Emergency department visits, use of imaging, and drugs for urolithiasis have increased in the United States (original) (raw)
Abstract
The occurrence of urolithiasis in the United States has increased; however, information on long-term trends, including recurrence rates, is lacking. Here we describe national trends in rates of emergency department visits, use of imaging, and drug treatment, primarily using the National Hospital Ambulatory Medical Care Survey to describe trends and the National Health and Nutrition Examination Survey to determine the frequency of lifetime passage of kidney stones. Emergency department visit rates for urolithiasis increased from 178 to 340 visits per 100,000 individuals from 1992 to 2009. Increases in visit rates were greater in women, Caucasians, and in those aged 25–44 years. The use of computed tomography in urolithiasis patients more than tripled, from 21 to 71%. Medical expulsive therapy was used in 14% of the patients with a urolithiasis diagnosis in 2007–2009. Among National Health and Nutrition Examination Survey participants who reported a history of kidney stones, 22.4% had passed three or more stones. Hence, emergency department urolithiasis visit rates have increased significantly, as has the use of computed tomography in the United States. Further research is necessary to determine whether recurrent stone formers receive unnecessary radiation exposure during diagnostic evaluation in the emergency department and allow development of corresponding evidence-based guidelines.
Keywords: computed tomography, NHAMCS, radiation
Urolithiasis is one of the most common urological diseases in the United States.1 The lifetime risk of symptomatic kidney stones is ∼13% in men and 7% in women.2, 3 The prevalence is highest in older white men and lowest in younger black women.2, 3, 4 Studies suggest that kidney stone presentation also varies by season and geographic region, with greater frequency observed during the warmer months and in the southern United States.4, 5, 6, 7 Only limited information is available on urolithiasis recurrence rates. The financial burden of urolithiasis is substantial.8 Total annual medical expenditures for urolithiasis in the United States exceeded $2 billion in 2000, and are expected to increase in the future.7 An important factor in the increased cost is the use of medical imaging technology for the evaluation of urolithiasis patients. However, there is also concern regarding the extent of use of radiation in the evaluation of patients because of potential adverse long-term sequelae, especially in patients with recurrent disease and in younger patients.9
Although individuals with kidney stones may be asymptomatic, many may experience severe pain from stone passage.10 The prevalence and incidence of urolithiasis is increasing globally11, 12, 13, 14 and in the United States.2, 15, 16, 17 However, reports of long-term trends in the occurrence of urolithiasis in the United States are lacking. We examined trends in diagnosis, use of imaging and drugs, and regional and seasonal variation for urolithiasis in a nationally representative sample of US emergency department (ED) visits (National Hospital Ambulatory Medical Care Survey, NHAMCS) over nearly a two-decade period beginning in the early 1990s. We determined urolithiasis ED return visits using the NHAMCS database and evaluated the number of episodes of self-reported kidney stones among a nationally representative sample of the population (National Health and Nutrition Examination Survey, NHANES) to identify a subgroup of patients who may receive unnecessary radiation exposure from imaging during evaluation in the ED for suspected urolithiasis.
The goals of this study were to assess secular trends in ED urolithiasis visits, including imaging use in the United States, and to estimate urolithiasis recurrence rates and return visits in national and ED populations.
RESULTS
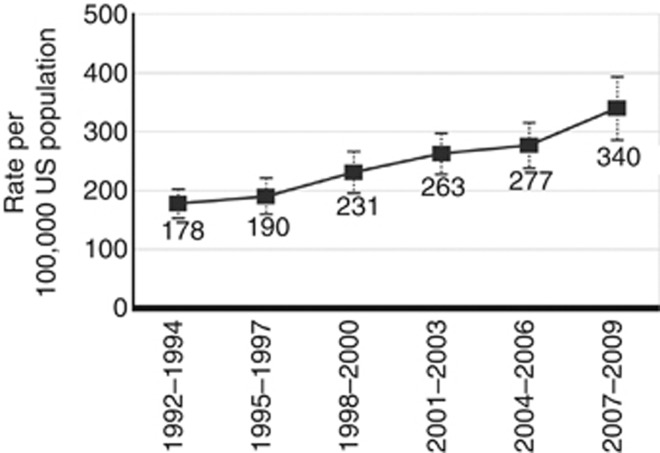
Emergency department visit rates
A total of 551,577 ED visits were sampled from 1992 to 2009. Upper tract urolithiasis was coded in 3403 visits. Accounting for the sampling weights and complex sample design, over this time, there were an estimated 12.45 million ED visits (95% confidence interval (CI), 11.22–13.67 million) with a diagnosis of upper tract urolithiasis, or about 700,000 visits per year in the United States. These visits accounted for about 0.65% (95% CI, 0.61–0.69%) of all ED visits. To examine temporal trends in urolithiasis, the number of ED visits with a diagnosis code for urolithiasis was calculated as the average annual ED visit rate. Among the entire U.S. noninstitutional population, the rate of ED visits with a diagnostic code for urolithiasis steadily increased from 178 (95% CI, 152–204) per 100,000 individuals in the 1992–1994 survey period to 340 (95% CI, 284–395) per 100,000 individuals in the 2007–2009 survey period (Figure 1), an increase of 91% (_P_trend<0.001). On the basis of a linear regression model by fitting the first five visit rates from the 1992–1994 survey period to the 2004–2006 survey period, we obtained a projected increase of 27 ED visits per 100,000 individuals by each 3-year period (rate=147+27* period). Compared with the predicted rate of 309 (95% CI, 280–337) for the 2007–2009 survey period, the observed rate of 340 (95% CI, 284–395) corresponded to an excess increase of 31 ED visits per 100,000 US population. However, the rate increase in the last period was not significantly greater than the trend seen in the previous surveys (_P_=0.15).
Figure 1.
Rates of visits per 100,000 US population with a diagnosis of upper tract urolithiasis to US emergency departments: 1992–2009. A weighted least-square regression analysis showed a significant linear trend. Error bars are 95% confidence intervals.
