 336 minutes. [29, 31] Similar results can be seen in multiple other series as compared with open procedures (see the table below).
Outcomes based on procedure type.
Complications and outcomes are significantly influenced by the volume of patients, because a large learning curve exists. High-volume centers tend to have more experience and therefore better outcomes than smaller-volume hospitals.
Wang et al carried out a propensity score-matched comparison of MIE and open esophagectomy with respect to outcomes, quality of life, and survival in patients with squamous cell carcinoma. [34] They found that MIE was associated with a shorter operating time (191 ± 47 vs 211 ± 44 min), reduced blood loss (135 ± 74 vs 163 ± 84 mL), a similar lymph node harvest (24.1 ± 6.2 vs 24.3 ± 6.0), a shorter postoperative hospital stay (11 vs 12 d), a lower rate of major complications (30.4% vs 36.9%), a lower rate of readmission to the ICU (5.6% vs 9.7%), and comparable perioperative mortality.
van der Sluis et al assessed the long-term oncologic results of RAMIE with two-field lymphadenectomy in 108 patients with potentially resectable esophageal cancer. [35] They found RAMIE to be oncologically effective and capable of providing good local control with a low percentage of local recurrence at long-term follow-up.
In a subsequent randomized controlled trial that included 112 patients with resectable intrathoracic esophageal cancer who were treated with either RAMIE or open transthoracic esophagectomy (OTE), van der Sluis et al found RAMIE to be associated with lower rates of overall surgery-related and cardiopulmonary complications, less postoperative pain, better short-term quality of life, and superior short-term postoperative functional recovery compared to OTE. [36] Oncologic outcomes were comparable for the two approaches.
In a prospective phase II study coordinated by the Eastern Cooperative Oncology Group (ECOG), which was aimed at assessing the feasibility of MIE in a multi-institutional setting, Luketich et al reported the following results [37] :
- The 30-day mortality in eligible patients who underwent MIE was 2.1%
- The median ICU stay was 2 days
- The median hospital stay was 9 days
- Adverse events classified as grade 3 or higher included anastomotic leakage (8.6%), acute respiratory distress syndrome (ARDS; 5.7%), pneumonitis (3.8%), and atrial fibrillation (2.9%)
- The estimated 3-year overall survival (median follow-up, 35.8 months) was 58.4%
- Locoregional recurrence occurred in only 7 patients (6.7%)
In a nationwide retrospective analysis from Japan that included 14,880 patients who underwent esophagectomy for clinical stage 0-III esophageal cancer, Sakamoto et al compared in-hospital mortality and morbidity for MIE versus open esophagectomy. [38] MIE was associated with lower incidences of in-hospital mortality, surgical-site infection (SSI), anastomotic leakage, blood transfusion, reoperation, tracheotomy, and unplanned intubation, as well as a shorter postoperative stay. However, MIE was also associated with higher rates of vocal cord dysfunction and prolonged intubation after esophagectomy, as well as a longer duration of anesthesia.
In a meta-analysis of 14 studies (N = 3468), Deng et al evaluated short-term outcomes for minimally invasive McKeown esophagectomy (MIME) vs minimally invasive Ivor Lewis esophagectomy (MILE) in patients with resectable esophageal or junctional tumors. [39] MIME led to more blood loss, longer operating times, and longer hospital stays, as well as higher rates of pulmonary complications, total anastomotic leak, stricture, and vocal cord injury/palsy. No significant differences were found in R0 resection rate; number of lymph modes retrieved; blood transfusion rate; length of ICU stay; incidence of cardiac arrhythmia, chyle leak, or severe anastomotic leak; 30-day/in-hospital mortality; or 90-day mortality.
In a study of 76 patients with resectable esophageal malignancies, Guerra et al assessed the results of robotic esophagectomy via three approaches: Ivor Lewis (n = 45), McKeown (n = 25), and transhiatal (n = 6). [40] No intraoperative complications and no conversions were noted. Postoperative morbidity was 41%, and the incidence of anastomotic leakage was 13%. Reintervention was required in eight of the 76 patients. The authors found all of the procedures to be associated with the expected perioperative morbidity and to yield excellent pathologic outcomes.
