Injection therapy and denervation procedures for chronic low-back pain: a systematic review (original) (raw)
Abstract
Injection therapy and denervation procedures are commonly used in the management of chronic low-back pain (LBP) despite uncertainty regarding their effectiveness and safety. To provide an evaluation of the current evidence associated with the use of these procedures, a systematic review was performed. Existing systematic reviews were screened, and the Cochrane Back Review Group trial register was searched for randomized controlled trials (RCTs) fulfilling the inclusion criteria. Studies were included if they recruited adults with chronic LBP, evaluated the use of injection therapy or denervation procedures and measured at least one clinically relevant outcome (such as pain or functional status). Two review authors independently assessed studies for eligibility and risk of bias (RoB). A meta-analysis was performed with clinically homogeneous studies, and the GRADE approach was used to determine the quality of evidence. In total, 27 RCTs were included, 14 on injection therapy and 13 on denervation procedures. 18 (66%) of the studies were determined to have a low RoB. Because of clinical heterogeneity, only two comparisons could be pooled. Overall, there is only low to very low quality evidence to support the use of injection therapy and denervation procedures over placebo or other treatments for patients with chronic LBP. However, it cannot be ruled out that in carefully selected patients, some injection therapy or denervation procedures may be of benefit.
Keywords: Injection, Back pain, Denervation, Review
Introduction
Chronic low-back pain (LBP) is related to disability and work absence and accounts for high social and health care costs in western societies [1]. The management of chronic LBP comprises a range of different intervention strategies including surgery, pharmacological interventions and non-medical interventions such as exercise, behavioural therapy and alternative therapies. Non-surgical interventions, such as injection therapy and denervation procedures, have rapidly increasing rates of utilization and associated costs [2]. Injection therapy for chronic LBP involves injections of medications, irritants, or proteolytic enzymes into soft tissues outside or within the spine. Denervation procedures involve the application of various types of thermal or radiofrequency energy within the spine.
Over the past years, a substantial number of randomized clinical trials have been published on injection therapy and denervation procedures. In order to appropriately evaluate the effects of these interventions in a systematic review, it is important to make valid comparisons that are homogeneous with regard to study population, indications, interventions and different anatomical structures being targeted, controls, outcome measures and follow-up. Based on the available literature, this overview presents the current evidence on injections into and outside the spine and radiofrequency or thermal denervation procedures for non-specific chronic LBP.
Objectives
The objective of this review was to determine the effectiveness of injection therapy (including injections into soft tissues outside or within the spine and chemonucleolysis), and radiofrequency or thermal denervation procedures for chronic LBP.
Criteria for considering studies for this review
Types of studies
Only randomized controlled trials with at least 1 day of follow-up were considered in this systematic review.
Types of participants
In order to be included in this review, participants of the randomized controlled trials (RCTs) must fulfil the following inclusion criteria: adult subjects (≥18 years of age) with chronic (>12 weeks duration) LBP (including subjects with radiculopathy or any other non-specific degenerative pathology, such as osteoarthritis). Exclusion criteria were (1) trials including subjects with specific LBP caused by pathological entities, such as vertebral spinal stenosis, ankylosing spondylitis, scoliosis, or coccydynia; (2) post-partum LBP or pelvic pain due to pregnancy; (3) post-operative studies; (4) prevention studies; and (5) abstracts or non-published studies.
Types of interventions
RCTs studying the following interventions were included in this overview: injection of medications or proteolytic enzymes (chemonucleolysis); and radiofrequency or thermal denervation procedures. All anatomical sites subject to injection therapy (intervertebral disc, facet joint, epidural space, intramuscular) and denervation procedures (facet joint, intervertebral disc, spinal nerves) for LBP were included. Additional interventions were allowed in all studies if there was a contrast for the injection therapy or denervation procedure in the study.
Types of outcome measures
To be included at least one of the following outcome measures should have been measured in the RCT: pain intensity [e.g. visual analog scale (VAS), numerical rating scale (NRS), McGill pain questionnaire], back specific functional status [e.g. Roland–Morris Disability Questionnaire, Oswestry Disability Index (ODI)], perceived recovery (e.g. overall improvement), and return to work (e.g. return to work status, sick leave days). The primary outcomes for this review were pain and functional status.
Search methods for identification of studies
Existing systematic reviews for the interventions were screened for studies fulfilling the inclusion criteria [3–6]. Then, the literature was searched in the Cochrane Back Review Group (CBRG) trial register from the last date onward for each of the interventions up to November 17, 2009.
References of relevant studies were screened and experts were approached in order to identify additional primary studies not identified in the previous steps. The language was limited to English, Dutch, French and German, because these are the languages that the authors are able to read and understand. The search strategy outlined by the CBRG was followed [7].
Methods of the review
Study selection
Two authors (NH, TK) independently screened the abstracts and titles retrieved by the search strategy and applied the inclusion criteria to all relevant abstracts. The full text version of an article was obtained if the title and abstract seemed to fulfill the inclusion criteria or if eligibility of the study was unclear. All full text articles from the existing reviews were compiled and independently screened for inclusion criteria by the authors. Any disagreements on study eligibility were resolved by discussion and a consensus meeting.
Risk of bias assessment
Two authors (NH, TK) independently assessed the risk of bias (RoB) of all eligible studies using the criteria list advised by the CBRG, which consists of 11 items [7]. Items were scored as ‘positive’ if they fulfilled the criteria, as ‘negative’ when there was a clear RoB, and as ‘inconclusive’ if there was insufficient information. Differences in assessment were discussed during a consensus meeting. A total score was computed by adding the number of positive scores, and low RoB was defined as fulfilling six or more (more than 50%) of the 11 internal validity criteria. Empirical evidence has shown that studies fulfilling <6 items report higher treatment effects than studies fulfilling 6 or more items [8].
Data extraction
A standardized form was used for data extraction which included collection of descriptive data on the study population and the type of intervention, as well as quantitative data regarding the outcome measures. Data on the characteristics of the study population (gender, age), type of therapy and control treatment, adverse events and complications were also collected.
Data analysis
If studies were clinically homogeneous regarding study population, types of treatment, outcomes and measurement instruments, a meta-analysis was performed. If possible, the weighted mean difference (WMD) was calculated because this improves the interpretability of the results. If a WMD was not possible the standardized mean difference (SMD) was calculated. If trials reported outcomes as graphs, the mean scores and standard deviations (SD) were estimated from these graphs. If SD were not reported, they were calculated using the reported values of the confidence intervals, if possible. If the SD of the baseline score was reported, we used the ratio between the baseline score and SD to calculate the SD for other follow-up moments. Finally, if none of these data were reported, an estimation of the SD was based on study data (population and score) of other studies. In order to correct for error introduced by “double-counting” of subjects of “shared” interventions (i.e. 2 comparisons within 1 study that used the same control group as contrast) in the meta-analyses, the number of subjects in the control group was divided by the number of comparisons that this one study added in the meta-analyses. For the comparisons where studies were too heterogeneous, no meta-analysis was performed.
Quality of the evidence
Grades of recommendation, assessment, development and evaluation (GRADE) profiles were used to evaluate the overall quality of the evidence and the strength of the recommendations [9]. The quality of the evidence for a specific outcome was based upon five principal factors: (1) limitations (for example due to study design), (2) inconsistency of results, (3) indirectness (e.g. generalizability of the findings), (4) imprecision (e.g. sufficient data) and (5) other considerations, such as reporting bias. The overall quality was considered to be high when multiple RCTs with a low RoB provide consistent, generalizable, and precise data for a particular outcome. The quality of the evidence was downgraded by one level when one of the factors described above was not met [9]. Single studies were considered inconsistent and imprecise (i.e. sparse data) and provide “low quality evidence”, which could be further downgraded to “very low quality evidence” if there were also limitations in design or indirectness. The following grading of quality of the evidence was applied [10]:
High quality
Further research is very unlikely to change our confidence in the estimate of effect.
Moderate quality
Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate.
Low quality
Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Very low quality
We are very uncertain about the estimate.
Results
Description of studies
Study selection
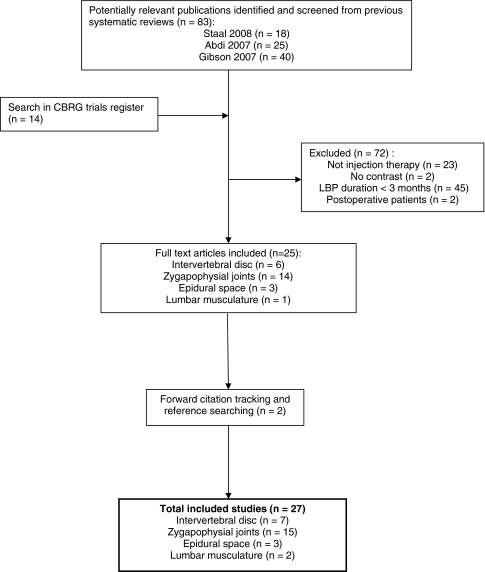
From three existing reviews a total of 83 references were screened for eligibility. Of these 83 articles, 11 studies fulfilled the inclusion criteria and were included in this overview (Fig. 1). The most important reason for exclusion was inclusion of acute or sub-acute patients in the study or lack of information about the duration of the complaints prior to the study. Additionally, 14 potentially relevant titles and abstracts were identified in the CBRG trial register for injection-related interventions and screened for potential inclusion. All of these abstracts fulfilled the inclusion criteria and were therefore included. Two additional studies were found by forward citation searching of included studies.
Fig. 1.
Flow diagram of selection process of studies on injection therapy for chronic LBP
In total 27 studies were included in this review. The study characteristics of all included (Appendix 1) and excluded studies (Appendix 2) are summarized in appendices.
Injection therapy
Intervertebral disc
One RCT was identified which evaluated injection therapy aimed at the intervertebral disc in chronic LBP patients [11]. The authors compared chemonucleolysis (intradiscal injection of chymopapain which digests the nucleus pulposus) to discectomy in patients with disc herniation which was confirmed by myelography [11]. This trial enrolled patients with both sub-acute and chronic LBP, but presented selected outcomes for the subgroup of patients (n = 58) with a duration of symptoms >6 months.
Zygapophysial joints (facet joints)
Eight trials, three of which were placebo controlled [12–14], evaluated intra-articular or peri-articular facet joint injections with corticosteroids (methyl-prednisolone, triamcinolone, or betamethasone) [12, 15], local anaesthetic (lidocaine, bupivacaine, or lignocaine) [14], sodium hyaluronate [16], Sarapin (a suspension of powdered pitcher plant in alkaline solution) [17], or a combination of these [13, 18, 19]. Three of these trials confirmed that pain was originating from the facet joint by including only patients with a positive response to local anaesthetic nerve block [12, 17, 18]. One trial used radiographic confirmation of facet joint arthritis as an inclusion criterion [16] while the remaining four trials used clinical criteria (e.g. unilateral pain, pain with sustained postures) to identify patients with facet joint pain [13–15, 19].
Epidural space
Three RCTs were identified that evaluated injections of corticosteroids [20, 21] or anaesthetic [22] into the epidural space. There were no placebo-controlled trials of injections into the epidural space. Comparisons in the included trials were made with benzodiazepine [21], spinal endoscopy [20] or between ropivacaine and bupivacaine [22]. One study excluded patients with a previous history of spinal surgery [20].
Spinal muscles (local injections)
Two RCTs were identified that evaluated local intramuscular injections for non-specific chronic LBP. One study compared injections of vitamin B12 with placebo [23], while the other compared injections of botulinum toxin A with placebo [24].
Denervation procedures
Intervertebral disc
Six RCTs were identified which evaluated denervation procedures [25–30] for chronic LBP targeted at or around the intervertebral disc. Five of the trials only included patients with positive responses to either analgesic [25] or provocative [26–29] discography.
Three trials evaluated the use of percutaneous intradiscal radiofrequency thermocoagulation (PIRFT). PIRFT involves the placement of an electrode or catheter into the intervertebral disc and applying an alternating radiofrequency current to reduce nociceptive input from the disc. Two of the trials were placebo controlled [25, 28], while the other compared high- with low-intensity PIRFT [26].
