Vitamin A: biomarkers of nutrition for development1 (original) (raw)
Abstract
Vitamin A is essential for multiple functions in mammals. Without vitamin A, mammals cannot grow, reproduce, or fight off disease. Because of its numerous functions in humans, biomarkers of vitamin A status are quite diverse. Assessment of liver reserves of vitamin A is considered the gold standard because the liver is the major storage organ. However, this measure is not feasible in human studies. Alternative biomarkers of status can be classified as biological, functional, histologic, and biochemical. Historically, signs of xerophthalmia were used to determine vitamin A deficiency. Before overt clinical damage to the eye, individuals who suffer from vitamin A deficiency are plagued by night blindness and longer vision-restoration times. These types of assessments require large population-based evaluations. Therefore, surrogate biochemical measures of vitamin A status, as defined by liver reserves, have been developed. Serum retinol concentrations are a common method used to evaluate vitamin A deficiency. Serum retinol concentrations are homeostatically controlled until liver reserves are dangerously low. Therefore, other biochemical methods that respond to liver reserves in the marginal category were developed. These included dose-response tests and isotope dilution assays. Dose-response tests work on the principle that apo-retinol–binding protein builds up in the liver as liver reserves become depleted. A challenge dose of vitamin A binds to this protein, and serum concentrations increase within a few hours if liver vitamin A concentrations are low. Isotope dilution assays use stable isotopes as tracers of total body reserves of vitamin A and evaluate a wide range of liver reserves. Resources available and study objectives often dictate the choice of a biomarker.
INTRODUCTION
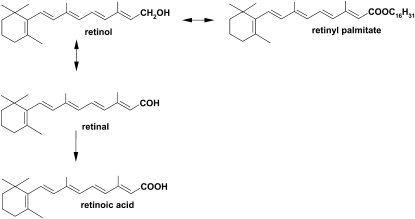
The most common forms of preformed vitamin A in the human diet are retinol and retinyl esters. Retinol has 20 carbons, and the functional group is located on carbon 15 (Figure 1). Vitamin A has many functions in the human body, including growth, vision, epithelial differentiation, immune function, and reproduction (1). The storage form is retinol esterified to fatty acids predominantly as retinyl palmitate. Retinal is the form involved in vision, whereas retinoic acid is involved in growth and cellular functions. The enzymatic formation of retinal and retinyl esters from retinol is reversible; however, the oxidation of retinal to retinoic acid is not reversible (Figure 1).
FIGURE 1.
Chemical structures of important functional forms of vitamin A. Retinol and retinyl esters (palmitate shown) are the dietary forms of preformed vitamin A. Retinal is essential in vision, and retinoic acid is involved in growth and cellular differentiation.
Unfortunately, many women and children suffer from vitamin A deficiency, which leads to vision loss, increased morbidity, and mortality. According to the World Health Organization (2), 45 countries have a public health problem at the clinical level, which includes overt signs of deficiency, and 122 countries have subclinical levels of vitamin A depletion with marginal liver reserves. Although progress has been made globally to alleviate overt clinical signs of vitamin A deficiency, marginal vitamin A status is still prevalent and difficult to diagnose.
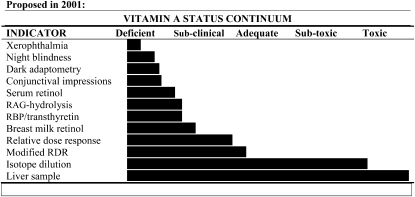
Because of concerns related to marginal vitamin A status, multiple indicators have been developed to diagnose different degrees of vitamin A status. In 2001, these indicators were reviewed (3) and ranked against a continuum of liver reserves (Figure 2). Vitamin A biomarkers can be grouped into 2 broad categories as follows: 1) biological, functional, and histologic indicators and 2) qualitative and quantitative biochemical indicators. This brief review will cover both of these categories and relate indicators to predicted liver stores of vitamin A.
FIGURE 2.
Biomarkers of vitamin A status relative to qualitative liver reserves of vitamin A. These relations were proposed as part of the James Allen Memorial symposium in 2001 (adapted from reference 3). RAG, retinoyl β-glucuronide; RBP, retinol-binding protein; RDR, relative dose response.
BIOLOGICAL, FUNCTIONAL, AND HISTOLOGIC INDICATORS
Biological: clinical signs of deficiency
The first group of biological indicators is clinical and involves the eye. If an individual presents with visual or ocular histologic indicators, they should be considered severely vitamin A deficient and treated with high-dose supplements. Xerophthalmia has different degrees of severity from Bitot's spots, which are reversible with vitamin A treatment, to irreversible blindness because of scarring of the cornea. Xerophthalmia is a population indicator, and a minimum prevalence of 0.5% in preschool children signifies a public health problem (4).
Functional
Night blindness results when the vitamin A pool in the eye becomes depleted, and the concentration in the rod cells is lowered. Many countries have a specific term in local languages for this symptom of deficiency. Night blindness that is due to vitamin A deficiency is reversible with increased vitamin A intake or supplementation. In countries where marginal vitamin A status is prevalent, night blindness may occur during pregnancy. Whether this is due to increased demands during pregnancy or lowered serum retinol concentrations because of plasma volume increases is not entirely known.
Although night blindness is typically used as a population indicator of vitamin A status, impaired dark adaptation has been used to evaluate intervention studies (5, 6). Specifically, dark adaptation measured by the pupillary threshold in Nepali women with night blindness improved when liver, fortified rice, amaranth leaves, carrots, or retinyl palmitate were consumed for 6 wk (5). Such improvement may be further enhanced with iron and riboflavin supplementation (6). The vision restoration time or adaptation under dark conditions has also been used to evaluate vitamin A depletion in groups. Zinc supplementation sometimes synergistically improves the vision restoration time (7).