Across all survey periods, ED visit rates for urolithiasis were higher in men than women (Table 1). Although urolithiasis ED visit rates increased in both genders from the survey periods 1992–1994 to 2007–2009, the percentage of increase in women (128%) was nearly twice that of men (70%). In 1992–1994, the highest rate of ED visits for urolithiasis was in individuals aged 45–64 years old. In all subsequent surveys, the highest rate was in individuals aged 25–44 years old. The increase in ED urolithiasis visit rates in each age group over the various surveys was statistically significant, except for individuals >64 years of age. The greatest increase (132%) was found in the 25–44 year age group. The ED visit rate for urolithiasis among whites was about twice that of non-whites for all survey periods except 2001–2003, where the white to non-white rate ratio was nearly 3:1.
Table 1. Rates of emergency department visits with a diagnosis of upper tract urolithiasis by gender, age, and race: 1992–2009.
| | 1992–1994 | 1995–1997 | 1998–2000 | 2001–2003 | 2004–2006 | 2007–2009 | | | | | | | | | | | | | | | | | ---------------- | -------------------- | ------------- | ------------- | -------------------- | ------------- | -------- | -------------------- | ---------- | -------- | -------------------- | ---------- | -------- | -------------------- | ---------- | -------- | -------------------- | ---------- | ------------------------------ | ----------------------------- | ------ | | | No. | Ratea | 95% CI | No. | Ratea | 95% CI | No. | Ratea | 95% CI | No. | Ratea | 95% CI | No. | Ratea | 95% CI | No. | Ratea | 95% CI | Percent changeb | P trendc | | | Total | 435 | 178 | 152, 204 | 326 | 190 | 158, 223 | 400 | 231 | 194, 268 | 731 | 263 | 226, 299 | 708 | 277 | 236, 317 | 803 | 340 | 284, 395 | 91 | <0.001 | | | | | | | | | | | | | | | | | | | | | | | | | _Sex_ | | | | | | | | | | | | | | | | | | | | | | Male | 272 | 231 | 189, 274 | 198 | 240 | 193, 288 | 264 | 301 | 250, 351 | 437 | 331 | 275, 387 | 417 | 325 | 276, 374 | 441 | 393 | 322, 464 | 70 | 0.002 | | Female | 163 | 127 | 99, 154 | 128 | 143 | 109, 176 | 136 | 165 | 127, 203 | 294 | 197 | 164, 231 | 291 | 230 | 187, 273 | 362 | 289 | 235, 343 | 128 | <0.001 | | | | | | | | | | | | | | | | | | | | | | | | | _Age_ | | | | | | | | | | | | | | | | | | | | | | <25 | 51 | 63 | 40, 86 | 39 | 72 | 44, 99 | 47 | 82 | 55, 110 | 77 | 73 | 49, 96 | 105 | 120 | 90, 150 | 101 | 112 | 83, 141 | 78 | 0.030 | | 25–44 | 208 | 258 | 205, 310 | 168 | 303 | 237, 370 | 196 | 384 | 305, 462 | 340 | 444 | 368, 521 | 303 | 433 | 345, 521 | 366 | 599 | 472, 725 | 132 | 0.002 | | 45–64 | 139 | 287 | 223, 350 | 83 | 240 | 175, 305 | 125 | 333 | 249, 416 | 258 | 367 | 299, 435 | 234 | 344 | 271, 417 | 275 | 431 | 345, 516 | 50 | 0.029 | | >64 | 37 | 133 | 70, 197 | 36 | 169 | 95, 243 | 32 | 112 | 69, 154 | 56 | 176 | 120, 231 | 66 | 224 | 161, 288 | 61 | 216 | 138, 294 | 62 | 0.092 | | | | | | | | | | | | | | | | | | | | | | | | | Race | | | | | | | | | | | | | | | | | | | | | | White | 391 | 191 | 163, 219 | 299 | 217 | 178, 256 | 354 | 252 | 211, 294 | 657 | 300 | 256, 344 | 629 | 309 | 263, 355 | 710 | 384 | 318, 450 | 101 | <0.001 | | Non-white | 44 | 112 | 61, 163 | 27 | — | — | 46 | 134 | 84, 184 | 74 | 104 | 70, 138 | 79 | 145 | 98, 192 | 93 | 165 | 118, 213 | 47 | 0.21 |
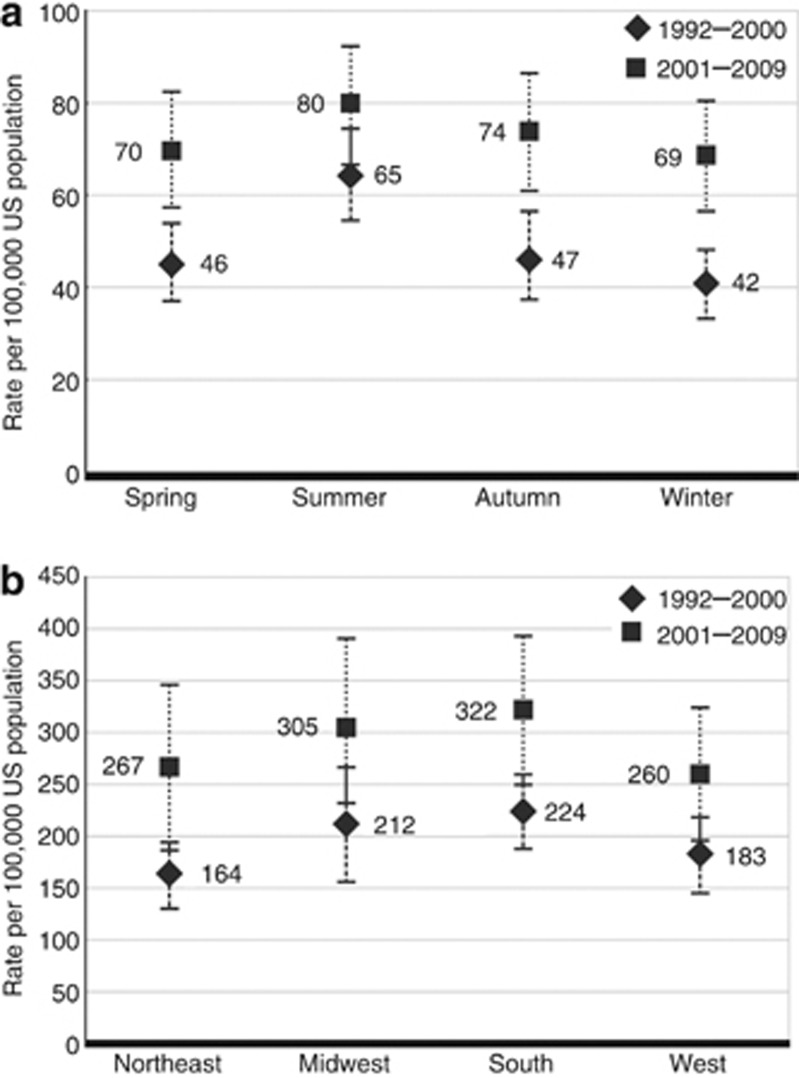
Although ED visit rates varied by season and by region of the country, none of these differences were statistically significant (Figure 2).