Two trials were identified which compared the use of intradiscal electrothermal therapy (IDET) with a placebo [27, 29]. IDET is similar to PIRFT and involves the insertion of an electrode into the annulus or nucleus of the intervertebral disc and application of electrothermal energy to alter the pain receptors.
One RCT evaluated radiofrequency denervation of the ramus communicans nerve compared with placebo denervation in patients who failed to respond to IDET [30]. This denervation is performed outside the intervertebral disc, unlike IDET and PIRFT.
Zygapophysial joints (facet joints)
Six trials compared radiofrequency denervation of the medial branch of the dorsal ramus with a sham denervation procedure [31–36], and one trial compared radiofrequency denervation of the dorsal root ganglion with a sham procedure [37]. The trial by Tekin and colleagues [34] included comparisons between conventional, pulsed, and sham radiofrequency denervation. All trials except one [32] included only patients with a positive response (~50–80% pain relief) to selective anaesthetic nerve blocks. The trial by Leclaire and colleagues [32] included patients who experienced significant relief of their LBP for at least 24 h during the week after intra-articular facet injections under fluoroscopy. This inclusion criterion was considered to be insufficiently sensitive and likely to have included patients with pain of non-facet joint origin [32]. Therefore, this trial was not included in the primary analysis, but a sensitivity analysis was performed to evaluate the addition of this study to the meta-analyses.
Risk of bias in included studies
The results of the RoB assessment are shown in Table 1. 18 studies (66%) had a low RoB. All studies were described as randomized; however, only nine studies (33%) used an adequate randomization procedure in combination with an adequate concealment of treatment allocation. In only four studies (15%) co-interventions were avoided or similar between groups. Many studies had acceptable compliance (20 studies; 77%) or acceptable drop-out rates (21 studies; 77%) or both (15 studies; 58%).
Table 1.
Risk of bias assessment of injection therapy studies
| Randomisation adequate? | Allocation concealed? | Groups similar at baseline? | Patient blinded? | Care provider blinded? | Outcome assessor blinded? | Co-interventions avoided or similar? | Compliance acceptable? | Drop-out rate described and acceptable? | Timing outcome assessment similar? | Intention-to-treat analysis? | Total score | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervertebral disc | ||||||||||||
| Barendse 2001 | + | + | + | + | + | + | ? | + | − | + | + | 9 |
| Kvarstein 2009 | + | + | + | + | − | + | − | − | + | + | + | 8 |
| Oh 2004 | ? | − | + | ? | − | ? | ? | + | ? | + | ? | 3 |
| Ercelen 2003 | + | − | + | ? | − | ? | ? | ? | + | + | ? | 4 |
| Pauza 2004 | + | + | + | + | − | + | + | + | + | + | − | 9 |
| Freeman 2005 | ? | + | + | + | + | + | ? | + | + | + | − | 8 |
| van Alphen 1989 | + | − | ? | − | − | − | ? | − | − | + | − | 2 |
| Facet joint | ||||||||||||
| Carette 1991 | + | ? | + | + | + | + | ? | + | + | + | − | 8 |
| Lilius 1989 | ? | ? | ? | − | − | − | ? | + | + | + | − | 3 |
| Fuchs 2005 | + | ? | + | − | − | ? | ? | + | + | + | − | 5 |
| Mayer 2004 | − | − | + | − | − | + | ? | ? | + | ? | ? | 3 |
| Manchikanti 2001 | ? | ? | + | − | − | ? | − | + | + | − | − | 3 |
| Manchikanti 2008 | + | + | + | + | − | ? | − | + | + | + | + | 8 |
| Marks 1992 | + | + | + | + | ? | + | − | + | + | + | − | 8 |
| Revel 1998 | ? | ? | + | + | + | + | ? | ? | + | + | + | 7 |
| van Kleef 1999 | + | ? | + | + | + | + | ? | + | ? | + | ? | 7 |
| Leclaire 2001 | + | + | + | + | − | + | + | + | + | + | + | 10 |
| van Wijk 2005 | + | + | + | + | + | + | ? | + | + | + | + | 10 |
| Gallagher 1994 | ? | ? | + | + | − | + | ? | ? | + | + | + | 6 |
| Nath 2008 | + | ? | − | + | + | + | ? | ? | + | + | ? | 6 |
| Tekin 2007 | + | ? | + | + | − | ? | + | + | + | + | ? | 7 |
| Geurts 2003 | + | + | + | + | + | + | ? | + | + | + | + | 10 |
| Epidural space | ||||||||||||
| Serrao 1992 | ? | ? | ? | + | ? | + | − | + | ? | + | ? | 4 |
| Dashfield 2005 | ? | + | − | + | − | + | ? | + | + | + | ? | 6 |
| Lierz 2004 | + | ? | + | + | + | ? | + | + | + | + | − | 8 |
| Intramuscular | ||||||||||||
| Mauro 2000 | ? | ? | − | ? | ? | + | ? | + | − | + | − | 3 |
| Foster 2001 | + | + | + | + | − | + | ? | + | + | + | + | 9 |
Effects of intervention
Feasibility of statistical pooling
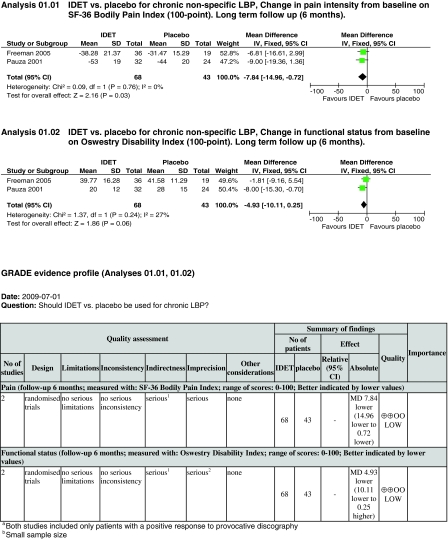
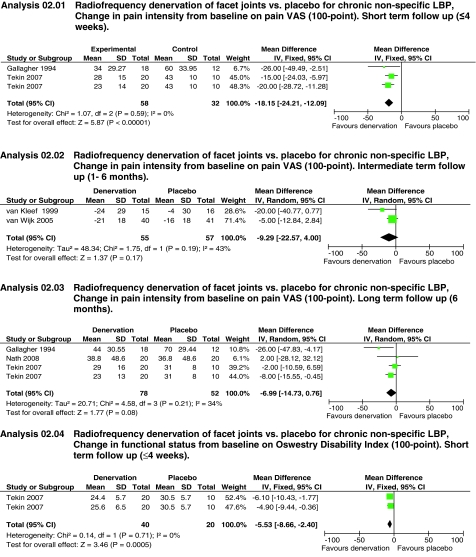
As stated in the methods section, statistical pooling was only considered if subgroups of studies were clinically homogeneous, and the authors provided sufficient information on study characteristics, outcome measures, and study results. After reviewing the included study characteristics, only two treatment subgroups (IDET vs. placebo and facet joint denervation vs. placebo) were sufficiently clinically homogeneous to perform statistical pooling (Table 2).
Table 2.
Pooled effect estimates for injection therapy and denervation procedures
| Outcome title | No. of studies | No. of participants | Statistical method | Effect size | |
|---|---|---|---|---|---|
| Comparison 01: IDET versus placebo for chronic non-specific LBP | |||||
| 01 | Change in pain intensity from baseline on SF-36 Bodily Pain Index (100-point). Long-term follow-up (6 months) | 2 | 111 | Weighted mean difference (fixed) 95% CI | −7.84 [−14.96, −0.72] |
| 02 | Change in functional status from baseline on Oswestry Disability Index (100-point). Long-term follow-up (6 months) | 2 | 111 | Weighted mean difference (fixed) 95% CI | −4.93 [−10.11, 0.25] |
| Comparison 02: radiofrequency denervation of lumbar facet joints compared with placebo for chronic LBP | |||||
| 01 | Change in pain intensity from baseline on 100-point VAS. Short-term follow-up (≤4 weeks) | 2 | 90 | Weighted mean difference (fixed) 95% CI | −18.15 [−24.21, −12.09] |
| 02 | Change in pain intensity from baseline on 100-point VAS. Intermediate-term follow-up (1–6 months) | 2 | 112 | Weighted mean difference (random) 95% CI | −9.29 [−22.57, 4.00] |
| 03 | Change in pain intensity from baseline on 100-point VAS. Long-term follow-up (6 months) | 3 | 130 | Weighted mean difference (random) 95% CI | −6.99 [−14.73, 0.76] |
| 04 | Change in functional status from baseline on Oswestry Disability Index. Short-term follow-up (≤4 weeks) | 1 | 60 | Weighted mean difference (fixed) 95% CI | −5.53 [−8.66, −2.40] |
Injection therapy
Intervertebral disc
Chemonucleolysis versus other treatment
In one RCT with a high RoB, chemonucleolysis (via intradiscal chymopapain injection) was compared with discectomy [11]. A subgroup of 68 patients had duration of symptoms >6 months prior to the start of the trial. There was no difference between groups in percentage of patients whose pain had disappeared or improved (87 vs. 85%) 12 months post-treatment. Within 12 months post-treatment, 25% of the chemonucleolysis group were considered treatment failures and underwent surgery.
There is very low quality evidence (1 RCT; n = 68; limitations in design, inconsistency, imprecision) that chemonucleolysis is no more effective than discectomy over a long-term follow-up.
Zygapophyseal joint (facet joint)
Facet joint injections with corticosteroids versus placebo
Two RCTs, one with low RoB [12] and one with high RoB [13], compared the effects of facet joint injections with corticosteroids to placebo injections. There was insufficient data on pain and functional status in the Lilius study [13] to allow for statistical pooling of outcomes. In the Carette study [12], no significant differences were found between the groups at 1 and 3 months for pain, functional status or self-rated improvement. At the 6-month follow-up, significant differences were found in favour of the corticosteroid group [12]. The high RoB study [13] compared intra-articular and peri-capsular corticosteroid injections with placebo injections. No significant differences between the groups were reported for pain, disability or work attendance at either short- or intermediate-term follow-ups [13]. No side effects apart from transient pain were reported.
There is very low quality evidence (1 RCT; n = 97; inconsistency, indirectness, imprecision) that there is no significant difference in effect between facet joint injections with corticosteroids and placebo injections for short- to intermediate-term pain relief and improvement of function.
Facet joint injections with corticosteroids versus other treatment
Five RCTs compared the effects of corticosteroids injections into and around the facet joints with other treatments [15–19]. Because of the clinical heterogeneity of the reference treatments, pooling was determined to be unsuitable.
In a study with low RoB [19], intra-articular facet joint injections with corticosteroids and lignocaine were compared with facet nerve blocks using similar medication. The facet joint injections provided slightly better pain relief than facet nerve blocks, although statistical significance was only reached at 1 month, not immediately post-treatment or after 3 months [19].
Two RCTs with high RoB compared intra-articular facet joint corticosteroid injections with other treatments; one compared facet joint injections with a mixture of local anaesthetics and corticosteroids combined with a home stretching exercise program with the home stretching exercise program only [15]. No significant post-treatment differences between the groups were found for pain and disability. The other trial compared the effects of facet joint corticosteroid injections with intra-articular sodium hyaluronate injections. No significant differences in pain relief, disability and quality of life between the groups were found at different follow-up points over a 6-month period [16].
One RCT with low RoB [18] compared the effects of multiple medial branch blocks of corticosteroids combined with local anaesthetics with multiple medial branch blocks consisting of only local anaesthetics. No significant differences between the groups were found at 3, 6 or 12 months post-treatment. One RCT with high RoB [17] compared the effects of multiple medial branch blocks of corticosteroids combined with local anaesthetics and Sarapin with multiple medial branch blocks consisting of local anaesthetics and Sarapin. No significant differences between the groups were found for pain relief, overall health, functional status and return-to-work over more than 2 years of follow-up.
