Effect of yogic colon cleansing (Laghu Sankhaprakshalana Kriya) on pain, spinal flexibility, disability and state anxiety in chronic low back pain (original) (raw)
Abstract
Background:
Studies have shown that Integrated Yoga reduces pain, disability, anxiety and depression and increases spinal flexibility and quality-of-life in chronic low back pain (CLBP) patients.
Objective:
The objective of this study was to compare the effect of two yoga practices namely laghu shankha prakshalana (LSP) kriya, a yogic colon cleansing technique and back pain specific asanas (Back pain special technique [BST]) on pain, disability, spinal flexibility and state anxiety in patients with CLBP.
Materials and Methods:
In this randomized control (self as control) study, 40 in-patients (25 were males, 15 were females) between 25 and 70 years (44.05 ± 13.27) with CLBP were randomly assigned to receive LSP or BST sessions. The measurements were taken immediately before and after each session of either of the practices (30 min) in the same participant. Randomization was used to decide the day of the session (3rd or 5th day after admission) to ensure random distribution of the hang over effect of the two practices. Statistical analysis was performed using the repeated measures analysis of variance.
Results:
Significant group * time interaction (P < 0.001) was observed in 11 point numerical rating scale, spinal flexibility (on Leighton type Goniometer) and (straight leg raise test in both legs), Oswestry Disability Index, State Anxiety (XI component of Spieldberger's state and trait anxiety inventory. There was significantly (P < 0.001, between groups) better reduction in LSP than BST group on all variables. No adverse effects were reported by any participant.
Conclusion:
Clearing the bowel by yoga based colon cleansing technique (LSP) is safe and offers immediate analgesic effect with reduced disability, anxiety and improved spinal flexibility in patients with CLBP.
Keywords: Chronic low back pain, spinal flexibility, yogic colon cleansing
INTRODUCTION
Chronic low back pain (CLBP) is a primary public health concern globally.[1] Four categories were proposed by Dunn _et al._[2] to classify CLBP patients representing diverse paths over time: Persistent mild, recovering, severe chronic and fluctuating type.[3] CLBP has turned out to be the cause for approximately 6-9% of middle-aged people to consult their family physician every year.[4] The present day conventional biomedical system alone cannot bear the burden of life-style related diseases like back pain. This has led 38.4% of CLBP patients to use (Complementary and Alternative Medicine [CAM]) including yoga.[5] Hsu et al. observed several positive outcomes that participants receiving CAM treatments reported which were not recorded with standardized quantitative outcome measures; these were increased body awareness, changes in thought process that facilitated the ability to cope with low back pain (LBP) and a positive emotional state of mind.[6] Yoga is not only an Indian psychology, which is disciplined by physical, mental and spiritual practices, but also a scientifically studied therapy that has shown benefits in management of several chronic conditions.[7] Previous studies on yoga and back pain have been successful in establishing the beneficial effects by reducing chronic pain and disability, anxiety and depression and also increasing flexibility and quality-of-life.[8,9,10,11,12]
In our earlier studies on CLBP, we used an integrated module of yoga therapy that included selected Asanas, Pranayama, meditation and healthy life-style program.[12] It is said by Patanjali Maharishi that all these yoga practices are meant to have a common end point, i.e., mastery over the modifications of the mind (Chitta Vrtti Nirodhah), which is the state of mind required for healing mind body diseases.[13] Yoga emphasizes the value of clearing the bowel before preparing for any practice and has evolved several colon cleansing techniques (Shankha Prakshalana, Basti etc). These are a part of a broad category of practices called Kriyas that offer mastery over the mind in conformity with the definition of yoga and also have a therapeutic role.[14] In our pilot studies during the routine yoga therapy courses for CLBP at the residential health home, many patients had reported a good feeling with pain reduction and better flexibility soon after clearing the bowel through a colon cleaning technique called Laghu Shankha Prakshalana (LSP).[14] Although, studies have shown the beneficial effects of selected Asanas combined with relaxation[15] or integrated yoga[12] in reducing chronic pain or anxiety or depression, there is no study to date that has looked at the effect of yogic cleansing techniques on LBP. Hence the present study was planned with the objective of comparing the immediate effect of LSP with an active session of back pain specific asanas in patients with mechanical CLBP with the hypothesis that, immediately after the practice of LSP, the spinal flexibility would increase with reduction in pain, disability and anxiety.
MATERIALS AND METHODS
Subjects
A total of 40 CLBP patients were admitted to a yoga therapy health home for in-patient treatment who satisfied the selection criteria were recruited for the study. Statistical calculation using G* power software version 3.0.10 (Erdfelder, Faul, and Buchner, 1996, Department of Psychology, Germany)yielded a sample size of 20 for an effect size (ES) of 1.5 (calculated from previous studies on yoga and LBP) with an alpha at 0.05 powered at 0.8.[12] The inclusion criteria were: (a) history of CLBP of more than 3 months,[16](b) pain in the lumbar spine with or without radiation to legs[17] and (c) age between 25 and 70 years. Exclusion criteria were:(a) CLBP due to organic pathology in the spine such as malignancy (primary or secondary), or chronic infections checked by X-ray of the lumbar spine, (b) severe degree of pain, (c) recommended surgical intervention, (d) severe obesity, (e) chronic cardio-pulmonary illnesses, and (f) women during their menstruation or pregnancy.
