Mesenteric fat as a source of C reactive protein and as a target for bacterial translocation in Crohn's disease (original) (raw)
Abstract
Objective
Mesenteric fat hyperplasia is a hallmark of Crohn's disease (CD), and C reactive protein (CRP) is correlated with disease activity. The authors investigated whether mesenteric adipocytes may be a source of CRP in CD and whether inflammatory and bacterial triggers may stimulate its production by adipocytes.
Design
CRP expression in the mesenteric and subcutaneous fats of patients with CD and the correlation between CRP plasma concentrations and mesenteric messenger RNA (mRNA) levels were assessed. The impact of inflammatory and bacterial challenges on CRP synthesis was tested using an adipocyte cell line. Bacterial translocation to mesenteric fat was studied in experimental models of colitis and ileitis and in patients with CD.
Results
CRP expression was increased in the mesenteric fat of patients with CD, with mRNA levels being 80±40 (p<0.05) and 140±65 (p=0.04) times higher than in the mesenteric fat of patients with ulcerative colitis and in the subcutaneous fat of the same CD subjects, respectively, and correlated with plasma levels. Escherichia coli (1230±175-fold, p<0.01), lipopolysaccharide (26±0.5-fold, p<0.01), tumour necrosis factor α (15±0.3-fold, p<0.01) and interleukin-6 (10±0.7-fold, p<0.05) increased CRP mRNA levels in adipocyte 3T3-L1 cells. Bacterial translocation to mesenteric fat occurred in 13% and 27% of healthy and CD subjects, respectively, and was increased in experimental colitis and ileitis. Human mesenteric adipocytes constitutively expressed mRNA for TLR2, TLR4, NOD1 and NOD2.
Conclusion
Mesenteric fat is an important source of CRP in CD. CRP production by mesenteric adipocytes may be triggered by local inflammation and bacterial translocation to mesenteric fat, providing a mechanism whereby mesenteric fat hyperplasia may contribute to inflammatory response in CD.
Keywords: C Reactive protein; mesenteric fat; bacterial translocation; Crohn's disease; IBD basic research; 6-mercaptopurine; bacterial translocation; IBD; thiopurine methyltransferase; antibacterial peptide; IBD models; azathioprine; IBD clinical; 2,4,6-trinitrobenzene sulfonic acid; acute hepatitis; alcoholic liver disease; anti-bacterial mucosal immunity; gut inflammation; anti-bacterial peptide; antibiotic therapy; antibiotics: clinical trials; bacteraemia; bacterial overgrowth; bacterial translocation; bacterial infection; bacterial pathogenesis; bacterial adherence; crohn's disease; TNF-alpha; ulcerative colitis; small intestine; cell biology; inflammatory bowel disease; mucosal immunology; Helicobacter pylori; non-ulcer dyspepsia; genetic polymorphisms; gastric neoplasia; non-alcoholic steatohepatitis; gut inflammation; alcoholic liver disease; cytokines
Significance of this study.
What is already known on this subject?
- Mesenteric fat hyperplasia is a characteristic feature of Crohn's disease (CD).
- Adipocytes are an extrahepatic source of C reactive protein (CRP) in humans.
- Increased mesenteric fat density correlates with serum CRP levels in CD.
What are the new findings?
- Mesenteric fat is an important source of CRP in CD.
- CRP production by mesenteric adipocytes is triggered by inflammatory and bacterial stimuli.
- Bacterial translocation to mesenteric adipocytes occurs at a rate similar to that for the translocation of mesenteric lymph nodes in CD.
How might it impact on clinical practice in the foreseeable future?
- These data further establish the role of adipose tissue as a contributor to inflammatory response in CD and provide a rationale for targeting mesenteric fat in the treatment of this chronic disorder.
Introduction
C reactive protein (CRP) was first discovered in 1930 in the serum of patients with pneumonia.1 Its name was derived from its ability to react to the cell wall C polypeptide of Streptococcus pneumoniae.1 For over 75 years, CRP has been extensively used in the clinic as a non-specific systemic marker of inflammation2 and is considered as one of the most important biomarkers in Crohn's disease (CD). High serum concentrations of CRP in CD have been associated with poor prognosis,3 a high response rate to anti-tumour necrosis factor (TNF) treatment4 and an increased risk of relapse following withdrawal of medical therapies.5
Mesenteric fat hyperplasia is a characteristic feature of CD that is not found in ulcerative colitis (UC).6 While the liver has long been considered as the unique source of CRP,2 recent evidence indicates that adipocytes may represent an extrahepatic source of CRP in humans.7 Body mass index has been correlated with plasma CRP levels in obese patients.8 Increased mesenteric fat density evaluated by CT enterography was found to correlate with serum CRP levels in patients with CD.9
The regulatory mechanisms of CRP synthesis by the liver include interleukin (IL)-6 as a potent inducer of its expression in humans.10 TNFα and IL-6 are the main pro-inflammatory cytokines secreted by the adipose tissue, suggesting that local inflammation within mesenteric fat may contribute to increased levels of CRP in CD.11 Furthermore, CD is characterised by increased intestinal permeability and bacterial translocation,12 and fat cells are able to respond to bacterial components.13 Recent studies have demonstrated that adipocytes can respond to bacterial challenge by constitutively expressing a broad set of pattern recognition molecules (PRMs), including Toll-like receptors (TLRs) 1–11, nucleotide oligomerisation domain (NOD) 1 and NOD2.13–16 We thus speculated that an increased cytokine production in the inflamed mesentery, together with translocating bacteria, may trigger CRP production by mesenteric adipocytes in CD and contribute to its elevated serum levels.
The aims of this study were therefore to investigate the production of CRP by mesenteric adipocytes in patients with CD and in controls and to assess in vitro and in vivo the effects of inflammatory and bacterial stimuli on CRP synthesis by adipocytes.