There is low quality evidence (1 RCT; n = 86; inconsistency, imprecision) that intra-articular facet joint injections are slightly more effective than facet nerve blocks for pain relief in the intermediate term. There is very low quality evidence (1 RCT; n = 70; limitations in design, inconsistency, imprecision) that intra-articular facet joint injections add no benefit to a home exercise stretching program in terms of pain and disability over the short term. There is very low quality evidence (1 RCT; n = 60; limitations in design, inconsistency, imprecision) that there is no significant difference in effect between intra-articular facet joint corticosteroid injections and intra-articular injections of sodium hyaluronate on pain and disability over a long-term follow up. There is very low quality evidence (1 RCT; n = 120; inconsistency, indirectness, imprecision) that the addition of corticosteroids does not increase the effectiveness of facet joint nerve blocks with local anaesthetic. There is very low quality evidence (1 RCT; n = 73; limitations in design, inconsistency, indirectness, imprecision) that the addition of corticosteroids does not increase the effectiveness of facet joint nerve blocks with anaesthetic and Sarapin in chronic LBP.
Facet joint injections with local anaesthetic versus placebo
One RCT with low RoB [14] compared intra-articular facet joint injections with lidocaine to intra-articular facet joint injections with saline. In both groups these injections were followed by an injection of corticosteroid (cortivazol) near the joints. The lidocaine group had significantly higher pain relief post-treatment than the saline group [14].
There is low quality evidence (1 RCT; n = 80; inconsistency, imprecision) that intra-articular facet joint injections with lidocaine combined with peri-articular corticosteroid injections are more effective for short-term pain relief than placebo.
Epidural space
Epidural corticosteroid injections versus other treatments
In an RCT with high RoB [21], an epidural injection with a corticosteroid and dextrose solution was compared with an intrathecal benzodiazepine with dextrose injection. Two weeks and 2 months post-treatment, no significant differences between the groups were reported for pain relief or general improvement.
One RCT with low RoB [20] compared caudal epidural local anaesthetic and steroid injection with targeted epidural local anaesthetic and steroid placement with a spinal endoscope. No significant differences were found between the groups for any of the outcome measures at any of the times. In all patients in the endoscope group, post-treatment low-back discomfort was experienced but this was not persistent.
There is very low quality evidence (2 RCTs; n = 88; limitations in design, imprecision, inconsistency) that epidural corticosteroid injection is not significantly different to benzodiazepine injection or targeted epidural placement for pain relief over the short to intermediate term.
Epidural injections with local anaesthetics versus other treatments
One RCT with low RoB [22] compared the effects of epidural blocks with ropivacaine with epidural blocks with bupivacaine. Eight single shot epidural injections followed by active physiotherapy were performed in all patients. There were no significant differences found between the groups in post-treatment analgesia. There were three cases of short episodes of headache post-injection.
There is low quality evidence (1 RCT; n = 40; imprecision, inconsistency) that there is no significant difference in analgesia provided by blocks of ropivacaine or bupivacaine in the short term.
Lumbar musculature
Intramuscular injections with vitamin B12 versus placebo
In one RCT with high RoB [23], the effects of intramuscular vitamin B12 injections were compared with intramuscular placebo injections. Post-treatment, there were significant improvements for pain and disability in favour of the vitamin B12 group.
There is very low quality evidence (1 RCT; n = 60; limitations in design, inconsistency, imprecision) that intramuscular vitamin B12 injections are more effective than intramuscular placebo injections for short-term pain relief and improvement of function.
Intramuscular injections with botulinum toxin A versus placebo
In one RCT with low RoB, intramuscular injections of botulinum toxin A were compared with intramuscular placebo injections of saline [24]. At 3 weeks follow-up, the degree of pain relief was significantly different between groups in favour of the botulinum toxin A group. At 8 weeks patients in the botulinum toxin A group had significantly more pain relief and better ODI scores than the placebo group.
There is low quality evidence (1 RCT; n = 31; inconsistency, imprecision) that intramuscular botulinum toxin A injections are more effective for pain relief in the short- and intermediate-term than placebo.
Denervation procedures
Intervertebral disc
Percutaneous intradiscal radiofrequency thermocoagulation versus placebo
In one placebo-controlled trial (n = 28) with low RoB, no significant differences were found between PIRFT and sham PIRFT in pain VAS scores, global perceived effect, ODI, or a composite outcome of overall treatment success 8 weeks post-treatment [25]. In a second placebo-controlled trial (n = 20) with low RoB, only follow-up data which were collected after 6 and 12 months post-treatment were reported [28]. No significant differences were seen between the PIRFT and sham-PIRFT groups on pain intensity or functional status at either of these time points. Because of the variability in the timing of outcome measures between these two studies, a decision was made not to pool the results.
A third trial (n = 37) with high RoB found minimal improvement over 6 months on pain (VAS) and disability (ODI) with both lower- and higher- intensity of PIRFT. No significant differences were found between the groups at any of the follow-up assessments [26]. No complications or adverse events were reported in the placebo-controlled trials. One patient was excluded from the analysis of Ercelen et al. [26] because of discitis.
There is low quality evidence (1 RCT; n = 28; inconsistency; imprecision) that there is no difference between PIRFT and placebo in pain and functional status outcomes over an intermediate term of follow-up. There is also low quality evidence (1 RCT; n = 20; inconsistency; imprecision) that there is no difference between PIRFT and placebo in pain and functional status outcomes over a long-term follow-up.
Intradiscal electrothermal therapy versus placebo: pain
In patients with a positive response to provocative discography, two small (n = 55 and n = 56), low RoB, placebo-controlled randomized trials evaluated IDET and both provided sufficient data for pooling [27, 29]. Both studies measured pain with the SF-36 Bodily Pain Index (100-point scale). The Chi-square value for homogeneity of the WMD was 0.09 (P > 0.05), indicating statistical homogeneity among these studies.
There is low quality evidence (2 RCTs; n = 111; indirectness, imprecision) that IDET is more effective than placebo for pain relief over a long-term (6 months) follow-up (WMD −7.84; 95% CI −14.96 to −0.72) (Table 2, Analysis 01.01).
Intradiscal electrothermal therapy versus placebo: functional status
The same two RCTs [27, 29] provided ODI scores on a 100-point scale which allowed statistical pooling. The Chi-square value for homogeneity of the WMD was 1.37 (P > 0.05), indicating statistical homogeneity among these studies.
There is low quality evidence (2 RCTs; n = 111; indirectness, imprecision) that IDET is no more effective than placebo in improving functional status over a long-term (6 months) follow-up (WMD −4.93; 95% CI −10.11 to 0.25) (Table 2, Analysis 01.02).
In patients unresponsive to treatment with IDET, one high RoB RCT found radiofrequency denervation of the ramus communicans nerve was associated with better VAS pain, SF-36 bodily pain and SF-36 physical function scores after 4 months compared to sham denervation [30]. In one RCT, four patients who underwent IDET experienced transient radiculopathy (<6 weeks) [27]. No other serious adverse events were reported in the three trials.
Zygapophyseal joint (facet joint)
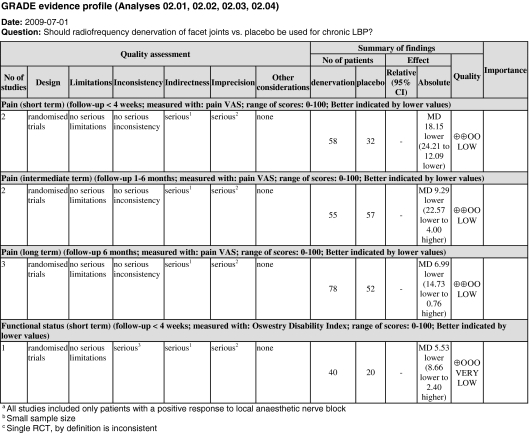
Radiofrequency denervation of facet joints versus placebo: pain
Five RCTs provided sufficient data on pain VAS scores to allow for pooling over a short-, intermediate- or long-term follow-up [31, 33–36]. All studies included only patients with a positive response (~50–80% pain relief) to local anaesthetic nerve block. One RCT was not included in the primary analyses due to clinical heterogeneity of patient selection procedures [32].
For short-term outcomes (<4 weeks), the Chi-square value for homogeneity of the WMD was 1.07 (_P_ > 0.05), indicating statistical homogeneity between two of the RCTs. There is low quality evidence (2 RCTs; n = 90; indirectness, imprecision) that radiofrequency denervation of lumbar facet joints is more effective than placebo for pain relief over a short-term follow-up (WMD −18.15; 95% CI −24.21 to −12.09) (Table 2, Analysis 02.01).
For intermediate-term outcomes (1–6 months), the Chi-square value for homogeneity of the WMD was 1.75 (P > 0.05). There is low quality evidence (2 RCTs; n = 112; indirectness, imprecision) that radiofrequency denervation of lumbar facet joints is no more effective than placebo for pain relief in the intermediate term (WMD −9.29; 95% CI −22.57 to 4.00) (Table 2, Analysis 02.02).
For long-term outcomes (6 months), the Chi-square value for homogeneity of the WMD was 4.58 (P > 0.05). There is low quality evidence (3 RCTs; n = 130; indirectness, imprecision) that radiofrequency denervation of lumbar facet joints is no more effective than placebo for pain relief in the long term (WMD −6.99; 95% CI −14.73 to 0.76) (Table 2, Analysis 02.03).
When the study by Leclaire and colleagues [32] was included in the analyses, the pooled WMD (95% CI) for pain intensity was −14.80 (−22.77 to −6.82) in the short-term and −3.85 (−16.27 to 8.57) in the intermediate term. While the addition of this study to the meta-analyses slightly altered the pooled WMD, it did not change the conclusions.
One RCT with low RoB [37] compared radiofrequency denervation of the dorsal root ganglion with sham denervation. No significant differences were found between groups at 3-month follow-up. Adverse events and complications did not differ between treatments, and no serious complications or side effects arose in either group. There is very low quality evidence (1 RCT; n = 83; inconsistency, indirectness, imprecision) that radiofrequency denervation of the dorsal root ganglion is no more effective than placebo for pain relief in the intermediate term.
Radiofrequency denervation of facet joints versus placebo: functional status
One RCT comparing conventional and pulsed radiofrequency denervation to placebo provided sufficient data on functional status outcomes (ODI 0–100 scale) to allow for statistical pooling [34].
There is very low quality evidence (1 RCT; n = 60; inconsistency, indirectness, imprecision) that radiofrequency denervation of lumbar facet joints is more effective than placebo for improvement of function in the short term (WMD −5.53; 95% CI −8.66 to −2.40) (Table 2, Analysis 02.04).
When the study by Leclaire and colleagues [32] was included in the analyses, the WMD (95% CI) became −3.45 (−7.68 to 0.77) in the short term and −6.57 (−17.00 to 3.85) in the intermediate term (when pooled with the study by van Kleef et al. [35]). While the addition of this study to the meta-analyses slightly altered the short-term pooled WMD, it also changed the GRADE profile and the overall quality of the evidence from very low to low.
Radiofrequency denervation of facet joints versus other treatment
In a study with low RoB [34], conventional radiofrequency denervation of the lumbar facet joints was compared with pulsed radiofrequency denervation. Both treatments improved pain VAS and ODI scores compared with placebo, with conventional denervation improving significantly more than pulsed denervation by 6 months and 1 year post-treatment.
There is very low quality evidence (1 RCT; n = 40; inconsistency, indirectness, imprecision) that conventional radiofrequency denervation is more effective than pulsed radiofrequency denervation of the facet joints for pain relief or improvement of function over the long term.
Discussion
In this review, 27 RCTs were included that evaluated the effectiveness of injection therapy and denervation procedures for chronic LBP.
