Personality and All-Cause Mortality: Individual-Participant Meta-Analysis of 3,947 Deaths in 76,150 Adults (original) (raw)
Abstract
Personality may influence the risk of death, but the evidence remains inconsistent. We examined associations between personality traits of the five-factor model (extraversion, neuroticism, agreeableness, conscientiousness, and openness to experience) and the risk of death from all causes through individual-participant meta-analysis of 76,150 participants from 7 cohorts (the British Household Panel Survey, 2006–2009; the German Socio-Economic Panel Study, 2005–2010; the Household, Income and Labour Dynamics in Australia Survey, 2006–2010; the US Health and Retirement Study, 2006–2010; the Midlife in the United States Study, 1995–2004; and the Wisconsin Longitudinal Study's graduate and sibling samples, 1993–2009). During 444,770 person-years at risk, 3,947 participants (54.4% women) died (mean age at baseline = 50.9 years; mean follow-up = 5.9 years). Only low conscientiousness—reflecting low persistence, poor self-control, and lack of long-term planning—was associated with elevated mortality risk when taking into account age, sex, ethnicity/nationality, and all 5 personality traits. Individuals in the lowest tertile of conscientiousness had a 1.4 times higher risk of death (hazard ratio = 1.37, 95% confidence interval: 1.18, 1.58) compared with individuals in the top 2 tertiles. This association remained after further adjustment for health behaviors, marital status, and education. In conclusion, of the higher-order personality traits measured by the five-factor model, only conscientiousness appears to be related to mortality risk across populations.
Keywords: meta-analysis, mortality, personality, psychology, survival analysis
Editor's note: An invited commentary on this article appears on page 676.
Personality is associated with various health outcomes (1–4), and some studies suggest that personality differences may also predict mortality risk (5–8). Personality represents enduring individual dispositions in domains of emotional reactivity, behavioral tendencies, and cognitive styles (9, 10). Mortality risk, in turn, quantifies the total illness burden that accumulates from multiple health risk factors. Thus, investigating associations between personality traits and mortality may provide insight into the most important links between personality and overall health (9, 11).
However, as illustrated by a recent literature review on personality and mortality (10), few studies have examined mortality risk by using all the major dimensions of personality variation at the same time. With some notable exceptions (6, 12–14), these studies have been based on nonrepresentative and relatively small samples (10, 15) (i.e., data that are particularly vulnerable to chance findings and publication bias). Given these limitations, currently available evidence is not yet sufficient for evaluating the public health relevance of personality dimensions in explaining mortality differentials.
To undertake an assessment of the association between personality and mortality, we pooled individual-participant data from 7 cohort studies and performed a meta-analysis to examine whether personality traits of the five-factor model predict all-cause mortality. The five-factor model is a widely accepted and validated conceptualization of personality (16), and it includes 5 higher-order personality traits—extraversion, neuroticism, agreeableness, conscientiousness, and openness to experience—that are assumed to capture the main dimensions of personality variation among individuals.
MATERIALS AND METHODS
We searched the data collections of the Inter-University Consortium for Political and Social Research (http://www.icpsr.umich.edu/icpsrweb/ICPSR/) and the Economic and Social Data Service (http://ukdataservice.ac.uk/) to identify eligible large-scale prospective cohort studies on personality and mortality. The studies had to include information on participants' vital status and personality assessed with at least the brief 15-item questionnaire based on the five-factor model. We located 7 such data sets, as follows: the British Household and Panel Survey (n = 13,823) (17); the German Socio-Economic Panel (GSOEP) Study (n = 20,434) (18); the Household, Income and Labour Dynamics in Australia (HILDA) Survey (n = 11,091) (19); the US Health and Retirement Study (n = 13,900) (20); the Midlife in the United States (MIDUS) Study (n = 6,259) (21); the Wisconsin Longitudinal Study graduate sample (n = 6,674); and the Wisconsin Longitudinal Study sibling sample (n = 3,969) (22). These are well-characterized, longitudinal cohort studies with large sample sizes. All of the studies were approved by the relevant local ethics committees. Associations between personality and all-cause mortality have been reported previously in the MIDUS sample (12) but not in the other data sets. Methodological details of the cohorts are provided in the Web Appendix, available at http://aje.oxfordjournals.org/.
In all studies, personality was assessed by using standardized questionnaire instruments based on the five-factor model of personality (16). The instruments measure 5 higher-order personality traits that sum up individual variation in several, more specific, lower-order personality dispositions. Extraversion reflects characteristics such as social assertiveness, sociability, and sensitivity to positive emotions; neuroticism is associated with low emotional stability, sensitivity to negative emotions, and anxiety proneness; agreeableness measures cooperativeness, altruism, and trust toward other people; conscientiousness is expressed as self-control, orderliness, and adherence to social norms; and openness to experience correlates with curiosity, broad-ranging interests, and open-mindedness.
Covariates included in the analyses were ethnicity/nationality (0 = white or non-Hispanic and 1 = other; except in the HILDA Survey and the GSOEP Study, in which 0 = native born and 1 = non–native born); education (0 = primary level/less than high school, 1 = secondary level/high school, and 3 = tertiary level/higher degree); marital status (0 = married/cohabiting and 1 = single); leisure-time physical inactivity (0 = moderate or high physical activity and 1 = low or no physical activity); current smoking (0 = nonsmoker and 1 = smoker); heavy alcohol consumption (frequent alcohol consumption or alcohol problems, depending on the study); and obesity (body mass index (weight (kg)/height (m)2) ≥30 calculated from self-reported height and weight).
