A Method for Purifying Obligate Intracellular Coxiella burnetii that Employs Digitonin Lysis of Host Cells (original) (raw)
. Author manuscript; available in PMC: 2008 Mar 31.
Published in final edited form as: J Microbiol Methods. 2008 Jan 12;72(3):321–325. doi: 10.1016/j.mimet.2007.12.015
Abstract
Purification of the obligate intracellular bacterium Coxiella burnetii requires physical disruption of infected cells. Here we describe a gentle and safe digitonin lysis procedure to release C. burnetii from infected cells. The purity, yield, and infectivity of digitonin-prepped organisms are comparable to that of organisms purified using cell lysis by sonication.
Coxiella burnetii is an obligate intracellular bacterium and the causative agent of human Q fever, a debilitating influenzae-like illness (Maurin and Raoult, 1999). The organism is highly infectious via the aerosol route, with a human infectious dose of less than 10 organisms (Benenson and Tigertt, 1956). Consequently, biosafety level 3 laboratory procedures are required for propagation and other manipulations of the organism. Infection of cultured mammalian cell lines is the preferred method of cultivating the pathogen although laboratory animals (primarily guinea pigs and mice) and embryonated hen’s eggs are also used (Maurin and Raoult, 1999). Commonly employed continuous cell lines that support vigorous growth of the organism include Vero (African green monkey kidney epithelial) (Coleman et al., 2004), BHK-21 (hamster kidney fibroblast) (Miller et al., 2004), L-929 (murine fibroblast) (Baca and Paretsky, 1983), and J774.1 (murine macrophage-like) (Brennan et al., 2004) cells. Intracellularly, C. burnetii replicates in a specialized membrane-bound parasitophorous vacuole (PV) with lysosomal characteristics (Voth and Heinzen, 2007). Optimal yields of C. burnetii are obtained when purifications are conducted during the stationary phase of the organism’s growth cycle. In Vero cells, this occurs at approximately 6 days post-infection, a time point at which large parasite-containing vacuoles are easily visible by phase contrast light microscopy (Coleman et al., 2004).
Owing to the intra-vacuolar niche of C. burnetii, disruption of not only the plasma membrane, but also the bacterium-containing vacuole, is required for purification of organisms from host cell material. A variety of cell disruption methods have been used in C. burnetii purification schemes including osmotic lysis by distilled water (Zamboni and Rabinovitch, 2003), shearing by passage through a syringe needle (Beron et al., 2002), vortexing in the presence of glass beads (Veras et al., 1994), blending in a tissue homogenizer (Baca et al., 1993) and cavitation using a sonic disruptor (Meconi et al., 1998). However, these methods are potentially hazardous for laboratory personnel and/or may damage the fragile large cell variant (LCV) developmental form of C. burnetii (Coleman et al., 2004). Regardless of the host cell lysis method, purification of C. burnetii from lysates involves a series of differential centrifugation steps including centrifugation through sucrose or RenoCal-76 (Weiss et al., 1975; Williams et al., 1981; Samuel et al., 1983).
