Efficacy of an Experiential, Dissonance-Based Smoking Intervention for College Students Delivered via the Internet (original) (raw)
. Author manuscript; available in PMC: 2015 Nov 10.
Published in final edited form as: J Consult Clin Psychol. 2013 May 13;81(5):810–820. doi: 10.1037/a0032952
Abstract
Objective
College represents a window of opportunity to reach the sizeable number of cigarette smokers who are vulnerable to lifelong smoking. The underutilization of typical cessation programs suggests the need for novel and more engaging approaches for reaching college smokers. The aim of the present study was to test the efficacy of a dissonance-enhancing, Web-based experiential intervention for increasing smoking cessation motivation and behavior.
Method
We used a 4-arm, randomized design to examine the efficacy of a Web-based, experiential smoking intervention (Web-Smoke). The control conditions included a didactic smoking intervention (Didactic), a group-based experiential intervention (Group), and a Web-based nutrition experiential intervention (Web-Nutrition). We recruited 341 college smokers. Primary outcomes were motivation to quit, assessed immediately postintervention, and smoking abstinence at 1 and 6 months following the intervention.
Results
As hypothesized, the Web-Smoke intervention was more effective than control groups in increasing motivation to quit. At 6-month follow-up, the Web-Smoke intervention produced higher rates of smoking cessation than the Web-Nutrition control intervention. Daily smoking moderated intervention outcomes. Among daily smokers, the Web-Smoke intervention produced greater abstinence rates than both the Web-Nutrition and Didactic control conditions.
Conclusion
Findings demonstrate the efficacy of a theory-based intervention delivered over the Internet for increasing motivation to quit and smoking abstinence among college smokers. The intervention has potential for translation and implementation as a secondary prevention strategy for college-aged smokers.
Keywords: smoking cessation, smoking cessation intervention, college student smokers, young adult smokers, Web-based intervention
Tobacco use among college students has been identified as a priority for tobacco control research (Orleans, 2007). This is underscored by a smoking rate among college students that is 66% higher than that of the general population (Centers for Disease Control and Prevention, 2009; Rigotti, Lee, & Wechsler, 2000), with young adults aged 18–24 representing the age group with the highest smoking prevalence in the United States (Freedman, Nelson, & Feldman, 2012). Consequently, the most recent Surgeon General’s report (U.S. Department of Health and Human Services, 2012) recommended multi-level interventions targeted at young adult smokers.
Given the high smoking prevalence among young adults, improvements in secondary prevention efforts (i.e., treatment of early-stage tobacco use and dependence) are essential, yet college student smoking cessation programs are poorly utilized (Wechsler, Kelley, Seibring, Kuo, & Rigotti, 2001). Young smokers are more likely to use unassisted strategies to quit smoking (e.g., decreasing the number of cigarettes smoked, exercising more) versus the assisted cessation methods recommended by Public Health Service guidelines (e.g., speaking with a health professional, using nicotine replacement therapy; Centers for Disease Control and Prevention, 2006; Fiore et al., 2008). This underutilization of typical cessation programs suggests the need for novel and more engaging approaches for reaching college smokers.
Prior research has identified several unique barriers to the efficacy of cessation programs among young adults (Backinger, Fagan, Matthews, & Grana, 2003). For example, college students are especially vulnerable to tactics used by tobacco companies to encourage lifelong addiction (Gilpin, White, Messer, & Pierce, 2007; Hammond, 2005; Sepe & Glantz, 2002; U.S. Department of Health and Human Services, 2012). These tactics include a strong presence of tobacco in bars and at social events and targeted marketing and packaging to appeal to young adults (Ling & Glantz, 2002; Sepe, Ling, & Glantz, 2002). Additional barriers include a social context with increased freedom (Colder et al., 2006) and a normative fallacy in which college smokers overestimate the proportion of peers who smoke (Cunningham & Selby, 2007). Furthermore, college smokers appear to feel invulnerable to the health effects of smoking (Prokhorov et al., 2003), supporting the need to present targeted youth-specific health risk information to this population.
Despite a clear need, systematic research aimed at developing smoking cessation interventions specifically for college student smokers has been slow (Backinger et al., 2003). Although some of the best programs have shown short-term efficacy (e.g., An et al., 2008; Harris et al., 2010), there is little evidence to date of long-term efficacy for college-based interventions.
Experiential Learning and Cognitive Dissonance Theory
The aim of the present study was to extend the recent research on college student smoking by creating and testing a novel intervention strategy that is designed to utilize an experiential/active learning approach and is rooted in the principles of the social psychological theory of cognitive dissonance. Interactive, experiential learning techniques have received considerable empirical support (Williams & Chinn, 2009), as experiential (or active) learning is more likely to produce lasting changes in attitudes and behavior than traditional didactic instruction (Miller, Wozniak, Rust, Miller, & Slezak, 1996; Onion & Bartzokas, 1998; Viswesvaran & Schmidt, 1992). Such approaches have proven efficacious for modifying college student drinking (Darkes & Goldman, 1993, 1998), as well as smoking attitudes and behavior (Simmons & Brandon, 2007; Simmons, Webb, & Brandon, 2004). These results may be in part due to greater emotional engagement evoked by experiential approaches (Cherney, 2008).
Importantly, experiential approaches may mitigate cognitive dissonance-reducing techniques employed by smokers. According to cognitive dissonance theory (Festinger, 1957), smokers experience discomfort caused by conflict between their behavior and the health messages they receive. Ways that smokers can lessen dissonance include misinterpreting or ignoring risk information or adding new cognitions that are congruent with the behavior (e.g., a smoker may adopt the belief that she is addicted and thus quitting is “out of her hands”; Jenks, 1992).
Consistent with the theory of cognitive dissonance, smokers endorse a greater number of rationalizations for smoking (e.g., smokers can totally reverse damage to their health by deciding to give up smoking) than nonsmokers or ex-smokers (Fotuhi et al., 2013; McMaster & Lee, 1991). Furthermore, college student smokers may deny being a “smoker,” despite having smoked in the past 30 days (Berg et al., 2009; Levinson et al., 2007). This denial may represent another example of a frequently utilized dissonance-reducing strategy.
Borrowing from a previously efficacious intervention for encouraging safe-sex practices in college students (Stone, Aronson, Crain, & Winslow, 1994), we initially applied an experiential framework with dissonance-enhancing techniques to college smokers in a group format (Simmons & Brandon, 2007). Participants in the experiential group (Exp-Smoke) engaged in interactive, videotaped group discussions on the short- and long-term consequences of smoking, thereby inducing an inconsistency between their smoking behavior and the attitudes that they were publicly reporting. This intervention was compared to two control groups: a standard didactic smoking intervention group (Standard) in which participants viewed a smoking cessation video and an experiential intervention on nutrition (Exp-Nutrition). As predicted, participants in the Exp-Smoke condition reported higher motivation to quit smoking immediately following the intervention than participants in both control conditions. One-month post-intervention, participants in the Exp-Smoke and Standard condition continued to report higher intentions to quit smoking than those in the Exp-Nutrition condition. However, moderator analyses indicated that the intervention was effective only for female smokers. Additionally, at 1-month follow-up, participants in the Exp-Smoke condition reported the highest rate of quitting or decreasing the amount smoked.
Despite these encouraging findings, the face-to-face group intervention was highly labor-intensive, limiting its potential implication and sustainability and, thus, its likely public health impact (Glasgow, Vogt, & Boles, 1999). However, these concerns may be attenuated via development of a Web-based modality for treatment delivery, which should be particularly amenable to young adults.
