Characterization of a New Metallo-β-Lactamase Gene, blaNDM-1, and a Novel Erythromycin Esterase Gene Carried on a Unique Genetic Structure in Klebsiella pneumoniae Sequence Type 14 from India (original) (raw)
Abstract
A Swedish patient of Indian origin traveled to New Delhi, India, and acquired a urinary tract infection caused by a carbapenem-resistant Klebsiella pneumoniae strain that typed to the sequence type 14 complex. The isolate, Klebsiella pneumoniae 05-506, was shown to possess a metallo-β-lactamase (MBL) but was negative for previously known MBL genes. Gene libraries and amplification of class 1 integrons revealed three resistance-conferring regions; the first contained bla_CMY-4 flanked by IS_EcP1 and blc. The second region of 4.8 kb contained a complex class 1 integron with the gene cassettes arr_-2, a new erythromycin esterase gene; ereC; aadA1; and cmlA7. An intact IS_CR1 element was shown to be downstream from the qac/sul genes. The third region consisted of a new MBL gene, designated bla_NDM-1, flanked on one side by K. pneumoniae DNA and a truncated IS_26 element on its other side. The last two regions lie adjacent to one another, and all three regions are found on a 180-kb region that is easily transferable to recipient strains and that confers resistance to all antibiotics except fluoroquinolones and colistin. NDM-1 shares very little identity with other MBLs, with the most similar MBLs being VIM-1/VIM-2, with which it has only 32.4% identity. As well as possessing unique residues near the active site, NDM-1 also has an additional insert between positions 162 and 166 not present in other MBLs. NDM-1 has a molecular mass of 28 kDa, is monomeric, and can hydrolyze all β-lactams except aztreonam. Compared to VIM-2, NDM-1 displays tighter binding to most cephalosporins, in particular, cefuroxime, cefotaxime, and cephalothin (cefalotin), and also to the penicillins. NDM-1 does not bind to the carbapenems as tightly as IMP-1 or VIM-2 and turns over the carbapenems at a rate similar to that of VIM-2. In addition to K. pneumoniae 05-506, _bla_NDM-1 was found on a 140-kb plasmid in an Escherichia coli strain isolated from the patient's feces, inferring the possibility of in vivo conjugation. The broad resistance carried on these plasmids is a further worrying development for India, which already has high levels of antibiotic resistance.
The growing increase in the rates of antibiotic resistance is a major cause for concern in both nonfermenting bacilli and isolates of the Enterobacteriaceae family. β-Lactams have been the mainstay of treatment for serious infections, and the most active of these are the carbapenems, which are advocated for use for the treatment of infections caused by extended-spectrum β-lactamase (ESBL)-producing Enterobacteriaceae, particularly Escherichia coli and Klebsiella pneumonia (21). However, carbapenemases are increasingly being reported; and the most prevalent of these would appear to be KPC, which has recently been characterized in the United States, Israel, Turkey, China, India, the United Kingdom, and Nordic countries (20, 24, 26). KPC has invariably been found in K. pneumoniae, although recent reports indicate that it can cross species boundaries (2). OXA-48 is a class D carbapenemase that is mainly found in K. pneumoniae and that is now reported from Turkey, China, India, and the United Kingdom (3, 5, 9). The mobile class B enzymes or metallo-β-lactamases (MBLs) have been mainly found in Pseudomonas aeruginosa, but they are increasingly being found in Enterobacteriaceae, particularly isolates from Greece and Turkey (39). Those mainly found in K. pneumoniae are the VIM-1/VIM-4 cluster (6).
The majority of resistance genes in Enterobacteriaceae are carried on class 1 integrons, and this is also true for the carbapenemases, such as VIM-1/VIM-4 (24, 40). In such cases, the genes are mobilized and evinced as gene cassettes and can theoretically move as separate entities independent of the integrase gene. Indeed, the majority of the mobile MBL genes are found as gene cassettes. These include _bla_IMP, _bla_VIM, _bla_GIM, _bla_SIM, and bla_KMH (41). The exception to these are genes encoding AIM-1 and SPM-1, which are adjacent to and thought to be mobilized by IS_CR elements via a transposition event called rolling circle recombination (36).
Herein, we report on the genetic and biochemical characterization of a new subgroup of MBL, designated NDM-1, originating from New Delhi, India. We also report on its novel genetic context and describe a new erythromycin resistance gene, designated _ere_C.
MATERIALS AND METHODS
Bacterial strains and susceptibility testing.
The identification of K. pneumoniae 05-506 was performed with automated systems (the Phoenix and BD systems). Etest strips (AB bioMerieux, Solna, Sweden) were used to determine susceptibility, and the susceptibility results were interpreted according to the CLSI guidelines. E. coli J53 and E. coli TOPO (Strategene, Amsterdam, The Netherlands) were used in the conjugation and cloning experiments, respectively.
Phenotypic and molecular detection of MBL.
Hodge and imipenem-EDTA double-disc synergy tests as well as Etest were used to screen for MBL production. In addition, the carbapenemase activities of cell sonicates from overnight broth cultures (Mueller-Hinton broth; BD) were determined by spectrophotometric assays. These were undertaken by using 150 μM imipenem as the substrate and 299 nm for the measurement of hydrolysis. The assays were performed with or without EDTA (25 mM) to examine the inhibition of carbapenemase activity. The strains were screened for the presence of known mobile MBL genes (_bla_VIM, _bla_IMP, _bla_SPM-1, _bla_GIM-1, _bla_SIM-1, _bla_AIM-1) by PCR with the primers reported previously (22). The strains were also screened for the presence of other β-lactamase genes (_bla_CTX, _bla_CMY, etc.) as well as class 1, 2, and 3 integron structures (24). Strains known to harbor MBL genes were used as positive controls for the PCR analysis.
Conjugation.
E. coli J53 was used as the recipient in the conjugation studies, and mating was carried out on blood agar medium without selection (25). After 18 h, the mixed cultures were taken from the plates, suspended in saline, and plated onto MacConkey medium containing sodium azide (100 μg/ml) and ceftazidime (8 μg/ml). Confirmation that conjugation had taken place in E. coli J53 was carried out by indole testing and testing for the presence of the MBL gene by PCR analysis.
DNA cloning.
