A Pilot Study of MUC-1/CEA/TRICOM Poxviral-Based Vaccine in Patients with Metastatic Breast and Ovarian Cancer (original) (raw)
. Author manuscript; available in PMC: 2012 Nov 15.
Abstract
Purpose
PANVAC is a recombinant poxviral vaccine that contains transgenes for MUC-1, CEA and 3 T-cell costimulatory molecules. This study was conducted to obtain preliminary evidence of clinical response in metastatic breast and ovarian cancer patients.
Experimental design
Twenty-six patients were enrolled and given monthly vaccinations. Clinical and immune outcomes were evaluated.
Results
These patients were heavily pretreated, with 21 of 26 patients having ≥ 3 prior chemotherapy regimens. Side effects were largely limited to mild injection-site reactions. Breast cancer: For the 12 patients enrolled, median time to progression was 2.5 months (1 – 37+) and median overall survival was 13.7 months. Four patients had stable disease. One patient had a complete response by RECIST and remains on study ≥ 37 months, with a significant drop in serum IL-6 and IL-8 by day 71. Another patient with metastatic disease confined to the mediastinum had a 17% reduction in mediastinal mass and was on study for 10 months. Patients with stable or responding disease had fewer prior therapies and lower tumor marker levels than patients with no evidence of response. Ovarian cancer:Median time to progression for patients (n=14) was 2 months (1 – 6) and median overall survival was 15.0 months. Updated data are presented here for one patient treated with this vaccine in a previous trial, with a time to progression of 38 months.
Conclusions
Some patients who had limited tumor burden with minimal prior chemotherapy appeared to benefit from the vaccine. Further studies to confirm these results are warranted.
Keywords: Therapeutic Vaccine, Immune Response, Immuno-Oncology
Introduction
Tumor-associated antigens (TAAs) are either weakly immunogenic or functionally nonimmunogenic. We have previously shown in preclinical models (1) that one strategy to break immune tolerance is to introduce TAAs to the immune system in the context of poxviral vectors. We report here the results of a study with PANVAC, a recombinant poxviral vaccine expressing the TAAs carcinoembryonic antigen (CEA) and mucin-1 (MUC-1), along with 3 costimulatory molecules. A previous safety study in patients with metastatic carcinoma (n = 25) showed evidence of clinical benefit in some patients with breast or ovarian cancer (2). This is a follow-up study consisting of 2 cohorts with either metastatic breast cancer or metastatic ovarian cancer, with clinical outcome as the primary endpoint.
The large poxviral genome allows for the insertion of multiple genes, including genes coding for multiple antigens or immunostimulatory molecules which, following vaccination, can be expressed within host cells (3). PANVAC is a recombinant poxviral vaccine platform that contains transgenes for the TAAs MUC-1 and CEA. MUC-1 is a transmembrane glycoprotein that is overexpressed in underglycosylated form in many human carcinoma cells (4, 5), and the cytoplasmic domain of MUC-1 has been shown to play a crucial role in carcinogenesis (6, 7). CEA is another glycoprotein overexpressed on the majority of adenocarcinomas. Its selective overexpression also makes it a potential target for immunotherapy (8, 9). PANVAC also includes transgenes for a triad of human T-cell costimulatory molecules designated TRICOM, composed of B7.1, intercellular adhesion molecule (ICAM)-1, and lymphocyte function-associated antigen (LFA)-3. Expression of costimulatory molecules in antigen-presenting cells (APCs) has been shown to generate a stronger immune response and higher numbers of TAA-specific T cells (1, 10-12). PANVAC is given in a diversified prime-boost fashion, which has been shown (13-15) to be superior to continuous use of a single vector. The first vaccination with recombinant vaccinia (PANVAC-V) elicits a strong initial immune response, but its continuous use is limited by the production of host-induced neutralizing antibodies to vaccinia. Subsequent vaccination with recombinant fowlpox (PANVAC-F), however, does not provoke neutralizing antibody production, since fowlpox is replication-deficient in humans and cannot produce late viral proteins, including coat proteins (14). Granulocyte-macrophage colony-stimulating factor (GM-CSF) is also given as a vaccine adjunct to enhance the migration and maturation of APCs, as previously described in several preclinical and clinical studies (14, 16).
Our previous study showed the safety of PANVAC in advanced solid tumors and evidence of clinical benefit in a subset of patients (17). Results of the study reported here provide further insight into clinical efficacy and immune response, and confirm the safety and tolerability of this vaccine regimen.
Patients and Methods
Patient selection and trial design
Twenty-six patients with metastatic breast or ovarian cancer who had progressive disease following standard chemotherapy, or were not candidates for standard chemotherapy, were enrolled in this trial approved by the National Cancer Institute (NCI) Institutional Review Board and conducted at the NCI. The study was designed as a pilot trial to evaluate clinical outcomes with the use of PANVAC vaccine in metastatic breast and ovarian cancer patients, with immunologic response as the secondary endpoint. Patients were required to have an Eastern Cooperative Oncology Group performance status of 0 or 1 and adequate hematologic, hepatic, and renal function. In addition, patients were not enrolled if there was evidence of immunosuppression (i.e., reactive HIV test, diagnosis of altered immune function, prior splenectomy, or concurrent steroid use). Prior vaccinia exposure (i.e., smallpox vaccination) was allowed but not required.
Exclusion criteria included known allergy to eggs; history ofor active skin disorders such as eczema, extensive psoriasis, varicella zoster, impetigo, or burns; history of seizures; serious intercurrent illness; noncutaneous malignant process; and close contact with immunocompromised individuals, individuals with the above-mentioned skin conditions, or children under 3 years of age. All patients gave written informed consent in accordance with federal, state, and institutional guidelines.
Vaccine formulation and treatment plan
Both of the viral vaccines used were manufactured as part of a Cooperative Research and Development Agreement between Therion Biologics and the Laboratory of Tumor Immunology and Biology, NCI. Vaccines were provided by the Cancer Therapy Evaluation Program, NCI. PANVAC-V [recombinant vaccinia-CEA(6D)/MUC-1(L93)/TRICOM; NSC #727026] was prepared from virus derived from the Wyeth (New York City Board of Health) strain of vaccinia, selected for its favorable toxicity profile. PANVAC-F [recombinant fowlpox-CEA(6D)/MUC-1(L93)/TRICOM; NSC #727027] was constructed by inserting the identical transgenes into the replication-defective fowlpox virus. All patients received the same dose and schedule of vaccine. The priming vaccine consisted of 2 × 108 pfu of PANVAC-V administered s.c. The boosting vaccine was given on or about days 15, 29, and 43, then every 28 days while on study. Sargramostim (GM-CSF) 100 μg s.c. was given the day of each vaccine and for the following 3 consecutive days. A sterile, nonadherent dressing (i.e., Telfa) was used to cover the site.