Figure 2.
Rates of emergency department visits with a diagnosis of upper tract urolithiasis by season and region, 1992–2009. (a) Seasonal and (b) regional variation of emergency department visit rates with a diagnosis of upper tract urolithiasis per 100,000 population from 1992–2000 to 2001–2009. Spring is March to May, summer is June to August, fall is September to November, and winter is December to February in this study. Error bars are 95% confidence intervals.
Use of imaging and drugs
The proportion of ED urolithiasis visits with any imaging used increased from 56% (95% CI, 48–64%) in 1995–1997 to 79% (75–83%) in 2007–2009 (_P_trend=0.015) (Table 2). The percent of ED urolithiasis visits at which X-rays were ordered decreased from 48% (95% CI, 40–55%) in 1995–1997 to 17% (12–22%) in 2007–2009 (_P_trend=0.005). In contrast, the use of computed tomography (CT) increased from 21% (95% CI, 15–26%) in 1998–2000 to 71% of visits (65–77%) in 2007–2009 (_P_trend=0.029). The frequency of the use of ultrasound was low: 5–6% in the survey periods 2001–2003 and 2004–2006.
Table 2. Percentage of use of imaging and drugs at emergency department visits with a diagnosis of upper tract urolithiasis: 1992–2009.
| | 1992–1994 | 1995–1997 | 1998–2000 | 2001–2003 | 2004–2006 | 2007–2009 | | | | | | | | | | | ----------------------------------------------------------- | ------------- | ------------- | ------------- | ------------- | ------------- | -------- | ---------- | -------- | ---------- | -------- | ---------- | ------------------------------ | ----------------------------- | ----- | | | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | Percent changea | P trendb | | | Imaging use | | | | | | | | | | | | | | | | Any imagingc | NA | NA | 56 | 48, 64 | 55 | 49, 60 | 66 | 61, 71 | 78 | 74, 81 | 79 | 75, 83 | 41 | 0.015 | | X-ray | NA | NA | 48 | 40, 55 | 34 | 28, 40 | 28 | 24, 32 | 21 | 17, 26 | 17 | 12, 22 | −65 | 0.005 | | Ultrasound | NA | NA | — | — | — | — | 6 | 4, 8 | 5 | 3, 7 | — | — | −17 | NA | | CT | NA | NA | — | — | 21 | 15, 26 | 44 | 38, 49 | 65 | 60, 70 | 71 | 65, 77 | 238 | 0.029 | | | | | | | | | | | | | | | | | | | Medication use | | | | | | | | | | | | | | | | Visits with medication provided or prescribedd | 88 | 84, 92 | 90 | 86, 95 | 89 | 85, 93 | 95 | 93, 97 | 95 | 93, 97 | 95 | 93, 97 | 8 | 0.020 | | Visits with analgesics provided or prescribede | 77 | 73, 81 | 84 | 79, 90 | 82 | 78, 86 | 91 | 89, 94 | 90 | 87, 93 | 91 | 89, 94 | 18 | 0.022 | | Visits with MET provided or prescribed | NA | NA | NA | NA | NA | NA | — | — | — | — | 14 | 10, 17 | NA | NA | | Number of medications provided or prescribed (mean, 95% CI) | 2.1 | 1.9, 2.2 | 2.4 | 2.2, 2.6 | 2.1 | 2.0, 2.3 | 2.8 | 2.7, 3.0 | 3.1 | 3.0, 3.3 | 3.4 | 3.1, 3.6 | 62 | 0.008 |
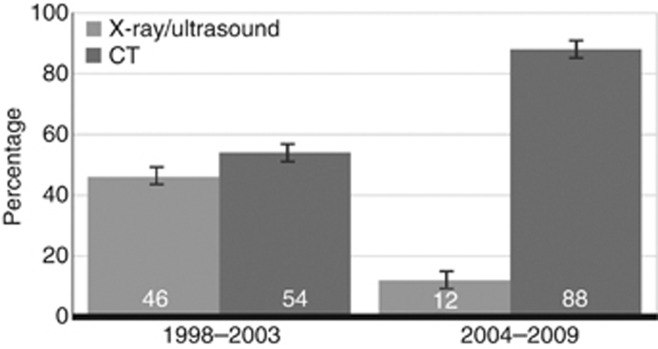
Among urolithiasis ED visits with any imaging, the proportion of CT or X-ray/ultrasound use in the survey periods 1998–2003 and 2004–2009 is shown in Figure 3. In 1998–2003, approximately half the visits used CT, increasing to 88% in 2004–2009. The use of CT increased from 19% (95% CI, 11–27%) in 1998–2000 to 73% (65–80%) in 2007–2009 in patients aged 25–44 years old (_P_trend=0.018) and from 42% (28–56%) in 2001–2003 to 64% (51–77%) in patients <25 years in 2007–2009 (_P_trend<0.001) (Table 3). The use of CT did not differ proportionally between men and women with urolithiasis visits during any of the time periods assessed, but increased in men (_P_trend=0.028). The use of CT did not differ proportionally between white and non-white patients with urolithiasis visits during any of the time periods assessed, but the proportion of use increased significantly in white patients (_P_trend=0.036).