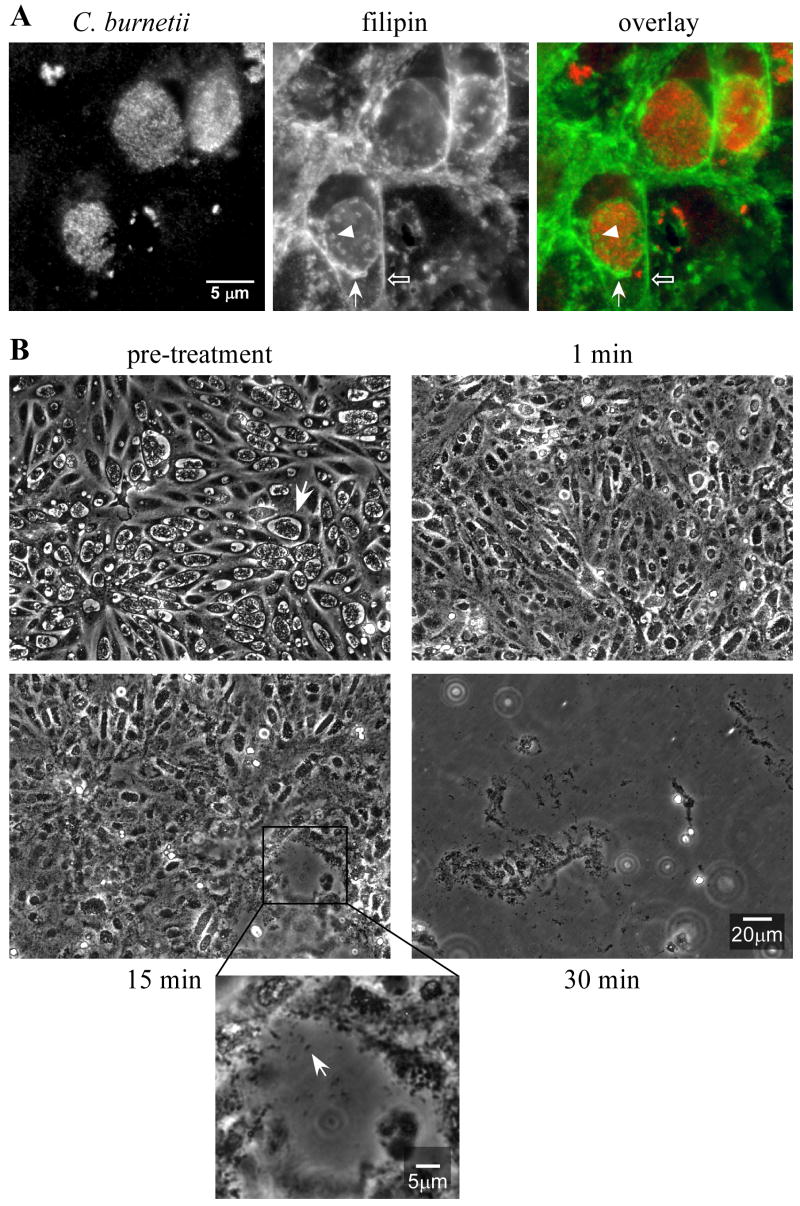
We recently discovered that the C. burnetii PV membrane, but not C. burnetii, is rich in cholesterol (Howe and Heinzen, 2006) (Fig. 1a). This prompted us to investigate whether a solution containing digitonin could be used to gently release organisms from infected host cells as an initial step in purification. Digitonin is a plant glycoalkaloid saponin detergent that forms water insoluble complexes with cholesterol, thereby dissolving cholesterol-rich membranes such as the plasma membrane (Lange et al., 1989; Paila et al., 2005). Here, we directly compare yield, infectivity, and relative purity of C. burnetii purified using a digitonin cell lysis procedure to those purified using a sonication lysis procedure.
Fig. 1.
The C. burnetii PV membrane is cholesterol-rich and solubilizes following treatment with SPD, a digitonin-containing buffer (A) Vero cells were infected with C. burnetii for 6 days, then fixed with methanol. C. burnetii (red) was stained by indirect immunofluorescence and cholesterol (green) was stained with filipin as previously described (Howe and Heinzen, 2006). Epifluorescence images show filipin labeling of the C. burnetii PV membrane (solid arrow) that is comparable to that of the cholesterol-rich plasma membrane (open arrow). Cholesterol-rich host material is also evident in the PV lumen (arrowhead) (B) Phase contrast light micrographs showing a time course of dissolution of a _Coxiella_-infected Vero cell monolayer during a 30 min treatment with SPD buffer. Prototypic phase-translucent and spacious replication vacuoles harboring Nine Mile phase II Coxiella are evident before treatment (arrow). After a 1 min treatment, the vacuolar membrane collapses and vacuoles lose their spacious appearance. Around 15 min post-treatment, holes in the monolayer begin to appear with a corresponding release of Coxiella (inset, arrow). At 30 min post-treatment, nearly the entire monolayer has disintegrated and extracellular Coxiella have become clearly visible. (Note: each micrograph is a different field of view.)
