The Women’s Recovery Group Study: A Stage I trial of women-focused group therapy for substance use disorders versus mixed-gender group drug counseling (original) (raw)
. Author manuscript; available in PMC: 2013 Jun 11.
Abstract
The aim of this Stage I Behavioral Development Trial was to develop a manual-based 12-session Women’s Recovery Group (WRG) and to pilot test this new treatment in a randomized controlled trial against a mixed-gender Group Drug Counseling (GDC), an effective manual-based treatment for substance use disorders. After initial manual development, two pre-pilot groups of WRG were conducted to determine feasibility and initial acceptability of the treatment among subjects and therapists. In the pilot stage, women were randomized to either WRG or GDC. No significant differences in substance use outcomes were found between WRG and GDC during the 12-week group treatment. However, during the 6-month post-treatment follow-up, WRG members demonstrated a pattern of continued reductions in substance use while GDC women did not. In addition, pilot WRG women with alcohol dependence had significantly greater reductions in average drinks/drinking day than GDC women 6 months post-treatment (p < .03, effect size = 0.81). While satisfaction with both groups was high, women were significantly more satisfied with WRG than GDC (p < .009, effect size = 1.11). In this study, the newly developed 12-session women-focused WRG was feasible with high satisfaction among participants. It was equally effective as mixed-gender GDC in reducing substance use during the 12-week in-treatment phase, but demonstrated significantly greater improvement in reductions in drug and alcohol use over the post-treatment follow-up phase compared with GDC. A women-focused single-gender group treatment may enhance longer-term clinical outcomes among women with substance use disorders.
Keywords: Gender differences, Women, Substance use disorders, Alcohol use disorders, Treatment outcomes, Group therapy
1. Introduction
While substance abuse is a growing health problem among women, females are underrepresented in most substance abuse treatment programs. Research has specified barriers to women’s entry into substance abuse treatment as well as some women’s preference for single-gender substance abuse treatment programs. There is also evidence that suggests benefits for women-only treatment. Women with substance use disorders (SUDs) have reported their perception that all-female groups provide a safer and more comfortable treatment environment (Kauffman et al., 1995). In addition, women with SUDs differ from their male counterparts in their risk factors, presenting problems, co-occurring disorders, medical consequences, and reasons for relapse. These differences may not be adequately addressed in mixed-gender settings (Greenfield et al., 2007).
Although some manual-based group treatments do exist for specific subpopulations of women with SUDs (Berkowitz et al., 1998; Hien et al., 2004; Killeen and Brady, 2000; Linehan et al., 1999; Luthar and Suchman, 2000; Mackie-Ramos and Rice, 1988; Najavits et al., 1996, 1998; Reynolds et al., 1995; Stevens and Arbiter, 1995), there is no empirically tested treatment for a heterogenous group of women with substance use disorders. Studies investigating women-only group treatments exist for parenting and pregnant women with substance use disorders (Berkowitz et al., 1998; Luthar and Suchman, 2000; Killeen and Brady, 2000; Mackie-Ramos and Rice, 1988; Stevens and Arbiter, 1995), for women with co-occurring post-traumatic stress and substance use disorders (Hien et al., 2004; Najavits et al., 1996, 1998), pregnant women to reduce alcohol consumption (Reynolds et al., 1995), and women with borderline personality disorder and drug dependence (Linehan et al., 1999). However, there is no study of a manual-based recovery group for women that is not specific for type of substance abused (e.g., opioids, alcohol, cocaine, etc.), co-occurring psychiatric disorders (e.g., post-traumatic stress disorder, borderline disorder), or stage of the life cycle (e.g., pregnancy, parenting). In addition, such a generic recovery group for women has not been tested in a randomized controlled trial against a standard, effective mixed-gender group therapy for substance abuse. This lack of research exists despite the fact that the majority of substance abuse treatment is delivered in group therapy format (Kominars and Dornheim, 2004). Furthermore, women’s recovery groups often include women with various substances of abuse who have many different co-occurring disorders and are at various ages and life stages (Beckman, 1994).
The Women’s Recovery Group (WRG) study hypothesized that both a single-gender group composition and women-focused group content would result in better substance abuse treatment outcomes than standard mixed-gender group treatment.1 The purpose of this Stage I behavioral development trial was two-fold: first, to develop the new manual-based Women’s Recovery Group treatment, and second, to conduct a pilot randomized controlled trial of this intervention compared with a standard mixed-gender Group Drug Counseling (GDC).
2. Methods
2.1. The Women’s Recovery Group
The Women’s Recovery Group (WRG) is a new 12-session manual-based relapse prevention group therapy that utilizes a cognitive-behavioral approach developed for this study by the principal investigator (SFG). The WRG utilizes a 90-min structured relapse prevention group therapy session that consists of the following: a brief check-in, review of past week’s skill practice, presentation of session topic, open discussion of topic and other recovery-related matters by participants, review of session’s “take-home message” and upcoming week’s skill practice, followed by a check-out. Content areas for individual sessions were based on gender-specific substance abuse antecedents, consequences, and treatment outcomes (Greenfield, 1996; Greenfield et al., 2007; Hernandez-Avila et al., 2004; Lex, 1991; Piazza et al., 1989). These included: the effect of drugs and alcohol on women’s health; women’s relationships and recovery; violence and substance abuse; mood, anxiety, and eating problems and substance use disorders; recovery skills; stigma, shame, and disclosure; being a caretaker and being in recovery; self-help groups; and achieving a balance. These content areas translated into 14 specific session topics2 that could be flexibly chosen in any order for a 12-week sequence of groups. The WRG emphasized that while differences might exist between individuals in the group, all participants were united in seeking treatment for their substance dependence. Characteristic signs and symptoms of substance dependence based on DSM-IV criteria were posted on the bulletin board for each session and could be referred to by the therapist when necessary to remind the participants about the central purpose of their work in the group and to emphasize commonality rather than differences among participants. In addition, the WRG central theme was posted at each session: “Recovery = Relapse Prevention + Repair Work.” Topic sessions were directed at relapse prevention (e.g., how to help yourself stay abstinent from drugs and alcohol) or repair work (e.g., learning to live in a balanced way without drugs and alcohol, repairing damages to your life, managing shame and stigma).