Figure 3.
Percentage of computed tomography (CT) and X-ray/ultrasound use in upper tract urolithiasis emergency department visits with any imaging used from 1998–2003 to 2004–2009. Error bars are 95% confidence intervals.
Table 3. Percentage of computed tomography use at emergency department visits with a diagnosis of upper tract urolithiasis, by selected characteristics: 1998–2009.
| | 1998–2000 | 2001–2003 | 2004–2006 | 2007–2009 | | | | | | | | --------------------- | ------------- | ------------- | ------------- | ------ | ---------- | ------ | ---------- | ----------------------------- | ------ | | | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | P trenda | | | Total | 21 | 15, 26 | 44 | 38, 49 | 65 | 60, 70 | 71 | 65, 77 | 0.029 | | | | | | | | | | | | | | Age | | | | | | | | | | | <25 | — | — | 42 | 28, 56 | 53 | 41, 65 | 64 | 51, 77 | <0.001 | | 25–44 | 19 | 11, 27 | 39 | 32, 47 | 64 | 57, 72 | 73 | 65, 80 | 0.018 | | 45–64 | — | — | 47 | 39, 55 | 71 | 62, 79 | 74 | 68, 80 | 0.24 | | >64 | — | — | — | — | 72 | 57, 86 | 60 | 45, 74 | NA | | P valueb | NA | 0.23 | 0.11 | 0.21 | | | | | | | | | | | | | | | | | | | Sex | | | | | | | | | | | Female | — | — | 44 | 37, 51 | 61 | 55, 68 | 68 | 60, 76 | 0.20 | | Male | 24 | 16, 31 | 44 | 36, 51 | 68 | 62, 75 | 74 | 68, 79 | 0.028 | | P valueb | NA | 0.99 | 0.15 | 0.14 | | | | | | | | | | | | | | | | | | | Race | | | | | | | | | | | White | 21 | 15, 27 | 44 | 38, 50 | 65 | 60, 70 | 70 | 74, 76 | 0.036 | | Non-white | — | — | 42 | 28, 57 | 66 | 52, 80 | 80 | 68, 92 | 0.10 | | P valueb | NA | 0.88 | 0.88 | 0.11 | | | | | |
The proportion of ED visits for codes indicating other disorders of the urethra and urinary tract, symptoms involving the urinary system, and other symptoms involving the abdomen and pelvis with any imaging used increased from 38% (95% CI, 35–40%) in 1995–1997 to 55% (53–57%) in 2007–2009 (_P_trend<0.001). CT use in this group increased from 2% (95% CI, 2–3%) in 1995–1997 to 30% (28–32%) in 2007–2009 (_P_trend<0.001) (data not shown).
Prescribed drugs were commonly used over the survey periods (range 88–95%). Analgesic prescriptions increased from 77% (95% CI, 73–81%) to 91% (89–94%) (_P_trend=0.022) of visits. Medical expulsive therapy (MET) use was infrequent before 2007. In 2007–2009, MET was prescribed in 14% (95% CI, 10–17%) of ED urolithiasis visits. The mean number of prescribed drugs per ED urolithiasis visit increased from 2.1 (95% CI, 1.9–2.2) in 1992–1994 to 3.4 (3.1–3.6) in 2007–2009 (_P_trend=0.008).
Recurrence estimates
In the survey period 2001–2003, 5% (95% CI, 3–7%) of urolithiasis ED visits were return visits, increasing to 10% (7–13%) in the survey period 2007–2009.
A total of 528 NHANES 2007–2008 participants reported a history of kidney stones. Among them, 22.4% (95% CI, 17.3–28.6%) reported that they had passed three or more stones and 13.7% (9.7–19.0%) reported having passed four or more stones.
These findings suggest that ED visits resulting in a diagnosis of urolithiasis may include a substantial number of individuals with recurrent episodes of kidney stones.
DISCUSSION
Over nearly 20 years beginning in the early 1990s, the rate of ED visits with a diagnosis of upper tract urolithiasis in the United States has steadily increased, nearly doubling from 178 to 340/100,000 population. In contrast, total ED visit rates increased by only 16% over the same time period.18, 19 Thus, the increase in ED urolithiasis visits was more than five times greater than the proportional increase for all ED visits. The greatest increases in ED urolithiasis visit rates occurred among women, whites, and individuals aged 25–44 years old. The use of all prescription drugs, including analgesics, increased during the study period. The frequency of the use of CT to aid in the diagnosis and management of urolithiasis in the ED also increased significantly. Because the use of MET began in 2007–2009, we are unable to report time trends.
Several recent US studies have also documented an increase in the use of health-care resources7, 20 and in the incidence and prevalence15, 16, 17 of urolithiasis. In a study using the NHAMCS, hospital outpatient urolithiasis visits increased nationally by 40% between 1994 and 2000.7 Although we confirmed prior studies that show urolithiasis to be more common in men, we found the percentage of increase in ED visits to be nearly twice as great in women. This finding is consistent with prior reports of an increase in incident symptomatic stone disease15, 21 and hospital discharges for ureteral and renal calculi.22, 23 In contrast, we did not observe regional or seasonal differences in ED visit rates for urolithiasis, using a large, comprehensive national survey. However, the rates for both 9-year survey periods were numerically highest in summer and in the South, in agreement with several other studies.2, 5, 6
The increase in ED visits with urolithiasis diagnoses might result from a combination of factors including an actual change in disease incidence, improvement in diagnostic methods, and/or an increase in the number of people who use the ED for primary medical care. However, we cannot identify the reasons for this increase from our data. We believe the contribution of enhanced detection as a result of improved imaging technology on the increase in urolithiasis was likely modest, as several recent studies, using the NHAMCS, have found that the increased use of CT was not associated with a change in the proportion of diagnosis of kidney stones among ED patients presenting with acute flank or groin pain.20, 24 Moreover, although we could not exclude the possibility that more people with kidney stone episodes use the ED for primary medical care, we would not expect most of the increases observed in our study to be because of this reason. Recent work suggests adults with Medicaid accounted for most of the increase in ED visits from 1997 to 2007 because of their increasing difficulties in accessing primary care.25 As we could not envision that patients with kidney stones are more likely to be Medicaid recipients, and the increase in ED visits for urolithiasis was much greater than the increase for all ED visits, our findings are consistent with other reports of increased hospital outpatient visits for urolithiasis.7
Because medical, lifestyle, or dietary information on individual patients was not collected in NHAMCS, we can only speculate on the reasons for the increased urolithiasis rate. Over the period of the surveys, three important risk factors for urolithiasis, obesity,26 diabetes,27 and the use of dietary supplemental calcium28 have substantially increased in the general population.29, 30, 31, 32 Decreasing water intake33 and other factors may also contribute to this increase in stone disease. Future studies with patient-level information are needed to identify specific risk factors for the increase in urolithiasis.