Cloning experiments were performed by using the cloning vector pK18, as described previously (35). Restriction endonucleases BamHI, EcoRI, and HindIII (Invitrogen, Carlsbad, CA) were used to cut both plasmid and K. pneumoniae 05-506 chromosomal DNA. Transformation was carried out by using electroporation and E. coli TOP10 cells (Invitrogen Ltd, Paisley, United Kingdom). Transformants were selected on LB agar plates containing 5-bromo-4-chloro-3-indolyl-β-d-galactopyranoside (30 μg/ml), ceftazidime (6 μg/ml), and kanamycin (25 μg/ml). Recombinant plasmids were recovered with a QIAprep spin miniprep kit (Qiagen, West Sussex, United Kingdom). Restriction endonuclease analysis of the plasmid was carried out with a variety of restriction enzymes to determine the size of the ligated nucleotide segment.
The PCR-amplified open reading frame of NDM-1 was digested with the appropriate enzymes and was subsequently ligated into the pVFT3S (six-His—trx fusion vector) bacterial expression vector. The construct was transformed into E. coli BL21 groEL/groES (pGro7/BL21; Takara Bio Inc., Japan).
DNA sequencing and computer analysis.
Both strands of the clones from the libraries that were produced were sequenced by using M13 forward and M13 reverse primers. The cloned insets containing _bla_NDM-1, the complex class 1 integron, and _bla_CMY-4 were fully sequenced. The nucleotide sequences, deduced amino acid sequences, and phylogenetic relationships were analyzed by using the Lasergene software package (DNAStar, Madison, WI). The sequences obtained were compared to the sequences available on the Internet (http://www.ebi.ac.uk/fasta33/).
Pulsed-field gel electrophoresis (PFGE) and genomic DNA digestion with endonucleases.
Genomic DNA was prepared in agarose blocks and digested with the restriction enzymes XbaI and SpeI (Roche Diagnostics, Mannheim, Germany), I-_Ceu_I (New England Biolabs, Beverly, MA), and S1 nuclease (Invitrogen, Abingdon, United Kingdom). The DNA fragments were separated by use of a CHEF-DR III apparatus (Bio-Rad, Hercules, CA) for 20 h at 6 V/cm and 14°C with initial and final pulse times of 0.5 and 30 s, respectively.
Southern blot analysis.
Southern blotting was performed on agarose gels by in-gel hybridization with the _bla_NDM-1 probe labeled with 32P (Strategene) and by a recently described random primer method (22).
MLST.
Multilocus sequence typing (MLST) of K. pneumoniae was performed as described by Diancourt et al. (7). Experimentally determined DNA sequences were uploaded into the MLST database (http://www.pasteur.fr/recherche/genopole/PF8/mlst/Kpneumoniae.html), and allelic numbers as well as sequence types (STs) were obtained.
ß-Lactamase purification.
Cell lysates were centrifuged at 12,000 rpm for 30 min at 4°C. The supernatant was obtained and loaded onto Ni-nitrilotriacetic acid agarose. The NDM-1 protein was eluted by the use of elution buffer with 300 mM imidazole. The protein was separated from the His-trx tag by tobacco etch virus protease and was finally purified by gel filtration on a GS320 column.
Kinetic measurements.
Purified ß-lactamase was used to determine the kinetic parameters _k_cat and Km. Reactions were performed at 30°C in 1 ml of assay buffer (10 mM HEPES, pH 7.5). The assays were performed in a UV-1601PC spectrophotometer (Shimadzu Corp., Tokyo, Japan) by observing the changes in absorption resulting from the opening of the ß-lactam ring at the specific wavelengths for each of the each antimicrobial agents evaluated, as described previously (18).
Nucleotide sequence accession number.
The nucleotide sequence data reported in the present study have been assigned EMBL/GenBank nucleotide accession number FN396876.
RESULTS
Clinical details for K. pneumoniae 05-506.
A 59-year-old male patient who was originally from India but who had lived in Sweden for many years and who often returned to India had type 2 diabetes mellitus and had had multiple strokes. In November 2007, he traveled to India and on 5 December was hospitalized in Ludhiana, Punjab, with a large gluteal abscess. In December 2007, he was admitted to a hospital in New Dehli, where he was again operated on and where he developed a decubital ulcer. On 8 January 2008 he was referred to Örebro, Sweden. During his stay in New Dehli he received amoxicillin (amoxicilline)-clavulanic acid, metronidazole, amikacin, and gatifloxacin (all of them parenterally).
Clinical isolate K. pneumoniae 05-506 was derived from a urinary culture on 9 January 2008. He had no clear symptoms of urinary tract infection at that time. The amount of bacteria found in a culture of his urine was only 1,000 CFU/ml. Both ESBL-positive Escherichia coli and a carbapenem-susceptible Acinetobacter sp. were isolated from his deep wounds. An ESBL-positive E. coli strain was also found in a culture of fluid resulting from external otitis.
On 6 March 2008, the patient was discharged to a nursing home. On 1 April a new urine sample for culture was taken, and an ESBL-producing K. pneumoniae isolate was found. The original carbapenem-resistant K. pneumoniae isolate has never been found in any other cultures of samples from the patient. As K. pneumoniae 05-506 was carbapenem resistant and positive by the MBL Etest (AB bioMerieux), it was investigated further. Moreover, fecal samples were collected from the patient during his stay at the nursing home to identify the source of 05-506; however, while 05-506 could not be recovered, an MBL-positive E. coli isolate was recovered and was designated E. coli NF-NDM-1.
Typing and phenotypic characterization of K. pneumoniae 05-560, E. coli NF-NDM-1, and transformants.
ST14 is a single-locus variant of ST15, which has been encountered with KPC- and CTX-M-producing K. pneumoniae strains (19, 30). We have also found ST14 among U.S. KPC producers (19).
The susceptibility patterns of K. pneumoniae 05-560, E. coli NF-NDM-1, E. coli TOP10, E. coli TOP10(pNDM-1), E. coli J53, and E. coli J53(pNDM-1) are listed in Table 1. K. pneumoniae 05-560 was resistant to all β-lactams and was sensitive only to colistin (Table 1). The susceptibility profile of E. coli NF-NDM-1 largely reflects that of 05-560, apart from susceptibility to aztreonam, cefepime, and ciprofloxacin, to which the level of resistance of 05-560 was not quite as high. When the cloned MBL gene and its adjacent DNA were expressed in an E. coli background, the strain was highly resistant to all cephalosporins, apart from cefepime (MIC, 8 μg/ml), and was sensitive to aztreonam. However, the aztreonam MICs differed significantly for TOP10 _bla_NDM-1 (MIC, 0.25 μg/ml) and J53 _bla_NDM-1 (MIC, 24 μg/ml), even though the aztreonam MICs for TOP10 and J53 were very similar. Interestingly, the MICs of imipenem and meropenem were relatively high for both E. coli TOP10 and J53 compared with those for strains with the other cloned MBL genes (31, 41).