The MIRO trial compared the long-term 5-year outcomes (eg, overall survival [OS], disease-free survival [DFS], and pattern of disease recurrence) of hybrid MIE (HMIE) with those of open esophagectomy in 207 patients (age range, 18-75 y; 175 men, 32 women) with resectable cancer of the middle or lower third of the esophagus. [41] No difference in long-term survival was found between the two groups: 5-year OS was 59% with HMIE vs 47% with open esophagectomy, and 5-year DFS was 52% with HMIE vs 44% with open esophagectomy. There were no statistically significant differences in recurrence rate or location between the two groups.

- Dziodzio T, Kröll D, Denecke C, Öllinger R, Pratschke J, Biebl M. Minimally invasive esophagectomy. Multimed Man Cardiothorac Surg. 2021 Apr 9. 2021:[QxMD MEDLINE Link]. [Full Text].
- Darwish MB, Nagatomo K, Jackson T, Cho E, Osman H, Jeyarajah DR. Minimally Invasive Esophagectomy for Achieving R0. JSLS. 2020 Oct-Dec. 24 (4):[QxMD MEDLINE Link]. [Full Text].
- Chang AC, Ji H, Birkmeyer NJ, Orringer MB, Birkmeyer JD. Outcomes after transhiatal and transthoracic esophagectomy for cancer. Ann Thorac Surg. 2008 Feb. 85 (2):424-9. [QxMD MEDLINE Link].
- Connors RC, Reuben BC, Neumayer LA, Bull DA. Comparing outcomes after transthoracic and transhiatal esophagectomy: a 5-year prospective cohort of 17,395 patients. J Am Coll Surg. 2007 Dec. 205 (6):735-40. [QxMD MEDLINE Link].
- Brewer LA 3rd. History of surgery of the esophagus. Am J Surg. 1980 Jun. 139 (6):730-43. [QxMD MEDLINE Link].
- Dubecz A, Schwartz SI. Franz John A. Torek. Ann Thorac Surg. 2008 Apr. 85 (4):1497-9. [QxMD MEDLINE Link].
- Vierra M. Minimally invasive surgery. Annu Rev Med. 1995. 46:147-58. [QxMD MEDLINE Link].
- Dallemagne B, Weerts JM, Jehaes C, Markiewicz S, Lombard R. Laparoscopic Nissen fundoplication: preliminary report. Surg Laparosc Endosc. 1991 Sep. 1 (3):138-43. [QxMD MEDLINE Link].
- Sarkaria IS, Schaheen L, Luketich JD. Video-assisted and robotic esophagectomy. LoCicero J III, Feins RH, Colson YL, Rocco G, eds. Shields' General Thoracic Surgery. 8th ed. Philadelphia: Wolters Kluwer; 2019. Vol 2: 1704-14.
- Dallemagne B, Weerts JM, Jehaes C, Markiewicz S, Bona S, Hosselet JL, et al. Case report: subtotal oesophagectomy by thoracoscopy and laparoscopy. Minim Invasive Ther. 1992. 1 (2):183-5. [Full Text].
- DePaula AL, Hashiba K, Ferreira EA, de Paula RA, Grecco E. Laparoscopic transhiatal esophagectomy with esophagogastroplasty. Surg Laparosc Endosc. 1995 Feb. 5 (1):1-5. [QxMD MEDLINE Link].
- Watson DI, Davies N, Jamieson GG. Totally endoscopic Ivor Lewis esophagectomy. Surg Endosc. 1999 Mar. 13 (3):293-7. [QxMD MEDLINE Link].