With dramatic increases in accessibility and use, especially among college students (An et al., 2006), the Internet is an attractive modality for disseminating and delivering health information. In addition to being cost-effective, a Web-based intervention can reach individuals who may not attend in-person groups. Initial attempts at employing Web-based intervention approaches for young adults have yielded promising results (e.g., O’Neill, Gillispie, & Slobin, 2000; Riley, Obermayer, & Jean-Mary, 2008), yet implications of these interventions are limited by the nature of the experimental designs used (e.g., nonrandomized, absence of long-term cessation outcomes).
Current Study
In the present study, our aim was to extend our recent research on a dissonance-based experiential intervention for college students by developing and testing a novel Web-delivered intervention strategy (Web-Smoke) that maintains the experiential/active learning approach, is grounded in the principles of cognitive dissonance theory, and delivers content specific to the college population. Using a randomized four-arm experimental design, college student participants were assigned to the intervention or one of three active control conditions designed to isolate three specific components of this approach: (a) the experiential dissonance-based treatment strategy (similar to Simmons & Brandon, 2007); (b) the smoking cessation content; and (c) the Web-based delivery channel. Thus, the control conditions, respectively, were (a) a traditional Web-based didactic smoking intervention (Didactic); (b) a Web-based experiential nutrition intervention (Web-Nutrition); and (c) a group-based experiential smoking intervention (Group).
The two primary dependent variables were motivation to quit smoking (measured immediately after the intervention) and smoking abstinence (measured 1 and 6 months after the intervention). We hypothesized that the Web-Smoke intervention would produce greater changes in readiness to quit and higher smoking abstinence than both the Didactic and the Web-Nutrition conditions. No predictions were made regarding outcome differences between the Group and Web-Smoke conditions. We also explored the role of potential mediators (e.g., risk perceptions, smoking-related outcome expectancies, cognitive dissonance, and smoking-related knowledge) and moderators (e.g., demographic and smoking status) on intervention outcomes.
Method
Participants
As depicted in Figure 1, 341 participants enrolled in the study, with the final sample composed of 331 college student smokers (44.1% female). Participants were recruited using a campus-wide questionnaire administered at the University of South Florida (distributed in classrooms and online). Prospective participants were then contacted by telephone to verify that they met eligibility criteria, including English speaking, 18–24 years of age, and smoking five or more cigarettes per week. To mitigate potential follow-up attrition rates, students in their final semester were excluded. All participants were randomly assigned to one of the four intervention conditions by an online random number generator.
Figure 1.
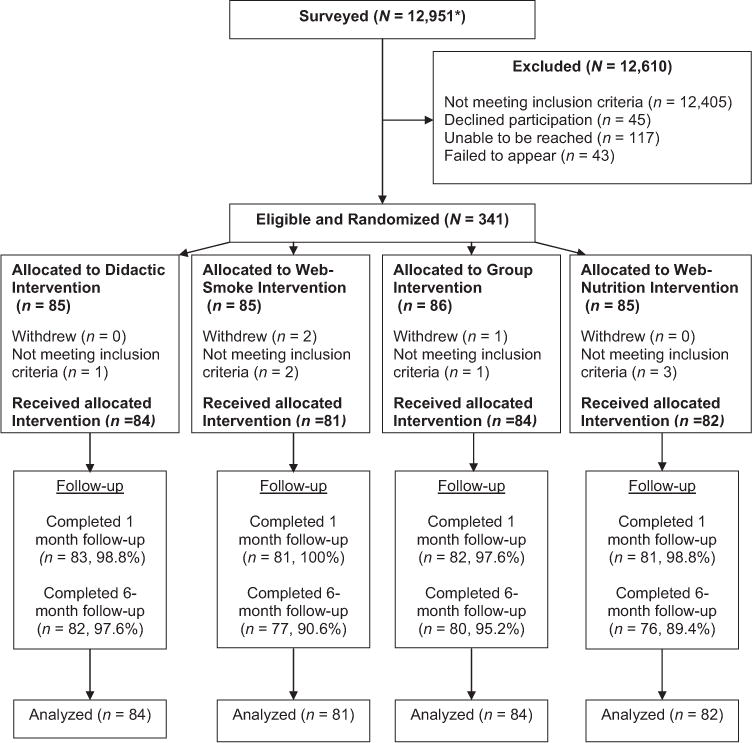
Flow chart of participants in the study. *Students could have been surveyed more than once due to surveys being completed in different classes.
Intervention Conditions
Web-based experiential smoking (Web-Smoke)
For the Web-Smoke condition, individual participants completed the Web-based intervention session in a private room in the university psychology building. Participants were not informed of the goal of the study. Instead, they were told that the purpose was to develop novel and more effective interventions promoting healthy lifestyle behaviors for high school seniors by designing a website with a series of health-related videos. After being told that high school seniors may be more receptive to messages delivered from peers rather than health professionals, participants in the Web-Smoke condition were asked to create a video message to be included on the website. The creation of a video message was an important component of this dissonance-enhancing intervention because the way individuals present themselves publicly (e.g., on video) can influence behavior (Wilson et al., 2002). In fact, prior research has demonstrated that health-related interventions that require participants to make a public commitment are more effective in changing behavior than educational (Wilson et al., 2002) or cognitive interventions aimed at modifying risk perceptions (Eitel & Friend, 1999; Leake, Friend, & Wadhwa, 1999). Research also suggests that attitude change is greater when individuals believe they chose to engage in the hypocritical behavior (Harmon-Jones, 2000; Zanna & Cooper, 2000). Thus, consistent with our previous study (Simmons & Brandon, 2007), a second method that we used for maximizing cognitive dissonance was to create the illusion of choice in selecting the topic of smoking. We did this by giving the participants the option of assisting in the creation of a smoking or nutrition-related website and using the following dialogue to guide them to choose the former:
We have completed all our health topics that we are covering except for smoking and nutrition. The nutrition website is almost complete, so if you could help us out by viewing the smoking website that would be really helpful, but the decision is totally up to you. Which website would you like to view?
All participants in this condition opted to view the smoking website. A website that we designed specifically for college students was then viewed on a laptop computer. The website included targeted content addressing common misconceptions (e.g., peer smoking rates, relative dangers of light vs. regular cigarettes) held by college smokers, acute and long-term consequences of smoking (e.g., health, physical appearance, reproductive effects, secondhand smoke, impact on sibling smoking status), tobacco industry marketing, cessation (e.g., nicotine withdrawal, benefits of quitting), and personal quotations (written by the study team to reinforce website content). Unique to this condition, however, the website also contained interactive components, such as brief content quizzes, a smoking widget (i.e., smoking cost calculator), and four “example” video messages that were made by confederates. These messages conveyed regrets over starting smoking (e.g., decreased sports performance, impact on relationships, increased smoking over time and associated cost, and difficulties quitting) and recommendations to never start or to quit as soon as possible.
After viewing the website, participants were asked to make their own video (using the laptop’s webcam) and to mention three things they thought were important from the website, as well as their own personal experience with smoking. Participants were also instructed to avoid saying anything positive about smoking. The mean duration of video messages was 2 min (range = 50 s to 6 min). To further enhance the public commitment and dissonance, the participants’ video messages were played back to them, so as to emphasize that their negative comments about smoking were inconsistent with their own smoking behavior.
Group-based experiential smoking (Group)
For the Group condition, procedures were identical to our previously demonstrated efficacious intervention (Simmons & Brandon, 2007). With the exception of participants being told that they were taking part in the creation of videos for high school seniors that would be presented in classrooms (rather than part of a website), all instructions were identical to those provided in the Web-Smoke intervention. The primary distinction between these two interventions was that group members (average group size was 5 students) were presented with the paper versions of the Web-Smoke website (i.e., identical content and visual presentation), and the video message was created during group discussion. These discussions were led by a master’s level clinical psychology doctoral student. Inclusion of this condition allowed us to isolate the effects of a Web-based channel of communication.