Patients were seen at least monthly while on study, at which time complete interval histories, physical examinations, blood chemistries, hemograms, and serum tumor markers were obtained. All patients were evaluated for toxicity by the NCI Common Toxicity Criteria version 3 and the previously published vaccinia toxicity grading scale (18). Patients had their first restaging exam at approximately day 71, with subsequent restaging exams approximately every 56 days thereafter.
Collection of peripheral blood mononuclear cells
Apheresis was done on selected patients before vaccination and again around day 71. Mononuclear cells (5 × 108 to 2 × 109) were obtained, processed and frozen as previously described.(2)
ELISPOT assay
Measurement of CD8 immune responses in HLA-A2+ patients was conducted by ELISPOT assay using a modification of the procedure previously described (19). The assay was performed using K562/A*0201 as APCs (20). ELISPOT measures the frequency of T cells releasing IFN-γ in response to a CEA peptide (CAP1-6D), a MUC-1 peptide, an HIV gag peptide, and a flu peptide (2) in pre- and post-vaccination peripheral blood mononuclear cells (PBMCs). A positive response was scored as a ≥ 2-fold increase in IFN-γ-secreting cells.
Detection of cytokines
Sera from patients pre- and post-vaccination were screened for IL-8, IL-6 and TNF-α using a multiple cytokine/chemokine kit (Meso Scale Discovery, Gaithersburg, MD).
Proliferation assay
CD4+ cells were isolated by column (Miltenyi Biotec, Auburn, CA) and used at a concentration of 1 × 106/mL in 96-well flat-bottom plates. CD4+ cells were mixed with irradiated (30 Gy), unfractionated PBMCs in the presence of various concentrations of antigens. Irradiated PBMCs at a concentration of 6 × 106/mL were used as APCs. CEA protein was used as antigen at a concentration of 10 μg/mL. PHA (2 μg/mL) and myoglobulin (10 μg/mL) (Sigma-Aldrich, St. Louis, MO) were used as controls. Cultures were incubated at 37°C at 5% CO2. The cell proliferation in cultures was estimated by [3H]thymidine (1 μCi [0.037 MBq] per well) (Perkin-Elmer, Boston, MA) incorporation pulsed on day 6 and quantified 18 h later using a liquid scintillation counter (Wallac, Gaithersburg, MD). All experiments were performed in triplicate. All results are expressed as stimulation index (SI), expressing the ratio of mean counts per minute (cpm +/− SD) in stimulated vs. unstimulated control cultures. An SI > 3 was interpreted as representing a significant positive response.
Flow cytometry analysis
Cryopreserved PBMCs were analyzed by 3-color flow cytometry for phenotypic characterization of regulatory T-cells (Tregs) as described by Yokokawa, et al. (21) Cells were stained with the following combination of antibodies: PerCP-Cy5.5-conjugated anti-CD4 and phycoerythrin (PE)-conjugated anti-CD25 (all from BD Pharmingen, San Diego, CA). FoxP3 intracellular staining was then performed on the cells stained with anti-CD4 and anti-CD25. Cells were fixed and permeabilized using a fix/perm kit (eBioscience, San Diego, CA) according to the manufacturer’s instructions, and were labeled with FITC-conjugated anti-FoxP3 antibody (236A/E7 clone) or its isotype control antibody (eBioscience). Flow cytometry was performed on a Becton Dickinson LSRII (BD Biosciences); 1 × 105 cells were acquired and data were analyzed using FACSDiva software (BD Biosciences). To determine the percentage of Tregs, lymphocytes were gated by plotting forward vs. side scatter, followed by gating on the CD4+ population. Then, CD25high and FoxP3+ populations were gated. The CD25high population was separated from CD25low cells on the basis of the level of CD25 expression in CD4− T cells, as previously described (21).
Results
Patients’ baseline characteristics are outlined in Table 1A. Median potential follow-up from date of enrollment was 51.2 months for breast and ovarian cancer patients combined (55.9 for ovarian and 46.9 for breast). Treatment was well tolerated, with no grade 3 or 4 toxicities attributable to vaccine or GM-CSF. The majority (85%) of grade 1 and 2 toxicities were injection-site reactions such as erythema, edema, and induration, which generally resolved spontaneously after a few days (Table 1B). One patient had a baseline grade 1 anemia, which transiently progressed to grade 2 before returning to baseline without any intervention while on study.
Table 1A.
Patient baseline characteristics
| Baseline characteristics | No. patients/median (range) | |
|---|---|---|
| Breast | Ovarian | |
| No. of patients | 12 | 14 |
| Measurable disease | 12 | 13 |
| Age (years) | 60 (32 – 75) | 55 (39-73) |
| Performance status | ||
| ECOG 0 | 2 | 5 |
| ECOG 1 | 10 | 9 |
| ER+/PR+ | 6 | N/A |
| Her2/neu+ | 2 | N/A |
| Prior therapy | ||
| Prior chemo regimens | 3 (0 – 8) | 5 (1-9) |
| < 3 chemo regimens | 3 | 2 |
| ≥ 3 chemo regimens | 9 | 12 |
| Radiation | 8 | 0 |
| Concurrent trastuzumab | 2 | N/A |
| Time since last chemo (months) | 3 (1 – 19) | 1.5 (1-13) |
| CEA level | 3.5 ng/mL (0.7 – 153.6) | N/A |
| CA 27.29 level | 167 U/mL (<12 – 276) | N/A |
| CA-125 level | N/A | 135 U/mL (11-17,333) |
Table 1B.
Grade 2 or greater toxicities associated with PANVAC + GM-CSF
| Grade 2 | ||
|---|---|---|
| Toxicity | No. | % |
| Injection-site reaction | 22 | 85 |
| Musculoskeletal pain | 2 | 7 |
| Anemia | 1 | 4 |
Breast cancer patients
The study enrolled 12 patients with a median age of 60 (range 32 – 75). Most of the patients (75%) had received at least 3 prior chemotherapy regimens, and 50% had received their last chemotherapy within 3 months prior to enrollment on study.
