Rethinking Prevention in Primary Care: Applying the Chronic Care Model to Address Health Risk Behaviors (original) (raw)
Abstract
This study examines the Chronic Care Model (CCM) as a framework for preventing health risk behaviors such as tobacco use, risky drinking, unhealthy dietary patterns, and physical inactivity. Data were obtained from primary care practices participating in a national health promotion initiative sponsored by the Robert Wood Johnson Foundation. Practices owned by a hospital health system and exhibiting a culture of quality improvement were more likely to offer recommended services such as health risk assessment, behavioral counseling, and referral to community-based programs. Practices that had a multispecialty physician staff and staff dieticians, decision support in the form of point-of-care reminders and clinical staff meetings, and clinical information systems such as electronic medical records were also more likely to offer recommended services. Adaptation of the CCM for preventive purposes may offer a useful framework for addressing important health risk behaviors.
Keywords: Chronic Care Model, health promotion/disease prevention, health risk behaviors, primary care practice
Half the mortality from the ten leading causes of death in the United States is due to preventable lifestyle-related behaviors that cause or exacerbate chronic illness (McGinnis and Foege 1993; Mokdad et al. 2004). Behaviors such as tobacco use, risky drinking, unhealthy dietary patterns, and physical inactivity are risk factors for many chronic diseases and are currently the nation's leading causes of death and disability (U.S. Department of Health and Human Services 2000). Owing to their impact on public health and the U.S. health care system, addressing multiple risk behaviors has become an urgent health priority (Pronk, Peek, and Goldstein 2004). Although behavioral modification can decrease morbidity and mortality and increase quality of life (Koop 1996), the opportunities to address patients' health behaviors in strategic settings such as primary care practices often are missed (Green et al. 2001; Kottke et al. 1997; Lewis 1988; Woolf and Atkins 2001).
With support from the Robert Wood Johnson Foundation's Improving Chronic Illness Care (ICIC) program, the Chronic Care Model (CCM) was developed as a comprehensive framework for managing chronic illness (Wagner 1998; Wagner, Austin, and Von Korff 1996a, 1996b). The CCM was motivated by the growing numbers of people with chronic diseases and also the deficiencies in the current efforts to manage them. These deficiencies include lapses in the ability of rushed practitioners to follow established practice guidelines, lack of care coordination, lack of active follow-up to ensure best outcomes, and inadequate education or training of patients to manage their illnesses (Improving Chronic Illness Care 2006a). There is a growing sense that overcoming these deficiencies will require a major transformation, in which the health care system shifts from its current focus on reacting to illness (i.e., responding mainly when a person is sick) to a more proactive focus on promoting health and preventing disease in individuals and populations (Calkins et al. 1999; Wagner, Austin, and Von Korff 1996a, 1996b).
The CCM identifies six essential elements of a health care system that facilitate high-quality care (Figure 1). Community resources and policies support care through community programs and local or state policies advocating improvements in health care. These resources and policies may include partnerships with community organizations to identify, create, and support needed services. The health system organization of care promotes a culture of quality improvement along with the means of providing safe, high-quality care. This is achieved through senior leadership support for quality improvement, the open and systematic handling of errors, and effective care coordination within and across organizations. Self-management support emphasizes patients' responsibility in managing their health through such strategies as setting goals, resolving problems, and devising action plans.
figure 1.
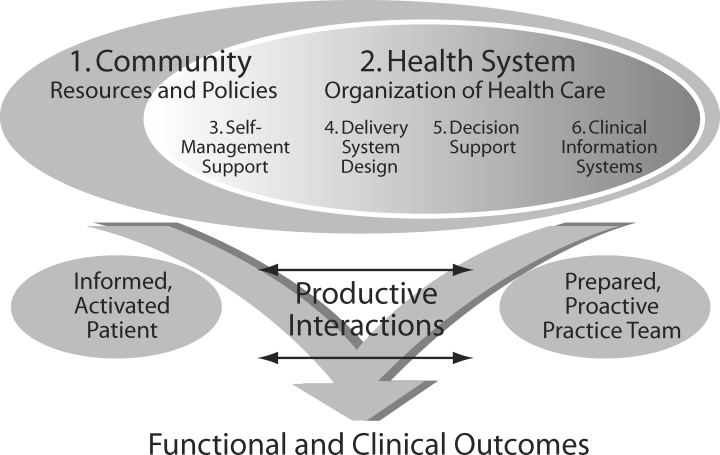
The Chronic Care Model
Source: Wagner 1998.
An effective delivery system design facilitates well-planned patient visits and may include specialist expertise or clinical case management services for complex cases. Decision support enhances adherence to evidence-based guidelines, which are incorporated in daily clinical practice through system reminders or prompts and are reinforced through provider training or other decision support mechanisms. Last, clinical information systems provide access to patient data and can be used to plan an individual patient's care, identify relevant subpopulations for care, and monitor the performance of health care providers or systems. The combination of these six elements fosters interaction between informed patients and prepared providers that may improve patient outcomes (Improving Chronic Illness Care 2006b).
The CCM is a heuristic tool that can be applied to a variety of chronic conditions, care settings, and populations. Experts also have suggested that the CCM may be an effective template for improving prevention because of the many similarities between preventive care and management of chronic diseases (Glasgow et al. 2001). Ideally, both would use a proactive rather than a reactive approach because regularly planned care, even in the absence of symptoms, is often more effective than treating symptoms after they develop. Both preventive care and management of chronic diseases also emphasize the importance of screening and counseling for specific target behaviors (e.g., eating habits, sedentary lifestyle, substance abuse), since the health issues related to chronic and preventive care often are complex and involve multiple risk factors. On a practical level, care can be delivered more rapidly when following a general set of principles, as is the case with the CCM, rather than when changes are made case by case. Since both preventing disease and managing chronic diseases are important functions of primary care, changes in practice may have a greater impact if similar strategies are used for both purposes.
