Nonalcoholic fatty liver disease: an emerging threat to obese and diabetic individuals (original) (raw)
Abstract
Nonalcoholic fatty liver disease (NAFLD) is the most common liver disease in the Western world and its incidence is increasing rapidly. NAFLD is a spectrum ranging from simple steatosis, which is relatively benign hepatically, to nonalcoholic steatohepatitis (NASH), which can progress to cirrhosis. Obesity, insulin resistance, type 2 diabetes mellitus, and dyslipidemia are the most important risk factors for NAFLD. Due to heavy enrichment with metabolic risk factors, individuals with NAFLD are at significantly higher risk for cardiovascular disease. Individuals with NAFLD have higher incidence of type 2 diabetes. The diagnosis of NAFLD requires imaging evidence of hepatic steatosis in the absence of competing etiologies including significant alcohol consumption. Liver biopsy remains the gold standard for diagnosing NASH and for determining prognosis. Weight loss remains a cornerstone of treatment. Weight loss of ∼5% is believed to improve steatosis, whereas ∼10% weight loss is necessary to improve steatohepatitis. A number of pharmacologic therapies have been investigated to treat NASH, and agents such as vitamin E and thiazolidinediones have shown promise in select patient subgroups.
Keywords: steatosis, steatohepatitis, fatty liver, thiazolidinediones
Introduction
Nonalcoholic fatty liver disease (NAFLD) is the name given to a spectrum of liver disorders associated with hepatic steatosis that is not due to significant alcohol consumption or other secondary causes, such as steatogenic medication, or inborn errors of metabolism (Table 1). This disorder encompasses a wide range of diseases, from simple steatosis, which is relatively benign, to hepatic inflammation, hepatocyte injury, and fibrosis, a syndrome referred to as nonalcoholic steatohepatitis (NASH), which can progress to cirrhosis.1–3 Over the last three decades, NAFLD has emerged as one of the leading causes of cirrhosis in the United States, and a large proportion of individuals who previously had been classified as having cryptogenic cirrhosis are now believed to have cirrhosis due to NASH.4
Table 1.
Common causes of hepatic macrovesicular steatosis
| - Obesity, type 2 diabetes, and dyslipidemia (NAFLD) |
|---|
| - Excessive alcohol consumption |
| - Hepatitis C (genotype 3) |
| - Wilson's disease |
| - Lipodystrophy |
| - Starvation |
| - Parenteral nutrition |
| - Abetalipoproteinemia and hypobetalipoproteinemia |
| - Medications (e.g., amiodarone, methotrexate, tamoxifen, corticosteroids) |
NAFLD is becoming an increasingly important health issue. In Western nations, including the United States, NAFLD has become the most common cause of chronic liver disease. The rate of NAFLD is increasing likely due to the rising prevalence of associated conditions such as obesity and type 2 diabetes mellitus (T2DM). It has been projected that, within the next two decades, NASH will become the predominant cause of cirrhosis requiring orthotopic liver transplantation.5,6
This review focuses on clinical aspects of NAFLD, such as epidemiology, natural history, need for liver biopsy, and treatment options. A detailed discussion of pathogenesis, genetic investigations, and histological classification is beyond the scope of this review, and interested readers are referred to several recent excellent reviews.7–14 A recently published multi-society practice guideline offers guidance on the diagnosis and management of NAFLD for practicing healthcare providers.15
Epidemiology of NAFLD
The epidemiology and natural history of NAFLD remain incompletely understood, although studies have begun to more clearly elucidate them. The incidence of fatty liver disease has been examined in only a few studies. In an early study from Japan, the incidence of NAFLD was estimated to be 31 per 1,000 person-years based on the incidence of elevated aminotransferases as a surrogate for NAFLD.16 In a more recent Japanese study, which employed biennially abdominal ultrasound examination of 1,635 Nagasaki atomic bomb survivors without NAFLD at baseline, the incidence of NAFLD was 19.9 per 1000 person-years (22.3 for men, 18.6 for women) and peaked in the sixth decade of life.17 The annual incidence of NAFLD in England was estimated to be 29 per 100,000 individuals in one study, but this frequency is likely an underestimation because it was based on outpatient hepatology referrals.18 In this study, the incidence of NAFLD was much higher than other types of chronic liver disease.
The estimated prevalence of NAFLD varies widely likely secondary to difference in the population studied and the method used to detect NAFLD. The prevalence of suspected NAFLD based on elevated aminotransferases without imaging is between 7% and 11%, but this likely is an underestimation because aminotransferases can be normal in individuals with NAFLD.19 The prevalence of significant hepatic steatosis in potential living donors for liver transplantation was 20% by liver biopsy.20 The prevalence of NAFLD in participants of the Dallas Heart Study, a multi-ethnic population based study in Dallas County, Texas, was 34% using magnetic resonance spectroscopy for hepatic triglyceride quantitation.21 The estimated prevalence of NASH is lower, ranging from 3 to 5% of the general population whereas the prevalence of NASH-related cirrhosis is unknown.19
Ethnicity has a significant impact on the prevalence of NAFLD. In the Dallas Heart Study, the prevalence of hepatic steatosis was 45% in Hispanics, 33% in non-Hispanic Caucasians, and 24% in African Americans.21 This difference in prevalence was only partially explained by differences in obesity and insulin resistance especially in African Americans where the prevalence of NAFLD was lower than in Caucasians with similar risk factors. This condition is highly prevalent in Asian population as well. For example, in a Korean study of potential liver donors who underwent liver biopsy, the presence of NAFLD was 51%, with 10% revealing >30% steatosis and 2.2% with NASH.22
Gender has a significant impact on the prevalence of NAFLD, with most epidemiologic studies demonstrating almost twice the prevalence of NAFLD in males compared with females. In a study of 26,527 subjects undergoing medical checkups in China, the prevalence of NAFLD by abdominal ultrasound was 31% in men and 16% in women.23 Similarly, a population based study in India demonstrated a 25% prevalence of NAFLD in men compared with 14% in women.24 The prevalence of NAFLD in the Dallas Heart Study was 42% in white men compared with only 24% in white women and this difference was not attributable to differences in body weight or insulin sensitivity.21 However, this study found no gender difference in the prevalence of NAFLD in Hispanic and Black Americans. Studies have suggested that estrogen may reduce the risk of developing NAFLD.25
Jejunoileal bypass surgery has long been recognized as a cause of NAFLD likely due to the rapidity of weight loss and bacterial overgrowth leading to increased levels of endotoxin in the portal circulation.26,27 This procedure has now been abandoned, and the current foregut bariatric surgical procedures are not believed to cause or significantly worsen NAFLD. The efficacy and role of foregut bariatric surgery in individuals with NAFLD will be discussed later in detail. Pancreaticoduodenectomy has also been associated with an increased risk of subsequent development of NAFLD. In one series from Japan, the incidence of NAFLD after pancreatico-duodenectomy NAFLD was 37% with 10% exhibiting NASH.28
A number of studies have examined the prevalence of NAFLD in patients attending obesity clinics or undergoing bariatric surgery. The reported prevalence of NAFLD in this group ranges from 57% to 91% whereas the prevalence of NASH ranged from 26% to 37%.22,29–31 Unsuspected cirrhosis was 1.6–1.7%.29,30
Although obesity, insulin resistance, T2DM, and dyslipidemia are the most important risk factors, other endocrine conditions, such as hypothyroidism, hypopituitarism, hypogonadism, and polycystic ovary syndrome, are also associated with NAFLD (Table 2).32–35
Table 2.
Risk factors associated with NAFLD
| Major risk factors | Conditions with emerging association |
|---|---|
| Truncal obesity and insulin resistance | Hypothyroidism |
| Obstructive sleep apnea | |
| Type 2 diabetes mellitus | Hypopituitarism |
| Hypogonadism | |
| Hypertriglyceridemia | Pancreaticoduodenal |
| Metabolic syndrome | resection |
| Polycystic ovary syndrome |
Relationship of NAFLD to obesity and diabetes
The majority of patients with NAFLD have metabolic risk factors, such as obesity, T2DM, and dyslipidemia. Conversely, the presence of NAFLD is a risk factor for the subsequent development of some metabolic disorders such as T2DM. T2DM is not only a risk factor for the development of NAFLD but also a risk factor for the development of cirrhosis and hepatocellular carcinoma.36,37
Obesity and dyslipidemia are well-established risk factors for NAFLD. A Japanese study found that obesity, low high-density lipoprotein-cholesterol, hypertriglyceridemia, glucose intolerance, and hypertension were risk factors for the development of NAFLD, though in the multivariate analysis, only obesity, hypertriglyceridemia, and hypertension remained predictive.17 Similarly, a Korean study of living donors found obesity, older age, and hypertriglyceridemia were independent risk factors for NAFLD.22 The prevalence of NAFLD in patients referred to a lipid clinic was found to be 50% in one series.38 Visceral fat accumulation appears to be a significant risk for the development of NAFLD. A study from Japan found that the severity of hepatic steatosis by ultrasound was positively correlated with visceral fat accumulation and insulin resistance in both obese and nonobese subjects, suggesting that hepatic steatosis may be influenced by visceral fat accumulation regardless of body mass index.39
Metabolic syndrome, as defined by the Adult Treatment Panel (ATP) III criteria, is defined by the presence of three or more of the following: (1) waist circumference greater than 102 cm in men or greater than 88 cm in women; (2) triglyceride level greater than 150 mg/dL (1.7 mmol/L) or drug treatment for elevated triglycerides; (3) high-density lipoprotein (HDL) cholesterol level less than 40 mg/dL (1.03 mmol/L) in men and less than 50 mg/dL (1.29 mmol/L) in women or on drug treatment for low HDL; (4) systolic blood pressure ≥130 mm Hg or diastolic pressure ≥85 mm Hg or treatment for hypertension; and (5) fasting plasma glucose level ≥110 mg/dL or drug treatment for elevated blood glucose.40 Patients with metabolic syndrome have an increased prevalence of NAFLD with 86% of patients with metabolic syndrome having NAFLD, 24% exhibiting steatohepatitis, and unexpected cirrhosis in 2% by liver biopsy.41 An observational study from Japan demonstrated that men and women with metabolic syndrome at baseline were more likely to develop NAFLD during a 14 month follow-up with an adjusted odds ratio of 4.0 and 11.2, respectively.42 Conversely, NAFLD increases the risk for subsequent development of metabolic syndrome.43
Insulin resistance and diabetes are both very important risk factors for the development of NAFLD. Several studies have demonstrated that an elevated insulin resistance index, either HOMA-IR greater than 5.8 or FAIR score of 2 or greater, is a risk factor for the development of NAFLD in overweight nondiabetic individuals.29,30 In one series of patients undergoing gastric bypass, the odds of NASH were 128 times greater and the odds of severe fibrosis 75 times greater in patients with T2DM than in those without T2DM.31 Several recent studies have observed that adipose tissue insulin resistance (Adipo IR) may be an important predictor of liver histology in individuals with NAFLD and may indeed predict fibrosis progression.44,45 There are unconfirmed reports that T1DM is associated with NAFLD but these reports have not provided histological confirmation of hepatic fat accumulation.46,47
NAFLD is an independent risk factor for the development of T2DM. A study from South Korea examined the effect of NAFLD on the risk of subsequent development of T2DM in patients with impaired fasting glucose. The incidence of T2DM in the NAFLD group was 9.9% compared with 3.7% in the non-NAFLD group suggesting that NAFLD has an independent and additive effect on the development of T2DM in individuals with insulin resistance.48
Natural history of NAFLD
The natural history of NAFLD has been examined in a number of studies, although it remains incompletely understood. The majority of patients with simple steatosis will not develop NASH or advanced fibrosis. However, simple steatosis may not be totally benign as a portion of patients will progress to NASH. Approximately 23% of patients with simple steatosis noted on an initial liver biopsy were found to have NASH on a subsequent liver biopsy 36 months later.37 However, patients with NASH are certainly at risk for histologic progression including the development of cirrhosis. Age and the degree of inflammation observed in the initial liver biopsy are risk factors for progression to advanced fibrosis.49 Although only a small percentage of patients with NAFLD will eventually develop cirrhosis, given the large number of patients with NAFLD, this represents a significant disease burden. It is estimated that approximately 5% of patients with NAFLD develop cirrhosis.1
Subjects with NAFLD are at significantly higher risk for cardiovascular disease, and in fact cardiovascular events are their most common cause of death (Table 3). This association likely reflects high prevalence of metabolic risk factors in individuals with NAFLD, rather than additional atherogenic risk posed by the hepatic steatosis itself. Compared to simple steatosis, NASH has higher liver-related mortality with an odds ratio (OR) of 5.71 for NASH and an OR of 10.06 for NASH with advanced fibrosis.50 The cardiovascular mortality was found to be similar between patients with simple steatosis and those with NASH.50 When compared to patients with chronic hepatitis C, patients with NAFLD with advanced fibrosis or cirrhosis have lower rates of liver-related complications and hepatocellular cancer but similar overall mortality.51
Table 3.