Web-based didactic smoking (Didactic)
For the Didactic condition, participants were asked to view a website and provide feedback on content and appearance. Participants then viewed a website identical to the Web-Smoke condition with respect to content and visual presentation; however, interactive features were absent (i.e., quizzes, widgets, and video messages) and they were not instructed to create a video message. This condition was included to test whether the Web-Smoke experiential intervention was more effective than a traditional didactic website that covers the same factual information. With this condition, it was possible to isolate the impact of the experiential, dissonance-enhancing component of the intervention.
Web-based experiential nutrition (Web-Nutrition)
For the Web-Nutrition condition, all instructions were identical to those provided in the Web-Smoke intervention; however, participants were guided to choose to view the nutrition website. Content, interactive features (e.g., nutrition widget, quizzes, video messages), and visual presentation of this website paralleled those shown in the Web-Smoke website. This condition was included to control for the effect of the smoking-related assessments, as well as for the non-specific effects of participating in an experiential intervention.
Measures
Demographic and smoking behavior questionnaire
This instrument was used to collect demographic data and to assess smoking behavior including nicotine dependence, as indexed by the Fagerström Test for Nicotine Dependence (FTND; Heatherton, Kozlowski, Frecker, & Fagerström, 1991). Due to the relatively brief smoking histories of college smokers, the Hooked On Nicotine Checklist (HONC) also was administered to detect symptoms of nicotine dependence in novice or light tobacco users (Wellman et al., 2005).
Primary outcome measures
Motivation to quit smoking
The Contemplation Ladder (Biener & Abrams, 1991) is a continuous measure of motivation to quit smoking using a 10-rung ladder. Participants circle the number on the ladder that best represents their status with respect to quitting smoking, ranging from no thoughts of quitting to taking action to quit. Higher responses on this measure have been found to predict smoking cessation (Abrams, Herzog, Emmons, & Linnan, 2000; Biener & Abrams, 1991). To provide an additional measure of smoking motivation, the Stages of Change Questionnaire (SOC) was also assessed (DiClemente et al., 1991). An algorithm was applied to this three-item measure to classify the quitting motivation status of smokers and exsmokers (i.e., precontemplator, contemplator, preparation, action, or maintenance).
Smoking status
The timeline follow-back method was used to recreate daily smoking behavior (Sobell & Sobell, 1992) and calculate 7-day point-prevalence rates at 1- and 6-month followups. Seven-day point prevalence is a traditionally used measure of smoking outcomes for the general smoking population; however, to capture sustained abstinence among the more intermittent smoking patterns typical of college students, 30-day point prevalence was also assessed for the 6-month follow-up. Self-reported abstinence was biochemically verified using breath carbon monoxide testing. Participants with carbon monoxide levels of < 10 ppm were classified as abstinent (SRNT Subcommittee on Biochemical Verification, 2002).
Process measures
Dissonance Thermometer (Devine, Tauer, Barron, Elliot, & Vance, 1999; Elliot & Devine, 1994)
A three-item affective discomfort factor (i.e., uncomfortable, uneasy, and bothered) was extracted from this 14-item measure and used to measure dissonance. This discomfort factor has been found to be susceptible to cognitive dissonance inductions (Devine et al., 1999) and has been shown to be reliable and predictive of intentions to quit smoking (Simmons et al., 2004).
Risk Perception Questionnaire (RPQ; Simmons et al., 2004)
Although there is no widely established assessment of smoking risk perceptions (see Weinstein, 1998), the RPQ was used because it has previously demonstrated differences across smoking cessation interventions (Simmons et al., 2004). The RPQ assessed participants’ perceptions of their overall likelihood of developing an illness related to their smoking behavior using a single item. The RPQ also assessed the likelihood of developing six specific smoking-related diseases (e.g., lung cancer, emphysema) using a 7-point Likert scale from 1 (extremely unlikely) to 7 (extremely likely). In addition to assessing individual risk perceptions, the RPQ assesses comparative risk estimates for the six smoking-related diseases (e.g., “compared to other smokers your same age and sex, how would you rate your risk of developing lung cancer?”).
Smoking Consequences Questionnaire
We used a 30-item brief version of the original Smoking Consequences Questionnaire-Adult (Brandon & Baker, 1991; Copeland, Brandon, & Quinn, 1995), which was validated for college smokers (Schleicher, Harris, Catley, Harrar, & Golbeck, 2008). Of the nine types of smoking-related outcome expectancies assessed, the Health Risk and Negative Social Impression subscales were examined as process measures.
Decisional Balance Questionnaire (Velicer, DiClemente, Prochaska, & Brandenburg, 1985)
This 24-item measure includes two scales labeled Pros of Smoking and Cons of Smoking. This measure was administered to capture participants’ negative and positive views toward smoking. These scales have been successful at predicting future smoking status (Velicer et al., 1985).
Test of Smoking Knowledge
To measure how well participants retained smoking information presented in the smoking intervention conditions, we administered a 10-item multiple-choice/true-false quiz developed specifically for this study.
Comparable diet/nutrition measures
The purpose of the study was presented under the guise of creating interventions to promote healthy lifestyle behaviors in general; thus, we also included several measures related to diet and nutrition. These measures were created to mirror several smoking-related measures (i.e., Contemplation Ladder, SOC, and RPQ) and were administered at comparable time points.
Procedure
Upon arrival, research assistants obtained informed consent and Health Insurance Portability and Accountability Act authorization. Participants then completed the baseline demographic, smoking history, smoking knowledge, and motivation to quit smoking measures. Next, participants took part in their specified intervention and completed the post-intervention motivation to quit assessment and the process measures. Regardless of the condition assignment, the session lasted approximately 60–90 min. Participants were compensated 25orreceivedextracreditpointsfortakingpartintheintervention.Oneand6monthsaftertheintervention,participantswerecontactedbytelephoneandadministeredthesmokingoutcomemeasures.Participantsreceived25 or received extra credit points for taking part in the intervention. One and 6 months after the intervention, participants were contacted by telephone and administered the smoking outcome measures. Participants received 25orreceivedextracreditpointsfortakingpartintheintervention.Oneand6monthsaftertheintervention,participantswerecontactedbytelephoneandadministeredthesmokingoutcomemeasures.Participantsreceived20 for each follow-up completed. To increase retention, a 25bonuspaymentwasprovidedifbothfollow−upswerecompleted.Thosereportingsmokingabstinenceattheir6−monthfollow−upwereinvitedtoattendabriefin−personassessmentsessionforbiochemicalverificationandcompensatedanadditional25 bonus payment was provided if both follow-ups were completed. Those reporting smoking abstinence at their 6-month follow-up were invited to attend a brief in-person assessment session for biochemical verification and compensated an additional 25bonuspaymentwasprovidedifbothfollow−upswerecompleted.Thosereportingsmokingabstinenceattheir6−monthfollow−upwereinvitedtoattendabriefin−personassessmentsessionforbiochemicalverificationandcompensatedanadditional20. Upon completion of the study, all participants were debriefed. All study procedures were approved by the University of South Florida’s Institutional Review Board.
Statistical Analysis
A priori power analyses demonstrated that our target sample size of 340 (85 per condition) would provide a power of .80 to detect small to medium sized effects when examining our primary dependent variables, with a two-tailed alpha level of .05 (Cohen, 1988).