Histologic
Conjunctival impression cytology evaluates the morphology of the surface of the eye. During vitamin A deficiency, the presence of mucin-containing goblet cells decreases, and epithelial cells become enlarged and distorted. Cells can be counted and evaluated by taking a filter paper sample from the surface of the eye and staining with hematoxlyin and eosinophil. Conjunctival impression cytology was used in the 1990s (7, 8), but because of concerns of its lack of utility in groups with trachoma (9) or subclinical deficiency in young children (10), the method has not been widely adopted.
QUALITATIVE BIOCHEMICAL INDICATORS
Serum retinol concentrations
Serum retinol concentrations are the most common population indicator used. In addition to analysis with HPLC, surrogate analyses for the carrier protein retinol-binding protein (RBP) have been developed by using either serum (11) or blood spots (12). The ratio of retinol to RBP may be influenced by vitamin A deficiency (13) or obesity (14), which may negatively affect prevalence rates of vitamin A deficiency when expressed as RBP concentrations. Both serum retinol and RBP concentrations are static measures and do not always change in response to an intervention. For example, in a study in 309 Indonesian children (15), the initial and final serum retinol concentrations did not differ between groups that received 210 μmol vitamin A and groups that did not 3–4 wk after supplementation. In groups of children who received vitamin A, the after-to-before ratio was 0.97–1.03, and in groups that did not receive vitamin A, the ratio was 0.96–0.99 (15).
On the other hand, distribution curves of serum retinol concentrations have shown distinct differences (8). When used as an evaluation tool, the serum retinol distribution differed in children between 2 areas in Indonesia. However, in the study, the degree of infection was not assessed. Therefore, it was unknown what effect correction for inflammatory markers would have had on the distribution curves (16). Infection and inflammation have a negative effect on serum retinol concentrations because RBP is an acute phase protein.
In women, serum retinol concentrations have responded to vitamin A supplementation if values are initially low, such as in Indonesian women given low-dose supplements for 35 d (17). However, in some groups, serum retinol concentrations may not respond even to high-dose supplements, such as in Ghanaian women given 210 or 420 μmol retinyl ester (18) or fed indigenous green leafy vegetables for 3 mo (19). The lack of response for serum retinol concentrations is partly due to retinol's homeostatic control over a wide range of liver reserves. For example, in rats that were on 3 different amounts of daily vitamin A supplements, serum retinol concentrations did not differ despite a 6-fold difference in liver reserves of vitamin A (20).
Retinoyl beta-glucuronide hydrolysis test and RBP:prealbumin measurements
Two biochemical methods that have not been widely applied include the retinoyl β-glucuronide (RAG) hydrolysis test (21, 22) and RBP:prealbumin measurements (23). Both of these methods were established in the rat model (21–23) and applied to humans (22–25). The RAG hydrolysis test is a response test in which a dose of RAG is given, and the change in the retinoic acid concentration is measured in the serum. The retinoic acid response is expected to be greater in individuals with poorer vitamin A status. Doses of 25, 50, and 75 mg RAG have been piloted in Indian children aged 3–18 y old (25). Elevated retinoic acid concentrations were observed in children whose serum retinol concentrations were <0.85 μmol/L. The advantages of this test compared with serum retinol concentrations corrected for the degree of infection or inflammation will need to be further investigated. The RBP:prealbumin method is a static measure and may have utility in groups of humans with a high degree of infection or inflammation. Measurements have been done in Zambian children with measles (23), children from Papua New Guinea, and Bangladeshi surgical patients (24). In the Bangladeshi surgical patients, a cutoff ≤0.36 for RBP:prealbumin was associated with vitamin A deficiency defined as <0.07 μmol retinol/g liver (24).
Breast-milk retinol concentrations
Breast-milk retinol concentrations are a unique indicator and evaluation tool for lactating women (26) with potential extrapolation to the nursing infant. However, the response to supplementation was modest in Kenyan mothers (27). As a biomarker, breast-milk retinol concentrations may reflect recent dietary intakes and not necessarily be a reflection of vitamin A status as shown in rats (28) and swine (29). A comparison among vitamin A indicators suggested that breast-milk retinol determined from a casual sampling, compared with full breast-milk expression, may have performed better when corrected for the fat content (30).
QUANTITATIVE BIOCHEMICAL INDICATORS
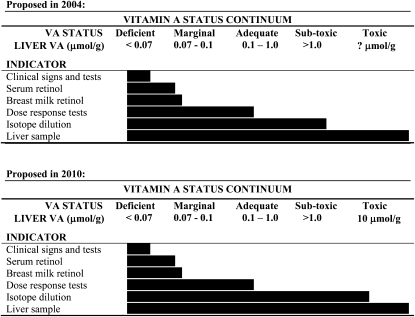
These described methods are largely qualitative. Methods that are semiquantitative and quantitative include the dose-response tests, isotope dilution assays, and direct measurement through biopsy or autopsy samples of the liver. In 2004, the Vitamin A Tracer Task Force (31) assigned liver-reserve concentration values to a variety of vitamin A biomarkers (Figure 3). The dose-response tests have utility from deficiency through the adequate range of vitamin A liver reserves. However, the tests likely do not quantitatively reflect a status above the adequate range. Isotope dilution assays yield a quantitative estimate of liver reserves, but it was unknown in 2004 how accurately liver reserves above the subtoxic level could be estimated. A liver biopsy can be used in rare circumstances but has limited utility for obvious reasons.
FIGURE 3.
Top: Recommended biomarkers of vitamin A (VA) status by the Vitamin A Tracer Task Force in 2004 (adapted from reference 31) in relation to liver-reserve concentrations (μmol VA/g liver). Bottom: Replacing the “?” in 2010 regarding the utility of isotope dilution testing in the hypervitaminotic state.