The study was approved by the institutional review board and the Ethical Committee of the University. Signed informed consent was obtained from all participants.
Study design
In this self as control study, 40 participants who satisfied the selection criteria were allotted to two groups by a computer generated random number table (www.randomizer.org). Numbered opaque envelopes were used to implement the random allocation to conceal the sequence until the day of the intervention was assigned. All 40 subjects were assessed on two occasions (3rd and 5th day) before and after the practice of either LSP or the active control intervention, the BST (Back pain Special Technique) Two groups (group A and B) randomization table was used to allocate subjects to the two interventions on the 3rd or 5th day after admission to ensure random distribution of the hang over effect of the two sessions. Demographic details, vital clinical data, personal, family and stress history were documented before starting the intervention on the 1st day. All subjects were taught the integrated yoga module as in our earlier studies.[8,9,10,11,12] It was ensured that all had learnt the back pain special technique (BST) within 3 days after admission before they were taken up for the experimental session. Group A was taken for the experiment on LSP on the 3rd day and BST on 5th day while group B was taken for BST on the 3rd day and LSP on the 5th day after admission. Outcome variables were recorded immediately before and after the sessions on the 3rd and 5th day.
Blinding and masking
As this was an interventional study the subjects and the therapists could not be blinded to the type of intervention. The researcher who carried out the assessments and the statistician, who randomized and analyzed data, were blind to the subject's group. After completion of this study, the psychologist scored the coded answer sheets of the questionnaires.
Techniques used
LSP
Standard procedure of LSP that formed an integral part of integrated approach of yoga therapy (IAYT) for CLBP[18] was formulated using the concepts from traditional yogic scriptures[19] and contemporary yoga manuals of Bihar school of yoga[14] and S-VYASA.[12] Both practices were taught by certified post-graduate yoga therapists. A physician trained in yoga was available for supervision.
Procedure of LSP
About 2 L of Luke warm saline (about 1% of sodium chloride) water is kept ready before starting the session. The participant dressed suitably is taken to the venue specially designed for the practice of LSP. The subject sits comfortably in a chair and drinks two glasses of water (about 100 ml/glass). After drinking, a series of five specific βsanas (Tβḍβsana [palm tree pose], Tiryanktβḍβsana [swaying palm tree pose], Kaṭi cakrβsana [waist rotating pose], Tiryanka bhujaṅgβsana [twisting cobra pose] and Udarβkar?aṇasana [abdominal stretch pose]) are repeated 5-10 times each[14] under the guidance of the instructor. If the participant gets the urge to empty the bowel in between the practices he/she is permitted to rush to the toilet and empty the bowel. If he/she does not get the sensation, the cycle of drinking water followed by the practice of five asanas is repeated (a total of three cycles only) until he/she gets the urge. If they failed to get the urge within three cycles then the practice is abandoned and planned to try the next day. Although it was planned that those who did not succeed on the first attempt would be dropped out of the study, there were no drop outs as all of them succeeded in completing the procedure with a good feeling of clearence of the bowel. After the practice, the participant is taken for a deep relaxation technique (DRT).
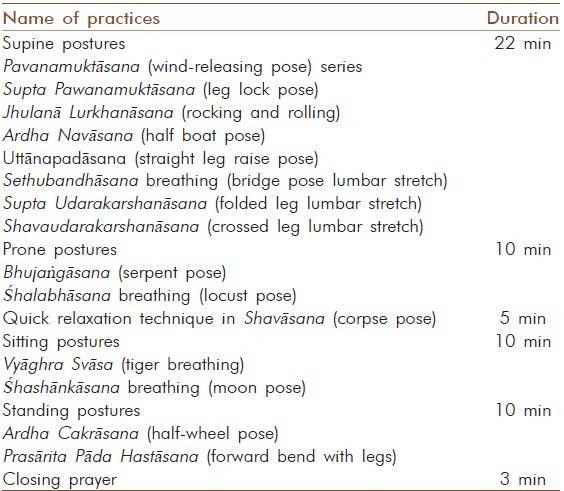
Control group intervention – BST
BST, used as part of the module of IAYT for CLBP, incorporates simple yogic movements [Table 1] followed by maintenance in the final posture of selected Asanas that provide stretch and relaxation. The safety of the practices was ensured by avoiding acute forward or backward movements of the spine or jerky movements while designing the module[20] these practices were followed by DRT.
Table 1.