Materials and methods
See supplemental material.
Patients and controls
Twenty-two patients with CD (mean age at the time of surgery: 32 years; male patients=14; pure ileal disease=11; ileocolonic disease=10; pure colonic disease=1; non-stricturing non-penetrating phenotype=7; structuring phenotype=12; penetrating phenotype=3; perianal disease=6; patients on azathioprine at the time of surgery =9), 17 patients with UC (mean age at the time of surgery: 42 years; male patients=7; patients on azathioprine at the time of surgery =5) and 21 controls (19 patients with colorectal neoplasia and 2 patients operated on for diverticulitis) who underwent surgery were prospectively included. All patients from the ‘diverticulitis’ group were operated on a few weeks after experiencing diverticulitis, and all adipose tissue biopsies were taken away from inflammatory lesions. All patients gave written informed consent, and the study protocol was approved by the local committee. The diagnosis of CD or UC was based on the usual criteria.17 All subjects were of normal weight (defined as 20 kg/m2<body mass index<5 kg/m2), had no personal history of diabetes mellitus and were not being treated with specific medications known to modulate visceral fat (infliximab, steroids and metformin18). Patients with CD underwent right ileocolectomy for symptomatic ileal stenosis or fistula. Patients with UC underwent colonic resection for disease refractory to standard treatment. Subcutaneous/mesenteric fat specimens were taken during surgery, and ileal and colonic transparietal biopsies were performed. Ethical guidelines in studies on humans were followed under the supervision of an investigator, and human samples were declared to Inserm according to French laws (articles L. 1243-3 and R. 1243-49, and the Code de la Santé Publique).
Adipose tissues and intestinal specimen
Specimens of mesenteric and subcutaneous adipose tissues, healthy and inflamed colonic samples, and healthy and inflamed terminal ileal samples were taken during surgery. Histological evaluation was performed to confirm the absence of inflammation on intestinal biopsies and to select fat specimens at a distance from mesenteric lymph nodes. Intestinal biopsies were immediately frozen in liquid nitrogen and stored at −80°C for messenger RNA (mRNA) and protein analyses. Three samples of mesenteric and subcutaneous fats were collected. One sample was fixed in 4% paraformaldehyde/phosphate-buffered formalin and embedded in paraffin for immunostaining. The second sample was immediately frozen in liquid nitrogen and stored at −80°C for mRNA and protein analyses. The third sample was taken under sterile conditions at the time of surgery and placed in normal saline for a short-term culture.
3T3-L1 cells
3T3-L1 pre-adipocytes (ATCC CL-173) were grown to confluence in Dulbecco's modified Eagle's medium (DMEM; Gibco Invitrogen, Grand Island, New York, USA) with 10% fetal calf serum (Eurobio, Paris, France) and penicillin and streptomycin (Gibco). The medium was supplemented with 1 M dexamethasone (Merck, Darmstadt, Germany), 0.2 mM isobutyl methyl xanthine (Gibco), 10 g/ml insulin (Actrapid; NovoNordisk, Bagsvaerd, Denmark) and 10% fetal calf serum (Eurobio) for 48 h.19 Cell viability was confirmed by testing lactate dehydrogenase activity in the culture medium taken during the course of the differentiation process or on mature 3T3-L1 cells. Adipogenesis was confirmed by staining fat droplets with oil red O (Acros Organics, Geel, Belgium), which made lipid accumulation visible (the hallmark of adipogenic conversion), and by measuring the synthesis of aP2 mRNA, an adipocyte-specific gene and well-established marker for terminal adipocyte differentiation.
Cytokine and bacterial challenge
To investigate the regulation of CRP expression in vitro, we stimulated differentiated 3T3-L1 cells with optimal concentrations of recombinant TNFα (50 ng/ml) or IL-6 (10 ng/ml)20 (Sigma-Aldrich, St Quentin Fallavier, France), lipopolysaccharide (LPS) (100 ng/ml; Invitrogen, Villebon sur Yvette, France), lipopeptide Pam3Cys (1 μg/ml) or muramyl dipeptide (10 μg/ml; Calbiochem, Fontenay sous bois, France) for 3, 6, 9, 12 or 24 h.19–21 3T3-L1 cells were also infected with Escherichia coli previously isolated from the mesenteric fat biopsy specimens of a CD patient or with Lactobacillus spp. (infectivity ratio: 100 bacteria/cell) for 90 min. Cell viability was assessed at the end of infection before cell washing in 1.0 ml of sterile phosphate-buffered saline and treatment with DMEM with gentamicin (10 μg/ml; Gibco) for 24 h.
CRP release in short-term cultures of human adipose tissue
Short-term cultures were prepared with surgical specimens to examine the release of CRP from mesenteric and subcutaneous fats, as previously described.22 Briefly, adipose tissue samples were diced finely into 1–2 mm pieces (150 mg, wet weight) and washed twice in Hanks' balanced salt solution containing 0.2% bovine serum albumin. Samples were placed in sterile tissue culture plates containing 2 ml of DMEM supplemented with 10% fetal bovine serum and antibiotics (penicillin and streptomycin) at 37°C under an atmosphere of air/CO2 (95:5, vol/vol) for 24 h. CRP concentration in the cultured adipose tissue supernatant was determined by enzyme-linked immunosorbent assay (R&D Systems, UK).
Determination of blood CRP concentrations
Blood samples were collected 1 day before surgery. Serum CRP was quantified using a highly sensitive immunoassay (Cortecnet, Paris, France).
