Diabetes: MedlinePlus Medical Encyclopedia (original) (raw)
Diabetes is a long-term (chronic) disease in which the body cannot regulate the amount of sugar in the blood.
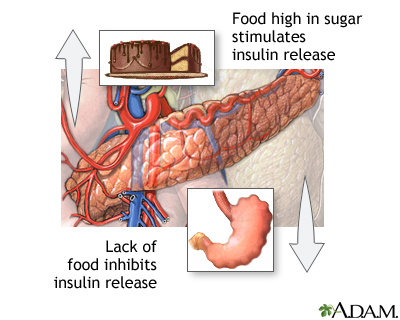
Insulin is a hormone produced by the pancreas to control blood sugar. Diabetes can be caused by too little insulin, resistance to the action of insulin, or both.
To understand diabetes, it is important to first understand the normal process by which food is broken down and used by the body for energy. Several things happen when food is digested and absorbed:
- A sugar called glucose enters the bloodstream. Glucose is a source of fuel for the body.
- An organ in the upper abdomen, below and behind the stomach, called the pancreas makes insulin. The role of insulin is to move glucose from the bloodstream into muscle, fat, and other cells, where it can be stored or used as fuel.
People with diabetes have high blood sugar because their body cannot move sugar from the blood into muscle and fat cells to be burned or stored for energy, and/or because their liver makes too much glucose and releases it into the blood. This is because either:
- Their pancreas does not make enough insulin
- Their cells do not respond to insulin normally (also called insulin resistance)
- Both of the above
There are two major types of diabetes. The causes and risk factors are different for each type:
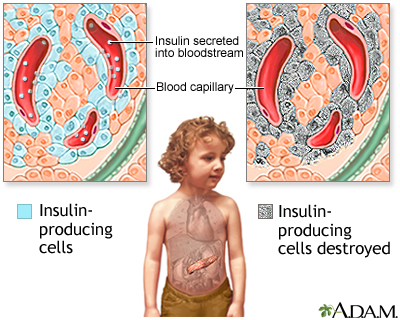
- Type 1 diabetes is less common, accounting for 5% to 10% of people with diabetes in the United States. It can occur at any age, but it is most often diagnosed in children, teens, or young adults. In this disease, the body makes little or no insulin. This is because the pancreas cells that make insulin are damaged by an immune process and stop working. Daily injections of insulin are needed. The exact cause of the immune process is unknown.
- Type 2 diabetes is more common, accounting for 90% to 95% of people with diabetes in the United States. It most often occurs in adulthood, but because of high obesity rates, children and teens are now being diagnosed with this disease. Some people with type 2 diabetes do not know they have it. With type 2 diabetes, the body is resistant to insulin and doesn't use insulin as well as it should. Not all people with type 2 diabetes are overweight or obese.
- There are other causes of diabetes, and some people cannot be classified as type 1 or type 2. Examples include LADA (latent autoimmune diabetes in adults, a variant of type 1 diabetes), MODY (maturity-onset diabetes of the young), and diabetes due to other illnesses.
Gestational diabetes is high blood sugar that develops at any time during pregnancy in a woman who does not already have diabetes.
If your parent, brother, or sister has diabetes, you are more likely to develop the disease.
A high blood sugar level can cause several symptoms, including:
- Blurry vision
- Excess thirst
- Fatigue
- Frequent urination
- Hunger
- Weight loss
Because type 2 diabetes develops slowly, some people with high blood sugar have no symptoms.
Symptoms of type 1 diabetes typically develop over a short period, usually weeks to months. People may be very sick by the time they are diagnosed.
After many years, diabetes can lead to other serious problems. These problems are known as diabetes complications, and include:
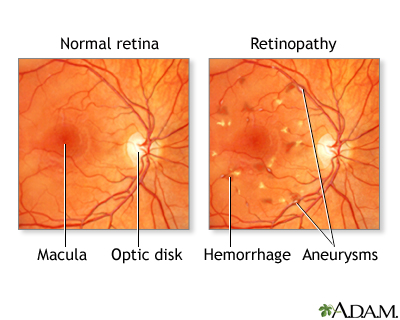
- Eye problems, including trouble seeing (especially at night), light sensitivity, cataracts, and blindness
- Sores and infections of the leg or foot, which if untreated, can lead to amputation of the leg or foot
- Damage to nerves in the body, causing pain, tingling, a loss of feeling, problems digesting food, and erectile dysfunction
- Kidney problems, which can lead to kidney failure
- Weakened immune system, which can lead to more frequent infections
- Increased chance of having a heart attack or stroke
A urine analysis may show high urine sugar. But a urine test alone does not diagnose diabetes.
Your health care provider may suspect that you have diabetes if your blood sugar level is 200 mg/dL or higher (11.1 mmol/L). To confirm the diagnosis, one or more of the following tests must be done.
Blood tests:
- Fasting blood glucose level. Diabetes is diagnosed if the fasting glucose level is 126 mg/dL (7.0 mmol/L) or higher on two different tests, when the person is in their usual state of health. Levels from 100 mg/dL to 125 mg/dL (5.6 mmol/L to 7.0 mmol/L) are called impaired fasting glucose or prediabetes. These levels are risk factors for developing type 2 diabetes.
- Hemoglobin A1C (A1C) test. Normal is less than 5.7%; prediabetes is 5.7% to 6.4%; and diabetes is 6.5% or higher.