Dose-response tests
The dose-response tests work on the principle that RBP accumulates as vitamin A liver reserves become low. In rats that were fed a vitamin A–deficient diet, apo-RBP accumulated in the liver before serum retinol concentrations decreased, and the liver was depleted (32). Thus, when a challenge dose of retinyl or 3,4-didehydroretinyl ester is administered, the retinol or 3,4-didehydroretinol binds to this accumulated RBP and is rapidly released into the serum. The relative-dose-response (RDR) test was originally applied to a rat model (33). When applied in the field today, 1 mg retinyl ester is administered dissolved in oil (8). Two blood samples are collected (ie, one sample at baseline and another sample 5 h after dosing). The RDR value, which is expressed as a percentage, is calculated as
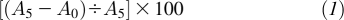
where _A_5 is the serum retinol concentration at 5 h postdosing, and _A_0 is the serum retinol concentration at baseline. If the percentage difference is >20%, the individual likely has deficient liver reserves.
Although the RDR test is a useful indicator, the test is somewhat invasive because it requires 2 blood samples from the same individual ≈5 h apart. An accurate RDR value is dependent on correct analysis and consistent retinol recovery from both serum samples. Therefore, the modified RDR (MRDR) test was developed in rats (34–36) and applied to humans in the United States (36, 37) and Indonesia (38). The test was further refined to make it more field friendly by establishing standard test doses and suggesting a range of response times to obtain the blood sample (39). The test works on the same principle as the RDR test, but because the 3,4-didehydroretinol analog is administered instead of retinol, a single blood sample can be taken. HPLC easily separates 3,4-didehydroretinol from retinol in the same sample. Endogenous concentrations of 3,4-didehydroretinol are quite low in humans ,and therefore, the baseline blood sample is not needed. A distinguishing response between depleted and sufficient liver reserves can be measured in ≥4 h and has been validated in rats and piglets against liver vitamin A reserves (34–36, 40) and compared with the RDR test in children (8). After the serum sample is analyzed, the molar ratio of 3,4-didehydroretinol to retinol is calculated, which is sometimes referred to as the MRDR value. A cutoff of 3,4-didehydroretinol to retinol ≥0.060 usually signifies low liver reserves of retinol that can be corrected with vitamin A supplements (15, 41).
The MRDR test has been applied in several countries to evaluate interventions and the prevalence of low liver reserves in surveys. One of the first comparisons was done in preschool-age children in Indonesia (8). In the first group, the distribution of values approached a normal distribution, and most children were vitamin A adequate. A child in the first group who had an MRDR value of 0.18 had just moved into the area. In the second group of children, MRDR values were quite disparate and reached a value of 0.83 in one female subject. An informal dietary interview in the community revealed that the first group of children ate a significant amount of eggs. Eggs provide a highly bioavailable source of preformed retinol and, thus, can make a measurable difference in the vitamin A status of children if consumed regularly.
The application of the MRDR test in a study of the combined treatment of vitamin A supplements and albendazole for deworming children infected with Ascaris lumbricoides showed a significant improvement in the mean (±SD) value of 0.055 ± 0.042 before supplementation to a value of 0.033 ± 0.017 after supplementation (P < 0.0001) (15). This magnitude of difference was not seen with serum retinol concentrations. In another evaluative study of children with helminthic infections, the MRDR test correctly identified children that had received a vitamin A supplement from the local health post (41). MRDR values were 0.021 ± 0.012 and 0.054 ± 0.038 in the children who had and had not received the supplement, respectively. Serum retinol concentrations did not differ between children who had received the supplement and children who had not, and the serum retinol concentrations did not respond to treatment.
The MRDR test has been used in a variety of countries to evaluate population status. It gives more information than serum retinol concentrations alone. For example, in a group of rural lactating women in Ghana, baseline serum retinol concentrations and MRDR values were 1.4 ± 0.5 μmol/L and 0.048 ± 0.037, respectively (18). After treatment with either 210 or 420 μmol retinyl ester, a significant improvement in vitamin A status occurred as assessed by the MRDR test (P < 0.0001), but serum retinol concentrations did not differ (P = 0.87). Furthermore, in an urban group of Ghanaian lactating women, the baseline serum retinol concentration was 1.5 ± 0.6 μmol/L, and the MRDR value was 0.09 ± 0.05 (19), which indicated a much poorer vitamin A status than in the rural women even though serum retinol concentrations were identical. After an intervention with indigenous African green leaves, serum retinol concentrations did not change or differ during the study (P ≥ 0.41), but the MRDR test improved within the intervention group (P = 0.0001). These results contradicted a simulated analysis in which the difference shown in MRDR values was proposed to occur because of underlying different serum retinol concentrations between groups (42).
Even in the United States, vitamin A status can be poor especially in low-income groups. Specifically, in children who qualified for the Special Supplemental Nutrition Program for Women, Infants, and Children, 32% of children were in the uncertain area for MRDR values, which was defined as 0.030–0.060 (43). This result was in contrast to that in children with a generally higher economic status in the United States where the mean MRDR value was 0.019 ± 0.010 in 22 children tested 2–10 h after an oral dose of 3,4-didehydroretinyl acetate (37). Only 2 children tested >0.030 at 4 and 6 h after the dose, which was within the recommended time interval for the test sample to be taken (39). Furthermore, an assessment of low-income pregnant women showed that an alarming 9% were above the international MRDR value cutoff of 0.060 (44). Serum carotenoid concentrations were also analyzed in these low-income women and children. In some cases, serum β-carotene concentrations were not detectable, which indicated that vegetable consumption was likely very low (43, 44).