Bacterial translocation to mesenteric adipose tissue and lymph nodes
Human samples
During surgery, mesenteric lymph nodes and mesenteric adipose tissue samples were immediately introduced in 8 ml of pre-weighed cysteinated 1/4 strength Ringer solution containing 0.5% Tween 80 (Flandre-Chimie, Villeneuve d'Ascq, France). The samples were transported to the laboratory within 2 h and treated immediately, weight was established and tissues were disrupted. Five milliliters of the suspension was inoculated in 100 ml flasks containing cysteinated brain–heart enrichment broth (detection level at about 2 bacteria/g), and 1 ml was inoculated in 10 ml of the same broth (detection level at about 10 bacteria/g). Enrichment broths were incubated under anaerobic conditions for 10 days, with regular checking of growth. About 0.1 ml of the samples was placed on two plates of Columbia blood agar: one plate was incubated under aerobic conditions for 48 h, and the second plate was incubated under anaerobic conditions for 7 days. Two further 10-fold dilutions were plated in the same manner. Positive enrichment broths were subcultured on anaerobic Columbia blood agar plates.23
Animal samples
Mesenteric lymph nodes and mesenteric adipose tissue samples were immediately introduced in 1.5 ml of cysteinated 1/4 strength Ringer solution in pre-weighed tubes. Weight was established, and samples were disrupted. One milliliter of the suspension was introduced in 10 ml of cysteinated brain–heart enrichment broth (detection level at about 100 bacteria/g). About 0.1 ml was plated on Columbia blood agar and incubated for 7 days under anaerobic conditions. Subcultures were obtained as described above.23 All animal studies were approved by the local investigational review board. Animal experiments were performed in an accredited establishment (no. B59-35009) according to governmental guidelines (no. 86/609/CEE) under the supervision of an authorised investigator (no. 59-350191).
Statistical analysis
All results are expressed as mean±SEM and analysed by non-parametric Mann–Whitney U test or Kruskal–Wallis test. Paired comparisons were analysed by Wilcoxon matched pairs test. Pearson's correlation coefficient (r) was used to evaluate associations between two variables. Fisher's exact test was used to analyse categorical data when sample sizes were small. Differences were judged as statistically significant if the p value was less than 0.05.
Results
CRP is overexpressed in CD mesenteric adipose tissue
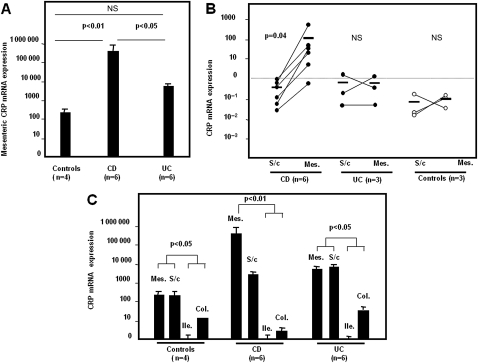
With real-time PCR, CRP mRNA was detected in all tissues analysed, that is, in ileal and colonic samples, as well as in mesenteric and subcutaneous adipose tissues. We first compared the expressions of CRP in adipose tissues taken from UC, CD and control subjects (figure 1A). The CRP gene was overexpressed in the mesenteric fat of patients with CD (n=6), with mRNA levels being 80±40 and 1450±750 times higher than those detected in the mesenteric fat of UC individuals (n=6; p<0.05 vs CD) and controls (n=4; p<0.01 versus CD), respectively (figure 1A). The mRNA levels of CRP within the mesenteric fat of patients with UC were not statistically different from controls (figure 1A). Of note, expression levels of CRP were similar in the ‘diverticulitis’ group and the ‘colorectal neoplasia’ group (data not shown). No statistical difference in CRP mRNA transcripts was seen in subcutaneous fat between patients with CD, patients with UC and controls (data not shown).
Figure 1.
Overexpression of CRP mRNA and protein in mesenteric fat in CD. (A) Comparison of CRP expressions measured by real-time PCR in the mesenteric fat of patients with CD, patients with UC and control individuals. Significantly higher levels of CRP transcript levels were found in patients with CD compared to patients with UC and controls. Results are expressed as mean±SEM. (B) CRP mRNA levels in samples of mesenteric adipose tissue (Mes.) and subcutaneous fat (S/c) taken from the same patients with CD (n=6), patients with UC (n=3) or patients without IBD (n=3). Unlike in UC and control subjects in whom CRP mRNA levels are similar in mesenteric and subcutaneous fats, the CRP gene is overexpressed in mesenteric fat compared to subcutaneous fat in patients with CD. Median values are indicated by the horizontal line. (C) Expression of CRP gene in human mesenteric (Mes.) and subcutaneous (S/c) fat samples and in biopsy specimens of macroscopically and histologically healthy ileum (Ile.) or healthy colon (Col.) obtained from six UC, six CD and four control subjects using real-time PCR. Compared with adipose tissues, a modest (colon) or a weak (ileum) expression of CRP mRNA was observed in intestinal wall samples obtained from patients with UC, patients with CD or controls. Results are expressed as mean±SEM. CD, Crohn's disease; UC, ulcerative colitis; IBD, inflammatory bowel disease.
To further examine the overexpression of CRP in mesenteric adipose tissues in CD, we compared paired CRP mRNA levels in subcutaneous and mesenteric fats in the same patients (figure 1B). In patients with CD, median CRP mRNA levels in mesenteric adipose tissue were 140±65 times higher than those in the subcutaneous adipose tissue of the same CD subjects (p=0.04). In contrast to CD, CRP mRNA levels were broadly similar in subcutaneous and mesenteric adipose tissues in patients with UC and controls (figure 1B).
To determine whether the intestine that is adjacent to mesenteric fat may be another significant local source of CRP in CD, we compared intestinal (small intestine and colon) and adipose tissue CRP mRNA levels. CRP mRNA levels in mesenteric or subcutaneous adipose tissue in the 10 patients without CD (UC, n=6; controls, n=4) were 150±90 times higher than those detected in the intestinal wall of the same patients (p<0.05) (figure 1C). Due in part to mesenteric fat hyperplasia, CRP mRNA levels in the mesenteric adipose tissue of patients with CD (n=6) were higher (217 500±67 500 times) than those detected in the intestinal wall of the same patients (p<0.01) (figure 1C). Of note, low and broadly similar CRP mRNA levels were detected in inflamed or healthy intestine (colon or small bowel) in patients with CD and patients with UC (data not shown), indicating that the enhanced CRP levels in active CD do not come directly from the intestinal wall.
