Iritis and Uveitis: Practice Essentials, Background, Pathophysiology (original) (raw)
Overview
Practice Essentials
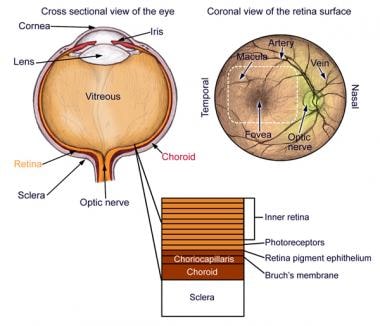
Uveitis is defined as inflammation of the uveal tract, which is further subdivided into anterior and posterior components. The anterior tract is composed of the iris and ciliary body, whereas the posterior tract includes choroid. Hence, uveitis is inflammation of any of these components and also may include other surrounding tissues such as sclera, retina, and optic nerve. [1] Uveitis often is idiopathic but may be triggered by genetic, traumatic, immune, or infectious mechanisms.
Anatomy of the eye.
Signs and symptoms
Symptoms of uveitis depend on several variables, the most important of which are type (ie, anterior, posterior, intermediate) and duration of symptoms (ie, acute, chronic). Furthermore, a thorough review of systems (eg, shortness of breath, arthritis, rash, trauma, back pain, travel history, etc) should be conducted to elucidate potential underlying etiologies.
Acute anterior uveitis presents as follows:
- Pain, generally developing over a few hours or days except in cases of trauma
- Redness
- Photophobia
- Blurred vision
- Increased lacrimation
Chronic anterior uveitis presents primarily as blurred vision and mild redness. Patients have little pain or photophobia except when having an acute episode.
Posterior uveitis presents as follows [2] :
- Blurred vision and floaters
- Absence of symptoms of anterior uveitis (ie, pain, redness, and photophobia)
The presence of symptoms of posterior uveitis, redness and pain suggests one of the following:
- Anterior chamber involvement
- Bacterial endophthalmitis
- Posterior scleritis
Intermediate uveitis presents as follows [2] :
- Painless floaters and decreased vision (similar to posterior uveitis)
- Minimal photophobia or external inflammation
Patients with panuveitis may present with any or all of the above symptoms.
Physical examination findings are as follows:
- Lids, lashes, and lacrimal ducts are normal.
- Conjunctival examination reveals 360° perilimbal injection, which increases in intensity as it approaches the limbus; this is the reverse of the pattern seen in conjunctivitis, in which the most severe inflammation occurs at a distance from the limbus. [3]
- Visual acuity may be decreased in the affected eye.
- Extraocular movement is generally normal.
- Pupillary examination may reveal direct photophobia when the light is directed into the affected eye, as well as consensual photophobia when light is directed into the uninvolved eye; consensual photophobia is typical of iritis, whereas photophobia due to more superficial causes, such as conjunctivitis, is direct but not consensual.
- Pupillary miosis is common.
Slit-lamp examination
- This is the most important aspect of the examination.
- Examine the cornea via direct illumination with a broad beam at a 30°-40° angle between the viewing microscope and the light source.
- Examine the epithelium for abrasions, edema, ulcers, or foreign bodies.
- Inspect the stroma for deep ulcers and edema.
- Keratitic precipitates (white blood cells) on the endothelium are a hallmark of iritis.
- Ciliary flush, a violaceous ring around the cornea, is highly indicative of intraocular inflammation. [1]
- Corneal edema and vitreous haze (large collection of inflammatory cells in the vitreous) may be observed.
- Intraocular pressure may be normal or slightly decreased in the acute phase owing to decreased aqueous humor production; however, pressure may become elevated as the inflammation subsides.
- Opacities of the lens (cataracts) may be present but are not specific for uveitis.
The most important structure to examine is the anterior chamber, as follows:
- Examine the anterior chamber using a vertically and horizontally short beam.
- Normally, the aqueous humor in the anterior chamber is optically clear.
