Pneumocystis jiroveci Pneumonia (PJP): Overview of Pneumocystis jiroveci Pneumonia, Microbiology of Pneumocystis jiroveci Pneumonia, Pathophysiology and Etiology of Pneumocystis jiroveci Pneumonia (original) (raw)
Overview of Pneumocystis jiroveci Pneumonia
Overview of Pneumocystis jiroveci Pneumonia
Pneumocystis jiroveci pneumonia (PJP), formerly known as Pneumocystis carinii pneumonia (PCP), is the most common opportunistic infection in persons with HIV infection. [1]
Pneumocystis first came to attention as a cause of interstitial pneumonia in severely malnourished and premature infants during World War II in Central and Eastern Europe. [2] Before the 1980s, fewer than 100 cases of PJP were reported annually in the United States, occurring in patients who were immunosuppressed (eg, cancer patients receiving chemotherapy and solid-organ transplant recipients receiving immunosuppressants). In 1981, the Centers for Disease Control and Prevention reported PJP in 5 previously healthy homosexual men residing in the Los Angeles area.
P jiroveci is one of several organisms known to cause life-threatening opportunistic infections in patients with advanced HIV infection worldwide. Well over 100,000 cases of PJP were reported in the first decade of the HIV epidemic in the United States in people with no other cause for immunosuppression.
While officially classified as a fungal pneumonia, PJP does not respond to antifungal treatment. [1] Although a histopathologic demonstration of the organism is required for a definitive diagnosis (see Histologic Findings), treatment should not be delayed. [3] Treatment of PJP may be initiated before the workup is complete in severely ill high-risk patients. Treatment of PJP depends on the degree of illness at diagnosis, determined on the basis of the alveolar-arterial gradient. See the A-a Gradient calculator.
Antibiotics are primarily recommended for treatment of mild, moderate, or severe PJP. Trimethoprim-sulfamethoxazole (TMP-SMX) has been shown to be as effective as intravenous pentamidine and more effective than other alternative treatment regimens. [4] Corticosteroids are used as adjunctive initial therapy only in patients with HIV infection who have severe PJP. Preventive measures (eg, smoking cessation and chemoprophylaxis) can play an important role in disease management.
For other discussions on pneumonia, [5] see the following:

Microbiology of Pneumocystis jiroveci Pneumonia
Pneumocystis is a genus of unicellular fungi found in the respiratory tracts of many mammals and humans. Distinct genomic variability exists between host-specific members of the genus. The organism was first described in 1909 by Chagas and then a few years later by Delanöes, who ultimately named the organism in honor of Dr. Carini after isolating it from infected rats. Years later, Dr. Otto Jirovec and his group isolated the organism from humans, and the organism responsible for PJP was renamed after him. [6, 7]
The taxonomic classification of the Pneumocystis genus was debated for some time. [1, 2] It initially was mistaken for a trypanosome and then later for a protozoan. In the 1980s, biochemical analysis of the nucleic acid composition of Pneumocystis rRNA and mitochondrial DNA identified the organism as a unicellular fungus rather than a protozoan. Subsequent genomic sequence analysis of multiple genes including elongation factor 3, a component of fungi protein synthesis not found in protozoa, further supported this notion.
The organism is found in 3 distinct morphologic stages, as follows:
- The trophozoite (trophic form), in which it often exists in clusters
- The sporozoite (precystic form)
- The cyst, which contains several intracystic bodies (spores)

Pathophysiology and Etiology of Pneumocystis jiroveci Pneumonia
Pneumocystis organisms commonly are found in the lungs of healthy individuals. Most children are believed to have been exposed to the organism by age 3 or 4 years, and its occurrence is worldwide. [8]
Transmission of Pneumocystis
Animal studies have suggested that Pneumocystis organisms are communicable; airborne transmission has been reported. Human evidence of this is provided by molecular analysis of Pneumocystis isolates obtained from groups of patients involved in hospital outbreaks. [9, 10]
Further evidence of human transmission has been found in cases of recurrent pneumonia in which the genotype of Pneumocystis organisms in the same person differed in prior episodes. Despite this, barrier precautions are not required for patients hospitalized with P jiroveci pneumonia (PJP) except to protect other patients with depressed immunity.
Development of PJP
Disease occurs when both cellular immunity and humoral immunity are defective. Once inhaled, the trophic form of Pneumocystis organisms attach to the alveoli. Multiple host immune defects allow for uncontrolled replication of Pneumocystis organisms and development of illness. Activated alveolar macrophages without CD4+ cells are unable to eradicate Pneumocystis organisms. Increased alveolar-capillary permeability is visible on electron microscopy.
Physiologic changes include the following [1, 3] :
- Hypoxemia with an increased alveolar-arterial oxygen gradient
- Impaired diffusing capacity
- Changes in total lung capacity and vital capacity
There have been reports of PJP occurring as part of the immune reconstitution syndrome. [11, 12, 13]
Risk factors for PJP
PJP is caused by infection with P jiroveci. The following groups are at risk for PJP [14, 15, 16, 3] :
- Persons with HIV infection whose CD4+ cells fall below 200/µL and who are not receiving PJP prophylaxis (In addition, in patients with HIV infection, findings of other opportunistic infections [eg, oral thrush] increases the risk of PJP, regardless of CD4+ count.) [17, 18]
- Persons receiving long-term immunosuppressive regimens for connective-tissue disorders, vasculitides, or solid-organ transplantation (eg, heart, lung, liver, kidney) [19]
- Persons with hematologic and nonhematologic malignancies, including solid tumors and lymphomas [20]
- Persons with severe malnutrition