- Matsunaga T, Shishido Y, Saito H, Sakano Y, Makinoya M, Miyauchi W, et al. Impact of Robot-Assisted Minimally Invasive Esophagectomy for Esophageal Cancer: A Propensity Score-Matched Short-Term Analysis. Yonago Acta Med. 2023 May. 66 (2):239-245. [QxMD MEDLINE Link]. [Full Text].
- Watanabe M, Kuriyama K, Terayama M, Okamura A, Kanamori J, Imamura Y. Robotic-Assisted Esophagectomy: Current Situation and Future Perspectives. Ann Thorac Cardiovasc Surg. 2023 May 23. [QxMD MEDLINE Link]. [Full Text].
- Okusanya OT, Sarkaria IS, Hess NR, Nason KS, Sanchez MV, Levy RM, et al. Robotic assisted minimally invasive esophagectomy (RAMIE): the University of Pittsburgh Medical Center initial experience. Ann Cardiothorac Surg. 2017 Mar. 6 (2):179-185. [QxMD MEDLINE Link]. [Full Text].
- Lin MW, Lee JM. Robotic-assisted minimally invasive esophagectomy: is it advantageous over thoracoscopic esophagectomy?. J Thorac Dis. 2017 Mar. 9 (3):490-491. [QxMD MEDLINE Link]. [Full Text].
- Zheng C, Li XK, Zhang C, Zhou H, Ji SG, Zhong JH, et al. Comparison of short-term clinical outcomes between robot-assisted minimally invasive esophagectomy and video-assisted minimally invasive esophagectomy: a systematic review and meta-analysis. J Thorac Dis. 2021 Feb. 13 (2):708-719. [QxMD MEDLINE Link]. [Full Text].
- Aslan S, Tiryaki GG, Pashayev J, Cetinkaya C, Durusoy AF, Ermerak NO, et al. Uniportal video-assisted thoracoscopic surgery esophagectomy outcomes in 40 consecutive patients. Interdiscip Cardiovasc Thorac Surg. 2023 May 4. 36 (5):[QxMD MEDLINE Link].
- Shah R, Jobe BA. Open versus minimally invasive esophagectomy: what is the best approach? Minimally invasive esophagectomy. J Gastrointest Surg. 2011 Sep. 15 (9):1503-5. [QxMD MEDLINE Link].
- Luketich JD, Fernando HC, Christie NA, Buenaventura PO, Keenan RJ, Ikramuddin S, et al. Outcomes after minimally invasive esophagomyotomy. Ann Thorac Surg. 2001 Dec. 72 (6):1909-12; discussion 1912-3. [QxMD MEDLINE Link].
- Pierre AF, Luketich JD, Fernando HC, Christie NA, Buenaventura PO, Litle VR, et al. Results of laparoscopic repair of giant paraesophageal hernias: 200 consecutive patients. Ann Thorac Surg. 2002 Dec. 74 (6):1909-15; discussion 1915-6. [QxMD MEDLINE Link].
- Krasna MJ, Jiao X. Thoracoscopic and laparoscopic staging for esophageal cancer. Semin Thorac Cardiovasc Surg. 2000 Jul. 12 (3):186-94. [QxMD MEDLINE Link].
- Luketich JD, Schauer P, Landreneau R, Nguyen N, Urso K, Ferson P, et al. Minimally invasive surgical staging is superior to endoscopic ultrasound in detecting lymph node metastases in esophageal cancer. J Thorac Cardiovasc Surg. 1997 Nov. 114 (5):817-21; discussion 821-3. [QxMD MEDLINE Link].
- Pennathur A, Zhang J, Chen H, Luketich JD. The "best operation" for esophageal cancer?. Ann Thorac Surg. 2010 Jun. 89 (6):S2163-7. [QxMD MEDLINE Link].
- Sihag S, Kosinski AS, Gaissert HA, Wright CD, Schipper PH. Minimally Invasive Versus Open Esophagectomy for Esophageal Cancer: A Comparison of Early Surgical Outcomes From The Society of Thoracic Surgeons National Database. Ann Thorac Surg. 2016 Apr. 101 (4):1281-8; discussion 1288-9. [QxMD MEDLINE Link].