Our study contributes empirically to this discussion by exploring whether the CCM can be used as a framework for delivering preventive services to modify risk behaviors as recommended by the U.S. Preventive Services Task Force (2005). We consider three main research questions: (1) To what extent do primary care practices offer behavior change interventions; (2) To what extent have real-world primary care practices implemented various components of the CCM; and (3) What are the associations between each of these CCM components and the use of recommended preventive services to address health risk behaviors?
Conceptual Framework and Study Hypotheses
Most studies to date have examined the CCM in relation to the management of chronic care or the health outcomes of chronically ill patients (Bodenheimer, Wagner, and Grumbach 2002b; Bonomi et al. 2002; Glasgow et al. 2005; Sperl-Hillen et al. 2004; Stroebel et al. 2005; Tsai et al. 2005; Wagner, Glasgow, et al. 2001). Our research, however, focuses on the use of preventive services such as health risk assessments, individual and group counseling, and referral to community-based programs to address patients' health risk behaviors. We examine whether clinical care approaches as defined by the CCM are associated with interventions targeting the behaviors of tobacco use, risky drinking, unhealthy dietary patterns, and physical inactivity.
Health System Organization of Care
Primary care practices may be influenced by wider health system incentives, reimbursement policies, and values (Wagner, Austin, et al. 2001). Small primary care practices typically have limited resources for preventive care, making it difficult to pay for the personnel or infrastructure to support organizational changes that could encourage health promotion and disease prevention. Affiliation with a larger entity invested in positive health outcomes may provide the support necessary for formal prevention efforts. Accordingly, we hypothesize that the primary care practices of a hospital health system, as compared with those of other entities (e.g., clinician, public sponsor), may be more likely to support behavior change interventions (hypothesis 1).
The health system organization element in the CCM also emphasizes visible leadership support for high-quality care and an open culture that promotes quality improvement (QI) efforts. High-quality care may be reflected in the availability of a wide range of patient services, including those addressing and improving health-related behaviors. Earlier research found that health care organizations characterized by participative, flexible, and innovative cultures were associated with successful quality improvement (Carman et al. 1996; Shortell et al. 1995). In this article, we hypothesize that practices with similar organizational cultures may be the most likely to offer services to modify patients' risk behaviors (hypothesis 2).
Self-Management Support
The CCM's self-management support element helps show patients how to participate in their own care (Bodenheimer et al. 2002; Wagner, Austin, and Von Korff 1996a, 1996b), including reminding them of their action plan goals, informing them about targeted health areas, and following up on their progress. Making patients aware of preventive steps also is important (Solberg, Kottke, and Brekke 1998) and works well for lifestyle modification efforts involving smoking cessation, dietary changes, and physical activity (Barr et al. 2003). Despite the many forms of self-management support, in this study we examined only the use of mailed patient reminder cards, as earlier research found that the use of reminder cards can aid preventive efforts (Glasgow et al. 2001). Here we examine whether the use of patient reminder cards encourages targeted preventive interventions to address risk behaviors (hypothesis 3).
Delivery System Design
Building a capacity to support prevention includes creating care delivery teams to address various risk factors and health risk behaviors. Primary care practices with specialist physicians as well as health professionals with expertise in areas like nutrition or smoking cessation may be important when addressing complex cases. Primary care delivery system designs may include specialist physicians' involvement in primary care (Bodenheimer et al. 2002; Pearson et al. 2005; Sperl-Hillen et al. 2004; Wagner, Austin, et al. 2001) and the use of specialized health professionals (Bodenheimer, Wagner, and Grumbach 2002b; Wagner 2000; Wagner, Glasgow, et al. 2001). Interventions addressing patients' risk factors and behaviors thus may be more common in primary care practices with a multispecialist physician staff (hypothesis 4). In addition, practices that employ staff dieticians may be more likely to offer specific preventive services regarding patients' dietary patterns (hypothesis 5).
Decision Support
Decision support refers to interventions or activities that improve providers' knowledge and skills (Wagner, Austin, et al. 2001). The purpose of this component of the CCM is to facilitate evidence-based clinical care. But even though treatment decisions based on evidence-based guidelines are important starting points, research has found that such guidelines have limited effectiveness unless they are integrated into practice through the use of point-of-care reminders for clinicians and other facilitative mechanisms (Woolf et al. 1999). While the U.S. Preventive Services Task Force (2005) has established guidelines for clinical preventive care, providers may not be aware of or motivated to perform these recommended services unless there is ongoing support. Past studies have identified various reminders and prompts for clinicians (Bodenheimer et al. 2002; Pearson et al. 2005; Solberg et al. 2000; Wagner, Glasgow, et al. 2001; Wagner et al. 2005), chart reviews to assess care and clinical outcomes (Bonomi et al. 2002; Wagner, Glasgow, et al. 2001), and regular meetings among physicians to coordinate care (Bodenheimer, Wagner, and Grumbach 2002b;Bonomi et al. 2002) as forms of decision support. Thus we expect that delivery of evidence-based preventive services may be more common in practices that use prompts like chart stickers to identify patients with various risk factors, for example, smoking or risky drinking (hypothesis 6); regular review of patients' charts (hypothesis 7); checklists or flowcharts to help manage diseases (hypothesis 8); and clinical staff meetings to coordinate care (hypothesis 9).
Clinical Information Systems
Clinical information systems, such as registries to monitor patient populations and electronic medical records to manage individual patients' data, are essential to effective chronic care programs and care management (Bodenheimer, Wagner, and Grumbach 2002a; Bonomi et al. 2002; Casalino et al. 2003; Rundall et al. 2002; Wagner et al. 1999; Wagner, Austin, et al. 2001). Information systems can also be useful in prompting and assisting preventive care efforts and have been used in a variety of ways, like disseminating evidence-based guidelines, providing performance feedback, and planning patient visits (Wagner, Glasgow, et al. 2001). Organized management of data and sophisticated distribution of health information may help practices monitor preventive health needs more effectively. Therefore, we hypothesize that practices using patient registries (hypothesis 10) and electronic medical records (hypothesis 11) may be more likely to provide preventive services that address health risk behaviors.
