Effect of Selected Yogic Practices on Pain and Disability in Patients with Lumbar Spondylitis (original) (raw)
Abstract
Aim:
The study was designed to find the effect of selected yogic practices on lumbar spondylitis.
Materials and Methods:
This was a prospective, randomized study without a control trial. A total of 172 participants with lumbar spondylitis (age 21–79 years) from the outpatient department (OPD) of neurosurgery, AIIMS, Bhubaneswar, were randomly assigned to receive yoga therapy. The module of selected yogic practices consisted of pawanamuktasana series 1 (loosening and strengthening), asana, pranayama, and relaxation techniques Yoga Nidra.
Statistics Analysis:
Within groups, comparison was done by paired _t_-test, and between groups, ANOVA test was carried out to determine the significant difference among the various groups under study. Correlation regression analysis was done to measure the degree of linear relationship between pre- and post-study for various groups.
Results:
Significant differences were observed with yoga therapy in instant relieve practice group, in short-term practice group, and in long-term practice group (LTPG) with better results in LTPG.
Conclusion:
Selected yoga therapy has got the better result in management of pain in lumbar spondylitis.
Keywords: Experimental group, lumbar spondylitis, Roland–Morris back pain questionnaire, yogic practice
Introduction
Backache, which was known as an ancient curse, is now known as a modern international epidemic. Lumbar disc disease is an important cause of low backache so much so that people have perceptions that all low backaches are due to disc prolapse.[1] According to one study, almost 80% of people in modern industrial society will experience back pain at some time in their life. It is common in women who have had several pregnancies.[2] The usual symptoms of back disorders are pain, stiffness and deformity in the back, and pain paresthesia or weakness in the lower limbs.[3] Minorities with low back pain (LBP) receive less patient education.[4] Back injury is the leading and most expensive cause of workers' compensation claims.[5,6] Back pain is one of the most common complaints seen in physician's offices. A survey done by the CDC in 2010 reported that back symptoms were the primary reason for 1.3% of office visits in the United States, and spinal disorders were responsible for 3.1% of diagnoses in outpatient clinics.[7] A 2012 systematic review by Hoy et al. estimated that the global point prevalence of activity-limiting LBP lasting more than a day was 12% and 1 month was 23%.[8] The etiology of back pain is not fully researched and understood; however, the psychological, psychosocial/occupational, and physical factors are considered as strong causative factors.[9]
Medical expenditures for LBP in minorities are 30% lower than for Whites' back surgery.[10] Patient satisfaction with the effectiveness of conventional LBP treatment is relatively low.[11] Spinal pain is a condition for which often - complementary therapies are being used.[12] Despite the ubiquity of back pain, it is one of the conditions that modern medicine does not treat well, partly due to imprecision of diagnosis and relative ineffectiveness of most conventional treatments. Although yoga may have the potential to ameliorate both chronic and acute pain in general, the mechanisms by which this is affected remain hypothetical.[12] Nevertheless, today, yoga is quite commonly used as complementary treatment for spinal pain.[13] There are many muscles in the low back including larger powerful muscles such as iliopsoas and erector spinae, as well as smaller muscles such as multifidi, semispinalis, and rotators. These muscles along with the external and internal oblique and rectus and transverse abdominis are responsible for the stability of the spine as well as the spine's basic movements. It is important for these muscles to be not only strong but also flexible. If these muscles are weak or deconditioned, they cannot efficiently stabilize the spine, leading to instability and injury. Muscular imbalances in strength and tone exert uneven forces on their bony or facial attachments, contributing to poor body mechanics, injury and pain. There is positive evidence of yoga therapy for the treatment and management of chronic low back pain. Thus, there is a substantial need for research to identify more helpful therapies. The art and science of yoga have infinite possibilities for providing answers to most health problems, troubling modern humankind. However, we often misunderstand this science and want it to be a miracle pill. A pill that we take only once and want all the problems to vanish into thin air. Yoga is a holistic science and must be learned and practiced with a holistic view.
