Microscopic Polyangiitis: Practice Essentials, Background, Pathophysiology (original) (raw)
Practice Essentials
Microscopic polyangiitis (MPA) is a vasculitis of small vessels. Patients frequently present with renal manifestations, but systemic manifestations, arthritis, mononeuritis multiplex, and other signs and symptoms are also common. [1, 2] (See Presentation and Workup.)
Vasculitis in small vessels, including arterioles, capillaries, and venules, a characteristic of MPA, is absent in polyarteritis nodosa. This absence is the proposed distinguishing feature between those two disorders. Granulomatosis with polyangiitis (Wegener granulomatosis, GPA), MPA, and eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome, EGPA) comprise a category of small vessel vasculitis related to antineutrophil cytoplasmic antibodies (ANCAs) and are characterized by a paucity of immune deposits.
MPA and GPA seem to be part of a clinical spectrum. However, an absence of granuloma formation and sparing of the upper respiratory tract are features of MPA. These features help to distinguish MPA from GPA, although the two conditions are occasionally difficult to distinguish.
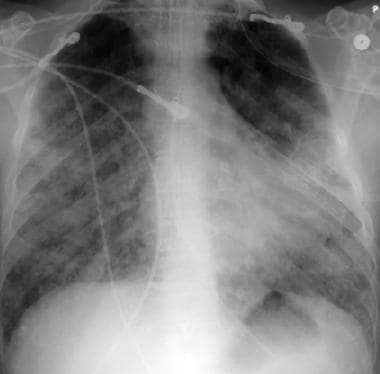
The image below depicts pulmonary alveolar capillaritis.
Pulmonary alveolar capillaritis.
Immunosuppressive medications are used to control MPA. [3] The choice of agents depends in part on the extent of disease, the rate of progression, and the degree of inflammation. See Treatment and Medication.

Background
MPA was initially considered as a microscopic form of polyarteritis nodosa. In 1990, the American College of Rheumatology developed classification criteria for several types of systemic vasculitis but did not distinguish between polyarteritis nodosa and microscopic polyarteritis nodosa. [4]
In 1994, a group of experts held an international consensus conference in Chapel Hill, North Carolina, to attempt to redefine the classification of small-vessel vasculitides. [5, 6] A second International Chapel Hill Consensus Conference was held in 2012. [7] The conference recommended categorizing small-vessel vasculitis as follows:
- ANCA-associated vasculitis (AAV) - MPA, GPA, EGPA
- Immune complex–associated small-vessel vasculitis - Anti-glomerular basement membrane (anti-GBM) disease, cryoglobulinemic vasculitis, IgA vasculitis (Henoch-Schönlein), hypocomplementemic urticarial vasculitis (anti-C1q vasculitis)
In addition, the conference recommended adding the following categories of vasculitis:
- Variable vessel vasculitis - Behcet disease, Cogan syndrome
- Single-organ vasculitis (eg, cutaneous leukocytoclastic angiitis, isolated aortitis)
- Vasculitis associated with systemic disease (eg, lupus, rheumatoid arthritis, sarcoid)
- Vasculitis associated with probable etiology (eg, hepatitis, drugs, cancer)
Classification criteria
The American College of Rheumatology (ACR) and the European Alliance of Associations for Rheumatology (EULAR) have published classification criteria for MPA. The criteria are intended tobe used for enrolling patients in studies, not for clinical diagnosis. The classification criteria should be applied after a diagnosis of small- or medium-vessel vasculitis has been made, and alternative disorders mimicking vasculitis have been excluded. [8]
Criteria and assigned scores are as follows [8] :
- Positive test for perinuclear antineutrophil cytoplasmic antibodies (p-ANCA) or antimyeloperoxidase (anti-MPO) antibodies: +6
- Pauci-immune glomerulonephritis: +3
- Lung fibrosis or interstitial lung disease: +3
- Sino-nasal symptoms or signs: -3
- Positive test for cytoplasmic antineutrophil cytoplasmic antibodies (c-ANCA) or antiproteinase 3 (anti-PR3) antibodies: -1
- Blood eosinophil count ≥ 1 × 10 9/L: -4
For the purposes of classification, a patient with a total score of 5 or more is said to have MPA. These criteria have a sensitivity of 91% and a specificity of 94%. [8]

Pathophysiology
Vasculitis is inflammation of the vessel walls. This may lead to necrosis and bleeding. MPA is characterized by pauci-immune, necrotizing, small-vessel vasculitis without clinical or pathological evidence of granulomatous inflammation.