- Oral glucose tolerance test. Diabetes is diagnosed if the glucose level is 200 mg/dL (11.1 mmol/L) or higher 2 hours after drinking a special 75 gram sugar drink (this test is used most often for type 2 diabetes and is rarely needed for type 1 diabetes).
Screening for type 2 diabetes in people who have no symptoms is recommended for:
- Overweight or obese adults (BMI of 25 kilograms per square meter or higher) starting at age 35 repeated every 3 years
- Overweight women who have other risk factors such as high blood pressure who are planning to become pregnant
- All adults age 35 or older, repeated every 3 years or at a younger age if the person has risk factors such as high blood pressure, or having a mother, father, sister, or brother with diabetes
In 2022, the US Preventive Services Task Force concluded that there was not enough evidence to recommend screening for type 2 diabetes in people 18 years old or younger. Some experts do advocate such screening for overweight children. Ask your child’s provider what is best for them.
Type 2 diabetes can sometimes be reversed with lifestyle changes, especially losing weight with exercise and by eating different foods. Some cases of type 2 diabetes can also be improved with weight loss surgery.
There is no cure for type 1 diabetes (except for a pancreas or islet cell transplant).
Treating either type 1 diabetes or type 2 diabetes involves nutrition, activity and medicines to control blood sugar level.
Everyone with diabetes should receive proper education and support about the best ways to manage their diabetes. Ask your provider about seeing a certified diabetes care and education specialist (CDCES).
Getting better control over your blood sugar, cholesterol, and blood pressure levels helps reduce the risk for kidney disease, eye disease, nervous system disease, heart attack, and stroke.
To minimize diabetes complications, visit your provider at least 2 to 4 times a year. Talk about any problems you are having. Follow your provider's instructions on managing your diabetes.
Many resources can help you understand more about diabetes. If you have diabetes, you can also learn ways to manage your condition and prevent diabetes complications.
More information and support for people with diabetes and their families can be found at :
- American Diabetes Association -- www.diabetes.org
- National Institute of Diabetes and Digestive and Kidney Diseases -- www.niddk.nih.gov/health-information/diabetes
Diabetes is a lifelong disease for most people who have it.
Tight control of blood glucose can prevent or delay diabetes complications. But these problems can occur, even in people with good diabetes control.
After many years, diabetes can lead to serious health problems:
- You could have eye problems, including trouble seeing (especially at night), cataracts, and light sensitivity. You could become blind.
- Your feet and skin can develop sores and infections. After a long time, your foot or leg may need to be amputated. Infection can also cause pain and itching in other parts of the body.
- Diabetes may make it harder to control your blood pressure and cholesterol. This can lead to a heart attack, stroke, and other problems. It can become harder for blood to flow to your legs and feet.
- Nerves in your body can get damaged, causing pain, tingling, and numbness.
- Because of nerve damage, you could have problems digesting the food you eat. You could feel weakness or have trouble going to the bathroom. Nerve damage can make it harder for men to have an erection.
- High blood sugar and other problems can lead to kidney damage. Your kidneys may not work as well as they used to. They may even stop working so that you need dialysis or a kidney transplant.
- Your immune system can weaken, which can lead to frequent infections.
Keeping an ideal body weight and an active lifestyle may prevent or delay the start of type 2 diabetes. If you're overweight, losing just 5% of your body weight can reduce your risk. Some medicines can also be used to delay or prevent the start of type 2 diabetes.
At this time, type 1 diabetes cannot be prevented. But there is promising research that shows type 1 diabetes may be delayed in some high risk people.
Diabetes - type 1; Diabetes - type 2; Diabetes - gestational; Type 1 diabetes; Type 2 diabetes; Gestational diabetes; Diabetes mellitus
Atkinson MA, McGill DE, Dassau E, Laffel L. Type 1 diabetes mellitus. In: Melmed S, Auchus RJ, Goldfine AB, Koenig RJ, Rosen CJ, eds. Williams Textbook of Endocrinology. 14th ed. Philadelphia, PA: Elsevier; 2020:chap 36.
American Diabetes Association Professional Practice Committee. 2. Classification and diagnosis of diabetes: standards of care in diabetes-2024. Diabetes Care. 2024;47(Suppl 1):S20-S42. PMID: 38078589 pubmed.ncbi.nlm.nih.gov/38078589/.
Riddle MC, Ahmann AJ. Therapeutics of type 2 diabetes mellitus. In: Melmed S, Auchus RJ, Goldfine AB, Koenig RJ, Rosen CJ, eds. Williams Textbook of Endocrinology. 14th ed. Philadelphia, PA: Elsevier; 2020:chap 35.
US Preventive Services Task Force website. Final recommendation statement: Prediabetes and type 2 diabetes: Screening. www.uspreventiveservicestaskforce.org/uspstf/recommendation/screening-for-prediabetes-and-type-2-diabetes. Released August 24, 2021. Accessed February 20, 2024.
US Preventive Services Task Force website. Final recommendation statement: Prediabetes and type 2 diabetes in children and adolescents: Screening. www.uspreventiveservicestaskforce.org/uspstf/recommendation/prediabetes-type2-diabetes-children-adolescents-screening. Released September 13, 2022. Accessed February 20, 2024.
Updated by: Sandeep K. Dhaliwal, MD, board-certified in Diabetes, Endocrinology, and Metabolism, Springfield, VA. Internal review and update on 02/20/2024 by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.