The CCM community resources and policies element supports and expands care for patients and may include community programs, local or state health policies, insurance benefits, and advocacy groups. While we do not explore this element due to the unavailability of appropriate measures, we believe that the community may be an important conduit for broad-based action in promoting health and preventing disease beyond the clinical setting, which we will discuss further.
Methods
Data Sources
This research used data collected from the Prescription for Health program, a national health promotion initiative sponsored by the Robert Wood Johnson Foundation. The initiative funded seventeen research projects that implemented innovative programs targeting two or more of the following health risk behaviors: tobacco use, risky drinking, unhealthy dietary patterns, and physical inactivity. All the primary care practices participating in these studies were members of practice-based research networks affiliated with the Agency for Healthcare Research and Quality (AHRQ) and were located in the northeastern, southern, midwestern, and western regions of the United States. None of the practices were owned by prevention-focused health care delivery systems such as health maintenance organizations, and none offered formal reimbursements for delivering preventive care.
All the practices participating in the initiative were asked to complete two cross-sectional survey instruments: the Practice Information Form (PIF) and the Practice Staff Questionnaire (PSQ). Each practice was to complete one PIF. This survey was designed to obtain a general description of each primary care practice (e.g., type of practice, staffing patterns, characteristics of patient panel) and was completed by a clinic administrator, medical director, or other staff member at each site. The PIF was sent to 124 primary care practices, and 104 practices returned a completed questionnaire (84 percent). The PSQ was distributed to all clinical and administrative members of the participating practices and measured the performance of clinical activities, the use of clinical tools or reminder systems, and perceptions of the work environment. To make sure that the PSQ responses represented a reasonable cross section of each practice's staff, we analyzed only those practices with at least a 50 percent PSQ response rate. Of the primary care practices that returned a PIF, fifty-two met the minimum PSQ response rate, so our study sample consisted of those fifty-two practices that both returned the PIF and had a 50 percent PSQ completion rate (_n_= 318). Further analysis comparing these fifty-two study practices with the excluded practices (those that did not have a 50 percent PSQ response rate) yielded no significant differences among the study variables except for the use of patient reminder cards. On average, our study practices reported using patient reminder cards 53 percent more frequently than did the excluded practices.
Measures
The outcome variables for this study were the practices' use of four preventive services as reported on the PSQ: health risk assessments, referral to community-based programs, individual counseling, and group counseling conducted within the practice. We selected these items based on the U.S. Preventive Services Task Force's recommendations and their identification as core services in a new model of family medicine created by the Future of Family Medicine Task Force (Green et al. 2004). Each service was assessed on four health behaviors: tobacco use, risky drinking, unhealthy dietary patterns, and physical inactivity. In addition, individual counseling was examined with regard to unhealthy dietary patterns alone. The responses for each behavior ranged from 0 (never) to 4 (always) and were averaged to obtain a mean score for each preventive service. This method of averaging behaviors within each service was validated by principal components analysis, which yielded four separate components with eigenvalues > 1.0 and factor-loading coefficients > 0.65. All components demonstrated high internal consistency and reliability with Cronbach alpha coefficients > 0.84. We then aggregated the preventive service scores to obtain a median score for each practice. This aggregation to the practice level was justified by significant analysis of variance results, which confirmed greater between-practice than within-practice variation (p < 0.001).
We examined various practice features as independent variables based on the CCM framework and measured two features consistent with the health system organization component of the CCM as follows: The practice ownership was binary coded, with “1” indicating practices owned by a hospital health system and “0” indicating ownership by a clinician(s), university, or public sponsor. The practice culture (i.e., shared values, norms, and beliefs) was used to identify practices that would likely value high-quality care and promote QI efforts. We examined this construct using a competing values framework (Quinn and Kimberly 1984; Quinn and Rohrbaugh 1981) that was adapted and used to evaluate culture in health care settings (Carman et al. 1996; Shortell et al. 1995; Shortell et al. 2000; Shortell et al. 2001). Data were collected on four variables that measured on a scale from 0 to 100 the degree of various culture types in a practice: (1) group-oriented, reflecting trust and belonging; (2) developmental, reflecting flexibility and innovation; (3) hierarchical, emphasizing security and stability; and (4) rational, emphasizing efficiency and pragmatism. Based on prior research, we combined the group-oriented and developmental culture scores to represent a practice culture likely to value quality improvement goals (Carman et al. 1996; Shortell et al. 1995).
The CCM's self-management support element was measured by the frequency with which a practice used patient reminder cards. This measure was based on a five-point Likert scale and rescaled to equal intervals from 0 to 1 (0 = never, 0.25 = rarely, 0.50 = occasionally, 0.75 = usually, 1 = always). The delivery system design included practice specialty type, which was binary coded as “1” indicating a multispecialty and “0” indicating a single-specialty physician staff. In our study sample, a multispecialty staff consisted of some combination of family physicians, pediatricians, internists, cardiologists, oncologists, and/or obstetricians. The number of full-time equivalent (FTE) dieticians employed by the practice also was included as a feature of the delivery system design.
Decision support was measured by how often the practices used risk factor chart stickers, checklists or flowcharts for disease management, and review of patient charts. These measures also were based on five-point Likert scales and rescaled to equal intervals ranging from 0 (never) to 1 (always). Another decision support measure was the frequency with which the practices held meetings to discuss clinical issues and was measured on a scale ranging from 0 (never) to 1 (daily). We examined clinical information systems using patient registries and electronic medical records. The frequency of using a registry to track patients with specific conditions was based on a five-point Likert scale ranging from 0 (never) to 1 (always). The use of electronic medical records was measured as a binary variable indicating whether electronic health records were used in the practice and was coded as “1,” yes, or “0,” no. Last, we included the practice's size, as defined by the number of its FTE employees, to control for possible effects on outcomes.
