West Nile Virus: Review of the Literature (original) (raw)
. Author manuscript; available in PMC: 2015 Sep 9.
Published in final edited form as: JAMA. 2013 Jul 17;310(3):308–315. doi: 10.1001/jama.2013.8042
Abstract
IMPORTANCE
Since its introduction in North America in 1999,West Nile virus has produced the 3 largest arboviral neuroinvasive disease outbreaks ever recorded in the United States.
OBJECTIVE
To review the ecology, virology, epidemiology, clinical characteristics, diagnosis, prevention, and control of West Nile virus, with an emphasis on North America.
EVIDENCE REVIEW
PubMed electronic database was searched through February 5, 2013. United States national surveillance data were gathered from the Centers for Disease Control and Prevention.
FINDINGS
West Nile virus is now endemic throughout the contiguous United States, with 16 196 human neuroinvasive disease cases and 1549 deaths reported since 1999. More than 780 000 illnesses have likely occurred. To date, incidence is highest in the Midwest from mid-July to early September. West Nile fever develops in approximately 25% of those infected, varies greatly in clinical severity, and symptoms may be prolonged. Neuroinvasive disease (meningitis, encephalitis, acute flaccid paralysis) develops in less than 1% but carries a fatality rate of approximately 10%. Encephalitis has a highly variable clinical course but often is associated with considerable long-term morbidity. Approximately two-thirds of those with paralysis remain with significant weakness in affected limbs. Diagnosis usually rests on detection of IgM antibody in serum or cerebrospinal fluid. Treatment is supportive; no licensed human vaccine exists. Prevention uses an integrated pest management approach, which focuses on surveillance, elimination of mosquito breeding sites, and larval and adult mosquito management using pesticides to keep mosquito populations low. During outbreaks or impending outbreaks, emphasis shifts to aggressive adult mosquito control to reduce the abundance of infected, biting mosquitoes. Pesticide exposure and adverse human health events following adult mosquito control operations for West Nile virus appear negligible.
CONCLUSIONS AND RELEVANCE
In North America, West Nile virus has and will remain a formidable clinical and public health problem for years to come.
West Nile virus has become endemic in all 48 contiguous United States as well as all Canadian provinces since its discovery in North America in New York City in1999.1 It has produced the 3 largest arboviral neuroinvasive disease (encephalitis, meningitis, or acute flaccid paralysis) outbreaks ever recorded in the United States, with nearly 3000 cases of neuroinvasive disease recorded each year in 2002, 2003, and 2012.
Evidence Review
This review is intended to provide a general overview of West Nile virus to the practicing physician or public health practitioner. Relevant background information was obtained by searching the PubMed electronic database through February 5, 2013, using the search term West Nile virus. Surveillance data from patients with disease onset from 1999 through 2012 and reported by May 15, 2013, were gathered from the national ArboNET surveillance system conducted by the Centers for Disease Control and Prevention.
Ecology
West Nile virus is maintained in a bird-mosquito-bird transmission cycle. Although West Nile virus has been detected in 65 different mosquito species and 326 bird species in the United States, only a few Culex mosquito species drive transmission of the virus in nature and subsequent spread to humans: Culex pipiens (northern house mosquito) in the northern half of the United States, the closely related species Cx quinquefasciatus (southern house mosquito) in the southern states, and Cx tarsalis in many areas of the plains and western states that overlap with the distribution of Cx pipiens and Cx quinquefasciatus. Numerous passerine birds (perching birds of the order Passeriformes) develop sufficient serum viremia to efficiently infect mosquitoes feeding upon them and thus are competent amplifier hosts.2 A relatively small subset of the bird community may significantly influence transmission dynamics and certain passerine species such as the American robin (Turdus migratorius) are important amplifiers despite their low abundance relative to other West Nile virus–susceptible birds.3 Humans are unlikely to infect mosquitoes because they only develop a low-level serum viremia4,5 and thus are considered dead-end hosts.
When conditions favor substantial viral amplification within the passerine-Culex transmission cycle, increasing numbers of infected mosquitoes present a human infection risk by mid to late summer. The complex and interrelated factors that promote viral amplification and hence human outbreaks are not well quantified and vary among the diverse ecological conditions present in North America. Warmer temperatures correlate with increased human incidence at national or regional (multistate) scales.6 Increased ambient temperature shortens the incubation time from infection to infectiousness in mosquitoes and increases viral transmission efficiency to birds, both critical factors for arboviral amplification.7,8 At smaller scales, urban and agricultural land covers,9 rural irrigated landscapes,10 increased temperature,11 increased rainfall,12 decreased rainfall,12 and several socioeconomic factors such as housing age and community drainage patterns,13 per capita income,10 and density of poorly maintained swimming pools14 relate to higher incidence in some locations. Nevertheless, considerable challenges remain in predicting how, when, and where these factors will combine to produce the focal, intense outbreaks that now characterize West Nile virus ecology in the United States.
Virology and Pathogenesis
West Nile virus is 1 of more than 70 viruses of the family Flaviviridae of the genus Flavivirus. Serologically, West Nile virus is a member of the Japanese encephalitis serocomplex, which includes Japanese encephalitis virus and an endemic North American flavivirus, St Louis encephalitis virus. West Nile viruses can be designated into at least 5 phylogenetic lineages.15 Only lineage 1 and 2 West Nile viruses have been associated with significant outbreaks in humans.