TABLE 1.
Antimicrobial susceptibility patterns of K. pneumoniae 05-560, E. coli NF-NDM-1, transformants, and conjugants
| Antibiotic | MIC (μg/ml) | |||||
|---|---|---|---|---|---|---|
| K. pneumoniae 05-560 | E. coli TOP10 | E. coli TOP10(NDM-1) | E. coli J53 | E. coli J53(pNDM-1) | E. coli NF-NDM-1 | |
| Ampicillin | >256 | 12 | >256 | 4 | >256 | >256 |
| Piperacillin | >256 | 0.5 | NT | 1 | >256 | >256 |
| Cephalothin | >256 | 8 | >256 | 4 | >256 | >256 |
| Cefoxitin | >256 | 4 | >256 | 2 | >256 | >256 |
| Cefotaxime | >256 | 0.125 | >256 | 0.064 | >256 | >256 |
| Cefuroxime | >256 | 8 | >256 | 8 | >256 | >256 |
| Ceftazidime | >256 | 1 | >256 | 0.125 | >256 | >256 |
| Aztreonam | >256 | 0.094 | 0.25 | 0.064 | 24 | 24 |
| Cefepime | >256 | 0.032 | 8 | 0.064 | 24 | 24 |
| Ertapenem | >32 | 0.125 | 24 | 0.5 | >32 | >32 |
| Imipenem | >32 | 0.094 | 12 | 0.25 | 16 | >32 |
| Meropenem | >32 | 0.064 | 12 | 0.064 | >32 | >32 |
| Ciprofloxacin | >32 | 0.004 | 0.006 | 0.032 | 0.047 | 4 |
| Colistin | 0.75 | 0.38 | 0.38 | 0.25 | 0.25 | 0.25 |
Phenotypic and molecular screening for MBLs.
The results of the MBL screening tests were positive by the imipenem-EDTA double-disc synergy test, the MBL Etest (256 μg/ml with imipenem and 3 μg/ml with imipenem plus inhibitor), and the determination of carbapenemase activities by spectrophotometry (data not shown). However, PCR analysis failed to detect previously known MBL genes when the control genes _bla_VIM, _bla_IMP, _bla_SPM-1, _bla_GIM-1, _bla_SIM-1, _bla_AIM-1 were used. PCR did detect a class 1 integron (intI and qacE_Δ_1/sul) of 4.8 kb.
Nucleotide and deduced amino acid sequences of three resistance-conferring regions.
Total DNA from K. pneumoniae 05-560 was used to construct a genomic library to isolate all genes conferring β-lactam resistance. After the plasmids of resistant colonies were analyzed by restriction profiling, it was evident that there were two different types of β-lactam resistance. One group carried a putative AmpC enzyme, on the basis of the fact that it was resistant to the effects of EDTA but sensitive to inhibition with cloxacillin. The other group possessed a putative MBL on the basis of the fact that it was resistant to the effects of cloxacillin and clavulanic acid but sensitive to EDTA. Restriction of the recombinant plasmids showed that the AmpC-type genes are carried on a 2.1-kb fragment and that the MBL gene is carried on a 4.3-kb fragment. Additionally, the 4.8-kb fragment containing the class 1 integron was also sequenced.
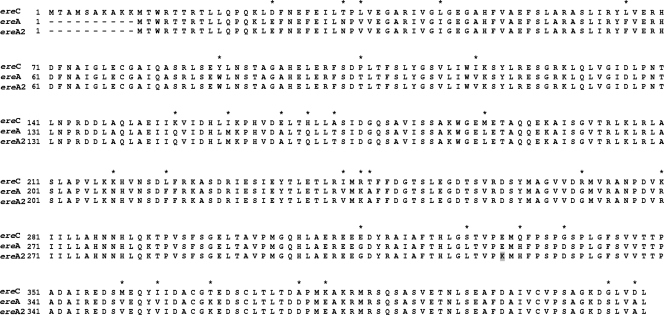
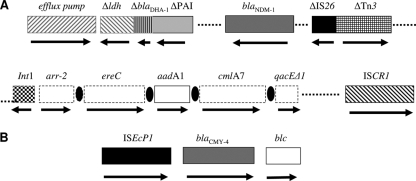
The class 1 integron contains a unique set of genes, some of which have been previously reported from Asia. Immediately next to the intI gene is an _arr_-2 cassette that mediates resistance to rifampin (rifampicin) and that has been found in isolates of Pseudomonas aeruginosa and Acinetobacter baumannii from China and Hong Kong, respectively (GenBank accession numbers EU886979 and AY038837, respectively) (1, 14, 27, 38). It has also been identified on the chromosome of Streptomyces coelicolor (GenBank accession number NC003888). Next to aar-2 is a novel erythromycin esterase gene (ereC) which has 92% nucleotide sequence identity with ereA from E. coli (GenBank accession number AY183453) (Fig. 1). The predicted protein sequence differs from the EreA sequence at an additional 10 amino acids at the N terminus and also has 31 amino acid substitutions throughout the sequence. At present, only two erythromycin esterases, ereA and ereB, have been found (GenBank accession numbers DQ157752 and X03988, respectively), and these share only 25% identity in their amino acid sequences (Fig. 1). Adjacent to the esterase gene is aadA1, which mediates resistance to gentamicin, and the _cml_A7 gene cassette, which mediates resistance to chloramphenicol, is present between aadA1 and qac/sul (Fig. 2).
FIG. 1.
Alignment of novel erythromycin esterase EreC (this study) with EreA and EreA2. Amino acid changes between EreC and EreA are indicated with asterisks. The single amino acid difference between EreA and EreA2 is highlighted in gray.
FIG. 2.
Three characterized antibiotic resistance-conferring regions from K. pneumoniae 05-506. (A) The 4.3-kb region is linked to the 4.8-kb complex class 1 integron region. The genes encoding the efflux pump and lactate dehydrogenase (gray diagonal lines) are of Klebsiella origin. bla_NDM-1 (dark gray) is flanked between the pathogenicity island (vertical black lines) and IS_26/Tn_3_ (black small squares). This region lies downstream of the 4.8-kb complex class 1 integron containing Int (checkered area), arr_-2, ere2A, aadA1, and cmlA7 as gene cassettes and qac_Δ_1 (white boxes). Downstream is an intact copy of IS_CR1 (black and white diagonal lines). Arrows, direction of transcription; black ellipses, 59-base elements; Δ, genes that are truncated. (B) bla_CMY-4 (gray) is located between IS_EcP1 (black) and blc (white), as reported previously (16).
