Pediatric Appendicitis: Practice Essentials, Anatomy, Pathophysiology (original) (raw)
Overview
Practice Essentials
Acute appendicitis is acute inflammation and infection of the vermiform appendix, which is most commonly referred to simply as the appendix. The appendix is a blind-ending structure arising from the cecum. Acute appendicitis is one of the most common causes of abdominal pain and is the most frequent condition leading to emergent abdominal surgery in children. The appendix may be involved in other infectious, inflammatory, or chronic processes that can lead to appendectomy; however, this article focuses on acute appendicitis. Appendicitis and acute appendicitis are used interchangeably.
Images of pediatric appendicitis are provided below.
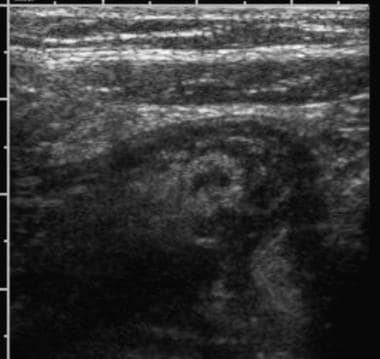
Ultrasonographic examination of the right lower quadrant reveals a greater than 6-mm noncompressible tubular structure shown in cross section. Discomfort was noted as the probe was depressed over this structure. A small amount of free fluid is also noted surrounding the appendix.
CT scan depicting a distended tubular structure descending into the pelvis and containing a round calcification (ie, an appendicolith).
Signs and symptoms
Common symptoms of acute appendicitis include abdominal pain, fever, and vomiting. The diagnosis of appendicitis can be difficult in children because the classic symptoms are often not present.
See Presentation for more detail.
Diagnosis
A delay in the diagnosis of appendicitis is associated with rupture and associated complications, especially in young children. Improvements in rupture rates have been made with advanced radiologic imaging. Appendicitis is a clinical diagnosis with imaging used to confirm equivocal cases.
See Workup for more detail.
Management
The definitive treatment for appendicitis is currently appendectomy. Initiation of antibiotics upon diagnosis is critical to initiate treatment, slow the infectious process and prevent progression of a nonperforated appendix. Key to any evaluation and treatment plan are the following: relieve the patient's pain and discomfort early and consistently; communicate with the patient and family about the plans; repeat the examination often; adjust the differential diagnosis as appropriate; and keep the patient for observation if a firm diagnosis is not made.
The most widely used antibiotic regimen is a penicillin-based regimen such as piperacillin/tazobactam or ampicillin/clavulanic acid or the combination of ampicillin, clindamycin (or metronidazole), and gentamicin. If a penicillin allergy exists, regimens including cephalosporins, aminoglycosides, and clindamycin may be used.
See Treatment and Medication for more detail.

Anatomy
The vermiform appendix is generally 5-10 cm in length. It arises from the cecum, which in most children is located in the right lower quadrant of the abdomen.
Although the base of the appendix is fixed to the cecum, the tip can be located in the pelvis, retrocecal, or extraperitoneal. Note that the anatomic position of the appendix determines the symptoms and the site of tenderness when the appendix becomes inflamed. Because the visceral nerve fibers associated with the appendix typically become inflamed first, there is often vague and referred symptoms to the periumbilical region through the T10 dermatome. As the somatic sensory fibers of the peritoneal lining become involved in the inflammatory process, the pain will frequently shift to the right lower abdomen and tenderness is focused at the site of inflammation.
The appendix is lined by typical colonic epithelium. The submucosa contains lymphoid follicles, which are very few at birth. This number gradually increases to a peak of about 200 follicles at age 10-20 years and then subsequently declines. In persons older than 30 years, less than half that number is present, and the number continues to decrease throughout adulthood. The appendix may act as a reservoir for the flora of the gut which may aid in recovery from intestinal infections. However, this function is not vital for life and removal of the appendix is well tolerated.