Each session began with a check-in. Each group member answered three questions posed to them on a laminated sheet of paper within 2–3 min (i.e., Did you have any cravings or urges to use?; Did you use, or if not, how were you able to remain sober?; Did you do the skill practice, and if so, what did you find helpful?) and then passed the sheet to the next member. After the check-in, the therapist presented the session topic in an interactive manner in 20–30 min. Each group session topic presented by the therapist was accompanied by material posted on a bulletin board and summarized in a handout received by each participant. After the session topic, group members engaged in open discussion of the topic and its relationship to other recovery topics for 30–40 min. At the end of the discussion, the therapist related discussion material to the session topic and pointed out the take-home message for that session. The session concluded with a review of the skill practice for the coming week and a brief check-out during which each group member stated one thing she planned to do to support her recovery in the coming week.
2.2. Treatment development
Following development of the 12-session Women’s Recovery Group manual, pre-pilot group 1 (N = 5) was recruited in a semi-closed format. Enrollment was open until session 3 and then the group was closed. The PI served as the first pre-pilot group therapist. Each member of the group completed group content rating forms following each group as well as group satisfaction and group cohesion questionnaires every three weeks. Based on therapist and patient ratings of the sessions and the review of the manual by a consultant, the manual was revised at the end of pre-pilot group 1. A new therapist was trained by the PI to deliver WRG, and subjects for pre-pilot group 2 were recruited (N = 8). At the end of pre-pilot group 2, the manual was revised again based on therapist and patient ratings of group content and satisfaction. Revisions to the manual at each of these stages were minimal and included rewording of handouts and bulletin board materials, including the addition of session take-home messages, as well as rewording of the check-in questions.
Following the final manual revision, a pilot randomized controlled trial was conducted in two rounds. Women were randomly assigned to the study condition (WRG) (N = 16) or the control condition, mixed-gender Group Drug Counseling (N = 7 females, 10 males).
2.3. Procedures
Patients with current substance dependence were recruited from McLean Hospital programs, advertisements, flyers, and clinician referrals. Advertisements were for investigational group therapy for substance abuse but did not specify the Women’s Recovery Group in order to minimize selection bias for women only interested in women’s treatment. The protocol was approved by the McLean Hospital Institutional Review Board. Written informed consent was obtained after study procedures were fully explained. Inclusion criteria were (1) current dependence diagnosis of at least one substance dependence other than nicotine dependence based on the Structured Clinical Interview for DSM-IV (SCID) (First et al., 1996), (2) substance use within 60 days of baseline assessment, (3) 18 years of age or older, (4) intention to remain within the geographic area to return for follow-up assessments, and (5) signed permission for the research team to communicate with any other mental health professional from whom they were receiving care. Exclusion criteria were (1) certain current co-occurring diagnoses (i.e., bipolar, post-traumatic stress, or psychotic disorders), (2) mandated to treatment, (3) residential treatment restricting substance use during the group treatment phase, (4) concurrent substance abuse treatment group (not including self-help) during the 12-week group treatment phase, and (5) clinical indication for medical detoxification (these patients were eligible to enter the study after detoxification). Individuals with co-occurring bipolar, psychotic, or post-traumatic stress disorders were excluded because other studies have demonstrated specific effective treatments for patients with these co-occurring psychiatric and substance use disorders (Hien et al., 2004; Mueser et al., 2003; Najavits et al., 1998; Weiss et al., 2007). In addition, while it is acknowledged that women with co-occurring post-traumatic stress and substance use disorders may have better outcomes in all-women group treatment (Hien et al., 2004; Najavits et al., 1998), the efficacy of single-gender women-focused substance abuse group treatment versus mixed-gender group treatment for women with and without other co-occurring psychiatric disorders other than PTSD has not been tested (Greenfield et al., 2007) and is the focus of this study.
In the pre-pilot phase of the study, of 18 subjects completing the baseline assessment, 13 were eligible for enrollment (72.0%) and 100% enrolled. Five subjects were excluded because they did not meet diagnostic inclusion criteria. Of the 13 enrolled subjects, 100% completed treatment and 6-month post-treatment follow-up. In the pilot randomized controlled trial 42 female subjects completed the baseline assessment and 31 (73.8%) were eligible to enroll. Of the 11 subjects excluded, five did not meet diagnostic criteria, two were court mandated to treatment, three required more intensive treatment (e.g., residential or partial hospitalization), and one had a prior treatment relationship with research staff that precluded study entry. Of the 31 who were eligible for randomization, 23 (74.2%) were randomized either to WRG (N = 16) or GDC (N = 7). Of the eight who were not randomized, one lost interest in treatment, two did not return telephone calls, three had time conflicts with the scheduled groups, one chose not to enter any treatment, and one required more intensive treatment. Of the 23 randomized, 18 (78.3% total subjects; 81.3% WRG and 71.4% GDC) completed all treatment sessions and 20 (87.0% total subjects; 87.5% WRG and 85.7% GDC) completed the 6-month post-treatment follow-up.
2.4. Control condition
Group Drug Counseling (GDC) (Daley et al., 2002) is a group treatment delivered in the NIDA Collaborative Cocaine Treatment Study (Crits-Christoph et al., 1999). GDC is designed to approximate the treatment delivered in community substance abuse treatment programs and was delivered as 12 weekly 90-min sessions, each focusing on a specific topic. The goals of GDC are to facilitate abstinence, encourage mutual support, and teach new ways to cope with substance-related problems. Sessions begin with a check-in on substance use and craving, followed by a substance-related topic. GDC is delivered in a mixed-gender group composition and does not specifically address gender-specific themes for men or for women.
2.5. Assessments
2.5.1. Schedule of assessments
Assessments of substance use were conducted at baseline (assessed for the 60 days prior to interview) and then monthly for months 1–6 and 9 (months 1–3 were in-treatment assessments and months 4–6 and 9 were post-treatment follow-up assessments). Client satisfaction was assessed at weeks 3, 6, 9, and 12.
2.5.2. Substance use assessments
Substance use data were obtained by trained, supervised research assistants with the Addiction Severity Index (ASI) (McLellan et al., 1992). The ASI is a widely employed multidimensional assessment of substance-related problems. The Timeline Follow-Back technique (Sobell and Sobell, 1992), which uses a calendar to assist recall, supplemented the drug and alcohol sections of the ASI. Urine toxicology screens to validate self-reports were obtained at group sessions and monthly assessments.
2.5.3. Group treatment assessments
The Client Satisfaction Questionnaire (CSQ-8) (Nguyen et al., 1983) plus four additional questions about the helpfulness of therapist, group content, and group composition assessed overall treatment satisfaction.