Practices of back pain special technique session
DRT
This practice used in all IAYT modules for all diseases at the health home is a guided mental relaxation technique that lasts 15 min. It has 3 phases: (1) relaxation with internal awareness of the part mentioned, from the toes to the head; (2) letting the body “collapse” on the ground with a feeling of “let go,” while chanting Om; and (3) inducing a feeling of expansion by visualization of the limitless sky or ocean.[21]
Measurements
All measurements were recorded immediately before and after both the sessions (LSP and BST) on the 3rd and 5th day.
Oswestry disability index
Section 1 of the revised ODI for LBP (ODI),[22,23] a self-administered questionnaire, was used. This section of ODI provides measures of pain intensity with 5 graded questions for assessing the degree of pain in 10 different activities of living such as walking, standing, social life, etc. Test-retest reliability of ODI is high, ranging from 0.83 to 0.99. It has good construct validity and Cronbach alpha ranges from 0.71 to 0.87.
Eleven point numerical rating scale
Pain intensity numerical rating scale[24,25] is an analog scale that has a 10 centimeter line drawn on a plain sheet of white paper with eleven dots (0-10) marked as no pain at “0” and worst possible pain at 11th dot.
Spieldberger's state and trait anxiety inventory
This self-reported inventory[26,27] comprises two components, i.e., X1 for measuring state anxiety and X2 for trait anxiety. In the present study, STAI X1 was used to measure the immediate effect of the practice. This consists of twenty statements that evaluate how the participant feels “right now, at this moment.” In responding to the state anxiety scale, the participant chooses the alternative that best represents the intensity of their feelings: (1) not at all, (2) somewhat, (3) moderately, (4) very much so. Each STAI item is given a weighted score of 1-4. STAI has concurrent validity ranging from 0.75 to 0.80 with other tests. The overall median co-efficient alpha is 0.92.
Spinal flexibility
Spinal mobility[28] was measured using Leighton type goniometer (Anand Agencies, Pune, India). This instrument is tied around the waist and has a dial with a calibration from 0° to 360°. The values for the range of the movement during forward and backward bending are observed on the dial and recorded in degrees.
Straight leg raising test
Spinal flexion was measured by SLR test using a caliper type goniometer (Anand Agencies, Pune, India), which comprises of 2 cm scales fixed at an axis with a compass (calibrated in degrees) fixed at this point. Participant is made to lie down on the couch comfortably and placed next to the body with the center of axis at the tip of the greater trochanter and the stationary arm resting on the couch. The other arm of the caliper is held by the examiner along the lateral midline of the thigh. The participant's leg is raised passively by the examiner, up to a point where the patient starts experiencing pain. The angle between the two scales is read off on the compass and recorded in degrees. The same procedure is repeated on both sides.
Data analysis
The data were analyzed using SPSS (Statistical Package for Social Sciences), version 18.0 (IBM corporation). Statistical tests used included Kolmogorov–Smirnov's test for normality of baseline data, independent samples “_t_” to check for baseline matching of the groups and repeated measures analysis of variance (repeated measures ANOVA) to compare the means within and between groups. ESs were also calculated.
RESULTS
Figure 1 shows the study profile. There were no drop outs in this study that recruited 40 participants. Table 2 gives the details of the socio-demographic and medical characteristics. The baseline data were normally distributed for all variables. There were 25 males and 15 females. The age range was 27-66 with mean and standard deviation of 44 ± 13.27. No adverse events were observed/reported during or after the practices in any of the participants. Tables 3 and 4 show the results of all variables.
Figure 1.
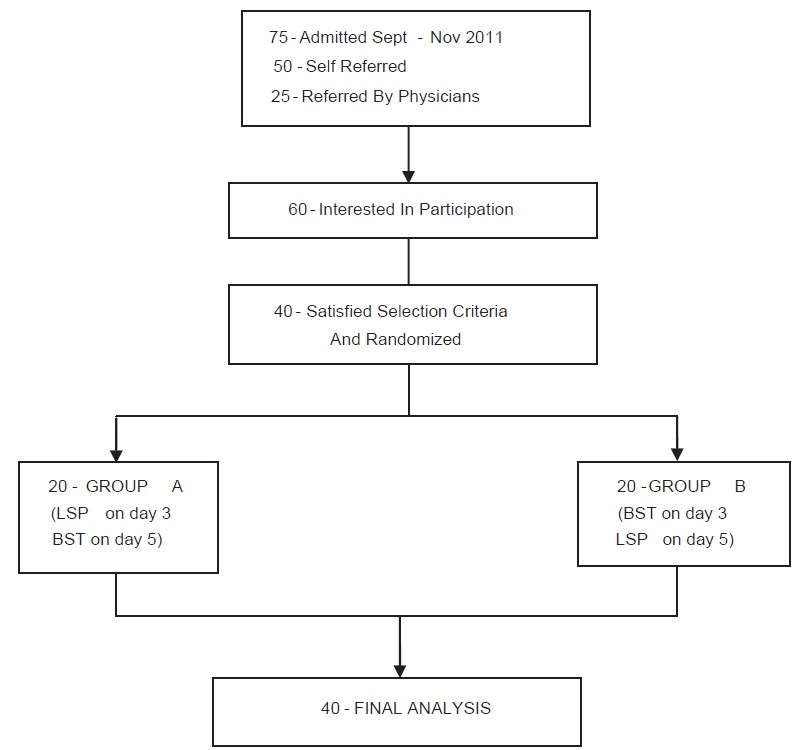
Trial profile
Table 2.