The effectiveness of the different therapies
In this review we found only low to very low quality evidence to support the use of injection therapy and denervation procedures in chronic LBP patients. Low quality evidence means that further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
From the 26 included RCTs, only two treatment subgroups (IDET vs. placebo, and radiofrequency denervation of facet joints vs. placebo) were considered to be clinically homogeneous enough to allow for statistical pooling. The results showed that IDET is more effective than placebo for pain relief over 6 months of follow-up and radiofrequency denervation of lumbar facet joints more effective than placebo for pain relief over a short-term (<4 weeks) follow-up. The quality of the evidence in both of these comparisons was downgraded to low quality due to imprecision and indirectness. Indirectness (lack of ability to generalize) refers to the extent to which the people, interventions and outcomes in the trials are not comparable to those defined in the inclusion criteria of the review. As all of the pooled RCTs selected patients for inclusion only if they had a positive response to either provocative discography (IDET vs. placebo) or local anesthetic nerve block (radiofrequency denervation of facet joints vs. placebo). While the selection of appropriate patients may be considered necessary for these therapies, the results cannot be generalized to all patients with chronic LBP. However, from the perspective of pain clinics or anesthesiologists these populations may be generalizable to their setting. In that case, the level of evidence is moderate, indicating that further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Consequently, further research is needed for a more confident estimate of effect.
Methodological considerations
The RoB assessment describes whether a RCT reported certain methodological features known to decrease bias when interpreting the results. However, despite the fact that the RoB of the included studies was generally low, many studies showed flaws regarding concealment of treatment allocation, care provider blinding, avoidance of co-interventions and performing intention-to-treat analyses. Overall, only low to very low quality evidence was found by this review. By using the GRADE approach, we were able to determine an overall judgment of the quality of the evidence not only from the limitations in design, but also considering aspects such as inconsistency among studies, imprecision and indirectness.
It is recommended that study features which are associated with a lower RoB in RCTs be considered when designing future trials of non-surgical interventional therapy, as well as adequate reporting of these features.
Adverse effects
In the majority of studies presented in this review, no adverse events or side effects associated with the treatments were reported. Transient symptoms such as increased low-back discomfort or paraesthesia were noted in a few studies. Epidural injections were associated with nausea and headache in some patients. In a study which used discectomy as a reference treatment [11], a dural defect with leakage of cerebrospinal fluid and a partial cauda equina were noted, though unsure whether these patients were in the injection therapy or surgery group. Most trials were small and not designed to evaluate adverse events, so no clear conclusion can be drawn regarding the risks of injection therapy and denervation procedures.
Strengths and limitations
Several biases can be introduced in systematic reviews by literature search and selection procedures. It is possible that in searching studies for this review, relevant but unpublished trials may have been missed, which are often likely to be small studies without positive results, leading to publication bias. However, because the majority of published trials was small and did not show a positive effect, publication bias does not seem to be a big problem in this review. Screening references of identified trials and systematic reviews may result in an over representation of positive studies in the review, because trials with a positive result are more likely to be referred to in other publications, leading to reference bias. Only studies published in English, Dutch, French or German were included in this review. It is not clear whether a language restriction is associated with bias [38].
Due to the study selection criterion used, including only trials of chronic (>3 months duration) LBP patients, this review included less studies than similar Cochrane reviews [3, 5]. Many excluded RCTs failed to explicitly state the duration of symptoms experienced by the patients, while others considered only the length of time patients were unresponsive to conservative treatment as part of their inclusion criteria. However, the main conclusions of our review appear to be similar to recent systematic reviews [3–6], which generally report a paucity of RCTs on injection therapy and denervation procedures for chronic LBP and insufficient evidence to support their use.
Implications for research
To conclude, we identified 27 RCTs that evaluated various types of injection therapy or denervation procedures at different locations for patients with chronic LBP. Most of the studies included in this review were small and had a low RoB, though there were methodological weaknesses, especially regarding concealment of allocation, co-interventions and use of intention-to-treat analyses. The quality of evidence was low or very low, indicating that further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. There is a need for future high-quality placebo-controlled RCTs with large sample sizes on injection therapy and denervation procedures.
Implications for practice
In patients with chronic LBP there is only low to very low quality evidence to support the use of injection therapy for pain relief and improvement of function. It cannot be ruled out that in carefully selected sub-groups of patients, such as those with a positive response to discography or local anaesthetic nerve block, certain interventional therapies may be of some benefit. Potential benefits must be weighed against possible adverse effects when deciding whether to provide injection therapy or denervation to chronic LBP patients.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Appendix 1
See Table 3.
Table 3.
Characteristics of included studies
| Study: Barendse 2001 | |
|---|---|
| Methods | RCT; “randomized to two treatment groups by computer program” |
| Participants | 28 patients, aged 30–65 years, with a history of chronic LBP >12 months referred to a pain management centre. Only patients with a positive response to analgesic discography (>50% temporary reduction in pain over 30 min) were included. Exclusion criteria were multilevel discogenic pain, spinal stenosis, spondylolisthesis, coagulation disturbances, pregnancy, high VAS, diabetes mellitus, and positive diagnostic block of L3, L4 or L5 zygapophysial joints |
| Interventions | Injection treatment (I): percutaneous intra-discal radiofrequency thermocoagulation (radiofrequency probe inserted via cannula into disc using tunnel vision fluoroscopy), creating a 90-s 70°C lesion (n = 13) Reference treatment (R): sham radiofrequency thermocoagulation (treated in an identical way, but no radiofrequency current was applied) (n = 15) |
| Outcomes | No significant differences were found for any of the primary or secondary outcomes after 8 weeks post-treatment. Change in VAS was −0.61 in (I) and −1.14 in (R); while change in Oswestry scale was −2.62 in (I) and −4.93 in (R) |
| Notes | No complications during or after the procedures were reported. Methodological quality: randomization +; treatment allocation +; baseline similarity +; patients blinded +; care providers blinded +; outcomes blinded +; co-interventions ?; compliance +; drop outs −; timing of outcomes +; intention-to-treat +. Total score = 9 |
| Study: Carette 1991 | |
| Methods | RCT; “generated from a table of random numbers” |
| Participants | 101 patients, aged 18–65 years, with chronic LBP and a positive response to lumbar facet joint anaesthetic block. Exclusion criteria included specific LBP, previous injections into the facet joints, previous low-back surgery, pregnancy, known allergy to local anaesthetic and the presence of a blood coagulation disorder Four patients were later excluded from the analysis. |
| Interventions | Injection treatment (I): lumbar facet joint injection of corticosteroid (1 ml methylprednisolone acetate mixed with 1 ml isotonic saline) (n = 49) Reference treatment (R): sham lumbar facet joint injection (2 ml isotonic saline) (n = 48) |
| Outcomes | One to 3 months post-treatment, the two groups did not differ clinically or statistically in any of the outcome measures. By 6 months post-treatment, patients treated with (I) reported significantly better VAS (mean difference −1.0, 95% CI −2.0 to −0.1) and sickness impact profile-physical dimension scores (mean difference −3.0, 95% CI −5.5 to −0.5) compared with (R) |
| Notes | No adverse events were reported, other than transient local pain at the injection sites. Methodological quality: randomization +; treatment allocation ?; baseline similarity +; patients blinded +; care providers blinded +; outcomes blinded +; co-interventions ?; compliance +; drop outs +; timing of outcomes +; intention-to-treat −. Total score = 8 |
| Study: Dashfield 2005 | |
| Methods | RCT; “allocated randomly” |
| Participants | 60 patients, aged 18 years or more, with sciatica (defined as pain in the distribution of a lumbar nerve root, ± neurosensory and motor deficits) for a minimum of 6 months, but not for longer than 18 months. Patients with previous spinal surgery, coagulopathy, progressive motor neurone disorders, or peripheral vascular disease were excluded |
| Interventions | Injection treatment (I): caudal epidural corticosteroid injection (10 ml lidocaine 1% with 40 mg triamcinolone) injected into the epidural space (n = 33) Injection treatment (I2): lumbar epiduroscopy (painful nerve root identified and instilled with 10 ml lidocaine 1% with triamcinolone 40 mg) (n = 27) |
| Outcomes | No significant differences were found between the groups after 6 weeks, 3 months and 6 months post-treatment for any of the measures. For the (I) group, there were more significant differences between pre-treatment and post-treatment outcome measures compared with the (I2) group |
| Notes | Non-persistent post-procedure low-back discomfort occurred in all (I2) patients, and in fewer (I) patients Methodological quality: randomization ?; treatment allocation +; baseline similarity −; patients blinded +; care providers blinded −; outcomes blinded +; co-interventions ?; compliance +; drop outs +; timing of outcomes +; intention-to-treat ?. Total score = 6 |
| Study: Ercelen 2003 | |
| Methods | RCT; “patients were randomized into two treatment groups by computer” |
| Participants | 39 patients with chronic LBP who had been receiving conservative treatment for at least 2 years. Patients with spinal stenosis, instability, spondylolisthesis, diabetes mellitus, tumour infiltration, coagulation disorders, clinical radiculopathy, other neurologic abnormalities or systemic inflammatory diseases were excluded from the study. Only patients with a positive provocative discography at L4–L5, L5–S1, or both locations were randomized Two patients were excluded from the analysis (one with discitis, one lost to follow up) |
| Interventions | Injection treatment (I1): percutaneous intradiscal radiofrequency thermocoagulation (radiofrequency probe inserted via cannula into disc using fluoroscopy) at 80°C. Lesioning was performed for 120 s (n = 19) Injection treatment (I2): percutaneous intradiscal radiofrequency thermocoagulation, identical procedure to (I1) but lesioning was performed at 80°C for 360 s (n = 18) |
| Outcomes | No significant differences were observed between groups at any of the follow-up time points (post-treatment, 1 and 2 weeks, 1, 3, and 6 months). Post-treatment to 1 month scores on pain VAS and Oswestry disability scale decreased significantly compared with pre-treatment scores (P < 0.05). There were no statistical differences between the final (6 month) and the pre-treatment VAS and ODS values in both groups |
| Notes | Adverse events were not reported Methodological quality: randomization +; treatment allocation −; baseline similarity +; patients blinded ?; care providers blinded −; outcomes blinded ?; co-interventions ?; compliance ?; drop outs +; timing of outcomes +; intention-to-treat ?. Total score = 4 |
| Study: Foster 2001 | |
| Methods | RCT; “randomly assigned by drawing a card from a deck of shuffled cards” |
| Participants | 31 patients aged >18 years with chronic LBP greater on one side than the other. Exclusion criteria were LBP for <6 months, presence of a systemic inflammatory disorder, acute pathology on MRI, known allergy or sensitivity to botulinum toxin, pregnancy, disorders of neuromuscular transmission and anaesthetic or corticosteroid injections to the lumbar spine within 12 weeks of enrolment |