Reviews and meta-analyses[14,15] and practice guidelines from the American Pain Society and the American College of Physicians[12] support yoga as an evidence-based treatment for LBP with at least moderate benefit. However, no studies to date have compared yoga's effectiveness to physical therapy (PT), the most commonly nonpharmacologic reimbursable treatment that physicians recommend.[16]
Materials and Methods
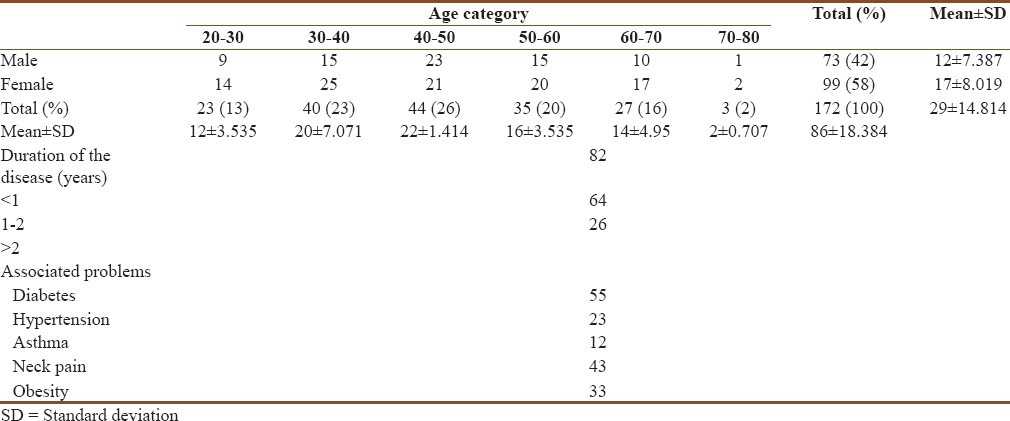
A total of 200 patients with lumbar spondylitis from OPD of neurosurgery were recruited for the study [Figure 1]. A sample size of 172 was randomly selected for the study in the age group between 21 and 79 years (29 ± 14.814) of both genders [Table 1]. All patients were referred from the Department of Neurosurgery to yoga therapy center, in the Department of AYUSH, AIIMS, Bhubaneswar.
Figure 1.
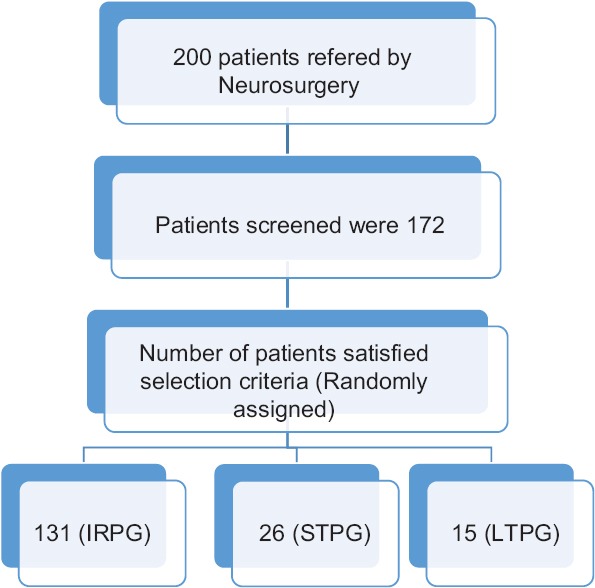
Trial profile
Table 1.
Demographic profile (age sex distribution of the respondents, _n_=172)
Inclusion criteria
- Patients having persistent pain for 6 months prior to recruitment
- Patients having moderate to severe pain while walking or standing
- People having diabetes, hypertension, and bronchial asthma
- The disease was diagnosed through chief complaint from patients along with X-ray and magnetic resonance imaging report.
Exclusion criteria
Persons suffering from trauma, tuberculous, arthritis, and major psychiatric problem were excluded from the study.
