Metabolic Acidosis in Emergency Medicine: Practice Essentials, Pathophysiology, Prognosis (original) (raw)
Overview
Practice Essentials
Metabolic acidosis occurs when an increased hydrogen ion level results in decreased bicarbonate (HCO3-) in the systemic circulation. Acidemia refers to a pH below the normal range of 7.35-7.45 and indicates that a precipitating disease process or ingestion has occurred. While the state of low pH is defined by the term acidemia, the process leading to this state is called acidosis. Acidosis only becomes acidemia when the body can no longer compensate for low serum bicarbonate, although the terms are often used in the literature interchangeably.
The pH is low with a pure metabolic acidosis but may be normal or high with mixed acid-base disturbances. A serum bicarbonate below 24 mEq/L is suggestive of metabolic acidosis but can be higher in someone with concomitant metabolic alkalosis or chronic respiratory acidosis, where there is metabolic compensation via bicarbonate retention in the kidney. Identification of the underlying condition that precipitates metabolic acidosis is essential to initiating appropriate therapy. [1]
The initial therapeutic goal for patients with severe acidemia is to raise the systemic pH above 7.1-7.2, a level at which dysrhythmias become less likely and cardiac contractility and responsiveness to catecholamines are restored. [2, 3] While the administration of bicarbonate may be indicated for severe acidosis, correction of acidosis should be achieved by identifying and treating the underlying disease process rather than by targeting pH correction directly.
This article discusses the differential diagnosis of metabolic acidosis and presents a scheme for identifying the underlying cause of acidosis by doing a complete history and physical exam as well as using laboratory tests that are available in the emergency department. Clinical strategies for treating metabolic acidosis are also reviewed.
Signs and symptoms of metabolic acidosis
Metabolic acidosis can result in a variety of nonspecific changes in several organ systems, producing, among others, neurologic, cardiovascular, pulmonary, gastrointestinal (GI), and musculoskeletal dysfunction. Symptoms are often a result of and specific to the underlying etiology of the metabolic acidosis.
Workup in metabolic acidosis
Lab studies in the workup of metabolic acidosis may include the following:
- Arterial blood gas (ABG) - A low HCO3 - level found on an automated sequential multiple analyzer (SMA) is often the first clue to the presence of metabolic acidosis
- Serum chemistry
- Urinalysis - If the urine pH is above 5.5 in the face of acidemia, this finding is consistent with a type I renal tubular acidosis (RTA)
- Anion gap (AG)
- Ketone levels
- Serum lactate levels
- Salicylate levels
- Iron levels
Once a metabolic acidosis has been identified, the type of metabolic acidosis present (elevated AG vs non-AG), as well as whether the patient has a mixed acid-base disorder, must be determined using a step-by-step approach (described in the Workup section).
Management of metabolic acidosis
Treating the underlying conditions in high AG states usually is sufficient to reverse the acidosis. Treatment with bicarbonate is unnecessary except in extreme cases of acidosis when the pH is less than 7.1-7.2. In such extreme cases, bicarbonate may be considered as a temporizing measure while the underlying cause is simultaneously addressed. However, the use of and indications for bicarbonate therapy are controversial.
Considerations
The primary goal of the emergency physician or practitioner in the treatment of metabolic acidosis is to identify and correct the underlying disease process. While metabolic acidosis has a broad differential, the underlying cause is often evident based on the patient’s presentation and on basic laboratory studies. Pursuit of subtle history and exam findings may elucidate the less common causes of metabolic acidosis and prompt investigation with additional laboratory testing. Mixed acid-base disorders are found using a stepwise approach to the arterial blood gases (ABGs).