Lineage 1 can be further subdivided into 3 sublineages: isolates from the western hemisphere, Africa, the Middle East, and Europe constitute lineage 1a; Kunjin virus from Australasia represents lineage 1b; and lineage 1c consists of viruses from India.16 The initial North American isolates (East Coast genotype) identified in 1999 in New York City have been most closely related to a lineage 1a West Nile virus isolated from Israel in 1998.17 Since approximately 2002, the East Coast genotype has largely been displaced by a new genotype (WN02 genotype) encompassing several conserved amino acid substitutions that may have increased the efficiency and rapidity of viral transmission in North American mosquito vectors.7,18
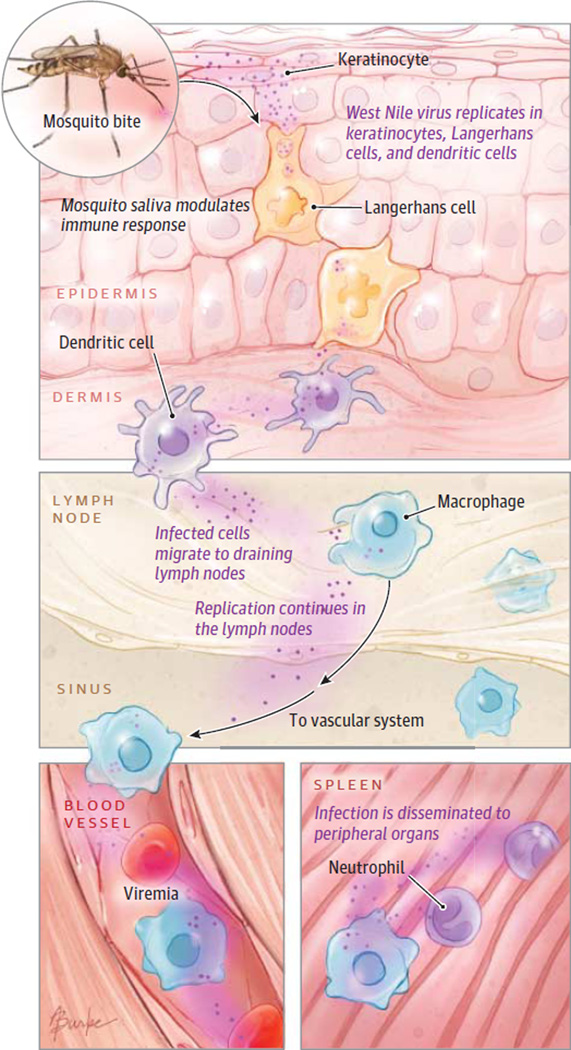
Mosquito salivary components introduced at the site of infection in vertebrates modulate initial infection of target cells such as keratinocytes19 and skin-resident dendritic cells through several mechanisms including focalized suppression of immune effector cell trafficking to the site of inoculation.20 Infected dendritic cells or keratinocytes migrate to draining lymph nodes from which a serum viremia is generated that then relays infection to visceral organs and potentially to the central nervous system (Figure 1).
Figure 1. Schematic of Pathogenesis of West Nile Virus Infection.
Following the bite of an infected mosquito, infection begins in keratinocytes and immune cells in the epidermis and spreads to draining lymph nodes. Viremia originating in the lymph nodes disseminates infection to peripheral organs.
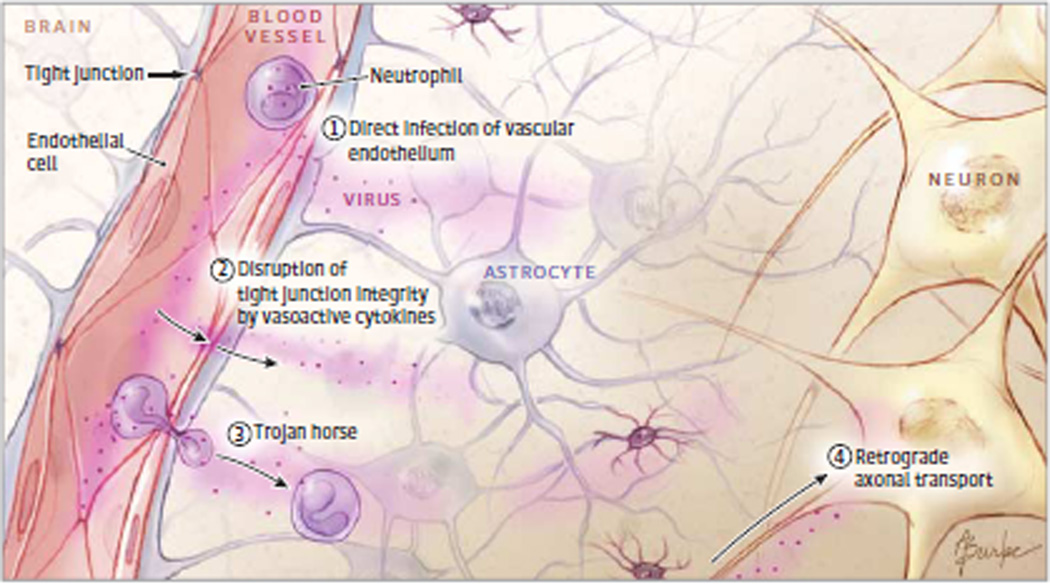
West Nile virus is capable of replicating and eliciting pathology in the brain (ie, neurovirulence); however, a critical prerequisite to generating neuroinvasive disease in humans is the virus’ capacity to gain access to the central nervous system (ie, neuroinvasiveness). Postulated West Nile virus neuroinvasive mechanisms include (1) direct viral crossing of the blood-brain barrier due to cytokine-mediated increased vascular permeability; (2) passage through the endothelium of the blood-brain barrier; (3) a Trojan horse mechanism in which infected tissue macrophages are trafficked across the blood-brain barrier; and (4) retrograde axonal transport of the virus to the central nervous system via infection of olfactory or peripheral neurons (Figure 2).21 Regardless of how the virus enters the central nervous system, murine models of infection have shown persistent viral replication in various tissues, including the central nervous system, suggesting a potential etiology for long-term neurological sequelae observed in patients with neuroinvasive disease.21
Figure 2. West Nile Virus Neuroinvasive Mechanisms.
Potential mechanisms for neuroinvasion of West Nile virus include (1) direct infection of the vascular endothelium and subsequent entry to the central nervous system, (2) viral passage through the vascular endothelium due to disruption of the blood-brain barrier integrity by vasoactive cytokines, (3) a Trojan horse mechanism through which infected monocytes are trafficked into the central nervous system, or (4) retrograde axonal transport to the central nervous system following infection of peripheral neurons.