A prior report using NHAMCS data showed the use of CT from 1996–1998 to 2005–2007 in patients presenting to the ED with flank pain increased 10-fold.24 We also observed a >3-fold increase in the use of CT in urolithiasis patients over the period 1998–2000 to 2007–2009.
The increased use of CT for evaluation of a common clinical syndrome such as urolithiasis raises important clinical questions. CT clearly provides important and accurate diagnostic information for physicians caring for patients with suspected urolithiasis. However, repeated use of CT evaluations for patients with recurrent urolithiasis contributes to increased radiation exposure for patients, as well as an increase in costs. Several investigators have noted that the potential burden of radiation exposure from medical imaging is an important health issue, especially in younger patients.9, 20, 24, 34, 35, 36, 37, 38, 39 Radiation reduction techniques, however, may limit patient exposure.40, 41, 42, 43, 44, 45 The findings from the NHANES suggest that a significant percentage of all ED visits with urolithiasis diagnoses may be because of patients with recurrent stones. Data from the NHAMCS suggest that return encounters comprise between 5 and 10% of ED urolithiasis visits. There are limited data regarding the number of recurrent stone formers in the United States and how frequently they visit emergency facilities.2, 46 Goldstone and Bushnell found that repeated CT imaging of patients with recurrent nephrolithiasis resulted in a change in diagnosis in only a small number of patients.47 The estimate from NHANES of approximately one in seven stone formers having four or more stone passages over the lifespan suggests a lower limit for opportunities to avoid the use of advanced radiologic imaging, thereby resulting in cost savings and reducing radiation exposure.
The reasons for the increased use of advanced radiologic evaluations in the ED for urolithiasis patients are unclear and cannot be determined from the study database. They may include increased sensitivity and specificity of CT evaluation for urolithiasis, pressures related to fear of medical malpractice claims, and patient demand.36, 48 Physician time pressures, increased reliance on technology, and use of radiologic techniques as default measures for consultation gateways and admission decisions may constitute incentives to lower the threshold for use of such tests. Although CT evaluation can locate a stone and assess hydronephrosis, the clinical decision-making for a urolithiasis patient, especially a recurrent stone former, in the absence of radiologic assessment is often straightforward. After evaluation of flank pain by physical examination and exclusion of other causes of abdominal pain, urinalysis can suggest infection, and hydration and provision of analgesics can be instituted. This is especially true in patients with a history of urolithiasis. If a stone is not passed during a follow-up observation period, radiologic assessment can then proceed, perhaps with an ultrasound. The proper balance between traditional physical examination and use of advanced radiologic techniques in patients with suspected urolithiasis is uncertain, in part, because of the lack of evidence and practice guidelines to inform clinical approaches for such patients.49
We documented the use of MET by ED physicians beginning in 2007, about the time when the management guideline became available,49 observing a rate of 14%, confirming prior reports of low MET use by ED physicians.50, 51 Education on the efficacy of MET for urolithiasis among ED physicians may increase the use and improve patient outcomes.52
This cross-sectional survey of ED encounters has several limitations. The NHAMCS identifies ED visits and may include multiple visits for a single patient. This is likely minimized by the four-stage sampling design of the NHAMCS in which a hospital is surveyed for ∼1 month every 15 months. We did not have information regarding factors that would account for increases in ED urolithiasis diagnoses, nor for understanding the reasons for the increased use of advanced imaging studies. We did not have information about the location, size, or composition of kidney stones, which limits our understanding of the clinical characteristics of patients with urolithiasis ED visits. As sample sizes in specific race/ethnicity categories were small, evaluation of race/ethnicity was limited to the white and non-white categories. Therefore, we were unable to assess the burden of urolithiasis in Hispanic Americans, an increasing segment of the US population, as well as in other racial/ethnic groups. Validation of the accuracy of the codes in the study was not determined by chart review. In addition, we could not definitively determine whether the ED visit was for new or recurring kidney stones.
In conclusion, over nearly the last 20 years, ED urolithiasis visit rates increased substantially in the United States. Visit rates increased disproportionately in women, whites, and in individuals aged 25–44 years old. We could not demonstrate seasonal or regional variation in ED visit rates for urolithiasis over the study period. The relatively high rate of recurrent kidney stone episodes and return ED visits for urolithiasis patients in the population is consistent with the hypothesis that such individuals presenting to the ED with flank pain may receive unnecessary radiation exposure. These issues need to be evaluated in appropriate, well-designed observational studies or randomized-controlled clinical trials. Appropriate use of imaging guided by evidence is necessary to minimize radiation exposure in individuals with suspected urolithiasis who present to the ED.
MATERIALS AND METHODS
Data sources
We analyzed data from the ED component of the NHAMCS from 1992 to 2009. The NHAMCS identifies a nationally representative sample of visits to noninstitutional general and short-stay hospitals, excluding Federal, military, and Veterans Administration hospitals, located in 50 states and the District of Columbia. The survey was approved by the Centers for Disease Control Institutional Review Board, including a waiver of the requirement for informed consent of sampled visits.