Design of the study
This was a prospective, randomized study on patients having lumbar spondylitis but without a control group. Patients attending the OPD of neurosurgery, AIIMS, Bhubaneswar, of who were diagnosed with lumbar spondylitis and satisfied the inclusion criteria were recruited for the study. After the initial screening for selection criteria, they were assigned to the yoga OPD for experimental group. The experimental group was divided into three subgroups such as instant relieve practice group (IRPG), short-term practice group (STPG), and long-term practice group (LTPG).
Experimental group
The patients of experimental group were divided into three subgroups such as IRPG, STPG, and LTPG. The sample size of IRPG was 131; STPG and LTPG were 26 and 15, respectively. The IRPG was practiced only 1 h of the very day after referred from the Department of Neurosurgery whereas the STPG and LTPG were practiced for 15 days and 1 month in a regular basis in the morning time from 9 AM to 10 AM, except Sunday.
Intervention for yoga group
At the yoga therapy center, 1 h of selected yoga therapy was given as a daily routine practice to the patients suffering from lumbar spondylitis. These practices include pawanamuktasana series 1 (joint exercises), backward bending series, pranayama nadisodhana and bhramari, and short relaxation Yoga Nidra.
Yoga module for lumbar spondylitis
Selected yogic practices were made to practice by the patient for 60 min for all groups such as IRPG, STPG, and LTPG in different intervals 1 h, 2 weeks, and 2 months at the yoga therapy center. This included the various practices [Table 2].
Table 2.
Yoga module for lumbar spondylitis
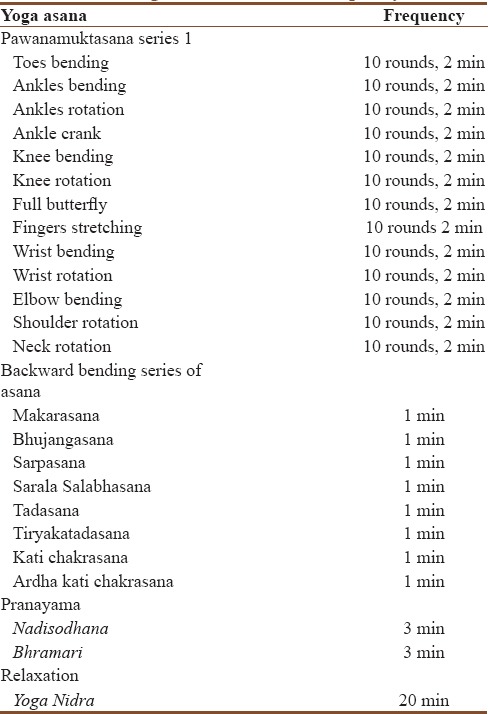
The concept used to develop a specific module of selected yogic approach of yoga therapy for lumbar spondylitis was taken from the authentic book called Asana Pranayama Mudra Bandha and Yoga Nidra developed by Swami Satyananda Saraswati from Bihar School of Yoga, which highlights a holistic approach for integral health at physical, mental, emotional, and spiritual levels.[17,18] Yoga is defined as a systematic approach or process of gaining control over the mind.[19] Yoga offers a holistic solution. The first-level handling is at the body level to use techniques of relaxation. Simple asanas provide mastery over different groups of muscles by increasing the elasticity of the muscles fibers and releasing tensions and stresses.[20] The daily routine included a 1 h practice of asana, pranayama, and relaxation practice such as Yoga Nidra.
Asana
Asanas are any physical posture featured by effortless maintenance in the final posture, i.e., sthira sukham asanam.
- Pawanamuktasana series 1 (loosening and strengthening practices): This group of asanas concerned with loosening of the joints of the body. By the practice of these asanas, all joints, muscles, and ligaments come to play and it gives gentle massage to eliminate the energy blockages in the joints
- Backward bending series: This series tones up the back muscles, followed by relaxation
- Standing and stretching asana: This series of asana gives a good stretch to the entire body including back muscles.