Distribution and Human Disease Incidence
West Nile virus has an extensive distribution throughout Africa, the Middle East, southern Europe, western Russia, south western Asia, and Australia (Kunjin subtype of West Nile virus), which derives from its ability to infect numerous mosquito and bird species. Until the early 1990s, human outbreaks, mainly associated with mild febrile illnesses, were reported infrequently from Israel and Africa. Since then, new viral strains with likely African origin have increased human disease incidence in parts of Russia and southern and eastern Europe, with large outbreaks of increased clinical severity occurring in Romania, Russia, Israel, and Greece.15,22 In the western hemisphere, West Nile virus spread from its 1999 discovery location in New York City1 to the Pacific Coast by 200323,24 and Argentina by 2005.24 Although West Nile virus now circulates in many countries in the western hemisphere, for unknown reasons only the United States and Canada have experienced substantial human disease incidence.24
Most patients with West Nile virus–related illnesses are unrecognized clinically. A follow-up study of asymptomatic, viremic blood donors who subsequently developed West Nile fever showed that 38% sought medical care and 2% were hospitalized for symptoms attributable to the infection; however, only 5% of those seeking medical care were correctly diagnosed.4 Thus, incidence trends are best monitored by the incidence of neuroinvasive disease because reporting of these cases is comparatively complete. Nevertheless, even during a well-publicized outbreak, only 40% of patients with clinically compatible meningitis or encephalitis were tested for West Nile virus.25
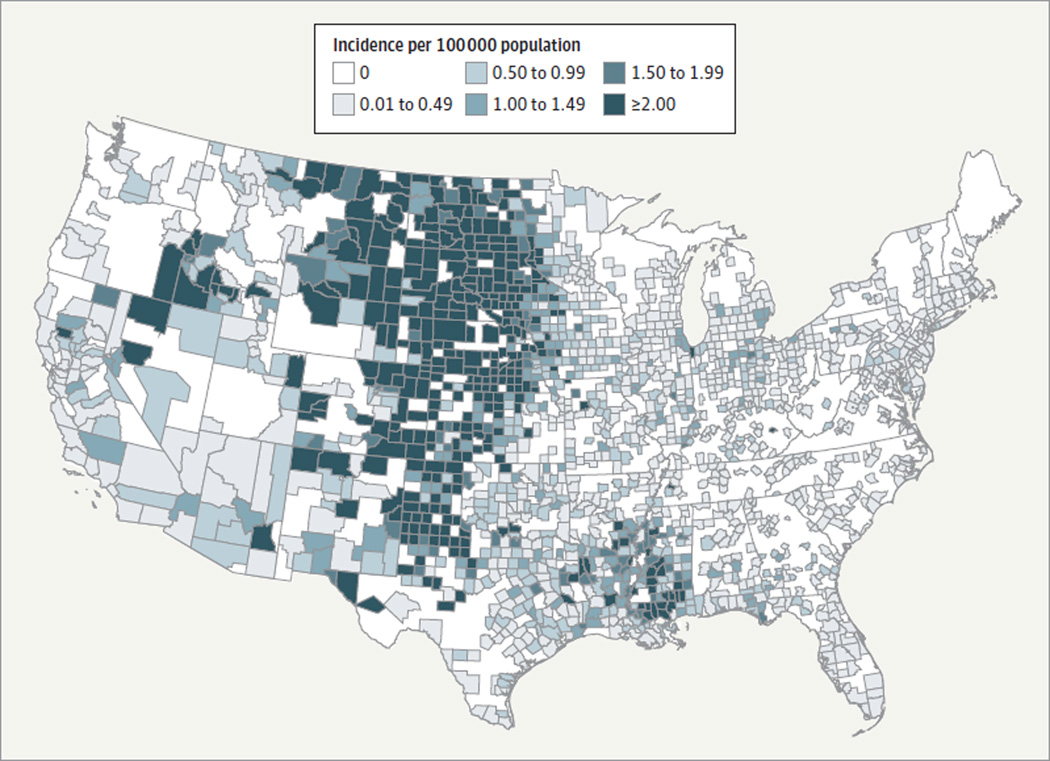
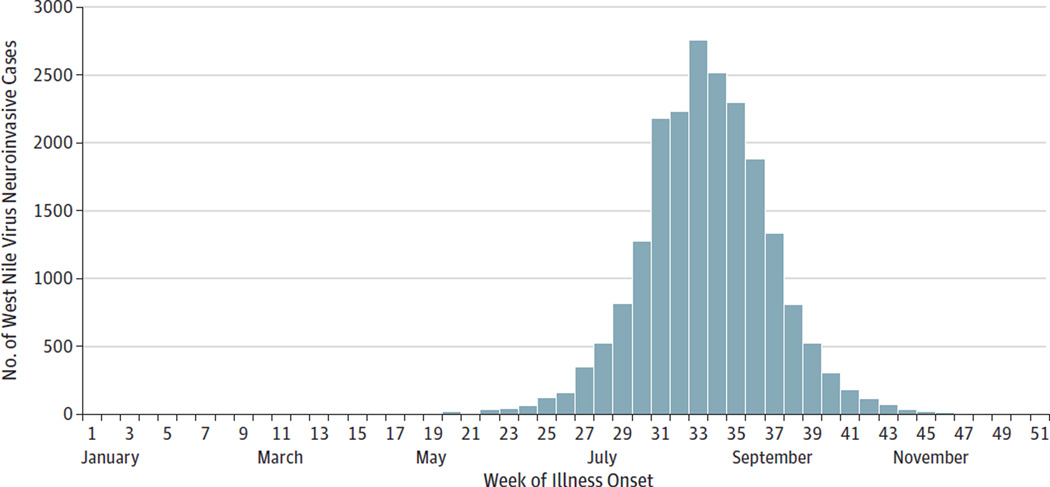
A total of 16 196 patients with West Nile virus neuroinvasive disease with onsets from 1999 through 2012 and 1549 deaths have been recorded in the United States. Although the number of patients with neuroinvasive disease fluctuates annually, some regions experience persistently higher incidence (Figure 3). Ninety-four percent of patients with West Nile virus infection have symptom onsets in July through September (Figure 4).23 Extrapolations from neuroinvasive disease case reporting in the United States suggest that through 2010 approximately 3 million persons were infected, of whom 780 000 developed West Nile fever.26 In Canada, West Nile virus was first detected in southern Ontario in 2001 and by 2009 the virus’ distribution had extended west ward to British Columbia. Through October 2012, 975 patients with neuroinvasive disease have been reported in Canada.
Figure 3.
Map of Average Annual Human Neuroinvasive Disease Incidence in the United States, 1999–2012
Figure 4.
Cumulative Number of Human West Nile Virus Neuroinvasive Disease Cases by Week of Onset, 1999–2012
Transmission to Humans
Mosquito bites account for nearly all human infections. West Nile virus can also be transmitted via transfused platelets, red blood cells, and fresh frozen plasma5 as well as through heart, liver, lung, and kidney transplants.27 Transmission via organ transplant has occurred from donors without detectable viremia, suggesting viral sequestration in organs shortly after viremia has cleared.