Demographic data
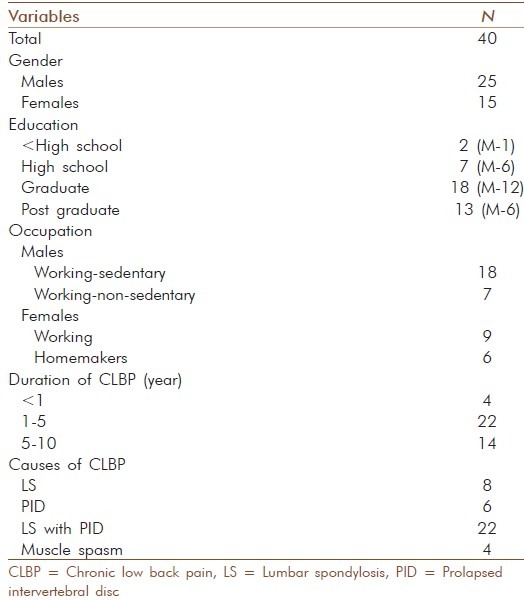
Table 3.
Results of psychological variables after intervention (repeated measures ANOVA)
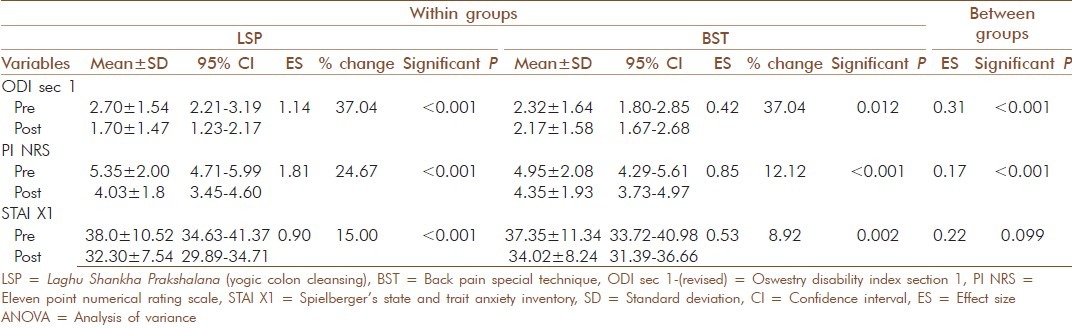
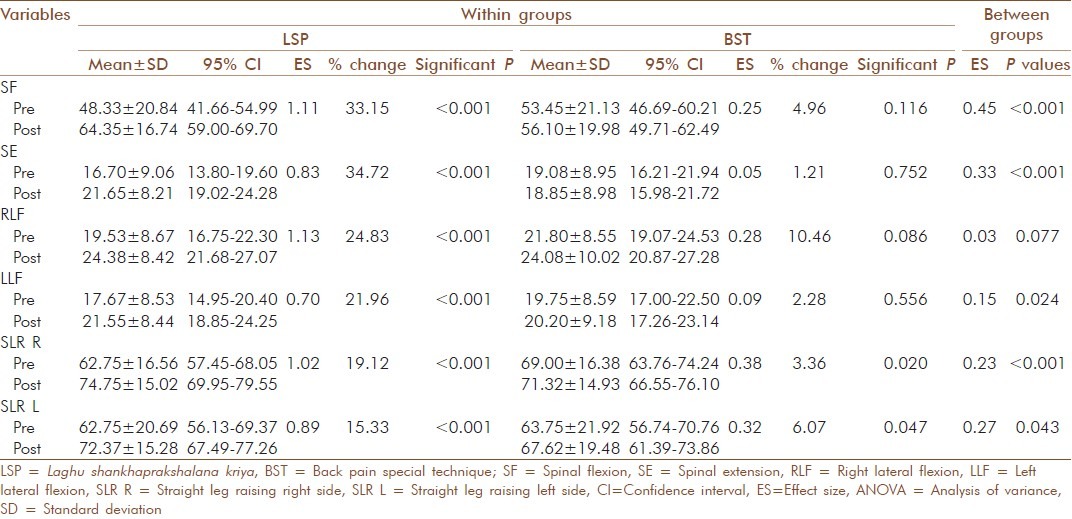
Table 4.
