Anal Canal Anatomy: Gross Anatomy, Tissue, Nerves, and Muscles, Pathophysiologic Variants (original) (raw)
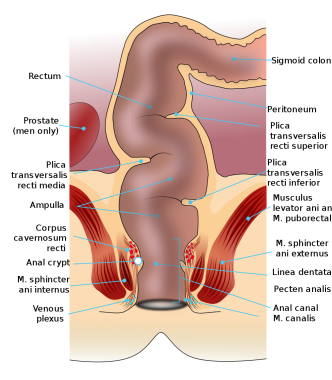
The anal canal is the most terminal part of the lower gastrointestinal (GI) tract/large intestine, which lies between the anal verge (anal orifice, anus) in the perineum below and the rectum above. It extends from the pelvic diaphragm to the anal orifice. [1] The description in this topic is from below upwards as that is how this region is usually examined in clinical practice. Images depicting the anal canal can be seen below. [2, 3]
Rectum and anal canal anatomy. Courtesy of Wikimedia Commons (https://commons.wikimedia.org/wiki/File:Rectum\_anatomy\_de\_01.svg; author Armin Kübelbeck).
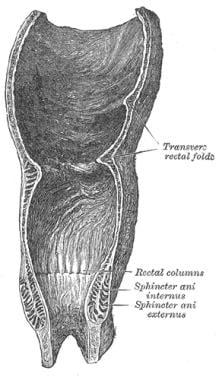
Coronal section of rectum and anal canal.
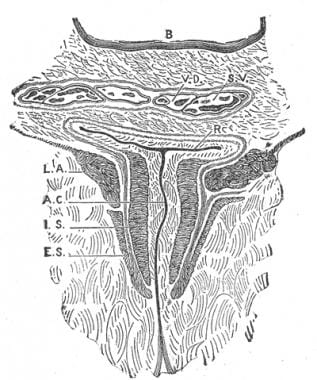
Coronal section through the anal canal.
The pigmented, keratinized perianal skin of the buttocks (around the anal verge) has skin appendages (e.g., hair, sweat glands, sebaceous glands), but the anal canal skin above the anal verge, which is also pigmented and keratinized, does not have skin appendages. [4]
The demarcation between the rectum above and the anal canal below is the anorectal ring or anorectal flexure, where the puborectalis muscle forms a sling around the posterior aspect of the anorectal junction, kinking it anteriorly.
The anal canal is completely extraperitoneal. The length of the anal canal is about 4 cm (range, 3-5 cm), with two thirds of this being above the pectinate line (also known as the dentate line) and one third below the pectinate line.
The epithelium of the anal canal between the anal verge below and the pectinate line above is variously described as anal mucosa or anal skin. The author believes that it should be called anal skin (anoderm) as it looks like (pigmented) skin, is sensitive like skin (why a fissure-in-ano is very painful), and is keratinized (but does not have skin appendages).
The pectinate line is the site of transition of the proctodeum below and the postallantoic gut above. It is a scalloped demarcation formed by the anal valves (transverse folds of mucosa) at the inferiormost ends of the anal columns. Anal glands open above the anal valves into the anal sinuses. The pectinate line is not seen on inspection in clinical practice, but under anesthesia, the anal canal descends, and the pectinate line can be seen on slight retraction of the anal canal skin.
The anal canal just above the pectinate line for about 1-2 cm is called the anal pecten or transitional zone. Above this transitional zone, the anal canal is lined with columnar epithelium (which is insensitive to cutting). Anal columns (of Morgagni) are 6-10 longitudinal (vertical) mucosal folds in the upper part of the anal canal.
At the bottom of these columns are anal sinuses or crypts, into which open the anal glands and anal papillae. Infection of the anal glands is likely the initial event in the causation of perianal abscess and fistula-in-ano. Three of these columns (left lateral, right posterior, and right anterior, at 3-, 7-, and 11-o'clock positions in the supine position) are prominent; they are called anal cushions and contain branches and tributaries of the superior rectal (hemorrhoidal) artery and vein. When prominent, veins in these cushions form the internal hemorrhoids.
The anorectal junction or anorectal ring is situated about 5 cm from the anus. At the anorectal flexure or angle, the anorectal junction is pulled anterosuperiorly by the puborectal sling to continue below as the anal canal.
Levator ani and coccygeus muscles form the pelvic diaphragm. Lateral to the anal canal are the pyramidal ischioanal (ischiorectal) fossae (one on either side), below the pelvic diaphragm and above the perianal skin. The paired ischioanal fossae communicate with each other behind the anal canal. The anterior relations of the anal canal are the seminal vesicles, prostate, and urethra in males and the cervix and vagina with perineal body in between in females. In front of (anterior to) the anal canal is the rectovesical fascia (of Denonvilliers) and behind (posterior) is the presacral endopelvic fascia (of Waldeyer), under which lies a rich presacral plexus of veins. Posterior to the anal canal lies the tip of the coccyx (joined to it by the anococcygeal ligament) and lower sacrum.