Pathophysiology
Tradition holds that once the appendix becomes obstructed, bacteria trapped within the appendiceal lumen begin to multiply, and the appendix becomes distended. The increased intraluminal pressure obstructs venous drainage, and the appendix becomes congested and ischemic.
The combination of bacterial infection and ischemia produce inflammation, which progresses to necrosis and gangrene. When the appendix becomes gangrenous, it may perforate. The progression from obstruction to perforation usually takes place over 72 hours.
One study noted that appendiceal perforation is more common in children, specifically younger children, than in adults. A substantial risk of perforation within 24 hours of onset was noted (7.7%) and was found to increase with duration of symptoms. While perforation was directly related to the duration of symptoms before surgery, the risk was associated more with prehospital delay than with in-hospital delay. [1]
During the initial stage of appendicitis, the patient may feel only periumbilical pain due to the T10 innervation of the appendix. As the inflammation worsens, an exudate forms on the appendiceal serosal surface. When the exudate touches the parietal peritoneum, a more intense and localized pain develops.
Perforation results in the release of inflammatory fluid and bacteria into the abdominal cavity. This further inflames the peritoneal surface, and peritonitis develops. The location and extent of peritonitis (diffuse or localized) depends on the degree to which the omentum and adjacent bowel loops can contain the spillage of luminal contents.
If the contents become walled off and form an abscess, the pain and tenderness may be localized to the abscess site. If the contents are not walled off and the fluid is able to travel throughout the peritoneum, the pain and tenderness become generalized.

Etiology
Acute appendicitis is a complex disease with quite a bit of variability in presentation and pathophysiology. Several theories have been promoted to explain the etiology, epidemiology and natural history of the disease. Many contend that appendicitis is due to obstruction of the blind ending appendix, resulting in a closed loop. In children, obstruction usually results from lymphoid hyperplasia of the submucosal follicles. The cause of this hyperplasia is controversial, but dehydration and viral infection have been proposed. Another common cause of obstruction of the appendix is a fecalith.
Rare causes include foreign bodies, parasitic infections (eg, nematodes), and inflammatory strictures.
The obstructive theory of appendicitis is widely taught but may not explain all the data regarding providers' experience with this common disease. Outbreaks and clusters of appendicitis have been reported making a true infectious etiology a possible etiologic agent. Appendicitis seems to run in families with first degree relatives of those who have had appendicitis being at a much higher risk of developing the condition which suggests an role of the host genetics. Finally, perforated and non-perforated appendicitis, which should be linked by the progression from early to late appendicitis, appear to act epidemiologically as two separate disease processes. Even though appendicitis is very common, much is not understood about the etiology or pathophysiology of this disease process.

Epidemiology
Appendicitis has an incidence of 70,000 pediatric cases per year in the United States. The incidence between birth and age 4 years is 1-2 cases per 10,000 children per year. The incidence increases to 25 cases per 10,000 children per year between 10 and 17 years of age. Overall, 7% of people in the United States have their appendix removed during their lifetime. The male-to-female ratio is approximately 2:1.
Appendicitis is much more common in developed countries. Although the reason for this discrepancy is unknown, potential risk factors include a diet low in fiber and high in sugar, family history, and infection. Gut flora and exposure to gastrointestinal infections have also been proposed as a hygiene theory of appendicitis. There may also be a role of the genetics of the host and the microbiome of the gut in the development of appendicitis and, possibly, with the risk of perforated appendicitis.
Appendicitis occurs in all age groups but is rare in infants. Liu et al found that preterm birth was associated with the development of appendicitis during the first year of life. [2]
Appendicitis is most common in the second decade of life (age 10-19 y), occurring at a rate of 23.3 cases per 10,000 per year. Thereafter, the incidence continues to decline, although appendicitis occurs in adulthood and into old age.
Interestingly, non-perforated appendicitis and perforated appendicitis are not linked when the epidemiology of the diseases is explored. The incidence for these two diagnoses differs over time suggesting that they are potentially unrelated to each other and may represent different pathologic processes. Similarities have been shown to other diseases such as diverticulitis and even hospital admissions for influenza.

