Dry Age-Related Macular Degeneration: Mechanisms, Therapeutic Targets, and Imaging (original) (raw)
Abstract
Age-related macular degeneration is the leading cause of irreversible visual dysfunction in individuals over 65 in Western Society. Patients with AMD are classified as having early stage disease (early AMD), in which visual function is affected, or late AMD (generally characterized as either “wet” neovascular AMD, “dry” atrophic AMD or both), in which central vision is severely compromised or lost. Until recently, there have been no therapies available to treat the disorder(s). Now, the most common wet form of late-stage AMD, choroidal neovascularization, generally responds to treatment with anti–vascular endothelial growth factor therapies. Nevertheless, there are no current therapies to restore lost vision in eyes with advanced atrophic AMD. Oral supplementation with the Age-Related Eye Disease Study (AREDS) or AREDS2 formulation (antioxidant vitamins C and E, lutein, zeaxanthin, and zinc) has been shown to reduce the risk of progression to advanced AMD, although the impact was in neovascular rather than atrophic AMD. Recent findings, however, have demonstrated several features of early AMD that are likely to be druggable targets for treatment. Studies have established that much of the genetic risk for AMD is associated with complement genes. Consequently, several complement-based therapeutic treatment approaches are being pursued. Potential treatment strategies against AMD deposit formation and protein and/or lipid deposition will be discussed, including anti-amyloid therapies. In addition, the role of autophagy in AMD and prevention of oxidative stress through modulation of the antioxidant system will be explored. Finally, the success of these new therapies in clinical trials and beyond relies on early detection, disease typing, and predicting disease progression, areas that are currently being rapidly transformed by improving imaging modalities and functional assays.
Keywords: drusen, complement, autophagy, functional imaging, therapeutic targets
Introduction
Age-related macular degeneration (AMD) is the leading cause of blindness in people 65 years of age or older in developed countries.1,2 Currently, patients with AMD are classified as having early AMD, intermediate, and late AMD based on the appearance of the macula.3 In early and intermediate AMD, drusen and pigmentary changes are visible and visual function is often affected. In late or advanced stage disease, neovascularization and/or atrophy are visible in the macula and central vision is more often severely compromised. Typical symptoms in late stage disease include decreased night vision and progressive loss of central vision. Loss of vision is attributed to macular drop out of RPE and photoreceptors (Fig. 1), termed geographic atrophy (GA); or from the invasion of RPE and/or retina by abnormal blood vessels, termed neovascular, exudative, or “wet” AMD as this involves choroidal neovascularization (CNV).4 In this review, we will focus on emerging therapeutic interventions in early AMD (Fig. 2A) and also GA (Fig. 2B), which accounts for 20% of legal blindness related to AMD and produces reduced visual function (e.g., reduced reading speed) due to ring-shaped vision loss sparing the center.5–7
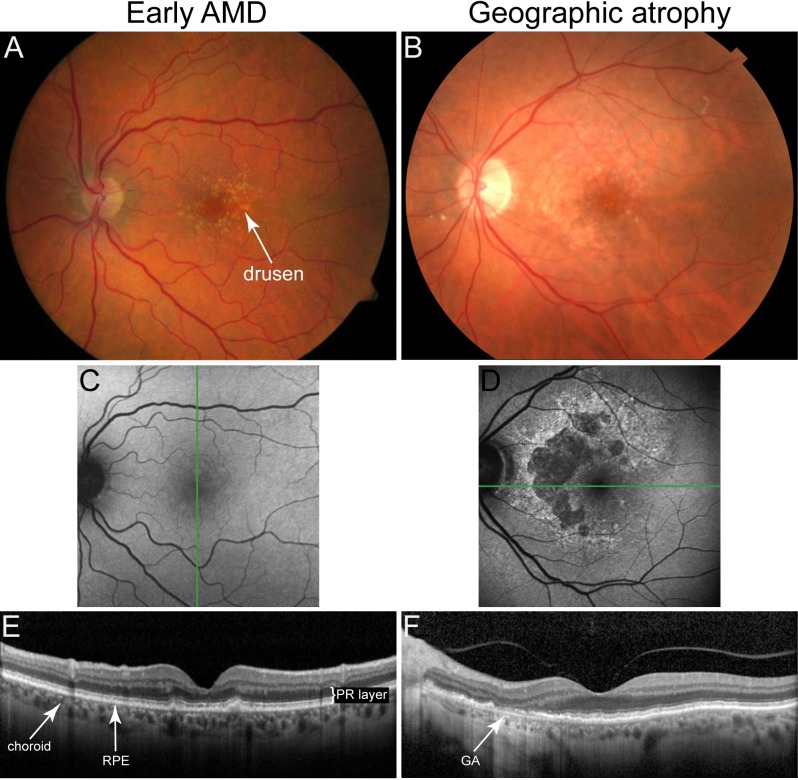
Figure 1.
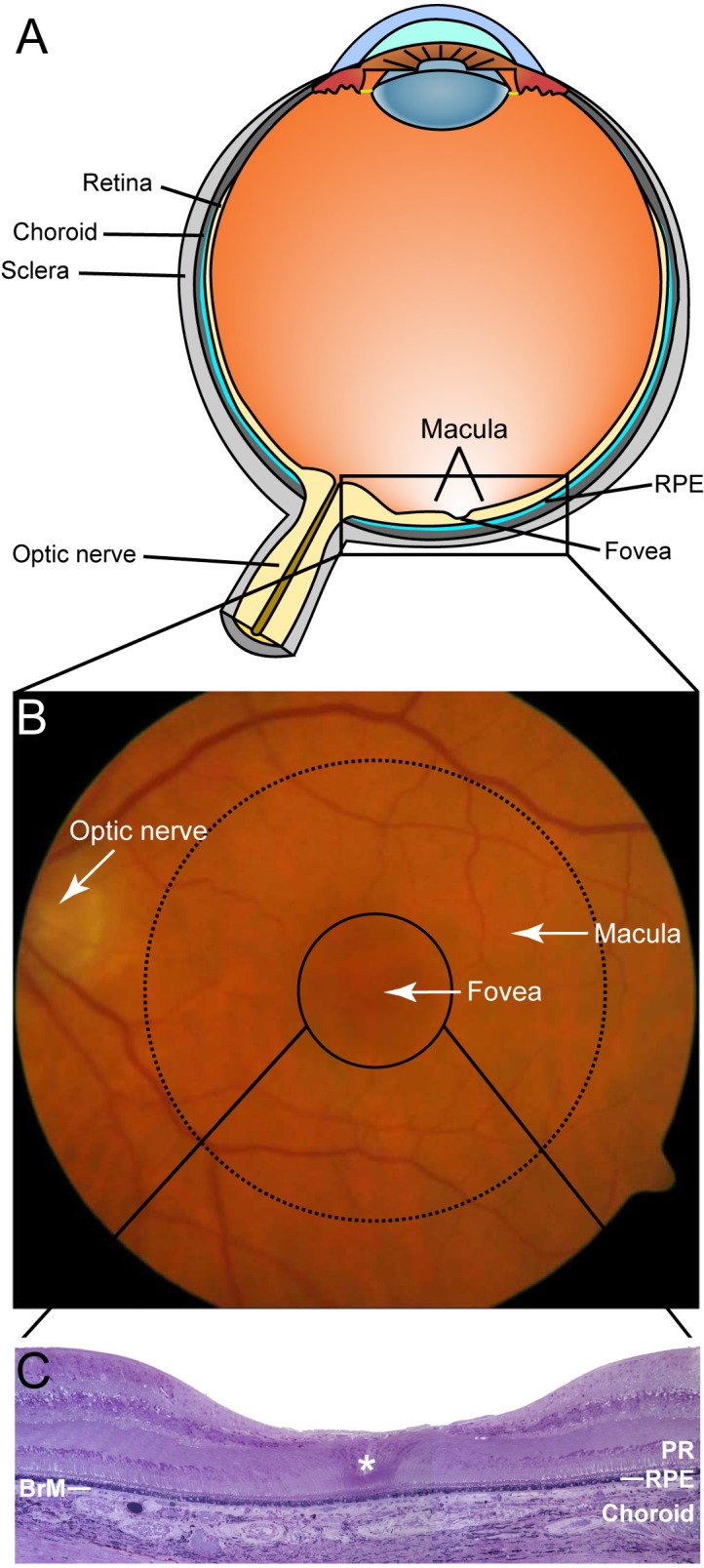
Ocular anatomy of a healthy eye relevant to AMD. (A) Cross-section schematic of a human eye showing major structures. (B) Color fundus photograph from an elderly patient covering the area indicated in (A) showing a healthy macula (dashed line, ø = ∼6 mm), healthy fovea (solid line, ø = ∼1.5–2 mm), and healthy optic nerve head (ø = ∼1.5–2 mm), respectively (photograph courtesy of Eleonora Lad). (C) Immunohistochemical cross-section of the foveal region indicated in (B), foveola (ø = 0.2–0.3 mm, indicated by *), which contains only cone photoreceptors and no rods, is located at the center of the foveal pit. Photoreceptor layer (PR), RPE, BrM, and choroid, are indicated (fovea image courtesy of Christine Curcio).
Figure 2.
Fundus photography, FAF, and SD-OCT images of early (A, C, E) and late cases (B, D, F) of dry AMD. Fundus photographs of early AMD (A) and GA (B) are not easily differentiated. However, in FAF images (C, D) the difference is striking. In SD-OCT B-scan images the RPE and PR layers can be delineated in early stage dry AMD (E) while these layers are missing in the area of GA (arrow in [F]). Spectral-domain OCT scans were acquired from the location indicated by the green lines on the FAF images (images courtesy of Eleonora Lad).
Progress in understanding CNV pathogenesis has led to development of several Food and Drug Administration (FDA)-approved therapies for wet AMD, including anti-VEGF agents, and emerging therapies targeting vessel maturation and remodeling versus angiogenesis.8–10 In contrast, the pathogenic mechanisms in GA are still unclear and there is no existing FDA-approved therapy. Presently, there is no treatment available to repair damaged RPE cells or photoreceptor cells. Thus, treatment approaches will likely be focused on early intervention that precedes RPE cell loss and in later stages, replacement with stem cell–derived RPE or photoreceptor cells.
Diagnosis of AMD is primarily achieved through various ocular-imaging techniques that have evolved considerably over the past few years and are facilitating development of evidence-based classification system for early forms of AMD as well as refining classification of late AMD.