Epidemiology of Pneumocystis jiroveci Pneumonia
Before the widespread use of prophylaxis for P jiroveci pneumonia (PJP), the frequency of Pneumocystis infection in lung transplant patients alone was as high as 88%. With the routine use of prophylaxis, PJP is very rare in solid-organ transplant patients and has significantly decreased in patients infected with HIV. [3]
Prior to the widespread use of highly active antiretroviral therapy (HAART), PJP occurred in 70-80% of patients with HIV infection. The frequency of PJP is decreasing with the use of PJP prophylaxis and HAART. PJP remains the most common opportunistic infection in patients with HIV infection. Patients with HIV infection are more prone to PJP recurrence than patients not infected with HIV.
In developing regions of the world, the prevalence of PJP once was thought to be much lower, [21] but studies have shown that the lower reported incidence likely reflects a failure to accurately diagnose PJP. An accurate diagnosis requires access to modern medical care, which is not available worldwide.
The frequency of documented Pneumocystis infection is increasing in Africa, with Pneumocystis organisms found in up to 80% of infants with pneumonia who have HIV infection. In sub-Saharan Africa, tuberculosis is a common co-infection in persons with PJP. [22]

Prognosis of Pneumocystis jiroveci Pneumonia
In patients with HIV infection, PJP once carried a mortality rate of 20-40%, depending on disease severity at presentation. Mortality rates of 10-20% are reported. PJP is still a major cause of death in patients with AIDS in the United States. [1, 3, 23]
In persons without HIV infection, PJP carries a worse prognosis [24] ; this has not changed significantly since the late 1900s. Mortality rates of 30-50% have been documented in several large studies.
The prognosis of PJP is worse in patients who present with concurrent pulmonary disease, in patients who develop pneumothorax, and in patients who require mechanical ventilation. [3] The higher mortality rate likely is a result of delayed diagnosis and delayed initiation of appropriate treatment.

Clinical Presentation of Pneumocystis jiroveci Pneumonia
Patient history
The symptoms of P jiroveci pneumonia (PJP) are nonspecific. PJP in patients with HIV infection tends to run a more subacute indolent course and to present much later, often after several weeks of symptoms, compared with PJP associated with other immunocompromising conditions. [25] Symptoms of PJP include the following [3] :
- Progressive exertional dyspnea (95%)
- Fever (>80%)
- Nonproductive cough (95%)
- Chest discomfort
- Weight loss
- Chills
- Hemoptysis (rare)
Physical examination
The physical examination findings of PJP are nonspecific and include the following:
- Tachypnea
- Fever
- Tachycardia
- Pulmonary symptoms: Pulmonary examination may reveal mild crackles and rhonchi but may yield normal findings in up to half of patients.
Additional findings in children with severe disease include cyanosis, nasal flaring, and intercostal retractions.
Extrapulmonary manifestations
Although Pneumocystis infection rarely causes extrapulmonary manifestations, such findings may be present in patients receiving aerosolized pentamidine for prophylaxis or in patients with advanced HIV infection who are not taking any prophylaxis. [3] They also may occur in the absence of lung involvement.
Based on most well-documented findings, Pneumocystis infection may present in almost any organ system, as follows:
- Central nervous system
- Bone marrow (may have necrosis with resultant pancytopenia)
- Lymphadenopathy
- Eyes (may have retinal cotton-wool spots)
- Thyroid (may present as a rapidly enlarging thyroid mass)
- Gastrointestinal tract
Complications
A pathophysiologic process similar to acute respiratory distress syndrome (ARDS) may occur in patients with severe PJP. [26] These patients may require intubation. This greatly diminishes the prognosis.

Differential Diagnosis of Pneumocystis jiroveci Pneumonia
The differential diagnoses of P jiroveci pneumonia (PJP) include the following conditions [27] :

Laboratory Studies
A lactic dehydrogenase (LDH) study is performed as part of the initial workup. [28] LDH levels are usually elevated (>220 U/L) in patients with P jiroveci pneumonia (PJP). They are elevated in 90% of patients with PJP who are infected with HIV. The study has a high sensitivity (78%-100%); its specificity is much lower because other disease processes can result in an elevated LDH level. [3]
LDH levels appear to reflect the degree of lung injury. They should decline with successful treatment. Consistently elevated LDH levels during treatment may indicate therapy failure and a worse prognosis.
Quantitative PCR for pneumocystis may be useful in distinguishing between colonization and active infection. [29, 3] Polymerase chain reaction (PCR) of respiratory fluid, in particular bronchoalveolar lavage (BAL), is increasingly used to make the diagnosis of PCP in both patients with and without HIV, and several clinical laboratories offer this test. A disadvantage is that PCR cannot distinguish between colonization and disease. [30]
Sputum P jirovecii PCR testing may be a viable alternative to invasive testing. [3] This could be a more timely method for sample collection and would provide a safer alternative to bronchoscopic evaluation in patients who already have respiratory failure. Further studies comparing the sensitivity, specificity, and positive and negative predictive values for each sample type are needed. [31]
β-D-Glucan (BDG) is a cell wall component found in various fungi, including Candida, Aspergillus, and Pneumocystis, but not in Zygomycetes. A meta-analysis of 13 studies has demonstrated that BDG is a sensitive test for detecting Pneumocystis jirovecii pneumonia (PJP). A negative serum BDG result can effectively exclude PJP in patients with HIV; however, in non-HIV cases, results should be interpreted alongside clinical and radiologic findings. [32] Elevated plasma levels of 1-3-beta-D-glucan, which is part of the cell wall of P jirovecii, have been observed in patients with HIV and PCP. In a study involving 282 HIV patients, those diagnosed with PCP exhibited significantly higher median BDG levels compared to those without the disease. Furthermore, blood (1→3)-β-D-glucan levels show a strong association with HIV-related Pneumocystis pneumonia. In specific clinical contexts, this test may offer greater sensitivity than induced sputum examinations, potentially reducing the need for bronchoscopy and empirical treatment for PCP. [33, 3]