Prognosis
Generally, the prognosis is excellent. At the time of diagnosis, the rate of appendiceal perforation is 20-35%. The rate of perforation is 80-100% for children younger than 3 years, compared with 10-20% in children 10-17 years old. Children with ruptured appendicitis are at risk for intra-abdominal abscess formation and small bowel obstruction, and they can have a prolonged hospital stay (several weeks or more). The mortality rate for children with appendicitis is 0.1-1%.
Initiation of antibiotics represents the single most critical step in the treatment of acute appendicitis. Multiple studies in children report safety and no increase in rates of perforation once antibiotics are initiated even if the appendectomy is delay to the next morning. Commonly, the most advanced cases of acute appendicitis are managed exclusively with antibiotics with the appendectomy delayed for several weeks to months, the so-called interval appendectomy. Data is mounting to expand this approach of using just antibiotics for the acute episode of appendicitis to all types of appendicitis. Many centers are pursuing this approach in ongoing research trials.
Death from appendicitis is most common in neonates and infants for the following 2 reasons:
- Appendicitis is rare in this age group; thus, unless the physician’s index of suspicion is high, appendicitis is often low on the list of suspected differential diagnoses.
- Very young patients are unable to communicate the location and nature of their pain. Some neonates may not even become febrile. Often, the patient’s only symptom is irritability or inconsolability.
Complications
Complications may include the following:
- Perforation
- Sepsis [3]
- Shock
- Postoperative adhesions
- Infertility
- Wound dehiscence
- Wound infection
- Bowel obstruction
Postoperative small bowel obstruction is a rare complication of laparoscopic appendectomy in children. Overman et al found that staples used during the appendectomy were often the cause of the obstruction. [4]

- Narsule CK, Kahle EJ, Kim DS, Anderson AC, Luks FI. Effect of delay in presentation on rate of perforation in children with appendicitis. Am J Emerg Med. 2011 Oct. 29(8):890-3. [QxMD MEDLINE Link].
- Liu Y, Yu X, Zhang G, et al. Preterm Birth and Infantile Appendicitis. Pediatrics. 2023 Dec 1. 152 (6):[QxMD MEDLINE Link].
- Arias-Llorente RP, Florez-Diez P, Oviedo-Gutierrez M, et al. Acute neonatal appendicitis: A diagnosis to consider in abdominal sepsis. J Neonatal Perinatal Med. 2014 Jan 1. 7(3):241-6. [QxMD MEDLINE Link].
- Overman RE Jr, Hilu MH, Gadepalli SH. Early Postoperative Small Bowel Obstruction After Appendectomy Because of Staples in Pediatric Patients. J Surg Res. 2020 Oct. 254:314-7. [QxMD MEDLINE Link].
- Rothrock SG, Pagane J. Acute appendicitis in children: emergency department diagnosis and management. Ann Emerg Med. 2000 Jul. 36(1):39-51. [QxMD MEDLINE Link].
- Becker T, Kharbanda A, Bachur R. Atypical clinical features of pediatric appendicitis. Acad Emerg Med. 2007 Feb. 14(2):124-9. [QxMD MEDLINE Link].
- Wiersma F, Toorenvliet BR, Bloem JL, Allema JH, Holscher HC. US examination of the appendix in children with suspected appendicitis: the additional value of secondary signs. Eur Radiol. 2009 Feb. 19(2):455-61. [QxMD MEDLINE Link].
- Pastore V, Cocomazzi R, Basile A, Pastore M, Bartoli F. Limits and advantages of abdominal ultrasonography in children with acute appendicitis syndrome. Afr J Paediatr Surg. 2014 Oct-Dec. 11(4):293-6. [QxMD MEDLINE Link].
- Gracey D, McClure MJ. The impact of ultrasound in suspected acute appendicitis. Clin Radiol. 2007 Jun. 62(6):573-8. [QxMD MEDLINE Link].