One possible transplacental transmission following a second trimester infection resulted in an infant with chorioretinitis, lissencephaly, and cerebral white matter loss. Fortunately, fetal abnormalities due to intrauterine infection are uncommon: none of 72 live infants born to 71 women infected during pregnancy had malformations linked to West Nile viral infection or had conclusive laboratory evidence of congenital infection.28 Nevertheless, 3 neonates born to women infected within 3 weeks’ prepartum developed symptomatic West Nile virus disease at or shortly after birth, indicating the possibility of intrauterine infection or infection at the time of delivery. Other rare or suspected modes of transmission include breast milk transmission, percutaneous or conjunctival exposure to laboratory workers, and by unknown means in patients undergoing dialysis and workers at a turkey breeder farm.24
Infection and Illness
It is not known what proportion of persons develop West Nile virus infection following an infected mosquito bite. Persons with a genetic defect in the_OAS1_ gene (HGNC 8086), which modulates host response to exogenous viral RNA, are more likely to have anti– West Nile virus antibodies than persons without this defect, suggesting that immune response function determines who becomes infected after exposure.29 Among persons who become infected, approximately 25% develop West Nile fever4 and 1 in 150 to 250 develops neuroinvasive disease.26,30 Risk factors for developing West Nile fever following infection are poorly defined. A follow-up study of asymptomatic, viremic blood donors indicated that increasing viral load and female sex, but not age, subsequently increased the risk of developing West Nile fever.4 A smaller follow-up study of viremic blood donors suggested that younger persons were more likely to develop West Nile fever.31 In contrast, advancing age profoundly increases the risk of neuroinvasive disease, particularly encephalitis.23,32 The risk may approach 1 in 50 among persons aged at least 65 years, a rate 16 times higher than that for persons aged 16 to 24 years.32 In addition, a history of cancer, diabetes, hypertension, alcohol abuse, renal disease, and chemokine receptor CCR5 deficiency as well as male sex may increase the risk of neuroinvasive disease.21,23,32–35 Persons infected through transplant of infected organs are at extreme risk of developing neuroinvasive disease27; however, conflicting data exist regarding risk among previous organ recipients infected via mosquito bite.36,37
Clinical Illness
The incubation period for clinical illness generally ranges from 2 to 14 days, but prolonged incubation periods of up to 21 days have been observed among immunocompromised patients.5,38 West Nile fever can range from a mild infirmity lasting a few days to a debilitating illness lasting weeks to months. Symptoms are of sudden onset and often include headache, malaise, fever, myalgia, chills, vomiting, rash, fatigue, and eye pain (Box 1).4 Fever may be low-grade or absent. A rash, which often appears around the time of defervescence, tends to be morbilliform, maculopapular, and nonpruritic, and predominates over the torso and extremities, sparing the palms and soles.39
Box 1. Characteristics of West Nile Fever.
Abrupt onset, usually July through September
Occurs in approximately 25% of those infected by mosquito bite
All ages affected, but no strong age predilection
Symptoms present in more than 50% of patients4:
- Headache, generalized weakness, morbilliform or maculopapular rash (often at time of defervescence), fever (often low grade), myalgia
Less common symptoms4:
- Joint pain, chills, painful eyes, vomiting or diarrhea, lymphadenopathy
Diagnosis most readily made by detection of West Nile virus– specific IgM antibody in serum, although a convalescent-phase sample maybe required because the antibody often is not present at the time of clinical presentation
Treatment is supportive
Illness duration days to weeks, generally with complete recovery, although prolonged fatigue may occur
West Nile meningitis, similar to that of other viral meningitides, is characterized by abrupt onset of fever and headache along with meningeal signs and photophobia. Headache may be severe, and associated gastrointestinal disturbance may result in dehydration (Box 2).40 West Nile encephalitis ranges in severity from a mild, self-limited confusional state to severe encephalopathy, coma, and death. Extrapyramidal disorders are frequently observed,41–44 and features of Parkinsonism may be seen.41,45 Patients with West Nile encephalitis frequently develop a coarse tremor, particularly in the upper extremities. The tremor tends to be postural and may have a kinetic component.41,43,44 Myoclonus, predominantly of the upper extremities and facial muscles, may occur and may be present during sleep. Cerebellar ataxia, increased intracranial pressure, cerebral edema, and seizures have been described but are uncommon.43,44,46
Box 2. Characteristics of West Nile Neuroinvasive Disease.
Abrupt onset, usually July through September
Occurs in less than 1% of those infected via mosquito bite
All ages affected, although very strong predilection with advancing age
Clinical Syndromes
- Meningitis characterized by clinical signs of meningeal inflammation, including nuchal rigidity, Kernig or Brudzinski sign, or photophobia or phonophobia
- Encephalitis characterized by depressed or altered level of consciousness, lethargy or personality change lasting more than 24 hours
- Acute flaccid paralysis characterized by acute onset of limb weakness with marked progression over 48 hours, which is usually asymmetric, are flexic or hyporeflexic, and without sensory abnormalities. Four-fifths of persons with acute flaccid paralysis occur in conjunction with encephalitis or meningitis
May be commonly accompanied by other symptoms and signs35:
- Nausea and vomiting, myalgia, chills, rash (less commonly reported than patients with West Nile fever), arthralgia, ataxia, visual disturbance, tremors, myoclonus, bulbar dysfunction (dysarthria, dysphagia)
Diagnosis most readily made by detection of West Nile virus–specific IgM antibody in cerebrospinal fluid or serum; in immunocompromised patients, development of IgM antibody may be delayed or absent, and nucleic acid amplification tests may be required
Cerebrospinal fluid generally shows normal glucose, elevated protein, pleocytosis (>5 leukocytes/µL)
Treatment is supportive
Illness duration weeks to months; long-term functional and cognitive difficulties common in patients with encephalitis, paralysis, or both
West Nile virus–associated paralysis most commonly results from destruction of the anterior horn cells of the spinal cord.47–49 Asymmetric weakness usually develops rapidly within the first 48 hours after symptom onset, although patients with extensive spinal cord involvement develop a more symmetric dense quadriplegia. Central facial weakness, frequently bilateral, may occur.48 Respiratory failure requiring emergent endotracheal intubation may result from diaphragmatic and intercostal muscle paralysis.47 Sensory loss or numbness is generally absent though some patients experience intense pain in the affected limbs just before or during the onset of weakness.47 Other causes of weakness associated with West Nile virus infection include Guillain-Barre syndrome and other demyelinating neuropathies, motor axonopathy, axonal polyneuropathy, involvement of ventral spinal roots, myasthenia gravis, and brachial plexopathies.49
Other manifestations described in the setting of West Nile virus infection include mulitfocal choroiditis, vitritis, myocarditis, pancreatitis, fulminant hepatitis, rhabdomyolysis, stiff-person syndrome, and autonomic instability.
Clinical Outcome
Full recovery is the norm for patients with uncomplicated West Nile fever or meningitis; however, initial symptoms, particularly extreme fatigue, may be prolonged.50 West Nile fever may precipitate death among persons of advanced age or with underlying medical conditions.51 Outcomes of West Nile encephalitis are variable and may not correlate with severity of initial illness. Patients hospitalized with West Nile virus encephalitis frequently require assistance with daily activities following acute care discharge42,52 and often report substantial functional and cognitive difficulties for up to a year following acute infection. Only 37% of patients in the 1999 New York City outbreak achieved full recovery at 1 year53 and 53% of patients in Idaho reported symptoms lasting at least 6 months, mostly fatigue, muscle aches, and difficulties with memory and concentration.54
Although some studies have documented neurocognitive deficits on standardized testing for as long as 1 year after acute illness,55,56 others have failed to confirm this finding.40 Nevertheless, self reported fatigue, somatic, and cognitive complaints lasting months or years are common among persons recovering from West Nile virus illness.53,57,58 Neuropsychiatric symptoms, including depression, anxiety, and apathy, have been reported.41,59 One investigator reported West Nile virus RNA in urine in patients up to 7 years following acute illness and implied an association with chronic renal failure60; however, 2 other studies failed to substantiate this finding.61,62
Among patients with acute flaccid paralysis due to poliomyelitis-like syndrome, roughly one-third recover strength to near baseline, one-third have some improvement, and one-third have little or no improvement.63 Little functional improvement has been documented 6 months after onset.