Associations between personality traits and mortality were estimated by using Cox's proportional hazards model. On the basis of Schoenfeld residuals, we found no violation of the proportional hazards assumption for any personality trait in any cohort (all P > 0.08). Hazard ratios were calculated for both continuously coded standardized personality scores (mean = 0; standard deviation, 1) and for personality scores categorized into quintiles. Personality traits were examined both separately and after mutual adjustment, and all models were further adjusted for sex, age at baseline, and ethnicity/nationality. To examine the combined roles of smoking, physical inactivity, alcohol use, and obesity, we created a categorical sum score of the 4 dichotomous indicators of these variables and used this in the analysis. Analyses including other covariates were carried out with slightly smaller sample sizes because of missing covariate data. To explore potential sources of heterogeneity in the associations, we undertook the proportional hazards models in different subgroups separately in each cohort, and the results from these subgroup analyses were then pooled. Although exploratory, these analyses were not adjusted for multiple testing.
In sensitivity analyses, we fitted proportional hazards models by using cubic splines to examine potential nonlinear associations between personality traits and mortality risk in more detail than was allowed by categorization of personality scores. Each trait modeled with cubic splines was examined separately, adjusting for the other 4 personality traits (coded as linear covariates), as well as sex, age, and ethnicity/nationality. The pooled analysis for these models was carried out with 1-step meta-analysis, that is, by first pooling the data and then fitting the models, stratified by study. Cubic splines with 3, 4, and 5 knots were examined; the results are presented for the 3-knot models because additional knots did not substantially improve the model fit.
All models were first fitted separately within each cohort, and the results from the individual cohorts were then pooled by using random-effects meta-analysis. Standard errors in cohorts based on household sampling were calculated by using a robust estimator method to take into account the nonindependence of individuals from the same households. Heterogeneity in the effect sizes was examined on the basis of _I_2 estimates. Meta-analysis was conducted by using the metan package of Stata, version 12.1, software (StataCorp LP, College Station, Texas).
RESULTS
Descriptive statistics for the cohorts are presented in Web Table 1. The mean age at baseline was 50.9 years, and 54.4% subjects were women. In total, there were 3,947 deaths during a follow-up of approximately 444,770 person-years at risk (mean follow-up = ∼5.9 years; lack of information on exact dates of death in the MIDUS Study precluded exact calculation). Kaplan-Meier plots of cumulative mortality risk in the cohorts are shown in Web Figure 1, and correlations between personality traits are reported in Web Table 2.
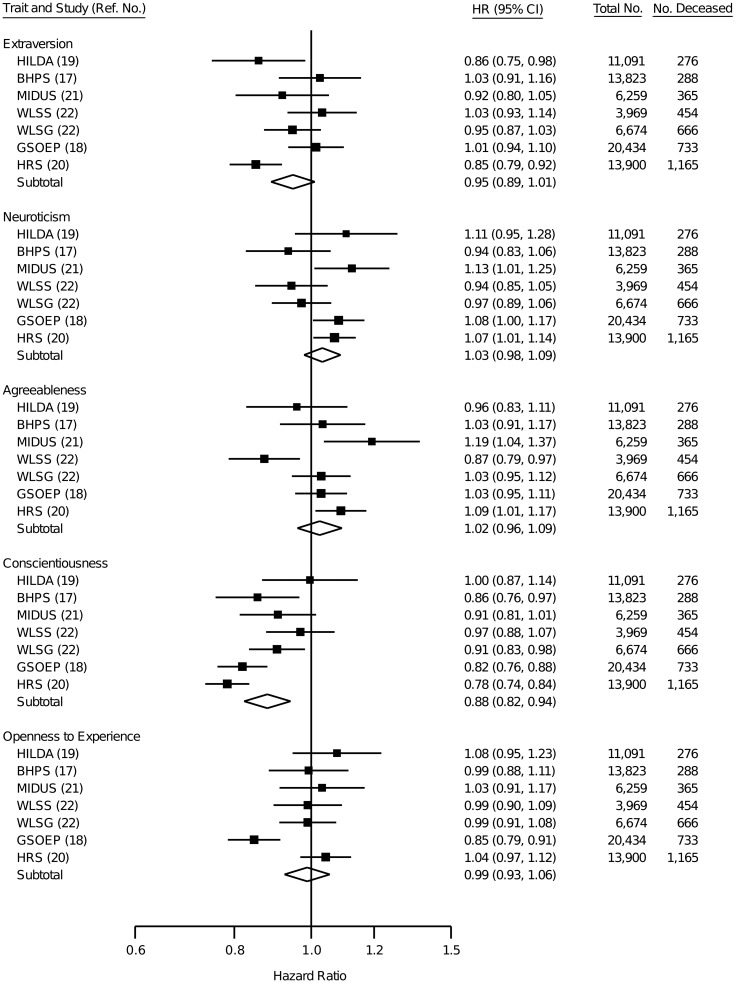
Associations between continuous personality scores and mortality risk showed that low conscientiousness was the only personality trait independently associated with higher mortality risk (Figure 1). This association was observed across studies fairly consistently, albeit not in all studies. In the pooled analysis, a conscientiousness score 1 standard deviation below the mean was associated with a 14% higher mortality risk (hazard ratio (HR) = 1 / 0.88 = 1.14). When not adjusted for the other personality traits, lower extraversion, higher neuroticism, and lower agreeableness were also associated with elevated mortality risk (model 1 in Web Table 3). Neuroticism and agreeableness were no longer associated with mortality when adjusted for conscientiousness (model 2 in Web Table 3), and only conscientiousness remained associated with mortality when all personality traits were included in the model (Figure 1; model 3 in Web Table 3). Adjustment for baseline health behaviors and obesity accounted for one-fifth of the association between low conscientiousness and mortality risk (Table 1), whereas education and marital status attenuated the association by less than 10%. Together, the covariates attenuated the hazard ratio of conscientiousness by 31%.