Etiology
Based on current understanding of the inflammatory response, cytokine-mediated changes in the expression and function of adhesion molecules coupled with inappropriate activation of leukocytes and endothelial cells are postulated to be the primary factors influencing the degree and location of vessel damage in the vasculitis syndromes. However, the stimuli that initiate these pathologic inflammatory changes are not well understood.
ANCA may play a role in the pathogenesis of MPA.
Case reports have described an association of MPA with medications (eg, propylthiouracil, hydralazine, rifampicin, ethambutol) and with diseases such as primary biliary cirrhosis. [9, 10, 11]

Epidemiology
With the increased availability of ANCA testing, reported cases of MPA have also risen. A 20-year population-based study in Rochester, Minnesota estimated the incidence of MPA at 1.6 per 100,000 persons. [12]
Internationally, the incidence is approximately two cases per 100,000 persons in the United Kingdom. In Sweden and Germany, the incidence is estimated to be 1.3 per 100,000 persons. [13, 14]
The median age of onset is approximately 50 years. MPA is more common in White persons than Black persons; males are affected slightly more frequently than females.

Prognosis
With treatment, 90% of patients with MPA improve and 75% achieve complete remission. The 5-year survival rate is approximately 75%. MPA carries a worse long-term survival rate than granulomatosis with polyangiitis (GPA) or Churg-Strauss syndrome, probably because of kidney involvement at disease onset.
Of patients with MPA, 30% relapse in 1-2 years. Oh et al reported that neither myeloperoxidase (MPO)-ANCA nor proteinase 3 (PR3)-ANCA positivity at diagnosis affected prognosis. However, risk of relapse was significantly higher in patients with chest and renal manifestations, Birmingham vasculitis activity score ≥13.5, or five factor score ≥1. [15]
Long-term damage in a study of 296 patients with MPA or GPA, as measured with the Vasculitis Damage Index (VDI), was associated with the severity of initial disease, older age, the number of relapses, and duration of glucocorticoid treatment. Patients were followed for 7 years post-diagnosis. Mean duration of glucocorticoid treatment was 40.4 months. [16]
In another study of 151 patients with ANCA-associated vasculitis, patients presenting with pulmonary involvement at baseline had higher damage and disease activity scores at 6, 12 and 24 months follow-up. Patients presenting with lung involvement had an increased risk of developing cardiovascular and kidney involvement and were more likely to develop pulmonary fibrosis. [17]
Complications of vasculitis depend on the particular organ system involvement (see Physical). One of the most significant complications of treatment is bladder cancer. Of patients treated with cyclophosphamide, 5% develop bladder cancer after 10 years and 16% develop bladder cancer after 15 years.
One study reviewed cardiovascular outcomes during long-term follow-up of patients with MPA and GPA in the first 4 European Vasculitis Study Group trials. A model was developed and validated to predict those at risk for a cardiovascular event. Older age, diastolic hypertension, and positive PR3-ANCA status were found to be independent determinants of cardiovascular outcomes. Within 5 years of diagnosis, 14% of patients experienced a cardiovascular event. [18]
The French Vasculitis Study Group Relapse Score (FRS) was developed to predict the probability of relapse in patients with MPA or GPA. [19] The FRS assigns each of the following features 1 point:
- PR3-ANCA positivity
- Estimated glomerular filtration rate (eGFR) ≥30 mL/min/1.73 m²
- Age ≤75 years
In the validation cohort, the FRS score and associated 5-year relapse risk was as follows:
- FRS 0: 8%
- FRS 1: 30%
- FRS 2: 48%
- FRS 3: 76%

Patient Education
Patients with MPA should be aware of the severity of the disease and the risk of recurrence. Compliance with medications and follow-up visits is critical.

- Hashmi MF, Jain V, Tiwari V. Microscopic Polyangiitis. 2023 Jan. [QxMD MEDLINE Link]. [Full Text].
- Chung SA, Seo P. Microscopic polyangiitis. Rheum Dis Clin North Am. 2010 Aug. 36 (3):545-58. [QxMD MEDLINE Link].