- In uveitis, an increase in the protein content of the aqueous causes an effect upon examination known as flare, which is similar to that produced by a moving projector beam in a dark smoky room.
- White or red blood cells may be observed; layering of white blood cells in the anterior chamber is called hypopyon.
Grading of blood cells in the anterior chamber is as follows:
- 0 - None
- 1+ - Faint (barely detectable)
- 2+ - Moderate (clear iris and lens details)
- 3+ - Moderate (hazy iris and lens details)
- 4+ - Intense (fibrin deposits, coagulated aqueous)
See Clinical Presentation for more detail.
Diagnosis
Laboratory studies are unlikely to be helpful in cases of mild, unilateral nongranulomatous uveitis in the following settings:
- Trauma
- Known systemic disease
- History and physical not suggestive of systemic disease
A nonspecific workup is indicated if the history and the physical examination findings are unremarkable in the presence of uveitis that is bilateral, granulomatous, or recurrent. [1, 2] The following tests may be ordered by the consulting ophthalmologist, to be followed and further coordinated by the primary care physician:
- Complete blood cell (CBC) count
- Erythrocyte sedimentation rate (ESR)
- Antinuclear antibody (ANA)
- Rapid plasma reagin (RPR)
- Venereal disease research laboratory (VDRL)
- Purified protein derivative (PPD)/Qantiferon
- Lyme titer
- HLA testing for ankylosing spondylarthroses
- Chest radiography (to assess for sarcoidosis or tuberculosis)
- Urinalysis (for red blood cells or casts)
- Infectious workup (eg, HIV, HSV, CMV, toxoplasmosis), depending on the presentation
See Workup for more detail.
Management
Uveitis has no standard treatment regimen. Usually, the initial course of management is a stepwise approach starting with cycloplegics and corticosteroid drops to control pain and reduce inflammation. Progression to immunosuppressive agents may be necessary after consideration of the baseline etiology; however, this progression would be initiated by a primary care physician in consultation with an ophthalmologist after including physician and patient factors, which are beyond the scope of this review. Topical corticosteroid eye drops or sustained-release implants are traditionally used as treatment modalities. Newer administration routes (eg, intravitreal injection, suprachoroidal injection) have been approved by the FDA. There is growing evidence for the use of anti-tumor necrosis factor-alpha agents, such as adalimumab (Humira), which has also been FDA approved for treatment of uevitis. [4, 5, 6]
Considerations prior to initiating treatment include the following:
- Supporting evidence is sparse
- Check intraocular pressure and rule out herpes simplex virus (HSV) keratitis before starting topical corticosteroids
- Initiate steroid treatment only in consultation with an ophthalmologist
See Treatment and Medication for more detail.

Background
Uveitis is defined as inflammation of the uveal tract, the anatomy of which includes the iris, ciliary body, and choroid.
Anatomy of the eye.
The iris regulates the amount of light that enters the eye, the ciliary body produces aqueous humor and supports the lens, and the choroid provides oxygen and nourishment for the retina.
A classification scheme for uveitis exists based upon anatomic location. [7]
Table 1. Classification of Uveitis (Open Table in a new window)
| Type | Primary Site of Inflammation | Manifestation |
|---|---|---|
| Anterior uveitis | Anterior chamber | Iritis/iridocyclitis/anterior cyclitis |
| Intermediate uveitis | Vitreous | Vitreitis/hyalitis/pars planitis |
| Posterior uveitis | Choroid | Choroiditis/chorioretinitis/retinochoroiditis/retinitis/neuroretinitis |
| Panuveitis | Anterior chamber, vitreous, and/or choroid | All of the above |
Uveitis, particularly posterior uveitis, is a common cause of preventable blindness, so it is deemed a sight-threatening condition. Anterior uveitis is the form most likely to present to the emergency department. When the inflammation is limited to the iris, it is termed iritis. If the ciliary body is also involved, it is called iridocyclitis.