The survey uses a four-stage probability design with samples of geographic areas, hospitals within these areas, EDs within hospitals, and patient visits within EDs. The number of selected hospitals with eligible EDs over the study period ranged from 379 in 2008 to 443 in 2003. The participation rate of sampled hospitals over the study period varied from 89% in 2007 to 98% in 1998.53 Trained personnel at participating hospitals completed standardized patient record forms for a systematic random sample of patient visits during a randomly assigned 4-week period. The number of forms collected in survey years varied from 21,103 in 1999 to 40,253 in 2003.53
Study population and variables
The NHAMCS permits recording of up to three physician diagnoses per ED visit based on the International Classification of Diseases, Ninth revision, Clinical Modification (ICD-9-CM). We identified all visits with a code of 592.0 (calculus of kidney), 592.1 (calculus of ureter), or 592.9 (urinary calculus, unspecified) as visits with upper tract urolithiasis. Seventy-five percent of the visits had calculus of kidney and ureter (592.x) as the primary diagnosis. Among the visits with 592.x listed second or third, the most common accompanying diagnoses were ‘other symptoms involving abdomen and pelvis' (789.x; 37%), ‘symptoms involving urinary system' (788.x; 24%), and ‘other disorders of urethra and urinary tract' (599.x; 15%). We identified a secondary population, which included all visits with a primary diagnostic code of 599.x, 788.x, or 789.x as a comparison group.
We examined overall rates of ED visits with a diagnosis of upper tract urolithiasis and rates according to gender, age (<25, 25–44, 45–64, and >64 years), race (white, non-white), season, and by the geographic region in which the surveyed hospital was located (Northeast, Midwest, South, and West). Months of the year were grouped into seasons as follows: spring: March–May; summer: June–August; fall: September–November; and winter: December–February. Geographic regions are defined by the US Bureau of the Census.53 The types of imaging for the diagnosis of urolithiasis available from NHAMCS beginning in 1995 were plain X-ray, abdominal ultrasound, and CT. In 2001–2004, the use of CT and magnetic resonance imaging (MRI) was coded together. As MRI is not generally used in the diagnostic evaluation of patients with suspected urolithiasis,54 we assumed the combined CT/MRI results represented CT use in 2001–2004. This approach was supported by observing the same percentage of use of CT only and the CT/MRI combined category in years in which CT and MRI were coded separately (data not shown).
Medications administered or prescribed were coded for drug class. As NHAMCS changed their coding system in 2006, we identified analgesics using the National Drug Code categories (code 17xx) before 2006 and the Multum Lexicon second-level therapeutic drug category (code 058) beginning in 2006 and thereafter. MET was identified by the following generic drugs: alfuzosin, prazosin, terazosin, doxazosin, silodosin, tamsulosin, and nifedipine. These agents might also be prescribed for patients with hypertension or benign prostatic hyperplasia. We cross-checked the concurrent diagnoses of visits with MET and found only one visit with urolithiasis and hypertension.
Estimate of lifetime stone passage and recurrence
We were unable to find reliable published information on the frequency of recurrence of kidney stone episodes in the United States to consider possible exposure of this subgroup of patients to unnecessary radiation from imaging during evaluation for suspected urolithiasis presenting in the ED. We analyzed data from the NHANES 2007–2008, a nationally representative sample of the noninstitutionalized population, to estimate the lifetime number of kidney stones passed in the US adult population.55 The number of stone passages was determined by the following question, asked only of those individuals who answered affirmatively regarding having ever had kidney stones: “How many times have you passed a kidney stone?” Of 5935 sampled individuals aged 20 years and older, 539 (9%) reported having had kidney stones. Eleven participants were excluded from the analyses as they did not provide an answer regarding the number of times they passed kidney stones. A total of 528 participants were used to estimate the number of lifetime stone passages. We set the following categories for lifetime stone passages: 0–2 times or >2 times; 0–3 times or >3 times.
The item ‘episode of care (initial or follow-up visit to this ED for problem)' was available from NHAMCS beginning in 2001, but unavailable in 2005 and 2006. Therefore, proportions of follow-up visits (termed return visits) could only be reported in two study periods (2001–2003 and 2007–2009). We used return visits as a proxy for recurrence.
Data analysis
We used the weights and masked sample design variables of the NHAMCS and NHANES, which were provided by the NCHS for each record, to calculate the nationally representative point and variance estimates for all analyses. The weight is an inflation factor to estimate national counts. The sample design variables reflected the complex multi-stage sample design of the surveys and were intended for use with software such as SUDAAN that requires such data for variance estimation.56 Details regarding the development of the weights and sample design variables are described at the NCHS website.53, 56 Survey data in the NHAMCS were combined into 3-year groups to improve reliability of our estimates as follows: 1992–1994, 1995–1997, 1998–2000, 2001–2003, 2004–2006, and 2007–2009. Survey data were also combined into two 9-year groups, 1992–2000 and 2001–2009, to estimate ED visit rates for season and geographic region. As reliable estimates of CT use were only available from 1998 onward, two 6-year groups, 1998–2003 and 2004–2009, were used to present the percent change of using CT or X-ray/ultrasound among ED visits with any imaging to aid in the diagnosis of urolithiasis.
ED visit rates are reported as average annual rates for each 3-year period (or 9-year period for season and region specific rate). The rates were computed using the sum of the three (or nine) mid-year total population estimates, or gender, age, race, and region-specific population estimates from the US Census Bureau.53 All rates were reported as number of visits per 100,000 U.S. noninstitutional population. Visits in which imaging was used and drugs for urolithiasis prescribed are expressed as percent of all visits with a urolithiasis diagnosis code. Proportions were compared across age, sex, and race groups using Wald _χ_2-tests. Ninety-five percent CI for all rates and proportions were calculated. Trends in the estimated visit rates and the temporal patterns of imaging and drug use were analyzed using weighted least-squares regression analyses. To test whether the rate in the 2007–2009 survey period was significantly higher than what would be projected from the preceding surveys, we created a linear regression model by fitting the first five visit rates from the 1992–1994 survey period to the 2004–2006 survey period to obtain a predicted rate for the 2007–2009 survey period. The predicted and observed rates were compared using the _t_-test.