Incidence of cardiovascular disease in patients with NAFLD in selected longitudinal studies148
| Author (Ref.) | Number of subjects | Diagnosis of NAFLD | Follow-up duration (years) | Proportion of deaths due to cardiovascular disease | Comment |
|---|---|---|---|---|---|
| Soderberg145 | 118 | Histology | 24 (median) | 30% | CVD is the most common cause of death |
| Ekstedt2 | 129 | Histology | 13.7 ± 1.3 (mean) | 16% | CVD is the most common cause of death |
| Adams1 | 421 | Imaging | 7.6 ± 4.0 (mean) | 25% | CVD is the 2nd most common cause of death after malignancy |
| Dam-Larsen146 | 170 | Histology | 20.4 (median) | 38% | CVD is the most common cause of death |
| Rafiq147 | 173 | Histology | 18.5 (median) | 12.7% | CVD is the most common cause of death |
Diagnosis of NAFLD
Diagnosis of suspected NAFLD involves establishing that the patient satisfies the diagnostic criteria for NAFLD and excluding the presence of other coexisting liver diseases. Diagnosis of NAFLD requires demonstration of hepatic steatosis by imaging or histology and exclusion of significant alcohol use or other secondary causes of steatosis. In addition to alcohol consumption, secondary causes of hepatic steatosis include medications, chronic hepatitis C infection, parenteral nutrition, and Wilson's disease (Table 1).
Liver biochemistries and other laboratory testing
In patients with suspected NAFLD, initial laboratory evaluation typically involves obtaining liver biochemistries and exclusion of chronic viral hepatitis, hemochromatosis, Wilson's disease, and autoimmune hepatitis via appropriate diagnostic tests.
In patients with NAFLD, serum aminotransferases can be normal or mildly elevated. Serum aminotransferases generally wax and wane and they rarely exceed 200 U/L. Typically, ALT exceeds AST although the serum AST frequently exceeds ALT when there is advanced fibrosis.52 Alkaline phosphatase can also be elevated as well, and patients can have only an isolated elevation of serum alkaline phosphatase with normal aminotransferase levels.53 NAFLD is the most common cause of incidentally found abnormal liver biochemistries in the primary care setting.54 The sensitivity of abnormal aminotransferases in detecting NAFLD is poor since 55% to 79% of individuals with NAFLD may have normal transaminase levels.21 In patients with NAFLD, neither the degree of elevation nor the pattern of abnormal liver biochemistries are reliable in determining that the disease activity and risk of disease progression. In addition, changes of aminotransferase levels do not parallel changes in fibrosis stage preventing them from being a reliable surrogate for fibrosis progression.55
Mildly elevated serum ferritin is common in patients with NAFLD though it is typically not associated with increased hepatic iron stores.56 However, elevated serum ferritin and transferrin saturation in patients with suspected NAFLD should prompt genetic testing for hereditary hemochromatosis. A liver biopsy should be considered in a patient with suspected NAFLD who is homozygous or compound heterozygous for the C282Y mutation in the HFE gene to assess hepatic iron concentration and to evaluate for significant liver injury and fibrosis.
Mild elevations of autoantibodies are relatively common in patients with NAFLD. A similar phenomenon has been observed in liver disorders such as viral hepatitis and drug-induced liver injury and is generally considered as an epiphenomenon. A recent study from the NASH Clinical Research Network (NASH CRN), found that positive serum autoantibodies, defined as antinuclear antibody (ANA) titer ≥1:160 or antismooth muscle antibody (ASMA) ≥1:40, were present in 21% of patients with biopsy-proven NAFLD and they were not associated with more advanced histologic features.57 However, if there are additional features suggestive of autoimmune hepatitis, such as markedly elevated aminotransferase, high γ-globulin, or high serum immunoglobulin G, then a liver biopsy may be considered necessary to firmly establish the diagnosis.
Several models have been developed that combine laboratory testing, demographic variables, and clinical data to predict NASH with advanced fibrosis, but their detailed discussion is beyond the scope of this review article. The NAFLD fibrosis score (http://nafldscore.com/) is a promising bedside tool for identifying NAFLD patients who are at high risk for advanced fibrosis, and it employs six easily available variables (age, hyperglycemia, body mass index, platelet count, albumin, and AST/ALT ratio).58 In a recent meta-analysis of 13 published studies, the NAFLD fibrosis score had a pooled area under the curve of a receiver operating characteristic (AUROC) of 0.85 for predicting advanced fibrosis (stage 3 or 4). The NAFLD fibrosis score less than 1.455 had 90% sensitivity and 60% specificity to exclude advanced fibrosis, while a score greater than 0.676 had 67% sensitivity and 97% specificity to identify the presence of advanced fibrosis.50 Enhanced liver fibrosis (ELF) panel employs automated immunoassay of three serum markers of matrix constituents and mediators of matrix remodeling (hyaluronic acid, amino-terminal propeptide of type III collagen, and tissue inhibitor of matrix metalloproteinase 1).59 The ELF panel has an AUROC of 0.90 for detection of advanced fibrosis with a threshold of 0.3576 associated with a sensitivity of 80%, a specificity of 90%, a positive predictive value of 71%, and a negative predictive value of 94%.60
Studies suggest that hepatocyte apoptosis plays an important role in the pathogenesis of NASH. Hepatocyte apoptosis results in caspase 3 generated cleavage fragment of cytokeratin-18 (CK-18) being released. The serum CK-18 fragments can be measured by ELISA, and they significantly increased in patients with NASH compared with simple steatosis and normal controls.61 The circulating levels of CK-18 fragments have been shown to reflect disease activity, and change in their level may correlate with the change in NAFLD activity score.37 In a recent meta-analysis, the pooled AUROC of serum CK-18 for detection of NASH was 0.82 with a sensitivity and specificity of 78% and 87%, respectively.50
Imaging
A number of imaging modalities have been employed in the diagnosis of NAFLD. Although several different imaging techniques are valuable in demonstrating steatosis, the ability of current imaging technologies to evaluate fibrosis and especially inflammatory activity is limited.
Abdominal ultrasound is a relatively inexpensive, noninvasive diagnostic test to demonstrate steatosis with excellent sensitivity in individuals with moderate to severe hepatic steatosis. Steatosis is visualized as increased echogenicity with bright liver echo pattern on ultrasound B-mode examination and increased attenuation.62 In a study of ultrasound paired with liver biopsy the reported sensitivity ultrasound for the detection steatosis of 64% to 91%, and a specificity of 93% to 97%.63,64 Morbid obesity was associated with a lower sensitivity, and higher degrees of steatosis with a greater sensitivity.
Noncontrast abdominal CT is also useful in demonstrating hepatic steatosis. When contrast enhanced CT is performed, the portal phase images should be employed for the determination of steatosis though contrast may result in decreased sensitivity and specificity compared with noncontrast scans.65 On a CT scan, hepatic steatosis is visualized as decreased attenuation of the liver, resulting in the liver appearing darker than the spleen and is associated with decreased liver attenuation index, which is the difference between the mean hepatic and splenic attenuation in Hounsfield units. The sensitivity of a CT scan for detecting steatosis greater than 30% was as high as 82% in a study involving potential living liver donors.65
Abdominal magnetic resonance imaging (MRI) is a sensitive technique for demonstrating steatosis. T1-weighted gradient-echo magnetic resonance images are acquired with an echo time such that water and lipid spins are in phase or opposed phase allowing lipid quantitation by relative loss of signal intensity on opposed-phase images compared with that on in-phase images.66 In a study of potential living donors MRI demonstrated a sensitivity, specificity, and accuracy of 100%, and 92.3%, and 93%, respectively, for detection of steatosis in patients with greater than 20% steatosis by liver biopsy.67 Magnetic resonance spectroscopy has been employed to quantitate hepatic steatosis by measuring hepatic triglyceride content although its use remains primarily investigational.68
Heterogeneity of hepatic steatosis including focal sparing is a relatively common finding with each of the imaging modalities.69–74 The most common locations are the gallbladder fossa, and the areas adjacent to the porta hepatis and falciform ligament. Conversely, focal fatty infiltration can also be observed where steatosis is increased in only one region of the liver.
Transient elastography is an ultrasound-based noninvasive method of assessing of fibrosis through measurement of liver stiffness. Although insensitive for detection of early fibrosis, transient elastography can be useful in screening for advanced fibrosis in many patients. In a study involving patients with NAFLD, transient elastography demonstrated a sensitivity of 91% and a specificity of 75% for detecting stage 3 or higher fibrosis with positive and negative predictive values of 52% and 97%, respectively.75 Unfortunately, body habitus can limit the application of this study since there is an increased failure rate in obtaining a successful transient elastography measurement with increasing degree of obesity. Also, transient elastography is not currently commercially available in the United States. Magnetic resonance elastography is a promising technique that measures liver stiffness over a larger region of the liver than transient elastography; this research tool is currently available at a limited number of centers.
Liver biopsy
Liver biopsy remains the gold standard for characterizing the histology of NAFLD. It can play an important role in the diagnosis of NAFLD, but it is expensive and carries risk of morbidity and very rarely mortality. Histological examination of liver tissue allows for exclusion of competing etiologies as well as for the assessment of coexisting liver diseases. Currently, liver biopsy is the only tool available for assessing the degree of inflammation and cell injury and to stage for the degree of fibrosis. It is invaluable to differentiate simple steatosis from NASH.