Confluent Vero cells (CCL-81, American Type Culture Collection) in 12 T-150 flasks were infected with avirulent C. burnetii Nine Mile, phase II, clone 4 (RSA439) at a multiplicity of infection of approximately 10. Infected cells were cultivated in 40 ml of RPMI medium (Invitrogen) supplemented with 10% fetal bovine serum for 8 days. Cell monolayers in 6 flasks were then subjected in parallel to digitonin and sonication lysis procedures. For digitonin lysis, tissue culture media was removed from each flask and monolayers briefly rinsed with 10 ml of phosphate buffered saline (PBS: 12.8 mM KH2PO4, 72.6 mM NaCl, 53.9 mM Na2HPO4, pH 7.4) containing 250 mM sucrose (SP buffer). Five ml of SP buffer containing 0.2 mg ml−1 digitonin (Fluka) (SPD buffer) was then added to each flask and the flasks incubated for 30 min at room temperature with gentle rocking. (Note: digitonin and digitonin solutions should be handled with care.) A time course observation during this treatment by phase contrast light microscopy revealed near complete dissolution of the cell monolayer with release of Coxiella (Fig. 1b). The buffer and insoluble cell debris clot were then transferred to 50 ml conical centrifuge tubes on ice. To extract the small amount of remaining monolayer, 5 ml of SPD buffer was added to each flask and the flasks incubated for 15 min at room temperature with gentle rocking. The buffer was removed and pooled with the first SPD lysate. Flasks were then rinsed with 5 ml of SPD buffer, which was also added to the existing SPD lysate.
For sonication lysis, infected cell monolayers were detached into the culture medium with a cell scraper. The medium containing infected cells was transferred to a 250 ml centrifuge bottle. Flasks were serially rinsed with 10 ml of SP, and the rinse solution transferred to the centrifuge bottle. Infected cells were pelleted by centrifugation at 21,000 × g for 15 min at 4° C. This centrifugation step also pellets C. burnetii that were released into the culture medium due to the scraping process. After centrifugation, the supernatant was discarded, the pellet resuspended in 30 ml of SP buffer, and the solution transferred to a sterile disposable 250 ml plastic beaker on ice. Infected cells were then lysed by two-15 sec sonication treatments at medium output (45 watts) using an Ultrasonics Model W-225R sonic disrupter equipped with a 0.5-inch sonication horn (Ultrasonics, Inc., Plainview, NY). Cell lysates were cooled on ice for 30 sec between each sonication. Lysates were then transferred to a 50 ml conical centrifuge tube on ice.
SPD and sonication-derived lysates were now processed identically. Insoluble cell debris in SPD lysates, and unbroken cells and nuclei in sonication lysates, were pelleted by centrifugation at 900 × g for 5 min at 4° C. Supernatants containing released C. burnetii were transferred to a 50 ml Oakridge O-ringed screw cap centrifuge tube and organisms pelleted by centrifugation at 31,000 × g for 15 min at 4° C. The supernatant was discarded and C. burnetii resuspended in 20 ml of SP buffer on ice. The C. burnetii suspension was then overlaid onto two-8 ml cushions consisting of a 30% solution (v/v) of RenoCal-76 (Bracco Diagnostics, Inc., Princeton, NJ) in SP buffer in 25 × 89 Ultra Clear centrifuge tubes (Beckman). The tubes were filled with SP and centrifuged at 58,400 × g for 30 min at 4° C. Following this procedure, most insoluble, buoyant host cell material remains at the RenoCal/SP interface while the organisms form a pellet. The supernatant was gently removed, and the two C. burnetii pellets resulting from each lysis procedure were each resuspended in a total of 20 ml cold (4° C) SP. Suspended organisms were transferred to a 50 ml Oakridge O-ringed screw cap centrifuge tube, the tube filled with cold (4° C) SP buffer, and C. burnetii pelleted by centrifugation at 31,000 × g for 15 min at 4° C. The supernatant was discarded and each sample resuspended in 6 ml of SP buffer. Purified C. burnetii was aliquoted and stored at −80° C.
In some experiments, organisms were subjected to an additional purification step by centrifugation to equilibrium in a 40%/44%/54% RenoCal-76 step gradient. Gradients were prepared in 25 × 89 Ultra Clear centrifuge tubes using 54% (8 ml), 44% (12 ml) and 40% (5 ml) solutions (v/v) of RenoCal-76 in SP buffer. Each 20 ml C. burnetii suspension following the 30% RenoCal-76 cushion was overlaid equally onto two step gradients. The tubes were then filled with SP and centrifuged at 58,400 × g for 60 min at 4° C. During this procedure, C. burnetii forms a band at the 44/54% RenoCal-76 interface. Using a pipette, organisms were carefully removed and transferred to a 50 ml Oakridge O-ringed screw cap centrifuge tube on ice. Tubes were filled with cold (4° C) SP and centrifuged at 31,000 × g for 15 min at 4° C to pellet C. burnetii. The supernatant was discarded and each sample resuspended in 6 ml of SP buffer. Purified C. burnetii was aliquoted and stored at −80° C.