All data management and analyses were performed using SAS version 9.2 (SAS Institute, Cary, NC) and SAS callable SUDAAN version 10.0.0 (Research Triangle Institute, Research Triangle Park, NC). Two-sided _P_-values<0.05 were considered statistically significant.
The views expressed herein do not necessarily represent the views of the Department of Health and Human Services, the National Institutes of Health, the National Institute of Diabetes and Digestive and Kidney Diseases, or the United States Government.
Acknowledgments
CWF is supported by a contract from the National Institute of Diabetes and Digestive and Kidney Diseases (HHSN267200700001G).
Author contributions
All authors were involved in the design of the study, interpretation of the data, and the writing of the manuscript.
All the authors declared no competing interests.
References
- Litwin MS, Saigal CS, Yano EM et al. Urologic diseases in America Project: analytical methods and principal findings. J Urol 2005; 173: 933–937. [DOI] [PubMed] [Google Scholar]
- Stamatelou KK, Francis ME, Jones CA et al. Time trends in reported prevalence of kidney stones in the United States: 1976-1994. Kidney Int 2003; 63: 1817–1823. [DOI] [PubMed] [Google Scholar]
- Scales CD, Smith AC, Hanley JM et al. Prevalence of kidney stones in the United States. Eur Urol 2012; 62: 160–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soucie JM, Thun MJ, Coates RJ et al. Demographic and geographic variability of kidney stones in the United States. Kidney Int 1994; 46: 893–899. [DOI] [PubMed] [Google Scholar]
- Soucie JM, Coates RJ, McClellan W et al. Relation between geographic variability in kidney stones prevalence and risk factors for stones. Am J Epidemiol 1996; 143: 487–495. [DOI] [PubMed] [Google Scholar]
- Chauhan V, Eskin B, Allegra JR et al. Effect of season, age, and gender on renal colic incidence. Am J Emerg Med 2004; 22: 560–563. [DOI] [PubMed] [Google Scholar]
- Pearle MS, Calhoun EA, Curhan GC. Urologic diseases in America project: urolithiasis. J Urol 2005; 173: 848–857. [DOI] [PubMed] [Google Scholar]
- Lotan Y. Economics and cost of care of stone disease. Adv Chronic Kidney Dis 2009; 16: 5–10. [DOI] [PubMed] [Google Scholar]
- Pearce MS, Salotti JA, Little MP et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 2012; 380: 499–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teichman JM. Clinical practice. Acute renal colic from ureteral calculus. N Engl J Med 2004; 350: 684–693. [DOI] [PubMed] [Google Scholar]
- Hesse A, Brandle E, Wilbert D et al. Study on the prevalence and incidence of urolithiasis in Germany comparing the years 1979 vs. 2000. Eur Urol 2003; 44: 709–713. [DOI] [PubMed] [Google Scholar]
- Yasui T, Iguchi M, Suzuki S et al. Prevalence and epidemiological characteristics of urolithiasis in Japan: national trends between 1965 and 2005. Urology 2008; 71: 209–213. [DOI] [PubMed] [Google Scholar]
- Romero V, Akpinar H, Assimos DG. Kidney stones: a global picture of prevalence, incidence, and associated risk factors. Rev Urol 2010; 12: e86–e96. [PMC free article] [PubMed] [Google Scholar]
- Turney BW, Reynard JM, Noble JG et al. Trends in urological stone disease. BJU Int 2012; 109: 1082–1087. [DOI] [PubMed] [Google Scholar]
- Penniston KL, McLaren ID, Greenlee RT et al. Urolithiasis in a rural Wisconsin population from 1992 to 2008: narrowing of the male-to-female ratio. J Urol 2011; 185: 1731–1736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sas DJ, Hulsey TC, Shatat IF et al. Increasing incidence of kidney stones in children evaluated in the emergency department. J Pediatr 2010; 157: 132–137. [DOI] [PubMed] [Google Scholar]
- Dwyer ME, Krambeck AE, Bergstralh EJ et al. Temporal trends in incidence of kidney stones among children: a 25-year population based study. J Urol 2012; 188: 247–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burt CW, McCaig LF. Trends in hospital emergency department utilization: United States, 1992–99. Vital Health Stat 2001; 13: 1–34. [PubMed] [Google Scholar]
- NHAMCS. National Hospital Ambulatory Medical Care Survey: 2008 emergency department summary tables. In http://www.cdc.gov/nchs/data/ahcd/nhamcs\_emergency/nhamcsed2008.pdf.
- Hyams ES, Korley FK, Pham JC et al. Trends in imaging use during the emergency department evaluation of flank pain. J Urol 2011; 186: 2270–2274. [DOI] [PubMed] [Google Scholar]
- Lieske JC, Pena de la Vega LS, Slezak JM et al. Renal stone epidemiology in Rochester, Minnesota: an update. Kidney Int 2006; 69: 760–764. [DOI] [PubMed] [Google Scholar]
- Strope SA, Wolf JS, Hollenbeck BK. Changes in gender distribution of urinary stone disease. Urology 2010; 75: 543–546 546 e541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scales CD, Curtis LH, Norris RD et al. Changing gender prevalence of stone disease. J Urol 2007; 177: 979–982. [DOI] [PubMed] [Google Scholar]
- Westphalen AC, Hsia RY, Maselli JH et al. Radiological imaging of patients with suspected urinary tract stones: national trends, diagnoses, and predictors. Acad Emerg Med 2011; 18: 699–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang N, Stein J, Hsia RY et al. Trends and characteristics of US emergency department visits, 1997-2007. JAMA 2010; 304: 664–670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor EN, Stampfer MJ, Curhan GC. Obesity, weight gain, and the risk of kidney stones. JAMA 2005; 293: 455–462. [DOI] [PubMed] [Google Scholar]
- Taylor EN, Stampfer MJ, Curhan GC. Diabetes mellitus and the risk of nephrolithiasis. Kidney Int 2005; 68: 1230–1235. [DOI] [PubMed] [Google Scholar]
- Wallace RB, Wactawski-Wende J, O'Sullivan MJ et al. Urinary tract stone occurrence in the Women's Health Initiative (WHI) randomized clinical trial of calcium and vitamin D supplements. Am J Clin Nutr 2011; 94: 270–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. Prevalence of overweight, obesity and extreme obesity among adults: United States, trends 1960–62 through 2007–2008. In http://www.cdc.gov/nchs/data/hestat/obesity\_adult\_07\_08/obesity\_adult\_07\_08.htm.