Case fatality rates among patients with neuroinvasive disease generally approximate 10%.23 Advanced age is the most important risk factor for death, ranging from 0.8 % among those aged less than 40 years to 17% among those aged at least 70 years.23 Encephalitis with severe muscle weakness, changes in the level of consciousness, diabetes, cardiovascular disease, hepatitis C virus infection, and immunosuppression are possible risk factors for death.1,23,34 Patients discharged from the hospital following acute West Nile virus illness experience a 2- to 3-fold increase in long-term, all-cause mortality compared with age-adjusted population norms, although not all of this increase may be attributable to West Nile virus.64
Diagnosis
Detection of IgM antibody in serum or cerebrospinal fluid (CSF) using the IgM antibody-capture enzyme-linked immunosorbent assay (MAC-ELISA) forms the cornerstone of West Nile virus diagnosis in most clinical settings. Because IgM antibody does not cross the blood-brain barrier, its presence in CSF indicates CNS infection. At least 90% of patients with encephalitis or meningitis have demonstrable IgM antibodies in CSF within 8 days of symptom onset. The West Nile virus–specific IgM antibody may not be detected initially in serum or plasma; 1 study showed that only 58% of patients with West Nile fever had a positive MAC-ELISA result at clinical presentation.65 Nevertheless, MAC-ELISA testing of acute- and convalescent- phase sera will provide definitive diagnosis. Testing for IgG antibodies has no utility in the acute clinical diagnostic setting.
Recent vaccination with yellow fever or Japanese encephalitis vaccines or recent infection with a related flavivirus (eg, St Louis encephalitis or dengue) may produce a positive West Nile virus–IgM antibody test result. The plaque-reduction neutralization test can help distinguish serologic cross-reactions among the flaviviruses, but the test is only available in reference laboratories. In 1 study, 17% of patients had demonstrable West Nile virus–specific IgM antibodies a year after initial infection; thus, persistent IgM antibody from a previous infection may be unrelated to current illness.66
Nucleic acid amplification testing has utility in certain clinical settings as an adjunct to MAC-ELISA. Among patients presenting with West Nile fever, 1 study showed that 45% of cases were identified with nucleic acid testing; 58% with serology, or 94% with a combined approach of these 2 methods.65 Nucleic acid amplification testing-may prove useful in immunocompromised patients when antibody development is delayed or absent and its use in blood donor screening in the United States and Canada has nearly eliminated the risk of West Nile virus transfusion transmission.
Total leukocyte counts in peripheral blood typically are normal or slightly elevated. Examination of CSF of patients with neuroinvasive disease shows normal glucose, elevated protein (generally <150 mg/dL) and moderate pleocytosis (generally <500 cells/µL) usually with a predominance of lymphocytes; however, neutrophils may predominate in early infection.67 Imaging studies are usually normal, but focal lesions in the pons, basil ganglia, thalamus, and anterior horns and enhancement of the leptomeninges, the periventricular areas, or both are occasionally seen. These lesions may appear hyperintenseonT2-weighted magnetic resonance and fluid-attenuated inversion recovery images.68
Treatment and Prevention
Treatment of West Nile virus infection remains supportive. Several investigated therapeutic approaches include immune γ-globulin, West Nile virus–specific neutralizing monoclonal antibodies, corticosteroids, ribavirin, interferon α-2b, and antisense oligomers.69,70 No study has documented efficacy, in part due to difficulty in recruiting sufficient numbers of patients. Case reports or uncontrolled clinical series suggesting efficacy should be interpreted with extreme caution due to West Nile virus’s highly variable clinical course.
Novaccine is licensed for humans. Despite 4 licensed equine vaccines and promising preliminary results from several phase 1 and 2 human vaccine candidates, phase 3 efficacy trials have not been attempted due the unknown market potential of a West Nile virus vaccine and logistical difficulties in conducting phase 3 clinical trials for this sporadic and widely dispersed disease.69 Preliminary analysis suggested that universal West Nile virus vaccine coverage would not be cost-effective71; however, the cost-effectiveness of vaccination of specific target groups such as elderly individuals has not yet been established. Because humans are dead-end hosts, a human vaccination program would not influence viral amplification in nature.
West Nile virus prevention relies in part on methods to reduce the numbers of West Nile virus–infected mosquitoes. Community-based mosquito control programs using integrated pest management principles proactively identify the sources of vector mosquitoes and use several methods such as elimination of breeding sites, larviciding, and targeted adult mosquito control to prevent adult mosquito populations from achieving levels that increase human infection risk.
When increasing human case incidence or surveillance of vector mosquito populations indicates an impending human epidemic, the immediate goal is to reduce rapidly the number of infected adult mosquitoes by widespread ultra-low volume application of organophosphate or synthetic pyrethroid insecticides. Organophosphates irreversibly block the enzyme acetylcholinesterase; pyrethroids open sodium channels of neuronal membranes, paralyzing the mosquito, and are usually combined with piperonyl butoxide, preventing the mosquito’s microsomal oxidase enzymes from metabolizing pyrethroids.
Although the efficacy of these control measures is difficult to measure, strategically timed early-season control of adult mosquitoes in the Coachella Valley of California using ultra-low volume insecticide applications decreased subsequent West Nile virus transmission.72 In addition, aerial ultra-low volume insecticide application decreased infected mosquito abundance and reduced human- case incidence during a West Nile virus outbreak in the Sacramento area.73 Human health risks associated with ultra-low volume organophosphate or synthetic pyrethroid use appear negligible, largely because the timing of application and low volume of pesticide used result in minimal human exposure.74,75
Insect repellent use has been associated with reduced West Nile virus risk.30 Unfortunately, few people report regular repellent use even during well-publicized outbreaks. Commercially available insect repellents containing DEET, IR3535, oil of lemon eucalyptus, and picaridin are registered by the US Environmental Protection Agency on the basis of their excellent safety profiles and proven efficacy in reducing or preventing mosquito biting. Many other commercially available unregistered products, such as those containing citronella oil, cedar oil, geraniumoil, peppermint oil, and soybeanoil, have unproven efficacy.
Future Perspectives
The resurgence of West Nile virus in 2012 after several years of decreasing incidence in the United States suggests that West Nile virus will continue to produce unpredictable local and regional outbreaks. These outbreaks are associated with considerable long- and short-term morbidity from West Nile virus neuroinvasive disease and West Nile fever, respectively. Thus, sustainable, community-based surveillance and vector management programs are critical, particularly in metropolitan areas with a history of West Nile virus and large human populations at risk. Community response plans must include provisions for rapidly implementing large-scale adult mosquito control interventions when surveillance indicates such measures are necessary. Further evaluation of target populations and cost-efficacy of a vaccine will help determine the need for continued human vaccine development. Practical pathways and paradigms for testing and approval of vaccines and therapeutics adapted to the sporadic outbreak nature of West Nile virus are required. These measures will not only help address the risks associated with West Nile virus but will add to our preparedness for all domestic and exotic mosquitoborne pathogens.
