MAFLD identifies patients with significant hepatic fibrosis better than MASLD (original) (raw)
Abstract
Background and aims
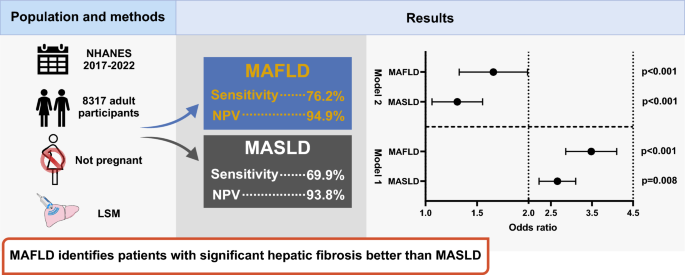
Diagnostic criteria for metabolic dysfunction-associated steatotic liver disease (MASLD) have been proposed but not yet validated. This study aimed to compare the diagnostic accuracy of the MASLD definition with the existing criteria for metabolic dysfunction-associated fatty liver disease (MAFLD) in identifying patients with significant fibrosis.
Methods
The analysis included a total of 8317 individuals who had complete biochemical and liver ultrasonography data from the National Health and Nutrition Examination Survey (2017–2020). In this study, significant fibrosis (≥ F2) was determined by a median liver stiffness of ≥ 8.0 kPa. To identify independent factors associated with significant fibrosis, multivariable logistic regression analyses were applied.
Results
MAFLD (OR 3.44; 95% CI 2.88–4.12; P < 0.0001) has a trend for stronger and independent association with significant fibrosis compared to MASLD (OR 2.63; 95% CI 2.22–3.11; P < 0.0001). Non-MASLD MAFLD is independently associated with a 14.28-fold higher odds of significant fibrosis compared to non-MAFLD MASLD. The sensitivity for detecting significant fibrosis for MAFLD and MASLD was 76.23% vs 69.94%, respectively. The performance of MAFLD remains consistent in a sub-analysis of patients with no or mild alcohol intake.
Conclusions
The definition of MAFLD provides a more precise identification of individuals who have both fatty liver and significant fibrosis, assessed by non-invasive tests.
Graphical Abstract
Access this article
Subscribe and save
- Starting from 10 chapters or articles per month
- Access and download chapters and articles from more than 300k books and 2,500 journals
- Cancel anytime View plans
Buy Now
Price excludes VAT (USA)
Tax calculation will be finalised during checkout.
Instant access to the full article PDF.
Similar content being viewed by others
Data availability
Not applicable.
References
- Chan KE, Koh TJL, Tang ASP, Quek J, Yong JN, Tay P, et al. Global prevalence and clinical characteristics of metabolic-associated fatty liver disease: a meta-analysis and systematic review of 10 739 607 individuals. J Clin Endocrinol Metab. 2022;107:2691–2700
Article PubMed Google Scholar - Eslam M, El-Serag HB, Francque S, Sarin SK, Wei L, Bugianesi E, et al. Metabolic (dysfunction)-associated fatty liver disease in individuals of normal weight. Nat Rev Gastroenterol Hepatol. 2022;19:638–651
Article PubMed Google Scholar - Eslam M, Newsome PN, Sarin SK, Anstee QM, Targher G, Romero-Gomez M, et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol. 2020;73:202–209
Article PubMed Google Scholar - Eslam M, Sanyal AJ, George J, Sanyal A, Neuschwander-Tetri B, Tiribelli C, et al. MAFLD: a consensus-driven proposed nomenclature for metabolic associated fatty liver disease. Gastroenterology. 2020;158(1999–2014):e1991
Google Scholar - Eslam M, Alkhouri N, Vajro P, Baumann U, Weiss R, Socha P, et al. Defining paediatric metabolic (dysfunction)-associated fatty liver disease: an international expert consensus statement. Lancet Gastroenterol Hepatol. 2021;6:864–873
Article PubMed Google Scholar - Rinella ME, Lazarus JV, Ratziu V, Francque SM, Sanyal AJ, Kanwal F, et al. A multi-society Delphi consensus statement on new fatty liver disease nomenclature. Ann Hepatol. 2023. https://doi.org/10.1097/HEP.0000000000000696
Article PubMed Google Scholar - Vilar-Gomez E, Calzadilla-Bertot L, Wong VW-S, Castellanos M, Aller-de la Fuente R, Metwally M, et al. Fibrosis severity as a determinant of cause-specific mortality in patients with advanced nonalcoholic fatty liver disease: a multi-national cohort study. Gastroenterology. 2018;155:443–457
Article PubMed Google Scholar - Petta S, Eslam M, Valenti L, Bugianesi E, Barbara M, Cammà C, et al. Metabolic syndrome and severity of fibrosis in nonalcoholic fatty liver disease: an age-dependent risk profiling study. Liver Int. 2017;37:1389–1396
Article CAS PubMed Google Scholar - Alharthi J, Eslam M. Biomarkers of metabolic (dysfunction)-associated fatty liver disease: an update. J Clin Transl Hepatol. 2022;10:134
