An intrinsic circadian clock of the pancreas is required for normal insulin release and glucose homeostasis in mice (original) (raw)
Abstract
Aims/hypothesis
Loss of circadian clocks from all tissues causes defective glucose homeostasis as well as loss of feeding and activity rhythms. Little is known about peripheral tissue clocks, so we tested the hypothesis that an intrinsic circadian clock of the pancreas is important for glucose homeostasis.
Methods
We monitored real-time bioluminescence of pancreas explants from circadian reporter mice and examined clock gene expression in beta cells by immunohistochemistry and in situ hybridisation. We generated mice selectively lacking the essential clock gene Bmal1 (also known as Arntl) in the pancreas and tested mutant mice and littermate controls for glucose and insulin tolerance, insulin production and behaviour. We examined islets isolated from mutants and littermate controls for glucose-stimulated insulin secretion and total insulin content.
Results
Pancreas explants exhibited robust circadian rhythms. Clock genes Bmal1 and Per1 were expressed in beta cells. Despite normal activity and feeding behaviour, mutant mice lacking clock function in the pancreas had severe glucose intolerance and defective insulin production; their isolated pancreatic islets had defective glucose-stimulated insulin secretion, but normal total insulin content.
Conclusions/interpretation
The mouse pancreas has an autonomous clock function and beta cells are very likely to be one of the pancreatic cell types possessing an intrinsic clock. The Bmal1 circadian clock gene is required in the pancreas, probably in beta cells, for normal insulin secretion and glucose homeostasis. Our results provide evidence for a previously unrecognised molecular regulator of pancreatic glucose-sensing and/or insulin secretion.
Introduction
Circadian clocks are cell-autonomous molecular oscillators that drive daily rhythms of physiology and behaviour. In mammals, the clock of the suprachiasmatic nucleus (SCN) in the brain drives the rest–activity cycle and modulates physiology through autonomic and neuroendocrine control of visceral organ function [1]. Many peripheral tissues have intrinsic clocks, but at present there is only limited information about their functions [2].
Mice with germ-line mutations of circadian clock function have abnormal glucose homeostasis, regardless of whether the mutation affects positive (Clock [3] or Bmal1 [also known as _Arntl_]−/− [2, 4]) or negative (Per1 −/−, Per2 −/− [2]) elements of the clock feedback loop. This suggests that glucose homeostasis abnormalities arise from disrupted clock function rather than from an unrelated function of a particular clock gene. Because these mice lack clock function in all tissues, abnormal glucose homeostasis could have arisen from (1) a defect of the SCN clock (and the consequent abnormal activity and feeding), (2) other brain clocks or (3) clocks of peripheral tissues. Bmal1 −/− mice have significantly reduced circulating insulin [2], so it is plausible that a clock within the pancreas, particularly in the insulin-producing beta cells of the islets of Langerhans, might be crucial for glucose homeostasis.
Methods
Mice
Mice (Pdx1-Cre) were provided by D. Melton (Harvard University, Department of Molecular and Cellular Biology, Cambridge, MA, USA) [5]. We generated Bmal1 lox/lox [6] and Bmal1-Luc mice [7]. Mice (hybrid C57BL/6;129 background) were entrained to a 12 h light–dark cycle for 2 weeks prior to experiments. Genotyping was performed as described [6]. Studies were performed in accordance with a protocol approved by the Harvard Medical School Standing Committee on Animals.
Real-time recordings of circadian bioluminescence
Explants of pancreas from Bmal1-Luc circadian reporter mice were dissected, placed in medium (2 ml DMEM, supplemented with protease inhibitors, 10% [vol./vol.] FBS, 100 U/ml penicillin, 100 μg/ml streptomycin and 250 μmol/l d-luciferin), cultured and monitored for bioluminescence as described [7].
Glucose and insulin tolerance tests
Glucose and insulin tolerance tests, and insulin determination were performed as described [2]. For glucose tolerance tests across the circadian cycle, manipulations were performed under dim red light.
Immunohistochemistry and in situ hybridisation
Mice with Bmal1 deleted from the pancreas (Panc-Bmal1 −/−) and Pdx1-Cre littermates (n = 3 for each) were killed and the pancreas dissected into 4% formaldehyde in PBS. Pancreases were post-fixed (2 h, 4°C), fixative was removed by washes in PBS and tissue was cryoprotected overnight (4°C, 30% [wt/vol.] sucrose in PBS). Pancreases were then embedded and frozen, and 10 μm sections were cut on a cryostat, dried and stored at −80°C.