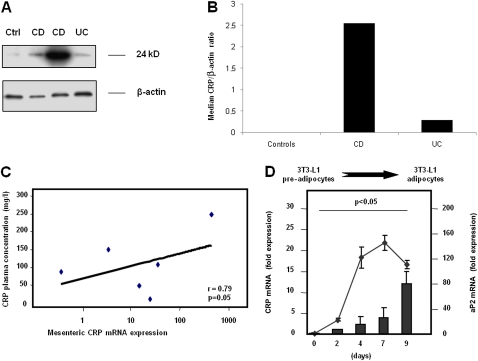
We next investigated CRP expression at the protein level to demonstrate that mesenteric adipocytes may be the main local source of plasma CRP in CD. The overexpression of CRP was confirmed at the protein level by western blot analysis using mesenteric adipose tissue explants (figure 2A); the median CRP/β-actin ratio was 0.01, 2.55 and 0.29 in controls, patients with CD and patients with UC, respectively (figure 2B).
Figure 2.
CRP expression by human mesenteric fat and correlation between mesenteric and plasma CRP concentrations in CD. (A) Levels of CRP by western blot analysis of mesenteric adipose tissue from one control patient who was operated on for colorectal cancer (Ctrl), CD subjects and UC subjects. Actin protein levels were determined to verify equal loading of samples. (B) The median CRP/β-actin ratio by western blot analysis is 0.01, 2.55 and 0.29 in controls (n=4), patients with CD (n=5) and patients with UC (n=4), respectively. (C) Correlation between plasma CRP concentrations measured at surgery and CRP mRNA levels quantified by real-time PCR in mesenteric adipose tissues taken during surgery from six patients with CD. (D) CRP mRNA levels parallel with and aP2 mRNA expression during the 9 days of 3T3-L1 pre-adipocyte differentiation into adipocytes on the indicated days. Results are expressed as fold induction as compared with undifferentiated pre-adipocytes (mean±SEM of three experiments). CD, Crohn's disease; UC, ulcerative colitis.
Collectively, these findings indicate that mesenteric adipose tissue is an important source of CRP in patients with CD.
CRP is released by mesenteric adipose tissue
To investigate whether mesenteric CRP overexpression may be a potential source of CRP in the serum of patients with CD, we evaluated the ability of mesenteric adipose tissue to release CRP and compared CRP mesenteric expression level with plasma CRP level in paired samples of patients with CD.
The release of CRP was detected at levels superior to 1 pg/ml in all culture media collected after a 24 h short-term culture of subcutaneous and mesenteric adipose tissue specimens taken from patients with inflammatory bowel disease (IBD) and controls (data not shown). Plasma CRP concentrations were positively correlated with mesenteric CRP transcript levels (r=0.79, p=0.05) in the six patients with CD (figure 2C), whereas no correlation was observed in UC and control subjects (data not show). Plasma CRP levels were not correlated with the intestinal mRNA levels of CRP in UC, CD and control subjects (data not shown).
Taken together, these results suggest that CRP released by mesenteric fat may be responsible, at least in part, for elevated plasma CRP levels in patients with CD.
CRP expression is enhanced by inflammatory and bacterial stimuli
To better understand the mechanisms that trigger CRP expression by adipocytes, we measured CRP mRNA levels according to the differentiation and activation states of adipocytes.
A 21±2.5-fold induction of CRP mRNA expression was observed during the differentiation of 3T3-L1 pre-adipocytes into adipocytes (p<0.05 vs pre-adipocytes) (figure 2D). The aP2 mRNA level (a well-established marker of terminal adipocyte differentiation) parallelled the increase in CRP mRNA, indicating that CRP expression is dependent on adipocyte differentiation (figure 2D).
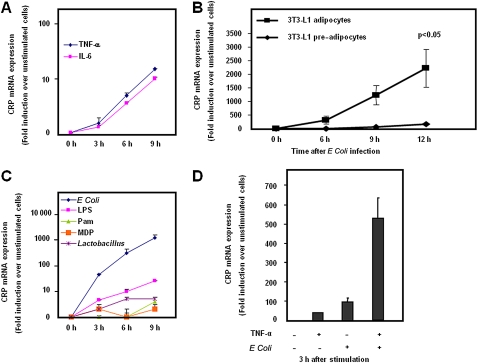
TNFα and IL-6 are the two main pro-inflammatory cytokines secreted by adipose tissue.6 With the use of differentiated 3T3-L1 adipocytes, treatment with TNFα and IL-6 resulted in a 15±0.3-fold and 10±0.7-fold increase in CRP mRNA expression, respectively (figure 3A).
Figure 3.
Induction of CRP expression in 3T3-L1 adipocytes following cytokine and/or bacterial challenge. (A) Differentiated 3T3-L1 adipocytes were stimulated with 10 ng/ml IL-6 or 50 ng/ml TNFα for 24 h. (B) Ability of 3T3-L1 pre-adipocytes and adipocytes to respond to the same bacterial challenge. Cells were infected with a strain of E coli isolated from a CD patient at a multiplicity of 100 pfu/cell for 1 h 30 min. Induction of CRP mRNA expression was then followed over time. (C) Differentiated 3T3-L1 adipocytes were infected with E coli or Lactobacillus spp. (infectivity ratio, 100 bacteria/cell) for 1 h 30 min, or treated with 100 ng/ml LPS, 1 μg/ml Pam3Cys or 10 μg/ml muramyl dipeptide for 24 h. (D) Synergistic effect of bacterial and cytokine stimuli on CRP expression in differentiated 3T3-L1 adipocytes. Cells were pre-treated with 50 ng/ml TNFα for 24 h before infection with E coli (infectivity ratio, 100 bacteria/cell). CRP mRNA expression was measured at 3 h after bacterial infection. In all experiments described in this figure, total RNA was isolated from 3T3-L1 cells at the indicated times, and levels of CRP mRNA were determined by real-time PCR. Results are expressed as the mean±SEM of three independent experiments and fold induction as compared with unstimulated adipocytes. IL, interleukin; LPS, lipopolysaccharide.