Dry AMD Deposits
The pathogenesis of early AMD is characterized by thickening of Bruch membrane (BrM) due to lipid and protein accumulation that lead to formation of sub-RPE deposits that occur as discrete accumulations, called drusen, which can be hard or soft, or as continuous accumulations. The lipid build up is thought to primarily interfere with the fluid efflux from the RPE across BrM, thereby inflicting stress on the RPE.11 These and other stressors (e.g., oxidative stress from smoking and aging) result in an increased accumulation of lipofuscin in RPE cells, which in turn affect lysosome function and cholesterol metabolism.12 Cells under stress are known to increase the release of membranous vesicles such as exosomes and it is possible that this process is in part responsible for the deposits in the sub-RPE region.13–16 In addition, a number of proteins found in drusen are serum proteins, suggesting that impairments in fluid transport across BrM also might play a more direct role in drusen formation and deposition.17,18
Sub–retinal pigment epithelial deposits are classified as basal laminar deposits (BlamD) or basal linear deposits (BlinD). Basal laminar deposits consist of membranous material and wide- or long-spaced collagen between the plasma membrane and basal lamina of the RPE.11 Basal linear deposits consist of vesicular material located in the inner collagenous layer of BrM. Basal linear deposits (0.4–2 μm) and soft drusen (30–300 μm) are considered differently sized assemblies (layer and protrusion) of the same aggregate.11 Hard drusen (<63 μm) have higher apolipoprotein content than soft drusen and are much less fragile upon dissection.11,19–21
The composition of drusen has been investigated and described by a number of investigators,18,22–26 and are discussed in more detail below for their potential as targets for AMD therapies. The role of drusen in the pathogenesis of AMD has not been clarified, although it has long been known that they constitute hallmark lesions of AMD. Studies focused on delineating their components and origin have provided insights into pathways associated with early AMD,23 including the complement pathway and amyloid deposition discussed later.
As a result of the decreased flow of nutrients across BrM and the physical displacement caused by drusen, areas of hypopigmentation of the RPE monolayer on histologic tissue sections can be observed in the macula. Hyperpigmented areas are often located adjacent to hypopigmented regions, and have been proposed to be due to RPE cell proliferation as a response to RPE cell loss.27 On RPE flat mounts of AMD eyes the macular region contain many large and multinucleate cells (≥2 nuclei) as opposed to a healthy cell monolayer composed of mostly equally-sized mononucleate and a small proportion binucleate (∼3%) RPE cells.28–31 These areas of RPE cell heterogeneity may be due to RPE cell death and dropout. Ultimately, areas of confluent RPE cell loss can occur, which can be visualized by fundus autofluorescence (FAF) and SD-OCT, and are classified as GA (Fig. 2D, 2F).
Current Treatment Option: Age-Related Eye Disease Study Formulation
A number of studies in the 1980s and 1990s identified a link between antioxidant status, zinc levels, and risk of AMD.32–36 To further investigate these associations, the Age-Related Eye Disease Study (AREDS) was implemented. Results reported from the first AREDS (AREDS1) documented slowed progression to the late wet form of AMD when taking a formulation of beta-carotene, vitamin C, vitamin E, and zinc.37 However, the benefit of zinc in this formulation has been debated.38–41 A recent meta-analysis on the effect of zinc supplementation in prevention of AMD also concluded that available data are inconclusive.42 Recently, it has been shown that daily zinc supplements for 3 months in AMD patients lowered complement activation as measured by C3d/C3 ratio in serum, but this effect was only statistically significant in patients that already had high complement activation at the start of treatment.43 While intriguing, it is unknown whether this systemic zinc-mediated effect on complement activation also occurs in the eye and if so, how AMD progression is altered.
Based on data from earlier studies suggesting protective effects of lutein plus zeaxanthin and omega-3 fatty acids in AMD,35,44,45 these ingredients were added to the AREDS formulation in AREDS2 and the results of AREDS2 supplementation are discussed in a companion chapter in this supplement by Emily Chew. To date, the only treatment for dry AMD consists of daily intake of an AREDS formulation.
Drusen-Associated Proteins
As discussed above, drusen, BlamD, and BlinD constitute some of the clinical hallmarks of AMD.11 These deposits consist of proteins and lipids that are also found in plaques and deposits in other age-related degenerative disorders such as atherosclerosis,26 Alzheimer's disease,46,47 and a subset of Prion diseases,48,49 among others.50 The deposited proteins include vitronectin, clusterin (ApoJ), apolipoprotein E (ApoE), (serum) amyloid P (SAP), complement components, and amyloid-β (Aβ).18,51 The appearance of a small number of hard drusen (< 63-μm diameter) is a normal age-related change in the eye.20,52 However, soft “diffuse” drusen correlate with progression of AMD.53–55
It is not known if drusen are the primary cause for the degeneration of RPE in AMD, but they do ultimately affect RPE health due to impaired transport across BrM.11 Thus, elimination of these soft drusen present as an obvious therapeutic target to slow or inhibit AMD progression. The direct approach to target individual components of drusen has demonstrated some promise.12,56 Recently, we demonstrated that systemic treatment with an antibody against Aβ protects against RPE damage and vision loss in an AMD mouse model.29,57 Clearance of Aβ from sub-RPE deposits coincided with protection of visual function and structural preservation of the RPE, identifying Aβ as a druggable target. Another approach to remove Aβ from these deposits could be to induce higher expression of ApoE. Apolipoprotein E promotes proteolytic degradation of Aβ,58 and this effect is thought to be the mechanism for the enhanced Aβ clearance in the brain of some models of Aβ deposition,59 although this study is being revisited due to recently published conflicting data.60–64
Other constituents of drusen being targeted in preclinical and clinical trials include components of the complement system (e.g., C3 and C5).65 In addition, there are a number of drusen components that are potential drug targets that have not yet been pursued in treatment of AMD. Some obvious targets include vitronectin and clusterin, molecules involved in the acute-phase response to inflammation such as amyloid P component, and elements of lipid metabolism in addition to ApoE such as Apolipoprotein B, and peroxidized lipids.19,25,26,66–68
Complement Pathway in AMD
The identification of polymorphisms in genes coding for complement factor H (CFH),69–72 factor B,73 and C3,74 which confer greater “risk” for developing AMD, supported earlier pathobiologic investigations that led to the identification of numerous complement proteins in drusen.25,75,76 These studies implicated the complement system as an important biological pathway in development of AMD. The complement system is a component of our antigen-nonspecific defense mechanism or innate immunity and it consists of three pathways, classical, lectin, and alternative that all converge on C3.77
It is now apparent that dysregulation of the complement cascade, and of the alternative pathway in particular,78,79 is a critical predisposing step in AMD development. Although the precise triggering event(s) that provokes RPE–choroidal pathology are unknown, it is clear that a major consequence is the deposition and sequestration of cellular and acellular debris in the sub-RPE space that leads to drusen formation.
Complement activation products, produced as part of the inflammatory response, can have beneficial effects by facilitating phagocytosis and removal of cellular debris, or they can be detrimental by causing bystander damage to surrounding tissues. Currently, the bystander damage through complement dysregulation is suspected in AMD, where those patients lacking sufficient alternative pathway-modulating activity have subsequently sustained complement attack, bystander injury to neighboring cells, continued formation of drusen and other sub-RPE deposits, and eventually vision loss.65,79 This is supported by the ocular phenotype in CFH knock-out mice, generated to model factor H deficiency in humans,80 which revealed that old CFH knock-out animals exhibit an age-related decrease in visual acuity (VA) with evidence of C3 deposition.81
CFH, which is implicated as the strongest genetic risk factor for AMD,69–72 is an inhibitor of the alternative pathway of complement. Despite knowing for many years that CFH variants confer AMD risk, the underlying molecular mechanisms attributing to the risk factor activity of CFH remains unclear. CFH circulates at high concentrations in plasma but is also synthesized in the eye by the RPE,79 and the relative contribution of these sources of CFH to local complement regulation within sub-RPE deposits is not known. Recently, a study has shown that CFH may neutralize the pro-inflammatory effects of malondialdehyde (MDA)-induced inflammation in an AMD-risk associated manner.82 This study suggests that CFH also functions to attenuate oxidative stress insults leading to AMD, which may explain why clinical trials using complement inhibition-based treatment of AMD (targeting C3 or C5, e.g.) have produced disappointing outcome data that show minimal improvement in VA or reduction in disease progression.65
Oxidative Stress
The retina is particularly susceptible to oxidative stress because of its high consumption of oxygen, large amounts of polyunsaturated fatty acids concentrated in the photoreceptors, and continual exposure to visible light.83 Oxidative stress has long been hypothesized to play a substantive role in the development of AMD due to the high oxidative stress environment of the fundus. Oxidative stress in the retina is aggravated by lipofuscin, which accumulates in the RPE with age,84 especially in AMD eyes.85 Cigarette smoking, considered a strong oxidative stressor, remains the most consistent preventable risk factor for AMD across all studies86; considering these stressors, it is remarkable that most individuals maintain homeostasis throughout life. This is likely due to the presence of a range of efficient antioxidants and repair systems. For example, the macular pigment, formed by lutein and zeaxanthin, is a natural barrier protecting the central retina against oxidative damage believed to limit retinal oxidative damage by absorbing incoming blue light and/or quenching reactive oxygen species.
Antioxidants beyond vitamins and minerals (i.e., AREDS supplements, which have only been shown to be efficacious in the eye) are also being investigated as AMD therapies and may be effective by acting as neuroprotective agents, preventing toxicity in the retina as well as interfering with cell death pathways. Agents that augment the intrinsic antioxidant functions of the retina are promising candidates for the prevention and treatment of early AMD. These compounds exert their protective effects by modulating nuclear factor erythroid 2-related factor 2 (Nrf2), commonly involved in regulating the expression of genes encoding various antioxidant and antistress proteins.87,88
Autophagy
Autophagy is an essential lysosomal pathway that degrades cytoplasmic proteins and damaged organelles.89 This is especially important in highly metabolically active and highly phagocytic nondividing cells such as the RPE, which phagocytose photoreceptor outer-segment discs daily. As discussed above, RPE cells run a high risk of oxidative damage due to their exposure to high levels of lipid peroxidation products from photoreceptors, constant exposure to light stimuli, and their high oxygen utilization.90 There are three autophagic pathways (chaperone-mediated, micro-, and macroautophagy), of which macroautophagy is the primary route for transport of organelles and protein aggregates to the lysosome.91 The focus, for this review, will be on the macroautophagy pathway, which will be referred to as autophagy. Autophagy is initiated by the formation of the autophagosome, a double-membrane vesicle containing lipids, damaged organelles and/or cytoplasmic proteins. After their formation, autophagosomes undergo a strictly controlled fusion process with lysosomes where their contents are degraded by lysosomal enzymes.92
Autophagy pathways also have intracellular quality control functions, especially in the turnover of proteins that are prone to aggregation.93 It has been suggested that aggregate formation is prevented by autophagic degradation into oligomers and monomers.94 Thus, disturbances in autophagy in RPE cells may be a contributing factor in generation of protein aggregates seen in sub-RPE deposits and drusen in AMD.
During RPE cell aging, autophagic, and lysosomal degradation pathways lead to the accumulation of lysosomal lipofuscin, which is considered to contribute toward the pathogenesis of AMD.95,96 There is considerable evidence that lipofuscin and one of its major fluorophores, A2E, can increase lysosomal pH and reduce lysosomal degradation which, in turn, further reduce the functional capacity of the RPE and increase cellular stress97–100; thus, lipofuscin accumulation is a hallmark of RPE cell aging, which adversely affects the lysosomes' capacity to degrade proteins.97–100 Numerous studies have shown a strong association between lipofuscin accumulation and retinal degenerations such as AMD.95 Furthermore, as a form of protein quality control, protein aggregates are delivered to the lysosome by autophagy pathways.101,102 This might be one of the few ways to remove large, preformed aggregates from the cell. Thus, disturbances in lysosomal function by accumulated lipofuscin97,98 may increase the misfolding of intracellular proteins by reducing the efficiency of this clearance mechanism.92 Though the precise mechanisms by which the RPE becomes compromised by aging and in AMD has not been elucidated, a decrease in the removal and replacement of aggregated proteins and damaged intracellular organelles is likely to play a significant role.