The AmpC fragment is shown in Fig. 2 and carries _bla_CMY-4, which is responsible for the AmpC phenotype. Upstream of bla_CMY-4 is an intact copy of IS_EcP1, which is probably responsible for the transposition and mobility of _bla_CMY-4. Downstream is blc, which is a common feature in many _bla_CMY regions and which has been reported by Kang et al. (16).
The 4.3-kb fragment contained a novel MBL gene, designated bla_NDM-1 (Fig. 2). This section of DNA was a chimera of truncated and intact genes. The bla_NDM-1 gene was found between a section of K. pneumoniae chromosomal DNA and truncated sections of the IS_26 and Tn_3 transposase genes. The Klebsiella DNA consisted of a putative efflux protein gene adjacent to another gene encoding l-lactate hydrogenase, and both were 99.5% identical to a section of chromosomal DNA from K. pneumoniae MGH78578 (GenBank accession number CP000647) and found in the same orientation in which they are present on the Klebsiella chromosome. The lactate dehydrogenase gene was truncated and missing approximately 750 bp of the 5′ end of the gene. Immediately upstream of the lactate dehydrogenase gene was a short internal part of the ampC gene, _bla_DHA-1 (base pair coordinates 1268 to 1478), consisting of the DNA encoding amino acids 196 to 265. This gene was truncated at both ends both by the lactate dehydrogenase gene and by a section of DNA encoding the 5′ end of a phosphoribosyl anthalinate isomerase gene. This section of DNA (coordinates 1478 to 2100) has identities ranging from 55% to 68% to the same gene from various members of the alphaproteobacteria, including Rhodobacter spp., Rhodopseudomonas spp., Caulobacter spp., and Novosphingobium spp. The highest degree of identity was found with Novosphingobium aromaticivor, with 68% nucleotide sequence identity over 575 nucleotides. Again, this gene was truncated and missing the DNA encoding the last 19 amino acids of the C terminus of the protein. The _bla_NDM-1 gene is encoded within a 1,350-bp section of DNA with a lower G+C content (57%) than that of the surrounding DNA, which has a G+C content of 62 to 65% and which consists of a gene of 807 nucleotides and flanking DNA on either side. Upstream of the _bla_NDM-1 gene is 250 nucleotides of DNA that contains several sequences that show similarity to conventional promoter sequences, and it is likely that the promoter driving the expression of bla_NDM-1 has been acquired along with the gene (Fig. 2). Farther upstream is a truncated left-hand end of an IS_26 insertion sequence, including 270 bp of the left-hand end of the element with the left-hand inverted repeat and DNA encoding the first 74 amino acids of the transposase. This element lies adjacent to a tnpA gene of a Tn_3_-like transposon (coordinates 3748 to 4318), which is itself truncated and missing the 5′ end of the gene encoding the first 128 amino acids of the transposase (Fig. 2).
Structural properties of NDM-1.
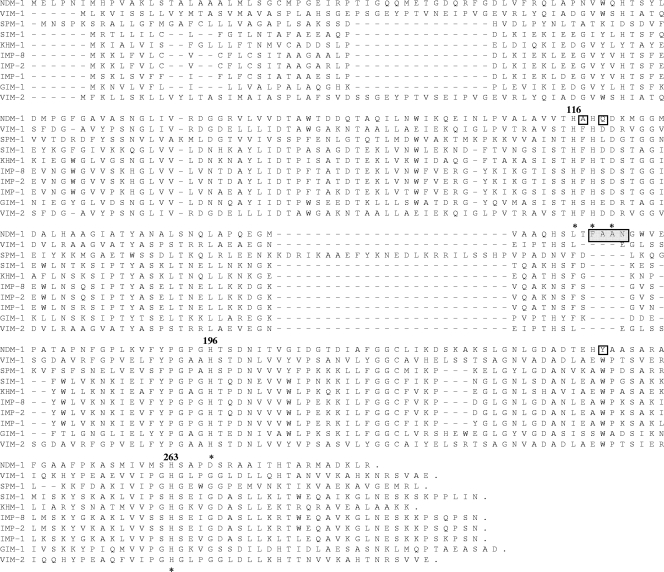
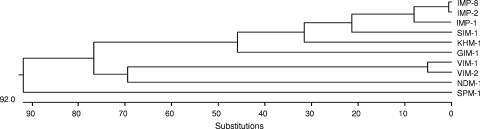
The _bla_NDM-1 open reading frame encodes a putative protein of 269 amino acids with a molecular mass of approximately 27.5 kDa (Fig. 3). The NDM-1 sequence and the behavior of NDM-1 during gel filtration and mass spectrometry (data not shown) indicate that it is actively present as a monomer. Sodium dodecyl sulfate-polyacrylamide gel electrophoresis analysis showed an approximate molecular mass of 28 kDa (data not shown). NDM-1 possesses a leader peptide, with the probable cleavage site occurring at position 19 between two alanines which are in a very similar position to the cleavage site for the VIM MBLs (Fig. 3). NDM-1 also shares the additional loop of the VIM enzymes at positions 34 and 47 but also possesses a unique additional sequence at positions 162 to 166 (_bla_NDM-1 and not BBL numbering) (Fig. 3) (4). NDM-1 shares very little identity with other MBLs and is the most closely related to VIM-1/VIM-2, with which it has only 32.4% identity (Fig. 4). Curiously, NDM-1 also has a unique HXHXD motif among the mobile MBLs, as it contains an alanine between the two histidines. NDM-1 also possesses a tyrosine at position 222 instead of the universally conserved tryptophan (Fig. 3). The mature peptide has a theoretical pI of 6.9.
FIG. 3.
Alignment of the amino acid sequences of NDM-1 with the amino acid sequences of IMP-1, IMP-2, IMP-8, VIM-1, VIM-2, GIM-1, SPM-1, SIM-1, and KHM-1. Conserved residues coordinating zinc ions are denoted with asterisks. Key amino acids are also numbered according to the BBL scheme (12). Additional amino acids unique to NDM-1 are enclosed in a light gray box. Amino acid substitutions near the active site are highlighted in plain boxes (13).
FIG. 4.
Phylogenetic tree obtained for MBL subgroup B1. The numbers for the substitutions should be multiplied by 100. The alignment used was prepared with the CLUSTALW program. The GenBank accession numbers for the sequences are as follows: IMP-1, S71932; IMP-2, AJ243491; IMP-8, AF322577; VIM-1, Y18050; VIM-2, AF191564; GIM-1, AJ620678; SPM-1, AJ492820; SIM-1, AY887066; KHM-1, AB364006.