Macrovesicular steatosis is a predominant feature of NAFLD, and the presence of steatosis in greater than 5% of hepatocytes is generally accepted as fatty liver (Fig. 1A).76 In addition to steatosis, common histologic findings in NASH include hepatocyte ballooning, lobular inflammation that is either mixed type or neutrophil predominant, and varying degrees of fibrosis (Figs. 1B and C).77 There are no histologic features that reliably differentiate NASH for alcoholic hepatitis, and the term NASH was originally employed in a report from the Mayo Clinic regarding 20 patients with a liver disease that histologically mimicked alcoholic hepatitis in patients without significant alcohol intake.78 A histopathological classification system for NASH was originally developed by Brunt et al., with histologic features distinctive to NASH employed in determining the necroinflammatory activity (grade) and architectural alterations (stage).79 The NAFLD activity score (NAS), an unweighted sum of steatosis, inflammation, and ballooning scores, was developed by the NASH CRN as a tool to quantify changes in liver histology in NAFLD therapeutic trials.76 There is not a threshold value of NAS that reliably identifies the presence of NASH.80
Figure 1.
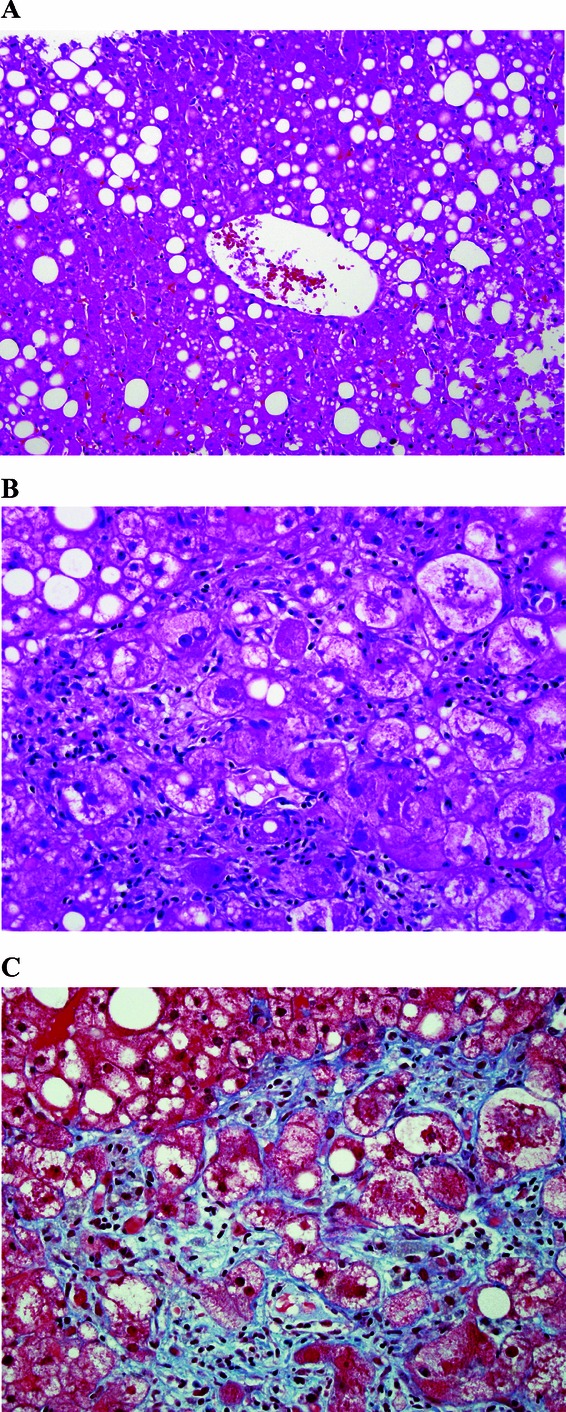
(A) Liver histology demonstrating moderate macrovesicular steatosis around the central vein. Hematoxylin and eosin staining, with magnification of 200×. (B) Liver histology demonstrating active steatohepatitis with steatosis, ballooned hepatocytes, inflammatory infiltrate, and Mallory's Hyaline. Hematoxylin and eosin staining, with magnification of 400×. (C) Liver histology demonstrating steatohepatitis with extensive pericellular fibrosis. Trichrome staining, with magnification 400×. Figure courtesy of David Kleiner, MD, National Cancer Institute.
There can be significant sampling error due to the small portion of the liver sampled by a biopsy and the inhomogeneous distribution of the histologic lesions of NASH. This sample variability is moderate for hepatocyte ballooning and perisinusoidal fibrosis and is somewhat higher for lobular inflammation.81,82
Pathogenesis of NAFLD
Several pathophysiologic mechanisms have been proposed to explain the basis for fat accumulation, liver injury, and fibrosis in NAFLD, but their detailed discussion is beyond the scope of this review article. Interested readers are alerted to several recent comprehensive reviews on this subject.7,8,10,83,84 Despite considerable research in this area, the pathogenesis of NAFLD remains incompletely understood. It has been very challenging to differentiate causative factors from associated phenomena and downstream effects. Although there is an increased understanding of the pathogenesis of hepatic fat accumulation, there are critical knowledge gaps in our understanding of mediators and mechanisms of hepatocyte injury, mediators of stellate cell activation, and fibrosis. It remains a puzzle why some individuals with NAFLD have advanced histological features and develop cirrhosis whereas others with comparable risk factor profile have simple steatosis with minimal or no disease progression. A genetic basis for inter-individual phenotypic variability is strongly suspected, but genetic studies are very limited in individuals with histologically characterized NASH.
Insulin resistance is nearly universal in NAFLD and it is believed to play a crucial role in the pathogenesis of NAFLD. In adipocytes, insulin resistance results in increased activity of hormone-sensitive lipase, which results in lipolysis of triglycerides and release of free fatty acids into circulation. Fatty acids taken up by hepatocytes from circulation and produced by de novo lipogenesis undergo esterification resulting in hepatocytes steatosis. Initially it was proposed that NASH resulted from a “two-hit” mechanism with hepatocyte steatosis being the initial metabolic insult that then allows a second injury leading to NASH.85 However, subsequent research has cast significant doubt on this paradigm, and it is now widely believed that free fatty acids and their metabolic products (e.g., diacylglycerol) and sequelae (e.g., free radicals) are the likely mediators of hepatocyte injury.8,86–89
At a cellular level, several different mechanisms have been proposed for causing hepatocyte injury, including apoptosis, perturbations in autophagy, mitochondrial dysfunction, alterations in natural killer T cell and Kupffer cell function, and an increase in inflammatory cytokines.8,90–96 Apoptosis appears to play an important role in hepatocyte death in NAFLD, and free fatty acids could be the primary mediators of hepatocyte apoptosis (lipoapoptosis).83,90 In addition, phagocytosis of hepatocyte apoptotic bodies by stellate cells leads to their activation and likely plays an important role in fibrosis.
Treatment of NALFD
Lifestyle modification
Lifestyle modification is the cornerstone of treatment of NAFLD. These interventions are not only effective in improving NAFLD but also associated conditions such as metabolic syndrome, T2DM, and the related risk of cardiovascular disease.
Weight reduction plays an important role in the treatment of NASH. Weight loss has been shown to decrease hepatic steatosis and improve abnormal aminotransferase levels.97–99 Weight loss can be an effective treatment to improve the histology of NASH if patients can attain sufficient weight reduction. In a study by Harrison et al., subjects with biopsy-proven NASH who lost 5% of body weight had improvement in insulin sensitivity and hepatic steatosis compared with those who lost less than 5% of their body weight.100 However, it was only in subjects who achieved at least 9% weight reduction that there was significant improvement in inflammation, ballooning, and NAS. A randomized controlled trial (RCT) involving patients with biopsy-proven NASH by Promrat et al. examined the efficacy of lifestyle intervention using a combination of diet, exercise, and behavior modification compared to the control group that received structured education.101 The primary end-point in this study was improvement in liver histology. Participants who achieved the study weight loss goal of at least 7% had significant improvements in steatosis, lobular inflammation, and ballooning injury. Percent weight reduction correlated significantly with improvement in NAS. Weight loss has been shown to prevent progression of fibrosis in NASH.37
However, very rapid weight loss may lead to increased portal inflammation and fibrosis. In a small study of severely obese patients with NAFLD who were placed on a very low calorie formula diet resulting in a median weight loss of 34 kg over an 8-week period, 24% of patients developed mild portal inflammation or portal fibrosis.102 Therefore, one should be cautious in recommending very low calorie diets for individuals with NAFLD.
Weight reduction surgery
Because NAFLD is present in the majority of patients who undergo bariatric surgery, there has been an interest in foregut bariatric surgery as a potential treatment option for NASH. Currently, there are no RCTs that have examined foregut bariatric surgery as a treatment option for NAFLD or NASH. However, several retrospective and prospective cohort studies have compared liver histology in the severely obese individuals before and after bariatric surgery. Unfortunately, a majority of them do not have uniform histologic evaluation by post-bypass liver biopsies and instead performed biopsies at varying intervals and only in selected patients undergoing other surgical procedures such as abdominal hernia repair. However, one exception is the seminal study by Mathurin et al., that prospectively correlated clinical and metabolic data with liver histology before and 1 and 5 years after bariatric surgery in 381 adult patients with severe obesity.103 There was a significant improvement in steatosis and ballooning at 1 and 5 years following bariatric surgery compared to baseline. In patients with probable or definite NASH at baseline, there was significant improvement in steatosis, ballooning, and NAS and resolution of probable or definite NASH at 1 and 5 years following bariatric surgery. The majority of histological benefits were present at 1 year with no differences in liver histology between 1 and 5 years following bariatric surgery. Because no patient in this study had cirrhosis at baseline, the effect of bariatric surgery in patients with cirrhosis could not be evaluated.
There are two meta-analyses that evaluated the influence of bariatric surgery on liver histology in adults with NAFLD. Mummadi et al. found that steatosis, steatohepatitis, and fibrosis improve or completely resolve after bariatric surgery in a significant proportion of patients.104 However, a Cochrane review concluded that lack of RCTs or other high-quality clinical studies prevents definitive determination of benefits and risks of bariatric surgery as a treatment option for patients with NASH.105
A recently published multi-society practice guideline concluded that it is premature to consider foregut bariatric surgery as an established option to specifically treat NASH.15 However, it concluded that foregut bariatric surgery is not contraindicated in otherwise eligible obese individuals with NAFLD or NASH.
Vitamin E
Oxidative stress has been proposed as an important mediator of hepatic injury in NASH.88,106,107 Vitamin E comprises a series of closely related compounds with antioxidant activity that have been employed in several therapeutic trials of NASH, although small sample sizes, differences in vitamin E preparations, and differences in endpoints have made them difficult to compare. The PIVENS trial, a recent randomized double blind placebo controlled trial, is the largest study to investigate the effectiveness of vitamin E supplementation on nondiabetic adults with histologically confirmed NASH.108 This study employed unmodified RRR-alpha-tocopherol administered as a once daily dose of 800 IU given for 96 weeks. Vitamin E supplementation resulted in significant improvement in pathologic features of NASH with improvement in NAS seen in 42% of patients receiving vitamin E compared with 19% of patients receiving placebo with a number needed to treat of 4.4. Compared with placebo, vitamin E significantly improved aminotransferases as well. Vitamin E was well tolerated in this trial. The effectiveness of vitamin E supplementation has not been evaluated in diabetic patients with NASH or in patients with NASH-related cirrhosis.