Pranayama
Pranayama means prolongation of breath to increase the efficiency of lungs capacity. It also promotes autonomic balance through mastery over the mind.[20]
Relaxation
Yoga Nidra: It is a relaxation technique developed by Swami Satyananda Saraswati of Bihar School of Yoga. It is a powerful technique of inducing complete physical, mental, and emotional relaxation including a qualitative sleep.[21]
Outcome variables
The Roland–Morris back pain and Disability Questionnaire (RMDQ) was used to assess the pain and disability after the intervention of yoga on different groups of experimental group. The questionnaire contains 24 questions aimed at assessments of the status of participant's pain and disability.[22]
Statistical methods
The data were analyzed using SPSS version 16.0 (IBM, Chicago, IL, USA) package under Windows XP environment. The baseline values of the three groups were checked for normal distribution by Kolmogorov–Smirnov one-sample test. Paired _t_-test was used to test the significant effect of yoga therapy on reduction of pain and disability in each study group (IRPG, STPG, and LTPG). ANOVA test was conducted for accessing the significant difference within and between the groups. The correlation and regression analysis were done to determine degree of linear relationship between yoga therapy and pain disability.
Results
Table 3a and b shows the results within the experimental group of IRPG, STPG, and LTPG.
Table 3a.
Analysis of variance (prescore)
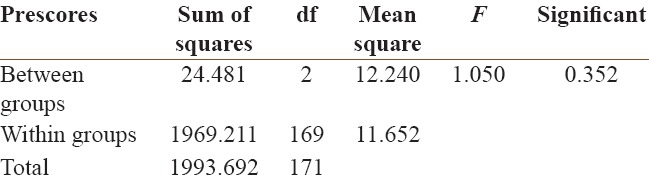
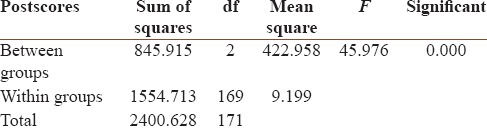
Table 3b.
Analysis of variance (postscore)
Pain
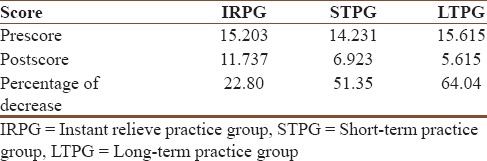
This measures all activities of 24 items in the questionnaire. In IRPG, mean ± standard deviation (SD) of the pain (pre-post) was 3.333 ± 2.967 and P < 0.001. Moreover, the prescore of pain was 15.203 and postscore was 11.737; the reduction of pain was 22.80% after 1 h practice of yoga therapy. This shows the reduction of pain and disability. In STPG, mean ± SD of the pain (pre-post) was 7.308 ± 1.995 and P < 0.001. Moreover, the prescore of pain was 14.231 and postscore was 6.923; the reduction of pain was 51.35% after 15 days practice of yoga therapy, which shows the reduction of pain and disability in the experimental group. Similarly, in LTPG, mean ± SD of the pain (pre-post) was 10.00 ± 1.915 and P < 0.001. Moreover, the prescore of pain was 15.615 and postscore was 5.615; the reduction of pain was 64.04% after 1 month practice of yoga therapy, which indicates the reduction of pain in this group [Table 4a and b].
Table 4a.
Experimental groups

Table 4b.
Percentage change
Analysis of variance (among all three IRPG, STPG and LTPG) did not contribute outcome (F = 1.050 which is insignificant at 5% level of significance) before yoga therapy. After yoga therapy, there is significant difference among the three groups where F = 45.976 which is highly significant at 5% level of significance. Multiple comparisons of the postscores after yoga therapy of the three groups by least square difference method reveal that there exists a high significant difference in mean between IRPG and STPG (mean difference [MD] = 4.81377*) and also between IRPG and LTPG (MD = 6.12146*). However, there exists no significant difference in mean postscores between STPG and LTPG (MD = 1.30769).
Regression analysis and model formulation
A linear regression analysis was conducted to determine the relationship between the effect of selected yogic practices on pain and disability in lumbar spondylitis. The result showed that there exists a high degree of linear association between pre- and post-score between yogic practices and pain and disability in IRPG (r = 0.897). They were positively correlated with each other [Table 3c].