2.6. Therapists
All group therapists were doctoral or master’s level therapists with ≥3 years of substance use disorder treatment experience. All therapists were women to eliminate any therapist–subject gender matching effects (Fiorentine and Hillhouse, 1999; Sterling et al., 1998). The two pre-pilot group sequences were conducted by a psychiatrist (SFG) and a psychologist. Two master’s level therapists were trained prior to randomization of the first pilot sequence. One of the therapists was trained in GDC and the other in WRG. In order to minimize therapist effects in the two pilot sequences, after the first pilot was completed, the therapists were retrained to deliver the other treatment (e.g., the GDC therapist was trained to deliver WRG and the WRG therapist was trained to deliver GDC in the second pilot sequence).
To encourage fidelity to the manuals, group sessions were videotaped and therapists were supervised weekly by the senior authors of the respective manuals (SFG for WRG; Dennis C. Daley for GDC). Adherence/competence rating scales were completed by the supervisor after each session.
2.7. Primary and secondary outcomes
Primary outcomes were the change from baseline in the number of days per month of any substance use (i.e., drug and/or alcohol) and the change from baseline in the number of drinking days per month. Secondary outcomes were the change from baseline in the number of drinks per drinking day and change from baseline in the Addiction Severity Index composite score. Outcomes were conducted by treatment phase and compared to baseline with the “in-treatment” phase comprising months 1–3, and the “post-treatment” phase comprising months 4–6 and 9.
2.8. Groups available for comparison
Analyses focus on comparative outcomes between women enrolled in single-gender WRG and mixed-gender GDC groups. Outcomes of male participants in GDC (N = 10) were not the focus of these analyses and are therefore not included. We focused on four sets of comparisons for analysis. We compared subjects in pre-pilot WRG (N = 13) with subjects in pilot WRG (N = 16) in order to assess any differences in baseline characteristics and outcomes among women enrolled in pre-pilot and pilot phases of WRG. In order to assess the differences in baseline characteristics and outcomes among women randomized to study versus control conditions, we compared women enrolled in the pilot WRG (N = 16) with women enrolled in GDC (N = 7). Finally, because the manual-based treatment changed very little between pre-pilot and pilot phases, in order to gain the broadest assessment of the experience of WRG versus GDC, we compared outcomes for all WRG subjects (N = 29) to those women enrolled in GDC (N = 7), as well as those enrolled in pre-pilot WRG (N = 13) compared with women enrolled in GDC (N = 7). We present results of all four sets of comparison by phase of treatment (i.e., in-treatment and post-treatment follow-up phases).
2.9. Statistical analysis
We implemented a general mixed model analysis of variance (MMANOVA) (Schwarz, 1993). This framework models the means per group over the respective time period and the covariance between the repeated measures over the assessments. The MMANOVA does not assume a linear relationship between the outcome variable and time. Specifically for this sample, the MMANOVA approach estimates a separate mean for each phase of treatment per group. The MMANOVA model is called a “mixed” model because it includes both fixed (e.g., treatment, phase, gender) and random (subject-specific) terms. MMANOVA allows for randomly missing observations, which are not included in the analysis. Inspection of the data indicated two WRG subjects and one GDC subject provided only baseline assessments; therefore, our analysis is a modified intent-to-treat analysis with three randomized subjects lost to follow-up who provided no post-baseline assessments. There were no significant differences in completeness of data between WRG subjects and female GDC subjects. Contrasts between groups within treatment, within groups between phases, and differences between groups across phase are made. To measure the difference between groups, a group main effect is modeled. The difference between groups across phase is modeled by including the interaction of treatment and phase. A similar utilization of the MMANOVA was conducted in Crits-Christoph et al. (1999) in the longitudinal study of cocaine addiction.
Keselman et al. (1998) discuss the need to inspect the validity of the assumptions for the statistical model used. A key assumption for the use of the General Linear Model (GLM) framework, and its extensions including the MMANOVA, is normality of the outcome measure, for which the primary and secondary measures under investigation were not met. Since our goal is comparing changes from baseline, we subtracted baseline from all outcomes to see if this resulted in improvement. Subtraction of baseline from all outcomes resulted in near normality for each. With the limited sample size, a compound symmetry covariance structure was fit. Effect size derivation for all effects of interest was derived based on the _F_-test for compound symmetry models discussed by Rosenthal and Rosnow (1991) and Verbeke and Molenberghs (2000).
3. Results
3.1. Baseline characteristics
Women in the study ranged in age from 23 to 67 years with a mean age of women in the pilot GDC of 58.3 years (S.E. = 2.72) and of all WRG women of 45.0 years (S.E. = 1.99). As indicated, randomization did not achieve equivalence between conditions as a function of age with the mean age of women in pilot WRG of 42.1 years (S.E. = 2.64, t(34) = −3.09, p < 0.01). Age was included as a covariate in all continuous outcome analyses. There were no other statistically significant differences in baseline characteristics between women enrolled in WRG and GDC treatment conditions.
The sample was predominantly white (e.g., one subject endorsed Native American ethnicity) and well-educated. All subjects had attained at least a high school education, and 86.2% of all WRG women and 85.7% of GDC women had attained at least a college education. Among all WRG women, 41.4% were married as were 42.9% of GDC women. More than half of subjects were employed outside the home with full or part-time status.
The majority of women enrolled in the study were diagnosed with current alcohol dependence as their primary substance (86.2% WRG and 100.0% GDC women), with the remaining 13.8% of WRG women diagnosed with current cannabis, cocaine, or stimulant dependence. WRG women had lifetime diagnoses of cannabis dependence and abuse (20.0%), cocaine dependence and abuse (17.0%), stimulant dependence (7.0%), sedative abuse (3.0%), and hallucinogen abuse (3.0%). GDC women had lifetime diagnoses of cannabis abuse (14.0%). None of these differences were statistically significant.
Over one-third of participants were diagnosed with other current co-occurring psychiatric disorders, including mood disorders (WRG 37.9% and GDC 42.9%), anxiety disorders (WRG 31.0% and GDC 42.9%), eating disorders (WRG 3.4% and GDC 0.0%), other Axis I disorder (WRG 3.4% and GDC 0.0%), and Axis II personality disorders (WRG 34.5% and GDC 57.1%). Approximately three-fourths of participants were diagnosed with lifetime co-occurring psychiatric disorders including mood disorders (WRG 75.9% and GDC 85.7%), anxiety disorders (WRG 44.8% and GDC 42.9%), eating disorders (WRG 20.7% and GDC 0.0%), and other Axis I disorders (WRG 3.4% and GDC 0.0%). None of these differences were statistically significant.