Chest Radiography
Chest radiography should be obtained in any immunocompromised patient with fever and/or respiratory signs or symptoms. [34, 3] The chest radiographic findings may be normal in patients with early mild disease. Diffuse bilateral infiltrates extending from the perihilar region are visible in most patients with P jiroveci pneumonia (PJP). Less-common findings include patchy asymmetric infiltrates, pneumothorax, and pneumatoceles. A radiographically normal chest radiograph has also been described. Pleural effusions and intrathoracic adenopathy are rare.
Pneumothorax may develop in patients using aerosolized pentamidine. Apical disease also may be found in patients using aerosolized pentamidine for prophylaxis, as shown in the image below.
Chest radiograph demonstrating diffuse bilateral infiltrates in a patient with Pneumocystis jiroveci pneumonia.
Go to Imaging Pneumocystis Carinii Pneumonia for complete information on this topic.

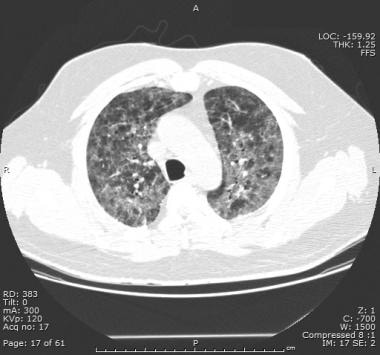
Computed Tomography
High-resolution computed tomography (HRCT) scanning of chest is helpful when the chest radiography findings are equivocal. HRCT yields a high sensitivity for P jiroveci pneumonia (PJP) in patients with HIV infection.
The typical appearance is patchy areas of ground-glass attenuation with a background of interlobular septal thickening. Negative (normal or unchanged) CT scan findings alone do not rule out PJP (see the image below).
CT scan of chest, with classic patchy areas of ground-glass attenuation.
Go to Imaging Pneumocystis Carinii Pneumonia for complete information on this topic.

Other Noninvasive Tests
Pulmonary function tests
Pulmonary function tests should be obtained as part of the initial noninvasive workup in patients with suspected P jiroveci pneumonia (PJP). Results may demonstrate a decreased diffusion capacity of carbon monoxide (DLCO) of less than 75% predicted. Decreased DLCO has a high sensitivity (89%-100%) but poor specificity (53%). PJP is unlikely if DLCO is normal.
When combined with normal or unchanged HRCT findings, pulmonary function tests may be used to identify patients unlikely to have PJP; such patients may be managed with observation alone.
Pulse oximetry
Pulse oximetry on room air should be measured in all patients. The oxygen saturation should be measured both at rest and with exertion. If any hypoxemia is found (O2 saturation < 90%), then an arterial blood gas (ABG) level should be obtained to evaluate the need for possible adjunctive corticosteroids.
HIV testing
The diagnosis of PJP should prompt consideration for HIV testing and other immune evaluations of lymphocytes and antibodies. If HIV testing is performed, appropriate pretest and posttest counseling guidelines must be followed.
Laboratory testing
Serum LDH may be elevated in patients with PJP.

Sputum Induction
If P jiroveci pneumonia (PJP) is strongly suspected, obtain a sputum sample by sputum induction for histopathologic testing. Pneumocystis organisms are frequently found in sputum induced by inhalation of a hypertonic saline solution. Sputum induction is the quickest and least-invasive method for definitively diagnosing PJP. [35] Expectorated sputum has a very low sensitivity and should not be submitted for diagnosis. Pneumocystis antigen detection assays on sputum may also be helpful but may have a low sensitivity.
The sensitivity of sputum induction varies widely (< 50% to >90%) and depends on proficiency in using the technique and the experience of the laboratory. Specificity is high (99-100%). This study may be less sensitive in patients without HIV infection, as the immunodeficiency caused by HIV infection typically leads to a greater alveolar load of Pneumocystis organisms. It may also be less sensitive in patients receiving aerosolized pentamidine for prophylaxis.

Invasive Procedures
Bronchoalveolar lavage
Bronchoalveolar lavage (BAL) is the most common invasive procedure used to diagnose P jiroveci pneumonia (PJP). It has a diagnostic yield that exceeds 90% (and may be higher if multiple lobes are sampled). [36] BAL yields a lower sensitivity in patients receiving aerosolized pentamidine, in which case a transbronchial biopsy may be performed in conjunction with BAL. [37]
Obtain BAL if PJP is strongly suspected and the induced sputum sample findings are negative. BAL may be used in patients who are unable to cooperate with an induced sputum sample (eg, because of altered mental status). BAL may be less useful in cases of suspected PJP relapse. Consultation with a pulmonologist is required for BAL.
Lung biopsy
Open lung biopsy is the most invasive procedure and yields 100% sensitivity and specificity because it provides the greatest amount of tissue for diagnosis. However, this procedure is reserved for rare cases when bronchoscopy findings are nondiagnostic.