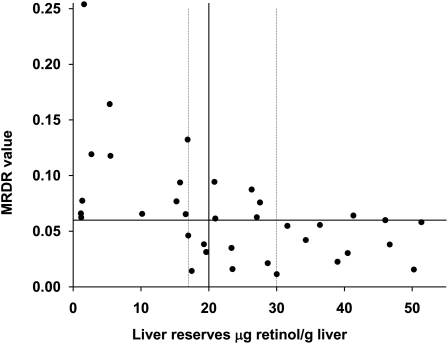
Although the MRDR test is very useful to evaluate a deficient through normal vitamin A status, as currently applied, it does not have utility in defining the subtoxic and toxic range of liver reserves. Nonetheless, the magnitude of the ratio is related to liver reserves. When data from several piglet studies were combined (40, 45–47), liver reserves <17 μg vitamin A/g liver (0.06 μmol vitamin A/g liver) were exclusively associated with an MRDR value ≥0.060 (Figure 4). Liver reserves from 0.06 to 0.1 μmol vitamin A/g liver were scattered above and below the MRDR cutoff, and liver values >0.1 μmol vitamin A/g liver were almost invariably associated with MRDR values <0.060. From these data by using the MRDR test and data obtained in rats in which the down-regulation of lecithin:retinol acyltransferase, which is responsible for retinol esterification, occurred at the same liver concentration (48), we propose that 0.1 μmol vitamin A/g liver should signify vitamin A deficiency instead of the current cutoff of 0.07 μmol vitamin A/g liver. If liver reserves illicit a biological response to a vitamin A challenge dose, the vitamin A status is not in equilibrium, and the individual should be considered at risk of vitamin A deficiency.
FIGURE 4.
The relation of the modified relative dose-response (MRDR) value to liver retinol concentrations in piglets. Below 17 μg retinol/g liver, the MRDR value was invariably positive (ie, ≥0.060); between 17 and 29 μg retinol/g liver, the response was split; and at >29 μg retinol/g liver, the MRDR value was usually <0.060. The solid lines are the current accepted cutoffs to define vitamin A deficiency. The dashed lines define the areas where the MRDR value had the best sensitivity to reflect deficient and adequate vitamin A status defined by liver reserves.
Retinol isotope dilution
The most sensitive biomarker of vitamin A status to liver reserves of vitamin A is isotope dilution testing (31, 49). The most widely used isotope test uses deuterated retinyl acetate as the tracer. 13C-retinyl acetate has been used as the tracer in rats (20), rhesus monkeys (50), and humans for the assessment of vitamin A status (51). The difference in practice is the type of equipment used for the analysis. The deuterated retinol test uses conventional gas chromatography–mass spectrometry (GC-MS), whereas the 13C-retinol test uses gas chromatography-combustion-isotope ratio mass spectrometry (GCCIRMS). GC-MS analysis requires the formation of the tert-butyldimethylsilyl derivative before injection into the gas chromatograph, whereas the GCCIRMS does not. GC-MS with electron-capture negative chemical ionization detection increased the sensitivity of the method (52, 53), but 13C-retinol with GCCIRMS requires a smaller dose to trace total body stores (50, 54).
All methods that calculate total body stores of vitamin A use the same fundamental mass-balance equation (55) as follows:
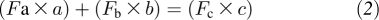
where a refers to the amount of dose absorbed and stored (experimentally determined to be 0.5–0.8 of the dose administered), b represents baseline reserves of vitamin A, c = a + b = total postdose reserves of vitamin A, and F = R ÷ (R + 1), where R is13C:12C. Various adaptations of this equation have been used to reflect the unique metabolism of vitamin A (49, 50).
Paired-isotope dilution tests to evaluate baseline and follow-up liver reserves have been used to determine changes in total-body vitamin A reserves in response to an intervention (56, 57). Examples of this included the estimation of relative vitamin A equivalency factors (58) and assessment of the effect of different intakes of vitamin A on calculations of total body reserves (59) and effects of supplementation on liver stores (53, 60). Vitamin A supplementation and abrupt changes in dietary intakes may result in the exaggeration of liver reserves or affect value estimates with the test (53, 59). With the use of a graded supplementation strategy, paired-isotope dilution testing predicted that higher intakes of vitamin A were needed to maintain a higher total-body vitamin A pool size (60). Thus, vitamin A utilization and requirements vary based on the amount of vitamin A contained in the body.
The 13C-retinol dilution test has been validated in rats against liver reserves with an r = 0.98 (20). When the atom percentage excess was evaluated at 3 different intakes of vitamin A supplementation at 4 time intervals after isotope dosage, none of the relations overlapped, which showed the robustness of the test to assess differences in liver vitamin A reserves. This test required very small doses of the isotope tracer, and thus, vitamin A trafficking was not perturbed. After the rat study, the test was applied to rhesus monkeys (50) that were known to have hypervitaminosis A based on liver-reserve analysis in monkeys from the same colony (61). Measured compared with predicted liver reserves in these monkeys revealed a linear relation, and all monkeys were diagnosed as having hypervitaminosis A by the predicted values (50). The 13C-retinol dilution test has been applied to humans.
A recent application of 13C-retinol analysis by GCCIRMS was to evaluate the compliance to a high vegetable intake (62). Plant foods have different enrichments of 13C depending on whether they are C4 or C3 plants, the former which contains higher amounts of 13C (63). Most vegetables consumed in the United States are C3 plants and therefore have less 13C than C4 plants such as maize. The shift in natural abundance of 13C in retinol was used as a biomarker of the formation of retinol from the β-carotene consumed in the diet. The provided diet was high in pumpkin, carrots, and spinach, which are all C3 plants. Indeed, the group that received more vegetables during the intervention had a lower enrichment of 13C in the purified retinol from their serum (62).
Although isotope dilution testing is usually too expensive to consider as a means to evaluate a program, an evaluation of a sugar-fortification program was performed in a small group of Nicaraguan children (64). The baseline mean liver retinol concentration was 0.57 μmol retinol/g liver, which was well above what is currently considered deficient (0.07 μmol retinol/g liver). All children had serum retinol concentrations between 0.74 and 1.31 μmol/L. One year after the sugar fortification was implemented, the estimated liver reserve concentration increased to an average of 1.2 μmol retinol/g liver. In 9 of 21 children, liver vitamin A concentrations were calculated to be >1.05 μmol vitamin A/g liver after fortification, which was defined as toxic in 1990 (65). Because many foods are being considered for fortification, this sensitive methodology may have to be used because no other method except a liver biopsy is able to diagnose hypervitaminosis A.