3.2. Substance use outcomes
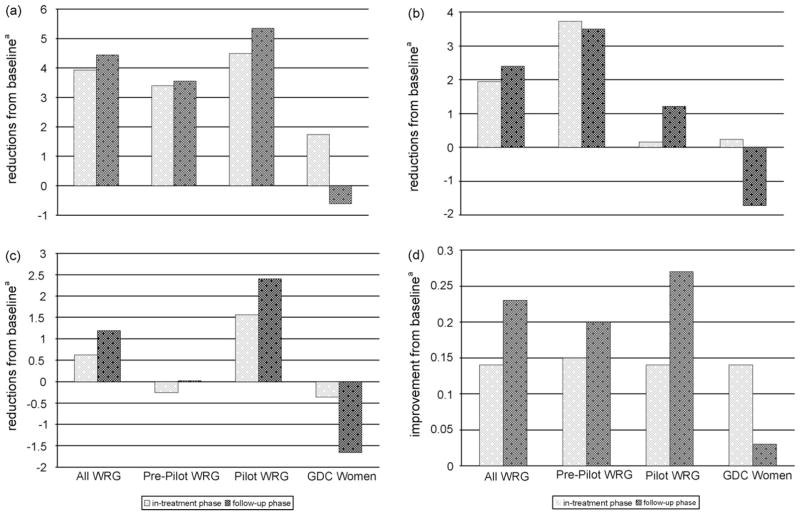
We found no differences in the mean (±S.E.) days of any substance use, drinking days, drinks per drinking day, or Addiction Severity Index composite scores at baseline across groups (see Table 1). Overall, substance use decreased from baseline during the 12-week in-treatment phase (comprising assessments at months 1–3) for all WRG and GDC groups with no significant differences in the randomized trial between the pilot WRG condition and the control GDC condition. However, reduction in mean days of substance use, mean days of alcohol use, and mean drinks per drinking day, and ASI alcohol composite scores showed continued improvement among women in the WRG treatment condition during the 6-month post-treatment follow-up phase (comprising assessments at months 4–6 and 9), while each of these outcomes worsened for the women in the GDC treatment condition (see Fig. 1a–d).
Table 1.
Baseline substance use characteristics (assessed for 60 days prior to interview)
| All WRG (n = 29) | Pre-pilot WRG (n = 13) | Pilot WRG (n = 16) | GDC women (n = 7) | |||||
|---|---|---|---|---|---|---|---|---|
| Mean | S.E. | Mean | S.E. | Mean | S.E. | Mean | S.E. | |
| Days any substance use | 13.17 | (1.87) | 14.44 | (2.57) | 12.14 | (2.72) | 11.09 | (2.11) |
| Drinking days | 10.38 | (1.42) | 12.60 | (2.31) | 8.58 | (1.68) | 10.23 | (1.80) |
| Drinks/drinking day | 6.56 | (0.93) | 7.44 | (1.01) | 5.80 | (1.50) | 6.14 | (1.18) |
| ASI alcohol comp. score | 0.45 | (0.05) | 0.46 | (0.06) | 0.44 | (0.07) | 0.44 | (0.11) |
Fig. 1.
Primary outcomes for the in-treatment phase and follow-up phase of the Women’s Recovery Group Study; (a) mean reduction in days of any substance use, in treatment and follow-up; (b) mean reduction in drinking days, in treatment and follow-up; (c) mean reduction in drinks per drinking day, in treatment and follow-up; (d) mean improvement in ASI alcohol composite score, in treatment and follow-up. aIncreasing numbers along the _y_-axis signify greater reductions from baseline or greater improvement from baseline ASI. Note: Means are adjusted for age.
3.2.1. Reduction in days of any substance use
Women in the WRG treatment groups, both pre-pilot and pilot, showed decreases from baseline in mean days of substance use during treatment and continued reductions during the 6-month post-treatment (assessments comprising months 4–6 and 9) (see Fig. 1a). The mean (±S.E.) reduction for all WRG groups during the in-treatment portion was 3.93 ± 1.35, with a mean (±S.E.) reduction during follow-up portion of 4.45 ± 1.32. While women in the GDC control condition improved with decreased mean days of any substance used during the 12-week in-treatment phase with a mean in-treatment reduction of 1.74 days ± 3.07, they did not continue to improve in the 6-month post-treatment follow-up period. In fact, GDC women showed an increase from baseline in mean days of any substance used (0.60 ± 3.02). The differences between WRG and GDC groups were not statistically significant but the effect size for this comparison between the pilot WRG groups versus the GDC groups in the follow-up phase was 0.59; between pre-pilot WRG and GDC groups was 0.45; and between all WRG groups and GDC was 0.55.
3.2.2. Reduction in drinking days
Women in the WRG treatment groups, both pre-pilot and pilot, showed decreases from baseline in mean days of alcohol use during treatment (1.95 ± 0.98) and continued reductions in the 6-month post-treatment phase (2.40 ± 0.95) (see Fig. 1b). Women in the GDC groups showed decreases in mean days of alcohol use during treatment (0.23 ± 2.23) but showed an increase in mean number of drinking days during the 6-month post-treatment phase (1.72 ± 2.17). The difference between pilot WRG and GDC groups did not reach statistical significance and had an effect size of 0.36. However, there was a trend toward statistical significance in the comparisons during the post-treatment follow-up phase between pre-pilot WRG and GDC (p = .053, effect size = 0.72) and all WRG groups versus GDC (p = .094, effect size = 0.62).
3.2.3. Reduction in drinks per drinking day
Overall, women in the WRG groups showed a decrease in the number of drinks per drinking day from baseline during the in-treatment phase (0.62 ± 0.72) and continued reductions in the 6-month post-treatment phase (1.19 ± 0.71) (see Fig. 1c). However, women in the GDC groups showed an increase in mean drinks per drinking day from baseline during the in-treatment phase (0.36 ± 1.64), as well as an even greater increase from baseline during the 6-month post-treatment phase (1.66 ± 1.62). The difference between pilot WRG groups and GDC groups reached statistical significance during the 6-month post-treatment follow-up phase (p < .031) with an effect size of 0.81. Although not statistically significant, the effect size for this difference during the 6-month post-treatment follow-up phase for pre-pilot WRG groups versus GDC was 0.39 and for all WRG groups compared with GDC groups was 0.58.