Some concerns have been raised regarding the long-term safety of vitamin E, although current data suggest that serious toxicity from vitamin E is likely very small if present. A recent RCT of vitamin E administered at a dose of 400 IU/day found a statistically non-significant increase in prostate cancer risk in the vitamin E group with an absolute increased risk of 1.6 per 1,000 person years of vitamin E use.109 Whether vitamin E supplementation may increase all-cause mortality remains controversial. While some early meta-analyses suggested a possible increase in all-cause mortality associated with vitamin E supplementation, subsequent studies have failed to demonstrate any increased mortality.110–115
Insulin-sensitizing agents
Insulin-sensitizing agents have been investigated extensively in therapeutic trials since insulin resistance is believed to play an important role in the pathogenesis of NAFLD.
Metformin has been employed in a number of therapeutic trials of NASH. While several small open-label studies suggested some improvement in aminotransferase levels with metformin therapy, a study in which only the metformin arm underwent biopsy suggested that it might lead to histologic improvement.116 However, subsequent randomized, placebo controlled clinical trials have failed to show a significant difference in liver histology in nondiabetic patients with insulin resistance and NASH.117,118 Because metformin does not have a significant effect on liver histology in patients with NASH compared with lifestyle modification alone, the use of metformin as therapy for NASH is not recommended.15
Thiazolidinediones (TZDs) are oral antidiabetic medications that increase insulin sensitivity by activation of peroxisome proliferator-activated receptors present in a number of tissues, including liver, skeletal muscle, and adipose tissue. An early nonrandomized trial, involving 22 patients with biopsy-proven NASH (including 50% with impaired glucose tolerance and diabetes) treated with rosiglitazone 4 mg twice daily for 48 weeks, demonstrated improvement in inflammation, hepatocyte ballooning, and fibrosis on an end-of-treatment liver biopsy.119 However, weight gain occurred in 67% of patients with a median body weight increase of 7.3%.
The RCTs of TZDs have generally shown histologic improvement with TZDs in patients with NASH, although there has been variability in certain parameters, such as improvement in inflammation and fibrosis. In an early double-blind placebo controlled study by Belfort et al., pioglitazone (45 mg/day) combined with a hypocaloric diet significantly improved steatosis, hepatocyte ballooning, and inflammation compared with a hypocaloric diet alone in patients with biopsy-proven NASH and either T2DM or insulin resistance.120 Improvement in the NAS was seen in 73% of patients treated with pioglitazone compared to 24% of placebo-treated patients (P < 0.001), and there was a trend toward improvement in fibrosis in patients receiving pioglitazone (P < 0.08). A randomized trial of 63 patients with biopsy-proven NASH by Ratziu et al., found that rosiglitazone treatment (4 mg/day for the first month and 8 mg/day thereafter) for one year improved aminotransferases and hepatic steatosis, but not necroinflammation, fibrosis or NAS.121 A two-year open-label extension phase of this study demonstrated similar results with no significant improvement in hepatocyte ballooning, intralobular inflammation, fibrosis, or NAS seen in the rosiglitazone treatment group compared with the control group.122 Aithal et al., conducted a randomized, placebo-controlled trial of lifestyle intervention with either pioglitazone (30 mg/day) or placebo for 12 months in a total of 74 nondiabetic patients with NASH.123 Although steatosis did not improve significantly compared to placebo, cellular injury and fibrosis improved significantly. Weight gain was observed in the TZD group in each of these studies and ranged from 1.5 to 2.77 kg, whereas the placebo control groups lost 0.55 to 1 kg.
The PIVENS study is a recent large RCT that randomized 247 nondiabetic patients with biopsy-proven NASH to pioglitazone (30 mg/day), vitamin E (800 IU/day), or placebo for 24 months.124 The primary endpoint was an improvement in NAS by at least 2 points, with at least a one-point improvement in hepatocellular ballooning and a one-point improvement in either the lobular inflammation or steatosis score, and no increase in the fibrosis score.108 This endpoint was achieved in 34% of the pioglitazone group (P = 0.04 vs. placebo) and 43% of the vitamin E group (P = 0.001 vs. placebo) compared with 19% in the placebo group. The resolution of NASH, a key secondary end point, was achieved in significantly higher percentage of patients receiving pioglitazone compared with placebo (47% vs. 21%, P = 0.001). Similar to prior trials, pioglitazone was associated with a 4.7 kg weight gain compared to placebo. A recent meta-analysis that included four high quality randomized placebo controlled trials showed that TZDs significantly improved steatosis (OR 3.39, 95% 2.19–5.25), inflammation (OR 2.58, 95% CI: 1.68–3.97), and ballooning (OR 2.11, 95% CI:1.33–3.36), but not fibrosis (combined OR 1.40, 95% CI 0.87–2.24).125 When studies involving pioglitazone alone were analyzed, there was statistically significant improvement in fibrosis (combined OR 1.68, 95% CI: 1.02–2.77).
The addition of metformin to rosiglitazone has recently been investigated but metformin did not offer additional histologic improvement over rosiglitazone treatment alone in two open-labeled RCTs and more importantly metformin did not mitigate TZD associated weight gain.118,126
There is considerable debate about the long-term safety of TZDs with reference to increased risk of cardiovascular events, congestive heart failure (CHF), bladder cancer, and bone loss. A meta-analysis of trials involving rosiglitazone demonstrated a significant increase in the rate of myocardial infarction (OR 1.43, 95% CI 1.03 to 1.98, P = 0.03).127 This is distinct from the meta-analysis of 19 trials of pioglitazone enrolling a total of 16,390 patients with T2DM, pioglitazone treatment was associated with a significant reduction in the primary outcome of death, myocardial infarction, or stroke (P = 0.005).128 However, there was increased incidence of CHF with pioglitazone (2.3% vs. 1.8% in the control group, P = 0.002). Therefore, caution must be exercised when considering TZDs in patients with preexisting cardiac disease. Owing to increased risk of cardiac events, rosiglitazone availability is highly restricted in the United States and is no longer marketed in Europe.
Statins, omega-3 fatty acids, and ursodeoxycholic acid
Dyslipidemia is almost universal in patients with NAFLD, and the effect of lipid-lowering therapy with statins on NALFD has been evaluated in several studies. The St. Francis Heart Study demonstrated that atorvastatin 20 mg combined with vitamins C and E is effective in reducing the odds of having hepatic steatosis as determined by CT although no histologic evaluation was performed.129 The post hoc analysis of the Greek Atorvastatin and Coronary Heart Disease Evaluation (GREACE) study of 227 patients with possible NAFLD based on moderately abnormal liver tests at baseline treated with a statin demonstrated improvement in liver tests without an increase in liver-related adverse effects compared with controls.130 Several other studies have demonstrated that statins are safe in patients with liver disease, and there is no evidence that patients with NAFLD are at increased risk for serious liver injury from statins compared with those without liver disease.131–134 There are no RCTs with histological end points that have examined the use of statins in the treatment of NASH, and thus statins specifically to treat NASH cannot be advocated at this time.15
Treatment of NAFLD with fish oil supplementation or polyunsaturated fatty acids that are enriched in fish oil omega 3 fatty acids has been investigated in animal studies and a small number of preliminary human studies. Epidemiologic studies have suggested that there may be an inverse relationship between the level of fish oil intake and risk of NAFLD.135,136 However, the association is relatively modest and was not statistically significant in some studies after adjusting for confounding factors. Several small nonrandomized open-label study of omega-3 fatty acids alone or with supplements such as olive oil have found improvement in liver tests, serum triglycerides, and steatosis by ultrasound.137–140 A large multicenter trial of the omega-3 fatty acid eicosapentanoic acid to treat NASH is ongoing in the United States. At this point, it is premature to recommend omega-3 fatty acids for the treatment of NAFLD although they may be considered for the treatment of hypertriglyceridemia.
There has been interest in the use of ursodesoxycholic acid (UDCA) to treat NAFLD although studies to date have yielded disappointing results. UDCA is a secondary bile acid that is approved for the treatment of primary biliary cirrhosis and has effects on cholesterol absorption and inflammation. Initial small uncontrolled clinical studies suggested that UDCA may offer benefit to individuals with NASH. However, a two-year prospective, double-blind trial of UDCA (13–15 mg/kg per day) of 166 patients failed to demonstrate improvement in laboratory data or liver histology.141 Subsequent studies have employed high dose UDCA with mixed results. A RCT of high-dose UDCA (28–35 mg/kg per day) given for 12 months in patients with NASH by Ratziu et al., demonstrated that UDCA improved transaminase levels and markers of insulin resistance and fibrosis.142 Critically, no histologic evaluation was performed. Leuschner et al. performed a double-blind, randomized, placebo-controlled trial of high-dose UDCA (23–28 mg/kg/day) in 185 patients with histologically proven NASH.143 The treatment was provided over 18 months with both pre- and posttreatment liver biopsies. Although lobular inflammation was improved in patients in the treatment group, there was no improvement in fibrosis and no significant difference in NAS between the treatment and control group. In summary, there is no evidence that UDCA is effective to treat NASH.
Emerging therapies
Table 4 describes selected compounds that are being tested in large phase 2/3 studies. A large randomized placebo controlled trial of two doses of eicosapentanoic acid is near completion in the United States and its results are eagerly awaited. Pentoxifylline has shown encouraging histological benefits in several small studies and it is a suitable candidate for further testing in large multicenter RCTs. The NASH CRN is conducting a multicenter RCT of obeticholic acid in adults with NASH and a multicenter RCT of cysteamine bitartrate in children with NASH. Their results will not be available until 2014 and 2015, respectively. Obeticholic acid is a novel FXR agonist, whereas cysteamine bitartrate is a potent antioxidant.
Table 4.
Selected compounds with high therapeutic potential that are currently being investigated in phase2/3 studies
| Compound | Nature of the trial | Potential mechanism of action | Primary end point | Comment |
|---|---|---|---|---|
| Eicosapentanoic acid | Multicenter phase 2/3 study in the United States; sponsored by Mochida Pharmaceuticals | Decreased lipogenesis and improved insulin sensitivity | Liver histology | To be completed soon; results awaited |
| Pentoxifylline | Several small studies have shown histological benefits | Anti-TNF-α | Liver histology | Suitable agent for large-scale definitive studies |
| Obeticholic acid | Large placebo-controlled, phase 2b is under way in the United States; conducted by the NASH CRN under a CRADA agreement with Intercept Pharmaceuticals | Farsenoid X receptor agonist | Liver histology | Results will become available in 2014 |
| Cysteamine bitartrate | Large placebo-controlled, phase 2b trial in children with NASH is under way; conducted by the NASH CRN under a CRADA agreement with Raptor Pharmaceuticals | Potent antioxidant | Liver histology | Results to become available in 2015 |
| GFT 505 | Multicenter, placebo-controlled RCT to be initiated soon; sponsored by Genfit | GFT 505 is a dual PPAR α/δ agonist | Liver histology | To be initiated soon |
| GS 6624 | Two separate phase 2b studies to be initiated internationally by Gilead Pharmaceuticals | GS 6624 is a parenteral compound, and it is a monoclonal antibody against a lysyl oxidase–like molecule | Reversal of cirrhosis by histology is the primary end point for the cirrhosis study; however, progression of fibrosis is the end point for the advanced fibrosis study | To be initiated soon |
| In adults with compensated cirrhosis | ||||
| In adults with advanced fibrosis |
Surveillance for the development of complications
In addition to their risk of developing cirrhosis, liver failure, and hepatocellular cancer, patients with NAFLD are at significantly higher risk for developing diabetes and cardiovascular disease, and thus there should be heightened attention to monitoring for the development of these conditions.