Results of objective measures of spinal mobility post intervention (repeated measures ANOVA)
ODI
There was a significant interaction between intervention and time (F(1,39)=32.11, P = 0.001) for section 1 of ODI. There was a significant difference within the two groups. The ODI for the LSP group significantly reduced (F(1,39)=58.78, P = 0.001), which was not significant in the BST group (F(1,39)=0.22, P = 0.001).
Numerical rating scale
There was a significant interaction between intervention and time (F(1,39)=17.00, P = 0.001) for NRS. NRS show. The changes after LSP (F(1,39)=176.38, P = 0.001) was higher (ES in LSP 1.81 vs. ES in BST 0.85) than in BST group, which was (F(1,39)=0.05, P = 0.001).
STAI X1
STAI-XI showed a significant reduction of state anxiety with significant interaction between intervention and time (F(1,39)=2.86, P = 0.001). The changes after LSP (F(1,39)=, P = 0.001) was higher (ES in LSP 0.90; in BST 0.53) compared with BST group (F(1,39)=0.294, P = 0.001).
Spinal flexibility
There was a significant interaction between intervention and time for Spinal flexion (F(1,39)=31.38, P = 0.001). The Spinal flexion for LSP group significantly increased (F(1,39)=34.25, P = 0.001) (ES in LSP 1.11; in BST 0.25), which was not significant in the BST group (F(1,39)=1.35, P = 0.001).
There was a significant interaction between intervention and time for Spinal extension (F(1,39)=18.29, P = 0.001). The Spinal extension for LSP group significantly increased (F(1,39)=13.02, P = 0.001) (ES in LSP 0.83; in BST 0.05), which was not significant in the BST group (F(1,39)=0.96, P = 0.001).
There was a significant interaction between intervention and time for Right lateral flexion (F(1,39)=3.29, P = 0.001). The Right lateral flexion for LSP group significantly increased (F(1,39)=22.78, P = 0.001) (ES in LSP 1.13; in BST 0.28), which was not significant in the BST group (F(1,39)=1.28, P = 0.001).
There was a significant interaction between intervention and time for Left lateral flexion (F(1,39)=5.50, P = 0.001). The Left lateral flexion for LSP group significantly increased (F(1,39)=33.90, P = 0.001) (ES in LSP 0.70; in BST 0.09) which was not significant in the BST group (F(1,39)=0.36, P = 0.001).
SLR
SLR test using a scale type of goniometer showed significant interaction between intervention and time (P = 0.001) (F(1,39)=19.20, P = 0.001). The Left lateral flexion for LSP group significantly increased (F(1,39)=52.81, P = 0.001) (ES in LSP 0.89; in BST 0.38), which was not significant in the BST group (F(1,39)=0.71, P = 0.001).
DISCUSSION
This was a single blind randomized self as control study with cross over feature, that compared the immediate effect of two yoga techniques, on 40 participants with CLBP. Results were showed significant group * time interaction (P < 0.01, Repeated Measures ANOVA) with better improvement after LSP than BSP on all variables.
Comparisons
There are no published studies on yogic colon cleansing practices and effect of such a practice in patients with CLBP or in normal volunteers. However three earlier randomized control studies on yoga for back pain,[9,12,15] have found a reduction in pain, increased spinal mobility and reduction in scores on state and trait anxiety, depression scales. A study by Tekur et al. reported 46% reduction in pain intensity, and increase in SLR (right side by 38%, left side by 35%) in Yoga group after 1 week of intervention.[12]
The present study measuring the immediate effect not only showed a significant reduction in subjective measures of pain (24.67% in NRS) and disability (37.04% in the disability caused by pain), but also in the objective measures of spinal flexibility with the increase in spinal extension by 34.72%, flexion by 33.15%, right lateral bending by 24.83% and left lateral bending by 21.96%. The results of Iyengar yoga had shown significant reduction in pain and functional disability, after 16 and 32 weeks of yoga (3 classes/week) with no significant improvement in the degree of spinal flexibility.[15]
Mechanisms
The mechanism of pain relief during LSP or BST in CLBP may involve both central and peripheral systems. It is known that the conscious awareness of pain involves cortical, limbic and autonomic systems.[29] At the cortical level, evidence suggests that yoga helps in pain reduction due to production of endorphin resulting from alternate stretch and relax procedures of physical postures done with awareness.[30] At limbic level, yoga offers mastery over the emotional surges through controlled and need based physiological responses to stressfully demanding situations instead of uncontrolled overtones of (HPA axis) hypothalamo-pituitary-adrenal axis during chronic pain.[31] Studies also point to reduction in sympathetic arousal following yoga based relaxation techniques.[21] Yoga changes the physiological responses to stressors by improving autonomic stability with better parasympathetic tone and reduction in sympathetic arousal with improved performance.[32]
Peripheral factors that are responsible for CLBP include muscle spasm and local inflammatory responses. Leask and Abraham observed that mechanical, emotional, behavioral and motor dysfunction in CLBP may result in inflammation and fibrosis in addition to spasm and wasting, that could be traced to tissue hypoxia, lowered Ph and release of cytokines such as transforming growth factor beta-1.[33] It is proposed that yoga reduces paraspinal muscle spasm and inflammation during BST and LSP through deep local rest and relaxation that follows safe stretches done with awareness.