- Berti A, Cornec D, Dua AB. Treatment Approaches to Granulomatosis with Polyangiitis and Microscopic Polyangiitis. Rheum Dis Clin North Am. 2023 Aug. 49 (3):545-561. [QxMD MEDLINE Link].
- Fries JF, Hunder GG, Bloch DA, et al. The American College of Rheumatology 1990 criteria for the classification of vasculitis. Summary. Arthritis Rheum. 1990 Aug. 33(8):1135-6. [QxMD MEDLINE Link].
- Jennette JC, Falk RJ, Andrassy K, et al. Nomenclature of systemic vasculitides. Proposal of an international consensus conference. Arthritis Rheum. 1994 Feb. 37(2):187-92. [QxMD MEDLINE Link].
- Lightfoot RW, Michel BA, Bloch DA, et al. The American College of Rheumatology 1990 criteria for the classification of polyarteritis nodosa. Arthritis Rheum. 1990 Aug. 33(8):1088-93. [QxMD MEDLINE Link].
- Jennette JC. Overview of the 2012 revised International Chapel Hill Consensus Conference nomenclature of vasculitides. Clin Exp Nephrol. 2013 Oct. 17 (5):603-606. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] Suppiah R, Robson JC, Grayson PC, Ponte C, Craven A, Khalid S, et al. 2022 American College of Rheumatology/European Alliance of Associations for Rheumatology classification criteria for microscopic polyangiitis. Ann Rheum Dis. 2022 Mar. 81 (3):321-326. [QxMD MEDLINE Link].
- Seligman VA, Bolton PB, Sanchez HC, Fye KH. Propylthiouracil-induced microscopic polyangiitis. J Clin Rheumatol. 2001 Jun. 7(3):170-4. [QxMD MEDLINE Link].
- Amezcua-Guerra LM, Prieto P, Bojalil R, Pineda C, Amigo MC. Microscopic polyangiitis associated with primary biliary cirrhosis: a causal or casual association?. J Rheumatol. 2006 Nov. 33(11):2351-3. [QxMD MEDLINE Link].
- Kuwabara G, Yamada K, Tanaka K, Nozuchi S, Imoto W, Shibata W, et al. Muscle Biopsy-proven Drug-induced Microscopic Polyangiitis in a Patient with Tuberculosis. Intern Med. 2023 Jan 1. 62 (1):129-133. [QxMD MEDLINE Link]. [Full Text].
- Berti A, Cornec D, Crowson CS, Specks U, Matteson EL. The Epidemiology of Antineutrophil Cytoplasmic Autoantibody-Associated Vasculitis in Olmsted County, Minnesota: A Twenty-Year US Population-Based Study. Arthritis Rheumatol. 2017 Dec. 69 (12):2338-2350. [QxMD MEDLINE Link]. [Full Text].
- Rathmann J, Segelmark M, Englund M, Mohammad AJ. Stable incidence but increase in prevalence of ANCA-associated vasculitis in southern Sweden: a 23-year study. RMD Open. 2023 Mar. 9 (1):[QxMD MEDLINE Link]. [Full Text].
- Hellmich B, Lamprecht P, Spearpoint P, Götte D, Deichmann A, Buchholz I, et al. New insights into the epidemiology of ANCA-associated vasculitides in Germany: results from a claims data study. Rheumatology (Oxford). 2021 Oct 2. 60 (10):4868-4873. [QxMD MEDLINE Link].
- Oh YJ, Ahn SS, Park ES, Jung SM, Song JJ, Park YB, et al. Chest and renal involvements, Birmingham vascular activity score more than 13.5 and five factor score (1996) more than 1 at diagnosis are significant predictors of relapse of microscopic polyangiitis. Clin Exp Rheumatol. 2017 Jan 19. [QxMD MEDLINE Link].
- Robson J, Doll H, Suppiah R, Flossmann O, Harper L, Höglund P, et al. Glucocorticoid treatment and damage in the anti-neutrophil cytoplasm antibody-associated vasculitides: long-term data from the European Vasculitis Study Group trials. Rheumatology (Oxford). 2014 Sep 8. [QxMD MEDLINE Link].