Statistical Analysis
We used multivariate regression analysis to examine the association between each CCM practice feature and the use of recommended preventive services to address health risk behaviors. Each of our five models had a different outcome pertaining to health risk assessment, individual counseling, group counseling, and referral to community programs for all health behaviors combined and also for individual counseling for diet alone. Each model also used an identical set of CCM elements to explain variances in the outcome measures.
Results
Table 1 describes the frequency with which the primary care practices used interventions recommended by the U.S. Preventive Services Task Force to address health risk behaviors. Practices reported occasionally assessing health risks and providing referrals to community programs and rarely offering individual or group counseling. The practices provided health risk assessments and referrals to community programs significantly more often than they offered behavioral counseling in the practice setting. The four health risk behaviors were addressed at similar levels, with tobacco use and dietary patterns significantly more often than risky drinking and physical inactivity.
TABLE 1.
Use of Recommended Preventive Services in Primary Care Practices (_n_= 52)
| Meana | SD | Range | |
|---|---|---|---|
| How often do you use a health risk assessment protocol or questionnaire to identify patients who may benefit from counseling or other interventions for the following? | 2.09 | 0.82 | (0–3.5) |
| Tobacco use | 2.36 | 1.09 | (0–4) |
| Risky drinking | 2.02 | 1.04 | (0–4) |
| Dietary patterns | 2.07 | 0.80 | (0–3.5) |
| Physical inactivity | 2.00 | 0.92 | (0–3.5) |
| How often do you use nurses or health educators in your practice for individual counseling to your patients with the following? | 1.42 | 0.69 | (0–3.5) |
| Tobacco use | 1.41 | 0.84 | (0–3.5) |
| Risky drinking | 1.20 | 0.77 | (0–3.5) |
| Dietary patterns | 1.66 | 0.77 | (0–3.5) |
| Physical inactivity | 1.37 | 0.75 | (0–3.5) |
| How often do you use group counseling in your practice for patients with the following? | 0.43 | 0.57 | (0–2.5) |
| Tobacco use | 0.49 | 0.62 | (0–2) |
| Risky drinking | 0.31 | 0.53 | (0–2) |
| Dietary patterns | 0.44 | 0.68 | (0–3) |
| Physical inactivity | 0.34 | 0.62 | (0–3) |
| How often do you refer your patients to community programs (e.g., patient education classes, support groups, and/or individual counseling) for the following? | 1.96 | 0.55 | (0.25–3) |
| Tobacco use | 1.91 | 0.73 | (0–4) |
| Risky drinking | 2.02 | 0.63 | (0–3) |
| Dietary patterns | 2.04 | 0.55 | (1–3) |
| Physical inactivity | 1.87 | 0.67 | (0–3) |
Table 2 describes the practices' characteristics and implementation of various CCM features. The most common type of owner was a hospital health system, followed by clinicians, universities, and public sponsors. A group-oriented organizational culture was the most common, followed by rational, hierarchical, and developmental cultures. Meetings to discuss clinical issues were held approximately once every month. The majority of practices were single specialty, and fewer than a quarter of our study practices reported using electronic medical records. Finally, the practices reported that they regularly used checklists or flowcharts to manage diseases, sometimes used patient reminder cards and chart reviews, and rarely used risk factor chart stickers and patient registries.
TABLE 2.
Practice Characteristics and Implementation of CCM Elements (_n_= 52)
| Mean or % | SD | Range | |
|---|---|---|---|
| Practice size (FTEs) | 17.9 | 15.6 | 1.5–64.7 |
| Health system organization of care | |||
| Practice ownership | |||
| Clinician (_n_= 13) | 25.0% | – | – |
| Hospital health system (_n_= 22) | 42.3% | – | – |
| University health system (_n_= 10) | 19.2% | – | – |
| Public sponsor (_n_= 7) | 13.5% | – | – |
| Practice culture | |||
| Group oriented | 34.6 | 11.2 | (17–58.5) |
| Developmental | 12.8 | 3.9 | (4–20) |
| Rational | 24.6 | 6.5 | (4.5–39) |
| Hierarchical | 24.4 | 8.6 | (12–55) |
| Self-management support | |||
| Patient reminder cards | 0.50 | 0.30 | (0–1) |
| Delivery system design | |||
| Specialty type | |||
| Single specialty (_n_= 40) | 76.9% | – | – |
| Multispecialty (_n_= 12) | 23.1% | – | – |
| Dietician FTEs (full-time equivalents) | 0.20 | 0.09 | (0–0.6) |
| Decision support | |||
| Risk factor chart stickers | 0.30 | 0.29 | (0–1) |
| Patient chart review | 0.52 | 0.21 | (0–1) |
| Checklists/flowcharts for disease management | 0.64 | 0.22 | (0–1) |
| Clinical staff meetings | 0.57 | 0.26 | (0–1) |
| Clinical information systems | |||
| Patient registry | 0.25 | 0.23 | (0–0.86) |
| Electronic medical record | |||
| Yes (_n_= 8) | 15.4% | – | – |
| No (_n_= 44) | 84.6% | – | – |
The regression results are presented in Table 3. The CCM components explained between 22 and 41 percent of the variance in the practices' use of preventive services to modify patient risk behaviors. Most of the hypotheses regarding the relationships between CCM components and the provision of preventive services received empirical support. Those practices owned by a hospital health system were more likely than other practices to conduct health risk assessments (hypothesis 1). Also, a combination of group-oriented and developmental cultures was consistently and positively associated with all preventive services, including risk assessment, behavioral counseling, and referral to community programs (hypothesis 2).
TABLE 3.