It has recently been demonstrated that lysosomal activity decreases, and markers of autophagy accumulate in human AMD donor samples.16 In addition, as discussed in an earlier section, it is known that stressed RPE releases exosomes that are coated with complement and can bind CFH,15,16 suggesting that this may be a mechanism for sub-RPE deposit formation. Preservation of autophagic activity might be associated with a decrease of intracellular accumulation of damaged proteins, which may delay the RPE aging process.103,104 Conversely, autophagy may trigger cell death by excessive self-digestion.105 Thus, dysregulation of autophagy can result in cellular dysfunction. AMD has degenerative characteristics including protein deposits, and in certain cases, proliferative characteristics as occurs in wet AMD; thus, there is no consensus as to whether autophagy inhibitors or activators would be beneficial in AMD therapy, and how they should be used for different phenotypes of AMD.
A recently identified target for modulation of autophagy in RPE cells is the serine/threonine kinase mammalian target of rapamycin (mTOR) that regulates the damaging hypertrophy and dedifferentiation of RPE cells exposed to oxidative stress. Rapamycin-induced inhibition of mTOR can prevent these effects and preserve photoreceptor functions.106 However, rapamycin has a number of off-target effects, which have limited its practicality in age-related neurological disorders.107
Intraocular delivery of drugs could potentially circumvent a number of systemic side effects that would otherwise be an issue with many autophagy-modulating therapies. Gene therapy for treatment of AMD targeting autophagic pathways is also an interesting future option.108
Several environmental and genetic risk factors for AMD progression may be associated with lysosomal dysfunction, including buildup of sub-RPE deposits, drusen, lipofuscin, and chronic inflammation and likely lead to decreased autophagy flux in RPE cells. Thus, autophagy may represent an important therapeutic target in AMD.
Immune Cells in AMD Microglia
Microglia are resident immune cells in the central nervous system (CNS) and retina and constitute the main immune defense in CNS.109,110 They enter the retina during development and are activated by retinal injury and degeneration, transforming from quiescent stellate-shaped cells into large amoeboid-shaped cells. Activated microglia proliferate, migrate to areas of damage, degrade and clear debris, and secrete pro-inflammatory cytokines and chemokines.110 Long-term activation of microglia results in chronic neuroinflammation. Studies of AMD retinas suggest that widespread activation and migration of microglia does not occur during early stages of AMD. However, at intermediate to late stage dry AMD and GA, RPE and photoreceptor damage leads to accumulation of activated microglia at the site of macular injury suggesting that these may be relevant targets in late disease.111
Macrophages
Though AMD is not a classical inflammatory disease, increased numbers of macrophages have been detected in areas of BrM damage and RPE atrophy.112–116 Importantly, macrophages are also found in the choroid of healthy human eyes, but do not express the activation marker inducible nitric oxide synthase (iNOS). However, choroidal macrophages (as well as endothelial cells and pericytes) do express iNOS when they have been recruited to BrM in early AMD eyes with soft drusen or thick continuous BlamD. Macrophages recruited to active disciform scars also express iNOS.117
There are two subtypes of macrophages: the pro-inflammatory M1 macrophages, and the mostly anti-inflammatory M2 macrophages, whose main function is scavenging and tissue remodeling. M2 macrophages are thought to perform the beneficial, long-term housekeeping role of scavenging deposits such as degrading and removing drusen in early stages of the disease. M1 macrophages on the other hand, might incite and exacerbate the inflammatory responses to retinal injury.118 Interestingly, a recent study by Sene et al.119 found that altered cholesterol homeostasis due to decreased ABCA1 expression in aging macrophages promoted a switch from the M1 to the M2 phenotype. In the paradigm of CNV, the pro-angiogenic properties of M2 macrophages has been shown to promote progression of wet AMD.119 However, in the case of dry AMD, it is entirely unknown which of the two macrophage subtypes would be the most beneficial for degradation of drusen and prevention of RPE cell loss. Thus, the mechanisms of polarization of macrophages into M1 or M2 subtypes represent an interesting target for cellular intervention in different stages (early versus late) of dry AMD pathogenesis and warrants further investigation.
Modulation of the recruitment of microglia and macrophages to the site of injury is also a potential target for AMD treatment. Polymorphisms in the CX3CR1 chemokine receptor found on microglia and macrophages have been associated with increased risk of AMD.120,121 The CX3CR1 polymorphisms result in decreased affinity for its ligand (CX3CL1), which in turn negatively affects microglial and macrophage migration.122 In vitro studies suggest that accumulation of microglia due to impaired migration may cause direct damage to the photoreceptors.123 In the case of macrophages, impairments in migration may interfere with recruitment from the circulation into the choroid and BrM in order to clear deposits at the site of injury.121,122 Previous reports on mice lacking expression of both the chemokine, CCL2, and the receptor, CX3CR1, described a phenotype similar to that seen in human AMD.124 However, the intraretinal rather than subretinal lesions seen in this mouse model suggest that the phenotype is due to the rd8 mutation, which is now known to be present in the background mouse strain used in these studies.125–127 The rd8 mutation is a single nucleotide deletion in the Crb1 gene that can cause a distinct clinical ocular phenotype due to formation of retinal folds, pseudorosettes, as well as focal retinal dysplasia and degeneration.128
There are still many details about the roles of microglia and macrophages in the pathophysiology of dry AMD that are unknown. Consequently, further studies will be needed to clarify whether microglia and macrophages do indeed represent feasible druggable targets in AMD. Mast cells have also emerged as immune cells of the choroid that may play a role in AMD. Lutty and colleagues recently described an accumulation of degranulated mast cells around GA lesions in the choroid of human donor eyes, suggesting that mast cell degranulation may contribute to the damage of this tissue in GA (Lutty GA, et al. IOVS 2013;54:ARVO E-Abstract 3051). This is particularly intriguing since activated complement stimulates degranulation of mast cells. Other immune cells and targets, including the inflammasome, will not be discussed in this review as they were addressed at length in a recent review by Ambati et al.65
Cell-Based Therapies
A large body of evidence supports the concept that RPE cell loss precedes photoreceptor loss in AMD.12 Thus, it follows that if the RPE loss can be mitigated, visual function can most likely be maintained. A number of fetal and stem cell–based approaches to replenish the RPE in vivo have been attempted in the last 20 years, resulting in varying levels of reconstitution and/or visual function rescue in animal models.129,130 RPE cells are a highly polarized cell type and some studies suggest that for transplanted RPE cells to survive, they need to be polarized prior to transplantation.131 Therefore, subretinal implantation of polarized RPE cells on biocompatible supports was pursued, with some success.131–134 However, the major drawbacks using this approach are the traumatic implantation procedures and the possibility of rejection of the support/scaffold if it is not sufficiently immunologically inert.131
Recently, studies using an approach based on adult hematopoietic stem cells (HSC) showed promising results in restoring damaged RPE layers in vivo.135,136 The authors reprogrammed adult HSCs by lentiviral expression of RPE65, which drove these cells to develop into RPE-like cells. Furthermore, systemic delivery via intravenous injection resulted in homing of these cells to the subretinal space in a mouse model of sodium iodate–induced RPE damage.135 This is significant since, in a human clinical setting, intravenous injection provides higher safety and ease of use than subretinal delivery. In addition, the prospect that the patient's own HSCs could be used is particularly appealing as it avoids any issues related to transplant rejection. A logical next step will be to determine whether use of systemically delivered RPE-like cells will also home to the retina in a mouse model of early AMD in which there is more subtle RPE damage, and, hence, are likely to release less chemokines.137 Such a mouse model mimics the human disease more closely and a successful outcome may be a more relevant proof of concept for human trials in AMD. Unfortunately, there are no good animal models of GA but the current advances in RPE cell-based therapies suggest these cells could be ideal for saving, and potentially restoring vision in patients with GA.
The challenge of replacing lost photoreceptors is more daunting than replacing RPE as the transplanted cells not only have to develop normally, but they must also integrate into the damaged retina and, potentially most difficult, establish the nerve connections required to transmit the visual information to the brain. Recently, successful photoreceptor transplantation has been achieved in mice by harvesting rod precursor cells from healthy mouse retina to restore functional vision in a mouse model of stationary night blindness (alpha-transducin knock-out, _GNAT1_−/−).138 The authors showed, for the first time, that the transplanted rods acquired the proper morphology including a classical triad synapse, had properly integrated into retinal circuits, and that signals from these cells were transmitted to the visual cortex.138 In order for photoreceptor cell transplantation to be a viable therapy in humans, a source of cells other than photoreceptor precursors will be required. Progress to this end was made by a team led by Robin Ali that established that embryonic stem cells can provide a source of photoreceptors for retinal cell transplantation.139 Although the percentage of integrated rod photoreceptors was low this is an important milestone toward developing cell therapy for regenerating lost photoreceptors.
Techniques for Diagnosis and Prediction of Dry AMD Progression
Currently, clinicians monitor morphological changes in the retina/RPE/choroid by fundus exam, color fundus photography, FAF, OCT, and infrared (IR) reflectance. In the past two decades, OCT140 imaging technologies have had a profound impact on early detection, monitoring of progression, and treatment-efficacy evaluation of dry AMD. The current generation of commercialized OCT systems, SD-OCT, provides volumetric and cross-sectional views of the retina facilitating the visualization, measurement, monitoring, and phenotyping of the retinal layers and RPE,141–143 hyperreflective foci,144 GA,145,146 and drusen147 in eyes with dry AMD (Figs. 2E, 2F). While SD-OCT imaging is currently widely used in clinics as the standard of care for dry AMD diagnosis and prognosis, some emerging developments in OCT technology may lead to paradigm shifts in the way that dry AMD imaging is performed for research and clinical applications. One such technology is the polarization-sensitive OCT (PS-OCT) with tissue-selective imaging capabilities.148 In PS-OCT imaging, the RPE layer appears distinct from other tissue layers and thus PS-OCT may provide complimentary information about RPE health, drusen subtyping, and GA progression.149 In the next decade, advances in OCT technology are expected to continue to impact our understanding of dry AMD pathologies. Development of swept-source OCT (SS-OCT) systems with speeds exceeding 1,000,000 A-scans/s (as compared with the current generation of ∼30,000 A-scans/s commercial SD-OCT systems) will facilitate imaging and image analysis by reducing image acquisition time, noise, and motion artifacts.150 Moreover, SS-OCT systems are well suited to operate at approximately 1060-nm wavelength, which allows for enhanced visualization and monitoring of the choroidal structure, thickness, and vasculature pattern,151 as well as the inner retina's distinct retinal capillary beds.152
Indeed, other modern and classic, noninvasive, imaging systems such as en face color fundus photography153 and FAF, which may predict the rate of GA progression,154–157 provide important and complementary information to OCT about dry AMD.158 It has been proposed that the in vivo hyperfluorescence detected by FAF around GA lesions (Fig. 2D), represents dying RPE cells full of lipofuscin, which is the main source of FAF in these cells.154 Recently, however, Rudolf et al.159 published evidence against this hypothesis by measuring the histologic autofluorescence in human donor eyes with GA as a means to establish the cellular basis of the hyperfluorescence in these GA border zones. They found that the areas with highest histologic autofluorescence at GA borders were often associated with vertically superimposed RPE cells and, therefore, that the increased FAF was not necessarily a harbinger of cell death. Their data also suggests that lipofuscin itself may not be a relevant target for AMD treatment.159
Integration of adaptive optics (AO) into modern scanning laser ophthalmoscope (SLO) systems has made the in vivo visualization of individual photoreceptors (initially cones160–163 and very recently rods164) and RPE cells165 in dry AMD eyes possible (Fig. 3). On another front, while SS- and SD-OCT create images based mainly on the scattering properties of the tissue, a novel three dimensional (3-D) imaging technology called photoacoustic ophthalmoscopy (PAOM) provides complementary information by creating images based on the absorption properties of the tissue. Photoacoustic ophthalmoscopy, which may operate in multiple wavelengths (e.g., 532 nm and 1064 nm), is especially suitable for melanin-related imaging (e.g., RPE), choroid capillary network imaging, and for measuring oxygen saturation in retinal microvasculature.166
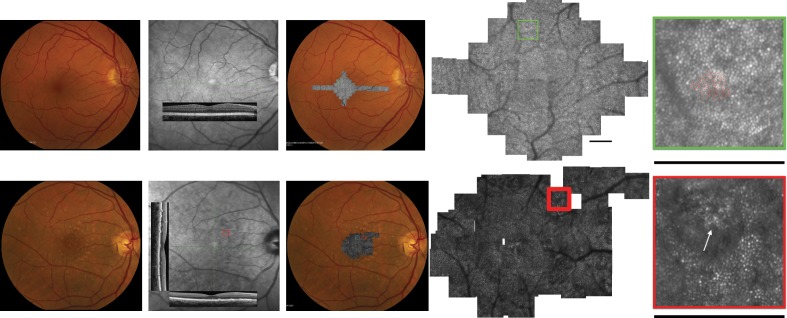
Figure 3.