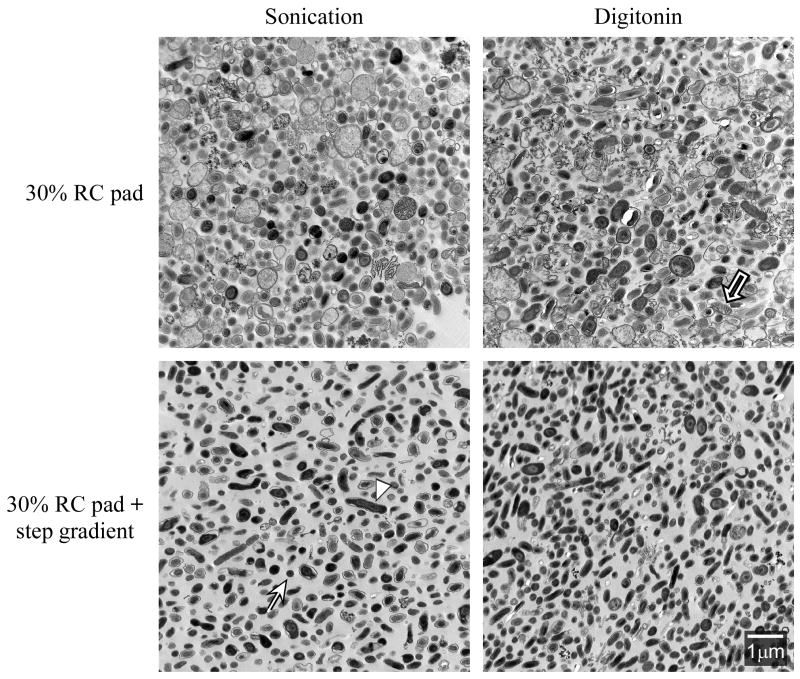
To assess the relative purity of C. burnetii following SPD and sonication purification procedures, transmission electron microscopy was conducted as previously described (Coleman et al., 2007). As depicted in Fig. 2, both small cell variants (SCV), with electron-dense compacted chromatin, and LCV, with dispersed chromatin, were significantly enriched in both SPD and sonication-prepped samples pelleted through a 30% RenoCal-76 pad. However, contaminating host material, largely consisting of damaged or intact mitochondria, was evident in roughly equal amounts in each sample. By subjecting samples to the additional RenoCal-76 step gradient, C. burnetii in both preparations was purified to near homogeneity.
Fig. 2.
Transmission electron micrographs of sonication and SPD-prepped C. burnetii. Transmission electron micrographs of sonication and SPD-prepped organisms after centrifugation through a 30% RenoCal cushion show that both preparations are highly enriched for C. burnetii (upper panels). Contaminating host cell material is also present, mostly in the form of intact or damaged mitochondria displaying characteristic cristae (black arrow). Substantially less host cell contamination is observed with organisms following an additional 40/44/54% RenoCal-76 step gradient (lower panels). Prototypic C. burnetii SCV and LCV developmental forms are denoted with an arrow and arrowhead, respectively. Abbreviation: RC, RenoCal-76.
We next compared the relative yield and infectivity of C. burnetii prepared by SPD and sonication lysis procedures. A 30% RenoCal-76 pad-purification was performed in triplicate for each lysis procedure. For each purification, infectivity for Vero cells was enumerated by immunofluorescence detection of infectious focus-forming units (FFU) and yield was determined by TaqMan quantitative PCR of genome equivalents (GE). Both of these procedures were conducted as previously described (Coleman et al., 2007). When averaged, SPD and sonication protocols yielded similar numbers of C. burnetii genome equivalents (2.85 and 2.70 × 1010 GE ml−1, respectively) (Table 1). On average, these preparations were also equally infectious with 4.79 and 4.62 and × 109 FFU ml−1 obtained with SPD and sonication-prepped C. burnetii, respectively. This result was important in showing that digitonin treatment did not adversely affect C. burnetii infectivity. Moreover, similar GE/FFU ratios were also observed for virulent C. burnetii Nine Mile phase I (RSA493) purified by SPD and sonication lysis procedures (data not shown), suggesting the SPD procedure is applicable to purification of C. burnetii strains differing in virulence and other phenotypes.