Article PubMed Google Scholar - Yamamura S, Eslam M, Kawaguchi T, Tsutsumi T, Nakano D, Yoshinaga S, et al. MAFLD identifies patients with significant hepatic fibrosis better than NAFLD. Liver Int. 2020;40:3018–3030
Article CAS PubMed Google Scholar - Ayada I, van Kleef LA, Alferink LJ, Li P, de Knegt RJ, Pan Q. Systematically comparing epidemiological and clinical features of MAFLD and NAFLD by meta-analysis: focusing on the non-overlap groups. Liver Int. 2022;42:277–287
Article PubMed Google Scholar - Lin S, Huang J, Wang M, Kumar R, Liu Y, Liu S, et al. Comparison of MAFLD and NAFLD diagnostic criteria in real world. Liver Int. 2020;40:2082–2089
Article PubMed Google Scholar - Siddiqui MS, Vuppalanchi R, Van Natta ML, Hallinan E, Kowdley KV, Abdelmalek M, et al. Vibration-controlled transient elastography to assess fibrosis and steatosis in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2019;17(156–163):e152
Google Scholar - Wong GL-H. Update of liver fibrosis and steatosis with transient elastography (Fibroscan). Gastroenterol Rep. 2013;1:19–26
Article Google Scholar - Eslam M, Sarin SK, Wong VW-S, Fan J-G, Kawaguchi T, Ahn SH, et al. The Asian Pacific Association for the Study of the Liver clinical practice guidelines for the diagnosis and management of metabolic associated fatty liver disease. Hepatol Int. 2020;14:889–919
Article PubMed Google Scholar - Kawaguchi T, Tsutsumi T, Nakano D, Eslam M, George J, Torimura T. MAFLD enhances clinical practice for liver disease in the Asia-Pacific region. Clin Mol Hepatol. 2022;28:150
Article PubMed Google Scholar - Alharthi J, Gastaldelli A, Cua IH, Ghazinian H, Eslam M. Metabolic dysfunction-associated fatty liver disease: a year in review. Curr Opin Gastroenterol. 2022;38:251–260
Article CAS PubMed Google Scholar - Tsutsumi T, Eslam M, Kawaguchi T, Yamamura S, Kawaguchi A, Nakano D, et al. MAFLD better predicts the progression of atherosclerotic cardiovascular risk than NAFLD: generalized estimating equation approach. Hepatol Res. 2021;51:1115–1128
Article CAS PubMed Google Scholar - Fukunaga S, Nakano D, Kawaguchi T, Eslam M, Ouchi A, Nagata T, et al. Non-obese MAFLD is associated with colorectal adenoma in health check examinees: a multicenter retrospective study. Int J Mol Sci. 2021;22:5462
Article CAS PubMed PubMed Central Google Scholar - Ramírez-Mejía MM, Jiménez-Gutiérrez C, Eslam M, George J, Méndez-Sánchez N. Breaking new ground: MASLD vs. MAFLD—which holds the key for risk stratification? Hepatol Int. 2024;18:168–178
Article PubMed Google Scholar
Acknowledgements
ME is supported by a National Health and Medical Research Council of Australia (NHMRC) Program Grant (APP1053206) and Project and ideas grants (APP2001692, APP1107178 and APP1108422).
Funding
National Health and Medical Research Council,APP1053206, Mohammed Eslam,APP2001692, Mohammed Eslam,APP1107178, Mohammed Eslam,APP1108422, Mohammed Eslam.
Author information
Authors and Affiliations
- Storr Liver Centre, Westmead Institute for Medical Research, Westmead Hospital and University of Sydney, Sydney, NSW, 2145, Australia
Ziyan Pan & Mohammed Eslam - Gastroenterology and Hepatology Unit, Department of Medicine, College of Medicine and Health Sciences, Sultan Qaboos University, Muscat, Oman
Said A. Al-Busafi - Department of Internal Medicine, Ibn Al Nafees Hospital, Manama, 54533, Bahrain
Maheeba Abdulla - Department of Endemic Medicine and Gastroenterology, Faculty of Medicine, Minia University, Minia, Egypt
Yasser Fouad - Division of Gastroenterology and Hepatology, Chronic Viral Illness Service, McGill University Health Centre, Royal Victoria Hospital, 1001 Blvd. Décarie, Montreal, Canada
Giada Sebastiani
Authors
- Ziyan Pan
- Said A. Al-Busafi
- Maheeba Abdulla
- Yasser Fouad
- Giada Sebastiani
- Mohammed Eslam
Corresponding author
Correspondence toMohammed Eslam.
Ethics declarations
Conflict of interest
The authors declare no competing financial interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pan, Z., Al-Busafi, S.A., Abdulla, M. et al. MAFLD identifies patients with significant hepatic fibrosis better than MASLD.Hepatol Int 18, 964–972 (2024). https://doi.org/10.1007/s12072-024-10673-7
- Received: 02 February 2024
- Accepted: 17 March 2024
- Published: 08 May 2024
- Version of record: 08 May 2024
- Issue date: June 2024
- DOI: https://doi.org/10.1007/s12072-024-10673-7