A clinical review of treatment outcomes in glioblastoma multiforme—the validation in a non-trial population of the results of a randomised Phase III clinical trial: has a more radical approach improved survival? (original) (raw)
Abstract
Objective
Glioblastoma multiforme (GBM) accounts for up to 60% of all malignant primary brain tumours in adults, occurring in 2–3 cases per 100 000 in Europe and North America. In 2005, a Phase III clinical trial demonstrated a significant improvement in survival over 2, and subsequently 5, years with the addition of concurrent and adjuvant temozolomide (TMZ) to radical radiotherapy (RT). The aim of this study was to investigate if the demonstrated improved survival in the literature translated to clinical practice.
Methods
This was a retrospective study including all patients with histologically proven GBM diagnosed from 1999 to 2008 and treated with adjuvant RT at our institution. A total of 273 patients were identified. Statistical analysis was carried out using SPSS® v.18 (SPSS, Chicago, IL).
Results
The median survival for the whole group (_n_=273) over the 10-year period was 7.6 months (95% confidence interval 6.7–8.4 months). Overall, the cumulative probability of survival at 1 and 2 years was 31.5% and 9.4%, respectively. In total, 146 patients received radical RT. 103 patients were treated with radical RT and TMZ and 43 patients received radical RT alone. The median survival for patients receiving radical RT with TMZ was 13.4 months (95% CI 10.9–15.8 months) vs 8.8 months for radical RT alone (95% CI 6.9–10.7 months, _p_=0.006). 2-year survival figures were 21.2% _vs_4.7%, respectively. On multivariate analysis, independent predictors of survival included Karnofsky Performance Status, RT dose, TMZ and extent of surgery. The strongest predictors of poorer outcome based on the hazard ratio were palliative RT, followed by not receiving TMZ chemotherapy, then KPS <90 and a biopsy only surgical approach.
Conclusion
This paper demonstrates improved survival outcomes consistent with those published in the literature for the addition of concurrent and adjuvant TMZ to radical RT for the treatment of GBM. Although 63% of patients seen in the clinic were suitable for a combined modality approach, the prognosis for the lower Radiation Therapy Oncology Group classes still remains poor.
Glioblastoma multiforme (GBM) accounts for up to 60% of all malignant primary brain tumours in adults [1], occurring in 2–3 cases per 100 000 in Europe and North America. Overall survival figures in the literature are poor. In 2005, Stupp et al [2] demonstrated significant improvements in 2-year survival figures with the addition of concurrent and adjuvant temozolomide (TMZ) to radical radiotherapy (RT).
The optimal management of patients with GBM provides a challenge owing to the diverse nature of this cohort in clinical practice. The aims of this study were to investigate whether or not the improved survival figures demonstrated in a Phase III randomised trial [3] translated to routine clinical practice with the introduction of protocol-driven standard of care and to analyse factors associated with improved outcome.
Corresponding to the publication of the Stupp protocol [2], we introduced a formalised consensus-based treatment approach for GBM at our institution, a designated national neuro-oncology centre. We designed a retrospective study evaluating the overall survival among patients receiving RT for treatment of GBM with or without TMZ. The treatment approach and outcome of patients diagnosed with GBM prior to and after the publication of the Stupp et al [2] results and the introduction of a formalised treatment approach were compared. The utilisation of Radiation Therapy Oncology Group (RTOG) classes allowed comparison over homogeneous subsets of patients.
Methods and materials
This was a retrospective study including all patients with histologically proven GBM diagnosed from 1999 to 2008 and treated with RT at our institution. A total of 273 patients were identified. The clinical notes, operative note, RT and chemotherapy prescriptions were examined. The extent of surgery was determined by reading operative notes and subdivided into three categories: biopsy only, subtotal debulking and radical debulking. With the introduction of TMZ, a formal multidisciplinary approach was taken, established in late 2005.
Overall survival times were calculated from the date of surgery to the date of death. The Kaplan–Meier method was used to estimate survival times. Survival functions were compared by the log-rank test. All statistical tests were two sided and assessed for significance at the 0.05 level. The Cox proportional hazards model was used to assess the effects of covariates on survival. RT dose, use of TMZ, extent of surgery, KPS and age were investigated as potential predictors of survival. Statistical analysis was carried out using SPSS® v.18 (SPSS Inc., Chicage, IL).