Figure 1.
Hazard ratios associated with a 1–standard deviation increment in personality trait score for mutually adjusted personality traits, additionally adjusted for sex, age, and ethnicity/nationality. The overall estimates are based on random-effects meta-analysis. Squares represent study-specific estimates, and diamonds represent pooled estimates of random-effects meta-analyses. Bars, 95% confidence interval (CI). BHPS, British Household Panel Survey (United Kingdom, 2006–2009); GSOEP, German Socio-Economic Panel Study (Germany, 2005–2010); HILDA, Household, Income and Labour Dynamics in Australia Survey (Australia, 2006–2010); HRS, Health and Retirement Study (United States, 2006–2010); MIDUS, Midlife in the United States Study (United States, 1995–2004); WLSG, Wisconsin Longitudinal Study's graduate sample (United States, 1993–2009); WLSS, Wisconsin Longitudinal Study's sibling sample (United States, 1994–2009).
Table 1.
Adjusted Associations Between Conscientiousness and Mortality Risk Based on Meta-Analysis of 7 Cohortsa
| Adjustment | Base Modelb | Adjusted Modelc | Attenuation, %d | Total No. | No. of Deaths | ||
|---|---|---|---|---|---|---|---|
| HR | 95% CI | HR | 95% CI | ||||
| Sex, age, ethnicity/nationality | 0.87 | 0.81, 0.93 | 76,150 | 3,947 | |||
| Additionally adjusted for | |||||||
| Behavior-related risk factorse | 0.86 | 0.79, 0.93 | 0.89 | 0.81, 0.97 | 21 | 54,372 | 3,659 |
| Marital status | 0.87 | 0.81, 0.93 | 0.88 | 0.82, 0.94 | 7 | 76,104 | 3,947 |
| Education | 0.86 | 0.81, 0.93 | 0.87 | 0.82, 0.93 | 5 | 74,984 | 3,947 |
| All of the above | 0.86 | 0.79, 0.93 | 0.90 | 0.83, 0.98 | 31 | 53,406 | 3,659 |
There was moderate to large heterogeneity in the effect sizes across studies for conscientiousness (_I_2 = 73%), extraversion (_I_2 = 65%), neuroticism (_I_2 = 54%), and agreeableness (_I_2 = 65%). The initial heterogeneity for openness to experience (_I_2 = 70%) was reduced to 0% when the GSOEP cohort was excluded from the analysis. To examine whether interaction effects between different personality traits accounted for any of the heterogeneity, we examined all the possible trait combinations (e.g., whether the association between extraversion and mortality risk was dependent on the other 4 personality traits). Of the 70 interaction effects tested, only 5 were statistically significant at conventional levels (data not shown), and none of these was sufficiently consistent across studies. We did not pursue these exploratory analyses further because we had no specific hypotheses regarding trait interactions.
Subgroup analysis
Subgroup analyses indicated that the association between higher conscientiousness and lower mortality risk did not differ by sex, ethnic/national majority versus minority, age, educational level, number of behavior-related health risks, or self-reported general health at baseline (Web Table 4). For the other 4 personality traits, the above subgroup analyses also suggested no systematic sources of heterogeneity in the effect sizes (Web Table 4). Of the 40 interaction tests undertaken, only 2 were statistically significant (P < 0.05), and both involved geographical location; conscientiousness was not associated with mortality in the Australian sample (HR = 1.00, 95% CI: 0.87, 1.14), although higher extraversion was associated with lower mortality in the Australian sample (HR = 0.86, 95% CI: 0.75, 0.98) but not in the European or US samples. However, these results need to be interpreted in light of the fact that the Australian estimate was based on only 1 study, and that 38 other interactions were tested at the same time with no adjustment for multiple testing.
Tests for nonlinearity
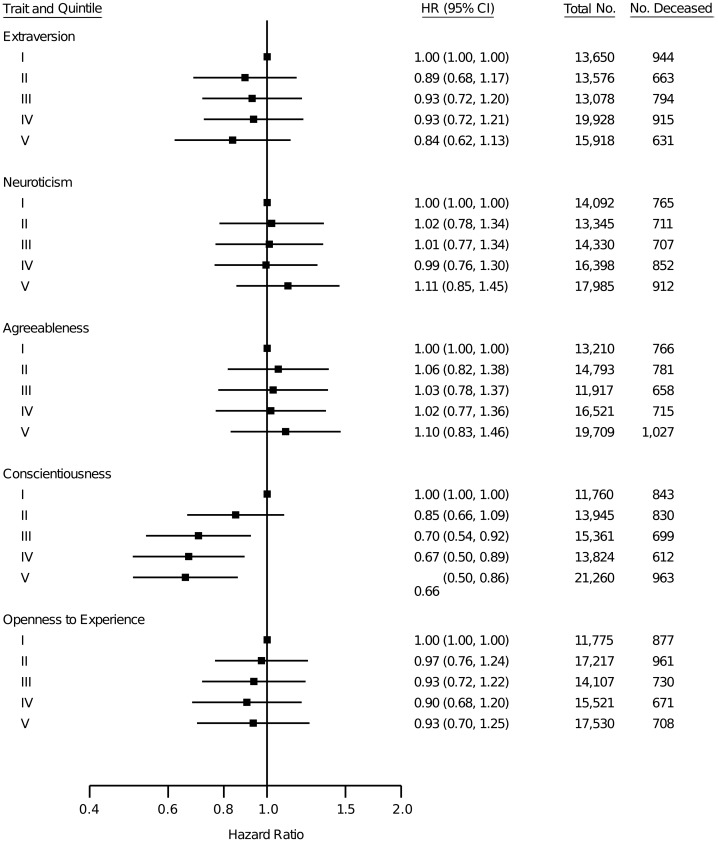
In the pooled analysis based on quintiles of personality scores (Figure 2), low conscientiousness was the only personality trait independently associated with higher mortality risk. Compared with individuals in the highest quintile of conscientiousness, individuals in the lowest quintile had 1.52 (95% CI: 1.15, 1.96) times higher mortality risk (note that, in Figure 2, the lowest quintile is the reference group). Differences in mortality risk were largest when comparing individuals who scored below versus above the mean of conscientiousness and were smaller among individuals scoring above the mean; categorization of individuals into low (the lowest tertile) versus high (2 of the highest tertiles) conscientiousness in each cohort indicated a pooled hazard ratio of 1.37 (95% CI: 1.18, 1.58) higher mortality risk in participants with low compared with high conscientiousness in the total sample.
