Aspiration Pneumonitis and Pneumonia: Overview of Aspiration Pneumonia, Predisposing Conditions for Aspiration Pneumonia, Pathophysiology of Aspiration Pneumonia (original) (raw)
Overview of Aspiration Pneumonia
Aspiration is defined as the inhalation of either oropharyngeal or gastric contents into the lower airways, that is, the act of taking foreign material into the lungs. This can cause a number of syndromes determined by the quantity and nature of the aspirated material, the frequency of aspiration, and the host factors that predispose the patient to aspiration and modify the response. [1]
There are four types of aspiration syndromes. Aspiration of gastric acid causes a chemical pneumonitis which has also been called Mendelson syndrome. [1] Aspiration of bacteria from oral and pharyngeal areas causes aspiration pneumonia. Aspiration of oil (eg, mineral oil or vegetable oil) causes exogenous lipoid pneumonia, an unusual form of pneumonia. Aspiration of a foreign body may cause an acute respiratory emergency and, in some cases, may predispose the patient to bacterial pneumonia. The pathophysiology, clinical presentation, treatment, and complications of each of these entities are different. [2]
This article concentrates on chemical pneumonitis and aspiration pneumonia.
Aspiration pneumonia is caused by bacteria that normally reside in the oral and nasal pharynx. Historically, aspiration pneumonia referred to an infection caused by less virulent bacteria, primarily oral pharyngeal anaerobes, after a large volume aspiration event. It is now recognized that many common community-acquired and hospital-acquired pneumonias result from small-volume aspiration of more virulent pathogens from the oral cavity or nasopharynx, such as Streptococcus pneumoniae, Haemophilus influenza, Staphylococcus aureus, and gram-negative bacteria.
For patient education information Lung Center, as well as Chemical Pneumonia, Bacterial Pneumonia and Bronchoscopy.
For more information, see the following:
The images below depict aspiration pneumonia in two different patients.
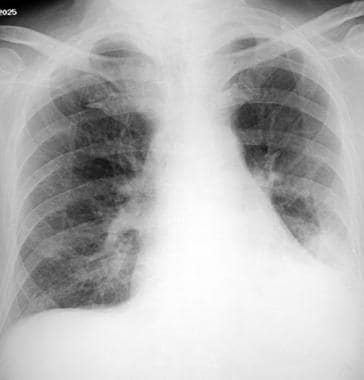
Aspiration pneumonia in an 84-year-old man in generally good health who had fever and cough. This posteroanterior radiograph demonstrates a left lower lobe opacity.
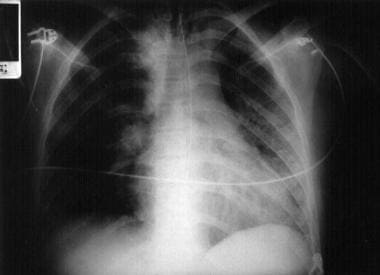
Chest radiograph of a patient with aspiration pneumonia of the left lung after a benzodiazepine overdose. The patient was probably positioned to the left at the moment of aspiration

Predisposing Conditions for Aspiration Pneumonia
Almost all patients who develop aspiration pneumonia have one or more of the predisposing conditions listed below. Although all the listed conditions predispose the patient to chemical pneumonitis, conditions that alter consciousness and periodontal disease specifically predispose the patient to bacterial pneumonia.
The basic pathogenesis of any aspiration event involves impaired swallowing, whether related to medications, anatomy, or neurologic dysfunction. A group that warrants special mention is head and neck cancer patients; they are considered a high-risk group. While likely acknowledged, the importance of the swallowing disorder is not well appreciated. Speech therapy can provide some amelioration of risk and is also under used in these patients.
Conditions associated with altered or reduced consciousness, including any condition that reduces a patient's gag reflex, ability to maintain an airway, or both, increase the risk of aspiration pneumonia or pneumonitis. Such conditions are as follows:
- Alcoholism
- Drug overdose
- Seizures
- Stroke
- Head trauma
- Intracranial mass lesion
Esophageal conditions associated with aspiration pneumonia include the following:
- Dysphagia: Oropharyngeal dysphagia has been found in the majority of elderly patients (mean age, 84 y). [3]
- Esophageal strictures
- Esophageal neoplasm
- Esophageal diverticula
- Tracheoesophageal fistula
- Gastroesophageal reflux disease
Neurologic disorders also predispose to aspiration pneumonia, such as the following:
- Multiple sclerosis
- Dementia
- Parkinson disease [4]
- Myasthenia gravis
- Pseudobulbar palsy
Aspiration pneumonia is also associated with the following mechanical conditions:
- Nasogastric tube [5]
- Endotracheal intubation
- Tracheostomy
- Upper gastrointestinal endoscopy
- Bronchoscopy
- Gastrostomy or postpyloric feeding tubes
Other types of associated conditions are as follows:
- Protracted vomiting
- Prolonged recumbency
- General deconditioning and debility
- Critical illness
- Down syndrome [6]