- Cowie CC, Rust KF, Byrd-Holt DD et al. Prevalence of diabetes and high risk for diabetes using A1C criteria in the U.S. population in 1988-2006. Diabetes Care 2010; 33: 562–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radimer K, Bindewald B, Hughes J et al. Dietary supplement use by US adults: data from the National Health and Nutrition Examination Survey, 1999-2000. Am J Epidemiol 2004; 160: 339–349. [DOI] [PubMed] [Google Scholar]
- Bailey RL, Dodd KW, Goldman JA et al. Estimation of total usual calcium and vitamin D intakes in the United States. J Nutr 2010; 140: 817–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kant AK, Graubard BI, Atchison EA. Intakes of plain water, moisture in foods and beverages, and total water in the adult US population—nutritional, meal pattern, and body weight correlates: National Health and Nutrition Examination Surveys 1999-2006. Am J Clin Nutr 2009; 90: 655–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CT use more than triples in the ED, but use of the technology may be linked with a significant drop in hospitalizations. ED Manag 2011; 23: 116–117. [PubMed] [Google Scholar]
- Griffey RT, Sodickson A. Cumulative radiation exposure and cancer risk estimates in emergency department patients undergoing repeat or multiple CT. AJR Am J Roentgenol 2009; 192: 887–892. [DOI] [PubMed] [Google Scholar]
- Korley FK, Pham JC, Kirsch TD. Use of advanced radiology during visits to US emergency departments for injury-related conditions, 1998-2007. JAMA 2010; 304: 1465–1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenner DJ, Hall EJ. Computed tomography—an increasing source of radiation exposure. N Engl J Med 2007; 357: 2277–2284. [DOI] [PubMed] [Google Scholar]
- Fazel R, Krumholz HM, Wang Y et al. Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med 2009; 361: 849–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrandino MN, Bagrodia A, Pierre SA et al. Radiation exposure in the acute and short-term management of urolithiasis at 2 academic centers. J Urol 2009; 181: 668–672 discussion 673. [DOI] [PubMed] [Google Scholar]
- Smith AB, Dillon WP, Gould R et al. Radiation dose-reduction strategies for neuroradiology CT protocols. AJNR Am J Neuroradiol 2007; 28: 1628–1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul JF, Abada HT. Strategies for reduction of radiation dose in cardiac multislice CT. Eur Radiol 2007; 17: 2028–2037. [DOI] [PubMed] [Google Scholar]
- Cousins C, Sharp C. Medical interventional procedures-reducing the radiation risks. Clin Radiol 2004; 59: 468–473. [DOI] [PubMed] [Google Scholar]
- Heron DE, Godette KD, Wynn RA et al. Radiation medicine innovations for the new millenium. J Natl Med Assoc 2003; 95: 55–63. [PMC free article] [PubMed] [Google Scholar]
- Bernhardt P, Lendl M, Deinzer F. New technologies to reduce pediatric radiation doses. Pediatr Radiol 2006; 36(Suppl 2): 212–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulson EK, Weaver C, Ho LM et al. Conventional and reduced radiation dose of 16-MDCT for detection of nephrolithiasis and ureterolithiasis. AJR Am J Roentgenol 2008; 190: 151–157. [DOI] [PubMed] [Google Scholar]
- Lotan Y, Pace K, Tolley D et al. Economics of stone disease. In: Denstedt J, Khoury S (eds) 2nd International Consultation on Stone Disease at the 29th Congress of the Société Internationale d'Urologie. Health Publications: Paris, France, 2008. pp 23–30. [Google Scholar]
- Goldstone A, Bushnell A. Does diagnosis change as a result of repeat renal colic computed tomography scan in patients with a history of kidney stones? Am J Emerg Med 2010; 28: 291–295. [DOI] [PubMed] [Google Scholar]
- Kenney PJ. CT evaluation of urinary lithiasis. Radiol Clin North Am 2003; 41: 979–999. [DOI] [PubMed] [Google Scholar]
- Preminger GM, Tiselius HG, Assimos DG et al. 2007 guideline for the management of ureteral calculi. J Urol 2007; 178: 2418–2434. [DOI] [PubMed] [Google Scholar]
- Picozzi SC, Marenghi C, Casellato S et al. Management of ureteral calculi and medical expulsive therapy in emergency departments. J Emerg Trauma Shock 2011; 4: 70–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingsworth JM, Davis MM, West BT et al. Trends in medical expulsive therapy use for urinary stone disease in U.S. emergency departments. Urology 2009; 74: 1206–1209. [DOI] [PubMed] [Google Scholar]
- Brede C, Hollingsworth JM, Faerber GJ et al. Medical expulsive therapy for ureteral calculi in the real world: targeted education increases use and improves patient outcome. J Urol 2010; 183: 585–589. [DOI] [PubMed] [Google Scholar]
- NHAMCS. Public Use Microdata File Documentation. In ftp://ftp.cdc.gov/pub/Health\_Statistics/NCHS/Dataset\_Documentation/NHAMCS/.
- Pearle MS, Calhoun EA, Curhan GC. Urolithiasis. In: Litwin MS, Saigal CS (eds) Urologic Diseases in America. US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. US Government Printing Office: Washington, DC, 2007, pp 283–319. [Google Scholar]
- CDC. National Health and Nutrition Examination Survey. In http://www.cdc.gov/nchs/nhanes.htm.
- NHAMCS. Using Ultimate Cluster Models with NAMCS and NHAMCS Public Use Files. In http://www.cdc.gov/nchs/data/ahcd/ultimatecluster.pdf.