Functional properties of NDM-1.
Analysis of the purified NDM-1 enzyme by sodium dodecyl sulfate-polyacrylamide gel electrophoresis analysis showed a single band corresponding to a size of 28 kDa (data not shown). Table 2 lists the _k_cat and Km values and compares them with the kinetic values of IMP-1 and VIM-2. NDM-1 shows tight binding (low Km values) to most cephalosporins and, in particular, to cefuroxime, cefotaxime, and cephalothin (cefalotin). It also shows relatively tight binding to the penicillins, which is unusual for an MBL, as both IMP-1 and VIM-2 possess higher Km values (Table 2). Interestingly, NDM-1 does not bind to the carbapenems as tightly as IMP-1 or VIM-2. The rate of turnover (_k_cat) of penicillins by NDM-1 is lower than that by IMP-1 and VIM-2 and is generally unusual for MBLs. The _k_cat values for the cephalosporins are more similar to those of IMP-1 than to those of VIM-2, yet the _k_cat values for the carbapenems (20 and 12 s−1 for imipenem and meropenem, respectively) are more similar to those for VIM-2 (10 and 1 s−1, respectively) than IMP-1 (46 and 50 s−1, respectively) (Table 2). Due to the fact that most of the Km values are low, the _k_cat/Km ratios are reasonably high and comparable to those of VIM-2. The exception is that of ceftazidime, which has a Km of 181 μM and a _k_cat of 5 s−1 and which thus presents with a _k_cat/Km of 0.03.
TABLE 2.
Steady-state kinetic constants of NDM-1, IMP-1, and VIM-2
| Compound | NDM-1 | IMP-1a | VIM-2b | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Km (μM) | _k_cat (s−1) | _k_cat/Km (s−1/μM) | Km (μM) | _k_cat (s−1) | _k_cat/Km (s−1/μM) | Km (μM) | _k_cat (s−1) | _k_cat/Km (s−1/μM) | |
| Penicillin G | 16 | 11 | 0.68 | 520 | 320 | 0.62 | 49 | 56 | 1.14 |
| Ampicillin | 22 | 15 | 0.66 | 200 | 950 | 4.8 | DNA | ||
| Piperacillin | 12 | 14 | 1.17 | NDc | ND | ND | 72 | 33 | 0.45 |
| Cephalothin | 10 | 4 | 0.40 | 21 | 48 | 2.4 | 44 | 57 | 1.28 |
| Cefoxitin | 49 | 1 | 0.02 | 8 | 16 | 2 | 24 | 3 | 0.12 |
| Cefotaxime | 10 | 6 | 0.58 | 4 | 1.3 | 0.35 | 32 | 28 | 0.86 |
| Cefuroxime | 8 | 5 | 0.61 | 37 | 8 | 0.22 | 22 | 12 | 0.55 |
| Ceftazidime | 181 | 5 | 0.03 | 44 | 8 | 0.18 | 98 | 89 | 0.90 |
| Aztreonam | ND | >1,000 | >0.01 | <0.0001 | ND | <0.5 | ND | ||
| Cefepime | 77 | 13 | 0.17 | 11 | 7 | 0.66 | 184 | 5 | 0.03 |
| Imipenem | 94 | 20 | 0.21 | 39 | 46 | 1.2 | 10 | 10 | 0.99 |
| Meropenem | 49 | 12 | 0.25 | 10 | 50 | 0.12 | 5 | 1 | 0.28 |
| Clavulanic acid | ND | NRd | NR |
Plasmid analysis and back probing with _bla_NDM-1.
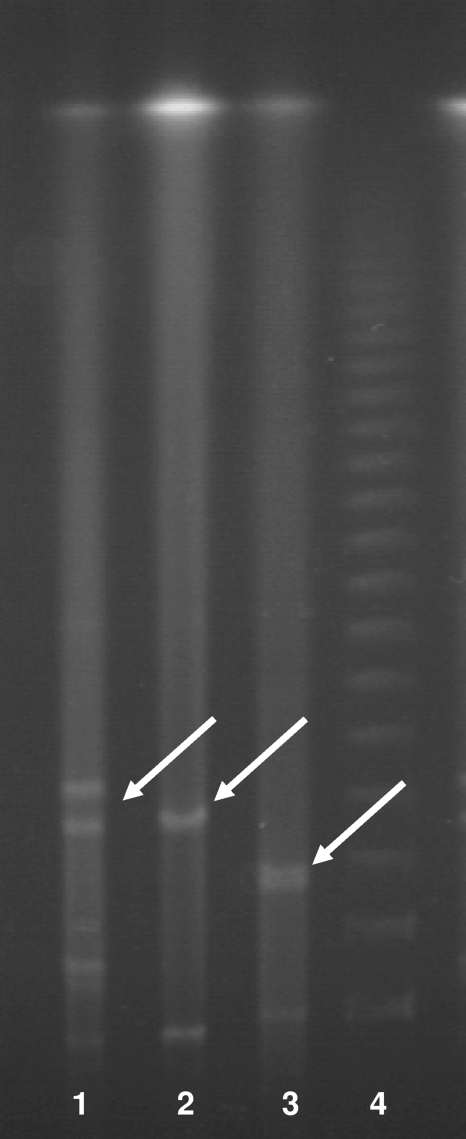
The plasmids carrying bla_NDM-1 from both K. pneumoniae 05-506 and E. coli NF-NDM-1 were successfully transferred to E. coli J53 at a frequency of approximately 10−4 to 10−5. PCR was undertaken with primers directed to IS_CR1 and _bla_NDM-1, and both were shown to be carried by pNDM-1. To examine the sizes of the plasmids from 05-506, E. coli J53(pNDM-1), and E. coli NF-NDM-1, genomic DNA was isolated from each of the strains, restricted with S1 nuclease, and examined by PFGE. The corresponding gel was blotted with _bla_NDM-1, and the data clearly show that _bla_NDM-1 is on a 180-kb plasmid in 05-506 and E. coli J53(pNDM-1), but in E. coli NF-NDM-1 it is on a smaller plasmid of 140 kb (Fig. 5). Inc typing was unsuccessful, and plasmid pNDM-1 is currently being sequenced to identify the origin of replication and other functions carried by pNDM-1.
FIG. 5.