Pathophysiology of Aspiration Pneumonia
In aspiration pneumonia, an infiltrate develops in a patient at increased risk of oropharyngeal aspiration. This occurs when a patient inhales material from the oropharynx that is colonized by upper airway flora.
The risk of aspiration is indirectly related to the level of consciousness of the patient (ie, decreasing Glasgow Coma Scale [GCS; see the Glasgow Coma Scale calculator] score is related with increased risk of aspiration). [7] Aspiration of small amounts of material from the buccal cavity, particularly during sleep, is not an uncommon event. No disease ensues in healthy persons, because the aspirated material is cleared by mucociliary action and alveolar macrophages. The nature of the aspirated material, volume of the aspirated material, and state of the host defenses are three important determinants of the extent and severity of aspiration pneumonia.
Chemical pneumonitis
Chemical pneumonitis, also known as aspiration pneumonitis and Mendelson syndrome, is due to the parenchymal inflammatory reaction caused by a large volume of gastric contents independent of infection. In fact, aspiration of a massive amount of gastric contents can produce acute respiratory distress within one hour. This disease occurs in people with altered levels of consciousness resulting from seizures, cerebrovascular accident (CVA), central nervous system (CNS) mass lesions, drug intoxication or overdose, and head trauma.
The acidity of gastric contents results in chemical burns to the tracheobronchial tree involved in the aspiration. If the pH of the aspirated fluid is less than 2.5 and the volume of aspirate is greater than 0.3 mL/kg of body weight (20-25 mL in adults), it has a greater potential for causing chemical pneumonitis. The initial chemical burn is followed by an inflammatory cellular reaction fueled by the release of potent cytokines, particularly tumor necrosis factor (TNF)–alpha and interleukin (IL)–8.
Aspiration pneumonia
Aspiration pneumonia most commonly occurs in individuals with chronically impaired airway defense mechanisms, such as gag reflex, coughing, ciliary movement, and immune mechanisms, all of which aid in removing infectious material from the lower airways. Aspiration pneumonia can occur in the community or in a hospital or health care facility (ie, nosocomial). In both situations, anaerobic organisms alone or in combination with aerobic and/or microaerophilic organisms play a role in the infection. In anaerobic pneumonia, the pathogenesis is related to the large volume of aspirated anaerobes (eg, as in persons with poor dentition, poor oral care, and periodontal disease) and to host factors (eg, as in alcoholism) that suppress cough, mucociliary clearance, and phagocytic efficiency, both of which increase the bacterial burden of oropharyngeal secretions.
Nosocomial bacterial pneumonia caused by aspiration is common, and the major pathogens involved are hospital-acquired florae through oropharyngeal colonization (eg, enteric gram-negative bacteria, staphylococci). Selection and colonization of gram-negative organisms in the oropharynx, sedation, and intubation of the patient's airways are important pathogenetic factors in nosocomial pneumonia.
Because of the relative sterility of normal gastric contents, bacteria do not play an important role in the early stages of the disease. This does not hold true in patients with gastroparesis or small-bowel obstruction or in those using antacids (proton pump inhibitors [PPIs], histamine 2-receptor antagonists). Regardless of the bacterial load of the inoculum, bacterial superinfection may occur after the initial chemical injury.
Causative microorganisms
Initial bacteriologic studies into the causative organisms revealed the anaerobic species to be the predominant pathogens in community-acquired aspiration pneumonia. However, subsequent studies revealed that Streptococcus pneumoniae, Staphylococcus aureus, Haemophilus influenzae, and Enterobacteriaceae are the most common organisms. [1] In fact, in two studies of patients with acute, witnessed aspiration with protective specimen brush sampling and anaerobic culturing, no anaerobes were isolated. [8, 9] Moreover, hospital-acquired aspiration pneumonia is often caused by gram-negative organisms including Pseudomonas aeruginosa, particularly in intubated patients. [10]
While previous studies have suggested multidrug-resistant organisms, such as methicillin-resistant S aureus (MRSA), were more commonly found in those with healthcare-associated pneumonia (HCAP) versus community-acquired aspiration pneumonia (CAP), a 2014 meta-analysis of 24 studies found that patients previously classified as having HCAP (including nursing home–associated pneumonia) are not more likely to have multidrug-resistant infections than patients classified as having CAP. [11, 12] These studies demonstrated a limited role of anaerobic pathogens in both the community and nosocomial variants of the disease.