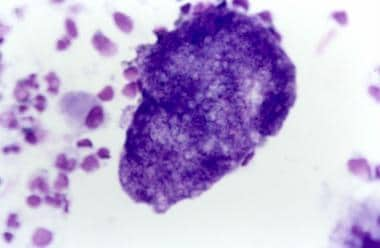
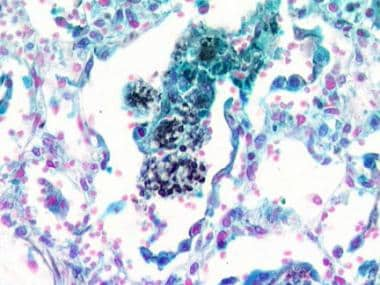
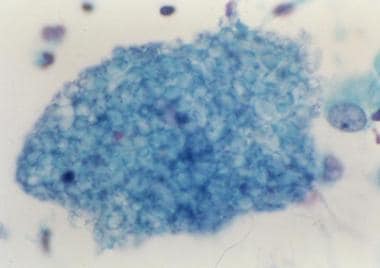
Histologic Findings
Because clinical and radiologic findings are not specific for PJP and because P jiroveci cannot be grown in vitro, histopathologic demonstration is necessary before a definitive diagnosis is established. The following are the staining techniques available for respiratory tract secretions.
Crystal violet, Giemsa, Diff-Quik, and Wright stain are used to detect both the trophozoite and cyst forms but not the cyst wall. Diff-Quik stain demonstrating P jiroveci is seen in the image below.
Diff-Quik stain demonstrating Pneumocystis jiroveci.
Methenamine silver, toluidine blue, and Gram-Weigert selectively stain the wall of Pneumocystis cysts. Silver Gram stain showing P jiroveci is seen in the image below .
Silver Gram stain showing Pneumocystis jiroveci.
Papanicolaou smear may demonstrate a foamy-appearing eosinophilic material surrounding Pneumocystis organisms (as seen in the image below).
Papanicolaou smear of Pneumocystis jiroveci.
Some facilities prefer to use direct immunofluorescence using monoclonal antibodies to detect Pneumocystis organisms because it may be more sensitive than histologic staining.

Treatment of PJP - General Considerations
While officially classified as a fungal pneumonia, P jiroveci pneumonia (PJP) does not respond to antifungal treatment. [1, 23] The treatment of choice is TMP-SMX, with second-line agents including pentamidine, dapsone (often in combination with pyrimethamine), or atovaquone. However, there are a few reports of successful caspofungin administration in PJP. Echinocandins such as caspofungin may be active against Pneumocystis based on their activity against the inclusion of (1-3)beta-D glucan into the fungal cell wall, but clinical data are lacking. Case reports suggest it may be worthy of consideration as a salvage treatment option in nonresponsive cases, and further research clearly is warranted. [38]
Although a histopathologic demonstration of the organism is required for a definitive diagnosis (see Histologic Findings), treatment should not be delayed. Treatment of PJP may be initiated before the workup is complete in severely ill high-risk patients.
Appropriate histopathologic testing may still be used to confirm a diagnosis of PJP after treatment is initiated. Endotracheal tube aspirates from severely ill patients on mechanical ventilation may be submitted for diagnosis. Pneumocystis organisms persist in the host for days to weeks after therapy is started, allowing time for completion of the appropriate workup.
Treatment of PJP depends on the degree of illness at diagnosis. Degree of illness is determined based on the alveolar-arterial gradient: mild (< 35 mm Hg), moderate/severe (35-45 mm Hg), or severe (>45 mm Hg). [1] Severe disease is also indicated by a room air partial pressure of oxygen lower than 70 mm Hg. Treatment of extrapulmonary manifestations of PJP is the same as that for other pneumonias.
In patients without HIV infection, response to treatment should begin within 4-5 days. In patients infected with HIV, the treatment response typically takes longer but should occur within the first 8 days. If no response occurs within the expected time, an appropriate alternative regimen should be used. Adding additional PJP medications to a current regimen only increases the risk for adverse drug reactions without improving the likelihood of a good outcome. Up to 10% of mild-to-moderate PJP cases fail to respond to antibiotic treatment because of lack of drug efficacy.
All patients who require corticosteroids should be admitted to the hospital because of the risk for progressive respiratory compromise.
Because of increasing evidence of possible human transmission (see Pathophysiology and Etiology of PJP), [39] the CDC Hospital Infection Control Practice Advisory Committee has recommended that patients with PJP not have direct contact with other immunocompromised patients.

Antibiotic Therapy
Antibiotics are primarily recommended for treatment of mild, moderate, or severe P jiroveci pneumonia (PJP). TMP-SMX has been shown to be as effective as intravenous pentamidine and more effective than other alternative treatment regimens. [4, 40] The parenteral route may be considered in patients who present with serious illness or in those with gastrointestinal side effects.
Thomas et al have reported that a lower dose of TMP-SMX (10 mg/kg/d) is effective for PJP associated with HIV infection and carries fewer side effects, [41] but this should not yet be taken as a recommendation. [3]
TMP-SMX is the preferred initial therapy during pregnancy according to consensus guidelines. The patient’s neonatologist should be informed if the medication is used near delivery because of potential for hyperbilirubinemia and kernicterus. For the treatment of infections that are resistant to TMP-SMX, the combination of clindamycin and primaquine is likely to be more effective than intravenous pentamidine. [42, 43]
Atovaquone 750 mg by mouth twice daily may be given as an alternative treatment, but its use is contraindicated in pregnancy.
The recommended duration of treatment for PJP is 21 days in patients with HIV infection and 14 days in all other patients. Patients infected with HIV tend to have a higher organism burden and respond to treatment slower than patients without HIV infection and therefore require a longer duration of therapy.