Yoga considers mechanical CLBP to be a mind-body disease (Adhija Vyadhi).[18] Accordingly, CLBP is the end point in the chain of events that starts in the mind (Manomaya Kosha) as an uncontrolled persistent emotional response to demanding situations of life. Yoga conceptualizes existence of a subtle energy (Prana)[18,34] in all living systems that intervenes between mind and body, that flows along different channels (Nadis or meridians), to promote all physiological functions. Prana flow increases on demand by the heightened activity in that zone and returns to base level during rest, i.e., as soon as one decides to sit or stand erect which demands continued contraction of the paraspinal muscles, Prana rushes to those muscles to keep it active as long as required. There are two subtle channels or nerves (Nadis) situated on either side of the spinal column from which thousands of branches spread all over the body to supply prana to different organs.[14] Based on the descriptions in traditional texts, some authors[14] propose that these meridians may correspond to the two sections of the autonomic outflow (left meridian (Ida) to the parasympathetic and the right (Pingala) to the sympathetic); a controlled flow of prana through both these channels maintains health; imbalance due to uncontrolled flow results in ill- health; the aim of therapy is to restore balance. Hence it is hypothesized that all yoga practices (including BST, Pranayama, LSP) help in restoring this balance, which can be seen as sympathovagal balance that has been observed in many physiological studies.[35]
How does bowel cleansing work? The clinicians of yoga and ayurveda (5000 years ago) observed that LBP is usually associated with disturbed bowel functions (constipation or IBS Irritable Bowel Syndrome) and proposed that this is a manifestation of uncontrolled excessive locked up flow in the local Prana control structures called Chakras.[19] Chakras are vortices of Prana, which seem to operate through the major nerve plexi,[14] that monitor and control the flow of Prana in six zones of the body starting from vertex (Sahasrara Chakra) to sacrum (Muladhara Chakra). The lowest of the seven vortices, the “root center,” situated at the base of the spine (Muladhara Chakra) controls the physiological functions in the lower zone of the trunk including all involuntary (e.g., defecation) and voluntary functions (Paraspinal and perennial muscles). Thus, it is proposed that CLBP is a manifestation of dysfunction of Muladhara Chakra. LSP clears the bowel by activating the peristaltic reflex by a combination of specific physical postures (Asanas) that are designed to release the locked up Prana in this Chakra.[14] The DRT that follows the practice of LSP (essential component after any Kriya) contributes to mastery over the local neuromuscular reflexes through internal awareness and releases the spasm of para-spinal muscles.[36] BST also has similar balancing effect on the Prana and uses safe movements to develop this mastery. Thus, it appears that LSP offers a greater degree of pain relief than BST by the added bowel clearing effect.
CONCLUSION
Both yoga practices, namely yoga based physical postures (BST) and yoga based colon cleansing (LSP) have beneficial effects immediately after the practice in patients with CLBP. The LSP is better than BST in reducing pain, disability and anxiety and also in increasing flexibility.
Strengths
To the best of our knowledge, this is the first study that has looked at the immediate effect of LSP in CLBP and shown significant results in all variables including subjective (pain and disability) and objective measures (spinal flexibility). The novel aspect of the design of this study was: (a) the self as control design, and (b) incorporation of randomization and blinding.
Limitations
There were a few limitations of the study: (a) The study compared two specific yoga practices and there was no neutral control session. (b) As the study was planned to observe only the immediate effects on CLBP, it does not answer the question of long term effect of LSP on CLBP. (c) Although we did not observe any subject with aggravation of pain after the practice during our study, it may be argued that the yoga practices used during the standard way of performing LSP have the potential to aggravate the pain. Hence, we had to select only those patients with moderate to mild pain in an indoor setting of a yoga university and monitored the practices carefully by expert trainers with medical supervision. Therefore, the conclusion from this study may not be universally applicable to all cases of LBP. There is a need to evolve simplified versions of LSP.
Suggestions for future research
Future studies may be designed to look at the long-term benefits of LSP. Considering that this is the first study that has pointed to the beneficial effects of LSP in pain management, it is necessary to design studies to compare LSP with simpler methods of bowel cleansing through enemas or simpler laxatives as control interventions.
Implication and recommendations
This study is a pointer to the immediate analgesic effect of LSP. When the result of this study gets established through more RCTs with larger sample sizes by other researchers, it would be very important evidence to the knowledge that cleansing the bowel is essential in pain management, which is strongly recommended in most CAM therapies such as yoga and Ayurveda. Based on the observation of this study, we recommend that “regular bowel clearing” may be included as an important vital parameter in the daily nursing procedures in all cases of acute and chronic pain.