PFGE of plasmids from K. pneumoniae 05-506, conjugant E. coli J53(pNDM-1), and E. coli NF-NDM-1 (from the patient's normal flora). The bands with white arrows showed positive signals by Southern blot hybridization with the NDM-1 probe (data nor shown). K. pneumoniae 05-506 carries _bla_NDM-1 on a 180-kb plasmid, whereas E. coli NF-NDM-1 carries _bla_NDM-1 on a plasmid of approximately 140 kb.
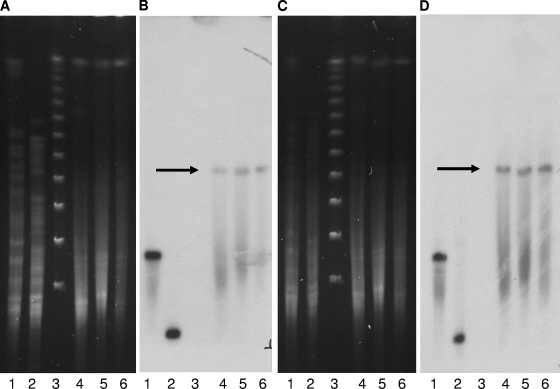
As the broader genetic context was not known and IS_CR1_ had been found in a large antibiotic resistance-conferring region, K. pneumoniae 05-506 was also digested with XbaI, SpeI, I-Ceu_I, and S1 nuclease and was then probed with radiolabeled bla_NDM-1. The probing results were compared to those of probing of IS_CR1 to ascertain whether bla_NDM-1 and IS_CR1 are on the same genetic structure (Fig. 6). The probing data for IS_CR1 and _bla_NDM-1 are identical and clearly indicated probing to the same 25-kb region, suggesting that the regions are adjacent to one another.
FIG. 6.
PFGE findings (A and C) and Southern blot hybridization (B and D) with bla_NDM-1 (A and B) and an IS_CR1 probe (C and D). The genomic DNA of the index strain (K. pneumoniae 05-506) was undigested (lane 1) or was digested with S1 nuclease (lane 2), XbaI (lane 4), SpeI (lane 5), or I_-Ceu_I (lane 6). Lane 3, DNA size marker.
DISCUSSION
K. pneumoniae 05-506 types as ST14, a single-locus variant of type ST15. Recently, K. pneumoniae ST15 has been branded as a new methicillin-resistant S. aureus type of pathogen due to its wide distribution and its carriage of _bla_CTX-M15 and other resistance markers (19, 30). Strain 05-506 clearly arose in India, but there are few data arising from India to suggest how widespread it is. We are currently undertaking studies in several Indian cities to examine these points. Interestingly, there appears to be the possible transfer of _bla_NDM-1 in vivo either from K. pneumoniae to E. coli or vice versa, but more interestingly, the plasmids carrying _bla_NDM-1 in the two species are of different sizes. This evidence would suggest that there is rearrangement in vivo which could result from either duplication and insertion, e.g., transposition or rolling circle replication from the smaller plasmid, or deletion from the larger plasmid (33, 34). The plasmid carrying _bla_NDM-1 also carries _bla_CMY-4 and the complex class 1 integron carrying several antibiotic resistance-conferring genes (33), and it has also shown itself to naturally have a broad host range. When the plasmid was transferred to E. coli J53, the E. coli strain containing pNDM-1 was resistant to all antibiotics except colistin and ciprofloxacin and was shown by blotting and PCR to carry bla_CMY-4, the IS_CR region, and _bla_NDM-1. Therefore, the rapid dissemination of this plasmid among clinical bacteria would be a nightmare scenario.
This is the first report of an MBL gene not carried in a class 1 integron or adjacent to IS_CR1_ elements. It appears to have an intact promoter sequence that is not dependent on the IS_26_ element inserted upstream, even though IS_26_ is found adjacent to other resistance genes and pathogenicity islands (8, 10, 11, 15). The plasmid clearly contains Klebsiella housekeeping genes (Fig. 2) as part of this capturing DNA machinery, and therefore, these have probably been purloined from the Klebsiella chromosome. Furthermore, restriction digests and probing experiments indicate that bla_NDM-1 and IS_CR1 are on a DNA fragment of less than 25 kb (Fig. 6). While Tn_3_ and IS_26_ are capable of movement, the amelioration of such a large region spanning from bla_NDM-1 to IS_CR1 could have occurred only through a series of duplications and homologous recombination (34). The known location of IS_CR1_ in all sequences analyzed so far is at the end of a complex class 1 integron that is more often than not contained within a Tn_3_-like transposon, and therefore, it is possible that the IS_CR1_ element is upstream of the bla_NDM-1 gene and farther downstream of the Tn_3 transposase. Additionally, the chimeric structure of the 4.3-kb insert with its composition of fused truncated and nontruncated genes is a classic signature of IS_CR1_ transposition activity (22, 34, 37).
NDM-1 not only is a new subclass of the B1 group of MBLs but also possesses novel amino acids near the active site, suggesting that it has a novel structure. NDM-1 possesses only 32.4% identity with VIM-2, and therefore, molecular replacement or threading cannot be undertaken to reasonably ascertain its structure. However, NDM-1 does show some similarities to the VIM group of MBLs; namely, it possesses the additional sequences at positions 226 to 228 (BBL numbering) not present in other MBLs (12). These residues contain R228 in VIM-2, which is thought to stabilize C221 and possibly H263, yet in NDM-1 the substitute R228A is unlikely to play such a role. VIM-2 also possesses Y224, which is in close proximity to C221, whereas NDM-1 has a lysine, which is likely to serve a similar role. Crystallographic insights into the mechanism of action of VIM-2 by Garcia-Saez et al. suggest that Y67 pivots in toward the enzyme away from bulk solvent and in so doing stabilizes H263; but NDM-1, like other non-VIM MBLs, possesses the substitution Y67V, which is unlikely to function in the same manner (13). However, NDM-1 does possess S69, which is in close proximity to Y67 and less so to R121 and H263 (13). The role of these substitutions is not apparent, as NDM-1 possesses kinetics similar to those of VIM-2 (23, 29). In general, NDM-1 binds more tightly (it has a lower Km) to most β-lactam substrates and hydrolyzes them less well (it has a lower _k_cat), with the exception being the less bulky carbapenems, for which NDM-1 possesses relatively high Km and _k_cat values for both imipenem and meropenem (23, 29).