After anatomic classification, uveitis is further described by the following [8] :
- Onset (sudden vs insidious)
- Duration (limited, < 3 months in duration; persistent, >3 months in duration)
- Course (acute, recurrent, or chronic)
- Laterality (unilateral vs bilateral)
The distribution of general uveitis cases by anatomic site of disease has been found to differ significantly between community-based practice (anterior, 90.6%; intermediate, 1.4%; posterior 4.7%; panuveitis, 1.4%) and university referral practice (anterior, 60.6%; intermediate, 12.2%; posterior, 14.6%; panuveitis, 9.4%; P< 0.00005). [9]

Pathophysiology
The etiology of uveitis varies between populations and is often idiopathic [8] ; however, genetic, traumatic, or infectious mechanisms are known to promote or trigger uveitis. Diseases that predispose a patient to uveitis and are likely to present to the emergency department include inflammatory bowel disease, rheumatoid arthritis, systemic lupus erythematosus (SLE), sarcoidosis, tuberculosis, syphilis, and AIDS.
The mechanism for trauma is believed to be a combination of microbial contamination and accumulation of necrotic products at the site of injury, stimulating the body to mount an inflammatory response in the anterior segment of the eye. [8, 10]
For infectious etiologies of uveitis, it is postulated that the immune reaction directed against foreign molecules or antigens may injure the uveal tract vessels and cells.
When uveitis is found in association with autoimmune disorders, the mechanism may be a hypersensitivity reaction involving immune complex deposition within the uveal tract.
In one study at a tertiary referral center by Rodriguez et al, [11] the distribution in etiology among all anatomic forms of uveitis, anterior, intermediate, and posterior, were as follows:
- Idiopathic (34%)
- Seronegative spondyloarthropathies (10.4%)
- Sarcoidosis (9.6%)
- Juvenile rheumatoid arthritis (JRA) (5.6%)
- SLE (4.8%)
- Behçet disease (2.5%)
- AIDS (2.4%)
Seronegative arthropathies include nonspecific, ankylosing spondylitis, Reiter syndrome, psoriatic arthropathy, and inflammatory bowel disease.
In the same Rodriguez et al study, [11] anterior uveitis was the most common form at 51.6%, and the etiologic distribution was as follows:
- Idiopathic (37.8%)
- Seronegative arthropathies (21.6%)
- JRA (10.8%)
- Herpes virus (9.7%)
- Sarcoidosis (5.8%)
- SLE (3.3%)
- Rheumatoid arthritis (0.9%)
Posterior uveitis was next most common, with 19.4% of cases, the most common etiologies being Toxoplasma (24.6%), idiopathic (13.3%), cytomegalovirus (CMV) (11.6%), SLE (7.9%), and sarcoidosis (7.5%).
A more rare cause of uveitis are medications. Few studies and case reports have associated bisphosphonates, fluoroquinolones, hormone replacement therapy, and etanercept with the development of uveitis. [12]

Frequency
United States
The approximate estimated annual incidence of uveitis in the United States ranges from 25-52 cases per 100,000 persons per year. [4, 13, 14] A 2021 systemic review found the estimated prevalence of non-infectious uveitis to be 121 per 100,000. [12]
International
The incidence and prevalence of uveitis vary widely internationally. Finland has one of the highest annual incidences of uveitis, probably because of the high frequency of HLA-B27 spondyloarthropathy among the population. [4] The reported prevalence of uveitis (infectious and non-infectious) in China ranged from 152 per 100,000 in China; 173 per 100,000 in South Korea; 194 per 100,000 persons in Taiwan; and 317-730 per 100,000 in India. [12]
Race
Racial predisposition to uveitis is related to the patient's underlying systemic disease, as follows [2] :
- Whites: HLA-B27, multiple sclerosis
- Blacks: Sarcoidosis, SLE
- Mediterranean/Middle Eastern descent: Behçet disease
- Asians: Behçet disease
Sex
In general, uveitis has no sexual predisposition except in cases secondary to autoimmune diseases, which are more common in women compared to men. [2, 12]
Age
Most people who develop uveitis are aged 20 to 50 years.