Clinical outcomes
A summary of clinical responses in the breast cancer patients is outlined in Table 2. Median time to progression for the 12 patients enrolled was 2.5 months (range 1 – 37+ months). The median overall survival for this group was 13.7 months (range 2.7 – 42.9), with one patient still alive on study at 37 months (supplemental Fig. 1). Five patients entered the trial with elevated CEA levels, and 2 of those had a decrease in serum CEA levels (patient 8 decreased by 38% and patient 12 decreased by 15%).
Table 2.
Clinical outcomes in breast cancer patients by best response
| Patientno. | Age | ER/PR | Her2/neu | No.priorchemoregimens | Timesincelastchemo(months) | BaselineCEA(ng/mL) | BaselineCA27.29(U/mL) | Bestresponse | PFS(months) | OS(months) |
|---|---|---|---|---|---|---|---|---|---|---|
| 8 | 62 | ER+,PR− | Negative | 5 | 1 | 153.6 | - | PD | 1 | 2.8 |
| 17 | 62 | ER+,PR− | Negative | 6 | 4 | 95.2 | 276 | PD | 1 | 4.9 |
| 12 | 57 | ER−,PR− | Negative | 3 | 4 | 71.4 | 254 | PD | 2 | 25.3 |
| 13 | 65 | ER+,PR+ | Negative | 3 | 1 | 48.6 | 182 | PD | 2 | 14.2 |
| 21 | 45 | ER−,PR− | Negative | 3 | 2 | 1.7 | 78.9 | PD | 2 | 4.9 |
| 25 | 48 | ER−,PR+ | Negative | 6 | 2 | 1.3 | 52.2 | PD | 2 | 2.7 |
| 22 | 51 | ER+,PR+ | Negative | 2 | 19 | 4.2 | 151 | PD | 3 | 31.3 |
| 23 | 75 | ER−,PR− | Negative | 2 | 1 | 1.8 | 36.5 | SD | 4 | 11.2 |
| 26 | 65 | ER−,PR− | Positive | 0 | N/A** | 8.4 | 16.2 | SD | 5 | 24.7 |
| 1 | 49 | ER+,PR− | Negative | 3 | 2 | 2.7 | - | SD, 20%↓ | 6 | 42.9 |
| 16 | 66 | ER−,PR− | Negative | 3 | 5 | 0.7 | 23.1 | SD, 17%↓ | 10 | 13.0*** |
| 24* | 32 | ER+,PR+ | Positive | 1 | 12 | 0.7 | <12.0 | CR | 37+ | 37.0+ |
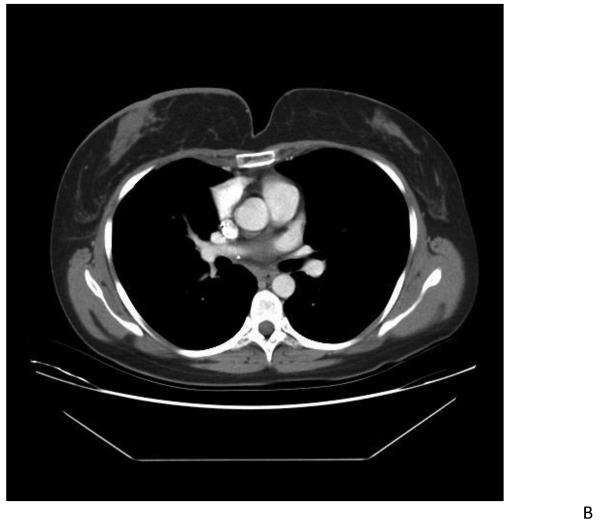
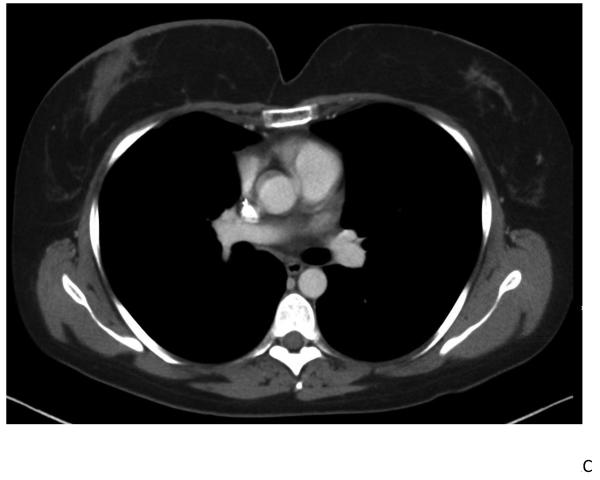
Patient 24 was a 32-year-old diagnosed with poorly differentiated invasive ductal carcinoma of the breast, ER+/PR+ and Her2/neu+ by IHC (+3). She underwent lumpectomy and radiation and was found to have liver metastasis soon after treatment. She underwent bilateral oophorectomy and then received 6 cycles of docetaxel followed by partial hepatectomy, with complete pathologic response. She received trastuzumab concurrently with chemotherapy. After liver metastectomy she received letrozole for one year, which was discontinued due to progressive disease. She was then enrolled on a Her2/neu peptide vaccine for 6 months and completed all planned 6-monthly cycles. When she enrolled on our study she had progressive but minimal disease in the hilar and mediastinal lymph nodes and was 12 months removed from her only prior chemotherapy regimen. She had a confirmed CR by RECIST, with complete resolution in mediastinal/hilar lymph nodes after 18 months of vaccine (Fig. 1). Trastuzumab was continued during the study and she remains on study 37 months after enrollment.
Fig. 1.
Patient 24 had a subcarinal lymph node mass measuring 2.8 cm (panel A) which decreased to 0.8 cm (panel B) after 10 months of vaccine, a > 50% reduction by RECIST, followed by a CR after 18 months (panel C). She remains on study 37 months after enrollment, with a durable CR.