Figure 2.
Associations between personality score quintiles and mortality risk based on random-effects meta-analysis of the 7 cohorts (representing 76,150 individuals and 3,947 deaths). For each trait, the lowest quintile is the reference category. Personality traits are mutually adjusted, and the model is further adjusted for sex, age, and ethnicity/nationality. Squares represent pooled estimates of random-effects meta-analyses for personality trait quintiles. Bars, 95% confidence interval (CI). Data were pooled from the British Household Panel Survey (United Kingdom, 2006–2009); the German Socio-Economic Panel Study (Germany, 2005–2010); Household, Income, and Labour Dynamics in Australia (Australia, 2006–2010); the Health and Retirement Study (United States, 2006–2010); Midlife in the United States (United States, 1995–2004); the Wisconsin Longitudinal Study's graduate sample (United States, 1993–2009); and the Wisconsin Longitudinal Study's sibling sample (United States, 1994–2009).
Regression analyses based on cubic splines suggested that scores for extraversion, conscientiousness, and openness to experience that were below the mean level, and scores for neuroticism and agreeableness that were above the mean level, might be more strongly related to mortality risk than the results based on overall linear association across the total range of personality scores (Web Figures 2–6). When assessed with linear models that allowed the associations to vary below versus above the mean level of personality score, the association for conscientiousness was slightly stronger below the mean (HR = 0.85, 95% CI: 0.78, 0.92) than above the mean (HR = 0.92, 95% CI: 0.86, 1.00) of conscientiousness (P for difference = 0.09) (Web Table 5). Higher neuroticism (HR = 1.10, 95% CI: 0.99, 1.22) and higher agreeableness (HR = 1.08, 95% CI: 1.00, 1.17) above the respective mean levels for each trait were weakly associated with higher mortality risk, whereas no associations were observed for neuroticism and agreeableness scores below the mean level (P for difference of below vs. above the mean = 0.07 for both personality traits; Web Table 5).
Reverse causality
Deteriorating health in the years before death might decrease conscientiousness, and such reverse causal effects could bias the association between conscientiousness and subsequent mortality risk. To evaluate reverse causation bias, we examined whether the hazard ratio of conscientiousness was affected when deaths occurring near the time of personality assessment were excluded from the analysis (the MIDUS cohort was excluded because of lack of information on date of death). The association remained largely unchanged when censoring from the analysis all 621 deaths occurring within 1 year (HR = 0.85, 95% CI: 0.79, 0.91), all 1,753 deaths occurring within 3 years (HR = 0.85, 95% CI: 0.78, 0.91), or all 2,922 deaths occurring within 5 years (HR = 0.90, 95% CI: 0.85, 0.96) of the personality assessment. This finding provides evidence against bias due to reverse causality.
DISCUSSION
With a pooled sample of more than 76,000 individuals from the United States, the United Kingdom, Germany, and Australia, this is the first individual-participant meta-analysis of personality and mortality. Our findings suggest that low conscientiousness is associated with an increased risk of death from all causes. Individuals in the lowest tertile of conscientiousness had a 37% higher mortality rate than individuals in the 2 higher tertiles of conscientiousness. The other 4 personality traits—extraversion, neuroticism, agreeableness, and openness to experience—were not consistently associated with mortality risk across studies when all of the personality traits were mutually adjusted, although some statistically significant associations were observed in individual studies.
The five-factor model and other detailed frameworks of personality composition started to receive wider attention only in the 1990s (16), which is why many long-running cohort studies have assessed personality with more limited instruments—often restricted to the traits of extraversion and neuroticism (23). Given the need for sufficient mortality follow-up, the health consequences of conscientiousness have received detailed attention only quite recently (24). The present finding on low conscientiousness and elevated mortality risk is in agreement with a previous literature-based meta-analysis of nearly 9,000 individuals from 20 studies, in which conscientiousness-related traits were assessed with different measures (15). The present study includes unpublished studies and is based on a larger sample, adding to the previous meta-analysis and suggesting that the association between conscientiousness and mortality risk may be weaker than previously estimated. The previous meta-analysis (15) reported a pooled odds ratio estimate of 0.64 (transformed from a correlation-based effect size of r = −0.11, 95% CI: −0.17, −0.05), and another literature review reported a similar pooled estimate of r = −0.09 (equal to an approximate OR of 0.72) between conscientiousness and mortality risk (10). Thus, the effect magnitude of a hazard ratio of 0.88 (95% CI: 0.82, 0.94) per 1–standard deviation increment in conscientiousness estimated in our analysis is only about one-half to one-third of the previously estimated effect magnitudes. This difference is similar to previously observed discrepancies between effect sizes in published versus unpublished data in other domains of psychosocial risks (25).