Since CD is characterised by increased bacterial translocation,12 we next tested the hypothesis that bacterial components may stimulate CRP synthesis by adipocytes. We first measured the capacity of pre-adipocytes and differentiated adipocytes to express CRP after E coli challenge (figure 3B). While bacterial infection strongly enhanced CRP mRNA expression in adipocytes (2290±700-fold induction over unstimulated cells), the CRP gene expression in pre-adipocytes was only modestly promoted by the same bacterial challenge (120±42-fold induction, p<0.05 vs adipocytes at 12 h) (figure 3B).
E coli infection induced a rapid and dramatic 1230±175-fold increase in CRP mRNA levels, which reached its maximum at 9 h after bacterial infection (figure 3C). Similarly, stimulation of adipocytes with LPS, a structural component of the outer wall of Gram-negative bacteria and a TLR4 ligand, led to a marked and sustained elevation (26±0.5-fold induction and p<0.01 over unstimulated adipocytes) in CRP mRNA levels, which parallelled that of adipocytes challenged with E coli. By contrast, stimulation with lipopeptide Pam3Cys (a TLR2 ligand) or muramyl dipeptide (a NOD2 ligand) had a modest effect or no effect on CRP expression in 3T3-L1 adipocytes, respectively (figure 3C). As controls, 3T3-L1 cells were stimulated with a non-pathogenic Gram-positive Lactobacillus strain, which was not able to significantly enhance CRP synthesis by adipocytes (figure 3C).
Because mesenteric adipocytes might be concomitantly exposed to both inflammatory and bacterial compounds, we next investigated the effects of such stimuli when administered separately or successively. The increase in CRP mRNA levels following challenge with E coli (96±20-fold induction over unstimulated cells) was higher when compared to treatment with TNFα (38±2-fold induction over unstimulated cells) (figure 3D). Interestingly, 3 h after the end of bacterial infection, the production of CRP in TNFα pre-treated 3T3-L1 cells was enhanced synergistically by the addition of E coli (527±104-fold induction over unstimulated cells), as shown in figure 3D.
Overall, CRP biogenesis in adipocytes is strongly inducible by Gram-negative bacteria and enhanced synergistically by pro-inflammatory cytokines.
Bacterial translocation to mesenteric adipocytes is increased during experimental colitis
Since we have shown that bacterial challenge was able to increase CRP synthesis by adipocytes in vitro, we next explored whether bacterial translocation occurred in mesenteric lymph nodes and directly in adipocytes of mesenteric tissue. Bacterial translocation is classically defined as the passage of viable bacteria from the gastrointestinal tract to mesenteric lymph nodes and then to peripheral organs such as the liver and spleen.24 Thus, in all animal experiments, the rate of bacterial translocation to mesenteric lymph nodes was used as an internal control.
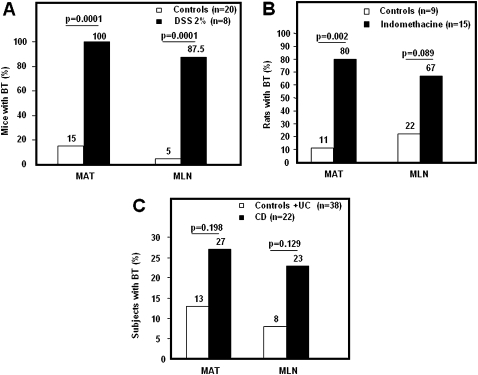
The induction of dextran sulfate sodium (DSS) colitis was confirmed macroscopically and histologically, as previously described.25 Bacterial translocation to mesenteric adipocytes occurred spontaneously in 15% of control mice (n=20) and was significantly enhanced in 100% of animals with DSS-induced colitis (n=8, p=0.0001) (figure 4A). Similarly, significantly higher rates of bacterial translocation to mesenteric lymph nodes were noted in animals receiving 2% DSS (n=8) when compared to control mice (87.5% vs 5%, p=0.0001). The rates of bacterial translocation were broadly similar in mesenteric adipose tissue and mesenteric lymph nodes (100% vs 87.5%, p=NS) in DSS-treated mice, as well as in control animals (15% vs 5%, p=NS) (figure 4A).
Figure 4.
Bacterial translocation to mesenteric adipose tissue following acute DSS-induced colitis in mice, acute indomethacin-induced ileitis in rats and bacterial translocation in humans. (A) Rates of bacterial translocation (BT) to mesenteric adipose tissue (MAT) and mesenteric lymph nodes (MLN) in C57BL/6 mice with acute colitis induced by 2% DSS for 5 days and killed after 2 days on day 7 (n=8) and in control animals (n=20). (B) Rates of bacterial translocation (BT) to mesenteric adipose tissue (MAT) and mesenteric lymph nodes (MLN) in rats with acute ileitis induced by indomethacin (n=15) and in control animals (n=9). (C) Rates of bacterial translocation (BT) to mesenteric adipose tissue (MAT) and mesenteric lymph nodes (MLN) in patients without CD (controls and patients with UC, n=38) and patients with CD (n=22). UC, ulcerative colitis; DSS, dextran sulfate sodium.