Mortality/Morbidity
No deaths due to iritis or uveitis have been reported.
Uveitis has been reported to be responsible for 5-20% of total blindness in Europe and North America and up to 25% of blindness in the developing world. [15, 12]
Morbidity results from posterior synechiae formation (adhesions between the iris and the lens) that may lead to high intraocular pressure, optic nerve loss and visual impairments. Blindness may result from inadequate treatment. Complications of medications, specifically topical steroids, may include glaucoma, cataracts, and potential vision deterioration. [1, 16]

Prognosis
Generally, the prognosis for iritis and uveitis is good with appropriate treatment. However, uveitis can be recurrent and affect the contralateral eye, especially with underlying inflammatory diseases.

Patient Education
For patient education resources, see the Eye and Vision Center. Also, see the patient education articles Anatomy of the Eye and Iritis.

- Dunn JP. Uveitis. Prim Care. 2015 Sep. 42 (3):305-23. [QxMD MEDLINE Link].
- Wills Eye Hospital. The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease. 5th ed. Philadelphia, Pa: Lippincott; 2008.
- Hashmi MF, Gurnani B, Benson S, Price KL. Conjunctivitis (Nursing). 2022 Jan. [QxMD MEDLINE Link]. [Full Text].
- Islam N, Pavesio C. Uveitis (acute anterior). Clin Evid (Online). November 2009. 04:705:
- Mozayan A, Farah S. Acute anterior uveitis following intravitreal injection of bevacizumab. Ophthalmic Surg Lasers Imaging Retina. 2013 Jan-Feb. 44(1):25-7. [QxMD MEDLINE Link].
- Syed BA, Kumar S, Bielory L. Current options and emerging therapies for anterior ocular inflammatory disease. Curr Opin Allergy Clin Immunol. 2014 Oct. 14 (5):485-9. [QxMD MEDLINE Link].
- Jabs DA, Nussenblatt RB, Rosenbaum JT; Standardization of Uveitis Nomenclature (SUN) Working Group. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. Sept 2005. 140:509-16. [QxMD MEDLINE Link].
- Yanoff and Duker. Uveitis and other intraocular inflammations. Ophthalmology. 3rd ed. Mosby; 2008.
- McCannel CA, Holland GN, Helm CJ, Cornell PJ, Winston JV, Rimmer TG. Causes of uveitis in the general practice of ophthalmology. UCLA Community-Based Uveitis Study Group. Am J Ophthalmol. 1996 Jan. 121(1):35-46. [QxMD MEDLINE Link].
- Logothetis HD, Leikin SM, Patrianakos T. Management of anterior segment trauma. Dis Mon. 2014 Jun. 60 (6):247-53. [QxMD MEDLINE Link].
- Rodriguez A, Calonge M, Pedroza-Seres M, Akova YA, Messmer EM, D'Amico DJ, et al. Referral patterns of uveitis in a tertiary eye care center. Arch Ophthalmol. 1996 May. 114(5):593-9. [QxMD MEDLINE Link].
- Joltikov KA, Lobo-Chan AM. Epidemiology and Risk Factors in Non-infectious Uveitis: A Systematic Review. Front Med (Lausanne). 2021. 8:695904. [QxMD MEDLINE Link].
- Acharya NR, Tham VM, Esterberg E, Borkar DS, Parker JV, Vinoya AC, et al. Incidence and prevalence of uveitis: results from the Pacific Ocular Inflammation Study. JAMA Ophthalmol. 2013 Nov. 131 (11):1405-12. [QxMD MEDLINE Link].
- Gritz DC, Wong IG. Incidence and prevalence of uveitis in Northern California; the Northern California Epidemiology of Uveitis Study. Ophthalmology. 2004 Mar. 111 (3):491-500; discussion 500. [QxMD MEDLINE Link].