Acknowledgments
Additional Contributions: We thank Nicole Lindsey, MS, Division of Vector-Borne Diseases, CDC, for gathering the ArboNET surveillance data and creating the corresponding figures. She did not receive compensation beyond her regular salary for her contribution.
Footnotes
Author Contributions: Dr Petersen had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: All authors.
Acquisition of data: All authors.
Analysis and interpretation of data: Nasci, Petersen.
Drafting of the manuscript: All authors.
Critical revision of the manuscript for important intellectual content: All authors.
Administrative, technical, or material support: Brault, Petersen.
Study supervision: Petersen.
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
REFERENCES
- 1.Nash D, Mostashari F, Fine A, et al. The outbreak of West Nile virus infection in the New York City area in 1999. N Engl J Med. 2001;344(24):1807–1814. doi: 10.1056/NEJM200106143442401. [DOI] [PubMed] [Google Scholar]
- 2.Komar N, Langevin S, Hinten S, et al. Experimental infection of North American birds with the New York 1999 strain of West Nile virus. Emerg Infect Dis. 2003;9(3):311–322. doi: 10.3201/eid0903.020628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kilpatrick AM, Daszak P, Jones MJ, et al. Host heterogeneity dominates West Nile virus transmission. Proc Biol Sci. 2006;273(1599):2327–2333. doi: 10.1098/rspb.2006.3575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zou S, Foster GA, Dodd RY, et al. West Nile fever characteristics among viremic persons identified through blood donor screening. J Infect Dis. 2010;202(9):1354–1361. doi: 10.1086/656602. [DOI] [PubMed] [Google Scholar]
- 5.Pealer LN, Marfin AA, Petersen LR, et al. Transmission of West Nile virus through blood transfusion in the United States in 2002. N Engl J Med. 2003;349(13):1236–1245. doi: 10.1056/NEJMoa030969. [DOI] [PubMed] [Google Scholar]
- 6.Soverow JE, Wellenius GA, Fisman DN, Mittleman MA. Infectious disease in a warming world. Environ Health Perspect. 2009;117(7):1049–1052. doi: 10.1289/ehp.0800487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kilpatrick AM, Meola MA, Moudy RM, Kramer LD. Temperature, viral genetics, and the transmission of West Nile virus by Culex pipiens mosquitoes. PLoS Pathog. 2008;4(6):e1000092. doi: 10.1371/journal.ppat.1000092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reisen WK, Fang Y, Martinez VM. Effects of temperature on the transmission of West Nile virus by Culex tarsalis (Diptera: Culicidae) J Med Entomol. 2006;43(2):309–317. doi: 10.1603/0022-2585(2006)043[0309:EOTOTT]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 9.Bowden SE, Magori K, Drake JM. Regional differences in the association between land cover and West Nile virus disease incidence in humans in the United States. Am J Trop Med Hyg. 2011;84(2):234–238. doi: 10.4269/ajtmh.2011.10-0134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.DeGroote JP, Sugumaran R. National and regional associations between human West Nile virus incidence and demographic, landscape, and land use conditions in the coterminous United States. Vector Borne Zoonotic Dis. 2012;12(8):657–665. doi: 10.1089/vbz.2011.0786. [DOI] [PubMed] [Google Scholar]
- 11.Hartley DM, Barker CM, Le Menach A, et al. Effects of temperature on emergence and seasonality of West Nile virus in California. Am J Trop Med Hyg. 2012;86(5):884–894. doi: 10.4269/ajtmh.2012.11-0342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Landesman WJ, Allan BF, Langerhans RB, et al. Inter-annual associations between precipitation and human incidence of West Nile virus in the United States. Vector Borne Zoonotic Dis. 2007;7(3):337–343. doi: 10.1089/vbz.2006.0590. [DOI] [PubMed] [Google Scholar]
- 13.Ruiz MO, Walker ED, Foster ES, Haramis LD, Kitron UD. Association of West Nile virus illness and urban landscapes in Chicago and Detroit. Int J Health Geogr. 2007;6:10. doi: 10.1186/1476-072X-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reisen WK, Takahashi RM, Carroll BD, Quiring R. Delinquent mortgages, neglected swimming pools, and West Nile virus, California. Emerg Infect Dis. 2008;14(11):1747–1749. doi: 10.3201/eid1411.080719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.May FJ, Davis CT, Tesh RB, Barrett AD. Phylogeography of West Nile virus. J Virol. 2011;85(6):2964–2974. doi: 10.1128/JVI.01963-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bondre VP, Jadi RS, Mishra AC, Yergolkar PN, Arankalle VA. West Nile virus isolates from India. J Gen Virol. 2007;88(pt 3):875–884. doi: 10.1099/vir.0.82403-0. [DOI] [PubMed] [Google Scholar]
- 17.Lanciotti RS, Roehrig JT, Deubel V, et al. Origin of the West Nile virus responsible for an outbreak of encephalitis in the northeastern United States. Science. 1999;286(5448):2333–2337. doi: 10.1126/science.286.5448.2333. [DOI] [PubMed] [Google Scholar]
- 18.Davis CT, Ebel GD, Lanciotti RS, et al. Phylogenetic analysis of North American West Nile virus isolates, 2001–2004. Virology. 2005;342(2):252–265. doi: 10.1016/j.virol.2005.07.022. [DOI] [PubMed] [Google Scholar]
- 19.Lim PY, Behr MJ, Chadwick CM, Shi PY, Bernard KA. Keratinocytes are cell targets of West Nile virus in vivo. J Virol. 2011;85(10):5197–5201. doi: 10.1128/JVI.02692-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schneider BS, Higgs S. The enhancement of arbovirus transmission and disease by mosquito saliva is associated with modulation of the host immune response. Trans R Soc Trop Med Hyg. 2008;102(5):400–408. doi: 10.1016/j.trstmh.2008.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cho H, Diamond MS. Immune responses to West Nile virus infection in the central nervous system. Viruses. 2012;4(12):3812–3830. doi: 10.3390/v4123812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sambri V, Capobianchi M, Charrel R, et al. West Nile virus in Europe. Clin Microbiol Infect. 2013 doi: 10.1111/1469-0691.12211. [DOI] [PubMed] [Google Scholar]