Insulin immunohistochemistry was performed using guinea pig anti-insulin (1:700; Dako, Glostrup, Denmark), followed by donkey anti-guinea pig secondary antibody (1:200; Invitrogen, Carlsbad, CA, USA). For double-label immunostaining with in situ hybridisation, fluorescence in situ hybridisation was performed as described in the Electronic supplementary material (ESM) Methods. Estimation of islet number was performed by counting the number of islets (identified by insulin immunostaining) per 10 μm section of four to seven sections per mouse, using three mice per genotype. Islet area and staining intensity (12–14 islets per genotype) were measured by circling islets in insulin immunofluorescence images and measuring area and mean grey value with ImageJ software (ESM Methods).
Glucose-stimulated insulin secretion
Pancreatic islets were isolated from mice and incubated overnight for recovery in DMED containing 1 mg/ml glucose (Sigma, St Louis, MO, USA) and 10% FBS. For glucose-stimulated insulin secretion, isolated islets were incubated in KRB containing bicarbonate and HEPES (KRBH; 129 mmol/l NaCl, 4.8 mmol/l KCl, 2.5 mmol/l CaCl2, 1.2 mmol/l KH2PO4, 1.2 mmol/l MgSO4, 5 mmol/l NaHCO3, 10 mmol/l HEPES, 0.1% (vol./vol.) BSA) with 2.8 mmol/l d-glucose for a 1 h for wash. Triplicates of ten islets were then incubated for 75 min in KRBH buffer containing either low (2.8 mmol/l) or high (16.7 mmol/l) d-glucose. Insulin in supernatant fractions was measured using an ELISA kit (Mouse Insulin Ultrasensitive; Alpco Diagnostics, Salem, NH, USA). For insulin content, groups of ten isolated islets were incubated overnight at −80°C in acidic ethanol (1.5% [vol./vol.] HCl in 70% [vol./vol.] ethanol), followed by centrifugation (20,000 g, 10 min) and measurement of insulin content as above.
Statistical analysis
Statistical analysis was performed by ANOVA or Student’s t test, as indicated. A value of p < 0.05 was considered significant.
Results
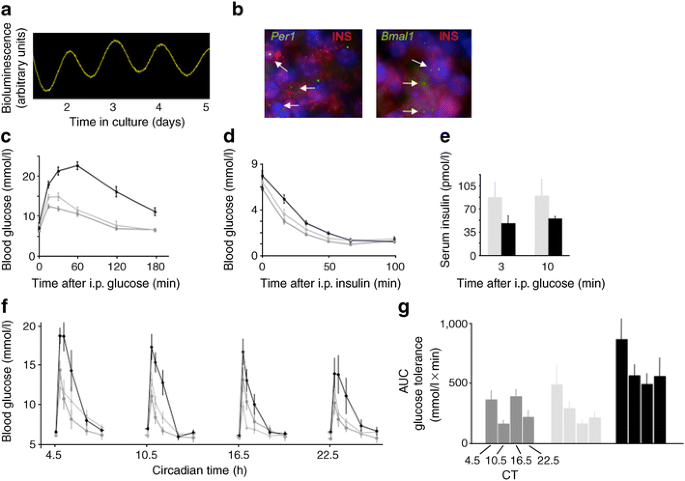
To determine whether the mouse pancreas contains a circadian clock, as reported in rats [8, 9], we cultured pancreas explants from Bmal1-Luc mice, a circadian reporter line [7]. The explants exhibited robust circadian rhythms of bioluminescence (Fig. 1a), demonstrating the presence of an autonomous clock. We detected co-expression of insulin and core clock component mRNAs (Fig. 1b), strongly suggesting that the insulin-producing beta cells of islets are among the pancreatic cell-types possessing an intrinsic clock.