ACKNOWLEDGMENT
We are grateful to Dr. Pradhan B and Amrit R who helped with data management and statistical analysis. We thank all the staff of S-VYASA for their cooperation in conducting the program, and our special thanks to Dr. Barve V, Mr. Singh D and Mr. Saraf G for technical assistance.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Hoy D, March L, Brooks P, Woolf A, Blyth F, Vos T, et al. Measuring the global burden of low back pain. Best Pract Res Clin Rheumatol. 2010;24:155–65. doi: 10.1016/j.berh.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 2.Dunn KM, Jordan K, Croft PR. Characterizing the course of low back pain: A latent class analysis. Am J Epidemiol. 2006;163:754–61. doi: 10.1093/aje/kwj100. [DOI] [PubMed] [Google Scholar]
- 3.Tamcan O, Mannion AF, Eisenring C, Horisberger B, Elfering A, Müller U. The course of chronic and recurrent low back pain in the general population. Pain. 2010;150:451–7. doi: 10.1016/j.pain.2010.05.019. [DOI] [PubMed] [Google Scholar]
- 4.Jordan KP, Kadam UT, Hayward R, Porcheret M, Young C, Croft P. Annual consultation prevalence of regional musculoskeletal problems in primary care: An observational study. BMC Musculoskelet Disord. 2010;11:144. doi: 10.1186/1471-2474-11-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fleming S, Rabago DP, Mundt MP, Fleming MF. CAM therapies among primary care patients using opioid therapy for chronic pain. BMC Complement Altern Med. 2007;7:15. doi: 10.1186/1472-6882-7-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hsu C, Bluespruce J, Sherman K, Cherkin D. Unanticipated benefits of CAM therapies for back pain: An exploration of patient experiences. J Altern Complement Med. 2010;16:157–63. doi: 10.1089/acm.2009.0188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pandey A, Tripathi P, Pandey R, Srivatava R, Goswami S. Alternative therapies useful in the management of diabetes: A systematic review. J Pharm Bioallied Sci. 2011;3:504–12. doi: 10.4103/0975-7406.90103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Williams AC, Nicholas MK, Richardson PH, Pither CE, Justins DM, Chamberlain JH, et al. Evaluation of a cognitive behavioural programme for rehabilitating patients with chronic pain. Br J Gen Pract. 1993;43:513–18. [PMC free article] [PubMed] [Google Scholar]
- 9.Sherman KJ, Cherkin DC, Erro J, Miglioretti DL, Deyo RA. Comparing yoga, exercise, and a self-care book for chronic low back pain: A randomized, controlled trial. Ann Intern Med. 2005;143:849–56. doi: 10.7326/0003-4819-143-12-200512200-00003. [DOI] [PubMed] [Google Scholar]
- 10.Williams K, Abildso C, Steinberg L, Doyle E, Epstein B, Smith D, et al. Evaluation of the effectiveness and efficacy of Iyengar yoga therapy on chronic low back pain. Spine (Phila Pa 1976) 2009;34:2066–76. doi: 10.1097/BRS.0b013e3181b315cc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tekur P, Chametcha S, Hongasandra RN, Raghuram N. Effect of yoga on quality of life of CLBP patients: A randomized control study. Int J Yoga. 2010;3:10–17. doi: 10.4103/0973-6131.66773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tekur P, Singphow C, Nagendra HR, Raghuram N. Effect of short-term intensive yoga program on pain, functional disability and spinal flexibility in chronic low back pain: A randomized control study. J Altern Complement Med. 2008;14:637–44. doi: 10.1089/acm.2007.0815. [DOI] [PubMed] [Google Scholar]
- 13.Satyananadasaraswati S. Four Chapters on Freedom. 3rd ed. Munger, Bihar, (India): Yoga Publication Trust; 2004. pp. 25–60. [Google Scholar]
- 14.Satyanandasaraswati S. Asana Pranayama Mudra Bandha. 4th ed. Munger, Bihar, (India): Yoga Publication Trust; 2004. pp. 485–99. [Google Scholar]
- 15.Williams KA, Petronis J, Smith D, Goodrich D, Wu J, Ravi N, et al. Effect of Iyengar yoga therapy for chronic low back pain. Pain. 2005;115:107–17. doi: 10.1016/j.pain.2005.02.016. [DOI] [PubMed] [Google Scholar]
- 16.Merskey H. Classification of chronic pain. Descriptions of chronic pain syndromes and definitions of pain terms. Prepared by the International Association for the Study of Pain, Subcommittee on Taxonomy. Pain Suppl. 1986;3:S1–226. [PubMed] [Google Scholar]