| Interventions | Injection treatment (I): intramuscular injections of botulinum toxin A at 5 lumbosacral sites, with each site receiving 40 units (n = 15) Reference treatment (R): intramuscular injections of saline to at 5 lumbosacral sites, with each site receiving 40 units (n = 16) |
| Outcomes | At 3 weeks, the degree of pain relief exceeded 50% (VAS score) in 11 of 15 patients (73.3%) in the (I) group compared with four of 16 (25%) in the (R) group (P < 0.012). The difference between these groups was 48% (95% CI 11.7–80.1). At 8 weeks, 9 of 15 patients (60%) in the (I) group and 2 of 16 (12.5%) in the (R) group reported pain relief exceeding 50% (P < 0.009), a difference of 47.5% (95% CI 10.5–79.1). For the Oswestry, 10 of 15 patients (66.7%) in the (I) group and 3 of 14 (18.8%) in the (R) group demonstrated improvement at 8 weeks (P < 0.011). The difference between groups was 47.9% (95% CI 10.9–79.6) |
| Notes | Injections were well tolerated by all patients and none had side effects Methodological quality: randomization +; treatment allocation +; baseline similarity +; patients blinded +; care providers blinded −; outcomes blinded +; co-interventions ?; compliance +; drop outs +; timing of outcomes +; intention-to-treat +. Total score = 9 |
| Study: Freeman 2005 | |
| Methods | RCT; “randomization schedule” |
| Participants | 57 patients with chronic LBP and evidence of degenerative disc disease on MRI. All subjects had one- or two-level symptomatic disc degeneration as determined by provocative lumbar discography. Exclusion criteria included the presence of a large contained or sequestered herniation, spinal stenosis, previous back surgery, spondylolisthesis, psychological disorders, and pregnancy Two subjects violated protocol and were not included in the analysis |
| Interventions | Injection treatment (I): intradiscal electrothermal therapy (IDET) at 90°C for 4 min, followed by a rehabilitation program (n = 38) Reference treatment (R): sham IDET, same procedure as (I) without connection to the generator, followed by a rehabilitation program (n = 19) |
| Outcomes | 6 months post-treatment, there were no significant differences between groups on any of the primary or secondary outcome measures. Mean difference (95% CI) between groups on the low-back outcome score was −1.71 (−3.82 to 0.41) and on Oswestry was −2.16 (−8.37 to 4.86) in favour of (I) |
| Notes | There were no serious adverse events in either arm of the study Methodological quality: randomization ?; treatment allocation +; baseline similarity +; patients blinded +; care providers blinded +; outcomes blinded +; co-interventions ?; compliance +; drop outs +; timing of outcomes +; intention-to-treat −. Total score = 8 |
| Study: Fuchs 2005 | |
| Methods | RCT; block randomization generated by computer |
| Participants | 60 patients with chronic LBP with radiologic confirmation of facet joint osteoarthritis. Patients with a history of hypersensitivity or contraindication to the test products, contraindication to intra-articular treatment, a current regimen of anticoagulants or radicular pain were excluded from the study |
| Interventions | Injection treatment (I): lumbar facet joint sodium hyaluronate injections (10 mg sodium hyaluronate in 1 ml buffer solution) bilaterally, under CT guidance at weekly intervals, for 3 weeks (n = 30) Injection treatment (I2): lumbar facet joint corticosteroid injection (10 mg triamcinolone acetonide in 1 ml crystalline suspension) bilaterally, under CT guidance at weekly intervals, for 3 weeks (n = 30) |
| Outcomes | No statistically significant differences between the groups in any outcomes were reported post-treatment, after 3 and 6 months. Pain VAS in the (I) group decreased from 69.2 ± 14.2 to 38.0 ± 26.5 mm by 3 months post-treatment. In the (I2) group the pain intensity decreased from 68.7 ± 11.5 to 33.4 ± 20.7 mm |
| Notes | No adverse effects were reported after administration of both therapies Methodological quality: randomization +; treatment allocation ?; baseline similarity +; patients blinded −; care providers blinded −; outcomes blinded ?; co-interventions ?; compliance +; drop outs +; timing of outcomes +; intention-to-treat −. Total score = 5 |
| Study: Gallagher 1994 | |
| Methods | RCT; randomisation method not stated |
| Participants | 41 patients, aged 25–55 years, with chronic LBP who fulfilled criteria for facet joint pain (including tenderness on palpation; pain on extension or rotation; pain exacerbated by exercise, sitting, and standing; and radiological evidence of facet joint degeneration). Subjects had a positive response to local anaesthetic injection into and around the painful joint. Exclusion criteria included previous back surgery, signs of nerve root compression, major mental illness, pending compensation claims and general ill health |
| Interventions | Injection treatment (I): radiofrequency denervation of lumbar facet joints at 80°C for 90 s (n = 24) Reference treatment (R): sham radiofrequency denervation with identical procedure except for the radiofrequency lesion (n = 27) |
| Outcomes | Analyses were split to allow comparisons between those with a good (n = 30) or equivocal (n = 11) response to facet joint block. Subjects with a good response in the (I) group had significantly lower mean (SE) VAS (34 (6.9) vs. 60 (9.8)) and McGill pain scores (9 (2.3) vs. 16 (2.8)) 1 month post-treatment, compared with the (R) group. 6 months post-treatment VAS scores were significantly low in the (I) compared with (R). In subjects with an equivocal response to facet joint block, no significant differences were found between groups at any time-point |
| Notes | Adverse events were not reported Methodological quality: randomization ?; treatment allocation ?; baseline similarity +; patients blinded +; care providers blinded −; outcomes blinded +; co-interventions ?; compliance ?; drop outs +; timing of outcomes +; intention-to-treat +. Total score = 6 |
| Study: Geurts 2003 | |
| Methods | RCT; “randomly allocated” |
| Participants | 83 patients, aged 18 years and more, with chronic LBP and a predominance of leg pain who responded positively to lumbar nerve blocks. Exclusion criteria were: previous radiofrequency treatment; indications for surgery (great pain, rapid progressive paresis, cauda equina syndrome); pregnancy; coagulation disorders; malignant disease; allergy to radiopaque contrast or local anaesthetics; and presence of neuropathic sensory or motor deficit, a non-segmental pattern of irradiating leg pain, or both Three patients required surgery post-treatment and were excluded from the analysis |
| Interventions | Injection treatment (I): radiofrequency lesioning of dorsal root ganglion at 67°C for 90 s (n = 44) Reference treatment (R): sham radiofrequency lesioning of dorsal root ganglion, identical procedure as (I) without the application of radiofrequency current (n = 36) |
| Outcomes | Three months post-treatment, 16% of (I) were assessed to have had successful treatment compared with 25% in (R) group, based on a composite outcome measure (difference −9.1% [95% CI −33.0 to 12.0], P = 0.43). No significant differences between groups were reported for mean change scores (SD) on back pain VAS (I) −0.6 (2.2) versus (R) −1.1 (2.4); change in daily activities (I) −0.5 (3.9) versus (R) −0.4 (3.4); change in analgesics use (I) 0.1 (1.4) versus (R) −0.2 (0.9); global subjective efficacy rating of benefit (I) 21% versus (R) 17%; or on any SF-36 subscales |
| Notes | 41 patients had at least one previous low-back surgery Adverse events did not differ between treatments, and no serious complications or side effects arose in either group Methodological quality: randomization +; treatment allocation +; baseline similarity +; patients blinded +; care providers blinded +; outcomes blinded +; co-interventions ?; compliance +; drop outs +; timing of outcomes +; intention-to-treat +. Total score = 10 |
| Study: Kvarstein 2009 | |
| Methods | RCT; “randomized” |
| Participants | 20 patients aged 20–65 years, with unremitting low-back pain for 6 months. All patients with signs of disc degeneration (MRI) or posterior annular tear (CT) underwent a three-level (L3/L4, L4/L5 and L5/S1) pressure-controlled provocation discography. Patients were eligible if the discography reproduced typical (‘‘concordant”) and intensive low-back pain (>7/10) at only one of the three levels. All eligible patients had pain >5/10 which was exacerbated by sitting and relieved by laying. Exclusion criteria included: positive medial branch blocks, acute infection, history of drug abuse, psychological disturbance, previous spine surgery, abnormal neurological examination, structural deformities or canal stenosis, pregnancy and disc herniations >4 mm |
| Interventions | Injection treatment (I): percutaneous intradiscal radiofrequency thermocoagulation (PIRFT) at a single level for 10 min (starting at 50°C, increasing by 5°C every 2 min, and ending with 4 min at 65°C) (n = 10) Reference treatment (R): sham percutaneous intradiscal radiofrequency thermocoagulation (PIRFT), same procedure as above but the annulus was not exposed to RF heating (n = 10) |
| Outcomes | After 6 months, there were no significant differences between (I) and (R) on pain intensity. Mean (SD) pain intensity at baseline, 6 and 12 months: (I) 5.4 (2.1), 4.4 (2.7), 4.0 (3.0) versus (R) 6.5 (2.2), 6.5 (2.0), 4.9 (2.7), respectively. No significant differences were observed between groups on any of the secondary outcome measures |
| Notes | Any serious adverse effects attributable to the treatment were not reported Methodological quality: randomization +; treatment allocation +; baseline similarity +; patients blinded +; care providers blinded −; outcomes blinded +; co-interventions −; compliance −; drop outs +; timing of outcomes +; intention-to-treat +. Total score = 8 |
| Study: Leclaire 2001 | |
| Methods | RCT; “randomization was performed in blocks of four” |
| Participants | 70 patients, aged 18–65 years, with chronic LBP and positive lumbar facet joint block. Exclusion criteria included allergy to local anaesthetic, blood coagulation disorder, cardiac pacemaker, sciatic pain with neurological deficit, specific low-back pain and previous low-back surgery |
| Interventions | Injection treatment (I): radiofrequency facet joint denervation under fluoroscopic guidance, 80°C for 90 s at a minimum of two levels (n = 36) Reference treatment (R): sham radiofrequency denervation, same procedure as (I), without radiofrequency lesion (n = 34) |
| Outcomes | After 4 weeks, mean (SD) Roland–Morris scores improved by 8.4 (17.4) in the (I) group and by 2.2 (14.7) in (R), showing a mean difference (95% CI) of 6.2 (−1.3 to 13.8). There was no significant treatment effect after 12 weeks. No significant differences were found at any time point for pain VAS, Oswestry score, or the secondary outcomes |
| Notes | No complications after the intervention was reported by patients Methodological quality: randomization +; treatment allocation +; baseline similarity +; patients blinded +; care providers blinded −; outcomes blinded +; co-interventions +; compliance +; drop outs +; timing of outcomes +; intention-to-treat +. Total score = 10 |
| Study: Lierz 2004 | |
| Methods | RCT; randomization performed by computer |
| Participants | 40 patients, aged 20–70 years, with chronic LBP. Exclusion criteria included presence of a motor deficit, recent change of analgesics, pulmonary hypertension, pulmonary artery stenosis, aortic stenosis, mitral stenosis, AV-block grade III, extreme hypovolaemia, coagulation disorders, pregnancy or sepsis/infection |
| Interventions | Injection treatment (I): lumbar epidural block (10 ml ropivacaine 0.2%) (n = 20) Injection treatment (I2): lumbar epidural block (10 ml bupivacaine 1.125%) (n = 20) Eight single shot epidural blocks at an interval of 2 or 3 days. Active physiotherapy was performed immediately after each session in both groups |
| Outcomes | There was no significant difference between groups in analgesia post-treatment. Mean (SD) pain intensity in (I) decreased from 7.0 (1.6) to 4.0 and from 7.1 (1.6) in (I2) to 4.2. No significant differences between groups were reported in haemodynamic variables |
| Notes | There were three cases of short episodes of headache, two in the (I) group and one in the (I2) group. Methodological quality: randomization +; treatment allocation ?; baseline similarity +; patients blinded +; care providers blinded +; outcomes blinded ?; co-interventions +; compliance +; drop outs +; timing of outcomes +; intention-to-treat −. Total score = 8 |
| Study: Lilius 1989 | |
| Methods | RCT; randomisation method not stated |
| Participants | 109 patients aged 19–64 years with chronic LBP |
| Interventions | Injection treatment (I): lumbar facet joint injection of corticosteroid and local anaesthetic [6 ml (30 mg) bupivacaine hydrochloride mixed with 2 ml (80 mg) methylprednisolone acetate] (n = 28) Injection treatment (I2): the same mixture, injected peri-capsularly around the lumbar facet joint (n = 39) Reference treatment (R): sham lumbar facet joint injection (8 ml of physiological saline) (n = 42) |