Pathophysiology
Metabolic acidosis can arise in the following instances:
- When there is a rise in H+, with the ion being generated from endogenous (eg, lactate, ketones) or exogenous (salicylate, ethylene glycol, methanol) sources
- When the kidneys are unable to excrete hydrogen from dietary protein (type 1 and type IV RTA)
- When bicarbonate (HCO3 -) is lost via wasting through the kidneys (type II RTA) or the GI tract (diarrhea) or through a response to respiratory alkalosis
Henderson-Hasselbalch approach to acid-base physiology
The Henderson-Hasselbalch equation describes the relationship between blood pH and the components of the H2CO3 buffering system. This qualitative description of acid-base physiology, as follows, allows the metabolic components to be separated from the respiratory components of the acid-base balance:
pH = 6.1 + log (HCO3-/H2CO3)
with 6.1 being the acid dissociation constant of H2CO3.
The metabolic components of the buffering system, specifically, bicarbonate, produced by the kidneys, and acid, from endogenous or exogenous sources, are in equilibrium.
Carbonic acid (H2CO3) is in equilibrium with the respiratory components, as shown by the following equation:
H2CO3 = pCO2 (mm Hg) X 0.03
Base excess approach to acid-base physiology
Unfortunately, the Henderson/Hasselbalch equation is not linear; the partial pressure of CO2 (pCO2) adjusts pH as part of the normal respiratory compensation for acid-base derangements. This nonlinearity of Henderson-Hasselbalch prevents the equation from quantifying the exact amount of bicarbonate deficit in a metabolic acidosis. This observation led to the development of a semiquantitative approach, base excess (BE):
BE = (HCO3- - 24.4 + [2.3 X Hgb + 7.7] X [pH - 7.4]) X (1 - 0.023 X Hgb)
Base excess attempts to give the quantitative amount of bicarbonate (mmol) that must be added or subtracted to restore 1 liter of whole blood to a pH of 7.4 at a pCO2 of 40 mmHg. To standardize BE for hemoglobin, the following formula for standardized based excess (SBE) was developed; it showed improved in vivo accuracy:
SBE = 0.9287 X (HCO3- - 24.4 + 14.83 X [pH – 7.4])
Strong ion gap approach to acid-base physiology
With regard to the evaluation of metabolic acidosis in the emergency department, the strong ion gap (SIG) theory has never really taken off; however, it may potentially have more use in the intensive care unit (ICU) setting. The SIG is similar to the AG in that accounts for the difference between unmeasured cations and anions, but the SIG approach also considers the presence of ions like lactate, beta hydroxybutyrate, acetate, and sulfates, as well as the presence of abnormal proteins, albumin, and phosphate. The AG ignores the effects that changes in strong ions may have on plasma pH. [4, 5, 6]
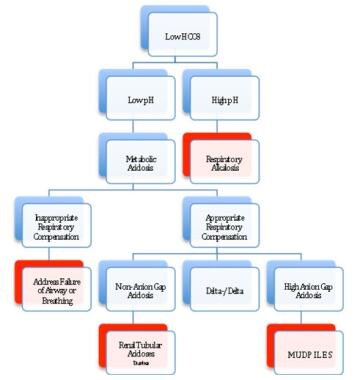
Approach for evaluating metabolic acidosis.

Prognosis
Because metabolic acidosis is a condition that occurs in response to a variety of disease states, the prognosis is directly related to the underlying etiology and the ability to treat or correct that particular disorder. Patients presenting with diabetic ketoacidosis (DKA) may have very good outcomes despite severe ketoacidosis (pH < 6.9). [7, 8] However, as may be expected, multiorgan failure is associated with poor prognosis. [9]
A study by Raikou indicated that in patients undergoing renal replacement therapy, an association exists between severe, uncorrected metabolic acidosis (serum bicarbonate concentrations < 20 mmol/L) and a 10-year risk for coronary heart disease of over 20%, as well as a high overall mortality rate. [10] . A study by Park et al indicated that a high rate of metabolic acidosis occurs in persons who receive kidney transplants; in about 30-70% of those transplant patients with an estimated glomerular filtration rate of under 30 mL/min per 1.73 m2, a low serum total CO2 concentration (< 22 mmol/L) was found. The study also found evidence that metabolic acidosis may increase the likelihood of graft failure and mortality in kidney transplant recipients. [11]
In a study of emergency department patients with acute kidney injury, Safari et al determined, through multivariate analysis, that metabolic acidosis is independently associated with mortality, along with sex, age over 60 years, blood urea nitrogen (BUN) concentration, hyperkalemia, cause of renal failure, and type of renal failure. [12]

- Hopkins E, Sanvictores T, Sharma S. Physiology, Acid Base Balance. StatPearls. 2022 Sep 12. [QxMD MEDLINE Link]. [Full Text].