Prior to the main analyses, chi-square and analyses of variance (ANOVAs) were used to examine potential group differences among baseline measures for a check of the randomization procedures. Primary analyses were conducted comparing the Web-Smoke condition to each of the three control conditions (Web-Nutrition, Didactic, Group). Post-intervention differences between conditions with respect to intention to quit smoking and several process measures were compared between conditions using ANOVA or analysis of covariance (ANCOVA), controlling for pre-intervention scores when available. To determine whether abstinence rates differed between the Web-Smoke versus Group, Didactic, and Web-Nutrition groups, we conducted logistic regressions to examine smoking abstinence at the 1- and 6-month follow-up points. For the 1-month follow-up, we present 7-day point prevalence outcomes; for the 6-month follow-up, we present 7-day and 30-day point prevalence abstinence. Analyses were conducted using an “intent-to-treat” approach, with missing outcome data imputed as smoking. However, analyses of only complete data sets produced an identical pattern of results. Mediation analyses were completed using bootstrapping techniques as outlined by Hayes (Hayes, 2009), with an indirect effect evidenced as statistically significant when the 95% CI did not overlap with 0. For each comparison, mediators were tested individually and then all statistically significant mediators were included in a multiple mediator model. Moderator analyses were conducted by testing interactions between potential moderator variables and the intervention condition.
Results
Baseline Characteristics and Randomization Check
Baseline means are presented in Table 1. On average, participants were 20.45 years of age (SD = 1.97). The majority of participants were Caucasian (81.3%), with 3.0% identifying as African American, 5.1% as Asian American/Oriental/Pacific Islander, .6% as Native American, and 10.0% as other. Of the sample, 11.8% were Hispanic or Latino (see Table 1). The sample was minimally dependent on tobacco (FTND M = 1.61; SD = 1.96) and indicated some loss of autonomy over smoking behavior (HONC M = 5.82; SD = 2.54). No significant differences were found across the four experimental conditions for demographic or smoking-related variables.
Table 1.
Baseline Characteristics, With Means (and Standard Deviations) or Percentages
| Variable | Condition | Total (N = 331) | |||
|---|---|---|---|---|---|
| Web–Smoke (n = 81) | Group (n = 84) | Didactic (n = 84) | Web–Nutrition (n = 82) | ||
| Demographic variables | |||||
| Gender (% female) | 45.7 | 34.5 | 44.0 | 52.4 | 44.1 |
| Race (% Caucasian) | 85.2 | 82.1 | 78.6 | 79.3 | 81.3 |
| Ethnicity (% Hispanic) | 9.2 | 10.7 | 12.2 | 15.2 | 11.8 |
| Age | 20.42 (2.05) | 20.35 (1.90) | 20.64 (1.88) | 20.77 (2.05) | 20.54 (1.97) |
| Smoking-related variables | |||||
| Daily smoker (%) | 74.1 | 67.9 | 72.6 | 69.1 | 70.9 |
| Days smoked in last 30 days | 26.22 (7.34) | 24.57 (7.16) | 25.73 (6.29) | 25.64 (6.86) | 25.54 (6.91) |
| Cigarettes per week | 46.44 (39.95) | 47.86 (46.59) | 44.76 (37.61) | 46.63 (38.03) | 46.43 (40.57) |
| FTND (0–10) | 1.85 (2.20) | 1.62 (1.98) | 1.58 (1.81) | 1.40 (1.86) | 1.61 (1.96) |
| HONC (0–10) | 5.68 (2.56) | 6.10 (2.48) | 5.62 (2.57) | 5.88 (2.56) | 5.82 (2.54) |
| Age 1st smoked | 15.66 (2.00) | 15.45 (3.20) | 15.58 (2.28) | 15.24 (2.55) | 15.48 (2.55) |
| CL (0–10) | 5.33 (3.02) | 6.14 (2.97) | 5.99 (2.37) | 5.45 (2.70) | 5.73 (2.78) |
Intervention Effects on Motivation to Quit and Process Measures
We examined post-intervention differences between conditions on motivation to quit smoking, smoking knowledge, dissonance, risk perceptions, and pros and cons of smoking (presented in Table 2). As predicted, immediately following the intervention, participants in the Web-Smoke condition reported higher intentions to quit smoking than participants in the Web-Nutrition, F(1, 160) = 33.61, p < .001 and Didactic conditions, F(1, 162) = 9.28, p = .003. Additionally, although an advantage was not hypothesized for the Web-Smoke compared to the Group condition, intentions to quit also were higher in the Web-Smoke than in the Group based experiential condition, F(1, 162) = 17.55, p < .001.
Table 2.
Process Variables; Web-Smoke Versus Comparison Conditions
| Variable | Condition | _F/_χ2 | |||
|---|---|---|---|---|---|
| Web–Smoke | Group | Didactic | Web–Nutrition | ||
| Smoking knowledge | 81.98 (1.38)a**, c** | 75.36 (1.36) | 79.90 (1.39) | 54.96 (1.41) | 77.06*** |
| Smoking pros (DBI) | 2.72 (.10) | 2.87 (.10) | 2.69 (.10) | 2.73 (.10) | 0.62 |
| Smoking cons (DBI) | 3.15 (.11)c* | 2.93 (.11) | 2.76 (.11) | 2.65 (.11) | 3.85* |
| Negative social impression (SCQ) | 5.77 (.21)b* | 5.21 (.21) | 4.96 (.21) | 5.22 (.21) | 2.61* |
| Health risk (SCQ) | 8.31 (.13)c* | 8.21 (.12) | 8.17 (.12) | 7.78 (.13) | 3.41* |
| Personal risk (RPQ) | 5.18 (.16)b*, c** | 4.70 (.16) | 4.54 (.16) | 4.34 (.16) | 4.80** |
| Comparative risk (RPQ) | 4.68 (.16)b*, c*** | 4.13 (.16) | 4.06 (.16) | 3.58 (.16) | 8.00*** |
| Overall risk (single item) | 5.41 (.15) | 5.28 (.15) | 5.19 (.14) | 5.05 (.15) | 1.09 |
| Dissonance | 3.08 (.16)c*** | 2.52 (.15) | 2.75 (.15) | 1.91 (.15) | 10.24*** |
| Contemplation Ladder | 7.53 (.16)a***, b**, c*** | 6.44 (.16) | 6.77 (.16) | 6.15 (.16) | 13.89*** |
| Stage of change (% advanced) | 46.2 | 41.5 | 43.9 | 37.5 | 1.38 |
Differences were observed among groups on several process variables. Smoking knowledge, perceived risk indices, endorsement of smoking-related cons, and dissonance were elevated for Web-Smoke, relative to the Web-Nutrition control condition. Participants in the Web-Smoke condition also reported higher risk perceptions (both personal and comparison risk estimates) and ratings of negative social impression, when compared to the Didactic control condition. Finally, the Web-Smoke participants performed better on the smoking knowledge quiz than participants in the Group control condition. In summary, the Web-Smoke condition demonstrated superiority over the other comparison conditions on several process measures.
Mediators of Contemplation Ladder Group Differences
Next, we evaluated whether a number of putative mediators would help to explain the relationship between group assignment and Contemplation Ladder scores as an outcome. To isolate mediation effects, we conducted a separate set of mediation analyses pairing the Web-Smoke condition against each of the control conditions. Tested mediators were Pros and Cons of Smoking scales from the Decisional Balance Scale, dissonance scores, smoking knowledge, risk perception items, and the health risk and social impression scale from the Smoking Consequences Questionnaire.