Patient 1 was a 49-year-old with a history of hormone receptor-positive early-stage breast cancer treated with modified radical mastectomy and adjuvant chemotherapy and tamoxifen. She relapsed with bone metastases 9 years after completing adjuvant endocrine treatment. She subsequently underwent oophorectomy and then received exemestane for almost a year before bone metastases progressed. She was started on gemcitabine and docetaxel chemotherapy, but it was poorly tolerated and treatment was discontinued. She was then enrolled on the study reported here with bone and lymph node metastases and had a 20% reduction in internal mammary lymphadenopathy. She came off study after 6 months due to disease progression and went on to receive chemotherapy for a short time, followed by palliative radiation to a brain metastasis. Eventually she entered hospice and died 3 years after coming off study.
Patient 16 was a 66-year-old with invasive ductal carcinoma of the breast showing absent expression of estrogen receptor, progesterone receptor, and Her2/neu (triple negative). She was initially treated with neoadjuvant chemotherapy (4 cycles of docetaxel and epirubicin), followed by surgery and further adjuvant chemotherapy (3 cycles of docetaxel and carboplatin) and radiation. Disease recurred one year later with mediastinal lymphadenopathy, and was treated with capecitabine for a total of 6 months, with complete radiographic remission of lymphadenopathy. She was enrolled on study when mediastinal lymphadenopathy recurred 5 months after her last capecitabine dose. She had a 17% reduction in mediastinal lymphadenopathy after 8 cycles of vaccine and remained on study for 10 months.
Five of the 12 patients had either SD for ≥ 4 months or evidence of tumor regression. Those patients had a mean of 1.8 prior chemotherapies, while those with no evidence of response had a mean of 4 prior chemotherapies. Moreover, the mean serum CEA on study was 2.9 for those with progression-free survival for ≥ 4 months and 53.7 for those with PD within 3 months, while mean serum CA27.29 was 22.0 vs. 165.7 for these groups, respectively.
Immune responses
Table 3 outlines immune responses in breast cancer patients as measured by various assays. Five breast cancer patients were HLA-A2+, but only 2 of these (patients 1 and 24, who were on study for 6 and 37+ months, respectively) had sufficient PBMC samples for the ELISPOT assay. While ELISPOT without in vitro stimulation did not show any increase in CEA- or MUC-1-specific T-cell response in patients 1 and 24, 1 of 3 patients had substantial increases (>7 X) in both CEA and MUC-1 T-cells following 1 cycle (72 hours) of in vitro stimulation. Furthermore, the CD4 functional/proliferation assay showed a > 3-fold increase in the 2 patients. Patient 1 had a 4-fold increase and patient 24 had an 8-fold increase from baseline. They also showed a significant drop in the cytokines and chemokines produced mainly by tumor cells, such as IL-8, IL-6, and TNF-α, corresponding with clinical response. Conversely, patient 8 had a significant rise in cytokine levels, corresponding with a rapidly progressive clinical course.
Table 3.
Immune responses in breast cancer patients
| Patientno. | CD4assay1 | ELISPOT2CEA | MUC-1 | IL-83 | IL-63 | TNF-α3 |
|---|---|---|---|---|---|---|
| 1 | + >4X | − | − | ↓ | ↓ | ↓ |
| 8 | + >2.3X | NA | NA | ↑ | ↑ | ↑ |
| 12 | − | + >7.7X | + >9.1X | NC | NC | NC |
| 13 | −4 | − | − | ↑ | NC | ↑ |
| 23 | − | NA | NA | ↓ | NC | NC |
| 24 | +5>8X | NA6 | NA6 | ↓ | ↓ | ↓ |
| 25 | NA | NA | NA | ↓ | NC | ↑ |
Sufficient PBMCs were available from 6 breast cancer patients to measure the number of CD4+CD25highFoxP3+ Tregs as the percent of CD4+ cells and the ratio of T effector cells to Tregs as detailed in Patients and Methods. We have previously reported (21) that the percent of Tregs per CD4+ cells in healthy donors is 3.28 ± 1.16% (range, 1.46 – 5.25). As seen in Table 4, 3 of the 6 patients (patients 1, 13, and 23) showed an increase in the T effector:Treg ratio post-vs. pre-vaccination.
Table 4.
Peripheral blood Tregs* pre- and post-vaccination
| Patient | Sample | % Treg in CD4+ | Ratio of Teff:Treg** |
|---|---|---|---|
| Breast cancer patients: | |||
| 1 | PreD131 | 5.3% 3.9% | 12.5:1 17.8:1 |
| 8 | PreD44 | 2.4%2.5% | 35.1:122.5:1 |
| 12 | PreD27 | 2.6%5.1% | 28.9:113.1:1 |
| 13 | PreD41 | 8.2% 6% | 7.5:1 11.5:1 |
| 23 | PreD70 | 3%2.3% | 22.3:1 29.3:1 |
| 24 | PreD71 | 4.2%5.9% | 13.6:110.4:1 |
| Ovarian cancer patients: | |||
| 2 | PreD71 | 3.3%4.2% | 21.8:116.9:1 |
| 3 | PreD28 | 4.5%4.0% | 16.2:116.9:1 |
| 5 | PreD70 | 3.1%3.7% | 21.6:117.7:1 |
| 7 | PreD76 | 6.2% 4.2% | 9.2:1 14.2:1 |
| 10 | PreD77 | 6.4% 3.4% | 9.1:1 17.7:1 |
| 11 | PreD76 | 3.8%4.4% | 17:114:1 |
| 14 | PreD71 | 5.1% 4.0% | 13.5:1 17.5:1 |
| 19 | PreD69 | 2.4%3.1% | 23.3:118.3:1 |
Ovarian cancer patients
The study enrolled 14 patients with a median age of 55 (39 – 73). Twelve of 14 had received ≥ 3 chemotherapy regimens (Table 5). Median time to progression was 2 months (range 1 – 6 months). Median overall survival was 15.0 months (range 1.5 – 57+), with one patient still alive (supplemental Fig. 1). Two patients (patients 3 and 6) had declines in CA-125 levels of 18% and 11%, respectively. There was no significant decline in CEA.
Table 5.