In patients with NASH related cirrhosis, regular surveillance for cirrhosis related complications such as hepatocellular carcinoma (HCC) and esophageal varices should be performed. As with other causes of cirrhosis, surveillance for HCC should be performed every 6 months with abdominal ultrasound, or intravenous contrast enhanced abdominal CT or MRI. Yearly cumulative incidence of HCC in patients with NASH-related cirrhosis was found to be 2.6% in one series. This was less than the yearly cumulative incidence in patients with hepatitis C cirrhosis of 4.0% though the difference was not statistically significant.144
Conclusions
Individuals with obesity and T2DM are at significantly higher risk for NAFLD. The incidence of NAFLD is rapidly increasing throughout the world due to the increasing frequency of obesity and T2DM. The NAFLD is a spectrum of chronic liver diseases ranging from simple steatosis, which is relatively benign from a liver standpoint, to NASH, which can progress to cirrhosis and liver failure. The diagnosis of NAFLD requires imaging evidence of hepatic steatosis while excluding competing etiologies, such as significant alcohol consumption, viral hepatitis, and hemochromatosis. Liver biopsy remains the gold standard for diagnosing NASH and for assessing fibrosis. Recent advances in laboratory testing and noninvasive imaging have shown promise for identifying steatohepatitis and advanced fibrosis in individuals with NAFLD. Weight loss of at least 5% is required to improve steatosis, whereas weight loss in the range of 7–10% may be needed to improve steatohepatitis. A number of pharmacologic therapies have been evaluated in NASH, and agents such as vitamin E and TZDs have shown some promise. Ongoing studies hold promise for developing more effective diagnostic tests and therapies.
Acknowledgments
This work is in part supported by NIH K24 DK069290A Grant to NC.
Conflicts of interest
N. Chalasani received fees from Merck, Glaxo SmithKline, Biolex, J & J, Mochida, Salix, Aegerion, and Sanofi-Aventis for providing consulting related to NAFLD/NASH or drug hepatotoxicity in the last 12 months. He has received research support from Lilly, Cumberland Pharmaceuticals, and Intercept. H. Masuoka has no financial conflicts to declare.
References
- 1.Adams LA, Lymp JF, St Sauver J, et al. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology. 2005;129:113–121. doi: 10.1053/j.gastro.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 2.Ekstedt M, Franzen LE, Mathiesen UL, et al. Long-term follow-up of patients with NAFLD and elevated liver enzymes. Hepatology. 2006;44:865–873. doi: 10.1002/hep.21327. [DOI] [PubMed] [Google Scholar]
- 3.Ratziu V, Poynard T. Assessing the outcome of nonalcoholic steatohepatitis? It's time to get serious. Hepatology. 2006;44:802–805. doi: 10.1002/hep.21391. [DOI] [PubMed] [Google Scholar]
- 4.Caldwell SH, Oelsner DH, Iezzoni JC, et al. Cryptogenic cirrhosis: clinical characterization and risk factors for underlying disease. Hepatology. 1999;29:664–669. doi: 10.1002/hep.510290347. [DOI] [PubMed] [Google Scholar]
- 5.Charlton M. Nonalcoholic fatty liver disease: a review of current understanding and future impact. Clin. Gastroenterol. Hepatol. 2004;2:1048–1058. doi: 10.1016/s1542-3565(04)00440-9. [DOI] [PubMed] [Google Scholar]
- 6.Charlton MR, Burns JM, Pedersen RA, et al. Frequency and outcomes of liver transplantation for nonalcoholic steatohepatitis in the United States. Gastroenterology. 2011;141:1249–1253. doi: 10.1053/j.gastro.2011.06.061. [DOI] [PubMed] [Google Scholar]
- 7.Nguyen TA, Sanyal AJ. Pathophysiology guided treatment of nonalcoholic steatohepatitis. J. Gastroenterol. Hepatol. 2012;27(Suppl 2):58–64. doi: 10.1111/j.1440-1746.2011.07018.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ibrahim SH, Kohli R, Gores GJ. Mechanisms of lipotoxicity in NAFLD and clinical implications. J. Pediatr. Gastroenterol. Nutr. 2011;53:131–140. doi: 10.1097/MPG.0b013e31822578db. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brunt EM. Non-alcoholic fatty liver disease: what's new under the microscope? Gut. 2011;60:1152–1158. doi: 10.1136/gut.2010.218214. [DOI] [PubMed] [Google Scholar]
- 10.Cohen JC, Horton JD, Hobbs HH. Human fatty liver disease: old questions and new insights. Science. 2011;332:1519–1523. doi: 10.1126/science.1204265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anstee QM, Daly AK, Day CP. Genetics of alcoholic and nonalcoholic fatty liver disease. Semin. Liver Dis. 2011;31:128–146. doi: 10.1055/s-0031-1276643. [DOI] [PubMed] [Google Scholar]
- 12.Fujii H, Kawada N. Inflammation and fibrogenesis in steatohepatitis. J. Gastroenterol. 2012;47:215–225. doi: 10.1007/s00535-012-0527-x. [DOI] [PubMed] [Google Scholar]
- 13.Cusi K. Role of obesity and lipotoxicity in the development of nonalcoholic steatohepatitis: pathophysiology and clinical implications. Gastroenterology. 2012;142:711–725 e716. doi: 10.1053/j.gastro.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 14.Aly FZ, Kleiner DE. Update on fatty liver disease and steatohepatitis. Adv. Anat. Pathol. 2011;18:294–300. doi: 10.1097/PAP.0b013e318220f59b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice Guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Hepatology. 2012;55:2005–2023. doi: 10.1002/hep.25762. [DOI] [PubMed] [Google Scholar]
- 16.Suzuki A, Angulo P, Lymp J, et al. Chronological development of elevated aminotransferases in a nonalcoholic population. Hepatology. 2005;41:64–71. doi: 10.1002/hep.20543. [DOI] [PubMed] [Google Scholar]
- 17.Tsuneto A, Hida A, Sera N, et al. Fatty liver incidence and predictive variables. Hyper Res. 2010;33:638–643. doi: 10.1038/hr.2010.45. [DOI] [PubMed] [Google Scholar]
- 18.Whalley S, Puvanachandra P, Desai A, Kennedy H. Hepatology outpatient service provision in secondary care: a study of liver disease incidence and resource costs. Clin Med. 2007;7:119–124. doi: 10.7861/clinmedicine.7-2-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vernon G, Baranova A, Younossi ZM. Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment. Pharm. Ther. 2011;34:274–285. doi: 10.1111/j.1365-2036.2011.04724.x. [DOI] [PubMed] [Google Scholar]
- 20.Marcos A, Fisher RA, Ham JM, et al. Selection and outcome of living donors for adult to adult right lobe transplantation. Transplantation. 2000;69:2410–2415. doi: 10.1097/00007890-200006150-00034. [DOI] [PubMed] [Google Scholar]
- 21.Browning JD, Szczepaniak LS, Dobbins R, et al. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology. 2004;40:1387–1395. doi: 10.1002/hep.20466. [DOI] [PubMed] [Google Scholar]
- 22.Lee JY, Kim KM, Lee SG, et al. Prevalence and risk factors of non-alcoholic fatty liver disease in potential living liver donors in Korea: a review of 589 consecutive liver biopsies in a single center. J. Hepatol. 2007;47:239–244. doi: 10.1016/j.jhep.2007.02.007. [DOI] [PubMed] [Google Scholar]
- 23.Chen ZW, Chen LY, Dai HL, et al. Relationship between alanine aminotransferase levels and metabolic syndrome in nonalcoholic fatty liver disease. J. Zhejiang Univ. Science B. 2008;9:616–622. doi: 10.1631/jzus.B0720016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Amarapurkar D, Kamani P, Patel N, et al. Prevalence of non-alcoholic fatty liver disease: population based study. Ann. Hepatol. 2007;6:161–163. [PubMed] [Google Scholar]
- 25.Gutierrez-Grobe Y, Ponciano-Rodriguez G, Ramos MH, et al. Prevalence of non alcoholic fatty liver disease in premenopausal, posmenopausal and polycystic ovary syndrome women. The role of estrogens. Ann. Hepatol. 2010;9:402–409. [PubMed] [Google Scholar]
- 26.Piepkorn MW, Mottet NK, Smuckler EA. Fatty metamorphosis of the liver associated with jejunoileal bypass. Report of five cases. Arch. Pathol. Lab. Med. 1977;101:411–415. [PubMed] [Google Scholar]
- 27.Peters RL, Gay T, Reynolds TB. Post-jejunoileal-bypass hepatic disease. Its similarity to alcoholic hepatic disease. Am. J. Clin. Pathol. 1975;63:318–331. doi: 10.1093/ajcp/63.3.318. [DOI] [PubMed] [Google Scholar]
- 28.Kato H, Isaji S, Azumi Y, et al. Development of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH) after pancreaticoduodenectomy: proposal of a postoperative NAFLD scoring system. J. Hepato-biliary-pancreatic sciences. 2010;17:296–304. doi: 10.1007/s00534-009-0187-2. [DOI] [PubMed] [Google Scholar]
- 29.Boza C, Riquelme A, Ibanez L, et al. Predictors of nonalcoholic steatohepatitis (NASH) in obese patients undergoing gastric bypass. Obes. Surg. 2005;15:1148–1153. doi: 10.1381/0960892055002347. [DOI] [PubMed] [Google Scholar]
- 30.Haentjens P, Massaad D, Reynaert H, et al. Identifying non-alcoholic fatty liver disease among asymptomatic overweight and obese individuals by clinical and biochemical characteristics. Acta clinica Belgica. 2009;64:483–493. doi: 10.1179/acb.2009.084. [DOI] [PubMed] [Google Scholar]
- 31.Beymer C, Kowdley KV, Larson A, et al. Prevalence and predictors of asymptomatic liver disease in patients undergoing gastric bypass surgery. Arch. Surg. 2003;138:1240–1244. doi: 10.1001/archsurg.138.11.1240. [DOI] [PubMed] [Google Scholar]
- 32.Loria P, Carulli L, Bertolotti M, Lonardo A. Endocrine and liver interaction: the role of endocrine pathways in NASH. Nat. Revs. 2009;6:236–247. doi: 10.1038/nrgastro.2009.33. [DOI] [PubMed] [Google Scholar]
- 33.Barclay JL, Nelson CN, Ishikawa M, et al. GH-dependent STAT5 signaling plays an important role in hepatic lipid metabolism. Endocrinology. 2011;152:181–192. doi: 10.1210/en.2010-0537. [DOI] [PubMed] [Google Scholar]