For the Web-Smoke versus Web-Nutrition group comparison, the only statistically significant mediator was the personal risk estimate from the RPQ (indirect effect = .16; 95% CI = .03–.39). For the Web-Smoke versus Didactic comparison, four of the variables were statistically significant mediators at the univariate-level, including the Cons of Smoking scale (indirect effect = .13; 95% CI = .03–.31) and the personal risk, comparative risk, and overall risk from the RPQ (indirect effect = .16; 95% CI = .04–.34; indirect effect = .14; 95% CI = .02–.34; indirect effect = .14; 95% CI = .03–.36, respectively). When entered in a multiple mediation model, only the Cons of Smoking remained a statistically significant mediator (indirect effect = .10; 95% CI = .01–.27). Finally, for the Web-Smoke versus Group comparison, the Cons of Smoking and the dissonance scores were significant mediators at the univariate level and both remained significant in the multivariate analyses (indirect effect = .07; 95% CI = .01–.24; indirect effect = .15; 95% CI = .04–.35, respectively).
Smoking Abstinence by Intervention Group
Figure 2A depicts 7-day and 30-day point prevalence abstinence rates.
Figure 2.
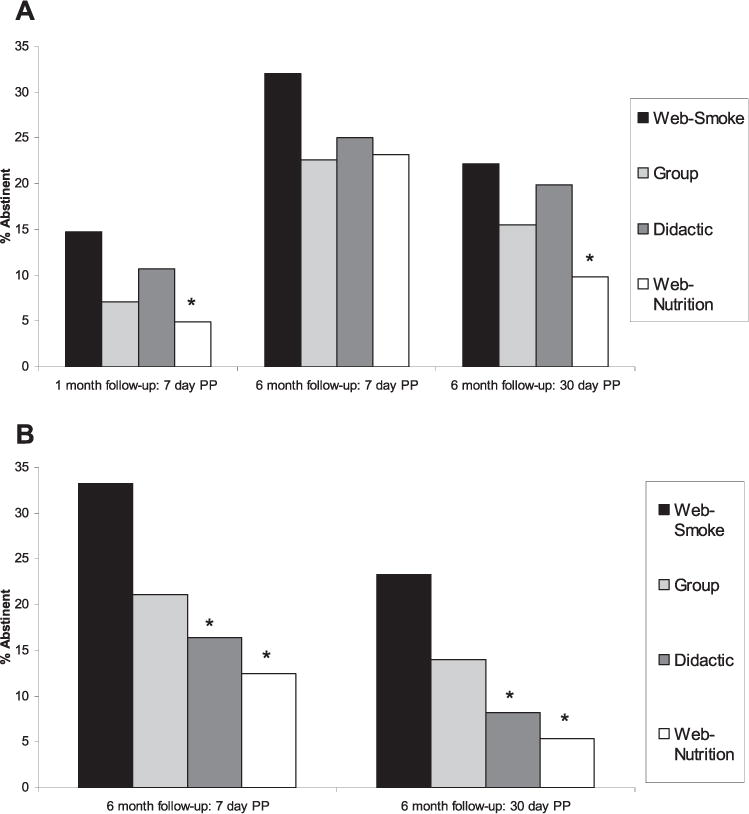
Smoking abstinence rates at 1 month and 6 months for total sample (A) and at 6 months for daily smokers only (B). PP = point prevalence. *Comparison group was significantly different from the Web-Smoke intervention at p < .05.
One-month follow-up
As hypothesized, 1 month after the intervention, the Web-Smoke group had significantly higher abstinence rates (7-day point-prevalence) than the Web-Nutrition group (14.8% vs. 4.9%; OR = 3.39, 95% CI = 1.05 – 11.00, p = .042). However, abstinence rates did not differ between the Web-Smoke and either the Group intervention (14.8% vs. 7.1%) or the Didactic intervention (14.8% vs. 10.7%; OR = 2.26, 95% CI = .81 – 6.35, p = .121; OR = 1.45, 95% CI = .58 – 3.65, p = .431, respectively).
Six-month follow-up
Six months after the intervention, 7-day point prevalence abstinence rates for the Web-Smoke condition (32.1%) did not differ from any of the control conditions (Group: 22.6%, OR = 1.62, 95% CI = .81 – 3.23, p = .173; Didactic: 25.0%, OR = 1.42, 95% CI = .72 – 2.80, p = .313; Web-Nutrition: 23.2%, OR = 1.57, 95% CI = .78 – 3.14, p = .204). However, with 30-day point prevalence criteria, the Web-Smoke condition had higher abstinence rates (22.2%) than the Web-Nutrition group (9.8%; OR = 2.64, 95% CI = 1.08 – 6.49, p = .034) and did not differ from Group (15.5%) or Didactic (17.9%) interventions (OR = 1.56, 95% CI = .71 – 3.44, p = .270; OR = 1.31, 95% CI = .61 – 2.83, p = .484, respectively).
Moderation Analyses of Abstinence Outcomes
Analyses revealed that baseline smoking status (daily vs. non-daily) smoking moderated intervention outcomes at the 6-month follow-up point. A significant interaction was observed between daily smoking status and condition for the Web-Smoke versus Web-Nutrition (OR = 8.08, 95% CI = 1.70 – 38.56, p = .009) and Web-Smoke versus Didactic (OR = 5.84, 95% CI = 1.28 – 26.74, p = .02) comparisons for the 7-day point prevalence intervention outcomes. This interaction was also significant for comparisons between Web-Smoke and Didactic using 30-day point prevalence-rates (OR = 11.14, 95% CI = 1.94 – 64.10, p = .007) and trended toward significance for comparisons between Web-Smoke and Web-Nutrition (OR = 5.71, 95% CI = .80–40.72, p = .08).
Follow-up analyses revealed that 30-day point prevalence estimates for the comparison between Web-Smoke and Didactic or Web-Nutrition showed significant intervention effects among daily smokers (OR = 3.41, 95% CI = 1.14 – 10.17, p = .028; OR = 5.38, 95% CI = 1.45 – 19.89, p = .012) but not among those who did not smoke everyday (OR = .31, 95% CI = .08–1.20, p = .089; OR = .94, 95% CI = .22 – 4.07, p = .935, respectively). Similar results were observed for the 7-day point prevalence estimates (see Figure 2B).
Mediation Analyses of 6-Month Abstinence Outcomes for Daily Smokers
Finally, we sought to examine several potential mediators of the effects of intervention among daily smokers. For these analyses, we focused on 30-day point prevalence at 6 months, as it can be considered the most meaningful and robust outcome variable. Potential mediators tested were dissonance, smoking knowledge, risk perception, smoking outcome expectancies (i.e., health risk and negative social impression), pros and cons of smoking, and motivation to quit smoking as measured by the SOC and contemplation ladder.
Several mediators were observed within the daily smoker subgroup. At the univariate level, contemplation ladder scores (controlling for baseline) and health risk expectancies mediated differential abstinence rates observed between Web-Smoke and Web-Nutrition conditions (indirect effect = .29; 95% CI = .02–.85; indirect effect = .79; 95% CI = −2.38 to −.21, respectively). When these variables were tested via multiple mediation, only health risk expectancies remained significant (indirect effect = .31; 95% CI = −.97 – −.03). Differential abstinence rates for the Web-Smoke versus Didactic comparison was mediated by the Cons of Smoking and Negative Social Impression expectancies (indirect effect = −.36; 95% CI = −.95 to −.06; indirect effect = −.25; 95% CI = −.75 to −.02, respectively), but only at the univariate level.
Discussion
The purpose of this study was to convert a face-to-face experiential, dissonance-enhancing smoking intervention into a Web-based modality and to test the efficacy of this intervention strategy for increasing both motivation to quit smoking and abstinence through 6 months. Immediately after the intervention, participants’ intentions to quit smoking were highest in the Web-Smoke condition relative to the Web-Nutrition experiential condition, and the content-matched Didactic control. Unexpectedly, Web-Smoke participants also reported higher motivation to quit than participants in the previously validated experiential Group condition. Thus, the results support the use of this Web-based experiential smoking intervention strategy for increasing motivation to quit smoking among college students.