To test whether biological and behavioral mechanisms underlie the associations between low conscientiousness and mortality risk, we adjusted the analyses for current smoking, physical inactivity, heavy alcohol use, and obesity. The 21% reduction in mortality risk after this adjustment suggests that the association of conscientiousness with mortality is mediated in part via well-established biological and behavioral factors (26–28). It has been hypothesized that highly conscientious individuals are more likely to follow social norms and public health recommendations concerning health behaviors (29). Given that conscientious individuals also have higher levels of self-discipline, it is reasonable to assume that they are also more likely to adhere to health and treatment recommendations provided by health professionals (30). The adjusted covariates in the present study did not fully explain the association, so several other mechanisms may also underlie the association between conscientiousness and mortality risk, including mental and cognitive functioning (31), immune and endocrine system functioning (32, 33), and genetic liability (34).
The current study places conscientiousness as a risk factor almost on par with some common health behaviors and sociodemographic risks for premature death. Heavy smoking more than doubles mortality risk, whereas light smoking increases mortality risk by 50% (35, 36). Physical inactivity versus recommended moderate physical activity has been associated with an increase in all-cause mortality risk with a relative risk of 1.23 (95% CI: 1.18, 1.32) (37). Having 1 versus none of a combined list of 5 behavior-related health risk factors (smoking, physical inactivity, alcohol consumption, obesity, and unhealthy diet) has been associated with a relative risk of mortality of 1.35 (95% CI: 1.23, 1.49) (38). Compared with individuals who have a high school education or more, individuals who have a lower educational level have an average 1.46 (95% CI: 1.33, 1.59) times higher mortality risk (39). Major depressive disorder, which is related to personality traits of high neuroticism (r = 0.47), low conscientiousness (r = −0.36), and low extraversion (r = −0.25) (3) is associated with elevated mortality risk (relative risk = 1.81, 95% CI: 1.58, 2.07) (40). These relative risks associated with unhealthy behaviors, education, and depression provide comparative estimates for the 1.37-fold (95% CI: 1.18, 1.58) elevated risk of death observed in the present analysis among individuals who have low conscientiousness (the lowest tertile) compared with high conscientiousness (the 2 highest tertiles).
Assuming that the association between conscientiousness and mortality was causal, the population mortality rate would decrease by 11% in the hypothetical absence of low conscientiousness in the population (population attributable risk fraction = [P × (HR – 1)] / [1 + P × (HR – 1)], with P = 1/3 and HR = 1.37). Interventions in children and adolescents have been effective in increasing self-control, a subcomponent of the broader conscientiousness trait, by an average of 0.30 standard deviations (41, 42). Assuming, again hypothetically, that the long-term effects of such early interventions were 0.20 standard deviations, and that these interventions were successfully targeted at the lowest one-third of the conscientiousness distribution, one could expect the proportion of individuals with low conscientiousness to drop to approximately one-fourth (assuming normal distribution) and the mortality rate thereby to decrease by 2.7% (proportion shift = [(PA – PB) × (HR – 1)] / [PA × (HR – 1) + 1], with PA = 1/3, PB = 1/4, and HR = 1.37). These crude calculations suggest that the decline in the population mortality rate from reductions in low conscientiousness would be equal in magnitude to decreasing smoking prevalence by 3 percentage points (from 20% to 17%) or to increasing moderate physical activity by 13 percentage points (from 50% to 63%) in current populations. However, evidence on the feasibility of long-term interventions to change personality is limited.
Many early theories of personality and health have emphasized the role of negative emotionality (i.e., high neuroticism) and interpersonal hostility (i.e., low agreeableness) in precipitating poor health (1). A literature-based meta-analysis of personality and all-cause mortality (10) suggested an increased relative risk of mortality of 1.15 (95% CI: 1.04, 1.26) associated with 1 standard deviation of difference in negative emotionality (or high neuroticism) and an increased relative risk of mortality of 1.14 (95% CI: 1.06, 1.23) associated with 1 standard deviation of difference in disagreeableness/hostility (or low agreeableness). Surprisingly, we observed no differences in mortality risk associated with the overall variation in neuroticism or agreeableness, so our findings provide little support for these hypotheses of personality and health with respect to mortality. However, there was some evidence to suggest that very high neuroticism may be associated with an elevated risk of death; this might reflect the heightened mortality risk associated with clinical depression and other mental health problems (3, 40, 43). Very high agreeableness also had a weak association with higher mortality, which is in contrast to most previous findings suggesting that a higher level of interpersonal hostility (i.e., low agreeableness) might be harmful for health (1, 10). Given this unexpected direction of the association and the number of tests conducted, the nonlinear pattern for agreeableness identified by our analysis may represent a chance finding.