- Hassan TM, Hassan AS, Igoe A, Logan M, Gunaratnam C, McElvaney NG, et al. Lung involvement at presentation predicts disease activity and permanent organ damage at 6, 12 and 24 months follow - up in ANCA - associated vasculitis. BMC Immunol. 2014 May 27. 15:20. [QxMD MEDLINE Link]. [Full Text].
- Suppiah R, Judge A, Batra R, Flossmann O, Harper L, Höglund P, et al. A model to predict cardiovascular events in patients with newly diagnosed wegener's granulomatosis and microscopic polyangiitis. Arthritis Care Res (Hoboken). 2011 Jan 14. [QxMD MEDLINE Link].
- Samson M, Devilliers H, Thietart S, Charles P, Pagnoux C, Cohen P, et al. Score to assess the probability of relapse in granulomatosis with polyangiitis and microscopic polyangiitis. RMD Open. 2023 Mar. 9 (1):[QxMD MEDLINE Link]. [Full Text].
- Massicotte-Azarniouch D, Herrera CA, Jennette JC, Falk RJ, Free ME. Mechanisms of vascular damage in ANCA vasculitis. Semin Immunopathol. 2022 May. 44 (3):325-345. [QxMD MEDLINE Link]. [Full Text].
- Gibson LE. Cutaneous manifestations of antineutrophil cytoplasmic antibody-associated vasculitis (AAV): a concise review with emphasis on clinical and histopathologic correlation. Int J Dermatol. 2022 Dec. 61 (12):1442-1451. [QxMD MEDLINE Link].
- Hervier B, Durant C, Masseau A, Ponge T, Hamidou M, Mussini JM. Use of muscle biopsies for diagnosis of systemic vasculitides. J Rheumatol. 2011 Mar. 38(3):470-4. [QxMD MEDLINE Link].
- Crickx E, Machelart I, Lazaro E, et al. Intravenous Immunoglobulin as an Immunomodulating Agent in Antineutrophil Cytoplasmic Antibody-Associated Vasculitides: A French Nationwide Study of Ninety-Two Patients. Arthritis Rheumatol. 2016 Mar. 68 (3):702-12. [QxMD MEDLINE Link].
- Walsh M, et al; PEXIVAS Investigators. Plasma Exchange and Glucocorticoids in Severe ANCA-Associated Vasculitis. N Engl J Med. 2020 Feb 13. 382 (7):622-631. [QxMD MEDLINE Link]. [Full Text].
- [Guideline] Chung SA, Langford CA, Maz M, et al. 2021 American College of Rheumatology/Vasculitis Foundation Guideline for the Management of Antineutrophil Cytoplasmic Antibody-Associated Vasculitis. Arthritis Care Res (Hoboken). 2021 Aug. 73 (8):1088-1105. [QxMD MEDLINE Link]. [Full Text].
- Little MA, Nightingale P, Verburgh CA, Hauser T, De Groot K, Savage C, et al. Early mortality in systemic vasculitis: relative contribution of adverse events and active vasculitis. Ann Rheum Dis. 2010 Jun. 69 (6):1036-43. [QxMD MEDLINE Link].
- Jayne DRW, Merkel PA, Schall TJ, Bekker P, ADVOCATE Study Group. Avacopan for the Treatment of ANCA-Associated Vasculitis. N Engl J Med. 2021 Feb 18. 384 (7):599-609. [QxMD MEDLINE Link].
- [Guideline] Hellmich B, Sanchez-Alamo B, Schirmer JH, et al. EULAR recommendations for the management of ANCA-associated vasculitis: 2022 update. Ann Rheum Dis. 2023 Mar 16. 28 (9):2756-2767. [QxMD MEDLINE Link].
- Gabilan C, Pfirmann P, Ribes D, Rigothier C, Chauveau D, Casemayou A, et al. Avacopan as First-Line Treatment in Antineutrophil Cytoplasmic Antibody-Associated Vasculitis: A Steroid-Sparing Option. Kidney Int Rep. 2022 May. 7 (5):1115-1118. [QxMD MEDLINE Link]. [Full Text].
- Springer JM, Kalot MA, Husainat NM, Byram KW, Dua AB, James KE, et al. Granulomatosis With Polyangiitis and Microscopic Polyangiitis: A Systematic Review and Meta-Analysis of Benefits and Harms of Common Treatments. ACR Open Rheumatol. 2021 Mar. 3 (3):196-205. [QxMD MEDLINE Link]. [Full Text].