Adjunctive Corticosteroid Therapy
Corticosteroids are used as adjunctive initial therapy only in patients with HIV infection who have severe P jiroveci pneumonia (PJP) as defined by a room air arterial oxygen pressure of less than 70 mm Hg or an arterial-alveolar O2 gradient that exceeds 35 mm Hg. Adjunctive steroids are not recommended in patients without HIV infection.
Microbial degradation and clearance may trigger further inflammation, which can provoke a severe inflammatory response in the lungs that often worsens after therapy is begun. Adjunctive corticosteroid therapy can blunt this inflammatory response, reduce deterioration of oxygenation, and reduce the incidence of respiratory failure. [44, 45]

Further Outpatient Care
Arranging close medical follow-up with a primary care provider upon hospital discharge is essential to monitor resolution of disease and to initiate prophylactic medication (see Prevention of PJP).
Oral therapy with TMP-SMX has been shown to be very effective in the outpatient setting. However, oral therapy should be considered only in patients with mild-to-moderate P jiroveci pneumonia (PJP) who have reliable outpatient follow-up care.

Prevention of PJP
Smoking cessation
Smoking cessation is strongly recommended in patients with HIV infection, as studies have shown that, in addition to the common deleterious effects of tobacco use, smokers are at an increased risk of P jiroveci pneumonia (PJP) and have a more complicated treatment course. [46]
Chemoprophylaxis in patients with HIV Infection
Two types of outpatient chemoprophylactic therapies exist. Primary prophylaxis is used in immunocompromised patients without a history of PJP. Secondary prophylaxis is used in patients with a prior bout of PJP.
An expert panel overseen by the US Public Health Service and Infectious Disease Society of America has published guidelines on prophylaxis against P jiroveci pneumonia (PJP) in adult and pediatric patients with HIV infection. Chemoprophylaxis is recommended for the following groups:
- Adults, adolescents, and pregnant patients with a CD4 count of less than 200/µL, oropharyngeal candidiasis, unexplained fever exceeding 100°F (37.7° C) for more than 2 weeks, and a prior episode of PJP regardless of CD4 count should receive prophylaxis.
- Children born to mothers with HIV infection should receive prophylaxis with TMP-SMX beginning at age 4-6 weeks, if HIV infection has not been "presumptively ruled out" by two negative HIV DNA PCRs (typically one at birth, with another after age 4 weeks). Many HIV-exposed newborns in the developed world with access to this kind of testing therefore may never need to start PJP prophylaxis.
- Children born to mothers with HIV infection who have had 4 negative HIV DNA PCRs (with one after at least age 4 months) or a negative HIV antibody test after age 6 months can be definitively said to be HIV-uninfected, and PJP prophylaxis can be safely discontinued.
- All children who are determined to be HIV-infected should receive prophylaxis through the first year of life, then as determined by age-specific CD4 levels.
- Prophylaxis may be discontinued in patients with HIV infection whose CD4 count exceeds 200/µL for 3 consecutive months while on HAART. Prophylaxis should be restarted if the CD4 count drops below 200/µL. Prophylaxis should be continued for life in patients who developed PJP while their CD4 level exceeded 200/µL.
One study suggests that discontinuation of prophylaxis may be safe in patients with HIV and CD4 counts of 101-200 cells/μL and suppressed viral load. [47]
Chemoprophylaxis in patients without HIV infection
Unlike in patients with HIV infection, no specific PJP prophylaxis guidelines exist for immunocompromised patients without HIV infection. In general, chemoprophylaxis should be considered in any of the following patients:
- Patients with an underlying primary immune deficiency (eg, severe combined immunodeficiency or hypogammaglobulinemia)
- Patients with a persistent CD4 count less than 200/µL
- Solid organ transplant recipients
- Hematopoietic stem cell transplant (HSCT) recipients, with prophylaxis administered (1) for 6 months after engraftment months or (2) for more than 6 months after HSCT in those who are still receiving immunosuppressive therapy (eg, prednisone, cyclosporine) or who have chronic graft versus host disease
- Patients receiving daily systemic corticosteroid therapy (at least 20 mg daily for at least 1 month)
- Patients with cancer, vasculitides, or collagen vascular disorders and others receiving cytotoxic or immunosuppressive treatments such as cyclosporine or the purine analogs fludarabine or cladribine
Chemoprophylactic regimens
TMP-SMX is the agent of choice for PJP prophylaxis in the absence of a contraindication. In patients who cannot tolerate TMP-SMX, other options include dapsone, dapsone plus pyrimethamine, atovaquone, and aerosolized pentamidine. Commonly used prophylactic regimens are discussed below.
For TMP-SMX, the normal dosage is one double-strength tablet (160 mg TMP to 800 mg SMX) daily. One single-strength tablet (80 mg TMP to 400 mg SMX) daily is also effective. Another alternative is one double-strength tablet 3 times per week. However, a daily-dosing regimen provides an additional benefit of cross protection against Toxoplasma gondii infection and other bacterial infections.
The use of TMP-SMX for long-term PJP prophylaxis does not seem to affect the rates of infection by drug-resistant organisms such as pneumococcus or Staphylococcus aureus. TMP-SMX resistance has been reported among some isolates of Pneumocystis. [48]
For dapsone, the dosage is 100 mg daily by mouth if it is administered alone. If dapsone is given with pyrimethamine (plus leucovorin), the dosage is 50 mg of dapsone daily by mouth with 50 mg of pyrimethamine weekly and 25 mg of leucovorin weekly. Dapsone with pyrimethamine (plus leucovorin) provides protection against T gondii infection, but not other bacterial infections.
For atovaquone, the dosage is 1500 mg by mouth once daily given with food. This agent has a low toxicity profile and is an alternative if the patient cannot tolerate TMP-SMX or dapsone. However, atovaquone is very expensive.
For aerosolized pentamidine, the normal dosage is 300 mg in 6 mL sterile water via Respirgard nebulizer every 4 weeks. This agent is better tolerated than dapsone or TMP-SMX. However, it is much more expensive and less effective than other prophylactic agents. Side effects include cough and bronchospasm. The potential for extrapulmonary Pneumocystis manifestations and apical lung disease exists. In addition, aerosolized pentamidine may diminish the diagnostic sensitivity of sputum induction and bronchoalveolar lavage.