Cone structures in a 61-year-old healthy subject (top panels) and a 64-year-old subject with dry AMD (bottom panels). The panels show (left to right) color fundus photos, infrared fundus photos with SD-OCT superimposed, color fundus photo with montage of AO-SLO images superimposed, AO-SLO image with a box highlighting a magnified AO-SLO image (far right panel). In the healthy subject, the far right panel shows red crosses where cones were quantified and cone spacing fell within normal limits for the eccentricity shown. In the AMD patient the red box includes a region over a druse, which can be seen on the SD-OCT. The highly magnified AO-SLO image shows coarse cones over the surface of the druse (arrow). Scale bars: 1° (figure courtesy of Jacque L. Duncan and her colleagues Katrina A. Woo, Shiri Zayit-Soudry, and Austin J. Roorda [Woo KA, et al. IOVS 2011;54:ARVO E-Abstract 1672]).
The large quantity of data created by these novel imaging technologies are often too large to be fully analyzed and interpreted manually. Thus, considerable work has been done in recent years to automate the segmentation of the imaging biomarkers of dry AMD. Due to the wide clinical applications of SD-OCT, most recent efforts have been focused on development of automatic segmentation algorithms to quantify individual retinal layer thicknesses, drusen, and GA in presence of dry AMD pathology (Fig. 4A).167–171 We have identified efficient quantitative imaging biomarkers to automatically distinguish intermediate AMD from healthy eyes by analyzing the topographic distribution of healthy and abnormal retinal layer thicknesses (Figs. 4B, 4C).147 On the laboratory science front, automated segmentation of RPE cells in confocal microscopy images of flat-mounted AMD mouse models yielding cell count and mean cell area measurements has drastically sped up the experiment and analysis time (Fig. 4D).172 Despite recent advances in automated segmentation of cones173–176 and rods173 in healthy eyes (Fig. 4E), lack of automated software is still one of the main obstacles in large-scale clinical utilization of adaptive optics scanning ophthalmoscope (AO-SLO) systems for diagnosis and prognosis of dry AMD. Moreover, regardless of the imaging modality or segmentation algorithm used, for many dry AMD patients with severe pathology (e.g., patients with cataracts which reduces the quality of captured images), automated image analysis methods fail to provide reliable measurements. Novel image enhancement methods have been demonstrated to significantly improve the quality of SD-OCT images of dry AMD patients,177,178 and may improve the performance of automated segmentation methods.
Figure 4.
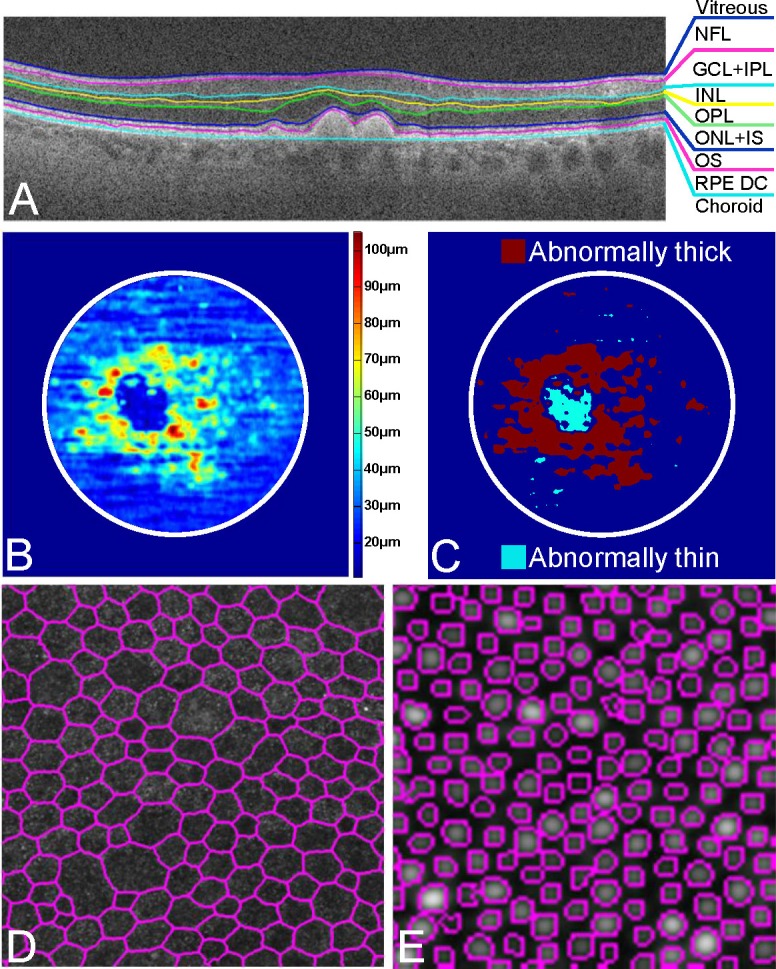
Application of novel automated segmentation algorithms for analysis of the anatomical and pathologic biomarkers of dry AMD. (A) Automated segmentation of the eight retinal boundaries on an SD-OCT image of a dry AMD patient with drusen using DOCTRAP software186 delineating the vitreous (at the top of the image) from the nerve fiber layer (NFL, blue line), NFL from ganglion cell layer and inner plexiform layer (GCL+IPL) complex (pink line), GCL+IPL from inner nuclear layer (INL, aqua line), INL from outer plexiform layer (OPL, yellow line), OPL from outer nuclear layer and inner segment (ONL+ IS) of the photoreceptor layer (green line), ONL+ IS from outer segments (OS) of the photoreceptor layer (blue line), OS from the RPE and drusen complex (RPE DC, pink line), and the RPE DC from the choroid (aqua line).169 The top and bottom boundaries correspond to the inner limiting membrane (ILM) and the Bruch membrane, respectively. (B) Example of a 5 mm in diameter RPE DC thickness map centered at the fovea from a dry AMD patient. Thickening around the fovea (red and yellow regions) is indicative of drusen, while thinning (blue regions) is representative of GA.147 (C) DOCTRAP software automatically extracts areas of abnormally thin (cyan region) and thick (red region) RPE DC from the thickness map in (B), which we use to automatically distinguish AMD from healthy eyes.147 (D) Automatically segmented confocal fluorescence image of the RPE cells in a flat-mounted APOE4 mouse retina.172 (E) Automatically segmented AO-SLO image of the cone photoreceptors in a healthy human subject.173
Functional Assessments of Vision in AMD
Functional changes in vision of AMD patients reflect early dysfunction of the neurosensory retina and the supporting RPE. These changes are assessed by a variety of methods including measuring VA at normal and low luminance and/or reading speed, and by using microperimetry, assaying dark adaptation and contrast sensitivity. As with fundus imaging, these tests of retinal function may also be confounded by media opacity such as progressive cataract.
One of the earliest complaints of patients with AMD is difficulty with vision under dark-adapted conditions and is in most cases due to a decrease of rod photoreceptor function.179,180 Thus, methods that could precisely distinguish the early changes in function are an obvious outcome measure for testing the efficacy of therapies targeting early AMD. To date, widespread use of a single method for functional testing has been hampered by the time to test a patient, the reproducibility of the test between instruments, testing methods, and patient visits. Measurements of dark adaptometry are underway in a longitudinal clinical trial of early and intermediate AMD (National Eye Institute, NCT01352975).181–184 Low luminance VA deficit, poorer foveal dark-adapted sensitivity, and reduced reading rate have all been shown to predict subsequent VA loss in eyes with atrophic AMD that started with good acuity.185 Contrast sensitivity changes in standard photopic lighting have been used for many years in assessment of AMD progression, especially to neovascularization; more recently mesopic testing has been explored.180 Recently, advances in microperimetry suggest greater utility in early AMD when nonphotopic testing is performed. Several methods to obtain non-photopic microperimetry have been proposed and larger scale studies are needed to evaluate these methods. To support future therapeutic studies, simplified tests that are reproducible and can be commonly used across centers for functional assessment will be important. Equally important will be assessing the relationship of these tests to the other systemic and ocular measures of disease.
Conclusions
In general terms, therapeutic approaches to GA should be aimed at (1) reducing or stopping the stimuli of continuing damage, which depends on continued progress in identifying and characterizing relevant targets; (2) protecting remaining cells from further damage; and (3) repairing, replacing, or regenerating damaged cells. Currently, the third approach is gaining traction with the advances in RPE and photoreceptor cell–based therapies described earlier. That being said, the first two areas are experiencing steady progress. Together, the current and continued advances in understanding the molecular pathogenesis of early AMD and GA, which are identifying relevant therapeutic targets, coupled with the advances in detecting and measuring disease progression, should expedite breakthroughs in developing therapies that block and/or reverse early AMD and GA. The new imaging, automated segmentation, and advances in visual function testing are directly impacting the great unmet need for devising therapeutic strategies for early AMD, which has been plagued by a lack of understanding of how to sub-classify types of early stage disease based on initial presentation and subtle changes over time. These new and evolving technologies are, for example, simplifying imaging and quantifying drusen (Figs. 4C, 4D) and should allow us to test whether changes in appearance of drusen (e.g., appearance and disappearance) can be correlated with vision effects and whether these are predictors of rates of progression. These advances will also have a large impact on the success of clinical trials as they will facilitate sub-stratification of early, intermediate and late AMD patients, by prediction of progression rates and appearance as well as refine quantifiable outcome measures of visual function changes and recovery. While there are many challenges and unmet needs in understanding and treating early and atrophic AMD this is an exciting time to be working in this area due to the convergence of advances in understanding retinal physiology, genetics, and technology.