Bacterial translocation to mesenteric adipocytes is increased during experimental ileitis
Bacterial translocation may require a bacterial load of >108 organisms per milliliter of faeces.26 Therefore, it is usually assumed that the colon is the main site of bacterial translocation. We thus investigated whether bacterial translocation to mesenteric fat and lymph nodes may also occur in an experimental model of ileitis. The induction of indomethacin-induced ileitis was confirmed macroscopically and histologically, as previously described.27 Bacterial translocation to mesenteric adipose tissue occurred in 80% of indomethacin-treated rats (n=15) compared with 11% of control rats (n=9) (p=0.002) (figure 4B). Higher rates of bacterial translocation to mesenteric lymph nodes were also noted in rats following intraperitoneal administration of indomethacin when compared to control animals (67% vs 22%, p=0.089). The rates of bacterial translocation were broadly similar in mesenteric adipose tissue and mesenteric lymph nodes (80% vs 67%, p=NS) in indomethacin-treated rats, as well as in control animals (11% vs 22%, p=NS) (figure 4B).
Bacterial translocation to mesenteric adipocytes that constitutively express PRMs in humans
We then investigated whether bacterial translocation to mesenteric adipocytes may occur in patients with CD. Consistent with our results in animals, the rate of bacterial translocation to mesenteric adipose tissue was similar to that observed in mesenteric lymph nodes in the 22 patients with CD (27% and 23%, respectively, p=NS) (figure 4C). When compared to control and UC subjects (n=38), the rate of bacterial translocation to mesenteric adipose tissue was higher in the 22 patients with CD, but the difference did not reach statistical significance (13% vs 27%, p=0.198). In line with previous reports,12 the rate of bacterial translocation to mesenteric lymph nodes was also higher in CD individuals than in non-CD individuals (control and UC individuals), even though the difference did not reach statistical significance (23% vs 8%, respectively, p=0.129) (figure 4C). Of note, rates of bacterial translocation did not differ between UC and control subjects, and the results in patients with CD were not influenced by disease behaviour or disease location according to the Montreal classification.28
Consistent with previous reports,14 16 29 human mesenteric adipocytes from control subjects were found to constitutively express a wide range of PRMs, namely TLR2, TLR4, NOD1 and NOD2, at the transcriptional level, thus confirming that mesenteric fat cells can respond to bacterial challenge (web figure 1). Similar mRNA expression levels of TLR2, TLR4, NOD1 and NOD2 were noted in controls, patients with UC and patients with CD (data not shown).
Collectively, our results demonstrate that bacterial translocation to mesenteric adipocytes expressing PRMs occurs physiologically at a rate similar to that of mesenteric lymph nodes in both animals and patients with CD.
Discussion
We identified mesenteric and subcutaneous adipose tissues as sources of CRP in humans at both RNA and protein levels. CRP mRNA and protein were overexpressed in mesenteric fat compared to the subcutaneous adipose tissue of patients with CD. A 140-fold increase in mesenteric CRP expression was noted when comparing the mesenteric and subcutaneous fats of the same CD subjects at the transcriptional level. In addition, a 105-fold higher expression of CRP was observed when comparing the mesenteric fats of CD and control subjects. These findings unravel a dysregulation of CRP expression that is confined to mesenteric fat in CD. These results are in line with a previous report in patients with other chronic inflammatory diseases.30 Of note, this overexpression may have been underestimated in our study, as all real-time PCR results were normalised to the unaffected housekeeping gene β-actin while hyperplasia of mesenteric adipose tissue is present in CD.11 Indeed, the abdominal fat area in CD is composed of a global 4-fold increase in the number of adipocytes as compared to controls, which is related to a reduced size of adipocytes in CD.6 To our knowledge, only one study investigated the expression of CRP in animals.31 In this study, the authors demonstrated for the first time that CRP is expressed by white adipose tissue in mice.31 However, data on an animal model of IBD are not available.
Mucosal lesions on endoscopy are not well correlated to plasma CRP levels in CD,32 suggesting that the intestine may not be the only source of CRP. Indeed, CRP mRNA transcripts were detectable in the intestinal wall of controls, but at much lower levels than in mesenteric fat. Furthermore, this expression was similar in the healthy and inflamed intestines, as well as in patients with CD and patients without CD. Overall, these results indicate that inflammation of the mesentery, resulting in increased CRP production by adipocytes, may be a prominent locoregional source of CRP in patients with CD. We cannot exclude that the liver is a significant source of plasma CRP in CD. A portal venous puncture or liver biopsy—an invasive procedure that we decided to avoid in these patients for ethical reasons—may have been performed to address this issue.
To investigate the regulatory mechanisms of CRP production by adipocytes, we analysed the response of differentiated 3T3-L1 adipocytes to cytokine stimuli. IL-6 is recognised as a potent inducer of CRP production by hepatocytes10 33 and adipocytes.7 Studies using IL-6-deficient mice have demonstrated that IL-6, although necessary, is not sufficient for induced expression of the CRP transgene, and have suggested that other regulators of CRP production exist.34 We found that CRP synthesis was inducible by IL-6 stimulation in vitro. IL-6 produced by the liver may thus contribute to enhancement of CRP synthesis by adipocytes in vivo. We also identified TNFα as a possible inducer of CRP expression in the mouse cell line 3T3-L1. These results should be interpreted with caution, since incubation of human adipose explants with TNFα was shown to have only a minor effect on CRP expression.7 Nevertheless, such discrepancy may be explained by a dose-dependent response, as Anty et al7 used TNFα at a lower dosage than in our experiments (20 vs 50 ng/ml, respectively).