- Nguyen QD, Merrill PT, Clark WL, Banker AS, Fardeau C, Franco P, et al. Intravitreal Sirolimus for Noninfectious Uveitis: A Phase III Sirolimus Study Assessing Double-masKed Uveitis TReAtment (SAKURA). Ophthalmology. 2016 Nov. 123 (11):2413-2423. [QxMD MEDLINE Link].
- Al-Dhibi HA, Al-Mahmood AM, Arevalo JF. A systematic approach to emergencies in uveitis. Middle East Afr J Ophthalmol. 2014 Jul-Sep. 21 (3):251-8. [QxMD MEDLINE Link].
- Yawn BP, Wollan PC, St Sauver JL, Butterfield LC. Herpes zoster eye complications: rates and trends. Mayo Clin Proc. 2013 Jun. 88(6):562-70. [QxMD MEDLINE Link].
- Wirbelauer C. Management of the red eye for the primary care physician. Am J Med. 2006 Apr. 119(4):302-6. [QxMD MEDLINE Link].
- Standardization of Uveitis Nomenclature (SUN) Working Group. Classification Criteria for Acute Retinal Necrosis Syndrome. Am J Ophthalmol. 2021 Aug. 228:237-244. [QxMD MEDLINE Link].
- Gandorfer A, Thurau S. [Acute retinal necrosis]. Ophthalmologe. 2009 Aug. 106 (8):751-59; quiz 760. [QxMD MEDLINE Link].
- Ganesh SK, Nair N, Thatikonda D. Ultrasound biomicroscopy as a tool in the evaluation and management of ocular hypotony in uveitis. Indian J Ophthalmol. 2022 Feb. 70 (2):443-447. [QxMD MEDLINE Link].
- Abad S, Seve P, Dhote R, Brezin AP. [Guidelines for the management of uveitis in internal medicine]. Rev Med Interne. 2009 Jun. 30(6):492-500. [QxMD MEDLINE Link].
- Lyon F, Gale RP, Lightman S. Recent developments in the treatment of uveitis: an update. Expert Opin Investig Drugs. 2009 May. 18(5):609-16. [QxMD MEDLINE Link].
- Lim LL, Smith JR, Rosenbaum JT. Retisert (Bausch & Lomb/Control Delivery Systems). Curr Opin Investig Drugs. 2005 Nov. 6(11):1159-67. [QxMD MEDLINE Link].
- Mohammad DA, Sweet BV, Elner SG. Retisert: is the new advance in treatment of uveitis a good one?. Ann Pharmacother. 2007 Mar. 41(3):449-54. [QxMD MEDLINE Link].
- Dunne JA, Travers JP. Topical steroids in anterior uveitis. Trans Opthalmol soc UK. 1979. 99(4):481-4. [QxMD MEDLINE Link].
- Kara C. LaMattina, Debra A. Goldstein. Adalimumab for the treatment of uveitis. Expert Review of Clinical Immunology. 2017. 13:3:181-188. [Full Text].
- Nguyen QD, Merrill PT, Jaffe GJ, Dick AD, Kurup SK, Sheppard J, et al. Adalimumab for prevention of uveitic flare in patients with inactive non-infectious uveitis controlled by corticosteroids (VISUAL II): a multicentre, double-masked, randomised, placebo-controlled phase 3 trial. Lancet. 2016 Sep 17. 388 (10050):1183-92. [QxMD MEDLINE Link].
- Hand L. Anti-TNF Agents Recommended for Ocular Disease. Available at https://www.medscape.com/viewarticle/818314. Accessed: January 6, 2014.
- Levy-Clarke G, Jabs DA, Read RW, Rosenbaum JT, Vitale A, Van Gelder RN. Expert Panel Recommendations for the Use of Anti-Tumor Necrosis Factor Biologic Agents in Patients with Ocular Inflammatory Disorders. Ophthalmology. 2013 Dec 17. [QxMD MEDLINE Link].
- Trivedi A, Katelaris C. The use of biologic agents in the management of uveitis. Intern Med J. 2019 Nov. 49 (11):1352-1363. [QxMD MEDLINE Link].