- 17.Spitzer WO, LeBlanc, Dupic M. Scientific approach to the assessment and management of activity-related spinal disorders. A monograph for clinicians. Report of the Quebec Task Force on Spinal Disorders. Spine (Phila Pa 1976) 1987;12:S1–59. [PubMed] [Google Scholar]
- 18.Nagarathna R, Nagendra HR. Integrated Approach of Yoga Therapy for Positive Health. 3rd ed. Bangalore, (India): Swami Vivekananda Yoga Prakashana; 2006. pp. 4–20. [Google Scholar]
- 19.Swatmaram S. Hatha Yoga Pradipika. 2nd ed. Munger (India): Yoga Publication Trust; 2004. pp. 4–30. [Google Scholar]
- 20.Nagarathna R, Nagendra HR. Yoga for Back Pain. 2nd ed. Bengaluru: Swami Vivekananda Yoga Prakashana; 2001. pp. 15–30. [Google Scholar]
- 21.Vempati RP, Telles S. Yoga-based guided relaxation reduces sympathetic activity judged from baseline levels. Psychol Rep. 2002;90:487–94. doi: 10.2466/pr0.2002.90.2.487. [DOI] [PubMed] [Google Scholar]
- 22.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976) 2000;25:2940–52. doi: 10.1097/00007632-200011150-00017. [DOI] [PubMed] [Google Scholar]
- 23.Mehra A, Baker D, Disney S, Pynsent PB. Oswestry disability index scoring made easy. Ann R Coll Surg Engl. 2008;90:497–99. doi: 10.1308/003588408X300984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ornetti P, Dougados M, Paternotte S, Logeart I, Gossec L. Validation of a numerical rating scale to assess functional impairment in hip and knee osteoarthritis: Comparison with the WOMAC function scale. Ann Rheum Dis. 2011;70:740–46. doi: 10.1136/ard.2010.135483. [DOI] [PubMed] [Google Scholar]
- 25.Gagliese L, Weizblit N, Ellis W, Chan VW. The measurement of postoperative pain: A comparison of intensity scales in younger and older surgical patients. Pain. 2005;117:412–20. doi: 10.1016/j.pain.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 26.Spielberger CD. Manual for the State-Trait Anxiety Inventory (Self-Evaluation Questionnaire) Palo Alto, CA: Consulting Psychologists Press; 1970. [Google Scholar]
- 27.Spielberger CD, Reheiser EC, Ritterband LM, Sydeman SJ, Unger KK. Assessment of emotional states and personality traits: Measuring psychological vital signs. In: Butcher JN, editor. Clinical Personality Assessment: Practical Approaches. New York: Oxford University Press; 1995. pp. 1–7. [Google Scholar]
- 28.Hsieh CY, Walker JM, Gillis K. Straight-leg-raising test. Comparison of three instruments. Phys Ther. 1983;63:1429–33. doi: 10.1093/ptj/63.9.1429. [DOI] [PubMed] [Google Scholar]
- 29.Carver A. Pain. In: Dale DC, Federman DD, editors. ACP Medicine. New York NY: WebMD; 2005. pp. 1–18. [Google Scholar]
- 30.Tekur P, Nagarathna R, Chametcha S, Hankey A, Nagendra HR. A comprehensive yoga programs improves pain, anxiety and depression in chronic low back pain patients more than exercise: An RCT. Complement Ther Med. 2012;20:107–18. doi: 10.1016/j.ctim.2011.12.009. [DOI] [PubMed] [Google Scholar]
- 31.Leonard BE. HPA and immune axes in stress: Involvement of the serotonergic system. Neuroimmunomodulation. 2006;13:268–76. doi: 10.1159/000104854. [DOI] [PubMed] [Google Scholar]
- 32.Telles S, Narendran S, Raghuraj P, Nagarathna R, Nagendra HR. Comparison of changes in autonomic and respiratory parameters of girls after yoga and games at a community home. Percept Mot Skills. 1997;84:251–57. doi: 10.2466/pms.1997.84.1.251. [DOI] [PubMed] [Google Scholar]
- 33.Leask A, Abraham DJ. TGF-beta signaling and the fibrotic response. FASEB J. 2004;18:816–27. doi: 10.1096/fj.03-1273rev. [DOI] [PubMed] [Google Scholar]
- 34.Lokeshwarananda S. Taittireya Upanishat. 1st ed. Kolkatta, India: The Ramakrishna Mission Institute of Culture; 1996. pp. 10–25. [Google Scholar]
- 35.Telles S, Nagarathna R, Nagendra HR. Breathing through a particular nostril can alter metabolism and autonomic activities. Indian J Physiol Pharmacol. 1994;38:133–37. [PubMed] [Google Scholar]
- 36.Shankardevananda S. The Practices of Yoga for the Digestive System. 2nd ed. Munger, (India): Yoga Publication Trust; 2008. pp. 30–45. [Google Scholar]