Results
Patient and treatment characteristics
Demographic and clinical characteristics for the whole group (_n_=273) are listed in Table 1. The median age at surgery was 59 years. Just over half the group (56%) had either partial or total radical debulking of their tumour. The mean start time from surgery to commencing RT was 29 days (mean 32.5 days for radical cases and 25.9 for palliative cases). At the time of analysis, 263 (96%) patients had died.
Table 1. Patient characteristics (_n_=273).
| Characteristic | Number of patients (_n_=273) | % |
|---|---|---|
| Age | ||
| <50 years | 52 | 19 |
| >50 years | 221 | 81 |
| Median age (years) | 59 | |
| Sex | ||
| Male | 158 | 58 |
| Female | 115 | 42 |
| KPS | ||
| 90–100 | 91 | 33 |
| 70–80 | 110 | 40 |
| 40–60 | 72 | 27 |
| Extent of surgery | ||
| Biopsy only | 121 | 44 |
| Partial debulking | 68 | 25 |
| Radical debulking | 84 | 31 |
| Radiation Therapy Oncology Group class | ||
| III | 34 | 13 |
| IV | 93 | 34 |
| V | 80 | 29 |
| VI | 66 | 24 |
| Radiotherapy | ||
| Radical (>54 Gy) | 146 | 53 |
| High dose palliative (40–53 Gy) | 71 | 26 |
| Palliative (<40 Gy) | 56 | 21 |
| Temozolomide | ||
| Yes | 117 | 43 |
| No | 156 | 57 |
| Temozolomide and radical radiotherapy | ||
| Yes | 103 | 38 |
| No | 170 | 62 |
| Alive | ||
| Yes | 10 | 4 |
| No | 263 | 96 |
Table 2 compares demographic and clinical characteristics of the patients receiving radical RT with or without TMZ. 103 patients were treated with radical RT and TMZ and 43 patients received radical RT alone. Of those treated with radical RT and TMZ, 71 (69%) received concurrent and adjuvant TMZ, 28 (27%) received concurrent only and 4 (4%) received adjuvant TMZ only.
Table 2. Patient characteristics for those receiving radical radiotherapy (RT) plus temozolomide chemotherapy (_n_=103) _vs_patients receiving radical RT alone (_n_=43).
| Characteristic | Radical RT plus TMZ Number (%) (_n_=103) | Radical RT alone Number (%) (_n_=43) |
|---|---|---|
| Age | ||
| <50 years | 34 (33) | 13 (30) |
| >50 years | 69 (67) | 30 (70) |
| Sex | ||
| Male | 57 (55) | 26 (60) |
| Female | 46 (45) | 17 (40) |
| KPS | ||
| 90–100 | 61 (59) | 23 (53) |
| 70–80 | 38 (37) | 17 (40) |
| 40–60 | 4 (4) | 3 (7) |
| Extent of surgery | ||
| Biopsy only | 25 (24) | 15 (35) |
| Partial debulking | 33 (32) | 10 (23) |
| Radical debulking | 45 (44) | 18 (42) |
| Radiation Therapy Oncology Group class | ||
| III | 24 (23) | 10 (23) |
| IV | 50 (49) | 14 (33) |
| V | 26 (25) | 18 (42) |
| VI | 3 (3) | 1 (2) |
| Temozolomide | ||
| Concurrent and adjuvant | 71 (69) | 0 |
| Concurrent only | 28 (27) | 0 |
| Adjuvant only | 4 (4) | 0 |
Overall in the total group, patients in higher RTOG classes were more likely to receive TMZ therapy (p<0.0001): in Class III 70.6% received TMZ, in Class IV 59.1% received TMZ, in Class V 36.3% received TMZ and in Class VI 13.6% received TMZ. There was a definite change in surgical trends over the 10-year period. Patients treated from 2006 onwards had higher rates of debulking surgery (66% for those treated from 2006 onwards vs 50% for those treated before 2006 _p_=0.013).