- Foster CS, Alter G, DeBarge LR, Raizman MB, Crabb JL, Santos CI, et al. Efficacy and safety of rimexolone 1% ophthalmic suspension vs 1% prednisolone acetate in the treatment of uveitis. Am J Ophthalmol. 1996 Aug. 122(2):171-82. [QxMD MEDLINE Link].
- Merck Manuals: Uveitis. Available at https://www.merck.com/mmhe/sec20/ch232/ch232a.html.
- Nishimoto JY. Iritis. How to recognize and manage a potentially sight-threatening disease. Postgrad Med. 1996 Feb. 99(2):255-7, 261-2. [QxMD MEDLINE Link].
- Nussenblatt R, Whitcup S, Palestine A. Uveitis: Fundamentals and Clinical Practice. 2nd ed. St. Louis, Mo: Mosby; 1996.
- Tessler H. Classification and symptoms and signs of uveitis. Duane T, ed. Clinical Ophthalmology. New York, NY: Harper and Row; 1987. 1-10.
- Sheppard JD, Toyos MM, Kempen JH, Kaur P, Foster CS. Difluprednate 0.05% versus prednisolone acetate 1% for endogenous anterior uveitis: a phase III, multicenter, randomized study. Invest Ophthalmol Vis Sci. 2014 May 6. 55 (5):2993-3002. [QxMD MEDLINE Link].
- Anatomy of the eye.
- Small stellate keratic precipitates with fine filaments in a patient with Fuchs heterochromic iridocyclitis.
Author
Zahra Ahmed, MD Resident Physician, Department of Emergency Medicine, NYC Health + Hospitals/Kings County Hospital Center
Disclosure: Nothing to disclose.
Coauthor(s)
Monalisa N Muchatuta , MD, MS Clinical Assistant Professor of Emergency Medicine, Faculty Director of Global EM Mini-Fellowships, Department of Emergency Medicine, State University of New York Downstate Medical Center
Monalisa N Muchatuta , MD, MS is a member of the following medical societies: African Federation for Emergency Medicine, American College of Emergency Physicians, Empire State Medical Association, Global Emergency Medicine Academy, International Federation for Emergency Medicine, Society for Academic Emergency Medicine, Stanford Center for Innovation in Global Health, Zimbabwe Emergency Medical Society, Zimbabwean Physicians Association in America
Disclosure: Nothing to disclose.
Specialty Editor Board
Francisco Talavera, PharmD, PhD Adjunct Assistant Professor, University of Nebraska Medical Center College of Pharmacy; Editor-in-Chief, Medscape Drug Reference
Disclosure: Received salary from Medscape for employment. for: Medscape.
Chief Editor
Gil Z Shlamovitz, MD, FACEP Professor of Clinical Emergency Medicine, Keck School of Medicine of the University of Southern California; Chief Medical Information Officer, Keck Medicine of USC
Gil Z Shlamovitz, MD, FACEP is a member of the following medical societies: American College of Emergency Physicians
Disclosure: Nothing to disclose.
Additional Contributors
Richard H Sinert, DO Professor of Emergency Medicine, Clinical Assistant Professor of Medicine, Research Director, State University of New York College of Medicine; Consulting Staff, Vice-Chair in Charge of Research, Department of Emergency Medicine, Kings County Hospital Center
Richard H Sinert, DO is a member of the following medical societies: American College of Physicians, Society for Academic Emergency Medicine
Disclosure: Nothing to disclose.
Robert E O'Connor, MD, MPH Professor and Chair, Department of Emergency Medicine, University of Virginia Health System
Robert E O'Connor, MD, MPH is a member of the following medical societies: American Academy of Emergency Medicine, American College of Emergency Physicians, American Heart Association, American Medical Association, National Association of EMS Physicians, Society for Academic Emergency Medicine
Disclosure: Nothing to disclose.
Acknowledgements
The authors and editors of Medscape Reference gratefully acknowledge the contributions of previous author, Kilbourn Gordon III, MD, to the development and writing of this article.