For cessation outcomes, the Web-Smoke intervention produced greater abstinence rates than the Web-Nutrition intervention at both the 1-month and 6-month follow-up time points. Abstinence rates did not differ between the Web-Smoke and Didactic or Group interventions, across the full sample. However, pre-intervention smoking status (daily vs. non-daily smoking) was found to moderate intervention outcomes. Specifically, the hypothesized pattern of results was observed only among daily smokers; participants in the Web-Smoke condition had higher 6-month abstinence rates than those in the Web-Nutrition or Didactic conditions. No significant intervention effects on abstinence outcomes were observed for non-daily smokers.
College student smokers are a heterogeneous group composed of both daily and non-daily smokers. Daily smokers, for whom the Web-Smoke intervention was most efficacious, obviously represent the highest risk group, with an alarming 87% of students continuing to smoke throughout college (Wetter et al., 2004). Although moderation by smoking status was not an a priori hypothesis, previous studies have reported differences between daily and non-daily smokers that may help to explain this finding. Non-daily smokers are less likely to consider themselves as “smokers” or view themselves as addicted and are more likely to minimize the health effects of smoking (Ames et al., 2009; Berg et al., 2009). The experiential Web-Smoke intervention strategy relies on the students viewing themselves as smokers and conveying what they did not like about smoking from that perspective. Among non-daily smokers, this process might have been hindered by their reluctance to consider themselves smokers. This suggests the possibility of adapting the Web-Smoke intervention for non-daily smokers by first encouraging them to acknowledge that they are smokers. Our findings, together with the emerging data on differences between non-daily and daily college smokers, support the development of targeted interventions for college smokers based on smoking patterns.
Outcome differences upon abstinence rates were not found between the Web-Smoke and Group conditions. We did not predict differences between these conditions because they contained equivalent content and experiential activity, differing only in their delivery modality. Nevertheless, despite similar outcomes, the Web-Smoke intervention has advantages of cost, ease of dissemination, convenience, and sustainability that rate it higher in terms of potential public health impact (Glasgow et al., 1999).
To understand the mechanisms related to differential intervention outcomes for daily smokers, we assessed several theoretically-derived process measures. An examination of mediating variables suggests that the Web-Smoke intervention increased immediate motivation to smoke primarily by raising the salience and impact of the health risks and other disadvantages of smoking. It is not surprising that an experiential intervention in which smokers had to actively consider the consequences of their smoking and record a personal testimonial would produce such an effect. However, the affective dissonance scale did not emerge as a robust mediator, although it did mediate the difference between the Web-Smoke and Group conditions. This was somewhat surprising, as these were the two conditions that targeted cognitive dissonance. Perhaps the Web’s potential for greater viewership of the testimonial video produced stronger dissonance than the Group-based video.
For the 6-month abstinence outcomes, health risks and cons of smoking remained as mediators. Contemplation Ladder scores also emerged as a mediator of the outcome difference between Web-Smoke and Web-Nutrition, suggesting perhaps that the early salience of health risk information was assimilating into a more general motivation and intention to quit smoking. Interestingly, the comparison between Web-Smoke and the Didactic control was also mediated by expectancies related to the negative social impression caused by smoking. This would seem to also reflect the impact of the video-recorded public testimonial. In summary, the identified mediators may provide targets for strengthening the intervention in the future.
Strengths and Limitations
Findings from the current study extend the results from our previous experiential group intervention (Simmons & Brandon, 2007) by demonstrating the efficacy of a Web-based experiential modality that produced comparable or, with some outcomes, superior results. Strengths of this study include a rigorous experimental design with appropriate control conditions and the development of an acceptable, accessible, and potentially cost-effective intervention strategy. Indeed, an obvious strength of a Web-based approach is the implementation and dissemination potential. However, a few key limitations in the current intervention strategy and research design must be addressed before fully realizing the dissemination potential of this intervention. First, the intervention was not presented as a smoking cessation program and participants were not seeking assistance to quit smoking. Rather, students participated in creating the video under the guise that it would be used on a website to prevent high school students from smoking. A future study is needed to investigate the interest and participation in a Web-Smoke intervention if presented as a brief intervention for the secondary prevention of smoking. Indeed, the current format may be critical for engaging college smokers, particularly smokers unmotivated to quit. If so, the intervention might be implemented as a requirement in college orientation or health courses or using prizes/contests to encourage students to visit the website and develop the anti-smoking videos.
Second, the Web-Smoke intervention condition was conducted in a laboratory setting. Although this laboratory setting was necessary for initial validation of this intervention strategy, a future study should be conducted in a more ecologically valid setting with students visiting the website outside of the laboratory. Moving the intervention outside of the laboratory setting presents the challenge of motivating students to view the website and may require efforts such as those described above. Prior research conducted by An et al. (2008) has demonstrated the feasibility and acceptability of sending weekly e-mail invitations/reminders and using incentives as viable strategies to encourage college students to view an intervention website.
Finally, participants in the current study came from a single 4-year research university; therefore, it is unknown how generalizable our results are to other young adult populations such as those attending 2-year community colleges or young adults who are not in college—groups that are more likely to be daily smokers (Berg et al., 2011). Thus, our intervention may actually be well-suited for these populations.
In summary, findings suggest that Web-Smoke, a Web-based experiential intervention, was efficacious in increasing motivation to quit smoking among college smokers and increasing smoking abstinence rates among daily college smokers. The next step is to continue the process of translating the intervention into a format that can be easily delivered to the college student population.
Acknowledgments
This research was supported by the James and Esther King Biomedical Research Program, Florida Department of Health. We wish to thank Riddhi Patel, Lauren Meltzer, Atalie Ashley-Gordon, and Lauren Bello for their contributions to the study.
Contributor Information
Vani Nath Simmons, Department of Health Outcomes and Behavior, H. Lee Moffitt Cancer Center, Tampa, Florida, and Departments of Psychology and Oncologic Sciences, University of South Florida.