| Outcomes | No significant differences between groups was seen post-treatment, after 2 weeks, or after 6 weeks in work status, pain intensity, or physical range of motion measurements. Data in graphs |
| Notes | Twenty-seven patients had a history of previous vertebral disc surgery Few side effects were reported and their occurrence did not differ between groups Methodological quality: randomization ?; treatment allocation −; baseline similarity ?; patients blinded −; care providers blinded −; outcomes blinded −; co-interventions ?; compliance +; drop outs +; timing of outcomes +; intention-to-treat −. Total score = 3 |
| Study: Manchikanti 2001 | |
| Methods | RCT; randomization procedure not described |
| Participants | 73 patients with LBP with or without lower extremity pain for more than 6 months who did not exhibit neurological deficits and who responded positively to lidocaine blocks |
| Interventions | Injection treatment (I): lumbar facet joint injection with local anaesthetic and Sarapin (0.5% lidocaine or 0.25% bupivacaine mixed with equal volumes of Sarapin) (n = 32) Injection treatment (I2): lumbar facet joint injection with a mixture of local anaesthetic, Sarapin, and corticosteroid (0.5% lidocaine or 0.25% bupivacaine mixed with equal volumes of Sarapin and 1 mg of methyl prednisolone/ml of the mixture) (n = 41) |
| Outcomes | Results showed that patients underwent multiple procedures over a period of 2½ years. Post-treatment, no significant differences were reported between the groups in pain relief, overall health status, physical, functional or psychological status. Average pain scores (mean ± SEM) decreased from 7.6 ± 0.13 to 3.5 ± 0.26 in (I) and from 7.7 ± 0.12 to 3.3 ± 0.15 in (I2) |
| Notes | 17 patients had previous lumbar laminectomy No complications were reported in any of the patients Methodological quality: randomization ?; treatment allocation −; baseline similarity +; patients blinded −; care providers blinded −; outcomes blinded ?; co-interventions −; compliance +; drop outs +; timing of outcomes −; intention-to-treat −. Total score = 3 |
| Study: Manchikanti 2008 | |
| Methods | RCT; “computer-generated random allocation sequence” |
| Participants | 120 patients aged over 18 years with chronic non-specific LBP and a diagnosis of lumbar facet joint pain by lumbar anaesthetic block. Exclusion criteria were lack of positive response to controlled comparative local anaesthetic blocks, uncontrollable or unstable opioid use, psychiatric disorders, pregnancy, and patients with a history or potential for adverse reaction(s) to local anaesthetic, Sarapin or steroid |
| Interventions | Injection treatment (I): lumbar facet joint nerve blocks with local anaesthetic (bupivacaine 0.25%) (n = 60) Injection treatment (I2): lumbar facet joint nerve blocks with a mixture of bupivacaine and betamethasone (n = 60) |
| Outcomes | There were no significant differences in treatment effect of (I) compared to (I2) at 3, 6, or 12 months post-treatment. Pain scores (mean ± SD) at baseline: (I) 8.2 ± 0.8, (I2) 7.9 ± 1.0; at 3 months (I) 3.8 ± 1.3, (I2) 3.5 ± 1.1; at 6 months (I) 3.6 ± 1.5, (I2) 3.3 ± 0.8; and at 12 months (I) 3.7 ± 1.7, (I2) 3.5 ± 1.1 |
| Notes | There were no major adverse events reported over a period of 1 year Methodological quality: randomization +; treatment allocation +; baseline similarity +; patients blinded +; care providers blinded −; outcomes blinded ?; co-interventions −; compliance +; drop outs +; timing of outcomes +; intention-to-treat +. Total score = 8 |
| Study: Marks 1992 | |
| Methods | RCT; “random number system” |
| Participants | 86 patients with chronic LBP present most of the time for at least 6 months. Exclusion criteria were a radicular pattern in either lower limb, straight leg raising limited at <60°, and evidence of any progressive spinal disorder of non-degenerative origin |
| Interventions | Injection treatment (I): lumbar facet joint injection with corticosteroids and anaesthetic (20 mg methylprednisolone acetate followed by 1.5 ml lignocaine) (n = 42) Injection treatment (I2): lumbar facet nerve block of the medial articular branch of the posterior primary ramus from L1 to L5 (20 mg methylprednisolone acetate followed by 1.5 ml lignocaine) (n = 44) |
| Outcomes | (I) was slightly better in relieving pain than (I2). This difference reached statistical significance only at 1 month (P < 0.005) but not immediately after treatment, at 2 weeks, or at 3 months. 1 month post-treatment, 65.9% (n = 29) of (I2) reported no change in pain severity compared to 42.9% (n = 18) in (I) |
| Notes | 5 subjects in each group had previous lumbar spine surgery No serious complications were reported. Transient symptoms, such as headache, paraesthesia of one leg, nausea and worsening of pain occurred 15 times in (I) and 18 times in (I2) Methodological quality: randomization +; treatment allocation +; baseline similarity +; patients blinded +; care providers blinded ?; outcomes blinded +; co-interventions −; compliance +; drop outs +; timing of outcomes +; intention-to-treat −. Total score = 8 |
| Study: Mauro 2000 | |
| Methods | RCT; randomization procedure not described |
| Participants | 60 patients, aged 18–65 years, with chronic LBP or sciatic neuritis of mechanical origin for at least 6 months, and a pain intensity of at least 60 mm on a VAS. Exclusion criteria included pregnancy, severe concurrent illnesses, and intolerance to paracetamol |
| Interventions | Injection treatment (I): intramuscular injection (2 ml ampoules containing 1,000 mg vitamin B12) once daily for a 2-week period (n = 30) Reference treatment (R): sham intramuscular injection (2 ml placebo ampoules) once daily for a 2-week period (n = 30) |
| Outcomes | At the end of the treatment period, pain VAS scores (mean ± SD) significantly decreased in (I) (75.53 ± 8.9 to 9.53 ± 16.5) compared with (R) (70.63 ± 7.9 to 36.83 ± 27.4) (P < 0.0001). Total scores on RDQ (mean ± SD) significantly declined more in (I) (from 13.27 ± 2.7 to 2.43 ± 2.6) than in (R) (from 11.53 ± 2.2 to 5.80 ± 3.3) (P < 0.0002). Mean consumption of paracetamol over the treatment period was higher in (R) compared to (I) (P < 0.01) |
| Notes | No changes in vital signs or adverse effects were noted Methodological quality: randomization ?; treatment allocation ?; baseline similarity −; patients blinded ?; care providers blinded ?; outcomes blinded +; co-interventions ?; compliance +; drop outs −; timing of outcomes +; intention-to-treat −. Total score = 3 |
| Study: Mayer 2004 | |
| Methods | RCT; assignment based on date of the month of their initial visit |
| Participants | 70 patients with chronic disabling work-related lumbar spine disorders who had lumbar rigidity between 1 and 3 levels. Exclusion criteria included failure to achieve insurance pre-authorization and more than three levels of spinal rigidity |
| Interventions | Injection treatment (I): lumbar facet joint injection on one to three levels bilaterally (1 ml 2% lidocaine, 1 ml 0.5% bupivacaine, and 1 ml of a depot corticosteroid preparation). In addition, a home stretching exercise program was instructed (n = 36) Reference treatment (R): home stretching exercise program (n = 34) |
| Outcomes | No significant differences were found in pain and disability between the groups. The (I) group had a significantly greater improvement in range of motion at 5–7 weeks compared withh (R). Pain intensity (mean ± SD) improved from 6.3 ± 1.5 to 5.4 ± 1.6 in (I) and 6.7 ± 1.8 to 5.9 ± 2.1 in (R) |
| Notes | 18 patients had a history of lumbar spinal surgery Adverse events were not reported by the study authors Methodological quality: randomization −; treatment allocation −; baseline similarity +; patients blinded −; care providers blinded −; outcomes blinded +; co-interventions ?; compliance ?; drop outs +; timing of outcomes ?; intention-to-treat ?. Total score = 3 |
| Study: Nath 2008 | |
| Methods | RCT; “computer generated randomization schedule” |
| Participants | 40 patients with chronic LBP of at least 2 years duration with 80% pain relief from two successive medial branch blocks. Excluded were patients with pregnancy, coagulopathies, malignancy, infections, mental handicap and psychiatric disorders; patients with a motor deficit or any other indication for surgical treatment |
| Interventions | Injection treatment (I): radiofrequency denervation of lumbar facet joint for 60 s at 85°C (n = 20) Reference treatment (R): sham radiofrequency denervation of lumbar facet joint, same procedure as (I) but without application of current (n = 20) |
| Outcomes | At baseline, (I) had significantly more generalised pain, low-back pain, hip ROM, and referred pain when compared with (R). 6 months post-treatment, on a 6-point global assessment scale, the (I) group had significantly more than the (R) group by 0.8 points (P < 0.004). Mean low-back pain VAS improved from 6.03 to 4.10 in (I) and from 4.35 to 3.98 in (R) (P = 0.02). In various secondary outcome measures, the (I) group exhibited improvements that were statistically and clinically greater than those in the (R) group |
| Notes | Adverse events were not reported Methodological quality: randomization +; treatment allocation ?; baseline similarity −; patients blinded +; care providers blinded +; outcomes blinded +; co-interventions ?; compliance ?; drop outs +; timing of outcomes +; intention-to-treat ?. Total score = 6 |
| Study: Oh 2004 | |
| Methods | RCT; “randomly allocated” |
| Participants | 49 patients with chronic discogenic LBP whose pain continued after undergoing intradiscal electrothermal annuloplasty (IDET) and who also had a positive diagnostic block of the ramus communicans nerve. Exclusion criteria were: spinal stenosis, spinal instability, multilevel (2 or more) disc lesions, previous spinal surgery, history of excessive bleeding or coagulopathy and obvious psychologic problems. Patients with a positive diagnostic block of the facet joints were also excluded |
| Interventions | Injection treatment (I): radiofrequency thermocoagulation of the ramus communicans nerve (1% lidocaine was injected followed by RF thermocoagulation) at 65°C for 60 s (n = 26) Reference treatment (R): sham radiofrequency thermocoagulation, same procedure as (I), injection of 2 ml of preservative-free 1% lidocaine without RF thermocoagulation (n = 23) |
| Outcomes | After 4 months, VAS pain scores were significantly lower in the (I) group than in the (R) group (P < 0.05). The scores of the (I) group were a mean of 11.3 points higher (P < 0.05) on the bodily pain subscale, and a mean of 12.4 points higher (P < 0.05) on the SF-36 physical function subscale, compared with the (R) group |
| Notes | One patient in the (I) group complained of mild lower limb dysesthesia and weakness Methodological quality: randomization ?; treatment allocation −; baseline similarity +; patients blinded ?; care providers blinded −; outcomes blinded ?; co-interventions ?; compliance +; drop outs ?; timing of outcomes +; intention-to-treat ?. Total score = 3 |
| Study: Pauza 2001 | |
| Methods | RCT; “computer-generated, random numbers” |
| Participants | 64 patients aged 18–65 years with chronic LBP greater than leg pain and a posterior tear of the annulus fibrosus on provocation discography. Exclusion criteria were previous lumbar spine surgery; abnormal neurological examination; radicular pain; structural deformities; large or sequestered disc herniations; cervical or thoracic pain; uncontrolled or acute medical illnesses; rheumatoid arthritis; ambulatory dysfunction; pregnancy; workman’s compensation; injury litigation; disability remuneration; and allergy to contrast media or drugs to be used in the intended procedure Eight patients violated the protocol and were excluded from the final analysis |
| Interventions | Injection treatment (I): intradiscal electrothermal therapy (IDET) to 90°C and a 12-week post-operative rehabilitation program (lumbar corset for 6 weeks, spine stabilization exercises for 6 weeks) (n = 32) Reference treatment (R): sham intradiscal electrothermal therapy, same procedure as above without application of current, and a 12-week post-operative rehabilitation program (n = 24) |
| Outcomes | 6 months post-treatment, pain VAS scores (mean ± SD) in the (I) group decreased significantly more (6.6 ± 1.4 to 4.2 ± 2.6) than the (R) group (6.5 ± 1.9 to 5.4 ± 2.7) (P < 0.05). Oswestry disability scores (mean ± SD) decreased from 31 ± 10 to 20 ± 12 in (I) and from 33 ± 11 to 28 ± 15 in (R) (P = 0.05) |
| Notes | No patient had any adverse effects attributable to their treatment Methodological quality: randomization +; treatment allocation +; baseline similarity +; patients blinded +; care providers blinded −; outcomes blinded +; co-interventions +; compliance +; drop outs +; timing of outcomes +; intention-to-treat −. Total score = 9 |
| Study: Revel 1998 | |