3.2.4. Improvement in ASI composite scores
Women in all WRG groups showed improvements in ASI alcohol composite scores during the in-treatment phase (0.14 ± 0.04) and continued to demonstrate improvement during the 6-month post-treatment follow-up (0.23 ± 0.04) (see Fig. 1d). Women in the GDC condition also showed improvements in ASI alcohol composite scores during the treatment phase (0.14 ± 0.10), but GDC women demonstrated less improvement in the post-treatment follow-up phase (0.03 ± 0.10). There was a trend toward statistical significance for the comparison of the pilot WRG group condition and the GDC group condition in the 6-month post-treatment follow-up phase (p = .051), with an effect size of 0.73. Effect sizes in the post-treatment follow-up phase comparing pre-pilot WRG with GDC groups and all WRG groups with GDC were 0.56 and 0.69, respectively.
3.2.5. Quality assurance
We assessed self-report validity of drug and alcohol use. Urine toxicology screens and breath alcohol tests were obtained at weekly group sessions. There were no positive breath alcohol tests for any subject prior to the weekly groups or monthly assessment sessions. The urine toxicology screens followed chain-of-custody procedures and identified opiates, amphetamines, barbiturates, benzodiazepine, cocaine, cannaboids, methadone, methaquaalone, phencyclidine, and propoxyphene, and using the Enzyme-Linked ImmunoSorbent Assay (ELISA) technique. Positive screen results were confirmed using gas chromatography/mass spectrometry (GC/MS). There were 12 weekly urine screens obtained at each weekly group session during the in-treatment phase and seven urine screens obtained at monthly research assessment visits at months 1–6 and 9. Urine toxicology results at each weekly group were compared to weekly self-report of substance use. Of these, 81.5% of self-report data were concordant with weekly urine screen. Of the 18.5% of non-concordant self-reports, the majority (15.5%) self-reported substance use not detected by urine screen, and only 3.0% had a positive urine screen when no use was self-reported. At each monthly research assessment interview, urine screens were obtained and substance use data were collected using the Timeline Follow-Back technique (Sobell and Sobell, 1992). These monthly assessments took place during the in-treatment phase at months 1–3, and in the post-treatment follow-up phase at months 4–6 and 9. In our comparison of monthly urine screens to the TLFB data, 84.8% of self-reports were concordant with urine screen results. Of the 15.2% self-reports that were non-concordant with urine screens, 7.8% reported substance use not detected by urine screen, and 7.3% demonstrated a positive urine screen when no use was self-reported. Thus, 97% of weekly in-treatment self-reports and 93% of monthly in- and post-treatment self-reports were either consistent with urine toxicology screens or reported use undetected by urine screens. In situations where participants did not report use detected by urine screen, discrepancies were resolved at the next visit.
3.3. Client satisfaction
Client satisfaction was high for women enrolled in the pilot WRG groups as well as the GDC groups with mean scores ranging from 43.13 to 45.46 (S.E. = 0.79) for the WRG women and mean scores ranging from 38.00 to 43.75 (S.E. = 1.17) for the GDC women. However, client satisfaction across the four ratings was significantly greater for women in pilot WRG compared to women in GDC, with an average score of 44.49 for WRG women and 40.44 for GDC women (p < .009 with effect size of 1.11).
4. Discussion
While treatment delivered in an all-women’s group context has been proposed to be most effective for women with co-occurring post-traumatic stress and substance use disorders or past histories of trauma (Hien et al., 2004; Najavits et al., 1998), no randomized controlled trial has compared single-gender women-focused substance abuse group therapy with standard mixed-gender group treatment for women with substance use disorders (Greenfield et al., 2007). This Stage I trial demonstrates that in this sample, the in-treatment efficacy for women with substance use disorders of a women-focused, single-gender Women’s Recovery Group is at least equivalent to an effective mixed-gender control group, Group Drug Counseling. More significant, however, is that in the 6 months following treatment completion, subjects in the experimental women-focused, single-gender WRG showed sustained improvements in all substance abuse treatment outcomes, whereas the subjects in the mixed-gender control condition, GDC, not only did not sustain these improvements, but their post-treatment outcomes worsened from baseline in three of four outcomes assessed.
The initial hypothesis of this study was that more favorable outcomes of WRG than GDC would result from a synergy between gender-specific content of WRG and enhanced group processes, including comfort and cohesion in the WRG compared with GDC group condition. Previous reports have suggested that gender differences in interaction styles might negatively affect women in mixed-gender groups (Greenfield et al., 2007; Hodgins et al., 1997; LaFave and Echols, 1999; Nelson-Zlupko et al., 1995; Schliebner, 1994; Welle et al., 1998; Wilke, 1994). Women differ significantly from men in antecedents, risks, progression, consequences, and presentation of their substance abuse problem, as well as in certain predictors of relapse to substance use (Davis, 1994; Hodgins et al., 1997; Hughes et al., 1995; Pelissier et al., 2003; Saunders et al., 1993). It is often asserted that women are more likely to address psychosocial issues relevant to recovery in a single-gender, women-focused treatment (Jansson et al., 1996; Knight et al., 1999; Nelson-Zlupko et al., 1995; Volpicelli et al., 2000). The women-focused content of the WRG group, combined with the enhanced comfort in discussing more intimate matters relevant to relapse and recovery in a single-gender setting, may have contributed to sustained and continued improvements in the 6 months following treatment for the WRG compared with the GDC groups.
Women in the WRG may have been able to more openly share specific concerns regarding their substance abuse and triggers to relapse (especially concerning intimate partners or family roles and substance abuse among other topics) because this information was presented as an integral part of the session topics and the treatment, and because the all-women’s group composition promoted comfort in openly discussing these topics and receiving support from other group members.