Acknowledgments
The authors thank Michael Boulton, Scott Cousins, Jindong Ding, Glenn Jaffe, Eleonora Lad, Priyatham (Prithu) Mettu, and W. Daniel Stamer for their input and discussions that were instrumental to developing this chapter. They also thank and acknowledge the support of the Beckman Initiative for Macular Research in support of interdisciplinary discussion.
Supported by National Institutes of Health Grants EY019038 (CBR), P30 EY005722, and an Edward N. & Della L. Thome Memorial Foundation Award (CBR), Genentech Grant in support of AREDS2 Ancillary SDOCT Study (CAT).
Disclosure: C. Bowes Rickman, Pfizer (F); S. Farsiu, P; C.A. Toth, Genentech (F), Bioptigen (F), Physical Sciences, Inc. (F), P; M. Klingeborn, None
References
- 1.Klein R, Klein BE, Jensen SC, Meuer SM. The five-year incidence and progression of age-related maculopathy: the Beaver Dam Eye Study.Ophthalmology. 1997; 104: 7–21 [DOI] [PubMed] [Google Scholar]
- 2.Klein R, Cruickshanks KJ, Nash SD, et al. The prevalence of age-related macular degeneration and associated risk factors.Arch Ophthalmol. 2010; 128: 750–758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ferris FL III, Wilkinson CP, Bird A, et al. Clinical classification of age-related macular degeneration.Ophthalmology. 2013; 120: 844–851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bird AC. Therapeutic targets in age-related macular disease.J Clin Invest. 2010; 120: 3033–3041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Klein R, Klein BE, Franke T. The relationship of cardiovascular disease and its risk factors to age-related maculopathy. The Beaver Dam Eye Study.Ophthalmology. 1993; 100: 406–414 [DOI] [PubMed] [Google Scholar]
- 6.Vingerling JR, Dielemans I, Hofman A, et al. The prevalence of age-related maculopathy in the Rotterdam Study.Ophthalmology. 1995; 102: 205–210 [DOI] [PubMed] [Google Scholar]
- 7.Sunness JS, Rubin GS, Zuckerbrod A, Applegate CA. Foveal-sparing scotomas in advanced dry age-related macular degeneration.J Vis Impair Blind. 2008; 102: 600–610 [PMC free article] [PubMed] [Google Scholar]
- 8.Couch SM, Bakri SJ. Review of combination therapies for neovascular age-related macular degeneration.Semin Ophthalmol. 2011; 26: 114–120 [DOI] [PubMed] [Google Scholar]
- 9.Lally DR, Gerstenblith AT, Regillo CD. Preferred therapies for neovascular age-related macular degeneration.Curr Opin Ophthalmol. 2012; 23: 182–188 [DOI] [PubMed] [Google Scholar]
- 10.Jo N, Mailhos C, Ju M, et al. Inhibition of platelet-derived growth factor B signaling enhances the efficacy of anti-vascular endothelial growth factor therapy in multiple models of ocular neovascularization.Am J Pathol. 2006; 168: 2036–2053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Curcio CA, Johnson M.Structure, Function, and Pathology of Bruch's Membrane. London: Elsevier, Inc.; 2013. [Google Scholar]
- 12.Miller JW. Age-related macular degeneration revisited–piecing the puzzle: the LXIX Edward Jackson memorial lecture.Am J Ophthalmol. 2013; 155: 1–35 e13 [DOI] [PubMed] [Google Scholar]
- 13.King HW, Michael MZ, Gleadle JM. Hypoxic enhancement of exosome release by breast cancer cells.BMC Cancer. 2012; 12: 421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang AL, Lukas TJ, Yuan M, Du N, Handa JT, Neufeld AH. Changes in retinal pigment epithelium related to cigarette smoke: possible relevance to smoking as a risk factor for age-related macular degeneration.PLoS One. 2009; 4: e5304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang AL, Lukas TJ, Yuan M, Du N, Tso MO, Neufeld AH. Autophagy, exosomes and drusen formation in age-related macular degeneration.Autophagy. 2009; 5: 563–564 [DOI] [PubMed] [Google Scholar]
- 16.Wang AL, Lukas TJ, Yuan M, Du N, Tso MO, Neufeld AH. Autophagy and exosomes in the aged retinal pigment epithelium: possible relevance to drusen formation and age-related macular degeneration.PLoS One. 2009; 4: e4160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Johnson LV, Forest DL, Banna CD, et al. Cell culture model that mimics drusen formation and triggers complement activation associated with age-related macular degeneration.Proc Natl Acad Sci U S A. 2011; 108: 18277–18282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang L, Clark ME, Crossman DK, et al. Abundant lipid and protein components of drusen.PLoS One. 2010; 5: e10329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Curcio CA, Johnson M, Rudolf M, Huang JD. The oil spill in ageing Bruch membrane.Br J Ophthalmol. 2011; 95: 1638–1645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Munch IC, Sander B, Kessel L, et al. Heredity of small hard drusen in twins aged 20–46 years.Invest Ophthalmol Vis Sci. 2007; 48: 833–838 [DOI] [PubMed] [Google Scholar]
- 21.Rudolf M, Clark ME, Chimento MF, Li CM, Medeiros NE, Curcio CA. Prevalence and morphology of druse types in the macula and periphery of eyes with age-related maculopathy.Invest Ophthalmol Vis Sci. 2008; 49: 1200–1209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Crabb JW, Miyagi M, Gu X, et al. Drusen proteome analysis: an approach to the etiology of age-related macular degeneration.Proc Natl Acad Sci U S A. 2002; 99: 14682–14687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hageman GS, Luthert PJ, Victor Chong NH, Johnson LV, Anderson DH, Mullins RF. An integrated hypothesis that considers drusen as biomarkers of immune-mediated processes at the RPE-Bruch's membrane interface in aging and age-related macular degeneration.Progr Retin Eye Res. 2001; 20: 705–732 [DOI] [PubMed] [Google Scholar]
- 24.Hageman GS, Mullins RF. Molecular composition of drusen as related to substructural phenotype.Mol Vis. 1999; 5: 28 [PubMed] [Google Scholar]
- 25.Johnson LV, Ozaki S, Staples MK, Erickson PA, Anderson DH. A potential role for immune complex pathogenesis in drusen formation.Exp Eye Res. 2000; 70: 441–449 [DOI] [PubMed] [Google Scholar]
- 26.Mullins RF, Russell SR, Anderson DH, Hageman GS. Drusen associated with aging and age-related macular degeneration contain proteins common to extracellular deposits associated with atherosclerosis, elastosis, amyloidosis, and dense deposit disease.Faseb J. 2000; 14: 835–846 [PubMed] [Google Scholar]
- 27.de Jong PT. Age-related macular degeneration.New Engl J Med. 2006; 355: 1474–1485 [DOI] [PubMed] [Google Scholar]
- 28.Al-Hussaini H, Schneiders M, Lundh P, Jeffery G. Drusen are associated with local and distant disruptions to human retinal pigment epithelium cells.Exp Eye Res. 2009; 88: 610–612 [DOI] [PubMed] [Google Scholar]
- 29.Ding JD, Johnson LV, Herrmann R, et al. Anti-amyloid therapy protects against retinal pigmented epithelium damage and vision loss in a model of age-related macular degeneration.Proc Natl Acad Sci U S A. 2011; 108: E279–E287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Friedman E, Ts'o MO. The retinal pigment epithelium. II. Histologic changes associated with age.Arch Ophthalmol. 1968; 79: 315–320 [DOI] [PubMed] [Google Scholar]
- 31.Ts'o MO, Friedman E. The retinal pigment epithelium. I. Comparative histology.Arch Ophthalmol. 1967; 78: 641–649 [DOI] [PubMed] [Google Scholar]
- 32.Risk factors for neovascular age-related macular degeneration The Eye Disease Case-Control Study Group.Arch Ophthalmol. 1992; 110: 1701–1708 [DOI] [PubMed] [Google Scholar]
- 33.Antioxidant status and neovascular age-related macular degeneration Eye Disease Case-Control Study Group.Arch Ophthalmol. 1993; 111: 104–109 [DOI] [PubMed] [Google Scholar]
- 34.Goldberg J, Flowerdew G, Smith E, Brody JA, Tso MO. Factors associated with age-related macular degeneration. An analysis of data from the first National Health and Nutrition Examination Survey.Am J Epidemiol. 1988; 128: 700–710 [DOI] [PubMed] [Google Scholar]
- 35.Seddon JM, Ajani UA, Sperduto RD, et al. Dietary carotenoids, vitamins A, C, and E, and advanced age-related macular degeneration. Eye Disease Case-Control Study Group.Jama. 1994; 272: 1413–1420 [PubMed] [Google Scholar]
- 36.VandenLangenberg GM, Mares-Perlman JA, Klein R, Klein BE, Brady WE, Palta M. Associations between antioxidant and zinc intake and the 5-year incidence of early age-related maculopathy in the Beaver Dam Eye Study.Am J Epidemiol. 1998; 148: 204–214 [DOI] [PubMed] [Google Scholar]
- 37.Age-Related Eye Disease Research Group A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report no. 8.Arch Ophthalmol. 2001; 119: 1417–1436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ambati J, Ambati BK. Age-related eye disease study caveats.Arch Ophthalmol. 2002; 120: 997, author reply 997–999 [PubMed] [Google Scholar]
- 39.Ferris FL, Lindblad AS, Milton RC. Age-related eye disease study caveats [author reply].Arch Ophthalmol. 2002; 120: 997–999 [PubMed] [Google Scholar]
- 40.Jampol LM. Antioxidants, zinc, and age-related macular degeneration: results and recommendations.Arch Ophthalmol. 2001; 119: 1533–1534 [DOI] [PubMed] [Google Scholar]
- 41.Seigel D. AREDS investigators distort findings.Arch Ophthalmol. 2002; 120: 100–101 [DOI] [PubMed] [Google Scholar]
- 42.Vishwanathan R, Chung M, Johnson EJ. A systematic review on zinc for the prevention and treatment of age-related macular degeneration.Invest Ophthalmol Vis Sci. 2013; 54: 3985–3998 [DOI] [PubMed] [Google Scholar]
- 43.Klevering BJ. Zinc and the complement system. Antioxidants and AMD: into the mechanisms. Paper presented at: The Annual Meeting of the Association for Research in Vision and Ophthalmology; May 2013; Seattle, Washington. [Google Scholar]
- 44.Moeller SM, Parekh N, Tinker L, et al. Associations between intermediate age-related macular degeneration and lutein and zeaxanthin in the Carotenoids in Age-related Eye Disease Study (CAREDS): ancillary study of the Women's Health Initiative.Arch Ophthalmol. 2006; 124: 1151–1162 [DOI] [PubMed] [Google Scholar]
- 45.Tan JS, Wang JJ, Flood V, Rochtchina E, Smith W, Mitchell P. Dietary antioxidants and the long-term incidence of age-related macular degeneration: the Blue Mountains Eye Study.Ophthalmology. 2008; 115: 334–341 [DOI] [PubMed] [Google Scholar]
- 46.Armstrong RA. The molecular biology of senile plaques and neurofibrillary tangles in Alzheimer's disease.Folia Neuropathol. 2009; 47: 289–299 [PubMed] [Google Scholar]
- 47.Isas JM, Luibl V, Johnson LV, et al. Soluble and mature amyloid fibrils in drusen deposits.Invest Ophthalmol Vis Sci. 2010; 51: 1304–1310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ghetti B, Piccardo P, Frangione B, et al. Prion protein amyloidosis.Brain Pathol. 1996; 6: 127–145 [DOI] [PubMed] [Google Scholar]