Regression Results for Preventive Services to Address Health Risk Behaviors (_n_= 52)
| CCM Elements | Health Risk Assessment b (SE) | Individual Counseling b (SE) | Group Counseling b (SE) | Referral to Programs b (SE) | Individual Counseling (Diet Only) b (SE) |
|---|---|---|---|---|---|
| Intercept | 0.21 (0.72) | 0.06 (0.54) | −1.08 (0.51)* | 0.58 (0.47) | −0.26 (0.63) |
| Practice size | −0.01 (0.01) | −0.01 (0.01) | −0.01 (0.01)* | 0.002 (0.01) | 0.01 (0.01) |
| Health system organization | |||||
| Hospital health system | 0.60 (0.22)** | 0.05 (0.17) | 0.20 (0.16) | −0.10 (0.14) | 0.02 (0.19) |
| Group/developmental culture | 0.03 (0.01)** | 0.02 (0.01)*** | 0.02 (0.01)** | 0.02 (0.01)** | 0.02 (0.01)** |
| Self-management support | |||||
| Patient reminder cards | −0.92 (0.41)* | −0.61 (0.30)* | 0.09 (0.29) | −0.04 (0.26) | −0.50 (0.35) |
| Delivery system design | |||||
| Multispecialty staff | 0.50 (0.29)* | −0.23 (0.22) | 0.24 (0.21) | −0.13 (0.19) | −0.49 (0.25) |
| Dietician FTEs | N/A | N/A | N/A | N/A | 2.04 (1.02)* |
| Decision support | |||||
| Risk factor chart stickers | 0.07 (0.45) | 1.33 (0.34)*** | 0.28 (0.32) | 0.39 (0.30) | 0.26 (0.10)** |
| Patient chart review | 0.38 (0.56) | 1.03 (0.42)** | 0.35 (0.39) | 0.30 (0.36) | 1.65 (0.48)*** |
| Checklists/flowcharts | 1.01 (0.52)* | −0.24 (0.39) | 0.28 (0.37) | 0.83 (0.34)** | −0.03 (0.46) |
| Clinical staff meetings | −0.57 (0.43) | 0.05 (0.32) | 0.55 (0.31)* | −0.53 (0.28)* | −0.08 (0.37) |
| Clinical information systems | |||||
| Patient registry | 0.53 (0.50) | −0.76 (0.37)* | −0.47 (0.36) | 0.08 (0.33) | −0.86 (0.44)* |
| Electronic medical record | 0.40 (0.31) | 0.44 (0.23)* | −0.22 (0.22) | 0.38 (0.20)* | 0.32 (0.26) |
| F | 2.59 | 4.27 | 2.28 | 3.06 | 3.27 |
| _p_-value | 0.014 | 0.000 | 0.029 | 0.005 | 0.002 |
| Adjusted R2 | 0.26 | 0.41 | 0.22 | 0.31 | 0.35 |
In regard to self-management support, a practice's use of patient reminder cards was not associated with more interventions to reduce risk behaviors (hypothesis 3) and was negatively associated with the performance of health risk assessments and individual counseling. In regard to the delivery system design, multispecialty practices more often assessed health risks (hypothesis 4), and practices that employed staff dieticians provided more individual counseling to patients concerning dietary patterns (hypothesis 5).
We found several positive associations between decision support mechanisms and interventions conducted in the practice setting. Those practices that used risk factor chart stickers and reviewed patients' charts were more likely to offer individual counseling on health risk behaviors (hypotheses 6 and 7). Those practices that used checklists or flowcharts to manage diseases were also more likely to provide health risk assessments and referral to community programs (hypothesis 8). Also, practices that held regular staff meetings to discuss clinical issues were more likely to offer group counseling at the practice and were less likely to refer patients to community programs (hypothesis 9).
There was mixed support for our study hypotheses regarding the relationship between prevention and the use of clinical information systems. Those practices that used patient registries were less likely to offer individual behavioral counseling (hypothesis 10), although practices using electronic medical records were more likely to provide both individual counseling and referral to community programs (hypothesis 11). Finally, the size of the practice was negatively associated with group-counseling activities conducted in the practice setting.
Discussion
Despite strong evidence supporting the use of health risk assessments, behavioral counseling, and referral to community-based programs, we found that they were infrequently offered by a nationwide sample of primary care practices. In addition, this study found incomplete implementation of the CCM, which is consistent with earlier research findings (Rundall et al. 2002; Stroebel et al. 2005; Tsai et al. 2005; Wagner et al. 1999; Wagner, Glasgow, et al. 2001). In particular, office tools and information systems that improved delivery system design, decision support, and access to patient data were either not available or not regularly used. Besides a general lack of resources and time, practices may experience internal resistance to change that sometimes hinders improvement efforts (Cohen et al. 2004; Crabtree 2003). Indeed, previous research suggests that practice cultures that are open to change and that value quality improvement are necessary for implementing the tools and care methods described by the CCM. Participative, flexible, and innovative cultures are especially conducive to quality improvement initiatives (Carman et al. 1996; Shortell et al. 1995).
A practice's culture not only influences the implementation of CCM components, but also is itself a “health system organization” component of the CCM that affects the provision of health services. According to our study, practices whose cultural beliefs and values support quality improvement are more likely to adopt recommended preventive services to reduce risk behaviors. Of all the CCM indicators we examined in this study, a combination of group-oriented and developmental cultures was most consistently and significantly associated with all behavioral interventions. Based on our findings, practices should cultivate openness to change and innovation while maintaining a trustful and participative environment. This blend may facilitate not only successful implementation of the CCM but also improvements in the delivery of recommended clinical care.
Other findings that support the use of the Chronic Care Model as a framework for prevention are the employment of allied health professionals and a multidisciplinary team approach in the delivery system design of primary care practices. Our results also support the integration of office-based reminders and regular meetings to enhance decision support for preventive care. Although the majority of our findings support the use of the CCM as a framework for prevention, two require further comment. A more prevention-focused use of patient reminder cards may encourage patients to seek screening or counseling services that promote health, for example, patient reminder cards for smoking cessation targets or for promoting nutrition and physical activity. Yet how the practices in this study used reminder cards was not clear. Possible uses were reminders of upcoming appointments or other administrative functions. Thus, the validity of these reminder cards as self-management support tools remains questionable, and further study of more appropriate measures specifically for health promotion and disease prevention is needed.