Table 3c.
Pre- and post-correlations for each variable
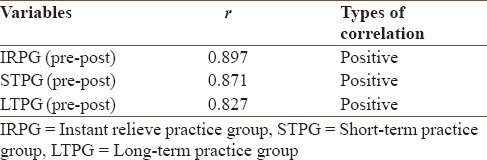
In STPG, there exists a positive correlation between pre- and post-study of yoga therapy and pain and disability where r = 0.871.
Similarly, in LTPG also, the correlation study is positive after 1 month practice of yoga therapy where r = 0.827.
Discussion
The RMDQ was used to assess the pain and disability after the intervention of yoga on different subgroups of experimental group. The questionnaire contains 24 questions aimed at assessments of the status of participant's pain and disability.[22]
This is a randomized experimental trial on 172 patients of both genders in age 21–79 years with lumbar spondylitis. In the current study, there is significant reduction in pain and disability in all groups: IRPG, STPG, and LTPG (P < 0.01). The LTPG group (1-month practice) showed a better result than STPG group (15 days practice) and IRPG (1 h practice) (P < 0.01).
There is significant difference in IRPG with STPG and LTPG (P < 0.01). However, there is no significant difference between STPG and LTPG (P < 0.05). The linear regression analysis showed that there is high correlation before and after practice of yoga in all three groups such as IRPG, STPG, and LTPG.
Pain reduction
The production in pain observed in our study points to the beneficial effect of only yoga on patients having pain and disability.
There are other studies on effect of yogic practices on back pain. Tekur et al.[23] studied the efficacy of the integrated approach of yoga therapy in patients with CLBP and documented 48.8% reduction in Numerical Rating Scale scores in the yoga group.
A meta-analysis of randomized controlled trial (RCT) done by Holtzman and Beggs in 2013 examined the current literature for the strongest evidence of the efficacy of yoga as a potential treatment for CLBP.[24] Tilbrook et al. found that offering a 12-week yoga program to adults with CLBP or recurrent LBP led to greater improvements in back function than usual care for up to 12 months. Yoga seems to be a safe and effective activity that clinicians could consider recommending for patients with a history of LBP.[25]
Saper et al. found that 108 participants in both the yoga and PT group would provide 90% power to detect whether yoga is truly noninferior to PT with respect to effect on pain. Similarly, 107 participants in both the yoga and PT group would provide 81% power to detect whether yoga is truly noninferior to PT with respect to effect on function.[26]
In the pilot RCT study of Cox et al.,[15] change as measured by the RMDQ was the primary clinical outcome (changes in the ABPS, short-form-12, EQ-5D, and pain self-efficacy were secondary clinical outcomes). The United Kingdom back pain exercise and manipulation trial found that a change in the RMDQ score of 1.57 points was a cost-effective difference. Although there is no consensus, a change of 1.1–2.5 on the RMDQ has been recommended as clinically important.[27,28] This scale has been found to be sensitive to change, reliable, and valid. At 4 weeks follow-up, 80% of the yoga group had improved by at least two points compared to 37.5% of the control group, MD 1.88 (95% confidence interval [CI] = −3.18–6.94), P = 0.43 for RMDQ and MD 8.39 (95% CI = 1.18–15.6), P = 0.03 for visual analog scale. At 12 weeks follow-up, 66.6% of the yoga group had improved by at least two points on the RMDQ compared to 55.6% of the usual care group (P = 0.72).[15]