Fig. 1
Glucose intolerance and defective insulin secretion in mice selectively lacking an intrinsic circadian clock of the pancreas. a Presence of an autonomous circadian clock in the pancreas. Real-time bioluminescence output of an explanted pancreas from a Bmal1_-Luc circadian reporter mouse [7]. b Combined immunohistochemistry and fluorescence in situ hybridisation to pancreas sections showing co-presence of insulin protein (red) and circadian clock component mRNA Per1 and Bmal1 as labelled (both green) in pancreatic islets. Punctate appearance of fluorescence signal for mRNAs is typical. Hoechst stain (blue) shows positions of cell nuclei. Arrows, double-labelled cells. c Glucose tolerance test performed at Zeitgeber time (ZT) 4.5 h in mice selectively lacking circadian clocks in the pancreas (Panc_-Bmal1 −/−; C57BL/6-129 hybrid) and littermate control genotypes. Mice used: Bmal1 lox/lox, Bmal1 conditional allele homozygote without Cre; Pdx1-Cre, single copy of Cre transgene and wild-type Bmal1. p < 0.001 (ANOVA). d Insulin tolerance tests, as above (c). No significant difference between genotypes (ANOVA). e Serum insulin concentrations at the indicated times after glucose administration. p < 0.02 (ANOVA). f Circadian profile of glucose tolerance for the three genotypes (n = 9–10 per genotype). g Quantification of circadian glucose tolerance curves shown above (f). CT, circadian time for all groups as for dark grey bars. c–g Values are mean±SEM. Light grey, Pdx1-Cre; dark grey, Bmal1 lox/lox; black, Panc-Bmal1 −/−
We next tested the hypothesis that an intrinsic circadian clock of the pancreas is important for glucose homeostasis. To generate mice with selective genetic ablation of clock function in the pancreas (Panc_-Bmal1_ −/− mice), we crossed Bmal1 conditional mice [6] with the Pdx1-Cre line [5]. As previously reported, Pdx1-Cre showed recombination activity throughout the pancreas and scattered activity in the duodenum, but no detectable activity in other peripheral tissues (ESM Fig. 1a). We detected no Cre activity in the SCN or in most of the brain, but did detect activity in the arcuate nucleus, ventromedial hypothalamus and dorsomedial hypothalamus (ESM Fig. 1b). Because these hypothalamic structures are well known to contribute to the neural regulation of glucose metabolism, this finding makes it essential to document a physiological defect in isolated pancreatic islets before concluding that a glucose homeostasis defect caused by Pdx1-Cre recombination is of pancreatic origin. In Panc-Bmal1 −/− mice, deletion of the conditional Bmal1 allele (ESM Fig. 2a) was consistent with the results of the indicator cross (ESM Fig. 1a). As expected, the protein brain, muscle Arnt-like 1 (BMAL1) was selectively lost from the pancreas (ESM Fig. 2b).
Unlike Bmal1 −/− mice lacking BMAL1 in all tissues [2], Panc-Bmal1 −/− mice exhibited normal locomotor activity, feeding behaviour, adiposity and body weight (ESM Fig. 3). Panc_-Bmal1_ −/− mice had an abnormality of glucose homeostasis essentially identical to that of Bmal1 −/− mice [2], characterised by severe glucose intolerance, normal responsiveness to insulin and defective insulin secretion in response to glucose (Fig. 1c–e). Panc-Bmal1 −/− mice exhibited intolerance to glucose throughout the circadian cycle, but a modest circadian modulation of glucose tolerance similar to that of controls persisted (Fig. 1f, g). Thus at least one clock outside the pancreas contributes to the circadian regulation of circulating glucose. The most likely candidate is the SCN clock, thought to modulate insulin secretion or sensitivity via autonomic efferents [1].
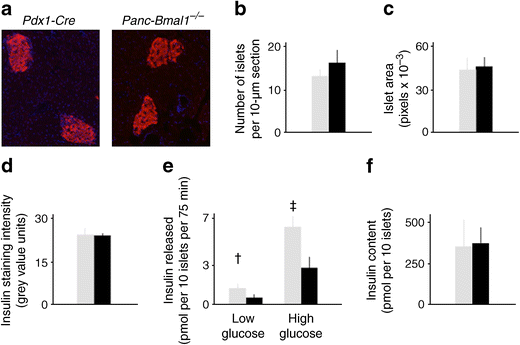
Pancreatic islets of Panc-Bmal1 −/− mice were indistinguishable in appearance from those of littermate Pdx1-Cre controls (Fig. 2a) and no significant difference was found between genotypes in the numbers of islets, mean size of islets or intensity of islet staining for insulin (Fig. 2b–d). Thus it is unlikely that the glucose intolerance and defective insulin secretion of Panc-Bmal1 −/− mice reflects a gross abnormality of islet development. Isolated, cultured islets from Panc-Bmal1 −/− mice secreted significantly less insulin in low and high glucose than islets from littermate Pdx1-Cre controls (Fig. 2e). There was no significant difference between genotypes in the total content of insulin per islet (Fig. 2f), indicating that the phenotype results from a defect in insulin secretion rather than insulin synthesis.