Considering the validation in monkeys and these results in children, an isotope methodology can be useful in defining the hypervitaminotic range of liver reserves. Specifically, liver reserves >10 μmol vitamin A/g were quantified (50). Thus, a question mark that vitamin A experts published in 2004 in relation to the upper useful limit for isotope dilution can now be replaced with the value of 10 μmol vitamin A/g liver (Figure 3) in 2010. However, a paucity of data exists in humans regarding the ramifications of a subtoxic or toxic vitamin A status. In 1990, excessive liver reserves were defined as 0.70–1.05 μmol vitamin A/g liver, and toxic status was defined as ≥1.05 μmol vitamin A/g in humans (65). However, after fortification of sugar with vitamin A in Nicaragua, many of the children had liver reserves greater than this range. The liver vitamin A concentration at which ill health in humans occurs needs to be examined more carefully. Are there ramifications of having a liver reserve that hovers at ≈1 μmol vitamin A/g liver, or is the human body able to sequester this concentration in the liver? Considering the degree of fortification in some developing countries, the improvements in the stability of fortificants used in formulations and the high consumption of some of these fortified foods, an additional examination of toxicity or hypervitaminosis A needs to occur. For example, in the study performed in hypervitaminotic rhesus monkeys, lactate dehydrogenase, aspartate aminotransferase, and serum albumin were elevated in 50%, 19%, and 44% of the monkeys, respectively (50). Elevations of these enzymes are markers of liver disease or malfunction (66) and may be a vitamin A–toxicity outcome (67, 68). The key questions are as follows: Should we be concerned about vitamin A toxicity in countries with a high degree of fortification? Or is the alleviation of vitamin A deficiency more important than the potential ramifications from hypervitaminosis A?
Liver biopsy or autopsy
The liver is the main storage organ for vitamin A. Liver biopsies have been done under surgical conditions in the United States and Bangladesh, in part to validate the isotope dilution assay (69, 70). These studies showed very good agreement between the estimated values for the liver vitamin A concentration from the isotope dilution assay and the measured liver vitamin A concentration of the group. Samples from autopsy and liver-transplant patients have also been analyzed under special circumstances (71). The distribution of vitamin A across the liver is not uniform (72), but biopsy samples likely reflect the vitamin A status of the individual better than any other biochemical method. However, for obvious reasons, a liver biopsy cannot be widely used.
CONCLUSIONS
If we could teach communities to garden and consume the produce or have a wide adoption of staple crops biofortified with provitamin A carotenoids (73, 74), markers of vitamin A status would not be needed. However, this ideal will likely not occur until poverty is alleviated (75). Therefore, biomarkers of vitamin A status are still needed for the near future to more specifically identify populations at risk of vitamin A deficiency and to evaluate the effectiveness of different interventions or programs. Obtaining vitamin A from provitamin A sources is ultimately safer than fortification with preformed vitamin A considering the potential risk of hypervitaminosis A (74). However, this obtainment requires an adequate distribution in the poor and often a behavior change, which are not easily accomplished.
Acknowledgments
The author has been working on vitamin A assessment methodology for most of her research career and received no financial gain from these activities apart from research grants, travel reimbursement, and speaker honoraria.
REFERENCES
- 1.Ross SA, McCaffery PJ, Drager UC, De Luca LM. Retinoids in embryonal development. Physiol Rev 2000;80:1021–54 [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization Global Database on Vitamin A Deficiency 2009. Global prevalence of vitamin A deficiency in populations at risk 1995-2005. Available from: http://www.who.int/vmnis/vitamina/en/ (cited April 2010)
- 3.Tanumihardjo SA. Assessing vitamin A status: past, present and future. J Nutr 2004;134:290S–3S [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization Indicators for assessing vitamin A deficiency and their application in monitoring and evaluating intervention programmes. WHO/NUT/96.10. Geneva, Switzerland: World Health Organization, 1996 [Google Scholar]
- 5.Haskell MJ, Pandey P, Graham JM, Peerson JM, Shrestha RK, Brown KH. Recovery from impaired dark adaptation in nightblind pregnant Nepali women who receive small daily doses of vitamin A as amaranth leaves, carrots, goat liver, vitamin A-fortified rice, or retinyl palmitate. Am J Clin Nutr 2005;81:461–71 [DOI] [PubMed] [Google Scholar]
- 6.Graham JM, Haskell MJ, Pandey P, Shrestha RK, Brown KH, Allen LH. Supplementation with iron and riboflavin enhances dark adaptation response to vitamin A-fortified rice in iron-deficient, pregnant, nightblind Nepali women. Am J Clin Nutr 2007;85:1375–84 [DOI] [PubMed] [Google Scholar]