- Sulowski C, Doria AS, Langer JC, Man C, Stephens D, Schuh S. clinical outcomes in obese and normal-weight children undergoing ultrasound for suspected appendicitis. Acad Emerg Med. 2011 Feb. 18(2):167-73. [QxMD MEDLINE Link].
- Lowe LH, Penney MW, Stein SM, et al. Unenhanced limited CT of the abdomen in the diagnosis of appendicitis in children: comparison with sonography. AJR Am J Roentgenol. 2001 Jan. 176(1):31-5. [QxMD MEDLINE Link].
- Bachur RG, Levy JA, Callahan MJ, Rangel SJ, Monuteaux MC. Effect of Reduction in the Use of Computed Tomography on Clinical Outcomes of Appendicitis. JAMA Pediatr. 2015 Aug 1. 169 (8):755-60. [QxMD MEDLINE Link].
- Nicole M, Desjardins MP, Gravel J. Bedside Sonography Performed by Emergency Physicians to Detect Appendicitis in Children. Acad Emerg Med. 2018 Sep. 25 (9):1035-1041. [QxMD MEDLINE Link].
- Peck J, Peck A, Peck C, Peck J. The clinical role of noncontrast helical computed tomography in the diagnosis of acute appendicitis. Am J Surg. 2000 Aug. 180(2):133-6. [QxMD MEDLINE Link].
- Anderson KT, Putnam LR, Caldwell KM, B Diffley M, A Hildebrandt A, Covey SE, et al. Imaging gently? Higher rates of computed tomography imaging for pediatric appendicitis in non-children's hospitals. Surgery. 2017 May. 161 (5):1326-1333. [QxMD MEDLINE Link].
- Muehlstedt SG, Pham TQ, Schmeling DJ. The management of pediatric appendicitis: a survey of North American Pediatric Surgeons. J Pediatr Surg. 2004 Jun. 39 (6):875-9; discussion 875-9. [QxMD MEDLINE Link].
- Mullins ME, Kircher MF, Ryan DP, et al. Evaluation of suspected appendicitis in children using limited helical CT and colonic contrast material. AJR Am J Roentgenol. 2001 Jan. 176(1):37-41. [QxMD MEDLINE Link].
- Callahan MJ, Rodriguez DP, Taylor GA. CT of appendicitis in children. Radiology. 2002 Aug. 224(2):325-32. [QxMD MEDLINE Link].
- Kharbanda AB, Taylor GA, Fishman SJ, Bachur RG. A clinical decision rule to identify children at low risk for appendicitis. Pediatrics. 2005 Sep. 116(3):709-16. [QxMD MEDLINE Link].
- Samuel M. Pediatric appendicitis score. J Pediatr Surg. 2002 Jun. 37(6):877-81. [QxMD MEDLINE Link].
- Schneider C, Kharbanda A, Bachur R. Evaluating appendicitis scoring systems using a prospective pediatric cohort. Ann Emerg Med. 2007 Jun. 49(6):778-84, 784.e1. [QxMD MEDLINE Link].
- Yadao S, Lamture Y, Huse S. Uses of Antibiotics Alone in Case of Uncomplicated Appendicitis. Cureus. 2022 Aug. 14 (8):e28488. [QxMD MEDLINE Link]. [Full Text].
- Kronman MP, Oron AP, Ross RK, Hersh AL, Newland JG, Goldin A, et al. Extended- Versus Narrower-Spectrum Antibiotics for Appendicitis. Pediatrics. 2016 Jul. 138 (1):[QxMD MEDLINE Link].
- Whyte C, Tran E, Lopez ME, Harris BH. Outpatient interval appendectomy after perforated appendicitis. J Pediatr Surg. 2008 Nov. 43(11):1970-2. [QxMD MEDLINE Link].
- Andersson RE, Petzold MG. Nonsurgical treatment of appendiceal abscess or phlegmon: a systematic review and meta-analysis. Ann Surg. 2007 Nov. 246(5):741-8. [QxMD MEDLINE Link].