- Sethi S. Pneumocystis jirovecii Pneumonia. Porter RE. The Merck Manual of Diagnosis and Therapy. Rahway, NJ: Merck & Co Inc; Reviewed/Revised February 2024. [Full Text].
- Stringer JR, Beard CB, Miller RF, Wakefield AE. A new name (Pneumocystis jiroveci) for Pneumocystis from humans. Emerg Infect Dis. 2002 Sep. 8 (9):891-6. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] NIH HIV.gov. Guidelines for the Prevention and Treatment of Opportunistic Infections in Adults and Adolescents With HIV: Pneumocystis Pneumonia. Clinical Info HIV.gov. Available at https://clinicalinfo.hiv.gov/en/guidelines/hiv-clinical-guidelines-adult-and-adolescent-opportunistic-infections/pneumocystis?view=full. September 16, 2024; Accessed: December 17, 2024.
- Safrin S, Finkelstein DM, Feinberg J, et al. Comparison of three regimens for treatment of mild to moderate Pneumocystis carinii pneumonia in patients with AIDS. A double-blind, randomized, trial of oral trimethoprim-sulfamethoxazole, dapsone-trimethoprim, and clindamycin-primaquine. ACTG 108 Study Group. Ann Intern Med. 1996 May 1. 124(9):792-802. [QxMD MEDLINE Link].
- Cunha BA. Pneumonia Essentials. 2nd ed. Royal Oak, Mich: Physicians Press; 2007.
- Cushion MT, Stringer JR. Has the name really been changed? It has for most researchers. Clin Infect Dis. 2005 Dec 15. 41(12):1756-8. [QxMD MEDLINE Link].
- Gigliotti F. Pneumocystis carinii: has the name really been changed?. Clin Infect Dis. 2005 Dec 15. 41(12):1752-5. [QxMD MEDLINE Link].
- Slogrove AL, Cotton MF, Esser MM. Severe Infections in HIV-Exposed Uninfected Infants: Clinical Evidence of Immunodeficiency. J Trop Pediatr. 2009 Jul 14. [QxMD MEDLINE Link].
- Schmoldt S, Schuhegger R, Wendler T, et al. Molecular evidence of nosocomial Pneumocystis jirovecii transmission among 16 patients after kidney transplantation. J Clin Microbiol. 2008 Mar. 46(3):966-71. [QxMD MEDLINE Link].
- de Boer MG, Bruijnesteijn van Coppenraet LE, Gaasbeek A, et al. An outbreak of Pneumocystis jiroveci pneumonia with 1 predominant genotype among renal transplant recipients: interhuman transmission or a common environmental source?. Clin Infect Dis. 2007 May 1. 44(9):1143-9. [QxMD MEDLINE Link].
- Mori S, Polatino S, Estrada-Y-Martin RM. Pneumocystis-associated organizing pneumonia as a manifestation of immune reconstitution inflammatory syndrome in an HIV-infected individual with a normal CD4+ T-cell count following antiretroviral therapy. Int J STD AIDS. 2009 Sep. 20(9):662-5. [QxMD MEDLINE Link].
- Kolditz M, Halank M, Bandt D, Spornraft-Ragaller P, Höffken G. Early recurrence of Pneumocystis jiroveci pneumonia in two HIV-infected patients: linking infection relapse and immune reconstitution syndrome. Respirology. 2009 Aug. 14(6):910-2. [QxMD MEDLINE Link].
- Reddy T, Bajwa R, Burke A. The IRIS paradox: Imaging findings in a case of PJP-IRIS. Respirol Case Rep. 2022 Sep. 10 (9):e01014. [QxMD MEDLINE Link]. [Full Text].
- Hui M, Kwok WT. Pneumocystis carinii pneumonia in Hong Kong: a 10 year retrospective study. J Med Microbiol. 2006 Jan. 55:85-8. [QxMD MEDLINE Link].
- Mori S, Cho I, Sugimoto M. A followup study of asymptomatic carriers of Pneumocystis jiroveci during immunosuppressive therapy for rheumatoid arthritis. J Rheumatol. 2009 Aug. 36(8):1600-5. [QxMD MEDLINE Link].
- Resnick IB, Averbuch D, Aker M, et al. Is Pneumocystis carinii pneumonia after stem cell transplantations a contagious disease?. Clin Transplant. 2005 Jun. 19(3):427-31. [QxMD MEDLINE Link].
- Byers DK, Decker CF. Unusual case of Pneumocystis jiroveci pneumonia during primary HIV infection. AIDS Read. 2008 Jun. 18(6):313-7. [QxMD MEDLINE Link].
- Sax P. HIV Essentials. Royal Oak, Mich: Physicians Press; 2007.
- Ritter ML, Pirofski L. Mycophenolate mofetil: effects on cellular immune subsets, infectious complications, and antimicrobial activity. Transpl Infect Dis. 2009 Aug. 11(4):290-7. [QxMD MEDLINE Link]. [Full Text].
- Barbounis V, Aperis G, Gambletsas E, et al. Pneumocystis carinii pneumonia in patients with solid tumors and lymphomas: predisposing factors and outcome. Anticancer Res. 2005 Jan-Feb. 25(1B):651-5. [QxMD MEDLINE Link].
- Abouya YL, Beaumel A, Lucas S, et al. Pneumocystis carinii pneumonia. An uncommon cause of death in African patients with acquired immunodeficiency syndrome. Am Rev Respir Dis. 1992 Mar. 145(3):617-20. [QxMD MEDLINE Link].
- Murray JF. Pulmonary complications of HIV-1 infection among adults living in Sub-Saharan Africa. Int J Tuberc Lung Dis. 2005 Aug. 9(8):826-35. [QxMD MEDLINE Link]. [Full Text].
- CDC. Pneumocystis Pneumonia Basics. US Centers for Disease Control and Prevention. Available at https://www.cdc.gov/pneumocystis-pneumonia/about. April 24, 2024; Accessed: December 17, 2024.
- Su YS, Lu JJ, Perng CL, Chang FY. Pneumocystis jirovecii pneumonia in patients with and without human immunodeficiency virus infection. J Microbiol Immunol Infect. 2008 Dec. 41(6):478-82. [QxMD MEDLINE Link].
- Fujii T, Nakamura T, Iwamoto A. Pneumocystis pneumonia in patients with HIV infection: clinical manifestations, laboratory findings, and radiological features. J Infect Chemother. 2007 Feb. 13(1):1-7. [QxMD MEDLINE Link].
- Festic E, Gajic O, Limper AH, et al. Acute respiratory failure due to pneumocystis pneumonia in patients without human immunodeficiency virus infection: outcome and associated features. Chest. 2005 Aug. 128(2):573-9. [QxMD MEDLINE Link].