An increased sense of comfort and safety afforded by an all-women’s setting is thought to enhance outcomes for women (Swift and Copeland, 1996; Nelson-Zlupko et al., 1996). The precise mechanisms by which such experience, as well as the focus on issues related to women’s substance abuse, might translate into enhanced 6-month post-treatment substance abuse outcomes have not been elucidated in previous studies. However, a psychotherapy-by-time effect has been previously reported for individual cognitive-behavioral therapy for cocaine dependent individuals compared with supportive clinical management (Carroll et al., 1994). The authors hypothesized that this effect might be due to a delayed emergence of the specific effects of the cognitive-behavioral relapse prevention treatment because the goals of such treatment are to provide generalizable coping skills that can be implemented after formal treatment ends (Carroll et al., 1994). It is possible that several aspects of WRG may have had a similar psychotherapy-by-time effect by enhancing acceptance of substance abuse as an illness (e.g., reducing denial, ambivalence, and feelings of stigma), increasing effective relapse prevention strategies through identification of gender-specific triggers to relapse, enhancing attachment to and retention in treatment, and increasing social support. Each of these has been postulated to heighten relapse prevention and produce better substance abuse treatment outcomes in general (Hser et al., 2004; Irvin et al., 1999), but may have specific importance to women in recovery (Blume, 1990; Brady and Randall, 1999; Green et al., 2004; Grella, 1999; Nelson-Zlupko et al., 1995; Strantz and Welch, 1995). Reducing feelings of denial and stigma may be of even greater significance for women seeking treatment for substance abuse (Blume, 1990). Identification of relapse prevention strategies that are women-specific, such as partner relationships or caretaking roles, may improve women’s outcome over time as they learned to implement these techniques (Hodgins et al., 1997; Nelson-Zlupko et al., 1995). The WRG may have enhanced attachment to and retention in treatment which have been demonstrated to improve substance abuse outcomes in women (Green et al., 2004; Greenfield et al., 2007; Hser et al., 2003). Through its emphasis on women-specific content as well as all-women group composition, the WRG may have improved 6-month post-treatment outcomes through one or more of these putative mechanisms of action. Such mechanisms of action within WRG compared with the control condition, GDC, will be the subject of future analysis.
While all women enrolled in this study had high satisfaction with their treatment, women enrolled in WRG reported significantly greater satisfaction than the women in the GDC group. This may reflect enhanced satisfaction with content of the sessions, subjective experiences of group process within an all women group composition, some combination of both of these, or other unidentified factors.
There are a number of limitations to this study. This is a Stage I behavioral therapy development trial, and therefore yields a small sample for comparison; it is possible that we were, therefore, unable to detect differences between groups. Only a small proportion of women enrolled in the study were diagnosed with current drug dependence, while the majority had current alcohol dependence. The women in this sample were almost all white and well-educated. These particular characteristics make it hard to know how the results of this study would generalize to other populations with different demographic characteristics or to populations predominantly with drug dependence. However, the manual contains material addressing a broad range of antecedents and consequences of substance abuse in women. It also contains language meant to be inclusive of diverse populations, as well as simplified language and ‘take-home messages’ meant to reach a population with lower educational attainment than the current sample. Only further testing can establish efficacy of the WRG in a larger, more heterogeneous population. Another potential limitation is that therapists were not blind to the study hypotheses and could have fostered greater improvements among those in the WRG. However, this possibility is belied by the finding of no difference in the in-treatment response, and greater improvements among those in the WRG than GDC condition during the 6-month post-treatment period.
The present study is the first randomized controlled trial of a new, manual-based, women-focused, single-gender group therapy compared with a manual-based mixed-gender group treatment with demonstrated effectiveness. While in-treatment improvement in substance abuse outcomes was not different between the two treatments, the Women’s Recovery Group demonstrated continued improvement in substance abuse outcomes 6-month post-treatment compared with the mixed-gender Group Drug Counseling. In spite of the small sample size, the magnitude of the effect of these differences was medium to large and reached statistical significance for one outcome measure. While demographic homogeneity limits generalizability of this Stage I trial, the results of the study nevertheless warrant a larger trial with a more diverse population. Further examination of mediators and moderators of this outcome, as well as of the relative contributions of group process compared with women-focused content, as potential mechanisms of action supporting the efficacy of this new group treatment for women, will also be necessary.
Supplementary Material
01
Acknowledgments
This research was supported by grants DA 15434 (SFG) and DA 019855 (SFG) from the National Institute on Drug Abuse. The authors gratefully acknowledge Roger D. Weiss, MD for his review of the manuscript; Grace Hennessy, MD and Hadine Joffe, MD, MSc for their contributions to the initial Women’s Recovery Group manual; Jessica Nargiso, MA for her contributions to research for the manual; Kathleen Brady, MD, PhD for her review of the manual; Dennis C. Daley, PhD for his training and supervision of Group Drug Counseling; and Monika Kolodziej, PhD, Barbara Raymond, MSW, and Laura Ruegg, MSW for serving as therapists.
Appendix A. Supplementary data
Supplementary data associated with this article can be found, in the online version, at doi:10.1016/j.drugalcdep.2007.02.009.
Footnotes
1
A figure depicting the hypothesized mechanism guiding the development of the WRG study is provided as supplementary material in the online version of this paper at doi:10.1016/j.drugalcdep.2007.02.009.
2
A table listing the session topics is provided as supplementary material in the online version of this paper at doi:10.1016/j.drugalcdep.2007.02.009.