- 34.Gabbi C, Carubbi F, Losi L, et al. Nonalcoholic fatty liver disease induced by leuprorelin acetate. J. Clin. Gastroenterol. 2008;42:107–110. doi: 10.1097/01.mcg.0000225583.32588.5e. [DOI] [PubMed] [Google Scholar]
- 35.Brzozowska MM, Ostapowicz G, Weltman MD. An association between non-alcoholic fatty liver disease and polycystic ovarian syndrome. J. Gastroenterol. Hepatol. 2009;24:243–247. doi: 10.1111/j.1440-1746.2008.05740.x. [DOI] [PubMed] [Google Scholar]
- 36.Kawamura Y, Arase Y, Ikeda K, et al. Large-scale long-term follow-up study of Japanese patients with non-alcoholic fatty liver disease for the onset of hepatocellular carcinoma. Am. J. Gastroenterol. 2012;107:253–261. doi: 10.1038/ajg.2011.327. [DOI] [PubMed] [Google Scholar]
- 37.Wong VW, Wong GL, Choi PC, et al. Disease progression of non-alcoholic fatty liver disease: a prospective study with paired liver biopsies at 3 years. Gut. 2010;59:969–974. doi: 10.1136/gut.2009.205088. [DOI] [PubMed] [Google Scholar]
- 38.Assy N, Kaita K, Mymin D, et al. Fatty infiltration of liver in hyperlipidemic patients. Digest. Dis. Sci. 2000;45:1929–1934. doi: 10.1023/a:1005661516165. [DOI] [PubMed] [Google Scholar]
- 39.Eguchi Y, Eguchi T, Mizuta T, et al. Visceral fat accumulation and insulin resistance are important factors in nonalcoholic fatty liver disease. J. Gastroenterol. 2006;41:462–469. doi: 10.1007/s00535-006-1790-5. [DOI] [PubMed] [Google Scholar]
- 40.Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–2752. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- 41.Marceau P, Biron S, Hould FS, et al. Liver pathology and the metabolic syndrome X in severe obesity. J. Clin. Endocrinol. Metabol. 1999;84:1513–1517. doi: 10.1210/jcem.84.5.5661. [DOI] [PubMed] [Google Scholar]
- 42.Hamaguchi M, Kojima T, Takeda N, et al. The metabolic syndrome as a predictor of nonalcoholic fatty liver disease. Ann. Int. Med. 2005;143:722–728. doi: 10.7326/0003-4819-143-10-200511150-00009. [DOI] [PubMed] [Google Scholar]
- 43.Hanley AJ, Williams K, Festa A, et al. Liver markers and development of the metabolic syndrome: the insulin resistance atherosclerosis study. Diabetes. 2005;54:3140–3147. doi: 10.2337/diabetes.54.11.3140. [DOI] [PubMed] [Google Scholar]
- 44.Lomonaco R, Ortiz-Lopez C, Orsak B, et al. Effect of adipose tissue insulin resistance on metabolic parameters and liver histology in obese patients with nonalcoholic fatty liver disease. Hepatology. 2012;55:1389–1397. doi: 10.1002/hep.25539. [DOI] [PubMed] [Google Scholar]
- 45.Musso G, Cassader M, De Michieli F, et al. Nonalcoholic steatohepatitis versus steatosis: Adipose tissue insulin resistance and dysfunctional response to fat ingestion predict liver injury and altered glucose and lipoprotein metabolism. Hepatology. 2012;56:933–942. doi: 10.1002/hep.25739. [DOI] [PubMed] [Google Scholar]
- 46.Targher G, Bertolini L, Padovani R, et al. Prevalence of non-alcoholic fatty liver disease and its association with cardiovascular disease in patients with type 1 diabetes. J. Hepatol. 2010;53:713–718. doi: 10.1016/j.jhep.2010.04.030. [DOI] [PubMed] [Google Scholar]
- 47.Regnell SE, Lernmark A. Hepatic steatosis in type 1 diabetes. RDS. 2011;8:454–467. doi: 10.1900/RDS.2011.8.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bae JC, Rhee EJ, Lee WY, et al. Combined effect of nonalcoholic fatty liver disease and impaired fasting glucose on the development of type 2 diabetes: a 4-year retrospective longitudinal study. Diabetes Care. 2011;34:727–729. doi: 10.2337/dc10-1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Argo CK, Northup PG, Al-Osaimi AM, Caldwell SH. Systematic review of risk factors for fibrosis progression in non-alcoholic steatohepatitis. J. Hepatol. 2009;51:371–379. doi: 10.1016/j.jhep.2009.03.019. [DOI] [PubMed] [Google Scholar]
- 50.Musso G, Gambino R, Cassader M, Pagano G. Meta-analysis: natural history of non-alcoholic fatty liver disease (NAFLD) and diagnostic accuracy of non-invasive tests for liver disease severity. Ann. Med. 2011;43:617–649. doi: 10.3109/07853890.2010.518623. [DOI] [PubMed] [Google Scholar]
- 51.Bhala N, Angulo P, van der Poorten D, et al. The natural history of nonalcoholic fatty liver disease with advanced fibrosis or cirrhosis: an international collaborative study. Hepatology. 2011;54:1208–1216. doi: 10.1002/hep.24491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Angulo P, Keach JC, Batts KP, Lindor KD. Independent predictors of liver fibrosis in patients with nonalcoholic steatohepatitis. Hepatology. 1999;30:1356–1362. doi: 10.1002/hep.510300604. [DOI] [PubMed] [Google Scholar]
- 53.Pantsari MW, Harrison SA. Nonalcoholic fatty liver disease presenting with an isolated elevated alkaline phosphatase. J. Clin Gastroenterol. 2006;40:633–635. doi: 10.1097/00004836-200608000-00015. [DOI] [PubMed] [Google Scholar]
- 54.Armstrong MJ, Houlihan DD, Bentham L, et al. Presence and severity of non-alcoholic fatty liver disease in a large prospective primary care cohort. J. Hepatol. 2012;56:234–240. doi: 10.1016/j.jhep.2011.03.020. [DOI] [PubMed] [Google Scholar]
- 55.Adams LA, Sanderson S, Lindor KD, Angulo P. The histological course of nonalcoholic fatty liver disease: a longitudinal study of 103 patients with sequential liver biopsies. J. Hepatol. 2005;42:132–138. doi: 10.1016/j.jhep.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 56.Vuppalanchi R, Chalasani N. Nonalcoholic fatty liver disease and nonalcoholic steatohepatitis: Selected practical issues in their evaluation and management. Hepatology. 2009;49:306–317. doi: 10.1002/hep.22603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Vuppalanchi R, Gould RJ, Wilson LA, et al. Clinical significance of serum autoantibodies in patients with NAFLD: results from the nonalcoholic steatohepatitis clinical research network. Hepatol. Int. 2011;6:379–385. doi: 10.1007/s12072-011-9277-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Angulo P, Hui JM, Marchesini G, et al. The NAFLD fibrosis score: a noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology. 2007;45:846–854. doi: 10.1002/hep.21496. [DOI] [PubMed] [Google Scholar]
- 59.Rosenberg WM, Voelker M, Thiel R, et al. Serum markers detect the presence of liver fibrosis: a cohort study. Gastroenterology. 2004;127:1704–1713. doi: 10.1053/j.gastro.2004.08.052. [DOI] [PubMed] [Google Scholar]
- 60.Guha IN, Parkes J, Roderick P, et al. Noninvasive markers of fibrosis in nonalcoholic fatty liver disease: Validating the European Liver Fibrosis Panel and exploring simple markers. Hepatology. 2008;47:455–460. doi: 10.1002/hep.21984. [DOI] [PubMed] [Google Scholar]
- 61.Wieckowska A, Zein NN, Yerian LM, et al. In vivo assessment of liver cell apoptosis as a novel biomarker of disease severity in nonalcoholic fatty liver disease. Hepatology. 2006;44:27–33. doi: 10.1002/hep.21223. [DOI] [PubMed] [Google Scholar]
- 62.Joseph AE, Dewbury KC, McGuire PG. Ultrasound in the detection of chronic liver disease (the “bright liver”) British J. Radiol. 1979;52:184–188. doi: 10.1259/0007-1285-52-615-184. [DOI] [PubMed] [Google Scholar]
- 63.Joseph AE, Saverymuttu SH, al-Sam S, et al. Comparison of liver histology with ultrasonography in assessing diffuse parenchymal liver disease. Clin. Radiol. 1991;43:26–31. doi: 10.1016/s0009-9260(05)80350-2. [DOI] [PubMed] [Google Scholar]
- 64.Palmentieri B, de Sio I, La Mura V, et al. The role of bright liver echo pattern on ultrasound B-mode examination in the diagnosis of liver steatosis. Digest. Liver Dis. 2006;38:485–489. doi: 10.1016/j.dld.2006.03.021. [DOI] [PubMed] [Google Scholar]
- 65.Jacobs JE, Birnbaum BA, Shapiro MA, et al. Diagnostic criteria for fatty infiltration of the liver on contrast-enhanced helical CT. AJR. 1998;171:659–664. doi: 10.2214/ajr.171.3.9725292. [DOI] [PubMed] [Google Scholar]
- 66.Outwater EK, Blasbalg R, Siegelman ES, Vala M. Detection of lipid in abdominal tissues with opposed-phase gradient-echo images at 1.5 T: techniques and diagnostic importance. Radiographics. 1998;18:1465–1480. doi: 10.1148/radiographics.18.6.9821195. [DOI] [PubMed] [Google Scholar]
- 67.Kim SH, Lee JM, Han JK, et al. Hepatic macrosteatosis: predicting appropriateness of liver donation by using MR imaging–correlation with histopathologic findings. Radiology. 2006;240:116–129. doi: 10.1148/radiol.2393042218. [DOI] [PubMed] [Google Scholar]
- 68.Szczepaniak LS, Nurenberg P, Leonard D, et al. Magnetic resonance spectroscopy to measure hepatic triglyceride content: prevalence of hepatic steatosis in the general population. Am. J. Physiol. Endocrinol. Metab. 2005;288:E462–E468. doi: 10.1152/ajpendo.00064.2004. [DOI] [PubMed] [Google Scholar]
- 69.Qayyum A, Nystrom M, Noworolski SM, et al. MRI steatosis grading: development and initial validation of a color mapping system. AJR. 2012;198:582–588. doi: 10.2214/AJR.11.6729. [DOI] [PubMed] [Google Scholar]
- 70.Choi JS, Kim MJ. Education and imaging: hepatobiliary and pancreatic: focal steatohepatitis mimicking a metastasis. J. Gastroenterol. Hepatol. 2011;26:415. doi: 10.1111/j.1440-1746.2010.06614.x. [DOI] [PubMed] [Google Scholar]
- 71.Tharayil V, Roberts LR. Evaluation of a focal lesion in the liver. answer to the clinical challenges and images in GI question: image 3: Focal fatty infiltration. Gastroenterology. 2010;139:e10–e11. doi: 10.1053/j.gastro.2009.09.072. [DOI] [PubMed] [Google Scholar]