- Cunha BA, Schoch PE, Berbari N. Cryptococcal vs Pneumocystis (carinii) jiroveci pneumonia (PCP): Clinical & Microbiology differential diagnsotic considerations. Infect Dis Pract. 2006. 30:514-517.
- Grover SA, Coupal L, Suissa S, et al. The clinical utility of serum lactate dehydrogenase in diagnosing pneumocystis carinii pneumonia among hospitalized AIDS patients. Clin Invest Med. 1992 Aug. 15(4):309-17. [QxMD MEDLINE Link].
- Fauchier T, Hasseine L, Gari-Toussaint M, Casanova V, Marty PM, Pomares C. Detection of Pneumocystis jirovecii by Quantitative PCR to Differentiate Colonization and Pneumonia in Immunocompromised HIV-Positive and HIV-Negative Patients. Journal of Clinical Microbiology. 2016 Jun. 54(6):1487-1494. [QxMD MEDLINE Link].
- Alanio A, Hauser PM, Lagrou K, et al. ECIL guidelines for the diagnosis of Pneumocystis jirovecii pneumonia in patients with haematological malignancies and stem cell transplant recipients. J Antimicrob Chemother. 2016 Sep. 71 (9):2386-96. [QxMD MEDLINE Link]. [Full Text].
- Pennington K,Wilson J, Limper AH, Escalante P. Positive Pneumocystis jirovecii Sputum PCR Results with Negative Bronchoscopic PCR Results in Suspected Pneumocystis Pneumonia. Canadian Respiratory Journal. 2018 April. 2018:1-5. [QxMD MEDLINE Link].
- Li WJ, Guo YL, Liu TJ, Wang K, Kong JL. Diagnosis of pneumocystis pneumonia using serum 1-3 -B-D Glucan:a bivariate mets-analysis and systematic review. J Thorac Dis. 2015 Dec. 7(12):2214-2225.
- Sax PE, Komarow L, Finkelman MA, Grant PM, Andersen J, Scully E, et al. Blood (1->3)-beta-D-glucan as a diagnostic test for HIV-related Pneumocystis jirovecii pneumonia. Clin Infect Dis. 2011 Jul 15. 53 (2):197-202. [QxMD MEDLINE Link]. [Full Text].
- DeLorenzo LJ, Huang CT, Maguire GP, et al. Roentgenographic patterns of Pneumocystis carinii pneumonia in 104 patients with AIDS. Chest. 1987 Mar. 91(3):323-7. [QxMD MEDLINE Link].
- Bigby TD, Margolskee D, Curtis JL, et al. The usefulness of induced sputum in the diagnosis of Pneumocystis carinii pneumonia in patients with the acquired immunodeficiency syndrome. Am Rev Respir Dis. 1986 Apr. 133(4):515-8. [QxMD MEDLINE Link].
- Bigby TD. Diagnosis of Pneumocystis carinii pneumonia. How invasive?. Chest. 1994 Mar. 105(3):650-2. [QxMD MEDLINE Link].
- Broaddus C, Dake MD, Stulbarg MS, et al. Bronchoalveolar lavage and transbronchial biopsy for the diagnosis of pulmonary infections in the acquired immunodeficiency syndrome. Ann Intern Med. 1985 Jun. 102(6):747-52. [QxMD MEDLINE Link].
- Ceballos ME, Ortega M, Andresen M, Wozniak A, García P, Balcells ME. Successful treatment with echinocandin in an HIV-infected individual failing first-line therapy for Pneumocystis jirovecii pneumonia. AIDS. 2011 Nov 13. 25(17):2192-3. [QxMD MEDLINE Link].
- Gianella S, Haeberli L, Joos B, Ledergerber B, Wüthrich RP, Weber R, et al. Molecular evidence of interhuman transmission in an outbreak of Pneumocystis jirovecii pneumonia among renal transplant recipients. Transpl Infect Dis. 2009 Sep 9. [QxMD MEDLINE Link].
- Estrada S, García-Campos F, Calderón R, Delgado E, Bengoa R, Enciso C. Pneumocystis jiroveci (carinii) pneumonia following a second infusion of infliximab in a patient with ulcerative colitis. Inflamm Bowel Dis. 2009 Feb. 15(2):315-6. [QxMD MEDLINE Link].
- Thomas M, Rupali P, Woodhouse A, Ellis-Pegler R. Good outcome with trimethoprim 10 mg/kg/day-sulfamethoxazole 50 mg/kg/day for Pneumocystis jirovecii pneumonia in HIV infected patients. Scand J Infect Dis. 2009 Aug 17. 1-7. [QxMD MEDLINE Link].
- Smego RA Jr, Nagar S, Maloba B, et al. A meta-analysis of salvage therapy for Pneumocystis carinii pneumonia. Arch Intern Med. 2001 Jun 25. 161(12):1529-33. [QxMD MEDLINE Link]. [Full Text].
- Benfield T, Atzori C, Miller RF, et al. Second-line salvage treatment of AIDS-associated Pneumocystis jirovecii pneumonia: a case series and systematic review. J Acquir Immune Defic Syndr. 2008 May 1. 48(1):63-7. [QxMD MEDLINE Link].
- Bozzette SA. The use of corticosteroids in Pneumocystis carinii pneumonia. J Infect Dis. 1990 Dec. 162(6):1365-9. [QxMD MEDLINE Link].
- Bozzette SA, Sattler FR, Chiu J, et al. A controlled trial of early adjunctive treatment with corticosteroids for Pneumocystis carinii pneumonia in the acquired immunodeficiency syndrome. California Collaborative Treatment Group. N Engl J Med. 1990 Nov 22. 323(21):1451-7. [QxMD MEDLINE Link].
- Miguez-Burbano MJ, Ashkin D, Rodriguez A, et al. Increased risk of Pneumocystis carinii and community-acquired pneumonia with tobacco use in HIV disease. Int J Infect Dis. 2005 Jul. 9(4):208-17. [QxMD MEDLINE Link].
- Opportunistic Infections Project Team of the Collaboration of Observational HIV Epidemiological Research. Is it safe to discontinue primary Pneumocystis jiroveci pneumonia prophylaxis in patients with virologically suppressed HIV infection and a CD4 cell count Clin Infect Dis. 2010 Sep 1. 51(5):611-9. [QxMD MEDLINE Link].
- Sibanda EL, Weller IV, Hakim JG, Cowan FM. Does trimethoprim-sulfamethoxazole prophylaxis for HIV induce bacterial resistance to other antibiotic classes? Results of a systematic review. Clin Infect Dis. 2011 May. 52(9):1184-94. [QxMD MEDLINE Link]. [Full Text].
- Diff-Quik stain demonstrating Pneumocystis jiroveci.
- Silver Gram stain showing Pneumocystis jiroveci.
- Papanicolaou smear of Pneumocystis jiroveci.
- Chest radiograph demonstrating diffuse bilateral infiltrates in a patient with Pneumocystis jiroveci pneumonia.
- CT scan of chest, with classic patchy areas of ground-glass attenuation.