Epidemiology of Aspiration Pneumonia
A reliable estimate of incidence of chemical pneumonitis is not available. Few studies have been designed that distinguish between aspiration pneumonia and aspiration pneumonitis. Several studies suggest that 5-15% of the 4.5 million cases of community-acquired pneumonia (CAP) result from aspiration pneumonia. [1] A retrospective review found that the 30-day mortality rate from aspiration pneumonia is 21% overall and slightly higher in healthcare-associated aspiration pneumonia (29.7%). [11]
Nosocomial bacterial pneumonia is the second most likely cause of nosocomial infections, second only to urinary tract infection, and it is the leading cause of death from hospital-acquired infections. Approximately 10% of patients who are hospitalized after drug overdoses will have an aspiration pneumonitis.
Nosocomial bacterial pneumonia caused by aspiration is much more frequent in adults than in children, and males are more commonly affected than females. Predisposing factors (see Predisposing Conditions for Aspiration Pneumonia) are more common among elderly people. Thus, this population is more prone to develop aspiration pneumonia. [13] Comparative studies of bacterial pneumonia in patients from the community with those in a continuing care facility have demonstrated a 3-fold increase of this disease in residents of the continuing care facilities (the majority of them had neurologic disease with dysphagia). [14]

Presentation of Aspiration Pneumonia
The clinical presentation of both aspiration pneumonia and pneumonitis ranges from mildly ill and ambulating to critically ill, with signs and symptoms of septic shock and/or respiratory failure.
Host factors and chronic conditions that result in a decreased ability to protect one's airway include a previous cerebrovascular accident (CVA), a history of esophageal diseases including achalasia [15] or esophageal web, being a nursing home patient, and being chronically fed by feeding tube (nasogastric [NG] tube or gastric tube).
Physical examination findings vary depending on the severity of the disease, presence of complications, and host factors. Patients with aspiration pneumonitis secondary to seizure, head trauma, or drug overdose should be inspected for signs related to these processes. In addition to exhibiting signs associated with the underlying disease that led to their aspiration, patients with aspiration pneumonia or pneumonitis may demonstrate the following:
- Fever or hypothermia
- Tachypnea
- Tachycardia
- Decreased breath sounds
- Dullness to percussion over areas of consolidation
- Rales
- Egophony and pectoriloquy
- Decreased breath sounds
- Pleural friction rub
- Altered mental status
- Hypoxemia
- Hypotension (in septic shock)
Chemical pneumonitis
Patients with chemical pneumonitis may present with an acute onset or abrupt development of symptoms within a few minutes to two hours of the aspiration event, as well as respiratory distress and rapid breathing, audible wheezing, and cough with pink or frothy sputum.
Findings on physical examination may include tachypnea, tachycardia, fever, rales, wheezing, and possibly cyanosis.
Bacterial aspiration pneumonia
The presentation of bacterial aspiration pneumonia is similar to that of community-acquired pneumonia (CAP) and may include nonspecific symptoms including headache, nausea/vomiting, anorexia, and weight loss. The onset of illness may be subacute or insidious, with the symptoms manifesting in days to weeks when anaerobic organisms are the pathogens. The patient may also describe the following:
- Cough with purulent sputum
- Fever or chills
- Malaise, myalgias
- Rigors may be present or absent
- Shortness of breath, dyspnea on exertion
- Pleuritic chest pain
- Putrid expectoration (a clue to anaerobic bacterial pneumonia)
In hospital acquired aspiration pneumonia, the symptoms of cough and shortness of breath of may be more acute in onset than in CAP when aerobic organisms are the pathogens. Fever and rigors may be present.
Patients brought in after witnessed large-volume vomitus and subsequent aspiration pneumonitis may have a history consistent with an acute change in mental status, which may include seizure, alcohol abuse, drug overdose, and/or head trauma.
On physical examination, findings may include periodontal disease (primarily noted as gingivitis), bad breath, fever, bronchial breath sounds and rales over a consolidated posterior area.

Diagnosis in Aspiration Pneumonia
Clinicians must consider the diagnosis of aspiration pneumonia when a patient presents with risk factors and radiographic evidence of an infiltrate suggestive of aspiration pneumonia (see Predisposing Conditions for Aspiration Pneumonia). The location of the infiltrate on chest radiograph depends on the position of the patient when the aspiration occurred and is discussed further in the Chest Radiography section.
The laboratory studies obtained should be guided by the patient’s clinical presentation (see Presentation of Aspiration Pneumonia). Patients with signs or symptoms of sepsis or septic shock require further laboratory testing than those with uncomplicated aspiration syndromes.
Differentials
When evaluating a patient with suspected aspiration pneumonia, other considerations include necrotizing pneumonia, bronchopleural fistula, lung carcinoma, lung abscess, mycoses, and hypersensitivity pneumonitis. In children, bronchiolitis, croup or laryngotracheobronchitis, epiglottitis, asthma, reactive airway disease, respiratory distress syndrome, and foreign bodies should be considered. In addition, assess for the following conditions:

Arterial Blood Gas and Mixed Venous Gas Analysis
Arterial blood gas (ABG) analysis is used to assess oxygenation and pH status. ABG analysis adds information that may guide oxygen supplementation. The results of ABG analysis typically demonstrate acute hypoxemia in patients with chemical pneumonitis and normal to low partial pressure of carbon dioxide. A lactate level can be used as an early marker of severe sepsis or septic shock.
A mixed venous gas measurement should be obtained in any patient in whom septic shock is suspected. Decreased mixed venous oxygen saturation can be employed as a marker for septic shock.