- Capovilla G, Uzun E, Scarton A, Moletta L, Hadzijusufovic E, Provenzano L, et al. Minimally invasive Ivor Lewis esophagectomy in the elderly patient: a multicenter retrospective matched-cohort study. Front Oncol. 2023. 13:1104109. [QxMD MEDLINE Link]. [Full Text].
- Macke RA, Campos GM. Esophagectomy. Chen H, ed. Illustrative Handbook of General Surgery. 2nd ed. New York: Springer; 2016. 265-98.
- Litle VR, Luketich JD. Minimally invasive esophagectomy. CTSNet. Available at https://www.ctsnet.org/article/minimally-invasive-esophagectomy-0. August 19, 2008; Accessed: June 2, 2023.
- Luketich JD, Alvelo-Rivera M, Buenaventura PO, Christie NA, McCaughan JS, Litle VR, et al. Minimally invasive esophagectomy: outcomes in 222 patients. Ann Surg. 2003 Oct. 238 (4):486-94; discussion 494-5. [QxMD MEDLINE Link].
- Luketich JD, Pennathur A, Awais O, Levy RM, Keeley S, Shende M, et al. Outcomes after minimally invasive esophagectomy: review of over 1000 patients. Ann Surg. 2012 Jul. 256 (1):95-103. [QxMD MEDLINE Link].
- Traverso LW, Shinchi H, Low DE. Useful benchmarks to evaluate outcomes after esophagectomy and pancreaticoduodenectomy. Am J Surg. 2004 May. 187 (5):604-8. [QxMD MEDLINE Link].
- Nguyen NT, Roberts P, Follette DM, Rivers R, Wolfe BM. Thoracoscopic and laparoscopic esophagectomy for benign and malignant disease: lessons learned from 46 consecutive procedures. J Am Coll Surg. 2003 Dec. 197 (6):902-13. [QxMD MEDLINE Link].
- Perry Y, Fernando HC, Buenaventura PO, Christie NA, Luketich JD. Minimally invasive esophagectomy in the elderly. JSLS. 2002 Oct-Dec. 6 (4):299-304. [QxMD MEDLINE Link]. [Full Text].
- Wang H, Shen Y, Feng M, Zhang Y, Jiang W, Xu S, et al. Outcomes, quality of life, and survival after esophagectomy for squamous cell carcinoma: A propensity score-matched comparison of operative approaches. J Thorac Cardiovasc Surg. 2015 Apr. 149 (4):1006-1015.e4. [QxMD MEDLINE Link].
- van der Sluis PC, Ruurda JP, Verhage RJ, van der Horst S, Haverkamp L, Siersema PD, et al. Oncologic Long-Term Results of Robot-Assisted Minimally Invasive Thoraco-Laparoscopic Esophagectomy with Two-Field Lymphadenectomy for Esophageal Cancer. Ann Surg Oncol. 2015 Dec. 22 Suppl 3:S1350-6. [QxMD MEDLINE Link].
- van der Sluis PC, van der Horst S, May AM, Schippers C, Brosens LAA, Joore HCA, et al. Robot-assisted Minimally Invasive Thoracolaparoscopic Esophagectomy Versus Open Transthoracic Esophagectomy for Resectable Esophageal Cancer: A Randomized Controlled Trial. Ann Surg. 2019 Apr. 269 (4):621-630. [QxMD MEDLINE Link].
- Luketich JD, Pennathur A, Franchetti Y, Catalano PJ, Swanson S, Sugarbaker DJ, et al. Minimally invasive esophagectomy: results of a prospective phase II multicenter trial--the Eastern Cooperative Oncology Group (E2202) study. Ann Surg. 2015 Apr. 261 (4):702-7. [QxMD MEDLINE Link].