In our study, there is significant reduction in pain and disability in all groups: IRPG, STPG, and LTPG. The LTPG group (1 month practice) showed a better result than STPG group (15 days practice) and IRPG (1 h practice). Tilbrook et al.[25] completed an RCT in 2011 that compared the effectiveness of yoga and usual care for CLBP or recurrent LBP. A total of 313 adults with CLBP were randomly assigned to either a yoga intervention group (n = 156) or usual care group (n = 157). All patients received a back pain education booklet. The intervention consisted of a 12-class progressive yoga program that spanned 3 months. Scores were measured on the RMDQ at 3, 6, and 12 months. The yoga group had better back function at 3, 6, and 12 months than the usual care group. The yoga group also had higher pain self-efficacy scores at 3 and 6 months but not at 12 months. The two groups however had similar back pain and general health scores at 3, 6, and 12 months.[29] Another 2013 systematic review and meta-analysis of the literature on yoga for LBP by Cramer et al.[30] screened studies published through 2012 that were RCT comparing yoga to control conditions in patients with CLBP. The main outcome measures were pain, back-specific disability, generic disability, health-related quality of life, and global improvement. Standardized MDs (SMDs) and 95% CIs were calculated for each outcome. The review included ten studies with 967 patients with CLBP. There was strong evidence for short-term effects on pain (SMD = −0.48; 95% CI = −0.65 to −0.31; P < 0.01) and back-specific disability (SMD = −0.59; 95% CI = −0.87 to − 0.30; P < 0.01). There was also strong evidence for a long-term effect on back-specific disability (SMD = −0.35; 95% CI = −0.55 to −0.15; P < 0.01). There was no evidence of short-term or long-term effects on health-related quality of life. Yoga was not associated with any serious adverse event in any of these studies.
In our study, the linear regression analysis showed that there is high correlation before and after practice of yoga in all three groups such as IRPG, STPG, and LTPG. An evaluation of yoga's impact on the gunas and self-ideal disparity found significant correlations between self and ideal self for the yoga group but not for the control.
A study on Hatha yoga practice and body mass index (BMI) and reduced medication use in women over 45 years by Moliver et al. performed bivariate correlations and multiple linear regressions to analyze the relationship of current hours per week, total lifetime hours, and total calendar years to BMI for yoga practitioner. Bivariate analyses showed a significant inverse relationship between extent of yoga experience and BMI. In the regression analysis, the relationship remained significant between total lifetime hours of yoga and BMI (P = 0.01) and between current hours of yoga per week and BMI (P = 0.04), after accounting for hours of weekly nonyogic exercise and refined and processed food consumption.[31]
Summary of evidence
One of the primary causes of back pain is muscle tension;[32] more people are now work stressed and have mechanical stiffness that primarily affect not only the spine but also the hips and shoulders. Regular yoga workup stretches the muscle and loosens them, which were previously tense.[33] Yoga directly helps people where back pain is directly related poor posture. The findings showed there was a significant reduction in pain intensity in the long-term yoga practice group. The authors reasoned that yoga might enhance both the toning of muscles and releasing of muscle tension. Relaxation responses, therefore, could reduce stress-related muscle tension and modify neurobiological pain perception. The authors also suggested that as yoga practitioners develop increasing awareness of muscle use and joint position, they could better change habitual posture patterns in daily life.
Yoga is often recommended as an evidence-based additional therapy intervention for back and neck pain. Being more than exercise, yoga seems to be able to improve body awareness and pain acceptance, and coping yoga is defined as “_samatvam yoga_” in Bhagavad Gita.[34] The harmony in between body, mind, and emotion is achieved by multifactorial approach of yoga such as asana, pranayama, and relaxation practice (Yoga Nidra).
Limitations
This study contained the unequal size of sample in experimental group without a control group.
Suggestions for future work
Further studies focus on the long-term effectiveness more than 6 months of yoga practice are necessary to check for acceptability on pain. Studies on biochemical variables may throw light on the mechanisms.