The anal canal is surrounded by several perianal spaces: subcutaneous, submucosal, intersphincteric, ischioanal (rectal), and pelvirectal.
Blood supply and lymphatics
The blood supply and lymphatics of the anal canal can be divided based on the pectinate (dentate) line as the anatomical landmark. [1, 5]
Arterial supply:
- The anal canal above the pectinate line is supplied by the terminal branches of the superior rectal (hemorrhoidal) artery, which is the terminal branch of the inferior mesenteric artery.
- The middle rectal artery (a branch of the internal iliac artery) and the inferior rectal artery (a branch of the internal pudendal artery) supply blood to the lower anal canal.
This vascular differentiation plays a role in various clinical conditions, particularly those affecting the anal and rectal regions, such as hemorrhoids. [1, 5]
Venous drainage:
Above the pectinate line, venous blood drains into the portal venous system via the internal hemorrhoidal (rectal) plexus. This connection is clinically significant as conditions such as liver cirrhosis may cause portal hypertension that can result in the formation of rectal varices. The anal canal is therefore an important area of portosystemic venous connection (the other being the esophagogastric junction). [1, 5]
Beneath the pectinate line lies the external hemorrhoidal plexus of veins, which drains into systemic veins. Venous drainage occurs through the inferior rectal veins into the internal pudendal veins, which then drain into the internal iliac vein. This pathway connects to systemic circulation, highlighting an important portosystemic anastomosis within the anal canal. [1, 5]
Lymphatic drainage:
- Lymphatics from the anal canal drain into the superficial inguinal group of lymph nodes.
- Lymphatic drainage from the anal canal above the pectinate line primarily flows into the internal iliac lymph nodes or inferior mesenteric lymph node. Below this line, the lymph drains into the superficial inguinal lymph nodes. [1, 5]
Summary [1, 5] (Open Table in a new window)
| | Above Pectinate Line | Below Pectinate Line | | | --------------------------- | ------------------------------------------------------------ | ------------------------------------------------------------ | | Arterial Supply | Superior rectal artery (from the inferior mesenteric artery) | Inferior rectal arteries (from the internal pudendal artery) | | Venous Drainage | Superior rectal vein to inferior mesenteric vein | Inferior rectal vein to internal pudendal vein | | Nerve Supply | Autonomic innervation via inferior hypogastric plexus | Somatic innervation via pudendal nerve | | Lymphatics | Drains into the perirectal nodes | Drains into the inguinal nodes |
Nerve supply:
The dual nerve supply allows for distinct physiological responses in each segment of the anal canal. For example, while the upper portion is sensitive mainly to stretch due to its autonomic innervation, the lower portion is responsive to pain and temperature due to somatic innervation. [1, 5]
Physiology
Anorectal sphincter tone can be assessed during digital rectal examinations (DREs) when the patient is asked to squeeze the examining finger.
Perianal ultrasound can also be used as an additional tool to visualize the anal canal and sphincter muscles, offering a more comfortable and reproducible alternative to DRE. [6, 7]
Anorectal manometry measures the pressures: resting and squeezing. Anorectal manometry remains the gold standard for quantitatively measuring anorectal pressures. This technique is crucial for evaluating anorectal function, particularly in cases of fecal incontinence. Manometry provides detailed information on the sphincter tone and rectal sensitivity, aiding in the diagnosis and management of various anorectal disorders. [6, 7]
High-resolution anorectal manometry (HR-ARM) utilizes multiple closely spaced sensors to provide a detailed pressure map along the anal canal. HR-ARM records pressures at rest, during contraction maneuvers, and during simulated defecation. This technology allows for improved assessment of rectoanal coordination and can identify functional disorders such as fecal incontinence and constipation more effectively than conventional manometry. [6, 7]
Three-dimensional high-definition ARM can also offer even greater detail by depicting circumferential pressure distribution around the anal canal, enhancing and improving diagnostic capabilities. [6, 7]
Embryology
The anal canal below the pectinate line develops from the proctodeum (ectoderm), while that above the pectinate line develops from the endoderm of the hindgut.
The formation of the anal canal follows the rupture of the cloacal membrane around the eighth week of development, separating the urogenital sinus from the anorectal canal. This separation is achieved by the growth of the urorectal septum. The pectinate line marks the transition between these two embryonic origins, influencing the vasculature, lymphatic drainage, and innervation. [6, 8, 9, 10]