- Sakamoto T, Fujiogi M, Matsui H, Fushimi K, Yasunaga H. Comparing Perioperative Mortality and Morbidity of Minimally Invasive Esophagectomy Versus Open Esophagectomy for Esophageal Cancer: A Nationwide Retrospective Analysis. Ann Surg. 2021 Aug 1. 274 (2):324-330. [QxMD MEDLINE Link].
- Deng J, Su Q, Ren Z, Wen J, Xue Z, Zhang L, et al. Comparison of short-term outcomes between minimally invasive McKeown and Ivor Lewis esophagectomy for esophageal or junctional cancer: a systematic review and meta-analysis. Onco Targets Ther. 2018. 11:6057-6069. [QxMD MEDLINE Link]. [Full Text].
- Guerra F, Gia E, Minuzzo A, Tribuzi A, Di Marino M, Coratti A. Robotic esophagectomy: results from a tertiary care Italian center. Updates Surg. 2021 Jun. 73 (3):839-845. [QxMD MEDLINE Link].
- Nuytens F, Dabakuyo-Yonli TS, Meunier B, Gagnière J, Collet D, D'Journo XB, et al. Five-Year Survival Outcomes of Hybrid Minimally Invasive Esophagectomy in Esophageal Cancer: Results of the MIRO Randomized Clinical Trial. JAMA Surg. 2021 Apr 1. 156 (4):323-332. [QxMD MEDLINE Link].
- Michelet P, D'Journo XB, Roch A, Doddoli C, Marin V, Papazian L, et al. Protective ventilation influences systemic inflammation after esophagectomy: a randomized controlled study. Anesthesiology. 2006 Nov. 105 (5):911-9. [QxMD MEDLINE Link].
- Ng JM. Update on anesthetic management for esophagectomy. Curr Opin Anaesthesiol. 2011 Feb. 24 (1):37-43. [QxMD MEDLINE Link].
- Ng JM. Perioperative anesthetic management for esophagectomy. Anesthesiol Clin. 2008 Jun. 26 (2):293-304, vi. [QxMD MEDLINE Link].
- Bartels H, Stein HJ, Siewert JR. [Early extubation vs. late extubation after esophagus resection: a randomized, prospective study]. Langenbecks Arch Chir Suppl Kongressbd. 1998. 115:1074-6. [QxMD MEDLINE Link].
- Cense HA, Lagarde SM, de Jong K, Omloo JM, Busch OR, Henny ChP, et al. Association of no epidural analgesia with postoperative morbidity and mortality after transthoracic esophageal cancer resection. J Am Coll Surg. 2006 Mar. 202 (3):395-400. [QxMD MEDLINE Link].
- Kent MS, Schuchert M, Fernando H, Luketich JD. Minimally invasive esophagectomy: state of the art. Dis Esophagus. 2006. 19 (3):137-45. [QxMD MEDLINE Link].
- Luketich JD, Nguyen NT, Weigel T, Ferson P, Keenan R, Schauer P. Minimally invasive approach to esophagectomy. JSLS. 1998 Jul-Sep. 2 (3):243-7. [QxMD MEDLINE Link].
- Wee JO, Schaheen LW, Luketich JD. Minimally invasive esophagectomy. Sugarbaker DJ, Bueno R, Burt BM, Groth SS, Loor G, Wolf AS, eds. Sugarbaker's Adult Chest Surgery. 3rd ed. New York: McGraw-Hill; 2020. 132-41.
- Benzoni E, Bresadola V, Terrosu G, Uzzau A, Cedolini C, Intini S, et al. Minimally invasive esophagectomy: a comparative study of transhiatal laparoscopic approach versus laparoscopic right transthoracic esophagectomy. Surg Laparosc Endosc Percutan Tech. 2008 Apr. 18 (2):178-87. [QxMD MEDLINE Link].