- Minneci PC, Mahida JB, Lodwick DL, Sulkowski JP, Nacion KM, Cooper JN, et al. Effectiveness of Patient Choice in Nonoperative vs Surgical Management of Pediatric Uncomplicated Acute Appendicitis. JAMA Surg. 2016 May 1. 151 (5):408-15. [QxMD MEDLINE Link].
- Bachur RG, Lipsett SC, Monuteaux MC. Outcomes of Nonoperative Management of Uncomplicated Appendicitis. Pediatrics. 2017 Jun 2. [QxMD MEDLINE Link].
- Lipsett SC, Monuteaux MC, Shanahan KH, Bachur RG. Nonoperative Management of Uncomplicated Appendicitis. Pediatrics. 2022 May 1. 149 (5):[QxMD MEDLINE Link]. [Full Text].
- Emil S, Elkady S, Shbat L, et al. Determinants of postoperative abscess occurrence and percutaneous drainage in children with perforated appendicitis. Pediatr Surg Int. 2014 Dec. 30(12):1265-71. [QxMD MEDLINE Link].
- Ultrasonographic examination of the right lower quadrant reveals a greater than 6-mm noncompressible tubular structure shown in cross section. Discomfort was noted as the probe was depressed over this structure. A small amount of free fluid is also noted surrounding the appendix.
- Ultrasonographic examination of the right lower quadrant reveals a greater than 6-mm noncompressible tubular structure shown in cross section. Discomfort was noted as the probe was depressed over this structure. A small amount of free fluid is also noted surrounding the appendix.
- CT scan depicting a distended tubular structure descending into the pelvis and containing a round calcification (ie, an appendicolith).
- CT scan revealing an enhancing tubular structure descending into the pelvis. Periappendiceal inflammation and streaking, so-called dirty fat, is noted surrounding the appendix.


Author
Adam C Alder, MD Assistant Professor, Department of Surgery, Division of Pediatric Surgery, Children's Medical Center, University of Texas Southwestern Medical Center at Dallas, Southwestern Medical School
Adam C Alder, MD is a member of the following medical societies: American College of Surgeons, Society of American Gastrointestinal and Endoscopic Surgeons, Texas Medical Association, International Pediatric Endosurgery Group
Disclosure: Nothing to disclose.
Coauthor(s)
Robert K Minkes, MD, PhD, MS Professor of Anatomy and Surgery, Founding Faculty, Orlando College of Osteopathic Medicine
Robert K Minkes, MD, PhD, MS is a member of the following medical societies: Alpha Omega Alpha, American College of Surgeons, American Medical Association, American Pediatric Surgical Association, Phi Beta Kappa
Disclosure: Nothing to disclose.
Chief Editor
Carmen Cuffari, MD Associate Professor, Department of Pediatrics, Division of Gastroenterology/Nutrition, Johns Hopkins University School of Medicine
Carmen Cuffari, MD is a member of the following medical societies: American College of Gastroenterology, American Gastroenterological Association, North American Society for Pediatric Gastroenterology, Hepatology and Nutrition, Royal College of Physicians and Surgeons of Canada
Disclosure: Received honoraria from Prometheus Laboratories for speaking and teaching; Received honoraria from Abbott Nutritionals for speaking and teaching. for: Abbott Nutritional, Abbvie, speakers' bureau.
Acknowledgements
Kirsten A Bechtel, MD Associate Professor, Department of Pediatrics, Yale University School of Medicine; Attending Physician, Department of Pediatric Emergency Medicine, Yale-New Haven Children's Hospital
Kirsten A Bechtel, MD is a member of the following medical societies: American Academy of Pediatrics
Disclosure: Nothing to disclose.
Deborah F Billmire, MD Associate Professor, Department of Surgery, Indiana University Medical Center
Deborah F Billmire, MD is a member of the following medical societies: Alpha Omega Alpha, American Academy of Pediatrics, American College of Surgeons, American Pediatric Surgical Association, Phi Beta Kappa, and Society of Critical Care Medicine
Disclosure: Nothing to disclose.