Bryan W. Heckman, Department of Psychology, University of South Florida, and Department of Health Outcomes and Behavior, H. Lee Moffitt Cancer Center
Angelina C. Fink, Department of Health Outcomes and Behavior, H. Lee Moffitt Cancer Center, and College of Public Health, University of South Florida
Brent J. Small, School of Aging Studies, University of South Florida, and Department of Health Outcomes and Behavior, H. Lee Moffitt Cancer Center
Thomas H. Brandon, Department of Health Outcomes and Behavior, H. Lee Moffitt Cancer Center, and Departments of Psychology and Oncologic Sciences, University of South Florida
References
- Abrams DB, Herzog TA, Emmons KM, Linnan L. Stages of change versus addiction: A replication and extension. Nicotine & Tobacco Research. 2000;2:223–229. doi: 10.1080/14622200050147484. [DOI] [PubMed] [Google Scholar]
- Ames S, Stevens S, Schroeder D, Werch C, Carlson J, Kiros GE, Offord K. Nondaily tobacco use among Black and White college undergraduates: A comparison of nondaily versus daily tobacco users. Addiction Research & Theory. 2009;17:191–204. doi: 10.1080/16066350802318366. [DOI] [Google Scholar]
- An LC, Klatt C, Perry CL, Lein EB, Hennrikus DJ, Pallonen UE, Ehlinger EP. The RealU online cessation intervention for college smokers: A randomized controlled trial. Preventive Medicine. 2008;47:194–199. doi: 10.1016/j.ypmed.2008.04.011. [DOI] [PubMed] [Google Scholar]
- An LC, Perry CL, Lein EB, Klatt C, Farley DM, Bliss RL, Ehlinger EP. Strategies for increasing adherence to an online smoking cessation intervention for college students. Nicotine & Tobacco Research. 2006;8(Suppl 1):S7–S12. doi: 10.1080/14622200601039881. [DOI] [PubMed] [Google Scholar]
- Backinger CL, Fagan P, Matthews E, Grana R. Adolescent and young adult tobacco prevention and cessation: Current status and future directions. Tobacco Control. 2003;12(Suppl 4):iv46–iv53. doi: 10.1136/tc.12.suppl_4.iv46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg CJ, An LC, Thomas JL, Lust KA, Sanem JR, Swan DW, Ahluwalia JS. Smoking patterns, attitudes and motives: Unique characteristics among 2-year versus 4-year college students. Health Education Research. 2011;26:614–623. doi: 10.1093/her/cyr017. [DOI] [PubMed] [Google Scholar]
- Berg CJ, Lust KA, Sanem JR, Kirch MA, Rudie M, Ehlinger E, An LC. Smoker self-identification versus recent smoking among college students. American Journal of Preventive Medicine. 2009;36:333–336. doi: 10.1016/j.amepre.2008.11.010. [DOI] [PubMed] [Google Scholar]
- Biener L, Abrams DB. The Contemplation Ladder: Validation of a measure of readiness to consider smoking cessation. Health Psychology. 1991;10:360–365. doi: 10.1037/0278-6133.10.5.360. [DOI] [PubMed] [Google Scholar]
- Brandon TH, Baker TB. The Smoking Consequences Questionnaire: The subjective expected utility of smoking in college students. Psychological Assessment. 1991;3:484–491. doi: 10.1037/1040-3590.3.3.484. [DOI] [Google Scholar]
- Centers for Disease Control and Prevention. Tobacco use among adults—United States, 2005. Morbidity and Mortality Weekly Report. 2006;55:1145–1148. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Cigarette smoking among adults and trends in smoking cessation. Morbidity and Mortality Weekly Report. 2009;58:1227–1232. [PubMed] [Google Scholar]
- Cherney ID. The effects of active learning on students’ memories for course content. Active Learning in Higher Education. 2008;9:152–171. doi: 10.1177/1469787408090841. [DOI] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Colder CR, Lloyd-Richardson EE, Flaherty BP, Hedeker D, Segawa E, Flay BR, The Tobacco Etiology Research Network The natural history of college smoking: Trajectories of daily smoking during the freshman year. Addictive Behaviors. 2006;31:2212–2222. doi: 10.1016/j.addbeh.2006.02.011. [DOI] [PubMed] [Google Scholar]
- Copeland AL, Brandon TH, Quinn EP. The Smoking Consequences Questionnaire–Adult: Measurement of smoking outcome expectancies of experienced smokers. Psychological Assessment. 1995;7:484–494. doi: 10.1037/1040-3590.7.4.484. [DOI] [Google Scholar]
- Cunningham JA, Selby PL. Implications of the normative fallacy in young adult smokers aged 19–24 years. American Journal of Public Health. 2007;97:1399–1400. doi: 10.2105/AJPH.2006.101071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darkes J, Goldman MS. Expectancy challenge and drinking reduction: Experimental evidence for a mediational process. Journal of Consulting and Clinical Psychology. 1993;61:344–353. doi: 10.1037/0022-006X.61.2.344. [DOI] [PubMed] [Google Scholar]
- Darkes J, Goldman MS. Expectancy challenge and drinking reduction: Process and structure in the alcohol expectancy network. Experimental and Clinical Psychopharmacology. 1998;6:64–76. doi: 10.1037/1064-1297.6.1.64. [DOI] [PubMed] [Google Scholar]
- Devine PG, Tauer JM, Barron KE, Elliot AJ, Vance KM. Moving beyond attitude change in the study of dissonance-related processes. Washington, DC: American Psychological Association; 1999. [DOI] [Google Scholar]
- DiClemente CC, Prochaska JO, Fairhurst SK, Velicer WF, Velasquez MM, Rossi JS. The process of smoking cessation: An analysis of precontemplation, contemplation, and preparation stages of change. Journal of Consulting and Clinical Psychology. 1991;59:295–304. doi: 10.1037/0022-006X.59.2.295. [DOI] [PubMed] [Google Scholar]
- Eitel P, Friend R. Reducing denial and sexual risk behaviors in college students: A comparison of a cognitive and a motivational approach. Annals of Behavioral Medicine. 1999;21:12–19. doi: 10.1007/BF02895028. [DOI] [PubMed] [Google Scholar]
- Elliot AJ, Devine PG. On the motivational nature of cognitive dissonance: Dissonance as psychological discomfort. Journal of Personality and Social Psychology. 1994;67:382–394. doi: 10.1037/0022-3514.67.3.382. [DOI] [Google Scholar]
- Festinger L. A theory of cognitive dissonance. Evanston, IL: Row; 1957. [Google Scholar]
- Fiore MC, Jaen CR, Baker TB, Bailey WC, Benowitz NL, Curry SJ. Treating tobacco use and dependence: 2008 update Clinical practice guideline. Rockville, MD: U.S. Department of Health and Human Services; 2008. [Google Scholar]
- Fotuhi O, Fong GT, Zanna MP, Borland R, Yong HH, Cummings KM. Patterns of cognitive dissonance-reducing beliefs among smokers: A longitudinal analysis from the International Tobacco Control (ITC) Four Country Survey. Tobacco Control. 2013;22:52–58. doi: 10.1136/tobaccocontrol-2011-050139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman KS, Nelson NM, Feldman LL. Smoking initiation among young adults in the United States and Canada, 1998–2010: A systematic review. Preventing Chronic Disease. 2012;9:E05. [PMC free article] [PubMed] [Google Scholar]
- Gilpin EA, White MM, Messer K, Pierce JP. Receptivity to tobacco advertising and promotions among young adolescents as a predictor of established smoking in young adulthood. American Journal of Public Health. 2007;97:1489–1495. doi: 10.2105/AJPH.2005.070359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: The RE-AIM framework. American Journal of Public Health. 1999;89:1322–1327. doi: 10.2105/AJPH.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammond D. Smoking behaviour among young adults: Beyond youth prevention. Tobacco Control. 2005;14:181–185. doi: 10.1136/tc.2004.009621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harmon-Jones E. Cognitive dissonance and experienced negative affect: Evidence that dissonance increases experienced negative affect even in the absence of aversive consequences. Personality and Social Psychology Bulletin. 2000;26:1490–1501. doi: 10.1177/01461672002612004. [DOI] [Google Scholar]