- Faurschou M, Westman K, Rasmussen N, de Groot K, Flossmann O, Höglund P, et al. Brief Report: long-term outcome of a randomized clinical trial comparing methotrexate to cyclophosphamide for remission induction in early systemic antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Rheum. 2012 Oct. 64 (10):3472-7. [QxMD MEDLINE Link]. [Full Text].
- Langford CA, Hoffman GS. Methotrexate remains a valuable option for remission induction of nonsevere antineutrophil cytoplasmic antibody-associated vasculitis: comment on the article by Faurschou et al. Arthritis Rheum. 2013 Mar. 65 (3):843. [QxMD MEDLINE Link]. [Full Text].
- Stone JH, Merkel PA, Spiera R, et al. Rituximab versus cyclophosphamide for ANCA-associated vasculitis. N Engl J Med. 2010 Jul 15. 363(3):221-32. [QxMD MEDLINE Link]. [Full Text].
- Jayne D, Rasmussen N, Andrassy K, et al. A randomized trial of maintenance therapy for vasculitis associated with antineutrophil cytoplasmic autoantibodies. N Engl J Med. 2003 Jul 3. 349(1):36-44. [QxMD MEDLINE Link].
- Pagnoux C, Mahr A, Hamidou MA, Boffa JJ, Ruivard M, Ducroix JP, et al. Azathioprine or methotrexate maintenance for ANCA-associated vasculitis. N Engl J Med. 2008 Dec 25. 359 (26):2790-803. [QxMD MEDLINE Link]. [Full Text].
- Puéchal X, Pagnoux C, Perrodeau É, et al. Long-Term Outcomes Among Participants in the WEGENT Trial of Remission-Maintenance Therapy for Granulomatosis With Polyangiitis (Wegener's) or Microscopic Polyangiitis. Arthritis Rheumatol. 2016 Mar. 68 (3):690-701. [QxMD MEDLINE Link].
- Specks U, Merkel PA, Seo P, Spiera R, Langford CA, Hoffman GS, et al. Efficacy of remission-induction regimens for ANCA-associated vasculitis. N Engl J Med. 2013 Aug 1. 369(5):417-27. [QxMD MEDLINE Link].
- Terrier B et al; French Vasculitis Study Group. Long-term efficacy of remission-maintenance regimens for ANCA-associated vasculitides. Ann Rheum Dis. 2018 May 3. [QxMD MEDLINE Link].
- Charles P et al; French Vasculitis Study Group. Comparison of individually tailored versus fixed-schedule rituximab regimen to maintain ANCA-associated vasculitis remission: results of a multicentre, randomised controlled, phase III trial (MAINRITSAN2). Ann Rheum Dis. 2018 Apr 25. [QxMD MEDLINE Link].
- Merkel PA, Niles JL, Mertz LE, Lehane PB, Pordeli P, Erblang F. Long-Term Safety of Rituximab in Granulomatosis With Polyangiitis and in Microscopic Polyangiitis. Arthritis Care Res (Hoboken). 2021 Sep. 73 (9):1372-1378. [QxMD MEDLINE Link].
- Reinhold-Keller E, De Groot K, Rudert H, Nölle B, Heller M, Gross WL. Response to trimethoprim/sulfamethoxazole in Wegener's granulomatosis depends on the phase of disease. QJM. 1996 Jan. 89(1):15-23. [QxMD MEDLINE Link].
- Stegeman CA, Tervaert JW, de Jong PE, Kallenberg CG. Trimethoprim-sulfamethoxazole (co-trimoxazole) for the prevention of relapses of Wegener's granulomatosis. Dutch Co-Trimoxazole Wegener Study Group. N Engl J Med. 1996 Jul 4. 335(1):16-20. [QxMD MEDLINE Link].
- Langford CA, Talar-Williams C, Sneller MC. Mycophenolate mofetil for remission maintenance in the treatment of Wegener's granulomatosis. Arthritis Rheum. 2004 Apr 15. 51(2):278-83. [QxMD MEDLINE Link].