- 72.Fasih N, Shanbhogue AK, Thipphavong S, et al. Gamut of focal fatty lesions in the liver: imaging manifestations with emphasis on magnetic resonance imaging. Curr. Prob. Diag. Radiol. 2010;39:137–151. doi: 10.1067/j.cpradiol.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 73.Karcaaltincaba M, Akhan O. Imaging of hepatic steatosis and fatty sparing. Eur. J. Radiol. 2007;61:33–43. doi: 10.1016/j.ejrad.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 74.Hamer OW, Aguirre DA, Casola G, et al. Fatty liver: imaging patterns and pitfalls. Radiographics. 2006;26:1637–1653. doi: 10.1148/rg.266065004. [DOI] [PubMed] [Google Scholar]
- 75.Wong VW, Vergniol J, Wong GL, et al. Diagnosis of fibrosis and cirrhosis using liver stiffness measurement in nonalcoholic fatty liver disease. Hepatology. 2010;51:454–462. doi: 10.1002/hep.23312. [DOI] [PubMed] [Google Scholar]
- 76.Kleiner DE, Brunt EM, Van Natta M, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313–1321. doi: 10.1002/hep.20701. [DOI] [PubMed] [Google Scholar]
- 77.Brunt EM. Nonalcoholic steatohepatitis. Semin. liver Dis. 2004;24:3–20. doi: 10.1055/s-2004-823098. [DOI] [PubMed] [Google Scholar]
- 78.Ludwig J, Viggiano TR, McGill DB, Oh BJ. Nonalcoholic steatohepatitis: Mayo Clinic experiences with a hitherto unnamed disease. Mayo Clin. Proc. 1980;55:434–438. [PubMed] [Google Scholar]
- 79.Brunt EM, Janney CG, Di Bisceglie AM, et al. Nonalcoholic steatohepatitis: a proposal for grading and staging the histological lesions. Am. J. Gastroenterol. 1999;94:2467–2474. doi: 10.1111/j.1572-0241.1999.01377.x. [DOI] [PubMed] [Google Scholar]
- 80.Brunt EM, Kleiner DE, Wilson LA, et al. Nonalcoholic fatty liver disease (NAFLD) activity score and the histopathologic diagnosis in NAFLD: distinct clinicopathologic meanings. Hepatology. 2011;53:810–820. doi: 10.1002/hep.24127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ratziu V, Charlotte F, Heurtier A, et al. Sampling variability of liver biopsy in nonalcoholic fatty liver disease. Gastroenterology. 2005;128:1898–1906. doi: 10.1053/j.gastro.2005.03.084. [DOI] [PubMed] [Google Scholar]
- 82.Merriman RB, Ferrell LD, Patti MG, et al. Correlation of paired liver biopsies in morbidly obese patients with suspected nonalcoholic fatty liver disease. Hepatology. 2006;44:874–880. doi: 10.1002/hep.21346. [DOI] [PubMed] [Google Scholar]
- 83.Alkhouri N, Carter-Kent C, Feldstein AE. Apoptosis in nonalcoholic fatty liver disease: diagnostic and therapeutic implications. Expert Rev. Gastroenterol. Hepatol. 2011;5:201–212. doi: 10.1586/egh.11.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Feldstein AE. Novel insights into the pathophysiology of nonalcoholic fatty liver disease. Semin. liver Dis. 2010;30:391–401. doi: 10.1055/s-0030-1267539. [DOI] [PubMed] [Google Scholar]
- 85.Day CP, James OF. Steatohepatitis: a tale of two “hits”? Gastroenterology. 1998;114:842–845. doi: 10.1016/s0016-5085(98)70599-2. [DOI] [PubMed] [Google Scholar]
- 86.Gorden DL, Ivanova PT, Myers DS, et al. Increased diacylglycerols characterize hepatic lipid changes in progression of human nonalcoholic fatty liver disease; comparison to a murine model. PloS one. 2011;6:e2:2775. doi: 10.1371/journal.pone.0022775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kotronen A, Seppanen-Laakso T, Westerbacka J, et al. Hepatic stearoyl-CoA desaturase (SCD)-1 activity and diacylglycerol but not ceramide concentrations are increased in the nonalcoholic human fatty liver. Diabetes. 2009;58:203–208. doi: 10.2337/db08-1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Rolo AP, Teodoro JS, Palmeira CM. Role of oxidative stress in the pathogenesis of nonalcoholic steatohepatitis. Free Rad. Biol. Med. 2012;52:59–69. doi: 10.1016/j.freeradbiomed.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 89.Soardo G, Donnini D, Domenis L, et al. Oxidative stress is activated by free fatty acids in cultured human hepatocytes. Metab. Synd. related Disord. 2011;9:397–401. doi: 10.1089/met.2010.0140. [DOI] [PubMed] [Google Scholar]
- 90.Malhi H, Gores GJ. Molecular mechanisms of lipotoxicity in nonalcoholic fatty liver disease. Semin. liver Dis. 2008;28:360–369. doi: 10.1055/s-0028-1091980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Amir M, Czaja MJ. Autophagy in nonalcoholic steatohepatitis. Exp. Rev. Gastroenterol. Hepatol. 2011;5:159–166. doi: 10.1586/egh.11.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Grattagliano I, de Bari O, Bernardo TC, et al. Role of mitochondria in nonalcoholic fatty liver disease–from origin to propagation. Clin. Biochem. 2012;45:610–618. doi: 10.1016/j.clinbiochem.2012.03.024. [DOI] [PubMed] [Google Scholar]
- 93.Kremer M, Hines IN. Natural killer T cells and non-alcoholic fatty liver disease: fat chews on the immune system. WJG. 2008;14:487–488. doi: 10.3748/wjg.14.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Zhan YT, An W. Roles of liver innate immune cells in nonalcoholic fatty liver disease. WJG. 2010;16:4652–4660. doi: 10.3748/wjg.v16.i37.4652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Braunersreuther V, Viviani GL, Mach F, Montecucco F. Role of cytokines and chemokines in non-alcoholic fatty liver disease. WJG. 2012;18:727–735. doi: 10.3748/wjg.v18.i8.727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ono M, Saibara T. Is impaired Kupffer cell function really important to the pathogenesis of nonalcoholic steatohepatitis? J. Gastroenterol. Hepatol. 2012;27:622–624. doi: 10.1111/j.1440-1746.2012.07084.x. [DOI] [PubMed] [Google Scholar]
- 97.Palmer M, Schaffner F. Effect of weight reduction on hepatic abnormalities in overweight patients. Gastroenterology. 1990;99:1408–1413. doi: 10.1016/0016-5085(90)91169-7. [DOI] [PubMed] [Google Scholar]
- 98.Park HS, Kim MW, Shin ES. Effect of weight control on hepatic abnormalities in obese patients with fatty liver. J. Kor. Med. Sci. 1995;10:414–421. doi: 10.3346/jkms.1995.10.6.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ueno T, Sugawara H, Sujaku K, et al. Therapeutic effects of restricted diet and exercise in obese patients with fatty liver. J. Hepatol. 1997;27:103–107. doi: 10.1016/s0168-8278(97)80287-5. [DOI] [PubMed] [Google Scholar]
- 100.Harrison SA, Fecht W, Brunt EM, Neuschwander-Tetri BA. Orlistat for overweight subjects with nonalcoholic steatohepatitis: a randomized, prospective trial. Hepatology. 2009;49:80–86. doi: 10.1002/hep.22575. [DOI] [PubMed] [Google Scholar]
- 101.Promrat K, Kleiner DE, Niemeier HM, et al. Randomized controlled trial testing the effects of weight loss on nonalcoholic steatohepatitis. Hepatology. 2010;51:121–129. doi: 10.1002/hep.23276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Andersen T, Gluud C, Franzmann MB, Christoffersen P. Hepatic effects of dietary weight loss in morbidly obese subjects. J. Hepatol. 1991;12:224–229. doi: 10.1016/0168-8278(91)90942-5. [DOI] [PubMed] [Google Scholar]
- 103.Mathurin P, Hollebecque A, Arnalsteen L, et al. Prospective study of the long-term effects of bariatric surgery on liver injury in patients without advanced disease. Gastroenterology. 2009;137:532–540. doi: 10.1053/j.gastro.2009.04.052. [DOI] [PubMed] [Google Scholar]
- 104.Mummadi RR, Kasturi KS, Chennareddygari S, Sood GK. Effect of bariatric surgery on nonalcoholic fatty liver disease: systematic review and meta-analysis. Clin. Gastroenterol. Hepatol. 2008;6:1396–1402. doi: 10.1016/j.cgh.2008.08.012. [DOI] [PubMed] [Google Scholar]
- 105.Chavez-Tapia NC, Tellez-Avila FI, Barrientos-Gutierrez T, et al. Bariatric surgery for non-alcoholic steatohepatitis in obese patients. Cochrane Database Syst Rev. 2010:CD007340. doi: 10.1002/14651858.CD007340.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Rezazadeh A, Yazdanparast R, Molaei M. Amelioration of diet-induced nonalcoholic steatohepatitis in rats by Mn-salen complexes via reduction of oxidative stress. J. Biomed. Sci. 2012;19:26. doi: 10.1186/1423-0127-19-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Narasimhan S, Gokulakrishnan K, Sampathkumar R, et al. Oxidative stress is independently associated with non-alcoholic fatty liver disease (NAFLD) in subjects with and without type 2 diabetes. Clin. Biochem. 2010;43:815–821. doi: 10.1016/j.clinbiochem.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 108.Sanyal AJ, Chalasani N, Kowdley KV, et al. Pioglitazone, vitamin E, or placebo for nonalcoholic steatohepatitis. N. Engl. J. Med. 2010;362:1675–1685. doi: 10.1056/NEJMoa0907929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Klein EA, Thompson IM, Jr, Tangen CM, et al. Vitamin E and the risk of prostate cancer: the Selenium and Vitamin E Cancer Prevention Trial (SELECT) JAMA. 2011;306:1549–1556. doi: 10.1001/jama.2011.1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Miller ER, 3rd, Pastor-Barriuso R, Dalal D, et al. Meta-analysis: high-dosage vitamin E supplementation may increase all-cause mortality. Ann. Int. Med. 2005;142:37–46. doi: 10.7326/0003-4819-142-1-200501040-00110. [DOI] [PubMed] [Google Scholar]
- 111.Bjelakovic G, Nikolova D, Gluud LL, et al. Mortality in randomized trials of antioxidant supplements for primary and secondary prevention: systematic review and meta-analysis. JAMA. 2007;297:842–857. doi: 10.1001/jama.297.8.842. [DOI] [PubMed] [Google Scholar]
- 112.Berry D, Wathen JK, Newell M. Bayesian model averaging in meta-analysis: vitamin E supplementation and mortality. Clin. Trials. 2009;6:28–41. doi: 10.1177/1740774508101279. [DOI] [PubMed] [Google Scholar]