The present findings for openness to experience are in contrast to a recent meta-analysis of 11 published studies (representing 19,941 subjects) (44), which suggested that higher openness to experience is associated with lower mortality risk with an odds ratio of 0.88 (transformed from a correlation-based effect size of r = 0.051). Among the present cohorts, higher openness to experience was associated with lower mortality risk in only 1 study (HR = 0.85, 95% CI: 0.79, 0.91), and the pooled estimate suggested no association (HR = 0.99, 95% CI: 0.93, 1.06). In the future, a more detailed analysis comparing the specific personality measures, their associations with other predictors of mortality (e.g., socioeconomic status), contextual factors, and potential publication bias would be helpful to increase understanding of these discrepancies in findings across studies.
Our study does not exclude the possibility that the “Big Five” personality traits may be associated with more specific physical and mental diseases even if they are not associated with mortality risk (1). Our study is also limited by the fact that personality was assessed by using only the 5 higher-order personality traits but not their more specific lower-order subscales (16). It is possible that some of the higher-order traits are too broad to identify mortality differences associated with more specific lower-order personality trait subscales.
Literature-based meta-analyses may be subject to publication bias resulting from selective reporting of positive findings. The current data were pooled from all eligible large-scale longitudinal studies that we were able to locate from 2 publicly available databases before performing any statistical analyses on the individual cohorts. Thus, our sampling of the studies minimized publication bias. There was evidence of heterogeneity in effect sizes across studies, suggesting that some of the variation in effect sizes may reflect true differences between studies rather than random sampling error. Stratified analyses for conscientiousness suggested no effect modification by sociodemographic characteristics, including sex, age, and education. It is possible that part of the effect of heterogeneity was related to the assessment of personality by using different personality inventories. However, this is an unlikely source of major heterogeneity because different inventories assessing the five-factor model personality traits have been shown to be highly convergent (16, 45–48).
CONCLUSION
Although many personality dispositions have been associated with health outcomes (1, 9), the present results suggest that low conscientiousness is the only higher-order personality trait of the five-factor model that predicts higher mortality risk across populations. The magnitude of this association appears to be weaker than previously estimated (15), which may reflect heterogeneity in cohort characteristics, differences in the personality instruments used to assess conscientiousness, and/or potential publication bias. Although personality has been considered as a potential target for early-life interventions (41, 42), more detailed information on the feasibility, costs, and benefits of such interventions compared with other interventions directed at specific health behaviors is needed to further evaluate the significance of personality variation as an opportunity to improve population health.
Supplementary Material
Web Material
ACKNOWLEDGMENTS
Author affiliations: Institute of Behavioural Sciences, University of Helsinki, Helsinki, Finland (Markus Jokela); Department of Psychology, University of Cambridge, Cambridge, United Kingdom (Markus Jokela); Department of Epidemiology and Public Health, University College London, London, United Kingdom (G. David Batty, Archana Singh-Manoux, Mika Kivimäki); Centre for Cognitive Ageing and Cognitive Epidemiology, Department of Psychology, University of Edinburgh, Edinburgh, Scotland (G. David Batty); Finnish Institute of Occupational Health, Helsinki, Finland (Solja T. Nyberg, Marianna Virtanen); and Centre for Research in Epidemiology and Population Health, Institut National de la Santé et de la Recherche Médicale, Villejuif, France (Hermann Nabi, Archana Singh-Manoux).
This research was supported by the Academy of Finland (grants 124322, 124271, and 132944); the Bupa Foundation, United Kingdom; the Medical Research Council (grant K013351); the National Institutes of Health (grants R01HL036310 and R01AG034454); the New Occupational Safety and Health ERA Research Program; and the Finnish Work Environment Fund. The Centre for Cognitive Ageing and Cognitive Epidemiology is supported by the Biotechnology and Biological Sciences Research Council, the Engineering and Physical Sciences Research Council, the Economic and Social Research Council, the Medical Research Council, and the University of Edinburgh as part of the cross-council Lifelong Health and Wellbeing Initiative. G.D.B. is a Wellcome Trust Fellow. M.V. is an Academy of Finland Research Fellow (grant 258598). M.K. is an Economic and Social Research Council Professor.
The study sponsors did not contribute to the study design and had no role in data collection, data analysis, data interpretation, or the writing of the report.
Conflict of interest: none declared.