- 49.Revesz T, Holton JL, Lashley T, et al. Genetics and molecular pathogenesis of sporadic and hereditary cerebral amyloid angiopathies.Acta Neuropathol. 2009; 118: 115–130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Armstrong RA, Lantos PL, Cairns NJ. What determines the molecular composition of abnormal protein aggregates in neurodegenerative disease?Neuropathology. 2008; 28: 351–365 [DOI] [PubMed] [Google Scholar]
- 51.Johnson LV, Leitner WP, Rivest AJ, Staples MK, Radeke MJ, Anderson DH. The Alzheimer's A beta-peptide is deposited at sites of complement activation in pathologic deposits associated with aging and age-related macular degeneration.Proc Natl Acad Sci U S A. 2002; 99: 11830–11835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bressler NM, Bressler SB, West SK, Fine SL, Taylor HR. The grading and prevalence of macular degeneration in Chesapeake Bay watermen.Arch Ophthalmol. 1989; 107: 847–852 [DOI] [PubMed] [Google Scholar]
- 53.Davis MD, Gangnon RE, Lee LY, et al. The Age-Related Eye Disease Study severity scale for age-related macular degeneration: AREDS Report No. 17.Arch Ophthalmol. 2005; 123: 1484–1498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ferris FL, Davis MD, Clemons TE, et al. A simplified severity scale for age-related macular degeneration: AREDS Report No. 18.Arch Ophthalmol. 2005; 123: 1570–1574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Klein R, Klein BE, Tomany SC, Meuer SM, Huang GH. Ten-year incidence and progression of age-related maculopathy: the Beaver Dam eye study.Ophthalmology. 2002; 109: 1767–1779 [DOI] [PubMed] [Google Scholar]
- 56.Landa G, Butovsky O, Shoshani J, Schwartz M, Pollack A. Weekly vaccination with Copaxone (glatiramer acetate) as a potential therapy for dry age-related macular degeneration.Curr Eye Res. 2008; 33: 1011–1013 [DOI] [PubMed] [Google Scholar]
- 57.Ding JD, Lin J, Mace BE, Herrmann R, Sullivan P, Bowes Rickman C. Targeting age-related macular degeneration with Alzheimer's disease based immunotherapies: anti-amyloid-beta antibody attenuates pathologies in an age-related macular degeneration mouse model.Vision Res. 2008; 48: 339–345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Jiang Q, Lee CY, Mandrekar S, et al. ApoE promotes the proteolytic degradation of Abeta.Neuron. 2008; 58: 681–693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cramer PE, Cirrito JR, Wesson DW, et al. ApoE-directed therapeutics rapidly clear beta-amyloid and reverse deficits in AD mouse models.Science. 2012; 335: 1503–1506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Fitz NF, Cronican AA, Lefterov I, Koldamova R. Comment on “ApoE-directed therapeutics rapidly clear beta-amyloid and reverse deficits in AD mouse models.”Science. 2013; 340: 924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Landreth GE, Cramer PE, Lakner MM, et al. Response to comments on “ApoE-directed therapeutics rapidly clear beta-amyloid and reverse deficits in AD mouse models.”Science. 2013; 340: 924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Price AR, Xu G, Siemienski ZB, et al. Comment on “ApoE-directed therapeutics rapidly clear beta-amyloid and reverse deficits in AD mouse models.”Science. 2013; 340: 924 [DOI] [PubMed] [Google Scholar]
- 63.Tesseur I, Lo AC, Roberfroid A, et al. Comment on “ApoE-directed therapeutics rapidly clear beta-amyloid and reverse deficits in AD mouse models.”Science. 2013; 340: 924 [DOI] [PubMed] [Google Scholar]
- 64.Veeraraghavalu K, Zhang C, Miller S, et al. Comment on “ApoE-directed therapeutics rapidly clear beta-amyloid and reverse deficits in AD mouse models.”Science. 2013; 340: 924 [DOI] [PubMed] [Google Scholar]
- 65.Ambati J, Atkinson JP, Gelfand BD. Immunology of age-related macular degeneration.Nat Rev Immunol. 2013; 13: 438–451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hageman GS, Mullins RF, Russell SR, Johnson LV, Anderson DH. Vitronectin is a constituent of ocular drusen and the vitronectin gene is expressed in human retinal pigmented epithelial cells.Faseb J. 1999; 13: 477–484 [DOI] [PubMed] [Google Scholar]
- 67.Sakaguchi H, Miyagi M, Shadrach KG, Rayborn ME, Crabb JW, Hollyfield JG. Clusterin is present in drusen in age-related macular degeneration.Exp Eye Res. 2002; 74: 547–549 [DOI] [PubMed] [Google Scholar]
- 68.Spaide RF, Ho-Spaide WC, Browne RW, Armstrong D. Characterization of peroxidized lipids in Bruch's membrane.Retina. 1999; 19: 141–147 [DOI] [PubMed] [Google Scholar]
- 69.Edwards AO, Ritter R, III, , Abel KJ, Manning A, Panhuysen C, Farrer LA. Complement factor H polymorphism and age-related macular degeneration.Science. 2005; 308: 421–424 [DOI] [PubMed] [Google Scholar]
- 70.Hageman GS, Anderson DH, Johnson LV, et al. A common haplotype in the complement regulatory gene factor H (HF1/CFH) predisposes individuals to age-related macular degeneration.Proc Natl Acad Sci U S A. 2005; 102: 7227–7232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Haines JL, Hauser MA, Schmidt S, et al. Complement factor H variant increases the risk of age-related macular degeneration.Science. 2005; 308: 419–421 [DOI] [PubMed] [Google Scholar]
- 72.Klein RJ, Zeiss C, Chew EY, et al. Complement factor H polymorphism in age-related macular degeneration.Science. 2005; 308: 385–389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gold B, Merriam JE, Zernant J, et al. Variation in factor B (BF) and complement component 2 (C2) genes is associated with age-related macular degeneration.Nat Genet. 2006; 38: 458–462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yates JR, Sepp T, Matharu BK, et al. Complement C3 variant and the risk of age-related macular degeneration.New Engl J Med. 2007; 357: 553–561 [DOI] [PubMed] [Google Scholar]
- 75.Anderson DH, Mullins RF, Hageman GS, Johnson LV. A role for local inflammation in the formation of drusen in the aging eye.Am J Ophthalmol. 2002; 134: 411–431 [DOI] [PubMed] [Google Scholar]
- 76.Johnson LV, Leitner WP, Staples MK, Anderson DH. Complement activation and inflammatory processes in drusen formation and age-related macular degeneration.Exp Eye Res. 2001; 73: 887–896 [DOI] [PubMed] [Google Scholar]
- 77.Thurman JM, Holers VM. The central role of the alternative complement pathway in human disease.J Immunol. 2006; 176: 1305–1310 [DOI] [PubMed] [Google Scholar]
- 78.Anderson DH, Ozaki S, Nealon M, et al. Local cellular sources of apolipoprotein E in the human retina and retinal pigmented epithelium: implications for the process of drusen formation.Am J Ophthalmol. 2001; 131: 767–781 [DOI] [PubMed] [Google Scholar]
- 79.Anderson DH, Radeke MJ, Gallo NB, et al. The pivotal role of the complement system in aging and age-related macular degeneration: hypothesis re-visited.Prog Retin Eye Res. 2010; 29: 95–112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Pickering MC, Cook HT, Warren J, et al. Uncontrolled C3 activation causes membranoproliferative glomerulonephritis in mice deficient in complement factor H.Nat Genet. 2002; 31: 424–428 [DOI] [PubMed] [Google Scholar]
- 81.Coffey PJ, Gias C, McDermott CJ, et al. Complement factor H deficiency in aged mice causes retinal abnormalities and visual dysfunction.Proc Natl Acad Sci U S A. 2007; 104: 16651–16656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Weismann D, Hartvigsen K, Lauer N, et al. Complement factor H binds malondialdehyde epitopes and protects from oxidative stress.Nature. 2011; 478: 76–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Beatty S, Koh H, Phil M, Henson D, Boulton M. The role of oxidative stress in the pathogenesis of age-related macular degeneration.Surv Ophthalmol. 2000; 45: 115–134 [DOI] [PubMed] [Google Scholar]
- 84.Feeney-Burns L, Hilderbrand ES, Eldridge S. Aging human RPE: morphometric analysis of macular, equatorial, and peripheral cells.Invest Ophthalmol Vis Sci. 1984; 25: 195–200 [PubMed] [Google Scholar]
- 85.Dorey K, Staurenghi G, Delori FC. Lipofuscin in aged and AMD eyes. In: Hollyfield JG, RE Anderson, LaVail MM. eds_Retinal Degeneration_. New York, NY: Plenum Press; 1993: 3–14 [Google Scholar]
- 86.Tomany SC, Wang JJ, Van Leeuwen R, et al. Risk factors for incident age-related macular degeneration: pooled findings from 3 continents.Ophthalmology. 2004; 111: 1280–1287 [DOI] [PubMed] [Google Scholar]
- 87.Cano M, Thimmalappula R, Fujihara M, et al. Cigarette smoking, oxidative stress, the anti-oxidant response through Nrf2 signaling, and age-related macular degeneration.Vision Res. 2010; 50: 652–664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Handa JT. How does the macula protect itself from oxidative stress?Mol Aspects Med. 2012; 33: 418–435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Eskelinen EL. New insights into the mechanisms of macroautophagy in mammalian cells.Int Rev Cell Mol Biol. 2008; 266: 207–247 [DOI] [PubMed] [Google Scholar]
- 90.Jarrett SG, Boulton ME. Consequences of oxidative stress in age-related macular degeneration.Mol Aspects Med. 2012; 33: 399–417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Klionsky DJ, Cuervo AM, Dunn WA, Jr, , Levine B, van der Klei I, Seglen PO. How shall I eat thee?Autophagy. 2007; 3: 413–416 [DOI] [PubMed] [Google Scholar]
- 92.Kaarniranta K, Sinha D, Blasiak J, et al. Autophagy and heterophagy dysregulation leads to retinal pigment epithelium dysfunction and development of age-related macular degeneration.Autophagy. 2013; 9: 973–984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Gestwicki JE, Garza D. Protein quality control in neurodegenerative disease.Progr Mol Biol Transl Sci. 2012; 107: 327–353 [DOI] [PubMed] [Google Scholar]
- 94.Klionsky DJ. Neurodegeneration: good riddance to bad rubbish.Nature. 2006; 441: 819–820 [DOI] [PubMed] [Google Scholar]
- 95.Boulton M. Lipofuscin of the RPE. In: Lois N, Forrester JV. eds_Fundus Autofluorescence_. Philadelphia, PA: Wolters Kluwer/Lippincott Williams and Wilkins; 2009: 14–26 [Google Scholar]
- 96.Sparrow JR, Boulton M. RPE lipofuscin and its role in retinal pathobiology.Exp Eye Res. 2005; 80: 595–606 [DOI] [PubMed] [Google Scholar]
- 97.Bergmann M, Schutt F, Holz FG, Kopitz J. Inhibition of the ATP-driven proton pump in RPE lysosomes by the major lipofuscin fluorophore A2-E may contribute to the pathogenesis of age-related macular degeneration.FASEB J. 2004; 18: 562–564 [DOI] [PubMed] [Google Scholar]