Similarly, while patient registries often are important to managing chronic diseases, they may not help prevent them unless they are used to track particular risk factors or for other preventive purposes. The current use of registries in these study practices and other organizations may reflect a greater interest in the clinical aspects of disease management rather than the prevention of disease and related risk behaviors. In the future, prevention-focused registries could be used to promote health and prevent disease by monitoring indicators such as cancer screenings and behavioral risk factors such as smoking, sedentary behavior, overweight or obesity, and substance abuse. Behavior-based registries may be particularly useful for targeted risk reduction programs and thus are an area for further research and development.
Study findings should be considered in the context of certain limitations. Because all the study sites were members of AHRQ practice-based research networks, the generalizability of these results to other primary care practices is not known. Other limitations are the voluntary nature of data collection, which may have introduced selection bias, and the cross-sectional study design, which limits the ability to make causal inferences. Last, all data, including the level of preventive services offered, were based on self-reports by the primary care staffs, which may have varied in accuracy. Because we were not able to verify these data, there may have been an upward bias in the practices' reports of behavioral interventions. However, reports of both recommended preventive services and the use of evidence-based clinical systems were generally low.
Our study focused on practices and therefore did not collect data on patients' perceptions, attitudes, or behaviors. Hence, we have little insight into the dynamics between the patients and the study practices and how they may differ with respect to chronic disease care and disease prevention in clinical settings. Psychological and economic theories (Kahneman and Tversky 1979) suggest that negative patient reactions to the time and other costs associated with health risk assessments, counseling, or use of community-based prevention programs are more likely when disease prevention rather than the control of existing chronic diseases is the goal. For example, with respect to disease prevention, patients are likely to discount the value of counseling for a risk factor that may not lead to clinical problems for several years, compared with counseling for an existing disease that, without therapy, may become more symptomatic within a matter of weeks. Clearly, the transfer of the CCM's benefits from managing a chronic disease to preventing disease depends heavily on these dynamics, and research is needed to understand them better.
Although data at the community level were unavailable for this study, future research should also explore the impact of community and intersectoral initiatives on health. The importance of the Chronic Care Model's community element has received increasing attention, particularly from those with international and broad-based health promotion goals. A recent collaboration between the World Health Organization and the MacColl Institute for Healthcare Innovation has resulted in an adapted CCM model emphasizing the community and policy components of chronic care (Epping-Jordan et al. 2004). This adapted model inserts community leaders and caregivers into the provider-patient relationship, thereby extending the original CCM dyad to a triad consisting of community partners, health care providers, and patients working together to improve health outcomes.
Similarly, Canadian researchers expanded the CCM framework to address the needs of broad-scale health promotion and disease prevention efforts (Barr et al. 2003). This model highlights the community level as an important component, not only as it relates to the clinical setting, but also as it reveals the social determinants and root causes of health. This expanded model emphasizes greater interaction between the health system and the community, and stresses community-level responsibility and action. The model is based on the recognition that health and health behaviors may be functions of broader social, cultural, political, and economic conditions. Health status is viewed as both a result of individual factors and a collection of societal factors influenced by policies in non–health care sectors such as housing and transportation. These adapted CCM frameworks featuring the role of the community should encourage further study of broad-based disease prevention efforts beyond the clinical setting.
Conclusion
This study has offered an empirical analysis of whether the Chronic Care Model can be expanded beyond chronic disease management to serve also as a framework for primary care practices to address health risk behaviors. Based on this framework, both enhancing care delivery systems and emphasizing the community's influence beyond the clinical setting may be critical to promoting health and preventing disease. In general, we found that the implementation of CCM elements in primary care practices was positively associated with the use of interventions targeting risk behaviors identified as leading causes of morbidity and mortality in the United States. Our findings suggest that primary care practices and their patients may benefit from more widespread implementation of the CCM adapted for prevention that not only better controls existing chronic illnesses, but also reduces patients' risk of developing chronic diseases in the future.
Acknowledgments
This study was supported by the Robert Wood Johnson Foundation under grant no. 47075. The authors would like to thank Dr. Steve Shortell and Dr. Laura Stoker for reviewing initial drafts of this manuscript and for their insights and expertise. We also thank Ms. Michelle Gibel for her help collecting data and the practices from the seventeen practice-based research networks for participating in this study.