- Burger M, Schaller DJ. Metabolic Acidosis. StatPearls. 2023 Jul 17. [QxMD MEDLINE Link]. [Full Text].
- Matyukhin I, Patschan S, Ritter O, Patschan D. Etiology and Management of Acute Metabolic Acidosis: An Update. Kidney Blood Press Res. 2020. 45 (4):523-31. [QxMD MEDLINE Link]. [Full Text].
- Stewart PA. Modern quantitative acid-base chemistry. Can J Physiol Pharmacol. 1983 Dec. 61(12):1444-61. [QxMD MEDLINE Link].
- Masevicius FD, Dubin A. Has Stewart approach improved our ability to diagnose acid-base disorders in critically ill patients?. World J Crit Care Med. 2015 Feb 4. 4 (1):62-70. [QxMD MEDLINE Link]. [Full Text].
- Constable PD. Clinical assessment of acid-base status. Strong ion difference theory. Vet Clin North Am Food Anim Pract. 1999 Nov. 15 (3):447-71. [QxMD MEDLINE Link].
- Wagner A, Risse A, Brill HL, et al. Therapy of severe diabetic ketoacidosis. Zero-mortality under very-low-dose insulin application. Diabetes Care. 1999 May. 22 (5):674-7. [QxMD MEDLINE Link]. [Full Text].
- Rodriguez-Gutierrez R, Camara-Lemarroy CR, Quintanilla-Flores DL, et al. Severe Ketoacidosis (pH ≤ 6.9) in Type 2 Diabetes: More Frequent and Less Ominous Than Previously Thought. Biomed Res Int. 2015. 2015:134780. [QxMD MEDLINE Link]. [Full Text].
- Oschatz E, Mullner M, Herkner H, Laggner AN. Multiple organ failure and prognosis in adult patients with diabetic ketoacidosis. Wien Klin Wochenschr. 1999 Aug 20. 111 (15):590-5. [QxMD MEDLINE Link].
- Raikou VD. Metabolic acidosis status and mortality in patients on the end stage of renal disease. J Transl Int Med. 2016 Dec 1. 4 (4):170-7. [QxMD MEDLINE Link]. [Full Text].
- Park S, Kang E, Park S, et al. Metabolic Acidosis and Long-Term Clinical Outcomes in Kidney Transplant Recipients. J Am Soc Nephrol. 2017 Jun. 28 (6):1886-97. [QxMD MEDLINE Link].
- Safari S, Hashemi B, Forouzanfar MM, Shahhoseini M, Heidari M. Epidemiology and Outcome of Patients with Acute Kidney Injury in Emergency Department; a Cross-Sectional Study. Emerg (Tehran). 2018. 6 (1):e30. [QxMD MEDLINE Link]. [Full Text].
- Whited L, Hashmi MF, Graham DD. Abnormal Respirations. StatPearls. 2023 Nov 5. [QxMD MEDLINE Link]. [Full Text].
- Mustaqeem R, Arif A. Renal Tubular Acidosis. StatPearls. 2023 Jul 17. [QxMD MEDLINE Link]. [Full Text].
- Manara A, Hantson P, Vanpee D, Thys F. Lactic acidosis following intentional overdose by inhalation of salmeterol and fluticasone. CJEM. 2012 Nov. 14(6):378-81. [QxMD MEDLINE Link].
- Gokhale YA, Vaidya MS, Mehta AD, Rathod NN. Isoniazid toxicity presenting as status epilepticus and severe metabolic acidosis. J Assoc Physicians India. 2009 Jan. 57:70-1. [QxMD MEDLINE Link].