References
- Beckman L. Entry of women of diverse backgrounds into alcoholism treatment. In: Lewis JA, editor. Addictions: Concepts and Strategies for Treatment. Aspen Publishers; Gaithersburg, MD: 1994. pp. 365–374. [Google Scholar]
- Berkowitz G, Peterson S, Brindis C. Methodological issues and practices in measuring perinatal alcohol and other drug treatment outcomes. Addict Res. 1998;6 (5):435–452. [Google Scholar]
- Blume S. Chemical dependency in women: important issues. Am J Drug Alcohol Abuse. 1990;16 (3):297–307. doi: 10.3109/00952999009001591. [DOI] [PubMed] [Google Scholar]
- Brady KT, Randall CL. Gender differences in substance use disorders. Psychiatr Clin North Am. 1999;22:241–252. doi: 10.1016/s0193-953x(05)70074-5. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Rounsaville BJ, Nich C, Gordon LT, Wirtz PW, Gawin F. One-year follow-up of psychotherapy and pharmacotherapy for cocaine dependence: delayed emergence of psychotherapy effects. Arch Gen Psychiatry. 1994;51:989–997. doi: 10.1001/archpsyc.1994.03950120061010. [DOI] [PubMed] [Google Scholar]
- Crits-Christoph P, Siqueland L, Blaine J, Frank A, Luborsky L, Onken LS, Muenz L, Thase ME, Weiss RD, Gastfriend DR, Woody G, Barber JP, Butler SF, Daley D, Salloum I, Bishop S, Najavits LM, Lis J, Mercer D, Griffin ML, Moras K, Beck AT. Psychosocial treatments for cocaine dependence: national Institute on Drug Abuse Collaborative Cocaine Treatment Study. Arch Gen Psychiatry. 1999;56:493–502. doi: 10.1001/archpsyc.56.6.493. [DOI] [PubMed] [Google Scholar]
- Daley DC, Mercer D, Carpenter G. Therapy Manuals for Drug Addiction. USDHHS; Rockville, MD: 2002. Group drug counseling for cocaine dependence. [Google Scholar]
- Davis S. Drug treatment decisions of chemically-dependent women. Int J Addict. 1994;29:1287–1304. doi: 10.3109/10826089409047943. [DOI] [PubMed] [Google Scholar]
- Fiorentine R, Hillhouse MP. Drug treatment effectiveness and client–counselor empathy. J Drug Issues. 1999;29:59–74. [Google Scholar]
- First M, McQueen L, Pincus H. DSM-IV Coding Update. 1996. American Psychiatric Publishing, Inc; Washington, D.C: 1996. [Google Scholar]
- Green CA, Polen MR, Lynch FL, Dickinson DM, Bennett MD. Gender differences in outcomes in an HMO-based substance abuse treatment program. J Addict Dis. 2004;23:47–70. doi: 10.1300/J069v23n02_04. [DOI] [PubMed] [Google Scholar]
- Greenfield SF. Women and substance use disorders. In: Jensvold MF, Hamilton JA, editors. Psychopharmacology of Women: Sex, Gender, and Hormonal Considerations. American Psychiatric Press, Inc; Washington, D.C: 1996. pp. 299–321. [Google Scholar]
- Greenfield SF, Brooks AJ, Gordon SM, Green CA, Kropp F, McHugh RK, Lincoln MF, Hien D, Miele G. Substance abuse treatment entry, retention, and outcome in women: a review of the literature. Drug Alcohol Depend. 2007;86:1–21. doi: 10.1016/j.drugalcdep.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grella CE. Women in residential drug treatment: differences by program type and pregnancy. J Health Care Poor Underserved. 1999;10:216–229. doi: 10.1353/hpu.2010.0174. [DOI] [PubMed] [Google Scholar]
- Hernandez-Avila CA, Rounsaville BJ, Kranzler HR. Opioid-, cannabis- and alcohol-dependent women show more rapid progression to substance abuse treatment. Drug Alcohol Depend. 2004;74:265–272. doi: 10.1016/j.drugalcdep.2004.02.001. [DOI] [PubMed] [Google Scholar]
- Hien DA, Cohen LR, Miele GM, Litt LC, Capstick C. Promising treatments for women with comorbid PTSD and substance use disorders. Am J Psychiatry. 2004;161:1426–1432. doi: 10.1176/appi.ajp.161.8.1426. [DOI] [PubMed] [Google Scholar]
- Hodgins DC, el-Guebaly N, Addington J. Treatment of substance abusers: single or mixed gender programs? Addiction. 1997;92:805–812. [PubMed] [Google Scholar]
- Hser Y, Evans E, Huang D, Anglin D. Relationship between drug treatment services, retention, and outcomes. Psychiatr Serv. 2004;55 (7):767–774. doi: 10.1176/appi.ps.55.7.767. [DOI] [PubMed] [Google Scholar]
- Hser Y, Huang D, Teruya CM, Anglin DM. Gender comparisons of drug abuse treatment outcomes and predictors. Drug Alcohol Depend. 2003;72:255–264. doi: 10.1016/j.drugalcdep.2003.07.005. [DOI] [PubMed] [Google Scholar]
- Hughes PH, Coletti SD, Neri RL, Urmann CF, Stahl S, Sicilian DM, Anthony JC. Retaining cocaine-abusing women in a therapeutic community: the effect of a child live-in program. Am J Public Health. 1995;85:1149–1152. doi: 10.2105/ajph.85.8_pt_1.1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irvin J, Bowers C, Dunn M, Wang M. Efficacy of relapse prevention: a meta-analytic review. J Cons Clin Psychol. 1999;67 (4):563–570. doi: 10.1037//0022-006x.67.4.563. [DOI] [PubMed] [Google Scholar]
- Jansson LM, Svikis D, Lee J, Paluzzi P, Rutigliano P, Hackerman F. Pregnancy and addiction: a comprehensive care model. J Subst Abuse Treat. 1996;13:321–329. doi: 10.1016/s0740-5472(96)00070-0. [DOI] [PubMed] [Google Scholar]
- Kauffman E, Dore M, Nelson-Zlupko L. The role of women’s therapy groups in the treatment of chemical dependence. Am J Orthopsychiatry. 1995;65 (3):355–363. doi: 10.1037/h0079657. [DOI] [PubMed] [Google Scholar]
- Keselman HJ, Algina J, Kowalchuk RK, Wolfinger RD. A comparison of two approaches for selecting covariance structures in the analysis of repeated measurements. Comm Stat Simul Comput. 1998;27:591–604. [Google Scholar]
- Killeen T, Brady K. Parental stress and child behavioral outcomes following substance abuse residential treatment: follow-up at 6 and 12 months. J Subst Abuse Treat. 2000;19 (1):23–29. doi: 10.1016/s0740-5472(99)00078-1. [DOI] [PubMed] [Google Scholar]
- Kominars K, Dornheim L. Group approaches in substance abuse treatment. In: DeLucia-Waack JL, Gerrity DA, Kalodner CR, Riva MT, editors. Handbook of Group Counseling and Psychotherapy. Sage Publications Ltd; Thousand Oaks, CA: 2004. pp. 563–575. [Google Scholar]
- Knight DK, Hood PE, Logan SM, Chatham LR. Residential treatment for women with dependent children: one agency’s approach. J Psychoactive Drugs. 1999;31:339–351. doi: 10.1080/02791072.1999.10471764. [DOI] [PubMed] [Google Scholar]