CD is characterised by increased bacterial translocation.12 Our results showing that LPS and E coli markedly induced the production of CRP by differentiated 3T3-L1 adipocytes led us to investigate whether bacterial translocation may occur through mesenteric adipose tissue. We demonstrated that mesenteric fat is a new site of bacterial translocation in humans. This phenomenon occurred spontaneously in 13% of healthy subjects at a rate broadly similar to that of mesenteric lymph nodes. Furthermore, bacterial translocation to mesenteric adipose tissue was observed in 27% of patients with CD also at a rate broadly similar to that of mesenteric lymph nodes. TLR1–11, NOD1 and NOD2 are known to be constitutively expressed in murine pre-adipocytes and adipocytes16 35 and, interestingly, bacterial translocation to mesenteric fat was increased in experimental models of colitis. DSS is known to cause UC-like disease in mice. Using an experimental model of ileitis, we also found an increased bacterial translocation in these animals. Here, we confirmed that human mesenteric adipocytes also constitutively express a wide range of PRMs, including TLR4, indicating that these fat cells are capable of sensing Gram-negative bacteria.
Collectively, the present data show that CRP biogenesis in adipose tissues may be preferentially triggered by TLR4 ligand, especially Gram-negative bacteria that translocate from the bowel lumen. Adenovirus-36 was shown to enhance the differentiation of pre-adipocytes in 3T3-L1 cells and increased adiposity in experimentally infected animals.36 The responsiveness of adipocytes to translocating bacteria may thus contribute to mesenteric fat hypertrophy in CD.13 We also found that TNFα synergistically enhanced the effect of a bacterial stimulus on adipocyte CRP expression. By stimulating the production of IL-6, TNFα may further enhance the production of CRP in CD.7 Local cytokine production and translocation of Gram-negative bacteria may thus synergise to promote CRP biogenesis by mesenteric adipocytes in CD.
In conclusion, our data further confirm that mesenteric fat is not an innocent bystander and may contribute to inflammatory response in patients with CD.37 Whether mesenteric fat has a protective role by killing translocating bacteria will require further investigation.
Footnotes
Funding: IRMAD/Astrazeneca, Institut Universitaire de France, Association François Aupetit.
Competing interests: None.
Ethics approval: Ethical guidelines in studies on humans were followed under the supervision of an investigator, and human samples were declared to Inserm according to French laws (articles L. 1243-3 and R. 1243-49, and the Code de la Santé Publique).
Contributors: LPB, CN, PD, study concept and design; LPB, FG, LD, CR, C Dubuquoy, C Decourcelle, MT, EB, MFO, CN, acquisition of data; LPB, FG, LD, analysis and interpretation of data; LPB, JFC, PD, drafting of the manuscript; JFC, critical revision of the manuscript for important intellectual content; LPB, FG, statistical analysis; LPB, LD, PD, obtainment of funding; AS, material support; PD, study supervision.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Black S, Kushner I, Samols D. C-reactive protein. J Biol Chem 2004;279:48487–90 [DOI] [PubMed] [Google Scholar]
- 2.Bottazzi B, Doni A, Garlanda C, et al. An integrated view of humoral innate immunity: pentraxins as a paradigm. Annu Rev Immunol 2010;28:157–83 [DOI] [PubMed] [Google Scholar]
- 3.Henriksen M, Jahnsen J, Lygren I, et al. C-reactive protein: a predictive factor and marker of inflammation in inflammatory bowel disease. Results from a prospective population-based study. Gut 2008;57:1518–23 [DOI] [PubMed] [Google Scholar]
- 4.Colombel JF, Sandborn WJ, Reinisch W, et al. Infliximab, azathioprine, or combination therapy for Crohn's disease. N Engl J Med 2010;362:1383–95 [DOI] [PubMed] [Google Scholar]
- 5.Treton X, Bouhnik Y, Mary JY, et al. Azathioprine withdrawal in patients with Crohn's disease maintained on prolonged remission: a high risk of relapse. Clin Gastroenterol Hepatol 2009;7:80–5 [DOI] [PubMed] [Google Scholar]
- 6.Peyrin-Biroulet L, Chamaillard M, Gonzalez F, et al. Mesenteric fat in Crohn's disease: a pathogenetic hallmark or an innocent bystander? Gut 2007;56:577–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anty R, Bekri S, Luciani N, et al. The inflammatory C-reactive protein is increased in both liver and adipose tissue in severely obese patients independently from metabolic syndrome, Type 2 diabetes, and NASH. Am J Gastroenterol 2006;101:1824–33 [DOI] [PubMed] [Google Scholar]
- 8.Greenfield JR, Samaras K, Jenkins AB, et al. Obesity is an important determinant of baseline serum C-reactive protein concentration in monozygotic twins, independent of genetic influences. Circulation 2004;109:3022–8 [DOI] [PubMed] [Google Scholar]
- 9.Colombel JF, Solem CA, Sandborn WJ, et al. Quantitative measurement and visual assessment of ileal Crohn's disease activity by computed tomography enterography: correlation with endoscopic severity and C reactive protein. Gut 2006;55:1561–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bataille R, Klein B. C-reactive protein levels as a direct indicator of interleukin-6 levels in humans in vivo. Arthritis Rheum 1992;35:982–4 [DOI] [PubMed] [Google Scholar]
- 11.Desreumaux P, Ernst O, Geboes K, et al. Inflammatory alterations in mesenteric adipose tissue in Crohn's disease. Gastroenterology 1999;117:73–81 [DOI] [PubMed] [Google Scholar]
- 12.Sedman PC, Macfie J, Sagar P, et al. The prevalence of gut translocation in humans. Gastroenterology 1994;107:643–9 [DOI] [PubMed] [Google Scholar]