- 98.Finnemann SC, Leung LW, Rodriguez-Boulan E. The lipofuscin component A2E selectively inhibits phagolysosomal degradation of photoreceptor phospholipid by the retinal pigment epithelium.Proc Natl Acad Sci U S A. 2002; 99: 3842–3847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Kaemmerer E, Schutt F, Krohne TU, Holz FG, Kopitz J. Effects of lipid peroxidation-related protein modifications on RPE lysosomal functions and POS phagocytosis.Invest Ophthalmol Vis Sci. 2007; 48: 1342–1347 [DOI] [PubMed] [Google Scholar]
- 100.Liu J, Lu W, Reigada D, Nguyen J, Laties AM, Mitchell CH. Restoration of lysosomal pH in RPE cells from cultured human and ABCA4(-/-) mice: pharmacologic approaches and functional recovery.Invest Ophthalmol Vis Sci. 2008; 49: 772–780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Ravikumar B, Duden R, Rubinsztein DC. Aggregate-prone proteins with polyglutamine and polyalanine expansions are degraded by autophagy.Hum Mol Genet. 2002; 11: 1107–1117 [DOI] [PubMed] [Google Scholar]
- 102.Waelter S, Boeddrich A, Lurz R, et al. Accumulation of mutant huntingtin fragments in aggresome-like inclusion bodies as a result of insufficient protein degradation.Mol Biol Cell. 2001; 12: 1393–1407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ryhanen T, Mannermaa E, Oksala N, et al. Radicicol but not geldanamycin evokes oxidative stress response and efflux protein inhibition in ARPE-19 human retinal pigment epithelial cells.Eur J Pharmacol. 2008; 584: 229–236 [DOI] [PubMed] [Google Scholar]
- 104.Salminen A, Kaarniranta K. Regulation of the aging process by autophagy.Trends Mol Med. 2009; 15: 217–224 [DOI] [PubMed] [Google Scholar]
- 105.Alers S, Loffler AS, Wesselborg S, Stork B. Role of AMPK-mTOR-Ulk1/2 in the regulation of autophagy: cross talk, shortcuts, and feedbacks.Mol Cell Biol. 2012; 32: 2–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Zhao C, Yasumura D, Li X, et al. mTOR-mediated dedifferentiation of the retinal pigment epithelium initiates photoreceptor degeneration in mice.J Clin Invest. 2011; 121: 369–383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Maiese K, Chong ZZ, Shang YC, Wang S. mTOR: on target for novel therapeutic strategies in the nervous system.Trends Mol Med. 2013; 19: 51–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Pastore N, Blomenkamp K, Annunziata F, et al. Gene transfer of master autophagy regulator TFEB results in clearance of toxic protein and correction of hepatic disease in alpha-1-anti-trypsin deficiency.EMBO Mol Med. 2013; 5: 397–412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Hanisch UK, Kettenmann H. Microglia: active sensor and versatile effector cells in the normal and pathologic brain.Nat Neurosci. 2007; 10: 1387–1394 [DOI] [PubMed] [Google Scholar]
- 110.Langmann T. Microglia activation in retinal degeneration.J Leukoc Biol. 2007; 81: 1345–1351 [DOI] [PubMed] [Google Scholar]
- 111.Gupta N, Brown KE, Milam AH. Activated microglia in human retinitis pigmentosa, late-onset retinal degeneration, and age-related macular degeneration.Exp Eye Res. 2003; 76: 463–471 [DOI] [PubMed] [Google Scholar]
- 112.Buschini E, Piras A, Nuzzi R, Vercelli A. Age-related macular degeneration and drusen: neuroinflammation in the retina.Prog Neurobiol. 2011; 95: 14–25 [DOI] [PubMed] [Google Scholar]
- 113.Cousins SW, Espinosa-Heidmann DG, Csaky KG. Monocyte activation in patients with age-related macular degeneration: a biomarker of risk for choroidal neovascularization?Arch Ophthalmol. 2004; 122: 1013–1018 [DOI] [PubMed] [Google Scholar]
- 114.Dastgheib K, Green WR. Granulomatous reaction to Bruch's membrane in age-related macular degeneration.Arch Ophthalmol. 1994; 112: 813–818 [DOI] [PubMed] [Google Scholar]
- 115.Green WR. Histopathology of age-related macular degeneration.Mol Vis. 1999; 5: 27 [PubMed] [Google Scholar]
- 116.Grossniklaus HE, Ling JX, Wallace TM, et al. Macrophage and retinal pigment epithelium expression of angiogenic cytokines in choroidal neovascularization.Mol Vis. 2002; 8: 119–126 [PubMed] [Google Scholar]
- 117.Cherepanoff S, McMenamin P, Gillies MC, Kettle E, Sarks SH. Bruch's membrane and choroidal macrophages in early and advanced age-related macular degeneration.Br J Ophthalmol. 2010; 94: 918–925 [DOI] [PubMed] [Google Scholar]
- 118.Mettu PS, Wielgus AR, Ong SS, Cousins SW. Retinal pigment epithelium response to oxidant injury in the pathogenesis of early age-related macular degeneration.Mol Aspects Med. 2012; 33: 376–398 [DOI] [PubMed] [Google Scholar]
- 119.Sene A, Khan AA, Cox D, et al. Impaired cholesterol efflux in senescent macrophages promotes age-related macular degeneration.Cell Metab. 2013; 17: 549–561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Chan CC, Tuo J, Bojanowski CM, Csaky KG, Green WR. Detection of CX3CR1 single nucleotide polymorphism and expression on archived eyes with age-related macular degeneration.Histol Histopathol. 2005; 20: 857–863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Tuo J, Smith BC, Bojanowski CM, et al. The involvement of sequence variation and expression of CX3CR1 in the pathogenesis of age-related macular degeneration.Faseb J. 2004; 18: 1297–1299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Combadiere C, Feumi C, Raoul W, et al. CX3CR1-dependent subretinal microglia cell accumulation is associated with cardinal features of age-related macular degeneration.J Clin Invest. 2007; 117: 2920–2928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Roque RS, Rosales AA, Jingjing L, Agarwal N, Al-Ubaidi MR. Retina-derived microglial cells induce photoreceptor cell death in vitro.Brain Res. 1999; 836: 110–119 [DOI] [PubMed] [Google Scholar]
- 124.Tuo J, Bojanowski CM, Zhou M, et al. Murine ccl2/cx3cr1 deficiency results in retinal lesions mimicking human age-related macular degeneration.Invest Ophthalmol Vis Sci. 2007; 48: 3827–3836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Luhmann UF, Carvalho LS, Robbie SJ, et al. Ccl2, Cx3cr1 and Ccl2/Cx3cr1 chemokine deficiencies are not sufficient to cause age-related retinal degeneration.Exp Eye Res. 2013; 107: 80–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Mattapallil MJ, Wawrousek EF, Chan CC, et al. The Rd8 mutation of the Crb1 gene is present in vendor lines of C57BL/6N mice and embryonic stem cells, and confounds ocular induced mutant phenotypes.Invest Ophthalmol Vis Sci. 2012; 53: 2921–2927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Vessey KA, Greferath U, Jobling AI, et al. Ccl2/Cx3cr1 knockout mice have inner retinal dysfunction but are not an accelerated model of AMD.Invest Ophthalmol Vis Sci. 2012; 53: 7833–7846 [DOI] [PubMed] [Google Scholar]
- 128.Chang B, Hawes NL, Hurd RE, Davisson MT, Nusinowitz S, Heckenlively JR. Retinal degeneration mutants in the mouse.Vision Res. 2002; 42: 517–525 [DOI] [PubMed] [Google Scholar]
- 129.Algvere PV, Berglin L, Gouras P, Sheng Y. Transplantation of fetal retinal pigment epithelium in age-related macular degeneration with subfoveal neovascularization.Graefes Arch Clin Exp Ophthalmol. 1994; 232: 707–716 [DOI] [PubMed] [Google Scholar]
- 130.Du H, Lim SL, Grob S, Zhang K. Induced pluripotent stem cell therapies for geographic atrophy of age-related macular degeneration.Semin Ophthalmol. 2011; 26: 216–224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Binder S, Stanzel BV, Krebs I, Glittenberg C. Transplantation of the RPE in AMD.Prog Retin Eye Res. 2007; 26: 516–554 [DOI] [PubMed] [Google Scholar]
- 132.Binder S. Scaffolds for retinal pigment epithelium (RPE) replacement therapy.Br J Ophthalmol. 2011; 95: 441–442 [DOI] [PubMed] [Google Scholar]
- 133.Hu Y, Liu L, Lu B, et al. A novel approach for subretinal implantation of ultrathin substrates containing stem cell-derived retinal pigment epithelium monolayer.Ophthalmic Res. 2012; 48: 186–191 [DOI] [PubMed] [Google Scholar]
- 134.Krishna Y, Sheridan C, Kent D, Kearns V, Grierson I, Williams R. Expanded polytetrafluoroethylene as a substrate for retinal pigment epithelial cell growth and transplantation in age-related macular degeneration.Br J Ophthalmol. 2011; 95: 569–573 [DOI] [PubMed] [Google Scholar]
- 135.Atmaca-Sonmez P, Li Y, Yamauchi Y, et al. Systemically transferred hematopoietic stem cells home to the subretinal space and express RPE-65 in a mouse model of retinal pigment epithelium damage.Exp Eye Res. 2006; 83: 1295–1302 [DOI] [PubMed] [Google Scholar]
- 136.Sengupta N, Caballero S, Sullivan SM, et al. Regulation of adult hematopoietic stem cells fate for enhanced tissue-specific repair.Mol Ther. 2009; 17: 1594–1604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Li Y, Reca RG, Atmaca-Sonmez P, et al. Retinal pigment epithelium damage enhances expression of chemoattractants and migration of bone marrow-derived stem cells.Invest Ophthalmol Vis Sci. 2006; 47: 1646–1652 [DOI] [PubMed] [Google Scholar]
- 138.Pearson RA, Barber AC, Rizzi M, et al. Restoration of vision after transplantation of photoreceptors.Nature. 2012; 485: 99–103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Gonzalez-Cordero A, West EL, Pearson RA, et al. Photoreceptor precursors derived from three-dimensional embryonic stem cell cultures integrate and mature within adult degenerate retina.Nat Biotechnol. 2013; 31: 741–747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Huang D, Swanson EA, Lin CP, et al. Optical coherence tomography.Science. 1991; 254: 1178–1181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Schuman SG, Koreishi AF, Farsiu S, Jung SH, Izatt JA, Toth CA. Photoreceptor layer thinning over drusen in eyes with age-related macular degeneration imaged in vivo with spectral-domain optical coherence tomography.Ophthalmology. 2009; 116: 488–496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Landa G, Su E, Garcia PMT, Seiple WH, Rosen RB. Inner segment–outer segment junctional layer integrity and corresponding retinal sensitivity in dry and wet forms of age-related macular degeneration.Retina. 2011; 31: 364–370 [DOI] [PubMed] [Google Scholar]