Table 1.
Comparison of yield and infectivity of C. burnetii purified using digitonin and sonication cell lysis procedures
| Purification | GE (× 1010 ml−1) | FFU (× 109 ml−1) | GE/FFU | |||
|---|---|---|---|---|---|---|
| Son | SPD | Son | SPD | Son | SPD | |
| 1 | 4.28 | 3.64 | 4.14 | 4.40 | 10.30 | 8.30 |
| 2 | 1.50 | 1.28 | 4.18 | 3.50 | 3.59 | 3.66 |
| 3 | 2.32 | 3.62 | 5.55 | 6.46 | 4.18 | 5.60 |
| Mean±SD: | 2.70±1.43 | 2.85±1.36 | 4.62±0.80 | 4.79±1.52 | 6.02±3.72 | 5.85±2.33 |
In summary, this study indicates that SPD lysis is an effective alternative procedure for isolating obligate intracellular C. burnetii from cell culture. Sonic disruption is routinely employed to release C. burnetii (Meconi et al., 1998) and other intracellular pathogens (Caldwell et al., 1981; Eremeeva and Silverman, 1998) from infected cells. However, C. burnetii is notorious for causing laboratory acquired infections (Johnson and Kadull, 1966) and sonication, with its potential to generate infectious aerosols, presents an occupational hazard for laboratory personnel. By exploiting a biochemical property of _Coxiella_’s vacuolar compartment (cholesterol content), we devised a mild chemical extraction procedure using digitonin that releases intracellular organisms. Some host cell contamination was observed with organisms purified only through the 30% RenoCal-76 pad. This contamination was largely eliminated with an additional separation on a RenoCal-76 step gradient. For this study, we used an avirulent phase II strain of C. burnetii. Phase II organisms differ from virulent phase I organisms in producing a severely truncated lipopolysaccharide (Williams et al., 1981). This characteristic renders phase II organisms highly hydrophobic (Williams et al., 1981), a property that may exacerbate the contamination observed in 30% pad-only preparations. The digitonin lysis procedure described herein may be broadly applicable to purification of other intracellular parasites.
Acknowledgments
We thank Harlan Caldwell and Shelly Robertson for critical reading of this manuscript, and Gary Hettrick for graphics. This research was supported by the Intramural Research Program of the National Institutes of Health, National Institute of Allergy and Infectious Diseases.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Baca OG, Paretsky D. Q fever and Coxiella burnetii: a model for host-parasite interactions. Microbiol Rev. 1983;47:127–149. doi: 10.1128/mr.47.2.127-149.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baca OG, Roman MJ, Glew RH, Christner RF, Buhler JE, Aragon AS. Acid phosphatase activity in Coxiella burnetii: a possible virulence factor. Infect Immun. 1993;61:4232–4239. doi: 10.1128/iai.61.10.4232-4239.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benenson AS, Tigertt WD. Studies on Q fever in man. Trans Assoc Am Physicians. 1956;69:98–104. [PubMed] [Google Scholar]
- Beron W, Gutierrez MG, Rabinovitch M, Colombo MI. Coxiella burnetii localizes in a Rab7-labeled compartment with autophagic characteristics. Infect Immun. 2002;70:5816–5821. doi: 10.1128/IAI.70.10.5816-5821.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brennan RE, Russell K, Zhang G, Samuel JE. Both inducible nitric oxide synthase and NADPH oxidase contribute to the control of virulent phase I Coxiella burnetii infections. Infect Immun. 2004;72:6666–6675. doi: 10.1128/IAI.72.11.6666-6675.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caldwell HD, Kromhout J, Schachter J. Purification and partial characterization of the major outer membrane protein of Chlamydia trachomatis. Infect Immun. 1981;31:1161–1176. doi: 10.1128/iai.31.3.1161-1176.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman SA, Fischer ER, Cockrell DC, Voth DE, Howe D, Mead DJ, Samuel JE, Heinzen RA. Proteome and antigen profiling of Coxiella burnetii developmental forms. Infect Immun. 