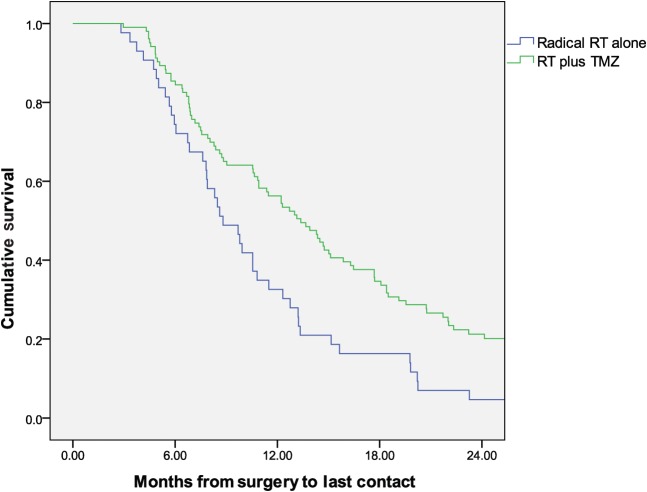
Survival
The median survival for the whole group (_n_=273) over the 10 year period was 7.6 months [95% confidence interval (CI) 6.7–8.4 months]. Overall, the cumulative probability of survival at 1 and 2 years was 31.5% and 9.4%, respectively. The median survival for patients receiving radical RT with TMZ was 13.4 months (95% CI 10.9–15.8 months) vs 8.8 months for radical RT alone (95% CI 6.9–10.7 months, _p_=0.006), as shown in Figure 1. The 2-year survival figures were 21.2% vs 4.7%, respectively.
Figure 1.
Kaplan–Meier survival curves for patients treated with radical radiotherapy with or without temozolomide (_n_=146).
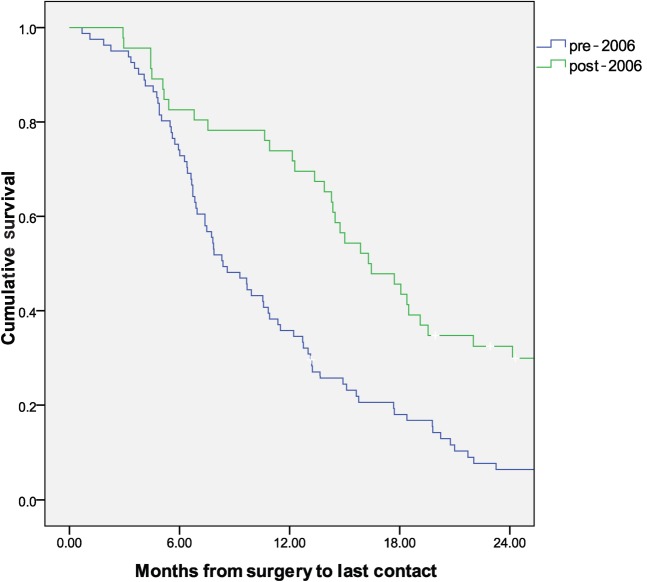
Overall survival was significantly better for all patients treated from 2006 onwards vs those treated before 2006 (8.7 _vs_7.1 months, _p_=0.009). This increase in survival was particularly evident in the higher RTOG classes. In Class III, overall survival improved from 10.5 to 18.4 months from 2006. In Class IV, overall survival increased from 7.9 to 14.4 months from 2006. Survival curves for Classes III and IV combined before and after 2006 are shown in Figure 2. No major change in survival occurred in the poorer RTOG class (Classes V and VI) over the entire 10-year period. In Class V, survival marginally improved from 6.5 to 6.8 months, and Class VI survival pre 2006 was 5.7 months and decreased to 4.1 months after 2006.
Figure 2.
Kaplan–Meier survival curves for Radiation Therapy Oncology Group Classes III and IV pre- and post-2006 (_n_=127).
Predictors of survival
Factors found to be significant on univariate analysis were included in a multivariate Cox proportional hazards model assessing prognostic factors. These included age at surgery, KPS category, RT dose, use of TMZ and extent of surgery. In the final model, KPS, extent of surgery, RT dose and TMZ remained as independent predictors for survival as summarised in Table 3. The strongest predictors of poorer outcome based on the hazard ratio (HR) were palliative RT, followed by not receiving TMZ chemotherapy, then KPS <90 and a biopsy only surgical approach.