- 7.Udomkesmalee E, Dhanamitta S, Sirisinha S, et al. Effect of vitamin A and zinc supplementation on the nutriture of children in Northeast Thailand. Am J Clin Nutr 1992;56:50–7 [DOI] [PubMed] [Google Scholar]
- 8.Tanumihardjo SA, Permaesih D, Dahro AM, et al. Comparison of vitamin A assessment techniques in children from two Indonesian villages. Am J Clin Nutr 1994;60:136–41 [DOI] [PubMed] [Google Scholar]
- 9.Lietman TM, Dhital SP, Dean D. Conjunctival impression cytology for vitamin A deficiency in the presence of infectious trachoma. Br J Ophthalmol 1998;82:1139–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rahman MM, Mahalanabis D, Wahed MA, et al. Conjunctival impression cytology fails to detect subclinical vitamin A deficiency in young children. J Nutr 1995;125:1869–74 [DOI] [PubMed] [Google Scholar]
- 11.Gamble MV, Ramakrishnan R, Palafox NA, Briand K, Berglund L, Blaner WS. Retinol binding protein as a surrogate measure for serum retinol: studies in vitamin A-deficient children from the Republic of the Marshall Islands. Am J Clin Nutr 2001;73:594–601 [DOI] [PubMed] [Google Scholar]
- 12.Craft NE. Innovative approaches to vitamin A assessment. J Nutr 2001;131:1626S–30S [DOI] [PubMed] [Google Scholar]
- 13.Wahed MA, Alvarez JO, Khaled MA, Mahalanabis D, Rahman MM, Habte D. Comparison of the modified relative dose response (MRDR) and the relative dose response (RDR) in the assessment of vitamin A status in malnourished children. Am J Clin Nutr 1995;61:1253–6 [DOI] [PubMed] [Google Scholar]
- 14.Mills JP, Furr HC, Tanumihardjo SA. Retinol to retinol-binding protein (RBP) is low in obese adults due to elevated _apo_-RBP. Exp Biol Med (Maywood) 2008;233:1255–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tanumihardjo SA, Permaesih D, Muherdiyantiningsih, et al. Vitamin A status of Indonesian children infected with Ascaris lumbricoides after dosing with vitamin A supplements and albendazole. J Nutr 1996;126:451–7 [DOI] [PubMed] [Google Scholar]
- 16.Thurnham DI, McCabe GP, Northrop-Clewes CA, Nestel P. Effects of subclinical infection on plasma retinol concentrations and assessment of prevalence of vitamin A deficiency: meta-analysis. Lancet 2003;362:2052–8 [DOI] [PubMed] [Google Scholar]
- 17.Tanumihardjo SA. Muherdiyantiningsih, Permaesih D, et al. Daily supplements of vitamin A (8.4 μmol; 8000 IU) improve the vitamin A status of lactating Indonesian women. Am J Clin Nutr 1996;63:32–5 [DOI] [PubMed] [Google Scholar]
- 18.Tchum SK, Tanumihardjo SA, Newton S, et al. Evaluation of vitamin A supplementation regimens in Ghanaian postpartum mothers using the modified-relative-dose-response test. Am J Clin Nutr 2006;84:1344–9 [DOI] [PubMed] [Google Scholar]
- 19.Tchum SK, Newton S, Tanumihardjo SA, Arthur FKN, Tetteh A, Owusu-Agyei S. Evaluation of a green leafy vegetable intervention in Ghanaian postpartum mothers. Afr J Food Agric Nutr Development 2009;9:1294–308 [Google Scholar]
- 20.Tanumihardjo SA. Vitamin A status assessment in rats with 13C4-retinyl acetate and gas chromatography/combustion/isotope ratio mass spectrometry. J Nutr 2000;130:2844–9 [DOI] [PubMed] [Google Scholar]
- 21.Barua AB, Duitsman PK, Olson JA. The role of vitamin A status in the conversion of all-trans retinoyl β-glucuronide to retinoic acid in male Sprague–Dawley rats. Nutr Biochem 1998;9:676–81 [Google Scholar]
- 22.Goswami BC, Reida AK, Ivanoff KD, Barua AB, Olson JA. Intestinal absorption and metabolism of retinoyl β-glucuronide in humans and of 15-[14C]-retinoyl β-glucuronide in rats of different vitamin A status. Nutr Biochem 2003;14:703–9 [DOI] [PubMed] [Google Scholar]
- 23.Rosales FJ, Ross AC. A low molar ratio of retinol binding protein to transthyretin indicates vitamin A deficiency during inflammation: studies in rats and a posterior analysis of vitamin A-supplemented children with measles. J Nutr 1998;128:1681–7 [DOI] [PubMed] [Google Scholar]
- 24.Rosales FJ, Chau KK, Haskell MH, Shankar AH. Determination of a cut-off value for the molar ratio of retinol-binding protein to transthyretin (RBP:TTR) in Bangladeshi patients with low hepatic vitamin A stores. J Nutr 2002;132:3687–92 [DOI] [PubMed] [Google Scholar]
- 25.Sarma PC, Goswami BC, Gogoi K, Bhattacharjee H, Barua AB. A new approach to the assessment of marginal vitamin A deficiency in children in suburban Guwahati, India: hydrolysis of retinoyl glucuronide to retinoic acid. Br J Nutr 2009;101:794–7 [DOI] [PubMed] [Google Scholar]
- 26.Tanumihardjo SA, Penniston KL. Simplified methodology to determine breast milk retinol concentrations. J Lipid Res 2002;43:350–5 [PubMed] [Google Scholar]
- 27.Ayah RA, Mwaniki DL, Magnussen P, et al. The effects of maternal and infant vitamin A supplementation on vitamin A status: a randomised trial in Kenya. Br J Nutr 2007;98:422–30 [DOI] [PubMed] [Google Scholar]
- 28.Ross AC, Pasatiempo AM, Green MH. Chylomicron margination, lipolysis, and vitamin A uptake in the lactating rat mammary gland: implications for milk retinoid content. Exp Biol Med (Maywood) 2004;229:46–55 [DOI] [PubMed] [Google Scholar]
- 29.Surles RL, Li J, Tanumihardjo SA. The modified-relative-dose-response values in serum and milk are positively correlated over time in lactating sows with adequate vitamin A status. J Nutr 2006;136:939–45 [DOI] [PubMed] [Google Scholar]