- Dell'aglio DM, Perino LJ, Kazzi Z, Abramson J, Schwartz MD, Morgan BW. Acute Metformin Overdose: Examining Serum pH, Lactate Level, and Metformin Concentrations in Survivors Versus Nonsurvivors: A Systematic Review of the Literature. Ann Emerg Med. 2009 Jun 24. [QxMD MEDLINE Link].
- Mahler SA, Conrad SA, Wang H, Arnold TC. Resuscitation with balanced electrolyte solution prevents hyperchloremic metabolic acidosis in patients with diabetic ketoacidosis. Am J Emerg Med. 2011 Jul. 29 (6):670-4. [QxMD MEDLINE Link].
- Mehta AN, Emmett JB, Emmett M. GOLD MARK: an anion gap mnemonic for the 21st century. Lancet. 2008 Sep 13. 372 (9642):892. [QxMD MEDLINE Link]. [Full Text].
- Emmett M. Acetaminophen toxicity and 5-oxoproline (pyroglutamic acid): a tale of two cycles, one an ATP-depleting futile cycle and the other a useful cycle. Clin J Am Soc Nephrol. 2014 Jan. 9 (1):191-200. [QxMD MEDLINE Link]. [Full Text].
- Figge J, Jabor A, Kazda A, Fencl V. Anion gap and hypoalbuminemia. Crit Care Med. 1998 Nov. 26 (11):1807-10. [QxMD MEDLINE Link].
- Posen AK, Paloucek FP, Petzel R. Anion gap physiology and faults of the correction formula. Am J Health Syst Pharm. 2022 Mar 7. 79 (6):446-51. [QxMD MEDLINE Link].
- Brubaker RH, Vashisht R, Meseeha M. High Anion Gap Metabolic Acidosis. StatPearls. 2023 Aug 7. [QxMD MEDLINE Link]. [Full Text].
- Berend K. Review of the Diagnostic Evaluation of Normal Anion Gap Metabolic Acidosis. Kidney Dis (Basel). 2017 Dec. 3 (4):149-59. [QxMD MEDLINE Link]. [Full Text].
- Reddy P, Mooradian AD. Clinical utility of anion gap in deciphering acid-base disorders. Int J Clin Pract. 2009 Oct. 63(10):1516-25. [QxMD MEDLINE Link].
- Castro D, Patil SM, Zubair M, Keenaghan M. Arterial Blood Gas. StatPearls. 2024 Jan 8. [QxMD MEDLINE Link]. [Full Text].
- Manaker S, Perry H. Carbon monoxide poisoning. UpToDate. Updated 2024 Mar 6.
- Viallon A, Zeni F, Lafond P, et al. Does bicarbonate therapy improve the management of severe diabetic ketoacidosis?. Crit Care Med. 1999 Dec. 27 (12):2690-3. [QxMD MEDLINE Link].
- Patel MP, Ahmed A, Gunapalan T, Hesselbacher SE. Use of sodium bicarbonate and blood gas monitoring in diabetic ketoacidosis: A review. World J Diabetes. 2018 Nov 15. 9 (11):199-205. [QxMD MEDLINE Link]. [Full Text].
- Wilson RF, Spencer AR, Tyburski JG, Dolman H, Zimmerman LH. Bicarbonate therapy in severely acidotic trauma patients increases mortality. J Trauma Acute Care Surg. 2013 Jan. 74(1):45-50; discussion 50. [QxMD MEDLINE Link].
- Chua HR, Schneider A, Bellomo R. Bicarbonate in diabetic ketoacidosis - a systematic review. Ann Intensive Care. 2011 Jul 6. 1 (1):23. [QxMD MEDLINE Link]. [Full Text].
- Green SM, Rothrock SG, Ho JD, et al. Failure of adjunctive bicarbonate to improve outcome in severe pediatric diabetic ketoacidosis. Ann Emerg Med. 1998 Jan. 31 (1):41-8. [QxMD MEDLINE Link].