References
- Barr VJ, Robinson S, Marin-Link B, Underhill L, Dotts A, Ravensdale D, Salivaras S. The Expanded Chronic Care Model: An Integration of Concepts and Strategies from Population Health Promotion and the Chronic Care Model. Hospital Quarterly. 2003;7(1):73–81. doi: 10.12927/hcq.2003.16763. [DOI] [PubMed] [Google Scholar]
- Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient Self-Management of Chronic Disease in Primary Care. Journal of the American Medical Association. 2002;288(19):2469–75. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- Bodenheimer T, Wagner EH, Grumbach K. Improving Primary Care for Patients with Chronic Illness. Journal of the American Medical Association. 2002a;288(14):1775–79. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]
- Bodenheimer T, Wagner EH, Grumbach K. Improving Primary Care for Patients with Chronic Illness: The Chronic Care Model, Part 2. Journal of the American Medical Association. 2002b;288(15):1909–14. doi: 10.1001/jama.288.15.1909. [DOI] [PubMed] [Google Scholar]
- Bonomi AE, Wagner EH, Glasgow RE, Von Korff M. Assessment of Chronic Illness Care (ACIC): A Practical Tool to Measure Quality Improvement. Health Services Research. 2002;37(3):791–820. doi: 10.1111/1475-6773.00049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calkins E, Boult C, Wagner EH, Pacala J. New Ways to Care for Older People: Building Systems Based on Evidence. New York: Springer; 1999. [Google Scholar]
- Carman JM, Shortell SM, Foster RW, Hughes EF, Boerstler H, O'Brien JL, O'Connor EJ. Keys for Successful Implementation of Total Quality Management in Hospitals. Health Care Management Review. 1996;21(1):48–60. [PubMed] [Google Scholar]
- Casalino L, Gillies RR, Shortell SM, Schmittdiel JA, Bodenheimer T, Robinson JC, Rundall T, Oswald N, Schauffler H, Wang MC. External Incentives, Information Technology, and Organized Processes to Improve Health Care Quality for Patients with Chronic Diseases. Journal of the American Medical Association. 2003;289(4):434–41. doi: 10.1001/jama.289.4.434. [DOI] [PubMed] [Google Scholar]
- Cohen D, McDaniel RRJ, Crabtree BF, Ruhe MC, Weyer SM, Tallia AF, Miller WL, Goodwin MA, Nutting P, Solberg LI, Zyzanski SJ, Jaen CR, Gilchrist V, Stange KC. A Practice Change Model for Quality Improvement in Primary Care Practice. Journal of Healthcare Management. 2004;49(3):155–68. [PubMed] [Google Scholar]
- Crabtree BF. Primary Care Practices Are Full of Surprises! Health Care Management Review. 2003;28(3):279–83. doi: 10.1097/00004010-200307000-00009. [DOI] [PubMed] [Google Scholar]
- Epping-Jordan JE, Pruitt SD, Bengoa R, Wagner EH. Improving the Quality of Health Care for Chronic Conditions. Quality and Safety in Health Care. 2004;13:299–305. doi: 10.1136/qshc.2004.010744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow RE, Nelson CC, Whitesides H, King DK. Use of the Patient Assessment of Chronic Illness Care with Diabetic Patients. Diabetes Care. 2005;28(11):2655–61. doi: 10.2337/diacare.28.11.2655. [DOI] [PubMed] [Google Scholar]
- Glasgow RE, Orleans CT, Wagner EH, Curry SJ, Solberg LI. Does the Chronic Care Model Serve Also as a Template for Improving Prevention? The Milbank Quarterly. 2001;79(4):579–612. doi: 10.1111/1468-0009.00222. iv–v. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green LA, Fryer GE, Yawn BP, Lanier D, Dovey SM. The Ecology of Medical Care Revisited. New England Journal of Medicine. 2001;344(26):2021–25. doi: 10.1056/NEJM200106283442611. [DOI] [PubMed] [Google Scholar]
- Green LA, Graham R, Bagley B, Kilo CM, Spann SJ, Bogdewic SP, Swanson J. Report of the Task Force on Patient Expectations, Core Values, Reintegration, and the New Model of Family Practice. Annals of Family Medicine. 2004;2(S1):S33–50. [Google Scholar]
- Improving Chronic Illness Care. The Chronic Care Model. [accessed August 2, 2006]. Available at, http://www.improvingchroniccare.org/change/index.html.
- Improving Chronic Illness Care. The Chronic Care Model: Model Elements. [accessed April 25, 2006]. Available at, http://www.improvingchroniccare.org/change/model/components.html.
- Kahneman D, Tversky A. Prospect Theory: An Analysis of Decision under Risk. Econometrica. 1979;47(2):263–92. [Google Scholar]
- Koop E. Health Promotion and Disease Prevention in Clinical Practice. In: Lawrence RS, Woolf SH, Jonas S, editors. Health Promotion and Disease Prevention in Clinical Practice. Baltimore: Williams and Wilkins; 1996. pp. vii–ix. [Google Scholar]
- Kottke TE, Solberg LI, Brekke ML, Cabrera A, Marquez MA. Delivery Rates for Preventive Services in 44 Midwestern Clinics. Mayo Clinic Proceedings. 1997;72(6):515–23. doi: 10.4065/72.6.515. [DOI] [PubMed] [Google Scholar]
- Lewis CE. Disease Prevention and Health Promotion Practices of Primary Care Physicians in the United States. American Journal of Preventive Medicine. 1988;4(S4):9–16. [PubMed] [Google Scholar]
- McGinnis JM, Foege WH. Actual Causes of Death in the United States. Journal of the American Medical Association. 1993;270(18):2207–12. [PubMed] [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual Causes of Death in the United States, 2000. Journal of the American Medical Association. 2004;291(10):1238–45. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- Pearson ML, Wu S, Schaefer J, Bonomi AE, Shortell SM, Mendel PJ, Marsteller JA, Louis TA, Rosen M, Keeler EB. Assessing the Implementation of the Chronic Care Model in Quality Improvement Collaboratives. Health Services Research. 2005;40(4):978–96. doi: 10.1111/j.1475-6773.2005.00397.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pronk NP, Peek CJ, Goldstein MG. Addressing Multiple Behavioral Risk Factors in Primary Care: A Synthesis of Current Knowledge and Stakeholder Dialogue Sessions. American Journal of Preventive Medicine. 2004;27:S4–17. doi: 10.1016/j.amepre.2004.04.024. [DOI] [PubMed] [Google Scholar]