- 30.Rice AL, Stoltzfus RJ, de Francisco A, Kjolhede CL. Evaluation of serum retinol, the modified-relative-dose-response ratio, and breastmilk vitamin A as indicators of response to postpartum maternal vitamin A supplementation. Am J Clin Nutr 2000;71:799–806 [DOI] [PubMed] [Google Scholar]
- 31.Vitamin A Tracer Task Force Appropriate uses of vitamin A tracer (stable isotope) methodology. (Members: Furr HC, Green MH, Haskell M, et al.). Lead drafters: Tanumihardjo SA, Nestel P. Washington, DC: ILSI Human Nutrition Institute, 2004 [Google Scholar]
- 32.Muto Y, Smith JE, Milch PO, Goodman DS. Regulation of retinol-binding protein metabolism by vitamin A status in the rat. J Biol Chem 1972;247:2542–50 [PubMed] [Google Scholar]
- 33.Loerch JD, Underwood BA, Lewis KC. Response of plasma levels of vitamin A to a dose of vitamin A as an indicator of hepatic vitamin A reserves in rats. J Nutr 1979;109:778–86 [DOI] [PubMed] [Google Scholar]
- 34.Tanumihardjo SA, Barua AB, Olson JA. Use of 3,4-didehydroretinol to assess vitamin A status in rats. Int J Vitam Nutr Res 1987;57:127–32 [PubMed] [Google Scholar]
- 35.Tanumihardjo SA, Olson JA. A modified relative dose-response assay employing 3,4-didehydroretinol (vitamin A2) in rats. J Nutr 1988;118:598–603 [DOI] [PubMed] [Google Scholar]
- 36.Tanumihardjo SA, Furr HC, Erdman JW, Jr, Olson JA. Use of the modified relative dose response (MRDR) assay in rats and its application to humans for the measurement of vitamin A status. Eur J Clin Nutr 1990;44:219–24 [PubMed] [Google Scholar]
- 37.Tanumihardjo SA, Koellner PG, Olson JA. The modified relative-dose-response assay as an indicator of vitamin A status in a population of well-nourished American children. Am J Clin Nutr 1990;52:1064–7 [DOI] [PubMed] [Google Scholar]
- 38.Tanumihardjo SA. Muhilal, Yuniar Y, et al. Assessment of vitamin A status in preschool-age Indonesian children by the modified relative dose response (MRDR) assay. Am J Clin Nutr 1990;52:1068–72 [DOI] [PubMed] [Google Scholar]
- 39.Tanumihardjo SA, Cheng JC, Permaesih D, et al . Refinement of the modified-relative-dose-response test as a method for assessing vitamin A status in a field setting: experience with Indonesian children. Am J Clin Nutr 1996;64:966–71 [DOI] [PubMed] [Google Scholar]
- 40.Valentine AR, Tanumihardjo SA. Adjustments to the modified relative dose response (MRDR) test for assessment of vitamin A status minimize the blood volume used in piglets. J Nutr 2004;134:1186–92 [DOI] [PubMed] [Google Scholar]
- 41.Tanumihardjo SA, Permaesih D. Muhilal. Vitamin A status and hemoglobin concentrations are improved in Indonesian children with vitamin A and deworming interventions. Eur J Clin Nutr 2004;58:1223–30 [DOI] [PubMed] [Google Scholar]
- 42.Verhoef H, West CE. Validity of the relative-dose-response test and the modified-relative-dose-response test as indicators of vitamin A stores in liver. Am J Clin Nutr 2005;81:835–9 [DOI] [PubMed] [Google Scholar]
- 43.Spannaus-Martin DJ, Cook LR, Tanumihardjo SA, Duitsman PK, Olson JA. Vitamin A and vitamin E statuses of preschool children of socioeconomically disadvantaged families living in the midwestern United States. Eur J Clin Nutr 1997;51:864–9 [DOI] [PubMed] [Google Scholar]
- 44.Duitsman PK, Cook LR, Tanumihardjo SA, Olson JA. Vitamin A inadequacy in socioeconomically disadvantaged Iowan women as assessed by the modified relative dose response (MRDR) test. Nutr Res 1995;15:1263–76 [Google Scholar]
- 45.Surles RL, Mills JP, Valentine AR, Tanumihardjo SA. One-time graded doses of vitamin A to weanling piglets enhance hepatic retinol but do not always prevent a deficient vitamin A status. Am J Clin Nutr 2007;86:1045–53 [DOI] [PubMed] [Google Scholar]
- 46.Valentine AR, Tanumihardjo SA. One-time vitamin A supplementation of lactating sows enhances hepatic retinol of offspring independent of dose size. Am J Clin Nutr 2005;81:427–33 [DOI] [PubMed] [Google Scholar]
- 47.Valentine AR. Evaluation of the modified relative dose response test and vitamin A supplementation in a swine model. MS thesis. University of Wisconsin-Madison, Madison, WI, 2004 [Google Scholar]
- 48.Ross AC, Zolfaghari R. Regulation of hepatic retinol metabolism: perspectives from studies on vitamin A status. J Nutr 2004;134:269S–75S [DOI] [PubMed] [Google Scholar]
- 49.Furr HC, Green M, Haskell M, et al. Stable isotope dilution techniques for assessing vitamin A status and bioefficacy of provitamin A carotenoids in humans. Public Health Nutr 2005;8:596–607 [DOI] [PubMed] [Google Scholar]
- 50.Escaron AL, Green MH, Howe JA, Tanumihardjo SA. Mathematical modeling of serum 13C-retinol in captive rhesus monkeys provides new insights on hypervitaminosis A. J Nutr 2009;139:2000–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tanumihardjo SA. A small physiological dose of vitamin A (17.5 μmol) takes 4 years to “disappear” in healthy individuals. In: Report of the XXI International Vitamin A Consultative Group Meeting, Improving the Vitamin A Status of Populations. Washington, DC: ILSI Human Nutrition Institute: 2003:55 (T9) [Google Scholar]