Clinical outcomes for ovarian cancer patients
| Patientno. | Age | No.priorchemoregimens | Timesince lastchemo(months) | BaselineCEA(ng/mL) | BaselineCA-125(U/mL) | Bestresponse | PFS(months) | OS(months) |
|---|---|---|---|---|---|---|---|---|
| 20 | 60 | 7 | 1 | 15 | 17333 | PD | 1 | 1.5 |
| 3 | 52 | 6 | 1 | <0.5 | 142 | PD | 1 | 2.4 |
| 11 | 70 | 3 | 1 | 1 | 1162 | PD | 2 | 11.6 |
| 15 | 55 | 7 | 1 | 1 | 277 | PD | 2 | 9.6 |
| 5 | 73 | 9 | 1 | 1.7 | 128 | PD | 2 | 35.0 |
| 6 | 54 | 7 | 2 | 1.3 | 117 | PD | 2 | 57.0+ |
| 14 | 57 | 1 | 13 | 0.8 | 115 | PD | 2 | 32.7 |
| 9 | 48 | 4 | 1 | 1.5 | 80 | PD | 2 | 15.0 |
| 7 | 45 | 2 | 3 | 1.2 | 11 | PD | 2 | 8.0 |
| 4 | 50 | 4 | 3 | 0.8 | 182 | PD | 3 | 41.9 |
| 18 | 57 | 5 | 6 | <0.5 | 592 | PD | 3 | 8.7 |
| 10 | 39 | 5 | 1 | 1 | 195 | SD | 4 | 29.3 |
| 2 | 56 | 4 | 4 | 0.5 | 46 | SD | 4 | 16.1 |
| 19 | 50 | 8 | 8 | 1.8 | 114 | SD | 6 | 40.5 |
Patient 19 was a 50-year-old diagnosed with stage III-C endometrioid-type ovarian adenocarcinoma 10 years prior to enrollment on study. She was initially treated with debulking surgery, followed by 8 cycles of carboplatin and taxol. Disease recurred 8 months later and was treated with another debulking surgery, followed by 8 cycles of liposomal doxorubicin. Her second recurrence occurred 2 years later, when she had another debulking surgery and autologous stem cell transplant, with a conditioning regimen of melphalan, cyclophosphamide, and paclitaxel. She had a second infusion of autologous stem cells shortly after the first one, conditioned by mitoxantrone and melphalan. She remained in remission for 3 years, then received 4 cycles of imatinib on a clinical trial. Upon progression, she was enrolled onto another clinical trial with sorafenib and bevacizumab and remained on study for 21 months. She was enrolled on our study when a CT scan of her abdomen and pelvis showed retroperitoneal disease (largest lesion, 3.6 cm). She remained stable for 4.5 months before disease progressed. She went on to receive palliative radiation and then surgical resection of a pelvic mass. She then had cisplatin and gemcitabine for 4 cycles. This had to be discontinued for cytopenias. She died 3 years after going off study.
We also report here further follow-up from a patient previously reported on the previous study of PANVAC (2). She is a 53-year-old with ovarian cancer originally diagnosed as stage III-A one year prior to her enrollment (patient 25 on that study). The treatment on that study was identical to the study reported here. She had undergone debulking followed by 6 cycles of carboplatin and paclitaxel. A second-look operation demonstrated microscopic residual disease, for which she received 4 cycles of intraperitoneal cisplatin. She enrolled on the previous study 4 months later with no radiographic evidence of disease and normal levels of CA-125 (3 U/mL). She was taken off study after 38 months when slowly rising CA-125 levels suggested recurrent disease. CT scan showed no evidence of recurrent disease; however, a small focus of uptake in the pelvis on PET scan suggested possible recurrence. When she went off study, her CA-125 was 15.4 U/mL, which was within normal range.
Immune response
Two HLA-A2+ ovarian cancer patients on study for 2 months were evaluable by ELISPOT assay, which revealed no significant changes in either CEA or MUC-1 without in vitro stimulation however with in vitro stimulation with HLA-A2 restricted CEA and MUC-1 peptides for 72 hours, 1 of 2 patients (pt 14) had an increase in CEA specific T-cells of 2.7 fold. Sufficient PBMCs were available from 8 patients for Treg evaluation (Table 4). Three patients (patients 7, 10, and 14) had increases in T effector:Treg ratios.
Discussion
This follow-up study was designed to evaluate the clinical outcome of therapy with PANVAC vaccine in metastatic breast and ovarian cancer patients. The first safety study consisted of 25 patients with metastatic GI, lung, breast, and ovarian malignancies (2).
In the study reported here, some patients who had limited tumor burden and whose immune system was not compromised by multiple rounds of prior chemotherapy appeared to benefit from the vaccine. Patient 24, with metastatic breast cancer, had her last chemotherapy 12 months prior to enrollment on study, with minimal hilar and mediastinal lymphadenopathy at the time of her first vaccine. She had a 50% reduction in the diameter of her lymph nodes after 10 months of vaccine, followed by complete radiographic resolution of disease by 18 months, and remains on study after 37 months with no sign of progression. While anecdotal findings must not be over interpreted, it is interesting to note that this patient, who has had a prolonged CR, also had the best CD4 response (Table 4). Due to limited pre-vaccination sample, a comparative analysis of CD8 immune response following in vitro stimulation could not be performed. At baseline, all patients tested had no evidence of CEA specific T-cells following IVS (lower limit of detection 1 in 200,000 PBMC). However, it is interesting to note that by day 71 following vaccine, she had 5 times that number of CEA specific T-cells. Another patient from the previous study (2) had advanced ovarian cancer, with no radiographic evidence of disease at the time of enrollment and a normal CA-125 level. She remained on study for 38 months before eventually progressing.
As previously reported, another patient from the prior study was a 42-year-old with stage III-C clear cell ovarian cancer. She had a substantial clinical response to PANVAC, with normalization of rapidly rising CA-125 (> 300 U/mL) and resolution of symptomatic ascites (2).