Conclusion
Based on the results obtained, the following conclusions were drawn:
- The effect of selected yogic practices is beneficial among people suffering from lumbar spondylitis for reduction of pain and disability
- The effect of selected yogic practices is effective in all three groups such as IRPG, STPG, and LTPG groups. However, it is more effective in LTPG group
- The effectiveness of selected yogic practices has significant difference in between IRPG and LTPG, IRPG and LTPG, but there is no significant difference in between STPG and LTPG
- The regression analysis shows that there exists a high degree of linear association in all three groups such as IRPG, STPG, and LTPG.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.John E. Outline of Orthopaedics and Fractures. New Delhi: CBS Publishers and Distributers Pvt. Ltd; 2011. [Google Scholar]
- 2.Maheswari J. Essential Orthopaedics. 5th ed. New Delhi, India: Jaypee; 2015. [Google Scholar]
- 3.Louis S. Apley's System of Orthopaedics and Fractures. 9th ed. New York: CRC Press; 2015. [Google Scholar]
- 4.Licciardone JC. The epidemiology and medical management of low back pain during ambulatory medical care visits in the United States. Osteopath Med Prim Care. 2008;2:11. doi: 10.1186/1750-4732-2-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guo HR, Tanaka S, Halperin WE, Cameron LL. Back pain prevalence in US industry and estimates of lost workdays. Am J Public Health. 1999;89:1029–35. doi: 10.2105/ajph.89.7.1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Andersson GB. Epidemiological features of chronic low-back pain. Lancet. 1999;354:581–5. doi: 10.1016/S0140-6736(99)01312-4. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. National Ambulatory Medical Care Survey. 2010 [Google Scholar]
- 8.Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F, et al. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012;64:2028–37. doi: 10.1002/art.34347. [DOI] [PubMed] [Google Scholar]
- 9.Carter C, Stratton C, Mallory D. Yoga to treat nonspecific low back pain. AAOHN J. 2011;59:355–61. doi: 10.3928/08910162-20110718-01. [DOI] [PubMed] [Google Scholar]
- 10.Luo X, Pietrobon R, Sun SX, Liu GG, Hey L. Estimates and patterns of direct health care expenditures among individuals with back pain in the United States. Spine (Phila Pa 1976) 2004;29:79–86. doi: 10.1097/01.BRS.0000105527.13866.0F. [DOI] [PubMed] [Google Scholar]
- 11.Carey TS, Garrett JM. The relation of race to outcomes and the use of health care services for acute low back pain. Spine (Phila Pa 1976) 2003;28:390–4. doi: 10.1097/01.BRS.0000048499.25275.51. [DOI] [PubMed] [Google Scholar]
- 12.Posadzki P, Ernst E. Yoga for low back pain: A systematic review of randomized clinical trials. Clin Rheumatol. 2011;30:1257–62. doi: 10.1007/s10067-011-1764-8. [DOI] [PubMed] [Google Scholar]
- 13.Eisenberg DM, Davis RB, Ettner SL, Appel S, Wilkey S, Van Rompay M, et al. Trends in alternative medicine use in the United States, 1990-1997: Results of a follow-up national survey. JAMA. 1998;280:1569–75. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 14.Chou R, Qaseem A, Snow V, Casey D, Cross JT., Jr Diagnosis and treatment of low back pain: A joint clinical practice guideline from the American College of physicians and the American pain society. Ann Intern Med. 2007;147:478–91. doi: 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- 15.Cox H, Tilbrook H, Aplin J, Semlyen A, Torgerson D, Trewhela A, et al. A randomised controlled trial of yoga for the treatment of chronic low back pain: Results of a pilot study. Complement Ther Clin Pract. 2010;16:187–93. doi: 10.1016/j.ctcp.2010.05.007. [DOI] [PubMed] [Google Scholar]
- 16.Büssing A, Ostermann T, Lüdtke R, Michalsen A. Effects of yoga interventions on pain and pain-associated disability: A meta-analysis. J Pain. 2012;13:1–9. doi: 10.1016/j.jpain.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 17.Satyananda SS. Asana Pranayama Mudra Bandha. Munger, Bihar: Yoga Publication Trust, Ganga Darsan; 2000. [Google Scholar]