Basic Metabolic Panel
Serum electrolyte, blood urea nitrogen (BUN), and creatinine levels can be used to assess fluid status and the need for intravenous hydration. This is especially important in patients who present with fever, vomiting, or diarrhea who may have significant fluid loss.
Serum BUN and creatinine levels can also be used to assess renal function in order to appropriately dose antibiotics. In addition, these values can be used to assess kidney injury in patients who present with sepsis or septic shock.

CBC Count With Differential
The complete blood cell (CBC) count may reveal an elevated white blood cell (WBC) count, increased neutrophils, anemia, and thrombocytosis in patients with bacterial pneumonia caused by anaerobic bacteria. An elevated WBC count and increased neutrophils may also be present in patients with chemical pneumonitis.

Sputum Gram Stain, Microscopy, and Culture
Although sputum culture and Gram stain are generally not helpful in the initial diagnosis or treatment, sputum Gram stain and microscopy often reveal a multitude of bacteria (eg, cocci, bacilli, coccobacillary forms, and fusiforms) in patients with bacterial pneumonia caused by anaerobic bacteria. In nosocomial bacterial aspiration pneumonia, sputum culture may be helpful in detecting gram-negative bacteria.
Findings on sputum culture may not isolate organisms when the major pathogens are anaerobes.

Blood Cultures
Blood cultures are used as a baseline screening for bacteremia. In uncomplicated pneumonia (no signs of sepsis or septic shock), blood cultures have a low yield and are not necessary for the initial management and treatment.

Chest Radiography
Radiographic evidence of aspiration pneumonia depends on the position of the patient when the aspiration occurred. [16] The right lower lung lobe is the most common site of infiltrate formation due to the larger caliber and more vertical orientation of the right mainstem bronchus. [16] Patients who aspirate while standing can have bilateral lower lung lobe infiltrates. Patients lying in the left lateral decubitus position are more likely to have left-sided infiltrates (see the following image). The right upper lobe may be involved particularly in alcoholics who aspirate while in the prone position.
Chest radiograph of a patient with aspiration pneumonia of the left lung after a benzodiazepine overdose. The patient was probably positioned to the left at the moment of aspiration
The presence of pleural effusion may indicate the need to perform thoracentesis to evaluate for possible empyema.
Chemical pneumonitis
Chest radiographic findings in patients with chemical pneumonitis are characterized by the presence of infiltrates, predominantly the alveolar type, in one or both lower lobes, or diffuse simulation of the appearance of pulmonary edema. Volume loss in any lobar area suggests obstruction (eg, by aspirated food particles or other foreign bodies) in the bronchus.
Bacterial pneumonia
Chest radiographic findings in patients with anaerobic bacterial pneumonia typically demonstrate an infiltrate with or without cavitation in one of the dependent segments of the lungs (ie, posterior segments of the upper lobes, superior segments of the lower lobes). Lucency within the infiltrate suggests a necrotizing pneumonia. Air-fluid levels within a circumscribed infiltrate indicate a lung abscess. Costophrenic angle blunting and the presence of a meniscus are signs of a parapneumonic pleural effusion.
More images in patients with aspiration pneumonia are provided below.
Aspiration pneumonia in an 84-year-old man in generally good health who had fever and cough. This posteroanterior radiograph demonstrates a left lower lobe opacity.
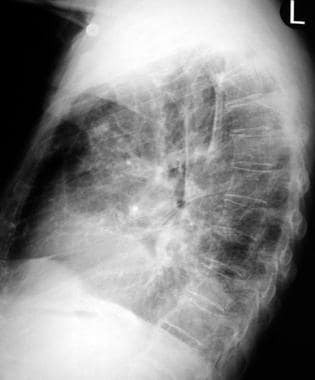
Lateral radiograph in an 84-year-old patient with aspiration pneumonia confirms the location of the abnormality in the left lower lobe.
Chest radiograph of a patient with massive aspiration pneumonia of the right lung.

Ultrasonography
Ultrasonography is helpful when confirming and locating pleural effusions. It is also an effective tool for initial diagnosis of aspiration pneumonia when chest radiography or computed tomography cannot be performed.
A systematic review and meta-analysis by Miura et al regarding the diagnostic accuracy of ultrasonography for detecting aspiraton in patients with dysphagia reported a sensitivity and specificity of 0.82 and 0.87, respectively. These results suggest that ultrasound may have a role as a bedside screening tool when aspiration is suspected. [36]

CT Scanning
Computed tomography (CT) scan of the chest is not required in the evaluation of all cases of suspected aspiration pneumonia. This imaging modality may be helpful in further characterizing pleural effusions and empyema and in detecting necrosis within infiltrates and cavitary lesions. CT scanning provides a better definition of the affected areas and is used to differentiate pulmonary abnormalities from pleural abnormalities.