- 52.Tang G, Qin J, Dolnikowski GG. Deuterium enrichment of retinol in humans determined by gas chromatography electron capture negative chemical ionization mass spectrometry. J Nutr Biochem 1998;9:408–14 [Google Scholar]
- 53.Ribaya-Mercado JD, Mazariegos M, Tang G, et al. Assessment of total body stores of vitamin A in Guatemalan elderly by the deuterated-retinol-dilution method. Am J Clin Nutr 1999;69:278–84 [DOI] [PubMed] [Google Scholar]
- 54.Escaron AL, Tanumihardjo SA. Orally ingested 13C2-retinol is incorporated into hepatic retinyl esters in a nonhuman primate (Macaca mulatta) model of hypervitaminosis A. Comp Med 2010;60:71–6 [PMC free article] [PubMed] [Google Scholar]
- 55.Goodman KJ, Brenna JT. High sensitivity tracer detection using high-precision gas chromatography-combustion isotope ratio mass spectrometry and highly enriched [U-13C]-labeled precursors. Anal Chem 1992;64:1088–95 [DOI] [PubMed] [Google Scholar]
- 56.Tang G, Gu X, Hu S, et al. Green and yellow vegetables can maintain body stores of vitamin A in Chinese children. Am J Clin Nutr 1999;70:1069–76 [DOI] [PubMed] [Google Scholar]
- 57.Haskell M, Ribaya-Mercado JD. Vitamin A Tracer Task Force. Handbook on vitamin A tracer dilution methods to assess status and evaluate intervention programs. Technical Monograph 5. Washington, DC: HarvestPlus, 2005 [Google Scholar]
- 58.Haskell MJ, Jamil KM, Hassan F, et al. Daily consumption of Indian spinach (Basella alba) or sweet potatoes has a positive effect on total-body vitamin A stores in Bangladeshi men. Am J Clin Nutr 2004;80:705–14 [DOI] [PubMed] [Google Scholar]
- 59.Haskell MJ, Mazumder RN, Peerson JM, et al. Use of the deuterated-retinol-dilution technique to assess total-body vitamin A stores of adult volunteers consuming different amounts of vitamin A. Am J Clin Nutr 1999;70:874–80 [DOI] [PubMed] [Google Scholar]
- 60.Haskell MJ, Jamil KM, Peerson JM, Wahed MA, Brown KH. The paired deuterated retinol dilution technique can be used to estimate the daily vitamin A intake required to maintain a targeted whole body vitamin A pool size in men. J Nutr 2011;141:428–32 [DOI] [PubMed] [Google Scholar]
- 61.Penniston KL, Tanumihardjo SA. Subtoxic hepatic vitamin A concentrations in captive Rhesus monkeys (Macaca mulatta). J Nutr 2001;131:2904–9 [DOI] [PubMed] [Google Scholar]
- 62.Howe JA, Valentine AR, Hull AK, Tanumihardjo SA. 13C natural abundance in serum retinol acts as a biomarker for increases in dietary provitamin A. Exp Biol Med (Maywood) 2009;234:140–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Smith BN, Epstein S. Two categories of 13C/12C ratios for higher plants. Plant Physiol 1971;47:380–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ribaya-Mercado JD, Solomons NW, Medrano Y, et al. Use of the deuterated-retinol-dilution technique to monitor the vitamin A status of Nicaraguan schoolchildren 1 y after initiation of the Nicaraguan national program of sugar fortification with vitamin A. Am J Clin Nutr 2004;80:1291–8 [DOI] [PubMed] [Google Scholar]
- 65.Olson JA. Vitamin A Brown ML, Present knowledge in nutrition. 6th ed. Washington, DC: International Life Science Institute, 1990:101 [Google Scholar]
- 66.Knight JA. Liver function tests: their role in the diagnosis of hepatobiliary diseases. J Infus Nurs 2005;28:108–17 [DOI] [PubMed] [Google Scholar]
- 67.Muenter MD, Perry HO, Ludwig J. Chronic vitamin A intoxication in adults. Hepatic, neurologic and dermatologic complications. Am J Med 1971;50:129–36 [DOI] [PubMed] [Google Scholar]
- 68.Russell RM, Boyer JL, Bagheri SA, Hruban Z. Hepatic injury from chronic hypervitaminosis A resulting in portal hypertension and ascites. N Engl J Med 1974;291:435–40 [DOI] [PubMed] [Google Scholar]
- 69.Furr HC, Amedee-Manesme O, Clifford AJ, et al. Vitamin A concentrations in liver determined by isotope dilution assay with tetradeuterated vitamin A and by biopsy in generally healthy adult humans. Am J Clin Nutr 1989;49:713–6 [DOI] [PubMed] [Google Scholar]
- 70.Haskell MJ, Handelman GJ, Peerson JM, et al. Assessment of vitamin A status by the deuterated-retinol-dilution technique and comparison with hepatic vitamin A concentration in Bangladeshi surgical patients. Am J Clin Nutr 1997;66:67–74 [DOI] [PubMed] [Google Scholar]
- 71.Tanumihardjo SA, Furr HC, Amedee-Manesme O, Olson JA. Composition of retinyl esters (vitamin A esters) and carotenoids in human liver. Int J Vitam Nutr Res 1990;60:307–13 [PubMed] [Google Scholar]
- 72.Olson JA, Gunning D, Tilton R. The distribution of vitamin A in human liver. Am J Clin Nutr 1979;32:2500–7 [DOI] [PubMed] [Google Scholar]
- 73.Tanumihardjo SA, Bouis H, Hotz C, Meenakshi JV, McClafferty B. Biofortification of staple crops: an emerging strategy to combat hidden hunger. Comp Rev Food Sci Food Safety 2008;7:329–34 [Google Scholar]
- 74.Tanumihardjo SA. Food-based approaches for ensuring adequate vitamin A nutrition. Comp Rev Food Sci Food Safety 2008;7:373–81 [Google Scholar]
- 75.Tanumihardjo SA, Anderson C, Kaufer-Horwitz M, et al. Poverty, obesity and malnutrition: an international perspective recognizing the paradox. J Am Diet Assn 2007;107:1966–72 [DOI] [PubMed] [Google Scholar]