- 13.Batra A, Zeitz M, Siegmund B. Adipokine signaling in inflammatory bowel disease. Inflamm Bowel Dis 2009;15:1897–905 [DOI] [PubMed] [Google Scholar]
- 14.Batra A, Pietsch J, Fedke I, et al. Leptin-dependent toll-like receptor expression and responsiveness in preadipocytes and adipocytes. Am J Pathol 2007;170:1931–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vitseva OI, Tanriverdi K, Tchkonia TT, et al. Inducible Toll-like receptor and NF-kappaB regulatory pathway expression in human adipose tissue. Obesity (Silver Spring) 2008;16:932–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stroh T, Batra A, Glauben R, et al. Nucleotide oligomerization domains 1 and 2: regulation of expression and function in preadipocytes. J Immunol 2008;181:3620–7 [DOI] [PubMed] [Google Scholar]
- 17.Declercq C, Gower-Rousseau C, Vernier-Massouille G, et al. Mapping of inflammatory bowel disease in northern France: spatial variations and relation to affluence. Inflamm Bowel Dis 2010;16:807–12 [DOI] [PubMed] [Google Scholar]
- 18.Franchimont D, Roland S, Gustot T, et al. Impact of infliximab on serum leptin levels in patients with Crohn's disease. J Clin Endocrinol Metab 2005;90:3510–16 [DOI] [PubMed] [Google Scholar]
- 19.Lin Y, Lee H, Berg AH, et al. The lipopolysaccharide-activated toll-like receptor (TLR)-4 induces synthesis of the closely related receptor TLR-2 in adipocytes. J Biol Chem 2000;275:24255–63 [DOI] [PubMed] [Google Scholar]
- 20.Hoch M, Eberle AN, Peterli R, et al. LPS induces interleukin-6 and interleukin-8 but not tumor necrosis factor-alpha in human adipocytes. Cytokine 2008;41:29–37 [DOI] [PubMed] [Google Scholar]
- 21.Netea MG, Ferwerda G, de Jong DJ, et al. Nucleotide-binding oligomerization domain-2 modulates specific TLR pathways for the induction of cytokine release. J Immunol 2005;174:6518–23 [DOI] [PubMed] [Google Scholar]
- 22.Yamamoto K, Kiyohara T, Murayama Y, et al. Production of adiponectin, an anti-inflammatory protein, in mesenteric adipose tissue in Crohn's disease. Gut 2005;54:789–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Neut C, Bulois P, Desreumaux P, et al. Changes in the bacterial flora of the neoterminal ileum after ileocolonic resection for Crohn's disease. Am J Gastroenterol 2002;97:939–46 [DOI] [PubMed] [Google Scholar]
- 24.Berg RD, Garlington AW. Translocation of certain indigenous bacteria from the gastrointestinal tract to the mesenteric lymph nodes and other organs in a gnotobiotic mouse model. Infect Immun 1979;23:403–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Desreumaux P, Dubuquoy L, Nutten S, et al. Attenuation of colon inflammation through activators of the retinoid X receptor (RXR)/peroxisome proliferator-activated receptor gamma (PPARgamma) heterodimer. A basis for new therapeutic strategies. J Exp Med 2001;193:827–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gatt M, Reddy BS, MacFie J. Review article: bacterial translocation in the critically ill—evidence and methods of prevention. Aliment Pharmacol Ther 2007;25:741–57 [DOI] [PubMed] [Google Scholar]
- 27.Piepoli AL, De Salvatore G, De Salvia MA, et al. Indomethacin-induced ileitis is associated with tensiometric, vascular and oxidative changes in the experimental rat model. Eur J Clin Invest 2005;35:271–8 [DOI] [PubMed] [Google Scholar]
- 28.Satsangi J, Silverberg MS, Vermeire S, et al. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut 2006;55:749–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Khazen W, M'Bika JP, Collinet M, et al. Differentiation-dependent expression of interferon gamma and toll-like receptor 9 in 3T3-F442A adipocytes. Biochimie 2007;89:669–75 [DOI] [PubMed] [Google Scholar]
- 30.Memoli B, Procino A, Calabro P, et al. Inflammation may modulate IL-6 and C-reactive protein gene expression in the adipose tissue: the role of IL-6 cell membrane receptor. Am J Physiol Endocrinol Metab 2007;293:E1030–5 [DOI] [PubMed] [Google Scholar]
- 31.Ouchi N, Kihara S, Funahashi T, et al. Reciprocal association of C-reactive protein with adiponectin in blood stream and adipose tissue. Circulation 2003;107:671–4 [DOI] [PubMed] [Google Scholar]
- 32.Cellier C, Sahmoud T, Froguel E, et al. Correlations between clinical activity, endoscopic severity, and biological parameters in colonic or ileocolonic Crohn's disease. A prospective multicentre study of 121 cases. The Groupe d'Etudes Therapeutiques des Affections Inflammatoires Digestives. Gut 1994;35:231–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Calabro P, Chang DW, Willerson JT, et al. Release of C-reactive protein in response to inflammatory cytokines by human adipocytes: linking obesity to vascular inflammation. J Am Coll Cardiol 2005;46:1112–13 [DOI] [PubMed] [Google Scholar]
- 34.Weinhold B, Bader A, Poli V, et al. Interleukin-6 is necessary, but not sufficient, for induction of the human C-reactive protein gene in vivo. Biochem J 1997;325:617–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pietsch J, Batra A, Stroh T, et al. Toll-like receptor expression and response to specific stimulation in adipocytes and preadipocytes: on the role of fat in inflammation. Ann N Y Acad Sci 2006;1072:407–9 [DOI] [PubMed] [Google Scholar]
- 36.Dhurandhar NV, Israel BA, Kolesar JM, et al. Increased adiposity in animals due to a human virus. Int J Obes Relat Metab Disord 2000;24:989–96 [DOI] [PubMed] [Google Scholar]
- 37.Schaffler A, Scholmerich J. Innate immunity and adipose tissue biology. Trends Immunol 2010;31:228–35 [DOI] [PubMed] [Google Scholar]