Bronchoscopy
Bronchoscopy is indicated in patients with chemical pneumonia only when aspiration of a foreign body or food material is suspected. Bronchoscopy with protected brush and a protected catheter are used to retrieve pathogens in bacterial pneumonia and may be helpful in guiding antibiotic therapy particularly when coupled with quantitative culture techniques. This procedure is useful when ruling out the presence of an obstructing neoplasm in anaerobic bacterial pneumonia with lung abscess. However, bronchoscopy is not useful in the treatment of community-acquired aspiration pneumonia.

Pulmonary Artery Catheterization
Pulmonary artery catheter placement may be helpful to differentiate cardiac from noncardiac pulmonary edema in the setting of chemical pneumonitis. The hemodynamic monitoring catheter may be utilized to guide appropriate fluid management.

Thoracentesis
Thoracentesis, also known as pleural fluid aspiration, is a diagnostic and therapeutic procedure in which fluid (or air) is removed from between the visceral and parietal pleurae. Analysis of the specimen can help determine the underlying cause of the pleural effusion as well as relief of symptoms attributed to the presence of pleural fluid. A chest radiographs should be obtained before and after this procedure to detect complications from the thoracentesis.

Mechanical Ventilation
Mechanical ventilation may be required in severe cases of chemical pneumonitis that cause acute respiratory distress syndrome (ARDS) and in respiratory insufficiency due to aspiration pneumonia.

Chest Tube Placement
Chest tube placement may be employed to drain a complicated pleural effusion or an empyema.

Prehospital Management of Aspiration Pneumonia
Prehospital care should focus on stabilizing the patient's airway, breathing, and circulation. In patients found with signs of gastric aspiration (ie, vomitus) suctioning of the upper airway may remove a significant amount of aspirate or potential aspirate.
Intubation should be considered in any patient who is unable to protect his or her airway. The ability of paramedics to provide this intervention depends on the level of their training. [17] In addition, emergency medical technicians (EMTs) trained in intubation may choose to intubate patients with poor gag reflex to prevent aspiration.
Other measures include the following:
- Oxygen supplementation
- Cardiac monitoring and pulse oximetry
- Intravenous (IV) catheter placement and IV fluids, as indicated

Emergency Department Management
Emergency department care should start with stabilizing the patient's airway, breathing, and circulation. Oropharyngeal/tracheal suctioning may be indicated to further remove aspirate.
Reassess the need for intubation on a frequent basis depending on the patient’s oxygenation, the patient's mental status, signs of increased work of breathing, or impending respiratory failure.
Continue supplemental oxygenation as needed, as well as continue cardiac monitoring and pulse oximetry and provide continued supportive care with intravenous fluids and electrolyte replacement.

Inpatient Management
Patients with aspiration pneumonia, both chemical pneumonitis (chemical pneumonia) and bacterial pneumonia (bacterial pneumonia), need inpatient care for several reasons, including the acuity of illness, host factors, and the uncertain course and prognosis of aspiration pneumonia. [18]
Patients with severe hemodynamic compromise and/or persistent respiratory distress should be admitted to the intensive care unit (ICU). Intubated and ventilated patients must be transferred to a hospital with an ICU, as well as patients with signs or symptoms indicating severe sepsis or septic shock.
Patients with stable respiratory and hemodynamic status can be managed on a general-care floor.
Complications
Complications of aspiration include acute respiratory failure, acute respiratory distress syndrome (ARDS), [19] and bacterial pneumonia. Complications of bacterial pneumonia include parapneumonic effusion, empyema, lung abscess, and suprainfection. Bronchopleural fistula is also a complication.
Aspiration pneumonitis can rapidly progress to respiratory failure.
Consultations
Consult with a pulmonologist for bronchoscopy when airway obstruction due to a foreign body is suspected in patients with chemical pneumonitis or for ruling out a neoplasm in bacterial pneumonia cases.
Consult with an intensivist (critical care specialist) for severe chemical pneumonia if hypoxemia is severe and ventilatory support is anticipated. [20, 21]
Consult with a thoracic surgeon for bacterial pneumonia complicated by empyema (eg, closed-tube drainage, open-tube drainage, and decortication). In general, there is no role for surgical care, except in such cases with complications.
Consult with an infectious disease specialist for advice about proper antibiotic therapy.
Consult with a speech and language therapist for a comprehensive swallowing evaluation in patients with stroke or other risk factors for aspiration. These therapists can perform a bedside swallowing evaluation and, if abnormalities are found, can teach the patient compensatory strategies with soft or pureed foods and thickened liquids.