REFERENCES
- 1.Smith TW, MacKenzie J. Personality and risk of physical illness. Annu Rev Clin Psychol. 2006;2:435–467. doi: 10.1146/annurev.clinpsy.2.022305.095257. [DOI] [PubMed] [Google Scholar]
- 2.Bogg T, Roberts BW. Conscientiousness and health-related behaviors: a meta-analysis of the leading behavioral contributors to mortality. Psychol Bull. 2004;130(6):887–919. doi: 10.1037/0033-2909.130.6.887. [DOI] [PubMed] [Google Scholar]
- 3.Kotov R, Gamez W, Schmidt F, et al. Linking “Big” personality traits to anxiety, depressive, and substance use disorders: a meta-analysis. Psychol Bull. 2010;136(5):768–821. doi: 10.1037/a0020327. [DOI] [PubMed] [Google Scholar]
- 4.Jokela M, Hintsanen M, Hakulinen C, et al. Association of personality with the development and persistence of obesity: a meta-analysis based on individual-participant data. Obes Rev. 2013;14(4):315–323. doi: 10.1111/obr.12007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Friedman HS, Tucker JS, Schwartz JE, et al. Psychosocial and behavioral predictors of longevity: the aging and death of the ‘Termites. Am Psychol. 1995;50(2):69–78. doi: 10.1037//0003-066x.50.2.69. [DOI] [PubMed] [Google Scholar]
- 6.Terracciano A, Lockenhoff CE, Zonderman AB, et al. Personality predictors of longevity: activity, emotional stability, and conscientiousness. Psychosom Med. 2008;70(6):621–627. doi: 10.1097/PSY.0b013e31817b9371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weiss A, Costa PT. Domain and facet personality predictors of all-cause mortality among Medicare patients aged 65 to 100. Psychosom Med. 2005;67(5):724–733. doi: 10.1097/01.psy.0000181272.58103.18. [DOI] [PubMed] [Google Scholar]
- 8.Deary IJ, Batty GD, Pattie A, et al. More intelligent, more dependable children live longer: a 55-year longitudinal study of a representative sample of the Scottish nation. Psychol Sci. 2008;19(9):874–880. doi: 10.1111/j.1467-9280.2008.02171.x. [DOI] [PubMed] [Google Scholar]
- 9.Deary IJ, Weiss A, Batty GD. Intelligence and personality as predictors of illness and death: how researchers in differential psychology and chronic disease epidemiology are collaborating to understand and address health inequalities. Psychol Sci Public Interest. 2010;11(2):53–79. doi: 10.1177/1529100610387081. [DOI] [PubMed] [Google Scholar]
- 10.Roberts BW, Kuncel NR, Shiner R, et al. The power of personality: the comparative validity of personality traits, socioeconomic status, and cognitive ability for predicting important life outcomes. Perspect Psychol Sci. 2007;2(4):313–345. doi: 10.1111/j.1745-6916.2007.00047.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Friedman HS. Long-term relations of personality and health: dynamisms, mechanisms, tropism. J Pers. 2000;68(6):1089–1107. doi: 10.1111/1467-6494.00127. [DOI] [PubMed] [Google Scholar]
- 12.Chapman BP, Fiscella K, Kawachi I, et al. Personality, socioeconomic status, and all-cause mortality in the United States. Am J Epidemiol. 2010;171(1):83–92. doi: 10.1093/aje/kwp323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wilson RS, Krueger KR, Gu L, et al. Neuroticism, extraversion, and mortality in a defined population of older persons. Psychosom Med. 2005;67(6):841–845. doi: 10.1097/01.psy.0000190615.20656.83. [DOI] [PubMed] [Google Scholar]
- 14.Weiss A, Gale CR, Batty GD, et al. Emotionally stable, intelligent men live longer: the Vietnam Experience Study cohort. Psychosom Med. 2009;71(4):385–394. doi: 10.1097/PSY.0b013e318198de78. [DOI] [PubMed] [Google Scholar]
- 15.Kern ML, Friedman HS. Do conscientious individuals live longer? A quantitative review. Health Psychol. 2008;27(5):505–512. doi: 10.1037/0278-6133.27.5.505. [DOI] [PubMed] [Google Scholar]
- 16.John OP, Naumann LP, Soto CJ. Paradigm shift to the integrative big-five trait taxonomy: history, measurement, and conceptual issues. In: John OP, Robins RW, Pervin LA, editors. Handbook of Personality: Theory and Research. 3rd ed. New York, NY: Guilford Press; 2008. pp. 114–158. [Google Scholar]
- 17.Taylor MF, Brice J, Buck N, et al. British Household Panel Survey User Manual Volume A: Introduction, Technical Report and Appendices. Colchester, England: University of Essex; 2010. [Google Scholar]
- 18.Wagner GG, Frick JR, Schupp J. The German Socio-Economic Panel Study (SOEP)—Scope, evolution and enhancements. J Appl Soc Sci Studies. 2007;127:139–169. [Google Scholar]
- 19.Wooden M, Watson N. The HILDA Survey and its contribution to economic and social research (so far) Econ Rec. 2007;83(261):208–231. [Google Scholar]
- 20.Juster FT, Suzman R. An overview of the Health and Retirement Study. J Hum Resour. 1995;30(suppl):7S–56S. [Google Scholar]
- 21.Brim OG, Baltes PB, Bumpass LL, et al. Ann Arbor, MI: Inter-University Consortium for Political and Social Research; 2007. National Survey of Midlife Development in the United States (MIDUS), 1995–1996. ICPSR02760-v4. [Google Scholar]
- 22.Wollmering E. Wisconsin Longitudinal Study Handbook. Madison, WI: University of Wisconsin; 2007. [Google Scholar]
- 23.Nakaya N, Tsubono Y, Hosokawa T, et al. Personality and the risk of cancer. J Natl Cancer Inst. 2003;95(11):799–805. doi: 10.1093/jnci/95.11.799. [DOI] [PubMed] [Google Scholar]
- 24.Martin LR, Friedman HS, Schwartz JE. Personality and mortality risk across the life span: the importance of conscientiousness as a biopsychosocial attribute. Health Psychol. 2007;26(4):428–436. doi: 10.1037/0278-6133.26.4.428. [DOI] [PubMed] [Google Scholar]