Median time to progression for patients on study was 2.5 months (breast cancer) and 2.0 months (ovarian cancer). The majority of patients had widely metastatic disease and a history of multiple lines of chemotherapy. Our findings agree with others that suggest RECIST may not be the best tool to measure clinical response in cancer vaccine studies (22-25). Many of our patients had progressed at or before their first scheduled restaging. As previously demonstrated, it takes at least a few months to mount an optimal immune response by vaccination, which is usually shorter than the interval between the initiation of immune therapy and the first restaging. Therefore, the reported progression may not truly represent the effect of vaccine therapy, but may reflect an ongoing process before immune activation (26, 27). Overall survival, rather than time to progression or tumor shrinkage, may be a more relevant endpoint in evaluating the effects of immunotherapies. Sipuleucel-T, the dendritic-cell vaccine for prostate cancer, failed to show a significant improvement in progression-free survival in advanced prostate cancer patients, but demonstrated an absolute overall survival benefit over placebo, despite a cross-over of more than 70% of patients in the placebo arm (27, 28). This result was reproduced in a larger study randomizing 512 patients with metastatic androgen-insensitive prostate cancer to either sipuleucel-T or placebo. There was a 4-month difference in median overall survival favoring the vaccine arm, with no significant delay in time to objective disease progression (24). Similar findings were reported (25) in a randomized, placebo (empty vector)-controlled, multicenter study employing another TRICOM-based vaccine in patients with metastatic castration-resistant prostate cancer. While no difference was observed in time to progression in both arms, patients receiving PSA-TRICOM (Prostvac) vaccine had an improved median overall survival of 8.5 months and a 44% reduction in death rate vs. the control arm. A discordance between median time to progression vs. survival has also recently been reported (29) in patients with metastatic melanoma receiving anti-CTLA-4 monoclonal antibody.
Some patients in the present study continued to show very good clinical response to subsequent therapies after coming off study. There is accumulating evidence that once a cancer vaccine provokes an immune response in the host, it may initiate a prolonged dynamic process leading to marked responses to subsequent therapies (2, 22, 30, 31). This may be a function of a number of mechanisms, including tumor phenotype alteration and antigen cascade. Also, subsequent therapies (i.e., chemotherapy or radiation therapy) may reduce suppressor cell populations, allowing for the enhancement of T-cell responses (22, 30, 32). However, some chemotherapies may be more likely to lead to immunologically relevant tumor-cell killing (33).
Future cancer vaccine studies should consider new endpoints and select patients with less aggressive tumors in the earlier stages of disease. Several studies have suggested that patients with more advanced disease or more heavily pretreated with chemotherapy may be less likely to mount immune responses or derive clinical benefit from therapeutic vaccines (34-37). Indeed PANVAC has been tested in patients with metastatic colorectal cancer rendered without evidence of disease surgically (i.e., low disease volume) with substantial improvements in overall survival compared with concurrent controls (38). Vaccines used in the adjuvant setting in breast cancer patients with early-stage disease and high-risk features, or in ovarian cancer patients with a rise in CA-125 and no evidence of metastatic disease, may confer more clinical benefit than in patients with more advanced, chemotherapy-refractory disease. An approach that may provide improved immune responses and clinical benefit is the combination of vaccines with conventional cancer treatments such as chemotherapy, monoclonal antibodies, small-molecule targeted therapies, or radiation. An ongoing randomized study in patients with metastatic breast cancer (39) is providing preliminary evidence of patient benefit in patients receiving PANVAC vaccine plus docetaxel vs. docetaxel alone. In these combinations, the enhanced effect of active immunotherapy may be a result of different mechanisms, including alteration of tumor-cell phenotype and microenvironment, better antigen presentation, and inhibition of Tregs (40-45).
Supplementary Material
1
Translational Relevance.
With the first FDA-approved therapeutic cancer vaccine providing definitive proof-of-concept for this class of agents, a further understanding of the types of patients most likely to benefit from therapeutic cancer vaccines is crucial. This trial provides additional insight into the potential of a therapeutic vaccine to lead to improved outcomes in select patients and supports the use of vaccines in patients with low tumor burden and minimal prior chemotherapy. This has implications for both the selection of patient populations for clinical trials utilizing therapeutic cancer vaccines as single agents, and also for timing of vaccine relative to other available therapeutics. The sustained complete response in a patient who remains on study for over 3 years also underscores the potential for therapeutic vaccines to provide patient benefit without toxicity. Further studies in appropriate patient populations may provide more insight into how to maximize the potential of therapeutic vaccines as monotherapy.
Acknowledgments
The authors acknowledge the Intramural Research Program of the NIH, National Cancer Institute, Center for Cancer Research for their support of this study. We also express appreciation to the professionals at the NIH Clinical Center Department of Transfusion Medicine for their role in apheresis procedures for study patients, and to the Medical Oncology fellows at the NCI for their attention to patient care. Finally, we thank Bonnie L. Casey and Debra Weingarten for their editorial assistance in the preparation of this manuscript.
References