In addition to _bla_NDM-1, this study also characterized a new erythromycin esterase gene, designated ereC (28). The esterase gene is part of the complex class 1 integron containing the Asian rifampin resistance gene, _arr_-2, which is also contained as a gene cassette (17). If this structure is stable, together with _bla_NDM-1, it will act as a unique genetic marker for the prevalence and stability of plasmid pNDM-1 throughout Indian Enterobacteriaceae strains. We are currently doing molecular epidemiological studies of Indian Enterobacteriaceae carbapenem-resistant strains to examine the prevalence and range of pNDM-1 among clinical and nonclinical isolates. In a country where there is little control on antibiotic prescriptions, the rapid dissemination of such a plasmid is alarming.
Acknowledgments
This work was funded by EU grant LSHM-CT-2005-018705 and Wellcome Trust grant 084627/Z/08.
D. Yong thanks Seok H. Jeong and Yunsop Chong for their valuable advice.
Footnotes
▿
Published ahead of print on 21 September 2009.
REFERENCES
- 1.Arlet, G., D. Nadjar, J. L. Herrmann, J. L. Donay, P. H. Lagrange, and A. Philippon. 2001. Plasmid-mediated rifampin resistance encoded by an _arr-2_-like gene cassette in Klebsiella pneumoniae producing an ACC-1 class C β-lactamase. Antimicrob. Agents Chemother. 45**:**2971-2972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bennett, J. W., M. L. Herrera, J. S. Lewis II, B. W. Wickes, and J. H. Jorgensen. 2009. KPC-2-producing Enterobacter cloacae and Pseudomonas putida coinfection in a liver transplant recipient. Antimicrob. Agents Chemother. 53**:**292-294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carrer, A., L. Poirel, H. Eraksoy, A. A. Cagatay, S. Badur, and P. Nordmann. 2008. Spread of OXA-48-positive carbapenem-resistant Klebsiella pneumoniae isolates in Istanbul, Turkey. Antimicrob. Agents Chemother. 52**:**2950-2954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crowder, M. W., J. Spencer, and A. J. Vila. 2006. Metallo-β-lactamases: novel weaponry for antibiotic resistance in bacteria. Acc. Chem. Res. 39**:**721-728. [DOI] [PubMed] [Google Scholar]
- 5.Cuzon, G., T. Naas, P. Bogaerts, Y. Glupczynski, T. D. Huang, and P. Nordmann. 2008. Plasmid-encoded carbapenem-hydrolyzing β-lactamase OXA-48 in an imipenem-susceptible Klebsiella pneumoniae strain from Belgium. Antimicrob. Agents Chemother. 52**:**3463-3464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Daikos, G. L., A. Karabinis, E. Paramythiotou, V. P. Syriopoulou, C. Kosmidis, A. Avlami, P. Gargalianos, K. Tzanetou, D. Petropoulou, and H. Malamou-Lada. 2007. VIM-1-producing Klebsiella pneumoniae bloodstream infections: analysis of 28 cases. Int. J. Antimicrob. Agents 29**:**471-473. [DOI] [PubMed] [Google Scholar]
- 7.Diancourt, L., V. Passet, J. Verhoef, P. A. Grimont, and S. Brisse. 2005. Multilocus sequence typing of Klebsiella pneumoniae nosocomial isolates. J. Clin. Microbiol. 43**:**4178-4182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Diestra, K., C. Juan, T. Curiao, B. Moya, E. Miro, J. Oteo, T. M. Coque, M. Perez-Vazquez, J. Campos, R. Canton, A. Oliver, and F. Navarro. 2009. Characterization of plasmids encoding blaESBL and surrounding genes in Spanish clinical isolates of Escherichia coli and Klebsiella pneumoniae. J. Antimicrob. Chemother. 63**:**60-66. [DOI] [PubMed] [Google Scholar]
- 9.Docquier, J. D., V. Calderone, F. De Luca, M. Benvenuti, F. Giuliani, L. Bellucci, A. Tafi, P. Nordmann, M. Botta, G. M. Rossolini, and S. Mangani. 2009. Crystal structure of the OXA-48 β-lactamase reveals mechanistic diversity among class D carbapenemases. Chem. Biol. 16**:**540-547. [DOI] [PubMed] [Google Scholar]
- 10.Doublet, B., S. A. Granier, F. Robin, R. Bonnet, L. Fabre, A. Brisabois, A. Cloeckaert, and F. X. Weill. 2009. Novel plasmid-encoded ceftazidime-hydrolyzing CTX-M-53 extended-spectrum β-lactamase from Salmonella enterica serotypes Westhampton and Senftenberg. Antimicrob. Agents Chemother. 53**:**1944-1951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Doublet, B., K. Praud, F. X. Weill, and A. Cloeckaert. 2009. Association of IS_26_-composite transposons and complex In4-type integrons generates novel multidrug resistance loci in Salmonella genomic island 1. J. Antimicrob. Chemother. 63**:**282-289. [DOI] [PubMed] [Google Scholar]
- 12.Galleni, M., J. Lamotte-Brasseur, G. M. Rossolini, J. Spencer, O. Dideberg, and J. M. Frere. 2001. Standard numbering scheme for class B β-lactamases. Antimicrob. Agents Chemother. 45**:**660-663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Garcia-Saez, I., J. D. Docquier, G. M. Rossolini, and O. Dideberg. 2008. The three-dimensional structure of VIM-2, a Zn-beta-lactamase from Pseudomonas aeruginosa in its reduced and oxidised form. J. Mol. Biol. 375**:**604-611. [DOI] [PubMed] [Google Scholar]
- 14.Girlich, D., L. Poirel, A. Leelaporn, A. Karim, C. Tribuddharat, M. Fennewald, and P. Nordmann. 2001. Molecular epidemiology of the integron-located VEB-1 extended-spectrum β-lactamase in nosocomial enterobacterial isolates in Bangkok, Thailand. J. Clin. Microbiol. 39**:**175-182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hammond, D. S., T. Harris, J. Bell, J. Turnidge, and P. M. Giffard. 2008. Selection of SHV extended-spectrum-β-lactamase-dependent cefotaxime and ceftazidime resistance in Klebsiella pneumoniae requires a plasmid-borne _bla_SHV gene. Antimicrob. Agents Chemother. 52**:**441-445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kang, M. S., T. E. Besser, and D. R. Call. 2006. Variability in the region downstream of the _bla_CMY-2 β-lactamase gene in Escherichia coli and Salmonella enterica plasmids. Antimicrob. Agents Chemother. 50**:**1590-1593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Krauland, M. G., J. W. Marsh, D. L. Paterson, and L. H. Harrison. 2009. Integron-mediated multidrug resistance in a global collection of nontyphoidal Salmonella enterica isolates. Emerg. Infect. Dis. 15**:**388-396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Murphy, T. A., A. M. Simm, M. A. Toleman, R. N. Jones, and T. R. Walsh. 2003. Biochemical characterization of the acquired metallo-β-lactamase SPM-1 from Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 47**:**582-587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nadkarni, A. S., T. Schliep, L. Khan, and C. B. Zeana. 2009. Cluster of bloodstream infections caused by KPC-2 carbapenemase-producing Klebsiella pneumoniae in Manhattan. Am. J. Infect. Control 37**:**121-126. [DOI] [PubMed] [Google Scholar]