- 23.Lindsey NP, Staples JE, Lehman JA, Fischer M. Surveillance for human West Nile virus disease. MMWR Surveill Summ. 2010;59(2):1–17. [PubMed] [Google Scholar]
- 24.Petersen LR, Hayes EB. West Nile virus in the Americas. Med Clin North Am. 2008;92(6):1307–1322. ix. doi: 10.1016/j.mcna.2008.07.004. [DOI] [PubMed] [Google Scholar]
- 25.Weber IB, Lindsey NP, Bunko-Patterson AM, et al. Completeness of West Nile virus testing in patients with meningitis and encephalitis during an outbreak in Arizona, USA. Epidemiol Infect. 2011;140(9):1632–1636. doi: 10.1017/S0950268811002494. [DOI] [PubMed] [Google Scholar]
- 26.Petersen LR, Carson PJ, Biggerstaff BJ, et al. Estimated cumulative incidence of West Nile virus infection in US adults, 1999–2010. Epidemiol Infect. 2012:1–5. doi: 10.1017/S0950268812001070. [published online ahead of print May 2012]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nett RJ, Kuehnert MJ, Ison MG, et al. Current practices and evaluation of screening solid organ donors for West Nile virus. Transpl Infect Dis. 2012;14(3):268–277. doi: 10.1111/j.1399-3062.2012.00743.x. [DOI] [PubMed] [Google Scholar]
- 28.O’Leary DR, Kuhn S, Kniss KL, et al. Birth outcomes following West Nile Virus infection of pregnant women in the United States, 2003–2004. Pediatrics. 2006;117(3):e537–e545. doi: 10.1542/peds.2005-2024. [DOI] [PubMed] [Google Scholar]
- 29.Lim JK, Lisco A, McDermott DH, et al. Genetic variation in OAS1 is a risk factor for initial infection with West Nile virus in man. PLoS Pathog. 2009;5(2):e1000321. doi: 10.1371/journal.ppat.1000321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mostashari F, Bunning ML, Kitsutani PT, et al. Epidemic West Nile encephalitis, 1999, New York. Lancet. 2001;358(9278):261–264. doi: 10.1016/S0140-6736(01)05480-0. [DOI] [PubMed] [Google Scholar]
- 31.Brown JA, Factor DL, Tkachenko N, et al. West Nile viremic blood donors and risk factors for subsequent West Nile fever. Vector Borne Zoonotic Dis. 2007;7(4):479–488. doi: 10.1089/vbz.2006.0611. [DOI] [PubMed] [Google Scholar]
- 32.Carson PJ, Borchardt SM, Custer B, et al. Neuroinvasive disease and West Nile virus infection, North Dakota, USA, 1999–2008. Emerg Infect Dis. 2012;18(4):684–686. doi: 10.3201/eid1804.111313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lindsey NP, Staples JE, Lehman JA, Fischer M. Medical risk factors for severe West Nile Virus disease, United States, 2008–2010. Am J Trop Med Hyg. 2012;87(1):179–184. doi: 10.4269/ajtmh.2012.12-0113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Murray K, Baraniuk S, Resnick M, et al. Risk factors for encephalitis and death from West Nile virus infection. Epidemiol Infect. 2006;134(6):1325–1332. doi: 10.1017/S0950268806006339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bode AV, Sejvar JJ, Pape WJ, et al. West Nile virus disease: a descriptive study of 228 patients hospitalized in a 4-county region of Colorado in 2003. Clin Infect Dis. 2006;42(9):1234–1240. doi: 10.1086/503038. [DOI] [PubMed] [Google Scholar]
- 36.Freifeld AG, Meza J, Schweitzer B, et al. Seroprevalence of West Nile virus infection in solid organ transplant recipients. Transpl Infect Dis. 2010;12(2):120–126. doi: 10.1111/j.1399-3062.2009.00464.x. [DOI] [PubMed] [Google Scholar]
- 37.Kumar D, Drebot MA, Wong SJ, et al. A seroprevalence study of West Nile virus infection in solid organ transplant recipients. Am J Transplant. 2004;4(11):1883–1888. doi: 10.1111/j.1600-6143.2004.00592.x. [DOI] [PubMed] [Google Scholar]
- 38.Rhee C, Eaton EF, Concepcion W, Blackburn BG. West Nile virus encephalitis acquired via liver transplantation and clinical response to intravenous immunoglobulin. Transpl Infect Dis. 2011;13(3):312–317. doi: 10.1111/j.1399-3062.2010.00595.x. [DOI] [PubMed] [Google Scholar]
- 39.Ferguson DD, Gershman K, LeBailly A, Petersen LR. Characteristics of the rash associated with West Nile virus fever. Clin Infect Dis. 2005;41(8):1204–1207. doi: 10.1086/444506. [DOI] [PubMed] [Google Scholar]
- 40.Sejvar JJ, Curns AT, Welburg L, et al. Neurocognitive and functional outcomes in persons recovering from West Nile virus illness. J Neuropsychol. 2008;2(pt 2):477–499. doi: 10.1348/174866407x218312. [DOI] [PubMed] [Google Scholar]
- 41.Sejvar JJ, Haddad MB, Tierney BC, et al. Neurologic manifestations and outcome of West Nile virus infection. JAMA. 2003;290(4):511–515. doi: 10.1001/jama.290.4.511. [DOI] [PubMed] [Google Scholar]
- 42.Pepperell C, Rau N, Krajden S, et al. West Nile virus infection in 2002. CMAJ. 2003;168(11):1399–1405. [PMC free article] [PubMed] [Google Scholar]
- 43.Burton JM, Kern RZ, Halliday W, et al. Neurological manifestations of West Nile virus infection. Can J Neurol Sci. 2004;31(2):185–193. doi: 10.1017/s0317167100053828. [DOI] [PubMed] [Google Scholar]
- 44.Sayao AL, Suchowersky O, Al-Khathaami A, et al. Calgary experience with West Nile virus neurological syndrome during the late summer of 2003. Can J Neurol Sci. 2004;31(2):194–203. doi: 10.1017/s031716710005383x. [DOI] [PubMed] [Google Scholar]
- 45.Robinson RL, Shahida S, Madan N, et al. Transient parkinsonism in West Nile virus encephalitis. Am J Med. 2003;115(3):252–253. doi: 10.1016/s0002-9343(03)00291-2. [DOI] [PubMed] [Google Scholar]
- 46.Kanagarajan K, Ganesh S, Alakhras M, et al. West Nile virus infection presenting as cerebellar ataxia and fever. South Med J. 2003;96(6):600–601. doi: 10.1097/01.SMJ.0000054912.04257.DC. [DOI] [PubMed] [Google Scholar]
- 47.Sejvar JJ, Bode AV, Marfin AA, et al. West Nile virus-associated flaccid paralysis. Emerg Infect Dis. 2005;11(7):1021–1027. doi: 10.3201/eid1107.040991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jeha LE, Sila CA, Lederman RJ, et al. West Nile virus infection. Neurology. 2003;61(1):55–59. doi: 10.1212/01.wnl.0000073617.08185.0a. [DOI] [PubMed] [Google Scholar]