Overview of Antimicrobial Therapy
Antibiotics are indicated for aspiration pneumonia. However, for aspiration pneumonitis, early presumptive antibiotics (ie, prophylactic) are not recommended. This practice is believed to lead to the selection of more resistant organisms. [24] In addition, those patients with recent aspiration, fever, and leukocytosis should not be treated even in the presence of a pulmonary infiltrate due to the risk of development of resistant organisms. The following situations call for the use of antibiotics in managing pneumonitis:
- Administer antibiotics if the pneumonitis fails to resolve within 48 hours.
- Patients with small-bowel obstruction, particularly of the lower region, should receive antibiotics (bacteria may colonize the gastric contents).
- Antibiotics should be considered for patients on antacids due to the potential for gastric colonization with micro-organisms.
Antibiotic choice
For patients without a toxic appearance, the antibiotic chosen should cover typical community-acquired pathogens. Ceftriaxone plus azithromycin, levofloxacin, or moxifloxacin are appropriate choices. [25]
For patients with a toxic appearance or who were recently hospitalized, although community-acquired pathogens are still the most common, gram-negative bacteria including Pseudomonas aeruginosa and Klebsiella pneumoniae as well as methicillin-resistant S aureus (MRSA) must be covered. Piperacillin/tazobactam or imipenem/cilastatin plus vancomycin would be appropriate. Telavancin is indicated for hospital-acquired pneumonia, including ventilator-associated bacterial pneumonia caused by susceptible isolates of S aureus, including methicillin-susceptible and resistant isolates, when alternative treatments are not suitable. However, the nephrotoxic risk of this antibiotic must be taken into consideration when choosing an appropriate antimicrobial therapy. The presence of chronic aspiration risks, putrid discharge, indolent hospital course, and necrotizing pneumonia should raise the suspicion for anaerobic bacteria involvement and prompt consideration of adding clindamycin or metronidazole to the antibiotic regimen. [26] Ceftaroline is an alternative to vancomycin for the treatment of community-acquired pneumonia due to MRSA.
The treatment of individuals with chemical pneumonitis should include maintenance of the airways and clearance of secretions with tracheal suctioning, oxygen supplementation, and mechanical ventilation as necessary. If the patient is unable to maintain adequate oxygenation despite a high fraction of inspired oxygen, positive end-expiratory pressure (PEEP) should be considered. The routine use of corticosteroids is not recommended, because supporting studies, both animal and human, are not convincing of a favorable benefit-to-risk ratio. The early prophylactic (before evidence of a bacterial pneumonia) use of antibiotics in chemical pneumonitis, although widely practiced, is not supported by evidence.
Choosing antibiotics based on organisms cultured from sputum, tracheal aspirates, or aspirate obtained through a protected catheter by bronchoscopy rather than empirically is more appropriate. However, because the chemically injured bronchi and lungs are very susceptible to bacterial infection, it is reasonable to use antimicrobial agents based on the probability of the bacteria, the severity of the pneumonia, patient-related risk factors (eg, malnutrition, comorbid illnesses), intervention-related factors (eg, previous use of antibiotics, corticosteroids, cytotoxic agents, endotracheal tube), and the duration of hospitalization.
Initial treatment of patients with suspected aspiration pneumonia without risk factors for anaerobic involvement should mirror the treatment of community-acquired pneumonia: a third-generation cephalosporin with a macrolide or a fluoroquinolone alone. However, in severe pneumonia occurring many days after initiation of mechanical ventilation, the probability of resistant organisms, including P aeruginosa, Acinetobacter species, and MRSA, is increased, and, therefore, antibiotic treatment should be broader.
One study in a respiratory ICU of aspiration pneumonia found that patients were more likely to have gram-negative bacilli (57.8%), fungal infections (28.9%), and gram-positive cocci (13.3%); antibiotic resistance was common. [27] The choices of antimicrobial agents include respiratory fluoroquinolones, aminoglycoside with antipseudomonal penicillin, fourth-generation cephalosporins, imipenem, and vancomycin.

Corticosteroid Management
Historically corticosteroids have been used in the treatment of aspiration pneumonitis, but randomized control studies have been unable to demonstrate a benefit to using high-dose corticosteroids.
The role of supplementing corticosteroids in patients with hypotension from septic shock remains controversial. Previously, it was recommended that septic patients who were hypotensive despite fluid resuscitation and vasopressor support be screened for occult adrenal insufficiency. However, current guidelines recommend empiric therapy with stress-dose steroids in these patients who remain hypotensive despite fluids and pressors, to avoid delay in treatment of presumed adrenal insufficiency. [28]
The role of corticosteroids in patients hospitalized for community-acquired pneumonia (CAP) was evaluated in a 2015 meta-analysis of 13 randomized controlled trials, which found with high certainty that systemic corticosteroid steroid treatment reduced the duration of hospitalization by approximately 1 day and had a 5% absolute reduction in risk for mechanical ventilation. [29] The study also found that patients with severe pneumonia who received systemic corticosteroids had an apparent mortality benefit over patients with severe pneumonia who did not receive systemic corticosteroids, which may be related to the higher incidence of acute respiratory distress syndrome and the need for mechanical ventilation in patients with severe pneumonia. However, this evidence was rated moderate as the confidence interval crossed 1 and because of a possible subgroup effect. All patients who received corticosteroids had a higher incidence of hyperglycemia requiring treatment in this study. Thus, in immunocompetent patients hospitalized with severe CAP, systemic corticosteroids should be considered given the possible mortality benefit of systemic corticosteroid treatment in this subgroup of patients.
Corticosteroid use should be considered for conditions that occur as a result of the aspiration event, as opposed to treatment specifically for a chemical aspiration. These would include bronchospasm, acute respiratory distress syndrome, pneumonia, and septic shock.