- 20.Nordmann, P., G. Cuzon, and T. Naas. 2009. The real threat of Klebsiella pneumoniae carbapenemase-producing bacteria. Lancet Infect. Dis. 9**:**228-236. [DOI] [PubMed] [Google Scholar]
- 21.Paterson, D. L. 2006. Resistance in gram-negative bacteria: Enterobacteriaceae. Am. J. Infect. Control 34**:**S20-S28. [DOI] [PubMed] [Google Scholar]
- 22.Patzer, J. A., T. R. Walsh, J. Weeks, D. Dzierzanowska, and M. A. Toleman. 2009. Emergence and persistence of integron structures harbouring VIM genes in the Children's Memorial Health Institute, Warsaw, Poland, 1998-2006. J. Antimicrob. Chemother. 63**:**269-273. [DOI] [PubMed] [Google Scholar]
- 23.Poirel, L., T. Naas, D. Nicolas, L. Collet, S. Bellais, J. D. Cavallo, and P. Nordmann. 2000. Characterization of VIM-2, a carbapenem-hydrolyzing metallo-β-lactamase and its plasmid- and integron-borne gene from a Pseudomonas aeruginosa clinical isolate in France. Antimicrob. Agents Chemother. 44**:**891-897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Poirel, L., J. D. Pitout, and P. Nordmann. 2007. Carbapenemases: molecular diversity and clinical consequences. Future Microbiol. 2**:**501-512. [DOI] [PubMed] [Google Scholar]
- 25.Poirel, L., Y. Yakupogullari, A. Kizirgil, M. Dogukan, and P. Nordmann. 2009. VIM-5 metallo-β-lactamase-producing Pseudomonas putida from Turkey. Int. J. Antimicrob. Agents 33**:**287. [DOI] [PubMed] [Google Scholar]
- 26.Queenan, A. M., and K. Bush. 2007. Carbapenemases: the versatile β-lactamases. Clin. Microbiol. Rev. 20**:**440-458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Roberts, M. C. 2004. Resistance to macrolide, lincosamide, streptogramin, ketolide, and oxazolidinone antibiotics. Mol. Biotechnol. 28**:**47-62. [DOI] [PubMed] [Google Scholar]
- 28.Roberts, M. C. 2008. Update on macrolide-lincosamide-streptogramin, ketolide, and oxazolidinone resistance genes. FEMS Microbiol. Lett. 282**:**147-159. [DOI] [PubMed] [Google Scholar]
- 29.Samuelsen, O., M. Castanheira, T. R. Walsh, and J. Spencer. 2008. Kinetic characterization of VIM-7, a divergent member of the VIM metallo-β-lactamase family. Antimicrob. Agents Chemother. 52**:**2905-2908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Samuelsen, O., U. Naseer, S. Tofteland, D. H. Skutlaberg, A. Onken, R. Hjetland, A. Sundsfjord, and C. G. Giske. 2009. Emergence of clonally related Klebsiella pneumoniae isolates of sequence type 258 producing plasmid-mediated KPC carbapenemase in Norway and Sweden. J. Antimicrob. Chemother. 63**:**654-658. [DOI] [PubMed] [Google Scholar]
- 31.Sekiguchi, J., K. Morita, T. Kitao, N. Watanabe, M. Okazaki, T. Miyoshi-Akiyama, M. Kanamori, and T. Kirikae. 2008. KHM-1, a novel plasmid-mediated metallo-β-lactamase from a Citrobacter freundii clinical isolate. Antimicrob. Agents Chemother. 52**:**4194-4197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Spencer, J., A. R. Clarke, and T. R. Walsh. 2001. Novel mechanism of hydrolysis of therapeutic beta-lactams by Stenotrophomonas maltophilia L1 metallo-β-lactamase. J. Biol. Chem. 276**:**33638-33644. [DOI] [PubMed] [Google Scholar]
- 33.Toleman, M. A., P. M. Bennett, and T. R. Walsh. 2006. Common regions e.g. orf513 and antibiotic resistance: IS_91_-like elements evolving complex class 1 integrons. J. Antimicrob. Chemother. 58**:**1-6. [DOI] [PubMed] [Google Scholar]
- 34.Toleman, M. A., P. M. Bennett, and T. R. Walsh. 2006. IS_CR_ elements: novel gene-capturing systems of the 21st century? Microbiol. Mol. Biol. Rev. 70**:**296-316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Toleman, M. A., K. Rolston, R. N. Jones, and T. R. Walsh. 2004. _bla_VIM-7, an evolutionarily distinct metallo-β-lactamase gene in a Pseudomonas aeruginosa isolate from the United States. Antimicrob. Agents Chemother. 48**:**329-332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Toleman, M. A., A. M. Simm, T. A. Murphy, A. C. Gales, D. J. Biedenbach, R. N. Jones, and T. R. Walsh. 2002. Molecular characterization of SPM-1, a novel metallo-β-lactamase isolated in Latin America: report from the SENTRY antimicrobial surveillance programme. J. Antimicrob. Chemother. 50**:**673-679. [DOI] [PubMed] [Google Scholar]
- 37.Toleman, M. A., and T. R. Walsh. 2008. Evolution of the IS_CR3_ group of IS_CR_ elements. Antimicrob. Agents Chemother. 52**:**3789-3791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tribuddharat, C., and M. Fennewald. 1999. Integron-mediated rifampin resistance in Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 43**:**960-962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vatopoulos, A. 2008. High rates of metallo-β-lactamase-producing Klebsiella pneumoniae in Greece—a review of the current evidence. Euro. Surveill. 13**:**. [PubMed]
- 40.Walsh, T. R. 2008. Clinically significant carbapenemases: an update. Curr. Opin. Infect. Dis. 21**:**367-371. [DOI] [PubMed] [Google Scholar]
- 41.Walsh, T. R., M. A. Toleman, L. Poirel, and P. Nordmann. 2005. Metallo-β-lactamases: the quiet before the storm? Clin. Microbiol. Rev. 18**:**306-325. [DOI] [PMC free article] [PubMed] [Google Scholar]