- Duhon B, Attridge RL, Franco-Martinez AC, Maxwell PR, Hughes DW. Intravenous sodium bicarbonate therapy in severely acidotic diabetic ketoacidosis. Ann Pharmacother. 2013 Jul-Aug. 47 (7-8):970-5. [QxMD MEDLINE Link].
- Wang H, Liang R, Liang T, et al. Effectiveness of Sodium Bicarbonate Infusion on Mortality in Critically Ill Children With Metabolic Acidosis. Front Pharmacol. 2022. 13:759247. [QxMD MEDLINE Link]. [Full Text].
- Smeltz AM, Arora H. Pro: Metabolic Acidosis Should be Corrected With Sodium Bicarbonate in Cardiac Surgical Patients. J Cardiothorac Vasc Anesth. 2022 Feb. 36 (2):616-8. [QxMD MEDLINE Link].
- Murdeshwar HN, Anjum F. Hemodialysis. StatPearls. 2023 Apr 27. [QxMD MEDLINE Link]. [Full Text].
- Nogi K, Shiraishi A, Yamamoto R, et al. Intermittent Hemodialysis for Managing Metabolic Acidosis During Resuscitation of Septic Shock: A Descriptive Study. Crit Care Explor. 2019 Dec. 1 (12):e0065. [QxMD MEDLINE Link]. [Full Text].
- Approach for evaluating metabolic acidosis.


Author
Renée S Lemieux, MD Resident Physician, Department of Emergency Medicine, Naval Medical Center San Diego
Disclosure: Nothing to disclose.
Coauthor(s)
Adam G Field, MD Staff Physician, Department of Emergency Medicine, Naval Medical Center San Diego and Sharp Grossmont Hospital
Disclosure: Nothing to disclose.
Specialty Editor Board
Francisco Talavera, PharmD, PhD Adjunct Assistant Professor, University of Nebraska Medical Center College of Pharmacy; Editor-in-Chief, Medscape Drug Reference
Disclosure: Received salary from Medscape for employment. for: Medscape.
Howard A Bessen, MD Professor of Medicine, Department of Emergency Medicine, University of California, Los Angeles, David Geffen School of Medicine; Program Director, Harbor-UCLA Medical Center
Howard A Bessen, MD is a member of the following medical societies: American College of Emergency Physicians
Disclosure: Nothing to disclose.
Chief Editor
Romesh Khardori, MD, PhD, FACP (Retired) Professor, Division of Endocrinology, Diabetes and Metabolism, Department of Internal Medicine, Eastern Virginia Medical School
Romesh Khardori, MD, PhD, FACP is a member of the following medical societies: American Association of Clinical Endocrinology, American College of Physicians, American Diabetes Association, Endocrine Society
Disclosure: Nothing to disclose.
Additional Contributors
Richard H Sinert, DO Professor of Emergency Medicine, Clinical Assistant Professor of Medicine, Research Director, State University of New York College of Medicine; Consulting Staff, Vice-Chair in Charge of Research, Department of Emergency Medicine, Kings County Hospital Center
Richard H Sinert, DO is a member of the following medical societies: American College of Physicians, Society for Academic Emergency Medicine
Disclosure: Nothing to disclose.
Erik D Schraga, MD Staff Physician, Department of Emergency Medicine, Mills-Peninsula Emergency Medical Associates
Disclosure: Nothing to disclose.
Antonia Quinn, DO Assistant Professor, Department of Emergency Medicine, State University of New York Downstate Medical Center; Assistant Residency Director, Attending Physician, Department of Emergency Medicine, Kings County Hospital Center, SUNY Downstate Medical Center
Antonia Quinn, DO is a member of the following medical societies: American College of Emergency Physicians, Society for Academic Emergency Medicine
Disclosure: Nothing to disclose.
Acknowledgements
The authors and editors of Medscape Reference gratefully acknowledge the contributions of previous author, Karen L Stavile, MD, to the development and writing of this article.