- Quinn RE, Kimberly JR. Paradox, Planning, and Perseverance: Guidelines for Managerial Practice. In: Kimberly JR, Quinn RE, editors. Managing Organization Transitions. Homewood, Ill.: Dow Jones-Irwin; 1984. pp. 295–313. [Google Scholar]
- Quinn RE, Rohrbaugh J. A Competing Values Approach to Organizational Effectiveness. Public Productivity Review. 1981;5:122–40. [Google Scholar]
- Rundall TG, Shortell SM, Wang MC, Casalino L, Bodenheimer T, Gillies RR, Schmittdiel JA, Oswald N, Robinson JC. As Good as It Gets? Chronic Care Management in Nine Leading U.S. Physician Organisations. British Medical Journal. 2002;325(7370):958–61. doi: 10.1136/bmj.325.7370.958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shortell SM, Jones RH, Rademaker AW, Gillies RR, Dranove DS, Hughes EF, Budetti PP, Reynolds KS, Huang CF. Assessing the Impact of Total Quality Management and Organizational Culture on Multiple Outcomes of Care for Coronary Artery Bypass Graft Surgery Patients. Medical Care. 2000;38:207–17. doi: 10.1097/00005650-200002000-00010. [DOI] [PubMed] [Google Scholar]
- Shortell SM, O'Brien JL, Carman JM, Foster RW, Hughes EF, Boerstler H, O'Connor EJ. Assessing the Impact of Continuous Quality Improvement/Total Quality Management: Concept versus Implementation. Health Services Research. 1995;30(2):377–401. [PMC free article] [PubMed] [Google Scholar]
- Shortell SM, Zazzali JL, Burns LR, Alexander JA, Gillies RR, Budetti PP, Waters TM, Zuckerman HS. Implementing Evidence-Based Medicine: The Role of Market Pressures, Compensation Incentives, and Culture in Physician Organizations. Medical Care. 2001;39(7):I62–I78. [PubMed] [Google Scholar]
- Solberg LI, Brekke ML, Fazio CJ, Fowles J, Jacobsen DN, Kottke TE, Mosser G, O'Connor PJ, Ohnsorg KA, Rolnick SJ. Lessons from Experienced Guideline Implementers: Attend to Many Factors and Use Multiple Strategies. Joint Commission Journal of Quality Improvement. 2000;26:171–88. doi: 10.1016/s1070-3241(00)26013-6. [DOI] [PubMed] [Google Scholar]
- Solberg LI, Kottke TE, Brekke ML. Will Primary Care Clinics Organize Themselves to Improve the Delivery of Preventive Services? A Randomized Controlled Trial. Preventive Medicine. 1998;27(4):623–31. doi: 10.1006/pmed.1998.0337. [DOI] [PubMed] [Google Scholar]
- Sperl-Hillen JM, Solberg LI, Hroscikoski MC, Crain AL, Engebretson KI, O'Connor PJ. Do All Components of the Chronic Care Model Contribute Equally to Quality Improvement? Joint Commission Journal on Quality and Safety. 2004;30(6):303–9. doi: 10.1016/s1549-3741(04)30034-1. [DOI] [PubMed] [Google Scholar]
- Stroebel RJ, Gloor B, Freytag S, Riegert-Johnson D, Smith SA, Huschka T, Nassens J, Kottke TE. Adapting the Chronic Care Model to Treat Chronic Illness at a Free Medical Clinic. Journal of Health Care for the Poor and Underserved. 2005;16:286–96. doi: 10.1353/hpu.2005.0041. [DOI] [PubMed] [Google Scholar]
- Tsai AC, Morton SC, Mangione CM, Keeler EB. A Meta-Analysis of Interventions to Improve Care for Chronic Illnesses. American Journal of Managed Care. 2005;11(8):478–88. [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Healthy People 2010. 2nd ed. Washington, D.C.: 2000. [Google Scholar]
- U.S. Preventive Services Task Force. Guide to Clinical Preventive Services 2005. Washington, D.C.: U.S. Department of Health and Human Services; 2005. [Google Scholar]
- Wagner EH. Chronic Disease Management: What Will It Take to Improve Care for Chronic Illness? Effective Clinical Practice. 1998;1(1):2–4. [PubMed] [Google Scholar]
- Wagner EH. The Role of Patient Care Teams in Chronic Disease Management. British Medical Journal. 2000;320(7234):569–72. doi: 10.1136/bmj.320.7234.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving Chronic Illness Care: Translating Evidence into Action. Health Affairs. 2001;20(6):64–78. doi: 10.1377/hlthaff.20.6.64. [DOI] [PubMed] [Google Scholar]
- Wagner EH, Austin BT, Von Korff M. Improving Outcomes in Chronic Illness. Managed Care Quarterly. 1996a;4(2):12–25. [PubMed] [Google Scholar]
- Wagner EH, Austin BT, Von Korff M. Organizing Care for Patients with Chronic Illness. The Milbank Quarterly. 1996b;74(4):511–44. [PubMed] [Google Scholar]
- Wagner EH, Bennett SM, Austin BT, Greene SM, Schaefer JK, Von Korff M. Finding Common Ground: Patient-Centeredness and Evidence-Based Chronic Illness Care. Journal of Alternative and Complementary Medicine. 2005;11(S1):S7–15. doi: 10.1089/acm.2005.11.s-7. [DOI] [PubMed] [Google Scholar]
- Wagner EH, Davis C, Schaefer J, Von Korff M, Austin B. A Survey of Leading Chronic Disease Management Programs: Are They Consistent with the Literature? Managed Care Quarterly. 1999;7(3):56–66. [PubMed] [Google Scholar]
- Wagner EH, Glasgow RE, Davis C, Bonomi AE, Provost L, McCulloch D, Carver P, Sixta C. Quality Improvement in Chronic Illness Care: A Collaborative Approach. Joint Commission Journal on Quality and Safety. 2001;27(2):63–80. doi: 10.1016/s1070-3241(01)27007-2. [DOI] [PubMed] [Google Scholar]
- Woolf SH, Atkins D. The Evolving Role of Prevention in Health Care: Contributions of the U.S. Preventive Services Task Force. American Journal of Preventive Medicine. 2001;20(S3):13–20. doi: 10.1016/s0749-3797(01)00262-8. [DOI] [PubMed] [Google Scholar]
- Woolf SH, Grol R, Hutchinson A, Eccles M, Grimshaw J. Clinical Guidelines: Potential Benefits, Limitations, and Harms of Clinical Guidelines. British Medical Journal. 1999;318(7182):527–30. doi: 10.1136/bmj.318.7182.527. [DOI] [PMC free article] [PubMed] [Google Scholar]