2007;75:290–298. doi: 10.1128/IAI.00883-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman SA, Fischer ER, Howe D, Mead DJ, Heinzen RA. Temporal analysis of Coxiella burnetii morphological differentiation. J Bacteriol. 2004;186:7344–7352. doi: 10.1128/JB.186.21.7344-7352.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eremeeva ME, Silverman DJ. Rickettsia rickettsii infection of the EA.hy 926 endothelial cell line: morphological response to infection and evidence for oxidative injury. Microbiology. 1998;144:2037–2048. doi: 10.1099/00221287-144-8-2037. [DOI] [PubMed] [Google Scholar]
- Howe D, Heinzen RA. Coxiella burnetii inhabits a cholesterol-rich vacuole and influences cellular cholesterol metabolism. Cell Microbiol. 2006;8:496–507. doi: 10.1111/j.1462-5822.2005.00641.x. [DOI] [PubMed] [Google Scholar]
- Johnson JE, Kadull PJ. Laboratory-acquired Q fever. A report of fifty cases. Am J Med. 1966;41:391–403. doi: 10.1016/0002-9343(66)90085-4. [DOI] [PubMed] [Google Scholar]
- Lange Y, Swaisgood MH, Ramos BV, Steck TL. Plasma membranes contain half the phospholipid and 90% of the cholesterol and sphingomyelin in cultured human fibroblasts. J Biol Chem. 1989;264:3786–3793. [PubMed] [Google Scholar]
- Maurin M, Raoult D. Q fever. Clin Microbiol Rev. 1999;12:518–553. doi: 10.1128/cmr.12.4.518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meconi S, Jacomo V, Boquet P, Raoult D, Mege JL, Capo C. Coxiella burnetii induces reorganization of the actin cytoskeleton in human monocytes. Infect Immun. 1998;66:5527–5533. doi: 10.1128/iai.66.11.5527-5533.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller JD, Curns AT, Thompson HA. A growth study of Coxiella burnetii Nine Mile Phase I and Phase II in fibroblasts. FEMS Immunol Med Microbiol. 2004;42:291–297. doi: 10.1016/j.femsim.2004.06.003. [DOI] [PubMed] [Google Scholar]
- Paila YD, Pucadyil TJ, Chattopadhyay A. The cholesterol-complexing agent digitonin modulates ligand binding of the bovine hippocampal serotonin 1A receptor. Mol Membr Biol. 2005;22:241–249. doi: 10.1080/09687860500093453. [DOI] [PubMed] [Google Scholar]
- Samuel JE, Frazier ME, Kahn ML, Thomashow LS, Mallavia LP. Isolation and characterization of a plasmid from phase I Coxiella burnetii. Infect Immun. 1983;41:488–493. doi: 10.1128/iai.41.2.488-493.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veras PS, de Chastellier C, Moreau MF, Villiers V, Thibon M, Mattei D, Rabinovitch M. Fusion between large phagocytic vesicles: targeting of yeast and other particulates to phagolysosomes that shelter the bacterium Coxiella burnetii or the protozoan Leishmania amazonensis in Chinese hamster ovary cells. J Cell Sci. 1994;107:3065–3076. doi: 10.1242/jcs.107.11.3065. [DOI] [PubMed] [Google Scholar]
- Voth DE, Heinzen RA. Lounging in a lysosome: the intracellular lifestyle of Coxiella burnetii. Cell Microbiol. 2007;9:829–840. doi: 10.1111/j.1462-5822.2007.00901.x. [DOI] [PubMed] [Google Scholar]
- Weiss E, Coolbaugh JC, Williams JC. Separation of viable Rickettsia typhi from yolk sac and L cell host components by renografin density gradient centrifugation. Appl Microbiol. 1975;30:456–463. doi: 10.1128/am.30.3.456-463.1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams JC, Peacock MG, McCaul TF. Immunological and biological characterization of Coxiella burnetii, phases I and II, separated from host components. Infect Immun. 1981;32:840–851. doi: 10.1128/iai.32.2.840-851.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zamboni DS, Rabinovitch M. Nitric oxide partially controls Coxiella burnetii phase II infection in mouse primary macrophages. Infect Immun. 2003;71:1225–1233. doi: 10.1128/IAI.71.3.1225-1233.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]