- Nowack R, Göbel U, Klooker P, Hergesell O, Andrassy K, van der Woude FJ. Mycophenolate mofetil for maintenance therapy of Wegener's granulomatosis and microscopic polyangiitis: a pilot study in 11 patients with renal involvement. J Am Soc Nephrol. 1999 Sep. 10(9):1965-71. [QxMD MEDLINE Link].
- Iatrou C, Zerbala S, Revela I, Spanou E, Marinaki S, Nakopoulou L, et al. Mycophenolate mofetil as maintenance therapy in patients with vasculitis and renal involvement. Clin Nephrol. 2009 Jul. 72(1):31-7. [QxMD MEDLINE Link].
- Haubitz M, Koch KM, Brunkhorst R. Cyclosporin for the prevention of disease reactivation in relapsing ANCA-associated vasculitis. Nephrol Dial Transplant. 1998 Aug. 13 (8):2074-6. [QxMD MEDLINE Link].
- Terrier B, Saadoun D, Sène D, Ghillani P, Amoura Z, Deray G, et al. Antimyeloperoxidase antibodies are a useful marker of disease activity in antineutrophil cytoplasmic antibody-associated vasculitides. Ann Rheum Dis. 2009 Oct. 68(10):1564-71. [QxMD MEDLINE Link].
- Watanabe H et al, for Japan Research Committee of the Ministry of Health Labour,Welfare for Intractable Vasculitis (JPVAS) Research Committee of Intractable Renal Disease of the Ministry of Health Labour, Welfare of Japan. Association between reappearance of myeloperoxidase-antineutrophil cytoplasmic antibody and relapse in antineutrophil cytoplasmic antibody-associated vasculitis: Subgroup analysis of nationwide prospective cohort studies. Arthritis Rheumatol. 2018 May 22. [QxMD MEDLINE Link].
- Guillevin L, Pagnoux C, Karras A, Khouatra C, Aumaître O, Cohen P, et al. Rituximab versus azathioprine for maintenance in ANCA-associated vasculitis. N Engl J Med. 2014 Nov 6. 371(19):1771-80. [QxMD MEDLINE Link].
- Falk RJ, Hogan S, Carey TS, Jennette JC. Clinical course of anti-neutrophil cytoplasmic autoantibody-associated glomerulonephritis and systemic vasculitis. The Glomerular Disease Collaborative Network. Ann Intern Med. 1990 Nov 1. 113(9):656-63. [QxMD MEDLINE Link].
- Haubitz M, Koch KM, Brunkhorst R. Cyclosporin for the prevention of disease reactivation in relapsing ANCA-associated vasculitis. Nephrol Dial Transplant. 1998 Aug. 13(8):2074-6. [QxMD MEDLINE Link].
- Jayne D. Review article: Progress of treatment in ANCA-associated vasculitis. Nephrology (Carlton). 2009 Feb. 14(1):42-8. [QxMD MEDLINE Link].
- Lane SE, Watts RA, Shepstone L, Scott DG. Primary systemic vasculitis: clinical features and mortality. QJM. 2005 Feb. 98(2):97-111. [QxMD MEDLINE Link].
Author
Coauthor(s)
Specialty Editor Board
Francisco Talavera, PharmD, PhD Adjunct Assistant Professor, University of Nebraska Medical Center College of Pharmacy; Editor-in-Chief, Medscape Drug Reference
Disclosure: Received salary from Medscape for employment. for: Medscape.
Chief Editor
Vecihi Batuman, MD, FASN Professor of Medicine, Section of Nephrology-Hypertension, Deming Department of Medicine, Tulane University School of Medicine
Vecihi Batuman, MD, FASN is a member of the following medical societies: American College of Physicians, American Society of Hypertension, American Society of Nephrology, Southern Society for Clinical Investigation
Disclosure: Nothing to disclose.
Additional Contributors
Bryan L Martin, DO Associate Dean for Graduate Medical Education, Designated Institutional Official, Associate Medical Director, Director, Allergy Immunology Program, Professor of Medicine and Pediatrics, Ohio State University College of Medicine
Bryan L Martin, DO is a member of the following medical societies: American Academy of Allergy Asthma and Immunology, American College of Allergy, Asthma and Immunology, American College of Osteopathic Internists, American College of Physicians, American Medical Association, American Osteopathic Association
Disclosure: Nothing to disclose.