- 113.Gerss J, Kopcke W. The questionable association of vitamin E supplementation and mortality–inconsistent results of different meta-analytic approaches. Cell. Mol. Biol. (Noisy-le-grand) 2009;55(Suppl):OL1111–1120. [PubMed] [Google Scholar]
- 114.Dietrich M, Jacques PF, Pencina MJ, et al. Vitamin E supplement use and the incidence of cardiovascular disease and all-cause mortality in the Framingham Heart Study: does the underlying health status play a role? Atherosclerosis. 2009;205:549–553. doi: 10.1016/j.atherosclerosis.2008.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Abner EL, Schmitt FA, Mendiondo MS, et al. Vitamin E and all-cause mortality: a meta-analysis. Curr. Ag. Sci. 2011;4:158–170. doi: 10.2174/1874609811104020158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Bugianesi E, Gentilcore E, Manini R, et al. A randomized controlled trial of metformin versus vitamin E or prescriptive diet in nonalcoholic fatty liver disease. Am. J. Gastroenterol. 2005;100:1082–1090. doi: 10.1111/j.1572-0241.2005.41583.x. [DOI] [PubMed] [Google Scholar]
- 117.Shields WW, Thompson KE, Grice GA, et al. The effect of metformin and standard therapy versus standard therapy alone in nondiabetic patients with insulin resistance and nonalcoholic steatohepatitis (NASH): a pilot trial. Ther. Adv. Gastroenterol. 2009;2:157–163. doi: 10.1177/1756283X09105462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Omer Z, Cetinkalp S, Akyildiz M, et al. Efficacy of insulin-sensitizing agents in nonalcoholic fatty liver disease. Eur. J. Gastroenterol. Hepatol. 2010;22:18–23. doi: 10.1097/MEG.0b013e32832e2baf. [DOI] [PubMed] [Google Scholar]
- 119.Neuschwander-Tetri BA, Brunt EM, Wehmeier KR, et al. Improved nonalcoholic steatohepatitis after 48 weeks of treatment with the PPAR-gamma ligand rosiglitazone. Hepatology. 2003;38:1008–1017. doi: 10.1053/jhep.2003.50420. [DOI] [PubMed] [Google Scholar]
- 120.Belfort R, Harrison SA, Brown K, et al. A placebo-controlled trial of pioglitazone in subjects with nonalcoholic steatohepatitis. N. Engl. J. Med. 2006;355:2297–2307. doi: 10.1056/NEJMoa060326. [DOI] [PubMed] [Google Scholar]
- 121.Ratziu V, Giral P, Jacqueminet S, et al. Rosiglitazone for nonalcoholic steatohepatitis: one-year results of the randomized placebo-controlled Fatty Liver Improvement with Rosiglitazone Therapy (FLIRT) Trial. Gastroenterology. 2008;135:100–110. doi: 10.1053/j.gastro.2008.03.078. [DOI] [PubMed] [Google Scholar]
- 122.Ratziu V, Charlotte F, Bernhardt C, et al. Long-term efficacy of rosiglitazone in nonalcoholic steatohepatitis: results of the fatty liver improvement by rosiglitazone therapy (FLIRT 2) extension trial. Hepatology. 2010;51:445–453. doi: 10.1002/hep.23270. [DOI] [PubMed] [Google Scholar]
- 123.Aithal GP, Thomas JA, Kaye PV, et al. Randomized, placebo-controlled trial of pioglitazone in nondiabetic subjects with nonalcoholic steatohepatitis. Gastroenterology. 2008;135:1176–1184. doi: 10.1053/j.gastro.2008.06.047. [DOI] [PubMed] [Google Scholar]
- 124.Sanyal AJ, Chalasani N, Kowdley KV, et al. Pioglitazone, vitamin E, or placebo for nonalcoholic steatohepatitis. N. Engl. J. Med. 2010;362:1675–1685. doi: 10.1056/NEJMoa0907929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Boettcher E, Csako G, Pucino F, et al. Meta-analysis: pioglitazone improves liver histology and fibrosis in patients with non-alcoholic steatohepatitis. Aliment. Pharmacol. Ther. 2012;35:66–75. doi: 10.1111/j.1365-2036.2011.04912.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Torres DM, Jones FJ, Shaw JC, et al. Rosiglitazone versus rosiglitazone and metformin versus rosiglitazone and losartan in the treatment of nonalcoholic steatohepatitis in humans: a 12-month randomized, prospective, open- label trial. Hepatology. 2011;54:1631–1639. doi: 10.1002/hep.24558. [DOI] [PubMed] [Google Scholar]
- 127.Nissen SE, Wolski K. Effect of rosiglitazone on the risk of myocardial infarction and death from cardiovascular causes. N. Engl. J. Med. 2007;356:2457–2471. doi: 10.1056/NEJMoa072761. [DOI] [PubMed] [Google Scholar]
- 128.Lincoff AM, Wolski K, Nicholls SJ, Nissen SE. Pioglitazone and risk of cardiovascular events in patients with type 2 diabetes mellitus: a meta-analysis of randomized trials. JAMA. 2007;298:1180–1188. doi: 10.1001/jama.298.10.1180. [DOI] [PubMed] [Google Scholar]
- 129.Foster T, Budoff MJ, Saab S, et al. Atorvastatin and antioxidants for the treatment of nonalcoholic fatty liver disease: the St Francis Heart Study randomized clinical trial. Am. J. Gastroenterol. 2011;106:71–77. doi: 10.1038/ajg.2010.299. [DOI] [PubMed] [Google Scholar]
- 130.Athyros VG, Tziomalos K, Gossios TD, et al. Safety and efficacy of long-term statin treatment for cardiovascular events in patients with coronary heart disease and abnormal liver tests in the Greek Atorvastatin and Coronary Heart Disease Evaluation (GREACE) Study: a post-hoc analysis. Lancet. 2010;376:1916–1922. doi: 10.1016/S0140-6736(10)61272-X. [DOI] [PubMed] [Google Scholar]
- 131.Chalasani N, Aljadhey H, Kesterson J, et al. Patients with elevated liver enzymes are not at higher risk for statin hepatotoxicity. Gastroenterology. 2004;126:1287–1292. doi: 10.1053/j.gastro.2004.02.015. [DOI] [PubMed] [Google Scholar]
- 132.Vuppalanchi R, Teal E, Chalasani N. Patients with elevated baseline liver enzymes do not have higher frequency of hepatotoxicity from lovastatin than those with normal baseline liver enzymes. Am. J. Med. Sci. 2005;329:62–65. doi: 10.1097/00000441-200502000-00002. [DOI] [PubMed] [Google Scholar]
- 133.Chalasani N. Statins and hepatotoxicity: focus on patients with fatty liver. Hepatology. 2005;41:690–695. doi: 10.1002/hep.20671. [DOI] [PubMed] [Google Scholar]
- 134.Browning JD. Statins and hepatic steatosis: perspectives from the Dallas Heart Study. Hepatology. 2006;44:466–471. doi: 10.1002/hep.21248. [DOI] [PubMed] [Google Scholar]
- 135.Zelber-Sagi S, Nitzan-Kaluski D, Goldsmith R, et al. Long term nutritional intake and the risk for non-alcoholic fatty liver disease (NAFLD): a population based study. J. Hepatol. 2007;47:711–717. doi: 10.1016/j.jhep.2007.06.020. [DOI] [PubMed] [Google Scholar]
- 136.Oya J, Nakagami T, Sasaki S, et al. Intake of n-3 polyunsaturated fatty acids and non-alcoholic fatty liver disease: a cross-sectional study in Japanese men and women. Eur. J. Clin. Nutr. 2010;64:1179–1185. doi: 10.1038/ejcn.2010.139. [DOI] [PubMed] [Google Scholar]
- 137.Capanni M, Calella F, Biagini MR, et al. Prolonged n-3 polyunsaturated fatty acid supplementation ameliorates hepatic steatosis in patients with non-alcoholic fatty liver disease: a pilot study. Aliment. Pharmacol. Ther. 2006;23:1143–1151. doi: 10.1111/j.1365-2036.2006.02885.x. [DOI] [PubMed] [Google Scholar]
- 138.Spadaro L, Magliocco O, Spampinato D, et al. Effects of n-3 polyunsaturated fatty acids in subjects with nonalcoholic fatty liver disease. Digest. liver Dis. 2008;40:194–199. doi: 10.1016/j.dld.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 139.Tanaka N, Sano K, Horiuchi A, et al. Highly purified eicosapentaenoic acid treatment improves nonalcoholic steatohepatitis. J. Clin. Gastroenterol. 2008;42:413–418. doi: 10.1097/MCG.0b013e31815591aa. [DOI] [PubMed] [Google Scholar]
- 140.Sofi F, Giangrandi I, Cesari F, et al. Effects of a 1-year dietary intervention with n-3 polyunsaturated fatty acid-enriched olive oil on non-alcoholic fatty liver disease patients: a preliminary study. Inter. J. Food Sci. Nutr. 2010;61:792–802. doi: 10.3109/09637486.2010.487480. [DOI] [PubMed] [Google Scholar]
- 141.Lindor KD, Kowdley KV, Heathcote EJ, et al. Ursodeoxycholic acid for treatment of nonalcoholic steatohepatitis: results of a randomized trial. Hepatology. 2004;39:770–778. doi: 10.1002/hep.20092. [DOI] [PubMed] [Google Scholar]
- 142.Ratziu V, de Ledinghen V, Oberti F, et al. A randomized controlled trial of high-dose ursodesoxycholic acid for nonalcoholic steatohepatitis. J. Hepatol. 2011;54:1011–1019. doi: 10.1016/j.jhep.2010.08.030. [DOI] [PubMed] [Google Scholar]
- 143.Leuschner UF, Lindenthal B, Herrmann G, et al. High-dose ursodeoxycholic acid therapy for nonalcoholic steatohepatitis: a double-blind, randomized, placebo-controlled trial. Hepatology. 2010;52:472–479. doi: 10.1002/hep.23727. [DOI] [PubMed] [Google Scholar]
- 144.Ascha MS, Hanouneh IA, Lopez R, et al. The incidence and risk factors of hepatocellular carcinoma in patients with nonalcoholic steatohepatitis. Hepatology. 2010;51:1972–1978. doi: 10.1002/hep.23527. [DOI] [PubMed] [Google Scholar]
- 145.Söderberg C, Stål P, Askling J, et al. Decreased survival of subjects with elevated liver function tests during a 28-year follow-up. Hepatology. 2010;51:595–602. doi: 10.1002/hep.23314. [DOI] [PubMed] [Google Scholar]
- 146.Dam-Larsen S, Franzmann M, Andersen IB, et al. Long term prognosis of fatty liver: risk of chronic liver disease and death. Gut. 2004;53:750–755. doi: 10.1136/gut.2003.019984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Rafiq N, Bai CH, Fang Y, et al. Long-term follow-up of patients with non-alcoholic fatty liver. Clin. Gastro. Hepatol. 2009;7:234–238. doi: 10.1016/j.cgh.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 148.Chatrath H, Vuppalanchi R, Chalasani N. Dyslipidemia in patients with nonalcoholic fatty liver disease. Semin. Liver Dis. 2012;32:22–29. doi: 10.1055/s-0032-1306423. [DOI] [PMC free article] [PubMed] [Google Scholar]