- Harris KJ, Catley D, Good GE, Cronk NJ, Harrar S, Williams KB. Motivational interviewing for smoking cessation in college students: A group randomized controlled trial. Preventive Medicine. 2010;51:387–393. doi: 10.1016/j.ypmed.2010.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF. Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs. 2009;76:408–420. doi: 10.1080/03637750903310360. [DOI] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström Test for Nicotine Dependence: A revision of the Fagerström Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Jenks RJ. Attitudes, perceptions, and risk-taking behaviors of smokers, ex-smokers, and nonsmokers. The Journal of Social Psychology. 1992;132:569–575. doi: 10.1080/00224545.1992.9713895. [DOI] [PubMed] [Google Scholar]
- Leake R, Friend R, Wadhwa N. Improving adjustment to chronic illness through strategic self-presentation: An experimental study on a renal dialysis unit. Health Psychology. 1999;18:54–62. doi: 10.1037/0278-6133.18.1.54. [DOI] [PubMed] [Google Scholar]
- Levinson AH, Campo S, Gascoigne J, Jolly O, Zakharyan A, Tran ZV. Smoking, but not smokers: Identity among college students who smoke cigarettes. Nicotine & Tobacco Research. 2007;9:845–852. doi: 10.1080/14622200701484987. [DOI] [PubMed] [Google Scholar]
- Ling PM, Glantz SA. Why and how the tobacco industry sells cigarettes to young adults: Evidence from industry documents. American Journal of Public Health. 2002;92:908–916. doi: 10.2105/AJPH.92.6.908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMaster C, Lee C. Cognitive dissonance in tobacco smokers. Addictive Behaviors. 1991;16:349–353. doi: 10.1016/0306-4603(91)90028-G. [DOI] [PubMed] [Google Scholar]
- Miller RL, Wozniak WJ, Rust MR, Miller BR, Slezak J. Counterattitudinal advocacy as a means of enhancing instructional effectiveness: How to teach students what they do not want to know. Teaching of Psychology. 1996;23:215–219. doi: 10.1207/s15328023top2304_2. [DOI] [Google Scholar]
- O’Neill HK, Gillispie MA, Slobin K. Stages of change and smoking cessation: A computer-administered intervention program for young adults. American Journal of Health Promotion. 2000;15:93–96. doi: 10.4278/0890-1171-15.2.93. [DOI] [PubMed] [Google Scholar]
- Onion CW, Bartzokas CA. Changing attitudes to infection management in primary care: A controlled trial of active versus passive guideline implementation strategies. Family Practice. 1998;15:99–104. doi: 10.1093/fampra/15.2.99. [DOI] [PubMed] [Google Scholar]
- Orleans CT. Helping young adult smokers quit: The time is now. American Journal of Public Health. 2007;97:1353. doi: 10.2105/AJPH.2007.117374. [DOI] [Google Scholar]
- Prokhorov AV, Warneke C, de Moor C, Emmons KM, Mullin Jones M, Rosenblum C, Gritz ER. Self-reported health status, health vulnerability, and smoking behavior in college students: Implications for intervention. Nicotine & Tobacco Research. 2003;5:545–552. doi: 10.1080/1462220031000118649. [DOI] [PubMed] [Google Scholar]
- Rigotti NA, Lee JE, Wechsler H. US college students’ use of tobacco products: Results of a national survey. Journal of the American Medical Association. 2000;284:699–705. doi: 10.1001/jama.284.6.699. [DOI] [PubMed] [Google Scholar]
- Riley W, Obermayer J, Jean-Mary J. Internet and mobile phone text messaging intervention for college smokers. Journal of American College Health. 2008;57:245–248. doi: 10.3200/JACH.57.2.245-248. [DOI] [PubMed] [Google Scholar]
- Schleicher HE, Harris KJ, Catley D, Harrar SW, Golbeck AL. Examination of a brief smoking consequences questionnaire for college students. Nicotine & Tobacco Research. 2008;10:1503–1509. doi: 10.1080/14622200802323175. [DOI] [PubMed] [Google Scholar]
- Sepe E, Glantz SA. Bar and club tobacco promotions in the alternative press: Targeting young adults. American Journal of Public Health. 2002;92:75–78. doi: 10.2105/AJPH.92.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sepe E, Ling PM, Glantz SA. Smooth moves: Bar and nightclub tobacco promotions that target young adults. American Journal of Public Health. 2002;92:414–419. doi: 10.2105/AJPH.92.3.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmons VN, Brandon TH. Secondary smoking prevention in a university setting: A randomized comparison of an experiential, theory-based intervention and a standard didactic intervention for increasing cessation motivation. Health Psychology. 2007;26:268–277. doi: 10.1037/0278-6133.26.3.268. [DOI] [PubMed] [Google Scholar]
- Simmons VN, Webb MS, Brandon TH. College-student smoking: An initial test of an experiential dissonance-enhancing intervention. Addictive Behaviors. 2004;29:1129–1136. doi: 10.1016/j.addbeh.2004.03.005. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline follow-back: A technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen JP, editors. Measuring alcohol consumption: Psychosocial and biochemical methods. Totowa, NJ: Humana Press; 1992. pp. 41–72. [DOI] [Google Scholar]
- SRNT Subcommittee on Biochemical Verification. Biochemical verification of tobacco use and cessation. Nicotine & Tobacco Research. 2002;4:149–159. doi: 10.1080/14622200210123581. [DOI] [PubMed] [Google Scholar]
- Stone J, Aronson E, Crain AL, Winslow MP. Inducing hypocrisy as a means of encouraging young adults to use condoms. Personality and Social Psychology Bulletin. 1994;20:116–128. doi: 10.1177/0146167294201012. [DOI] [Google Scholar]
- US Department of Health and Human Services. Preventing tobacco use among youth and young adults: A report of the Surgeon General, 2012. Atlanta, GA: Centers for Disease Control and Prevention; 2012. [PubMed] [Google Scholar]
- Velicer WF, DiClemente CC, Prochaska JO, Brandenburg N. Decisional balance measure for assessing and predicting smoking status. Journal of Personality and Social Psychology. 1985;48:1279–1289. doi: 10.1037/0022-3514.48.5.1279. [DOI] [PubMed] [Google Scholar]
- Viswesvaran C, Schmidt FL. A meta-analytic comparison of the effectiveness of smoking cessation methods. Journal of Applied Psychology. 1992;77:554–561. doi: 10.1037/0021-9010.77.4.554. [DOI] [PubMed] [Google Scholar]
- Wechsler H, Kelley K, Seibring M, Kuo M, Rigotti NA. College smoking policies and smoking cessation programs: Results of a survey of college health center directors. Journal of American College Health. 2001;49:205–212. doi: 10.1080/07448480109596305. [DOI] [PubMed] [Google Scholar]
- Weinstein ND. Accuracy of smokers’ risk perceptions. Annals of Behavioral Medicine. 1998;20:135–140. doi: 10.1007/BF02884459. [DOI] [PubMed] [Google Scholar]
- Wellman RJ, DiFranza JR, Savageau JA, Godiwala S, Friedman K, Hazelton J. Measuring adults’ loss of autonomy over nicotine use: The Hooked on Nicotine Checklist. Nicotine & Tobacco Research. 2005;7:157–161. doi: 10.1080/14622200412331328394. [DOI] [PubMed] [Google Scholar]
- Wetter DW, Kenford SL, Welsch SK, Smith SS, Fouladi RT, Fiore MC, Baker TB. Prevalence and predictors of transitions in smoking behavior among college students. Health Psychology. 2004;23:168–177. doi: 10.1037/0278-6133.23.2.168. [DOI] [PubMed] [Google Scholar]
- Williams J, Chinn SJ. Using Web 2.0 to support the active learning experience. Journal of Information Systems Education. 2009;20:165–174. [Google Scholar]
- Wilson DK, Friend R, Teasley N, Green S, Reaves IL, Sica DA. Motivational versus social cognitive interventions for promoting fruit and vegetable intake and physical activity in African American adolescents. Annals of Behavioral Medicine. 2002;24:310–319. doi: 10.1207/S15324796ABM2404_07. [DOI] [PubMed] [Google Scholar]
- Zanna MP, Cooper J. Dissonance and the pill: An attribution approach to studying the arousal properties of dissonance. In: Higgins ET, Kruglanski AW, editors. Motivational science: Social and personality perspectives. Philadelphia, PA: Psychology Press; 2000. pp. 306–312. [DOI] [PubMed] [Google Scholar]