Fig. 2
Defective glucose-stimulated insulin secretion from pancreatic islets of mice selectively lacking an intrinsic circadian clock of the pancreas. a Normal general appearance of pancreatic islets in Panc-Bmal1 −/− mice vs Pdx-Cre. Immunofluorescence micrographs of pancreas sections were stained for insulin. b–d No significant differences were detected between Panc-Bmal1 −/− mice and littermate controls in variables reflecting the number, size or insulin expression of pancreatic islets (Student’s t test). e Defective insulin secretion from isolated islets of Panc-Bmal1 −/− mice under low and high glucose conditions, † p = 0.03, ‡ p = 0.002 (Student’s t test). f No significant difference in total insulin content of isolated islets from Panc-Bmal1 −/− mice and control littermates (Student’s t test). b–f Values are mean±SEM. Light grey, Pdx1-Cre; black, Panc-Bmal1 −/−
Discussion
Previous reports of clock gene expression in the pancreas [8] and rhythmic insulin release from isolated islets [9] suggested that a pancreatic clock regulates glucose homeostasis in vivo, a hypothesis our experiments have explicitly tested. Our results indicate that the Bmal1 gene, and probably circadian clock function, is required in the pancreas for normal insulin secretion and normal glucose homeostasis. The glucose intolerance of Panc-Bmal1 −/− mice is essentially identical to that of Bmal1 −/− mice [2], indicating that the loss of SCN clock function and consequent behavioural abnormalities in Bmal1 −/− mice contribute little, if anything to the glucose homeostasis phenotype. A similar, independent analysis has recently been reported [10].
We do not know the molecular mechanism underlying the defect in insulin release in Panc-Bmal1 −/− mice. The known role of clocks in regulating cell-autonomous gene expression suggests that a circadian clock within pancreatic beta cells regulates levels of one or more proteins of the glucose-sensing and/or insulin secretion pathways. In the absence of BMAL1, levels of one or more such proteins might fall below the usual circadian trough value, limiting insulin secretion. Our results provide evidence for a previously-unrecognised molecular regulator of pancreatic glucose-sensing and/or insulin secretion.
Abbreviations
BMAL1:
Brain, muscle Arnt-like 1
KRBH:
KRB containing bicarbonate and HEPES
SCN:
Suprachiasmatic nucleus
ZT:
Zeitgeber
References
- La Fleur SE, Kalsbeek A, Wortel J, Fekkes ML, Buijs RM (2001) A daily rhythm in glucose tolerance: a role for the suprachiasmatic nucleus. Diabetes 50:1237–1243
Article PubMed Google Scholar - Lamia KA, Storch K-F, Weitz CJ (2008) Physiological significance of a peripheral tissue circadian clock. Proc Natl Acad Sci U S A 105:15172–15177
Article CAS PubMed Google Scholar - Turek FW, Joshu C, Kohsaka A et al (2005) Obesity and metabolic syndrome in circadian Clock mutant mice. Science 308:1043–1045
Article CAS PubMed Google Scholar - Rudic RD, McNamara P, Curtis AM et al (2004) BMAL1 and CLOCK, two essential components of the circadian clock, are involved in glucose homeostasis. PLoS Biol 2:e377
Article PubMed Google Scholar - Gu G, Dubauskaite J, Melton DA (2002) Direct evidence for the pancreatic lineage: NGN3+ cells are islet progenitors and are distinct from duct progenitors. Development 129:2447–2457
CAS PubMed Google Scholar - Storch K-F, Paz C, Signorovitch J et al (2007) Intrinsic circadian clock of the mammalian retina: importance for retinal processing of visual information. Cell 130:730–741
Article CAS PubMed Google Scholar - Robles MS, Boyault C, Knutti D, Padmanabhan K, Weitz CJ (2010) Identification of RACK1 and protein kinase C alpha as integral components of the mammalian circadian clock. Science 327:463–466
Article CAS PubMed Google Scholar - Mühlbauer E, Wolgast S, Finckh U, Peschke D, Peschke E (2004) Indication of circadian oscillations in the rat pancreas. FEBS Lett 564:91–96
Article PubMed Google Scholar - Peschke E, Peschke D (1998) Evidence for a circadian rhythm of insulin release from perifused rat pancreatic islets. Diabetologia 41:1085–1092
Article CAS PubMed Google Scholar - Marcheva B, Ramsey KM, Buhr ED et al (2010) Disruption of the clock components CLOCK and BMAL1 leads to hypoinsulinaemia and diabetes. Nature 466:627–631
Article CAS PubMed Google Scholar
Acknowledgements