Table 3. Cox regression analysis (_n_=273).
| Variable | Reference category | Significance | HR | 95% CI for HR |
|---|---|---|---|---|
| Lower | Upper | |||
| Dose group | Radical | 0.000 | ||
| High dose palliative | 0.571 | 1.122 | 0.753 | 1.673 |
| Palliative | 0.001 | 2.193 | 1.375 | 3.495 |
| Chemo | 0.001 | 1.664 | 1.224 | 2.264 |
| KPS category | 90–100 | 0.017 | ||
| KPS 70–80 | 0.054 | 1.532 | 0.992 | 2.365 |
| KPS 40–60 | 0.004 | 1.600 | 1.157 | 2.211 |
| Extent of surgery | Any debulking | 0.005 | ||
| Biopsy only | 0.003 | 1.496 | 1.130 | 1.980 |
| Age at surgery | 0.062 | 1.014 | 0.999 | 1.029 |
Palliative RT had an HR of 2.19 (95% CI 1.38–3.5, _p_=0.001) as compared with radical RT. Patients who did not receive TMZ had a significantly higher risk of death than those patients who did (HR 1.664, 95% CI 1.2–2.26, _p_=0.001). With regards to surgical procedure, biopsy only was inferior to any attempt at debulking (HR 1.496, 95% CI 1.13–1.98, _p_=0.005).
Discussion
This retrospective review demonstrates clear overall survival benefits in a general clinic population as a result of introducing TMZ therapy and adopting a more aggressive surgical approach. However, only 38% of the total group were considered suitable for radical RT and TMZ therapy. In this group, we have demonstrated similar median survival figures to those in the randomised Phase III clinical trial for patients receiving RT and TMZ therapy. Stupp et al [2] showed a 2-year survival rate of 26.5% for RT plus TMZ _vs_10.4 % for RT alone. In our population we demonstrated 2-year survival rates of 21.2% for RT plus TMZ vs 4.7% for RT alone. Furthermore, Stupp et al [3] were able to show a long-term benefit to combined modality treatment with 9.8% of patients treated with RT and TMZ alive at 5 years _vs_1.9% for RT alone. We identified no 5-year survivors in either treatment group.
Over many decades the prognosis for patients diagnosed with GBM remained poor despite a variety of research approaches including adjuvant chemotherapy schedules, hypoxia targeting and radiation dose escalation [4,5].
Based on response rates of 8–15% in the recurrence setting and a promising Phase II trial in the adjuvant setting, TMZ was the subject of a large multi-institutional study in which 83% of participants were treated with radical RT [2]. This study demonstrated a significant survival advantage with the addition of concurrent and adjuvant TMZ to radical RT with a 2 year survival rate of 26.5% for RT plus TMZ vs 10.4% for RT alone. However, as this trial included well-selected patients with >80% of patients radically debulked, it is unclear whether or not these excellent results could be replicated in a non-selected community setting. Our study confirms that replication of clinical trial data in the routine clinical setting requires optimal patient selection. Patients deemed suitable for treatment with TMZ and radical RT in this study had similar characteristics to the original Stupp et al [2] trial population.
In our study, 72% of patients belonged in the higher RTOG classes (RTOG Classes III and IV) vs 68% in the trial. 86% of the trial population had a World Health Organization performance status of 0 or 1, and 96% of our population had a KPS >70. Slightly more patients in the trial population underwent more radical surgery than in our population (83% vs 73%). As in the published trial [2], the extent of surgery is classified by the neurosurgeon at the time of operation. There was no mandate for immediate post-operative imaging.
Curran et al [6] have proposed six RTOG classes based on recursive partitioning analysis. Scott et al [7] validated the prognostic value of these classes on separate RTOG trial databases. Median survival times for RTOG Classes III and IV in the RTOG database were 17.9 and 11.1 months, respectively, with 2-year survival of 35% and 15%, respectively [6,7]. Our study demonstrated a similar median survival for Classes III and IV of 15.9 and 10.6 months, respectively (_n_=273).
Our study demonstrated median survival for patients in Classes III and IV treated with radical RT of 15.9 and 13.1 months, respectively (_n_=146). There was a significant increase in survival by class from 2006 with the introduction of concurrent and/or adjuvant TMZ and a more aggressive surgical approach (_p_=0.017 adjusted for RTOG class). Survival in Class III increased from a median of 10.5 months to 18.4 months. Survival in class IV increased from a median of 10.8 to 14.7 months.
Analysis of the Stupp et al [2] trial data according to the RTOG classes demonstrated that the benefit of TMZ therapy is largely confined to those patients in RTOG Classes III and IV [8]. With the addition of TMZ, survival in Class III improved by 4 months from 14.8 to 18.7 months and survival in class IV improved by 3 months from 13.3 to 16.3 months. There was no meaningful improvement in survival in the lower RTOG classes. Our study has validated these results in a community setting—the benefit of TMZ therapy is largely seen in the patients with better prognosis (RTOG Class III/IV). Median survival of those in Classes III and IV treated with radical RT and TMZ was 14.7 vs 8.7 months for those in Classes V and VI (_p_=0.042).