- Palanivelu C, Prakash A, Parthasarathi R, Senthilkumar R, Senthilnathan PR, Rajapandian S. Laparoscopic esophagogastrectomy without thoracic or cervical access for adenocarcinoma of the gastroesophageal junction: an Indian experience from a tertiary center. Surg Endosc. 2007 Jan. 21 (1):16-20. [QxMD MEDLINE Link].
- Avital S, Zundel N, Szomstein S, Rosenthal R. Laparoscopic transhiatal esophagectomy for esophageal cancer. Am J Surg. 2005 Jul. 190 (1):69-74. [QxMD MEDLINE Link].
- Jobe BA, Kim CY, Minjarez RC, O'Rourke R, Chang EY, Hunter JG. Simplifying minimally invasive transhiatal esophagectomy with the inversion approach: Lessons learned from the first 20 cases. Arch Surg. 2006 Sep. 141 (9):857-65; discussion 865-6. [QxMD MEDLINE Link].
- Hoppo T, Jobe BA, Hunter JG. Minimally invasive esophagectomy: the evolution and technique of minimally invasive surgery for esophageal cancer. World J Surg. 2011 Jul. 35 (7):1454-63. [QxMD MEDLINE Link].
- Levy RM, Wizorek J, Shende M, Luketich JD. Laparoscopic and thoracoscopic esophagectomy. Adv Surg. 2010. 44:101-16. [QxMD MEDLINE Link].
- Orringer MB, Marshall B, Iannettoni MD. Transhiatal esophagectomy for treatment of benign and malignant esophageal disease. World J Surg. 2001 Feb. 25 (2):196-203. [QxMD MEDLINE Link].
- Swanson SJ, Batirel HF, Bueno R, Jaklitsch MT, Lukanich JM, Allred E, et al. Transthoracic esophagectomy with radical mediastinal and abdominal lymph node dissection and cervical esophagogastrostomy for esophageal carcinoma. Ann Thorac Surg. 2001 Dec. 72 (6):1918-24; discussion 1924-5. [QxMD MEDLINE Link].
- Bailey SH, Bull DA, Harpole DH, Rentz JJ, Neumayer LA, Pappas TN, et al. Outcomes after esophagectomy: a ten-year prospective cohort. Ann Thorac Surg. 2003 Jan. 75 (1):217-22; discussion 222. [QxMD MEDLINE Link].
- Feingold PL, Bryan D, Kuckelman J, Kennedy-Shaffer L, Wang V, Deeb A, et al. Anastomotic Stricture After Minimally Invasive Esophagectomy. Ann Thorac Surg. 2023 May 24. [QxMD MEDLINE Link].
- Brown AM, Pucci MJ, Berger AC, Tatarian T, Evans NR 3rd, Rosato EL, et al. A standardized comparison of peri-operative complications after minimally invasive esophagectomy: Ivor Lewis versus McKeown. Surg Endosc. 2018 Jan. 32 (1):204-211. [QxMD MEDLINE Link].
Author
Coauthor(s)
Allison J McLarty, MD Associate Professor of Surgery, The School of Medicine at Stony Brook University Medical Center; Associate Program Director, Department of Surgery, Codirector of Ventricular Assist Device Program, Stony Brook University Medical Center; Director of Thoracic Surgery, Northport Veterans Affairs Medical Center
Allison J McLarty, MD is a member of the following medical societies: American College of Surgeons, American Heart Association, American Medical Association, Medical Society of the State of New York, Society of Thoracic Surgeons
Disclosure: Nothing to disclose.
Chief Editor
Kurt E Roberts, MD Associate Professor, Division of Bariatric and Minimally Invasive Surgery, Department of Surgery, Yale University School of Medicine; Chair, Department of Surgery, Saint Francis Hospital, Trinity Health of New England Medical Group
Kurt E Roberts, MD is a member of the following medical societies: American College of Surgeons, Society of American Gastrointestinal and Endoscopic Surgeons, Society of Laparoscopic and Robotic Surgeons
Disclosure: Nothing to disclose.
Additional Contributors