| Methods | RCT; randomisation method not stated |
| Participants | 80 patients aged 18 years or more with chronic LBP unrelieved by analgesics, NSAIDs, and physical therapy. Exclusion criteria included previous back surgery, sciatica, sacroiliac joint pain, pregnancy, psychiatric disease and a history of adverse reaction to a lidocaine or corticosteroid injection |
| Interventions | Injection treatment (I): lumbar facet joint injection with anaesthetic (1 ml 2% lidocaine) (n = 42) Reference treatment (R): lumbar facet joint injection with 1 ml saline (n = 38) Patients had 4–6 lower joints injected on both sides or 2–3 on the same side |
| Outcomes | Post-treatment, pain relief was significantly better in the (I) group compared with the (R) group. In patients with fewer pain characteristics, pain (mean ± SD) decreased by −35.36 ± 23.6 in (I) compared to −11.87 ± 17.44 in (R) (P = 0.01) |
| Notes | Adverse events were not reported Methodological quality: randomization ?; treatment allocation ?; baseline similarity +; patients blinded +; care providers blinded +; outcomes blinded +; co-interventions ?; compliance ?; drop outs +; timing of outcomes +; intention-to-treat +. Total score = 7 |
| Study: Serrao 1992 | |
| Methods | RCT; “randomly allocated” |
| Participants | 28 patients attending chronic LBP treatment. Patients with disc lesions and spinal claudication were excluded |
| Interventions | Injection treatment (I): lumbar epidural injection with corticosteroid (80 mg prednisolone) plus 3 ml 5% dextrose injected into the intrathecal space (n = 14) Injection treatment (I2): lumbar epidural injection (10 ml normal saline) plus 2 mg midazolam dissolved in 3 ml 5% dextrose injected into the intrathecal space (n = 14) |
| Outcomes | There were no significant differences between the groups post-treatment, or after 2 months follow-up for either pain intensity or unpleasantness. No significant differences were found between groups on psychological measures. Data in graphs |
| Notes | Eight patients in the (I) group and seven in the (I2) group experienced headaches following treatment; nausea was experienced in two of the (I) patients and by one patient in the (R) group Methodological quality: randomization ?; treatment allocation ?; baseline similarity ?; patients blinded +; care providers blinded ?; outcomes blinded +; co-interventions −; compliance +; drop outs ?; timing of outcomes +; intention-to-treat ?. Total score = 4 |
| Study: Tekin 2007 | |
| Methods | RCT; “random number generation” |
| Participants | 60 patients, aged >17 years, with chronic LBP with or without radiating pain into the upper leg, focal tenderness over the facet joints and pain on hyperextension. Exclusion criteria were prior radiofrequency treatment, coagulation disturbances, allergies to contrast media or local anaesthetics, malignancy, psychiatric conditions and pregnancy. Only patients with a positive response (>50% pain relief for sufficient duration) to a diagnostic medial branch block were included |
| Interventions | Injection treatment (I): radiofrequency denervation (conventional) medial branch lumbar nerve roots at 80°C for 90 s (n = 20) Injection treatment (I2): radiofrequency denervation (pulsed) medial branch lumbar nerve roots at 42°C for 240 s (n = 20) Reference treatment (R): sham radiofrequency denervation, similar procedure as (I), but only bupivacaine 0.5% 0.3 ml was injected (n = 20) |
| Outcomes | Post-treatment VAS and ODI scores (mean ± SD) were lower in (I) (2.3 ± 1.4; 25.6 ± 6.5) and (I2) (2.8 ± 1.5; 24.4 ± 5.7) than in (R) (4.3 ± 1.0; 30.5 ± 5.7) (P < 0.001). At 6 months and 1 year follow-up, mean VAS score was similar in (R) and (I2) groups but lower in the (I) group compared with the others (P < 0.05). Mean ODI was lower in (I) and (I2) groups than (R) group at 1 year (P < 0.05) Patient satisfaction was lower in (R) than other groups (P = 0.03), and highest in (I) (P = 0.004) |
| Notes | There were no complications related to the procedure during the follow-up period Methodological quality: randomization +; treatment allocation ?; baseline similarity +; patients blinded +; care providers blinded −; outcomes blinded ?; co-interventions +; compliance +; drop outs +; timing of outcomes +; intention-to-treat ?. Total score = 7 |
| Study: van Alphen 1989 | |
| Methods | RCT; randomization method not stated |
| Participants | 151 patients, aged 18–45 years, with proven disc herniation on myelography. 68 patients had symptoms for >6 months. Exclusion criteria were severe neurological deficits, previous lumbar disc surgery or chemonucleolysis, and pregnancy |
| Interventions | Injection treatment (I): chemonucleolysis [2 ml (4,000 U) chymopapain injected into intervertebral disc] followed by physiotherapy (n = 34) Reference treatment (R): discectomy under general anaesthetic using an interlaminar approach followed by post-operative physiotherapy (n = 34) |
| Outcomes | 12 months post-treatment, status of pain (disappeared, improved, unchanged, increased) = (I): n = 13, 14, 4, 0; (R): n = 16, 13, 5, 0 (not significant) |
| Notes | Complications in both groups included increased neurological symptoms, dural defect with leakage of cerebrospinal fluid, and partial cauda equina in one patient Methodological quality: randomization +; treatment allocation −; baseline similarity ?; patients blinded −; care providers blinded −; outcomes blinded −; co-interventions ?; compliance −; drop outs −; timing of outcomes +; intention-to-treat −. Total score = 2 |
| Study: van Kleef 1999 | |
| Methods | RCT; “[randomized] with help of a computer program” |
| Participants | 31 patients, aged 20–60 years, with chronic LBP for >12 months and a positive diagnostic dorsal ramus nerve block. Patients with previous back surgery or known specific LBP were excluded. One patient refused follow-up and was excluded from the analysis |
| Interventions | Injection treatment (I): radiofrequency denervation of lumbar facet joints (posterior primary ramus of the segmental nerves L3–L5) at 80°C for 60 s on one or both sides (n = 15) Reference treatment (R): sham radiofrequency denervation, electrodes introduced as in (I) but no radiofrequency current was applied (n = 16) |
| Outcomes | After 8 weeks, the mean VAS ± SD for (R) and (I) was 4.8 ± 2.5 and 2.8 ± 2.4, respectively. This difference, and the difference in effect on the Oswestry disability scale and globally perceived effect were statistically significant. Three, 6, and 12 months after treatment there were significantly more “success” patients in the (I) group compared with (R) |
| Notes | There were no complications during or after the interventions Methodological quality: randomization +; treatment allocation ?; baseline similarity +; patients blinded +; care providers blinded +; outcomes blinded +; co-interventions ?; compliance +; drop outs ?; timing of outcomes +; intention-to-treat ?. Total score = 7 |
| Study: van Wijk 2005 | |
| Methods | RCT; randomisation method not stated |
| Participants | 81 patients, aged 17 years and over, with chronic LBP and a 50% pain VAS reduction on lumbar facet joint diagnostic block. Exclusion criteria were prior radiofrequency treatment, radicular syndrome, coagulopathies, specific allergies, cancer and pregnancy |
| Interventions | Injection treatment (I): radiofrequency lumbar facet denervation (dorsal ramus medial branches) at 80°C for 60 s (n = 40) Reference treatment (R): sham radiofrequency denervation, same procedure as (I) but without applying radiofrequency current (n = 41) |
| Outcomes | 3 months post-treatment, a combined outcome measure (VAS, physical activities, analgesic intake) showed no differences between (I) (success 27.5%) and (R) (success 29.3%) (P = 0.86). Globally perceived effect improved after (I) (P < 0.05). The other secondary outcome parameters showed no significant differences. Data in graphs |
| Notes | 30% of patients reported treatment-related pain severe enough to necessitate analgesics. No differences were found between groups on the incidence of adverse events and complications Methodological quality: randomization +; treatment allocation +; baseline similarity +; patients blinded +; care providers blinded +; outcomes blinded +; co-interventions ?; compliance +; drop outs +; timing of outcomes +; intention-to-treat +. Total score = 10 |
Appendix 2
See Table 4.
Table 4.
Characteristics of excluded studies
| Review | Study | Reason for exclusion |
|---|---|---|
| Staal 2008 | Aldrete 2003 | Duration of LBP not reported |
| Beliveau 1971 | Duration of LBP not reported | |
| Breivik 1976 | Duration of LBP not reported | |
| Collee 1991 | Duration of LBP not reported | |
| Garvey 1989 | Included patients with duration <3 months | |
| Rocco 1989 | All patients had previous laminectomy | |
| Sonne 1985 | Included patients with duration <3 months | |
| Takada 2005 | Included patients with duration <3 months | |
| Gibson 2007a | Schwetschenau 1976 | Included patients with duration <3 months |
| Fraser 1982 | Included patients with duration <3 months | |
| Javid 1983 | Included patients with duration <3 months | |
| Feldman 1986 | Duration of LBP not reported | |
| Dabezies 1988 | Duration of LBP not reported | |
| Ejeskar 1983 | Duration of LBP not reported | |
| Crawshaw 1984 | Duration of LBP not reported | |
| Lavignolle 1987 | Duration of LBP not reported | |
| Muralikuttan 1992 | Included patients with duration <3 months | |
| Benoist 1993 | Duration of LBP not reported | |
| Hedtmann 1992 | Duration of LBP not reported | |
| Bourgeois 1988 | Included patients with duration <3 months | |
| Bontoux 1990 | Included patients with duration <3 months | |
| Bromley 1984 | Included patients with duration <3 months | |
| Yu 1996 | Article in Chinese/Mandarin | |
| Steffen 1996 | Included patients with duration <3 months | |
| Revel 1993 | Included patients with duration <3 months | |
| Abdi 2007 | Wilson-McDonald 2005 | Duration of LBP not reported |
| Arden 2005 | Included patients with duration <3 months | |
| Carette 1997 | Included patients with duration <3 months | |
| McGregor 2001 | Duration of LBP not reported | |
| Pirbudak 2003 | No comparisons with injection therapy | |
| Snoek 1977 | Included patients with duration <3 months | |
| Cuckler 1985 | Duration of LBP not reported | |
| Dilke 1973 | Included patients with duration <3 months | |
| Ridley 1988 | Duration of LBP not reported | |
| Rogers 1992 | Duration of LBP not reported | |
| Kraemer 1997 | Duration of LBP not reported | |
| Riew 2006 | Duration of LBP not reported | |
| Ng 2005 | Duration of LBP not reported | |
| Karppinen 2001 | Included patients with duration <3 months | |
| Vad 2002 | Included patients with duration <3 months | |
| Devulder 1999 | Duration of LBP not reported | |
| Thomas 2003 | Included patients with duration <3 months | |
| Bush 1991 | Included patients with duration <3 months | |
| Matthews 1987 | Included patients with duration <3 months | |
| Helsa 1979 | Article in Norwegian | |
| Meadeb 2001 | Included patients with duration <3 months | |
| Chou 2009 | Hameroff 1981 | Duration of LBP not reported |
| Dechow 1999 | Outside the scope of this review (prolotherapy) | |
| Klein 1993 | Outside the scope of this review (prolotherapy) | |
| Ongley 1987 | Outside the scope of this review (prolotherapy) | |
| Yelland 2004 | Outside the scope of this review (prolotherapy) | |
| Ackerman 2007 | Included patients with duration <3 months | |
| Bonetti 2005 | Included patients with duration <3 months | |
| Fukusaki 1998 | Included patients with duration <3 months | |
| Gallucci 2007 | Included patients with duration <3 months | |
| Jeong 2007 | Included patients with duration <3 months | |
| Manchikanti 2004 | No injection therapy comparison | |
| Helliwell 1985 | Included patients with duration <3 months | |
| Klenerman 1984 | All patients had acute sciatica (<6 weeks duration) | |
| Zahaar 1991 | Included patients with duration <3 months | |
| Buchner 2000 | Included patients with duration <3 months | |
| Butterman 2004 | Included patients with duration <3 months | |
| Kolsi 2000 | Included patients with duration <3 months | |
| Pirbudak 2003b | Included patients with duration <3 months | |
| Nash 1989 | Duration of LBP not reported | |
| Luukkainen 2002 | Duration of LBP not reported | |
| Buttermann 2004 | Patients randomized to surgery, not injection therapy | |
| Graham 1975 | Included patients with duration <3 months | |
| Khot 2004 | Duration of LBP not reported | |
| Simmons 1992 | Duration of LBP not reported | |
| Graham 1976 | Included patients with duration <3 months | |
| Hoogland 2006 | All subjects underwent endoscopic discectomy | |
| Wittenberg 2001 | Duration of LBP not reported | |
| Burton 2000 | Duration of LBP not reported | |
| Krugluger 2000 | Duration of LBP not reported | |
| Steffen 1997 | Included patients with duration <3 months | |
| Sanders 1999 | No injection therapy comparison | |
| Kumar 2007 | All patients had failed back surgery | |
| North 2005 | All patients had failed back surgery |
Appendix 3
See Table 5.