- 49.Leis AA, Stokic DS. Neuromuscular manifestations of West Nile virus infection. Front Neurol. 2012;3:1–10. doi: 10.3389/fneur.2012.00037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Watson JT, Pertel PE, Jones RC, et al. Clinical characteristics and functional outcomes of West Nile fever. Ann Intern Med. 2004;141(5):360–365. doi: 10.7326/0003-4819-141-5-200409070-00010. [DOI] [PubMed] [Google Scholar]
- 51.Sejvar JJ, Lindsey NP, Campbell GL. Primary causes of death in reported cases of fatal West Nile fever, United States, 2002–2006. Vector Borne Zoonotic Dis. 2011;11(2):161–164. doi: 10.1089/vbz.2009.0086. [DOI] [PubMed] [Google Scholar]
- 52.Emig M, Apple DJ. Severe West Nile virus disease in healthy adults. Clin Infect Dis. 2004;38(2):289–292. doi: 10.1086/380458. [DOI] [PubMed] [Google Scholar]
- 53.Klee AL, Maidin B, Edwin B, et al. Long-term prognosis for clinical West Nile virus infection. Emerg Infect Dis. 2004;10(8):1405–1411. doi: 10.3201/eid1008.030879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cook RL, Xu X, Yablonsky EJ, et al. Demographic and clinical factors associated with persistent symptoms after West Nile virus infection. Am J Trop Med Hyg. 2010;83(5):1133–1136. doi: 10.4269/ajtmh.2010.09-0717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Haaland KY, Sadek J, Pergam S, et al. Mental status after West Nile virus infection. Emerg Infect Dis. 2006;12(8):1260–1262. doi: 10.3201/eid1208.060097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sadek JR, Pergam SA, Harrington JA, et al. Persistent neuropsychological impairment associated with West Nile virus infection. J Clin Exp Neuropsychol. 2010;32(1):81–87. doi: 10.1080/13803390902881918. [DOI] [PubMed] [Google Scholar]
- 57.Carson PJ, Konewko P, Wold KS, et al. Long-term clinical and neuropsychological outcomes of West Nile virus infection. Clin Infect Dis. 2006;43(6):723–730. doi: 10.1086/506939. [DOI] [PubMed] [Google Scholar]
- 58.Loeb M, Hanna S, Nicolle L, et al. Prognosis after West Nile virus infection. Ann Intern Med. 2008;149(4):232–241. doi: 10.7326/0003-4819-149-4-200808190-00004. [DOI] [PubMed] [Google Scholar]
- 59.Berg PJ, Smallfield S, Svien L. An investigation of depression and fatigue post West Nile virus infection. S D Med. 2010;63(4):127–129. 131–133. [PubMed] [Google Scholar]
- 60.Murray K, Walker C, Herrington E, et al. Persistent infection with West Nile virus years after initial infection. J Infect Dis. 2010;201(1):2–4. doi: 10.1086/648731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Baty SA, Gibney KB, Staples JE, et al. Evaluation for West Nile Virus (WNV) RNA in urine of patients within 5 months of WNV infection. J Infect Dis. 2012;205(9):1476–1477. doi: 10.1093/infdis/jis221. [DOI] [PubMed] [Google Scholar]
- 62.Gibney KB, Lanciotti RS, Sejvar JJ, et al. West Nile virus RNA not detected in urine of 40 people tested 6 years after acute West Nile virus disease. J Infect Dis. 2011;203(3):344–347. doi: 10.1093/infdis/jiq057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sejvar JJ, Bode AV, Marfin AA, et al. West Nile Virus-associated flaccid paralysis outcome. Emerg Infect Dis. 2006;12(3):514–516. doi: 10.3201/eid1203.050643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lindsey NP, Sejvar JJ, Bode AV, et al. Delayed mortality in a cohort of persons hospitalized with West Nile virus disease in Colorado in 2003. Vector Borne Zoonotic Dis. 2012;12(3):230–235. doi: 10.1089/vbz.2011.0721. [DOI] [PubMed] [Google Scholar]
- 65.Tilley PA, Fox JD, Jayaraman GC, Preiksaitis JK. Nucleic acid testing for West Nile virus RNA in plasma enhances rapid diagnosis of acute infection in symptomatic patients. J Infect Dis. 2006;193(10):1361–1364. doi: 10.1086/503577. [DOI] [PubMed] [Google Scholar]
- 66.Busch MP, Kleinman SH, Tobler LH, et al. Virus and antibody dynamics in acute West Nile virus infection. J Infect Dis. 2008;198(7):984–993. doi: 10.1086/591467. [DOI] [PubMed] [Google Scholar]
- 67.Tyler KL, Pape J, Goody RJ, Corkill M, Kleinschmidt-DeMasters BK. CSF findings in 250 patients with serologically confirmed West Nile virus meningitis and encephalitis. Neurology. 2006;66(3):361–365. doi: 10.1212/01.wnl.0000195890.70898.1f. [DOI] [PubMed] [Google Scholar]
- 68.Gyure KA. West Nile virus infections. J Neuropathol Exp Neurol. 2009;68(10):1053–1060. doi: 10.1097/NEN.0b013e3181b88114. [DOI] [PubMed] [Google Scholar]
- 69.Beasley DW. Vaccines and immunotherapeutics for the prevention and treatment of infections with West Nile virus. Immunotherapy. 2011;3(2):269–285. doi: 10.2217/imt.10.93. [DOI] [PubMed] [Google Scholar]
- 70.Diamond MS. Progress on the development of therapeutics against West Nile virus. Antiviral Res. 2009;83(3):214–227. doi: 10.1016/j.antiviral.2009.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zohrabian A, Hayes EB, Petersen LR. Cost-effectiveness of West Nile virus vaccination. Emerg Infect Dis. 2006;12(3):375–380. doi: 10.3201/eid1203.050782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lothrop HD, Lothrop BB, Gomsi DE, Reisen WK. Intensive early season adulticide applications decrease arbovirus transmission throughout the Coachella Valley, Riverside County, California. Vector Borne Zoonotic Dis. 2008;8(4):475–489. doi: 10.1089/vbz.2007.0238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Macedo PA, Schleier JJ, III, Reed M, et al. Evaluation of efficacy and human health risk of aerial ultra-low volume applications of pyrethrins and piperonyl butoxide for adult mosquito management in response to West Nile virus activity in Sacramento County, California. J Am Mosq Control Assoc. 2010;26(1):57–66. doi: 10.2987/09-5961.1. [DOI] [PubMed] [Google Scholar]
- 74.Centers for Disease Control and Prevention. Human exposure to mosquito-control pesticides. MMWR Morb Mortal Wkly Rep. 2005;54(21):529–532. [PubMed] [Google Scholar]
- 75.Duprey Z, Rivers S, Luber G, et al. Community aerial mosquito control and naled exposure. J Am Mosq Control Assoc. 2008;24(1):42–46. doi: 10.2987/5559.1. [DOI] [PubMed] [Google Scholar]