We thank D. Melton (Harvard University, Cambridge, MA, USA) for Pdx1-Cre mice, B. Lowell and D. Kong (Beth Israel Deaconess Medical Center, Boston, MA, USA) for advice and M. Liu (Department of Neurobiology, Harvard Medical School, Boston, MA, USA) for technical assistance. This work was supported by NIH grant R01 NS060860 (to C. J. Weitz), a Merck Fellowship of the Life Sciences Research Foundation (to K. A. Lamia), a Training Program in Sleep, Circadian and Respiratory Neurobiology Pre-Doctoral Fellowship T32 HL07901 (to L. A. Sadacca), and a Research Training in Digestive Diseases Fellowship T32 DK07191 (to A. S. deLemos). B. Blum is supported by an EMBO long-term post-doctoral fellowship.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Author notes
- K. A. Lamia
Present address: The Salk Institute for Biological Studies, La Jolla, CA, USA
Authors and Affiliations
- Department of Neurobiology, Harvard Medical School, 220 Longwood Ave, Boston, MA, 02115, USA
L. A. Sadacca, K. A. Lamia, A. S. deLemos & C. J. Weitz - Gastrointestinal Unit, Department of Medicine, Massachusetts General Hospital, Boston, MA, USA
A. S. deLemos - Harvard Stem Cell Institute, Department of Stem Cell and Regeneration Biology, Harvard University, Cambridge, MA, USA
B. Blum
Authors
- L. A. Sadacca
You can also search for this author inPubMed Google Scholar - K. A. Lamia
You can also search for this author inPubMed Google Scholar - A. S. deLemos
You can also search for this author inPubMed Google Scholar - B. Blum
You can also search for this author inPubMed Google Scholar - C. J. Weitz
You can also search for this author inPubMed Google Scholar
Corresponding author
Correspondence toC. J. Weitz.
Additional information
L. A. Sadacca and K. A. Lamia contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM Fig. 1
Sites of Cre recombinase activity from the Pdx1-Cre transgene in R26r indicator mice. a Peripheral tissue beta galactosidase histochemistry of the indicated tissue sections confirming the previously reported pattern of Pdx1-Cre activity. b Beta galactosidase histochemistry of indicated coronal brain sections. No activity was detected in the SCN or in the brain generally, but scattered activity was detected in the arcuate nucleus (AN), dorsomedial hypothalamus (DMH) and ventomedial hypothalamus (VMH) as indicated. Images are representative of those derived from three mice (PDF 54 kb)
ESM Fig. 2
Analysis of the Bmal1 gene and BMAL1 protein in Panc-Bmal1−/− mice. a PCR analysis of genomic DNA from the indicated tissues from mice of the indicated genotypes (lane designations same for each tissue). b Western blot analysis of BMAL1 protein from nuclear extracts of the indicated tissues from mice of the indicated genotypes. Nuclear protein SAP155 served as a loading control. Trace BMAL1 in pancreas sample is likely to have derived from vascular cells within the pancreas, in which recombination by Pdx1-Cre should not occur (PDF 75 kb)
ESM Fig. 3
Panc-Bmal1−/− mice and littermate controls were indistinguishable in behaviour, adiposity and body weight**. a** Representative double-plotted actograms for locomotor activity (running wheel behaviour) and feeding behaviour (food approach beam-breaks) of mice of the indicated genotypes. Horizontal axes represent time (2 × 24 h), successive lines (top to bottom) on vertical axes represent successive days. Tick marks represent running wheel revolutions (>0 per 6-min time bin, left) or food-approach beam-breaks. b Quantification of population data for the indicated variables for locomotor activity or feeding behaviour as indicated. Black bars, Panc_-Bmal1−/−_ mice (locomotor activity n = 25, feeding behaviour n = 9); light grey bars, littermate Pdx1-Cre controls (locomotor activity n = 17, feeding behaviour n = 10). Values are mean±SEM. No significant differences between genotypes were observed for any variable (Student’s t test). c No significant differences were detected between genotypes for body composition at 24 weeks of age (% fat) or (d) bodyweight at 2 and 7 months of age. Genotypes labelled as above (b). Values are means±SEM. c, d n = 10 and 8 respectively for Panc-Bmal1−/− mice and littermate Pdx1-Cre controls (PDF 116 kb)
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Sadacca, L.A., Lamia, K.A., deLemos, A.S. et al. An intrinsic circadian clock of the pancreas is required for normal insulin release and glucose homeostasis in mice.Diabetologia 54, 120–124 (2011). https://doi.org/10.1007/s00125-010-1920-8
- Received: 09 June 2010
- Accepted: 09 August 2010
- Published: 03 October 2010
- Issue Date: January 2011
- DOI: https://doi.org/10.1007/s00125-010-1920-8