- LaFave LM, Echols LD. An argument for choice. An alternative women’s treatment program. J Subst Abuse Treat. 1999;16:345–352. doi: 10.1016/s0740-5472(98)00051-8. [DOI] [PubMed] [Google Scholar]
- Lex BW. Some gender differences in alcohol and polysubstance users. Health Psychol. 1991;10:121–132. doi: 10.1037//0278-6133.10.2.121. [DOI] [PubMed] [Google Scholar]
- Linehan MM, Schmidt H, III, Dimeff LA, Craft JC, Kanter J, Comtois KA. Dialectical behavior therapy for patients with borderline personality disorder and drug-dependence. Am J Addict. 1999;8:279–292. doi: 10.1080/105504999305686. [DOI] [PubMed] [Google Scholar]
- Luthar SS, Suchman NE. Relational Psychotherapy Mothers’ Group: a developmentally informed intervention for at-risk mothers. Dev Psychopathol. 2000;12:235–253. doi: 10.1017/s0954579400002078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackie-Ramos R, Rice J. Group psychotherapy with methadone-maintained pregnant women. J Subst Abuse Treat. 1988;5 (3):151–161. doi: 10.1016/0740-5472(88)90004-9. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Noordsy DL, Drake RE, Fox L. Integrated Treatment for Dual Disorders: A Guide to Effective Practice. The Guilford Press; New York: 2003. [Google Scholar]
- McLellan A, Kushner H, Metzger D, Peters R. The fifth edition of the Addiction Severity Index. J Subst Abuse Treat. 1992;9 (3):199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- Najavits L, Weiss R, Liese B. Group cognitive-behavioral therapy for women with PTSD and substance use disorder. J Subst Abuse Treat. 1996;13 (1):13–22. doi: 10.1016/0740-5472(95)02025-x. [DOI] [PubMed] [Google Scholar]
- Najavits L, Weiss R, Shaw S, Muenz L. ‘Seeking safety’: outcome of a new cognitive-behavioral psychotherapy for women with posttraumatic stress disorder and substance dependence. J Trauma Stress. 1998;11 (3):437–456. doi: 10.1023/A:1024496427434. [DOI] [PubMed] [Google Scholar]
- Nelson-Zlupko L, Dore MM, Kauffman E, Kaltenbach K. Women in recovery: their perceptions of treatment effectiveness. J Subst Abuse Treat. 1996;13:51–59. doi: 10.1016/0740-5472(95)02061-6. [DOI] [PubMed] [Google Scholar]
- Nelson-Zlupko L, Kauffman E, Dore MM. Gender differences in drug addiction and treatment: implications for social work intervention with substance-abusing women. Soc Work. 1995;40:45–54. [PubMed] [Google Scholar]
- Nguyen T, Attkisson C, Stegner B. Assessment of patient satisfaction: development and refinement of a service evaluation questionnaire. Eval Program Plann. 1983;6 (3):299–314. doi: 10.1016/0149-7189(83)90010-1. [DOI] [PubMed] [Google Scholar]
- Pelissier BMM, Camp SD, Gaes GG, Saylor WG, Rhodes W. Gender differences in outcomes from prison-based residential treatment. J Subst Abuse Treat. 2003;24 (2):149–160. doi: 10.1016/s0740-5472(02)00353-7. [DOI] [PubMed] [Google Scholar]
- Piazza NJ, Vrbka JL, Yeager RD. Telescoping of alcoholism in women alcoholics. Int J Addict. 1989;24:19–28. doi: 10.3109/10826088909047272. [DOI] [PubMed] [Google Scholar]
- Reynolds KD, Coombs DW, Lowe JB, Peterson PL, Gayoso E. Evaluation of a self-help program to reduce alcohol consumption among pregnant women. Int J Addict. 1995;30:427–443. doi: 10.3109/10826089509048735. [DOI] [PubMed] [Google Scholar]
- Rosenthal R, Rosnow RL. Essentials of Behavioral Research: Methods and Data Analysis. 2. McGraw Hill; New York: 1991. [Google Scholar]
- Saunders B, Baily S, Phillips M, Allsop S. Women with alcohol problems: do they relapse for reasons different to their male counterparts? Addiction. 1993;88:1413–1422. doi: 10.1111/j.1360-0443.1993.tb02028.x. [DOI] [PubMed] [Google Scholar]
- Schliebner CT. Gender-sensitive therapy. An alternative for women in substance abuse treatment. J Subst Abuse Treat. 1994;11:511–515. doi: 10.1016/0740-5472(94)90002-7. [DOI] [PubMed] [Google Scholar]
- Schwarz CJ. The Mixed-Model ANOVA: the truth, the computer packages, the books. Am Statistician. 1993;47:48–59. [Google Scholar]
- Sobell L, Sobell M. Timeline follow-back: a technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen JP, editors. Measuring Alcohol Consumption: Psychosocial and Biochemical Methods. Humana Press, Inc; Totowa, NJ: 1992. pp. 41–72. [Google Scholar]
- Sterling R, Gottheil E, Weinstein S, Serota R. Therapist/patient race and sex matching: treatment retention and 9-month follow-up outcome. Addiction. 1998;93 (7):1043–1050. doi: 10.1046/j.1360-0443.1998.93710439.x. [DOI] [PubMed] [Google Scholar]
- Stevens S, Arbiter N. A therapeutic community for substance-abusing pregnant women and women with children: process and outcome. J Psychoactive Drugs. 1995;27 (1):49–56. doi: 10.1080/02791072.1995.10471672. [DOI] [PubMed] [Google Scholar]
- Strantz IH, Welch SP. Postpartum women in outpatient drug abuse treatment: correlates of retention/completion. J Psychoactive Drugs. 1995;27:357–373. doi: 10.1080/02791072.1995.10471701. [DOI] [PubMed] [Google Scholar]
- Swift W, Copeland J. Treatment needs and experiences of Australian women with alcohol and other drug problems. Drug Alcohol Depend. 1996;40:211–219. doi: 10.1016/0376-8716(95)01209-5. [DOI] [PubMed] [Google Scholar]
- Verbeke G, Molenberghs G. Linear Mixed Models for Longitudinal Data. Spinger-Verlag; New York: 2000. [Google Scholar]
- Volpicelli J, Markman I, Monterosso J, Filing J, O’Brien C. Psychosocially enhanced treatment for cocaine-dependent mothers: evidence of efficacy. J Subst Abuse Treat. 2000;18:41–49. doi: 10.1016/s0740-5472(99)00024-0. [DOI] [PubMed] [Google Scholar]
- Weiss RD, Griffin ML, Kolodziej ME, Greenfield SF, Najavits LM, Daley DC, Doreau HR, Hennen JA. A randomized trial of integrated group therapy versus group drug counseling for patients with bipolar disorder and substance dependence. Am J Psychiatry. 2007;164 (4):100–107. doi: 10.1176/ajp.2007.164.1.100. [DOI] [PubMed] [Google Scholar]
- Welle D, Falkin GP, Jainchill N. Current approaches to drug treatment for women offenders. J Subst Abuse Treat. 1998;15:151–163. doi: 10.1016/s0740-5472(97)00135-9. [DOI] [PubMed] [Google Scholar]
- Wilke D. Women and alcoholism: how a male-as-norm bias affects research, assessment, and treatment. Health Soc Work. 1994;19:29–35. doi: 10.1093/hsw/19.1.29. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
01