Postdischarge Management
Patients who recover from chemical pneumonitis generally do not require additional outpatient care, except for adherence to measures to prevent further aspiration episodes.
Unlike chemical pneumonia, anaerobic bacterial infections complicated by empyema or lung abscess require prolonged antibiotic treatment; therefore, outpatient treatment is necessary. Patients can be discharged from the hospital after clinical improvement and stability (eg, no fever, no leucocytosis, resolution of hypoxemia) and radiographic improvement (eg, decreased infiltrate or cavity size, no pleural effusion).

Prevention of Aspiration Pneumonia
Good dental hygiene including regular visits to a dentist for professional cleanings have been shown effective in preventing aspiration pneumonia. This is particularly important in older adults, patients with Parkinson disease or dementia. [38, 39]
Position patients with altered consciousness in a semirecumbent position with the head of the bed at a 30-45° angle. This reduces the risk of aspiration leading to pneumonia. [17]
For patients with known swallowing dysfunction (eg, dysphagia and/or a poor gag reflex), helpful compensatory techniques to reduce aspiration include a soft diet reducing the bite size, nectar-thick or honey-thickened liquids, keeping the chin tucked and the head turned, and repeated swallowing. Although body positioning and changing the consistency of food/liquids are reasonable steps, their efficacy has not been proven in controlled trials. [30, 31] Feeding through a nasogastric or gastric tube may be required for patients with severe dysphagia.
A study found that treatment of patients with gastrostomy tubes with Mosapride citrate (a gastroprokinetic agent) was associated with a lower risk of aspiration pneumonia in comparison to both placebo and proton pump inhibitor treatment. [32] This therapy holds promise in this specific cohort of patients.
The use of nonparticulate antacids and histamine 2 (H2) blockers to reduce gastric acidity has been a common practice. However, gastric acid suppression and consequent loss of the acid barrier to bacteria is associated with a higher rate of pneumonia.
Before initiating enteral tube feeding, the tip location should be confirmed radiographically. Residual gastric volume should be regularly monitored. For those on a bolus tube feeding, the residual volume should not exceed 150 mL before the next bolus feed.
Avoid oversedating patients.

Prognosis of Aspiration Pneumonia
The prognosis of both chemical pneumonitis and bacterial aspiration pneumonia is dependent on underlying diseases, complications, and the patient's health status.
A retrospective study found the 30-day mortality rate in aspiration pneumonia to be 21% overall and 29.7% in hospital-associated aspiration pneumonia. [11] This mortality range depends on complications of the disease.
Results from a study on short-term prognosis in patients with community-acquired aspiration pneumonia showed that while pneumonia severity index, SCAP (Infectious Diseases Society of America/American Thoracic Society criteria for severe community-acquired pneumonia), and CURB-65 (confusion, urea nitrogen, respiratory rate, blood pressure, age ≥65 years) showed only modest prognostic predictability, blood biomarkers such as albumin and N-terminal of prohormone brain natriuretic peptide (NT-proBNP) showed good predictive accuracy in determining 30-day mortality. [33]
In Mendelson's original series in 1946, Mendelson described 61 obstetric patients who aspirated gastric acid during anesthesia, all of whom had a complete clinical recovery within 24-36 hours. [34] In subsequent studies, which have included older sicker patients, chemical pneumonia has a reported mortality rate of 30-62%, because chemical pneumonia often leads to acute respiratory distress syndrome (ARDS). The mortality rate for severe chemical pneumonitis (Mendelson syndrome) can be up to 70%.
If bacterial aspiration pneumonia is not treated early, it can lead to development of complications, including lung abscess and bronchopleural fistula. Nosocomial pneumonia is associated with a longer period of hospitalization and increased mortality rates.
The mortality rate for aspiration pneumonia complicated by empyema is approximately 20%. The mortality for uncomplicated pneumonia is approximately 5%. An animal model study demonstrated that mice with aspiration pneumonitis were more susceptible to subsequent respiratory infection with certain pathogens. [35]

Special Considerations
The following may be medicolegal pitfalls:
- Not recognizing or not weighing the risk for aspiration based on predisposing conditions
- Feeding patients at high risk for aspiration
- Resumption of feeding after intubation without assessing patient's ability to swallow and gastric motility
- Delay in diagnosis of anaerobic lung abscess because of subacute presentation
- Misdiagnosis of anaerobic lung abscess (mistaken for lung carcinoma or tuberculosis)