- 18.Satyananda SS. Four Chapters on Freedom. Munger, Bihar: Yoga Publication Trust, Ganga Darsan; 2000. [Google Scholar]
- 19.Nagendra HR, Nagaratna R, Telles S. Yoga and Cancer. Chennai, Tamilnadu: Vivekananda Kendra Yoga Prakashana; 1999. [Google Scholar]
- 20.Telles S, Nagarathna R, Nagendra HR. Breathing through a particular nostril can alter metabolism and autonomic activities. Indian J Physiol Pharmacol. 1994;38:133–7. [PubMed] [Google Scholar]
- 21.Satyananda SS. Yoga Nidra. Munger, Bihar: Yoga Publication Trust, Ganga Darsan; 2000. [Google Scholar]
- 22.Roland M, Morris R. A study of the natural history of back pain. Part I: Development of a reliable and sensitive measure of disability in low-back pain. Spine (Phila Pa 1976) 1983;8:141–4. doi: 10.1097/00007632-198303000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Tekur P, Singphow C, Nagendra HR, Raghuram N. Effect of short-term intensive yoga program on pain, functional disability and spinal flexibility in chronic low back pain: A randomized control study. J Altern Complement Med. 2008;14:637–44. doi: 10.1089/acm.2007.0815. [DOI] [PubMed] [Google Scholar]
- 24.Holtzman S, Beggs RT. Yoga for chronic low back pain: A meta-analysis of randomized controlled trials. Pain Res Manag. 2013;18:267–72. doi: 10.1155/2013/105919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tilbrook HE, Cox H, Hewitt CE, Kang'ombe AR, Chuang LH, Jayakody S, et al. Yoga for chronic low back pain: A randomized trial. Ann Intern Med. 2011;155:569–78. doi: 10.7326/0003-4819-155-9-201111010-00003. [DOI] [PubMed] [Google Scholar]
- 26.Saper RB, Sherman KJ, Delitto A, Herman PM, Stevans J, Paris R, et al. Yoga vs. physical therapy vs. education for chronic low back pain in predominantly minority populations: Study protocol for a randomized controlled trial. Trials. 2014;15:67. doi: 10.1186/1745-6215-15-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Erik JG, Marisa S, Douglas C. VA San Diego Healthcare System. USA: University of California San Diego, SDSU/UCSD Joint Doctoral Program in Clinical Psychology; 2013. Yoga as a Treatment for Low Back Pain: A Review of the Literature; pp. 332–52. [Google Scholar]
- 28.Wolsko PM, Eisenberg DM, Davis RB, Kessler R, Phillips RS. Patterns and perceptions of care for treatment of back and neck pain: Results of a national survey. Spine (Phila Pa 1976) 2003;28:292–7. doi: 10.1097/01.BRS.0000042225.88095.7C. [DOI] [PubMed] [Google Scholar]
- 29.Rani JN. Impact of yoga training on triguna and self ideal disparity. Psychological studies. Natl Acad Psychol India. 2007;52:174–7. [Google Scholar]
- 30.Cramer H, Lauche R, Haller H, Dobos G. A systematic review and meta-analysis of yoga for low back pain. Clin J Pain. 2013;29:450–60. doi: 10.1097/AJP.0b013e31825e1492. [DOI] [PubMed] [Google Scholar]
- 31.Moliver N, Mika E, Chartrand M, Burrus S, Haussmann R, Khalsa S. Increased Hatha yoga experience predicts lower body mass index and reduced medication use in women over 45 years. Int J Yoga. 2011;4:77–86. doi: 10.4103/0973-6131.85490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chou R, Huffman LH. American Pain Society; American College of Physicians. Nonpharmacologic therapies for acute and chronic low back pain: A review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med. 2007;147:492–504. doi: 10.7326/0003-4819-147-7-200710020-00007. [DOI] [PubMed] [Google Scholar]
- 33.Tekur P, Nagarathna R, Chametcha S, Hankey A, Nagendra HR. A comprehensive yoga programs improves pain, anxiety and depression in chronic low back pain patients more than exercise: An RCT. Complement Ther Med. 2012;20:107–18. doi: 10.1016/j.ctim.2011.12.009. [DOI] [PubMed] [Google Scholar]
- 34.Goyandaka J. Srimadbhagvadgita Tattvavivecani. 19th ed. Gorakhpur: Gita Press Publication; 2004. [Google Scholar]