Author
Shelley A Gilroy, MD, FACP, FIDSA Associate Professor of Medicine, Infectious Disease and HIV Medicine, Albany Medical College; Associate Chief of Staff for Education/DEO, Lead Physician for HIV Medicine, Division of Infectious Diseases, Albany Stratton VA Medical Center
Shelley A Gilroy, MD, FACP, FIDSA is a member of the following medical societies: American College of Physicians, American Medical Association, Infectious Diseases Society of America
Disclosure: Nothing to disclose.
Specialty Editor Board
Francisco Talavera, PharmD, PhD Adjunct Assistant Professor, University of Nebraska Medical Center College of Pharmacy; Editor-in-Chief, Medscape Drug Reference
Disclosure: Received salary from Medscape for employment. for: Medscape.
Chief Editor
Pranatharthi Haran Chandrasekar, MBBS, MD Professor, Chief of Infectious Disease, Department of Internal Medicine, Wayne State University School of Medicine
Pranatharthi Haran Chandrasekar, MBBS, MD is a member of the following medical societies: American College of Physicians, American Society for Microbiology, International Immunocompromised Host Society, Infectious Diseases Society of America
Disclosure: Nothing to disclose.
Additional Contributors
Klaus-Dieter Lessnau, MD, FCCP Former Clinical Associate Professor of Medicine, New York University School of Medicine; Medical Director, Pulmonary Physiology Laboratory, Director of Research in Pulmonary Medicine, Department of Medicine, Section of Pulmonary Medicine, Lenox Hill Hospital
Klaus-Dieter Lessnau, MD, FCCP is a member of the following medical societies: American College of Chest Physicians, American College of Physicians, American Medical Association, American Thoracic Society, Society of Critical Care Medicine
Disclosure: Nothing to disclose.
Acknowledgements
Frederick Burton Rose, MD, FACP Professor, Department of Medicine, University Hospital Epidemiologist, State University of New York Upstate Medical University
Frederick Burton Rose, MD, FACP is a member of the following medical societies: American College of Physicians and Infectious Diseases Society of America
Disclosure: Nothing to disclose.
- Sections Pneumocystis jiroveci Pneumonia (PJP)
- Overview of Pneumocystis jiroveci Pneumonia
- Microbiology of Pneumocystis jiroveci Pneumonia
- Pathophysiology and Etiology of Pneumocystis jiroveci Pneumonia
- Epidemiology of Pneumocystis jiroveci Pneumonia
- Prognosis of Pneumocystis jiroveci Pneumonia
- Clinical Presentation of Pneumocystis jiroveci Pneumonia
- Differential Diagnosis of Pneumocystis jiroveci Pneumonia
- Laboratory Studies
- Chest Radiography
- Computed Tomography
- Other Noninvasive Tests
- Sputum Induction
- Invasive Procedures
- Histologic Findings
- Treatment of PJP - General Considerations
- Antibiotic Therapy
- Adjunctive Corticosteroid Therapy
- Further Outpatient Care
- Prevention of PJP
- Show All
- Media Gallery
- References