Jeffrey J DuBois, MD Chief of Children's Surgical Services, Division of Pediatric Surgery, Kaiser Permanente, Women and Children's Center, Roseville Medical Center
Jeffrey J DuBois, MD, is a member of the following medical societies: Alpha Omega Alpha, American Academy of Pediatrics, American College of Surgeons, American Pediatric Surgical Association, and California Medical Association
Disclosure: Nothing to disclose.
Michael Stephen Freitas, MS State University of New York at Buffalo School of Medicine and Biomedical Sciences
Michael Stephen Freitas, MS is a member of the following medical societies: American College of Surgeons, American Medical Association, American Physical Therapy Association, and Medical Society of the State of New York
Disclosure: Nothing to disclose.
Philip Glick, MD, MBA Professor, Departments of Surgery, Pediatrics, and Gynecology and Obstetrics, Vice-Chairperson for Finance and Development, Department of Surgery, State University of New York at Buffalo
Philip Glick, MD, MBA is a member of the following medical societies: Alpha Omega Alpha, American Academy of Pediatrics, American College of Surgeons, American Medical Association, American Pediatric Surgical Association, American Thoracic Society, Association for Academic Surgery, Association for Surgical Education, Central Surgical Association, Federation of American Societies for Experimental Biology, Medical Society of the State of New York, Phi Beta Kappa, Physicians for Social Responsibility, Royal College of Surgeons of England, Sigma Xi, Society for Pediatric Research, Society for Surgery of the Alimentary Tract, Society of Critical Care Medicine, and Society of University Surgeons
Disclosure: Nothing to disclose.
Kara E Hennelly, MD Fellow, Department of Pediatric Emergency Medicine, Children's Hospital Boston
Kara E Hennelly, MD is a member of the following medical societies: American Academy of Pediatrics
Disclosure: Nothing to disclose.
Michael S Katz, MD Research Fellow, Department of Pediatric Surgery, St Christopher's Hospital for Children
Michael S Katz, MD is a member of the following medical societies: American College of Surgeons, American Medical Association, and American Medical Student Association/Foundation
Disclosure: Nothing to disclose.
Robert Kelly, MD Chairman, Department of Surgery, Departments of Surgery and Pediatrics, Children's Hospital of the King's Daughters; Associate Professor, Eastern Virginia Medical School
Robert Kelly, MD is a member of the following medical societies: American Academy of Pediatrics, American College of Surgeons, American Medical Association, American Pediatric Surgical Association, American Society of Abdominal Surgeons, Medical Society of Virginia, Norfolk Academy of Medicine, and Southern Medical Association
Disclosure: Nothing to disclose.
David A Piccoli, MD Chief of Pediatric Gastroenterology, Hepatology and Nutrition, The Children's Hospital of Philadelphia; Professor, University of Pennsylvania School of Medicine
David A Piccoli, MD is a member of the following medical societies: American Association for the Study of Liver Diseases, American Gastroenterological Association, and North American Society for Pediatric Gastroenterology and Nutrition
Disclosure: Nothing to disclose.
Jeffrey R Tucker, MD Assistant Professor, Department of Pediatrics, Division of Emergency Medicine, University of Connecticut School of Medicine, Connecticut Children's Medical Center
Disclosure: Merck Salary Employment
Mary L Windle, PharmD Adjunct Associate Professor, University of Nebraska Medical Center College of Pharmacy; Editor-in-Chief, Medscape Drug Reference
Disclosure: Nothing to disclose.
Wayne Wolfram, MD, MPH Associate Professor, Department of Emergency Medicine, Mercy St Vincent Medical Center
Wayne Wolfram, MD, MPH is a member of the following medical societies: American Academy of Emergency Medicine, American Academy of Pediatrics, and Society for Academic Emergency Medicine
Disclosure: Nothing to disclose.