- 1.Hodge JW, Grosenbach DW, Aarts WM, Poole DJ, Schlom J. Vaccine therapy of established tumors in the absence of autoimmunity. Clin Cancer Res. 2003;9:1837–49. [PubMed] [Google Scholar]
- 2.Gulley JL, Arlen PM, Tsang KY, Yokokawa J, Palena C, Poole DJ, et al. Pilot study of vaccination with recombinant CEA-MUC-1-TRICOM poxviral-based vaccines in patients with metastatic carcinoma. Clin Cancer Res. 2008;14:3060–9. doi: 10.1158/1078-0432.CCR-08-0126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Essajee S, Kaufman HL. Poxvirus vaccines for cancer and HIV therapy. Expert Opin Biol Ther. 2004;4:575–88. doi: 10.1517/14712598.4.4.575. [DOI] [PubMed] [Google Scholar]
- 4.Karsten U, von Mensdorff-Pouilly S, Goletz S. What makes MUC1 a tumor antigen? Tumour Biol. 2005;26:217–20. doi: 10.1159/000086956. [DOI] [PubMed] [Google Scholar]
- 5.Duraisamy S, Kufe T, Ramasamy S, Kufe D. Evolution of the human MUC1 oncoprotein. Int J Oncol. 2007;31:671–7. [PubMed] [Google Scholar]
- 6.Raina D, Ahmad R, Joshi MD, Yin L, Wu Z, Kawano T, et al. Direct targeting of the mucin 1 oncoprotein blocks survival and tumorigenicity of human breast carcinoma cells. Cancer Res. 2009;69:5133–41. doi: 10.1158/0008-5472.CAN-09-0854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khodarev NN, Pitroda SP, Beckett MA, MacDermed DM, Huang L, Kufe DW, et al. MUC1-induced transcriptional programs associated with tumorigenesis predict outcome in breast and lung cancer. Cancer Res. 2009;69:2833–7. doi: 10.1158/0008-5472.CAN-08-4513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Benchimol S, Fuks A, Jothy S, Beauchemin N, Shirota K, Stanners CP. Carcinoembryonic antigen, a human tumor marker, functions as an intercellular adhesion molecule. Cell. 1989;57:327–34. doi: 10.1016/0092-8674(89)90970-7. [DOI] [PubMed] [Google Scholar]
- 9.Marshall J. Carcinoembryonic antigen-based vaccines. Semin Oncol. 2003;30:30–6. doi: 10.1016/s0093-7754(03)00233-1. [DOI] [PubMed] [Google Scholar]
- 10.Hodge JW, Sabzevari H, Yafal AG, Gritz L, Lorenz MG, Schlom J. A triad of costimulatory molecules synergize to amplify T-cell activation. Cancer Res. 1999;59:5800–7. [PubMed] [Google Scholar]
- 11.Grosenbach DW, Barrientos JC, Schlom J, Hodge JW. Synergy of vaccine strategies to amplify antigen-specific immune responses and antitumor effects. Cancer Res. 2001;61:4497–505. [PubMed] [Google Scholar]
- 12.Hodge JW, Chakraborty M, Kudo-Saito C, Garnett CT, Schlom J. Multiple costimulatory modalities enhance CTL avidity. J Immunol. 2005;174:5994–6004. doi: 10.4049/jimmunol.174.10.5994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hodge JW, McLaughlin JP, Kantor JA, Schlom J. Diversified prime and boost protocols using recombinant vaccinia virus and recombinant non-replicating avian pox virus to enhance T-cell immunity and antitumor responses. Vaccine. 1997;15:759–68. doi: 10.1016/s0264-410x(96)00238-1. [DOI] [PubMed] [Google Scholar]
- 14.Marshall JL, Hoyer RJ, Toomey MA, Faraguna K, Chang P, Richmond E, et al. Phase I study in advanced cancer patients of a diversified prime-and-boost vaccination protocol using recombinant vaccinia virus and recombinant nonreplicating avipox virus to elicit anti-carcinoembryonic antigen immune responses. J Clin Oncol. 2000;18:3964–73. doi: 10.1200/JCO.2000.18.23.3964. [DOI] [PubMed] [Google Scholar]
- 15.Kaufman HL, Wang W, Manola J, DiPaola RS, Ko YJ, Sweeney C, et al. Phase II randomized study of vaccine treatment of advanced prostate cancer (E7897): a trial of the Eastern Cooperative Oncology Group. J Clin Oncol. 2004;22:2122–32. doi: 10.1200/JCO.2004.08.083. [DOI] [PubMed] [Google Scholar]
- 16.Kass E, Panicali DL, Mazzara G, Schlom J, Greiner JW. Granulocyte/macrophage-colony stimulating factor produced by recombinant avian poxviruses enriches the regional lymph nodes with antigen-presenting cells and acts as an immunoadjuvant. Cancer Res. 2001;61:206–14. [PubMed] [Google Scholar]
- 17.Madan RA, Arlen PM, Gulley JL. PANVAC-VF: poxviral-based vaccine therapy targeting CEA and MUC1 in carcinoma. Expert Opin Biol Ther. 2007;7:543–54. doi: 10.1517/14712598.7.4.543. [DOI] [PubMed] [Google Scholar]
- 18.Gulley J, Chen AP, Dahut W, Arlen PM, Bastian A, Steinberg SM, et al. Phase I study of a vaccine using recombinant vaccinia virus expressing PSA (rV-PSA) in patients with metastatic androgen-independent prostate cancer. Prostate. 2002;53:109–17. doi: 10.1002/pros.10130. [DOI] [PubMed] [Google Scholar]
- 19.Arlen P, Tsang KY, Marshall JL, Chen A, Steinberg SM, Poole D, et al. The use of a rapid ELISPOT assay to analyze peptide-specific immune responses in carcinoma patients to peptide vs. recombinant poxvirus vaccines. Cancer Immunol Immunother. 2000;49:517–29. doi: 10.1007/s002620000145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Britten CM, Meyer RG, Kreer T, Drexler I, Wolfel T, Herr W. The use of HLA-A*0201-transfected K562 as standard antigen-presenting cells for CD8(+) T lymphocytes in IFN-gamma ELISPOT assays. J Immunol Methods. 2002;259:95–110. doi: 10.1016/s0022-1759(01)00499-9. [DOI] [PubMed] [Google Scholar]
- 21.Yokokawa J, Cereda V, Remondo C, Gulley JL, Arlen PM, Schlom J, et al. Enhanced functionality of CD4+CD25(high)FoxP3+ regulatory T cells in the peripheral blood of patients with prostate cancer. Clin Cancer Res. 2008;14:1032–40. doi: 10.1158/1078-0432.CCR-07-2056. [DOI] [PubMed] [Google Scholar]
- 22.Schlom J, Arlen PM, Gulley JL. Cancer vaccines: moving beyond current paradigms. Clin Cancer Res. 2007;13:3776–82. doi: 10.1158/1078-0432.CCR-07-0588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Finke LH, Wentworth K, Blumenstein B, Rudolph NS, Levitsky H, Hoos A. Lessons from randomized phase III studies with active cancer immunotherapies-- outcomes from the 2006 meeting of the Cancer Vaccine Consortium (CVC) Vaccine. 2007;25(Suppl 2):B97–B109. doi: 10.1016/j.vaccine.2007.06.067. [DOI] [PubMed] [Google Scholar]
- 24.Kantoff PW, Higano CS, Shore ND, Berger ER, Small EJ, Penson DF, et al. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N Engl J Med. 2010;363:411–22. doi: 10.1056/NEJMoa1001294. [DOI] [PubMed] [Google Scholar]