British Thoracic Society (BTS) Guidelines
In 2023 the British Thoracic Society (BTS) released a clinical statement on the prevention and management of aspiration pneumonia as a complement to their formal guidelines on community-acquired pneumonia (CAP). [38]
Key recommendations for preventing aspiration pneumonia include the following:
- The practice of good dental hygiene should include brushing the teeth, tongue and palate with a soft toothbrush, using non-foaming toothpaste, at least two times per day.
- Oral examination should be performed in hospitalized patients at risk of AP and at least weekly in patients at long-term care facilities, checking for infection (eg, candidiasis), quality of dentition, food residue and cleanliness of mucosal surfaces. Any abnormalities should be treated.
- People with swallowing difficulties should be referred to a speech and language therapist (SLT).
- In patients with a newly diagnosed abnormality of swallowing that presents a high risk of AP, early nasogastric feeding (within 3 days of presentation with swallowing difficulties) can improve nutritional status and outcomes.
- Percutaneous endoscopic gastrostomy (PEG) should be considered when nasogastric tubes do not provide adequate nutrition. If safe swallow returns PEG tubes can be removed.
The BTS makes the following recommendations for the management of aspiration pneumonia:
- The antibiotic regimen for hospitalized patients should be informed by local epidemiology including recent antibiotic exposure, recent microbiology results when available, and where the patient was when the pneumonia began.
- Aspiration pneumonia should be treated with a 5-day course of antibiotics. Failure to improve should trigger investigation of alternative sources of illness and/or complications of aspiration pneumonia and alternative antibiotic regimens are needed
- Treatment should include thromboprophylaxis (unless contraindicated), adequate hydration and (if required) supplemental oxygen.

The Infectious Diseases Society of America (IDSA) and American Thoracic Society (ATS) Guidelines
The Infectious Diseases Society of America (IDSA) and American Thoracic Society (ATS) issued updated clinical practice guidelines for community-acquired pneumonia (CAP) in October 2019. The following antibiotics are recommended in adult patients with CAP who are otherwise healthy37:
- Amoxicillin 1 g three times daily OR
- Doxycycline 100 mg twice daily OR
- In areas with pneumococcal resistance to macrolides < 25%: a macrolide (azithromycin 500 mg on day one and then 250 mg daily or clarithromycin 500 mg twice daily or clarithromycin extended-release 1,000 mg daily)
In outpatient adults with CAP who have comorbidities, the following antibiotic regimens are recommended [37] :
- Combination therapy:
- Amoxicillin/clavulanate 500 mg/125 mg 3 times daily or amoxicillin/clavulanate 875 mg/125 mg twice daily or 2,000 mg/125 mg twice daily or a cephalosporin (cefpodoxime 200 mg twice daily or cefuroxime 500 mg twice daily) AND
- A macrolide (azithromycin 500 mg on day one then 250 mg daily or clarithromycin [500 mg twice daily or extended release 1,000 mg once daily]) or doxycycline 100 mg twice daily OR
- Monotherapy:
- Respiratory fluoroquinolone (levofloxacin 750 mg daily, moxifloxacin 400 mg daily)
The following empiric treatment regimens are recommended in inpatient adults with nonsevere CAP who do not have risk factors for MRSA or P aeruginosa [37] :
- Combination therapy:
- A beta-lactam (ampicillin plus sulbactam 1.5-3 g every 6 hours or cefotaxime 1-2 g every 8 hours or ceftriaxone 1-2 g daily or ceftaroline 600 mg every 12 hours) AND
- A macrolide (azithromycin 500 mg daily or clarithromycin 500 mg twice daily) OR
- Monotherapy:
- A respiratory fluoroquinolone (levofloxacin 750 mg daily, moxifloxacin 400 mg daily)
- If macrolides and fluoroquinolones are contraindicated:
- A beta-lactam as above AND doxycycline
The following regimens are recommended among inpatient adults with severe CAP without risk factors for MRSA or P aeruginosa (agents and doses as above)37:
- A beta-lactam plus a macrolide OR
- A beta-lactam plus a respiratory fluoroquinolone
Routine addition of anaerobic coverage for suspected aspiration pneumonia is not recommended except when lung abscess or empyema is suspected. [37]
Empiric coverage for MRSA or P aeruginosa is recommended in adults with CAP only in the presence of locally validated risk factors. Empiric treatment options for MRSA include vancomycin (15 mg/kg every 12 hours) or linezolid (600 mg every 12 hours). Empiric treatment options for P aeruginosa include piperacillin-tazobactam (4.5 g every 6 hours), cefepime (2 g every 8 hours), ceftazidime (2 g every 8 hours), aztreonam (2 g every 8 hours), meropenem (1 g every 8 hours), or imipenem (500 mg every 6 hours). [37]
The duration of antibiotic therapy should be guided by a validated measure of clinical stability. Antibiotics should be continued until stability is achieved, for a total antibiotic duration of at least 5 days. [37]