- 25.Kivimäki M, Nyberg ST, Batty GD, et al. Job strain as a risk factor for coronary heart disease: a collaborative meta-analysis of individual participant data. Lancet. 2012;380(9852):1491–1497. doi: 10.1016/S0140-6736(12)60994-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hagger-Johnson G, Sabia S, Nabi H, et al. Low conscientiousness and risk of all-cause, cardiovascular and cancer mortality over 17 years: Whitehall II Cohort Study. J Psychosom Res. 2012;73(2):98–103. doi: 10.1016/j.jpsychores.2012.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lodi-Smith J, Jackson J, Bogg T, et al. Mechanisms of health: education and health-related behaviours partially mediate the relationship between conscientiousness and self-reported physical health. Psychol Health. 2010;25(3):305–319. doi: 10.1080/08870440902736964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hampson SE, Goldberg LR, Vogt TM, et al. Mechanisms by which childhood personality traits influence adult health status: educational attainment and healthy behaviors. Health Psychol. 2007;26(1):121–125. doi: 10.1037/0278-6133.26.1.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Roberts BW, Smith J, Jackson JJ, et al. Compensatory conscientiousness and health in older couples. Psychol Sci. 2009;20(5):553–559. doi: 10.1111/j.1467-9280.2009.02339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Goodwin RD, Friedman HS. Health status and the five-factor personality traits in a nationally representative sample. J Health Psychol. 2006;11(5):643–654. doi: 10.1177/1359105306066610. [DOI] [PubMed] [Google Scholar]
- 31.Wilson RS, Schneider JA, Arnold SE, et al. Conscientiousness and the incidence of Alzheimer disease and mild cognitive impairment. Arch Gen Psychiatry. 2007;64(10):1204–1212. doi: 10.1001/archpsyc.64.10.1204. [DOI] [PubMed] [Google Scholar]
- 32.O'Cleirigh C, Ironson G, Weiss A, et al. Conscientiousness predicts disease progression (CD4 number and viral load) in people living with HIV. Health Psychol. 2007;26(4):473–480. doi: 10.1037/0278-6133.26.4.473. [DOI] [PubMed] [Google Scholar]
- 33.Biondi M, Peronti M, Pacitti F, et al. Personality, endocrine and immune changes after eight months in healthy individuals under normal daily stress. Psychother Psychosom. 1994;62(3-4):176–184. doi: 10.1159/000288920. [DOI] [PubMed] [Google Scholar]
- 34.Distel MA, Trull TJ, Willemsen G, et al. The five-factor model of personality and borderline personality disorder: a genetic analysis of comorbidity. Biol Psychiatry. 2009;66(12):1131–1138. doi: 10.1016/j.biopsych.2009.07.017. [DOI] [PubMed] [Google Scholar]
- 35.Shavelle RM, Paculdo DR, Strauss DJ, et al. Smoking habit and mortality: a meta-analysis. J Insur Med. 2008;40(3-4):170–178. [PubMed] [Google Scholar]
- 36.Gellert C, Schottker B, Brenner H. Smoking and all-cause mortality in older people: systematic review and meta-analysis. Arch Intern Med. 2012;172(11):837–844. doi: 10.1001/archinternmed.2012.1397. [DOI] [PubMed] [Google Scholar]
- 37.Woodcock J, Franco OH, Orsini N, et al. Non-vigorous physical activity and all-cause mortality: systematic review and meta-analysis of cohort studies. Int J Epidemiol. 2011;40(1):121–138. doi: 10.1093/ije/dyq104. [DOI] [PubMed] [Google Scholar]
- 38.Loef M, Walach H. The combined effects of healthy lifestyle behaviors on all cause mortality: a systematic review and meta-analysis. Prev Med. 2012;55(3):163–170. doi: 10.1016/j.ypmed.2012.06.017. [DOI] [PubMed] [Google Scholar]
- 39.Baker DP, Leon J, Smith Greenaway EG, et al. The education effect on population health: a reassessment. Popul Dev Rev. 2011;37(2):307–332. doi: 10.1111/j.1728-4457.2011.00412.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cuijpers P, Smit F. Excess mortality in depression: a meta-analysis of community studies. J Affect Disord. 2002;72(3):227–236. doi: 10.1016/s0165-0327(01)00413-x. [DOI] [PubMed] [Google Scholar]
- 41.Piquero AR, Jennings WG, Farrington DP. Self-control interventions for children under age 10 for improving self-control and delinquency and problem behaviors: a systematic review. Campbell Syst Rev. 2010;2:1–117. [Google Scholar]
- 42.Reynolds AJ, Temple JA, Robertson DL, et al. Long-term effects of an early childhood intervention on educational achievement and juvenile arrest: a 15-year follow-up of low-income children in public schools. JAMA. 2001;285(18):2339–2346. doi: 10.1001/jama.285.18.2339. [DOI] [PubMed] [Google Scholar]
- 43.Russ TC, Stamatakis E, Hamer M, et al. Association between psychological distress and mortality: individual participant pooled analysis of 10 prospective cohort studies. BMJ. 2012;345:e4933. doi: 10.1136/bmj.e4933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ferguson E, Bibby PA. Openness to experience and all-cause mortality: a meta-analysis and r(equivalent) from risk ratios and odds ratios. Br J Health Psychol. 2012;17(1):85–102. doi: 10.1111/j.2044-8287.2011.02055.x. [DOI] [PubMed] [Google Scholar]
- 45.Lang FR, John D, Ludtke O, et al. Short assessment of the Big Five: robust across survey methods except telephone interviewing. Behav Res Methods. 2011;43(2):548–567. doi: 10.3758/s13428-011-0066-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rammstedt B, John OP. Measuring personality in one minute or less: a 10-item short version of the Big Five Inventory in English and German. J Res Pers. 2007;41(1):203–212. [Google Scholar]
- 47.Soto CJ, John OP. Ten facet scales for the Big Five Inventory: convergence with NEO PI-R facets, self-peer agreement, and discriminant validity. J Res Pers. 2009;43(1):84–90. [Google Scholar]
- 48.Hahn E, Gottschling J, Spinath FM. Short measurements of personality—validity and reliability of the GSOEP Big Five Inventory (BFI-S) J Res Pers. 2012;46(3):355–359. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Web Material