- 25.Kantoff PW, Schuetz TJ, Blumenstein BA, Glode LM, Bilhartz DL, Wyand M, et al. Overall survival analysis of a phase II randomized controlled trial of a Poxviral-based PSA-targeted immunotherapy in metastatic castration-resistant prostate cancer. J Clin Oncol. 2010;28:1099–105. doi: 10.1200/JCO.2009.25.0597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Small EJ, Fratesi P, Reese DM, Strang G, Laus R, Peshwa MV, et al. Immunotherapy of hormone-refractory prostate cancer with antigen-loaded dendritic cells. J Clin Oncol. 2000;18:3894–903. doi: 10.1200/JCO.2000.18.23.3894. [DOI] [PubMed] [Google Scholar]
- 27.Higano CS, Schellhammer PF, Small EJ, Burch PA, Nemunaitis J, Yuh L, et al. Integrated data from 2 randomized, double-blind, placebo-controlled, phase 3 trials of active cellular immunotherapy with sipuleucel-T in advanced prostate cancer. Cancer. 2009;115:3670–9. doi: 10.1002/cncr.24429. [DOI] [PubMed] [Google Scholar]
- 28.Small EJ, Schellhammer PF, Higano CS, Redfern CH, Nemunaitis JJ, Valone FH, et al. Placebo-controlled phase III trial of immunologic therapy with sipuleucel-T (APC8015) in patients with metastatic, asymptomatic hormone refractory prostate cancer. J Clin Oncol. 2006;24:3089–94. doi: 10.1200/JCO.2005.04.5252. [DOI] [PubMed] [Google Scholar]
- 29.Hodi FS, O’Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363:711–23. doi: 10.1056/NEJMoa1003466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gribben JG, Ryan DP, Boyajian R, Urban RG, Hedley ML, Beach K, et al. Unexpected association between induction of immunity to the universal tumor antigen CYP1B1 and response to next therapy. Clin Cancer Res. 2005;11:4430–6. doi: 10.1158/1078-0432.CCR-04-2111. [DOI] [PubMed] [Google Scholar]
- 31.Petrylak D. Defining the optimal role of immunotherapy and chemotherapy: advanced prostate cancer patients who receive sipuleucel-T (PROVENGE) followed by docetaxel derive greatest survival benefit [abstract]; Chemotherapy Foundation Symposium 14th Annual Meeting; November 2006. [Google Scholar]
- 32.Arlen PM, Gulley JL, Parker C, Skarupa L, Pazdur M, Panicali D, et al. A randomized phase II study of concurrent docetaxel plus vaccine versus vaccine alone in metastatic androgen-independent prostate cancer. Clin Cancer Res. 2006;12:1260–9. doi: 10.1158/1078-0432.CCR-05-2059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zitvogel L, Kepp O, Kroemer G. Immune parameters affecting the efficacy of chemotherapeutic regimens. Nat Rev Clin Oncol. 2011;8:151–60. doi: 10.1038/nrclinonc.2010.223. [DOI] [PubMed] [Google Scholar]
- 34.Gulley JL, Madan RA, Schlom J. Impact of tumour volume on the potential efficacy of therapeutic vaccines. Curr Oncol. 2011;18:e150–7. doi: 10.3747/co.v18i3.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.von Mehren M, Arlen P, Gulley J, Rogatko A, Cooper HS, Meropol NJ, et al. The influence of granulocyte macrophage colony-stimulating factor and prior chemotherapy on the immunological response to a vaccine (ALVAC-CEA B7.1) in patients with metastatic carcinoma. Clin Cancer Res. 2001;7:1181–91. [PubMed] [Google Scholar]
- 36.Harrop R, Shingler WH, McDonald M, Treasure P, Amato RJ, Hawkins RE, et al. MVA-5T4-induced immune responses are an early marker of efficacy in renal cancer patients. Cancer Immunol Immunother. 2011;60:829–37. doi: 10.1007/s00262-011-0993-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gulley JL, Arlen PM, Madan RA, Tsang KY, Pazdur MP, Skarupa L, et al. Immunologic and prognostic factors associated with overall survival employing a poxviral-based PSA vaccine in metastatic castrate-resistant prostate cancer. Cancer Immunol Immunother. 2010;59:663–74. doi: 10.1007/s00262-009-0782-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Morse M, Niedzwiecki D, Marshall J, Garnett CR, Chang DZ, Aklilu M, et al. Survival rates among patients vaccinated following resection of colorectal cancer metastases in a Phase II randomized study compared with contemporary controls. American Society of Clinical Oncology 2011 Annual Meeting J Clin Oncol. 2011;29(suppl) abstr 3557. [Google Scholar]
- 39.Arlen PM, Pazdur M, Skarupa L, Rauckhorst M, Gulley JL. A randomized phase II study of docetaxel alone or in combination with PANVAC-V (vaccinia) and PANVAC-F (fowlpox) in patients with metastatic breast cancer (NCI 05-C-0229) Clin Breast Cancer. 2006;7:176–9. doi: 10.3816/CBC.2006.n.032. [DOI] [PubMed] [Google Scholar]
- 40.Curiel TJ, Coukos G, Zou L, Alvarez X, Cheng P, Mottram P, et al. Specific recruitment of regulatory T cells in ovarian carcinoma fosters immune privilege and predicts reduced survival. Nat Med. 2004;10:942–9. doi: 10.1038/nm1093. [DOI] [PubMed] [Google Scholar]
- 41.Kawaida H, Kono K, Takahashi A, Sugai H, Mimura K, Miyagawa N, et al. Distribution of CD4+CD25high regulatory T-cells in tumor-draining lymph nodes in patients with gastric cancer. J Surg Res. 2005;124:151–7. doi: 10.1016/j.jss.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 42.Chakraborty M, Abrams SI, Camphausen K, Liu K, Scott T, Coleman CN, et al. Irradiation of tumor cells up-regulates Fas and enhances CTL lytic activity and CTL adoptive immunotherapy. J Immunol. 2003;170:6338–47. doi: 10.4049/jimmunol.170.12.6338. [DOI] [PubMed] [Google Scholar]
- 43.Garnett CT, Palena C, Chakraborty M, Tsang KY, Schlom J, Hodge JW. Sublethal irradiation of human tumor cells modulates phenotype resulting in enhanced killing by cytotoxic T lymphocytes. Cancer Res. 2004;64:7985–94. doi: 10.1158/0008-5472.CAN-04-1525. [DOI] [PubMed] [Google Scholar]
- 44.Machiels JP, Reilly RT, Emens LA, Ercolini AM, Lei RY, Weintraub D, et al. Cyclophosphamide, doxorubicin, and paclitaxel enhance the antitumor immune response of granulocyte/macrophage-colony stimulating factor-secreting whole-cell vaccines in HER-2/neu tolerized mice. Cancer Res. 2001;61:3689–97. [PubMed] [Google Scholar]
- 45.Garnett CT, Schlom J, Hodge JW. Combination of docetaxel and recombinant vaccine enhances T-cell responses and antitumor activity: effects of docetaxel on immune enhancement. Clin Cancer Res. 2008;14:3536–44. doi: 10.1158/1078-0432.CCR-07-4025. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
1