This is a retrospective study and is subject to the biases inherent in this type of study design. However, multivariate analysis including all known potential predictors of survival identified TMZ therapy as a significant predictor of improved survival with an HR of 1.7. The other important factors in improving outcomes include radical RT and a more definitive surgical approach.
Although it is clear that those patients eligible for treatment according to aggressive combined modality therapies benefit from the implementation of advances in therapy, the majority of patients seen in the clinic are not eligible for treatment on these protocols; therefore, the prognosis for those patients remains poor.
Individualising therapy has contributed to further progress in the treatment of GBM. The cytotoxicity of TMZ is mediated mainly through methylation of the O6 position of guanine. O6-methylguanine deoxyribonucleic acid (DNA) methyltransferase (MGMT) repairs tumour DNA damaged by chemotherapy. Patients with low tumour MGMT activity may be more likely to respond to alkylating agents. In a comparison study by Hegi et al [9], MGMT promoter methylation status was found to be a potent prognostic factor. In the Stupp et al paper [3], the subgroup of patients with MGMT methylation who were treated with radical RT plus TMZ had a median survival of 23.4 vs 15.3 months in the group treated with radical RT alone. While this approach is not yet available in the clinic, it provides hope that we may be better able to individualise treatment in the future with improved outcomes as a result.
Conclusion
This paper demonstrates improved survival outcomes consistent with those published in the literature for the addition of concurrent and adjuvant TMZ to radical RT for the treatment of GBM thus validated in a community setting. The survival benefit is largely seen in the higher RTOG classes, illustrating the need for optimal patient selection when choosing those most likely to benefit from combined modality therapy. In reality, 63% of patients were suitable for combined modality therapy. The survival for the lower RTOG Classes V and VI still remains poor and in our study did not improve over a 10 year period.
References
- 1.Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin 2010;60:277. [DOI] [PubMed] [Google Scholar]
- 2.Stupp R, Mason WP, van denBent MJ, Weller M, Fisher B, Taphoorn MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 2005;352:987–96 [DOI] [PubMed] [Google Scholar]
- 3.Stupp R, Hegi ME, Mason WP, van denBent MJ, Taphoorn MJ, Janzer RC, et al. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol 2009;10:459–66 [DOI] [PubMed] [Google Scholar]
- 4.Laperriere N, Zuraw L, Cairncross G. Radiotherapy for newly diagnosed malignant glioma in adults: a systematic review. Radiother Oncol 2002;64:259–73 [DOI] [PubMed] [Google Scholar]
- 5.González DG, Menten J, Bosch DA, van derSchueren E, Troost D, Hulshof MC, et al. Accelerated radiotherapy in glioblastoma multiforme: a dose searching prospective study. Radiother Oncol 1994;32:98–105 [DOI] [PubMed] [Google Scholar]
- 6.Curran WJ, Jr, Scott CB, Horton J, Nelson JS, Weinstein AS, Fischbach AJ, et al. Recursive partitioning analysis of prognostic factors in three Radiation Therapy Oncology Group malignant glioma trials. J Natl Cancer Inst 1993;85:690–1 [DOI] [PubMed] [Google Scholar]
- 7.Scott CB, Scarantino C, Urtasun R, Movsas B, Jones CU, Simpson JR, et al. Validation and predictive power of Radiation Therapy Oncology Group (RTOG) recursive partitioning analysis classes for malignant glioma patients: A report using RTOG 90-60. Int J Radiat Oncol Biol Phys 1998;40:51–5 [DOI] [PubMed] [Google Scholar]
- 8.Mirimanoff RO, Gorlia T, Mason W, Van denBent MJ, Kortmann RD, Fisher B, et al. Radiotherapy and temozolomide for newly diagnosed glioblastoma: recursive partitioning analysis of the EORTC 26981/22981-NCIC CE3 Phase III randomized trial. J Clin Oncol;24:2563–9 [DOI] [PubMed] [Google Scholar]
- 9.Hegi ME, Diserens AC, Gorlia T, Hamou MF, de Tribolet N, Weller M, et al. MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med 2005;352:997–1003 [DOI] [PubMed] [Google Scholar]