Table 5.
Forest plots and GRADE evidence profiles
References
- 1.Manchikanti L, Singh V, Datta S, Cohen SP, Hirsch JA. Comprehensive review of epidemiology, scope, and impact of spinal pain. Pain Physician. 2009;12(4):E35–E70. [PubMed] [Google Scholar]
- 2.Martin BI, Deyo RA, Mirza SK, Turner JA, Comstock BA, Hollingworth W, Sullivan SD. Expenditures and health status among adults with back and neck problems. JAMA. 2008;299(6):656–664. doi: 10.1001/jama.299.6.656. [DOI] [PubMed] [Google Scholar]
- 3.Staal JB, de Bie R, de Vet HCW, Hildebrandt J, Nelemans P (2008) Injection therapy for subacute and chronic low-back pain. Cochrane Database Syst Rev (3):Art. No.: CD001824. doi:10.1002/14651858.CD001824.pub3 [DOI] [PMC free article] [PubMed]
- 4.Abdi S, Datta S, Trescot AM, et al. Epidural steroids in the management of chronic spinal pain: a systematic review. Pain Physician. 2007;10:185–212. [PubMed] [Google Scholar]
- 5.Gibson JNA, Waddell G (2007) Surgical interventions for lumbar disc prolapse. Cochrane Database Syst Rev (2):Art. No.: CD001350. doi:10.1002/14651858.CD001350.pub4 [DOI] [PMC free article] [PubMed]
- 6.Chou R, Atlas SJ, Stanos SP, Rosenquist RW. Nonsurgical interventional therapies for low back pain: a review of the evidence for an American Pain Society clinical practice guideline. Spine. 2009;34(10):1078–1093. doi: 10.1097/BRS.0b013e3181a103b1. [DOI] [PubMed] [Google Scholar]
- 7.Furlan AD, Pennick V, Bombardier C, van Tulder M. Updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine. 2009;34(18):1929–1941. doi: 10.1097/BRS.0b013e3181b1c99f. [DOI] [PubMed] [Google Scholar]
- 8.van Tulder M, Suttorp M, Morton S, Bouter L, Shekelle P. Empirical evidence of an association between internal validity and effect size in randomized controlled trials of low-back pain. Spine. 2009;34(16):1685–1692. doi: 10.1097/BRS.0b013e3181ab6a78. [DOI] [PubMed] [Google Scholar]
- 9.Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328:1490. doi: 10.1136/bmj.328.7454.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guyatt GH, Oxman AD, Vist G, et al. Rating quality of evidence and strength of recommendations GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van Alphen HA, Braakman R, Bezemer PD, et al. Chemonucleolysis or discectomy: a randomized multicenter trial. J Neurosurg. 1989;70:869–875. doi: 10.3171/jns.1989.70.6.0869. [DOI] [PubMed] [Google Scholar]
- 12.Carette S, Marcoux S, Truchon R, Grondin C, Gagnon J, Allard Y, et al. A controlled trial of corticosteroid injections into facet joints for chronic low back pain. N Eng J Med. 1991;325(14):1002–1007. doi: 10.1056/NEJM199110033251405. [DOI] [PubMed] [Google Scholar]
- 13.Lilius G, Laasonen EM, Myllynen P, Harilainen A, Gronlund G. Lumbar facet joint syndrome. A randomised clinical trial. J Bone Joint Surg. 1989;71:681–684. doi: 10.1302/0301-620X.71B4.2527856. [DOI] [PubMed] [Google Scholar]
- 14.Revel M, Poiraudeau S, Auleley GR, Payan C, Nguyen M, Chevrot A, et al. Capacity of the clinical picture to characterize low back pain relieved by facet joint anesthesia. Proposed criteria to identify patients with painful facet joints. Spine. 1998;23(18):1972–1976. doi: 10.1097/00007632-199809150-00011. [DOI] [PubMed] [Google Scholar]
- 15.Mayer TG, Gatchel RJ, Keeley J, McGeary D, Dersh J, Anagnostis C. A randomized clinical trial of treatment for lumbar segmental rigidity. Spine. 2004;29(20):2199–2205. doi: 10.1097/01.brs.0000142009.73869.8d. [DOI] [PubMed] [Google Scholar]
- 16.Fuchs S, Erbe T, Fischer HL, Tibesku CO. Intraarticular hyaluronic acid versus glucocorticoid injections for nonradicular pain in the lumbar spine. J Vasc Interv Radiol. 2005;16(11):1493–1498. doi: 10.1097/01.RVI.0000175334.60638.3F. [DOI] [PubMed] [Google Scholar]
- 17.Manchikanti L, Pampati V, Bakhit C, Rivera JJ, Beyer CD, Damron KS, et al. Effectiveness of lumbar facet joint nerve blocks in chronic low back pain: a randomized clinical trial. Pain Physician. 2001;4(1):101–107. [PubMed] [Google Scholar]
- 18.Manchikanti L, Singh V, Falco FJE, Cash KA, Pampati V. Lumbar facet joint nerve blocks in managing chronic facet joint pain: one-year follow-up of a randomized, double-blind controlled trial: clinical trial NCT00355914. Pain Physician. 2008;11:121–132. [PubMed] [Google Scholar]
- 19.Marks RC, Houston T, Thulbourne T. Facet joint injection and facet nerve block: a randomised comparison in 86 patients with chronic low back pain. Pain. 1992;49(3):325–328. doi: 10.1016/0304-3959(92)90239-8. [DOI] [PubMed] [Google Scholar]
- 20.Dashfield AK, Taylor MB, Cleaver JS, et al. Comparison of caudal steroid epidural with targeted steroid placement during spinal endoscopy for chronic sciatica: a prospective, randomized, double-blind trial. Br J Anaesth. 2005;94:514–519. doi: 10.1093/bja/aei084. [DOI] [PubMed] [Google Scholar]
- 21.Serrao JM, Marks RL, Morley SJ, Goodchild CS. Intrathecal midazolam for the treatment of chronic mechanical low back pain: a controlled comparison with epidural steroid in a pilot study. Pain. 1992;48(1):5–12. doi: 10.1016/0304-3959(92)90125-U. [DOI] [PubMed] [Google Scholar]
- 22.Lierz P, Gustorff B, Markow G, Felleiter P. Comparison between bupivacaine 0.125% and ropivacaine 0.2% for epidural administration to outpatients with chronic low back pain. Eur J Anaesthesiol. 2004;21(1):32–37. doi: 10.1017/s0265021504001061. [DOI] [PubMed] [Google Scholar]
- 23.Mauro GL, Martorana U, Cataldo P, Brancato G, Letizia G. Vitamin B12 in low back pain: a randomised, double-blind placebo-controlled study. Eur Rev Med Pharmacol Sci. 2000;4(3):53–58. [PubMed] [Google Scholar]
- 24.Foster L, Clapp L, Erickson M, et al. Botulinum toxin A and chronic low back pain: a randomized, double-blind study. Neurology. 2001;56:1290–1293. doi: 10.1212/wnl.56.10.1290. [DOI] [PubMed] [Google Scholar]
- 25.Barendse GA, van Den Berg SG, Kessels AH, et al. Randomized controlled trial of percutaneous intradiscal radiofrequency thermocoagulation for chronic discogenic back pain. Spine. 2001;26:287–292. doi: 10.1097/00007632-200102010-00014. [DOI] [PubMed] [Google Scholar]
- 26.Ercelen O, Bulutcu E, Oktenoglu T, et al. Radiofrequency lesioning using two different time modalities for the treatment of lumbar discogenic pain: a randomized trial. Spine. 2003;28:1922–1927. doi: 10.1097/01.BRS.0000083326.39944.73. [DOI] [PubMed] [Google Scholar]
- 27.Freeman BJ, Fraser RD, Cain CM, et al. A randomized, double-blind, controlled trial: intradiscal electrothermal therapy versus placebo for the treatment of chronic discogenic low back pain. Spine. 2005;30:2369–2377. doi: 10.1097/01.brs.0000186587.43373.f2. [DOI] [PubMed] [Google Scholar]
- 28.Kvarstein G, Måwe L, Indahl A, Hol PC, Tennøe B, Digernes R, Stubhaug A, Tønnessen TI, Beivik H. A randomized double-blind controlled trial of intra-annular radiofrequency thermal disc therapy—a 12-month follow-up. Pain. 2009;145:279–286. doi: 10.1016/j.pain.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 29.Pauza KJ, Howell S, Dreyfuss P, et al. A randomized, placebo-controlled trial of intradiscal electrothermal therapy for the treatment of discogenic low back pain. Spine J. 2004;4:27–35. doi: 10.1016/j.spinee.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 30.Oh WS, Shim JC. A randomized controlled trial of radiofrequency denervation of the ramus communicans nerve for chronic discogenic low back pain. Clin J Pain. 2004;20(1):55–60. doi: 10.1097/00002508-200401000-00011. [DOI] [PubMed] [Google Scholar]
- 31.Gallagher J, Petriccione D, Wedley J, et al. Radiofrequency facet joint denervation in the treatment of low back pain: a prospective controlled double-blind study to assess its efficacy. Pain Clin. 1994;7:193–198. [Google Scholar]
- 32.Leclaire R, Fortin L, Lambert R, et al. Radiofrequency facet joint denervation in the treatment of low back pain: a placebo-controlled clinical trial to assess efficacy. Spine. 2001;26:1411–1416. doi: 10.1097/00007632-200107010-00003. [DOI] [PubMed] [Google Scholar]
- 33.Nath S, Nath C, Pettersson K. Percutaneous lumbar zygapophysial (facet) joint neurotomy using radiofrequency current, in the management of chronic low back pain. Spine. 2008;33:1291–1297. doi: 10.1097/BRS.0b013e31817329f0. [DOI] [PubMed] [Google Scholar]
- 34.Tekin I, Mirzai H, OK G, et al. A comparison of conventional and pulsed radiofrequency denervation in the treatment of chronic facet joint pain. Clin J Pain. 2007;23:524–529. doi: 10.1097/AJP.0b013e318074c99c. [DOI] [PubMed] [Google Scholar]
- 35.van Kleef M, Barendse G, Kessels A, et al. Randomized trial of radiofrequency lumbar facet denervation for chronic low back pain. Spine. 1999;24:1937–1942. doi: 10.1097/00007632-199909150-00013. [DOI] [PubMed] [Google Scholar]
- 36.van Wijk R, Geurts J, Wynne H, et al. Radiofrequency denervation of lumbar facet joints in the treatment of chronic low back pain: a randomized, double-blind, sham lesion-controlled trial. Clin J Pain. 2005;21:335–344. doi: 10.1097/01.ajp.0000120792.69705.c9. [DOI] [PubMed] [Google Scholar]
- 37.Geurts J, van Wijk RM, Wynne HJ, et al. Radiofrequency lesioning of dorsal root ganglia for chronic lumbosacral radicular pain: a randomised, double-blind, controlled trial. Lancet. 2003;361:21–26. doi: 10.1016/S0140-6736(03)12115-0. [DOI] [PubMed] [Google Scholar]
- 38.Egger M, Smith GD. Meta-analysis bias in location and selection of studies. BMJ. 1998;316:61–66. doi: 10.1136/bmj.316.7124.61. [DOI] [PMC free article] [PubMed] [Google Scholar]