- 143.Leuschen JN, Schuman SG, Winter KP, et al. Spectral-domain optical coherence tomography characteristics of intermediate age-related macular degeneration.Ophthalmology. 2013; 120: 140–150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Christenbury JG, Folgar FA, O'Connell RV, Chiu SJ, Farsiu S, Toth CA. Progression of intermediate age-related macular degeneration with proliferation and inner retinal migration of hyperreflective foci.Ophthalmology. 2013; 120: 1038–1045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Yehoshua Z, Rosenfeld PJ, Gregori G, et al. Progression of geographic atrophy in age-related macular degeneration imaged with spectral domain optical coherence tomography.Ophthalmology. 2011; 118: 679–686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Brar M, Kozak I, Cheng L, et al. Correlation between spectral-domain optical coherence tomography and fundus autofluorescence at the margins of geographic atrophy.Am J Ophthalmol. 2009; 148: 439–444.e431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Farsiu S, Chiu SJ, O'Connell RV, et al. Quantitative classification of eyes with and without intermediate age-related macular degeneration using optical coherence tomography.Ophthalmology. In press [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Zotter S, Pircher M, Torzicky T, et al. Large-field high-speed polarization sensitive spectral domain OCT and its applications in ophthalmology.Biomed Opt Express. 2012; 3: 2720–2732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Ahlers C, Götzinger E, Pircher M, et al. Imaging of the retinal pigment epithelium in age-related macular degeneration using polarization-sensitive optical coherence tomography.Invest Ophthalmol Vis Sci. 2010; 51: 2149–2157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Klein T, André R, Wieser W, Pfeiffer T, Huber R. Joint aperture detection for speckle reduction and increased collection efficiency in ophthalmic MHz OCT.Biomed Opt Express. 2013; 4: 619–634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Motaghiannezam R, Schwartz DM, Fraser SE. In vivo human choroidal vascular pattern visualization using high-speed swept-source optical coherence tomography at 1060 nm.Invest Ophthalmol Vis Sci. 2012; 53: 2337–2348 [DOI] [PubMed] [Google Scholar]
- 152.Hendargo HC, Estrada R, Chiu SJ, Tomasi C, Farsiu S, Izatt JA. Automated non-rigid registration and mosaicing for robust imaging of distinct retinal capillary beds using speckle variance optical coherence tomography.Biomed Opt Express. 2013; 4: 803–821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Klein ML, Ferris FL, III, , Armstrong J, et al. Retinal precursors and the development of geographic atrophy in age-related macular degeneration.Ophthalmology. 2008; 115: 1026–1031 [DOI] [PubMed] [Google Scholar]
- 154.Holz FG, Bellman C, Staudt S, Schutt F, Völcker HE. Fundus autofluorescence and development of geographic atrophy in age-related macular degeneration.Invest Ophthalmol Vis Sci. 2001; 42: 1051–1056 [PubMed] [Google Scholar]
- 155.Holz FG, Bellman C, Staudt S, Schütt F, Völcker HE. Fundus autofluorescence and development of geographic atrophy in age-related macular degeneration.Invest Ophthalmol Vis Sci. 2001; 42: 1051–1056 [PubMed] [Google Scholar]
- 156.Hwang JC, Chan JWK, Chang S, Smith RT. Predictive value of fundus autofluorescence for development of geographic atrophy in age-related macular degeneration.Invest Ophthalmol Vis Sci. 2006; 47: 2655–2661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Brader HS, Ying G-S, Martin ER, Maguire MG. New grading criteria allow for earlier detection of geographic atrophy in clinical trials.Invest Ophthalmol Vis Sci. 2011; 52: 9218–9225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Jain N, Farsiu S, Khanifar AA, et al. Quantitative comparison of drusen segmented on SD-OCT versus drusen delineated on color fundus photographs.Invest Ophthalmol Vis Sci. 2010; 51: 4875–4883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Rudolf M, Vogt SD, Curcio CA, et al. Histologic basis of variations in retinal pigment epithelium autofluorescence in eyes with geographic atrophy.Ophthalmology. 2013; 120: 821–828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Godara P, Dubis AM, Roorda A, Duncan JL, Carroll J. Adaptive optics retinal imaging: emerging clinical applications.Optom Vis Sci. 2010; 87: 930–941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Godara P, Siebe C, Rha J, Michaelides M, Carroll J. Assessing the photoreceptor mosaic over drusen using adaptive optics and spectral-domain optical coherence tomography.Ophthalmic Surg Lasers Imaging. 2010; 41: S104–S108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Boretsky A, Khan F, Burnett G, et al. In vivo imaging of photoreceptor disruption associated with age-related macular degeneration: a pilot study.Lasers Surg Med. 2012; 44: 603–610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Lombardo M, Serrao S, Devaney N, Parravano M, Lombardo G. Adaptive optics technology for high-resolution retinal imaging.Sensors. 2013; 13: 334–366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Dubra A, Sulai Y, Norris JL, et al. Noninvasive imaging of the human rod photoreceptor mosaic using a confocal adaptive optics scanning ophthalmoscope.Biomed Opt Express. 2011; 2: 1864–1876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Roorda A, Zhang Y, Duncan JL. High-resolution in vivo imaging of the RPE mosaic in eyes with retinal disease.Invest Ophthalmol Vis Sci. 2007; 48: 2297–2303 [DOI] [PubMed] [Google Scholar]
- 166.Li S, Yin H, Fang L. Group-sparse representation with dictionary learning for medical image denoising and fusion.IEEE Trans Biomed Eng. 2012; 59: 3450–3459 [DOI] [PubMed] [Google Scholar]
- 167.Zawadzki RJ, Fuller AR, Wiley DF, Hamann B, Choi SS, Werner JS. Adaptation of a support vector machine algorithm for segmentation and visualization of retinal structures in volumetric optical coherence tomography data sets.J Biomed Opt. 2007; 12: 041206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Cabrera DeBuc D. A review of algorithms for segmentation of retinal image data using optical coherence tomography. In: Ho P-G. ed_Image Segmentation_. Rijeka, Croatia: Intech; 2011: 15–54 Available at: http://www.intechopen.com/source/pdfs/15371/InTech-A_review_of_algorithms_for_segmentation_of_retinal_image_data_using_optical_coherence_tomography.pdf. Accessed July 1, 2013. [Google Scholar]
- 169.Chiu SJ, Izatt JA, O'Connell RV, Winter KP, Toth CA, Farsiu S. Validated automatic segmentation of AMD pathology including drusen and geographic atrophy in SD-OCT images.Invest Ophthalmol Vis Sci. 2012; 53: 53–61 [DOI] [PubMed] [Google Scholar]
- 170.Gregori G, Wang F, Rosenfeld PJ, et al. Spectral domain optical coherence tomography imaging of drusen in nonexudative age-related macular degeneration.Ophthalmology. 2011; 118: 1373–1379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Kajić V, Esmaeelpour M, Považay B, Marshall D, Rosin PL, Drexler W. Automated choroidal segmentation of 1060 nm OCT in healthy and pathologic eyes using a statistical model.Biomed Opt Express. 2012; 3: 86–103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Chiu SJ, Toth CA. Bowes Rickman C, Izatt JA, Farsiu S. Automatic segmentation of closed-contour features in ophthalmic images using graph theory and dynamic programming.Biomed Opt Express. 2012; 3: 1127–1140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Chiu SJ, Dubis AM, Cooper RF, et al. Validated automatic segmentation of photoreceptors in adaptive optics scanning ophthalmoscope images. Paper presented at: SPIE Photonics West, Ophthalmic Technologies XXIII; February 2013; San Francisco, CA: [Google Scholar]
- 174.Li KY, Roorda A. Automated identification of cone photoreceptors in adaptive optics retinal images.J Opt Soc Am A. 2007; 24: 1358–1363 [DOI] [PubMed] [Google Scholar]
- 175.Loquin K, Bloch I, Nakashima K, Rossant F, Boelle P-Y, Paques M.Automatic Photoreceptor Detection in In-Vivo Adaptive Optics Retinal Images: Statistical Validation Image Analysis and Recognition. Berlin/Heidelberg: Springer; 2012. [Google Scholar]
- 176.Xue B, Choi SS, Doble N, Werner JS. Photoreceptor counting and montaging of en-face retinal images from an adaptive optics fundus camera.J Opt Soc Am A. 2007; 24: 1364–1372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Fang L, Li S, McNabb R, et al. Fast acquisition and reconstruction of optical coherence tomography images via sparse representation.IEEE Trans Med Imag. In press [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Fang L, Li S, Nie Q, Izatt JA, Toth CA, Farsiu S. Sparsity based denoising of spectral domain optical coherence tomography images.Biomed Opt Express. 2012; 3: 927–942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Owsley C, Jackson GR, Cideciyan AV, et al. Psychophysical evidence for rod vulnerability in age-related macular degeneration.Invest Ophthalmol Vis Sci. 2000; 41: 267–273 [PubMed] [Google Scholar]
- 180.Puell MC, Barrio AR, Palomo-Alvarez C, Gomez-Sanz FJ, Clement-Corral A, Perez-Carrasco MJ. Impaired mesopic visual acuity in eyes with early age-related macular degeneration.Invest Ophthalmol Vis Sci. 2012; 53: 7310–7314 [DOI] [PubMed] [Google Scholar]
- 181.Dimitrov PN, Robman LD, Varsamidis M, et al. Relationship between clinical macular changes and retinal function in age-related macular degeneration.Invest Ophthalmol Vis Sci. 2012; 53: 5213–5220 [DOI] [PubMed] [Google Scholar]
- 182.Dimitrov PN, Robman LD, Varsamidis M, et al. Visual function tests as potential biomarkers in age-related macular degeneration.Invest Ophthalmol Vis Sci. 2011; 52: 9457–9469 [DOI] [PubMed] [Google Scholar]
- 183.Owsley C, Jackson GR, White M, Feist R, Edwards D. Delays in rod-mediated dark adaptation in early age-related maculopathy.Ophthalmology. 2001; 108: 1196–1202 [DOI] [PubMed] [Google Scholar]
- 184.Patryas L, Parry NR, Carden D, et al. Assessment of age changes and repeatability for computer-based rod dark adaptation.Graefes Arch Clin Exp Ophthalmol. 2013; 251: 1821–1827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Sunness JS, Rubin GS, Broman A, Applegate CA, Bressler NM, Hawkins BS. Low luminance visual dysfunction as a predictor of subsequent visual acuity loss from geographic atrophy in age-related macular degeneration.Ophthalmology. 2008; 115: 1480–1488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Chiu SJ, Li XT, Nicholas P, Toth CA, Izatt JA, Farsiu S. Automatic segmentation of seven retinal layers in SDOCT images congruent with expert manual segmentation.Opt Express. 2010; 18: 19413–19428 [DOI] [PMC free article] [PubMed] [Google Scholar]