Yoga for People With Chronic Pain in a Community-Based Setting: A Feasibility and Pilot RCT (original) (raw)
Abstract
The purpose of this feasibility pilot study was to assess benefits of 8 weeks of yoga in people with chronic pain. Participants completed baseline assessments and were randomized to yoga or usual care. Yoga was offered twice a week for 8 weeks. We assessed feasibility and the Brief Pain Inventory (BPI) was the primary outcome, assessing pain-severity and pain interference on daily activities. Eighty-three people were recruited; 67 people completed the study and were included in the analyses. Average age of participants was 50.78 ± 10.43 years and most participants had pain >10 years. The intervention appeared feasible and there were significant improvements (P < .05) in multiple measures for the yoga group, including a decrease in BPI interference scores from 7.15 ± 1.70 to 6.14 ± 2.21 (P = .007). There was a significant difference in body responsiveness and pain management scores between groups at 8 weeks. It appears that yoga was feasible and positively influenced multiple outcome measures for people with chronic pain.
Keywords: chronic pain, alternative therapies, yoga, feasibility
Chronic pain is a significant national issue that leads to decreased quality of life and an annual cost of $635 billion a year.1 Direct and indirect costs are associated with loss of paid work and increases in disability benefits, and increased use of opioids.1,2 As society finds itself in an opioid epidemic, treatment costs and mortality rates are quickly increasing.3 However, despite increased use of opioids and other treatments, chronic pain continues to be disabling and persistent for many individuals. Perhaps this is why treatment of chronic pain requires multifaceted interventions that address the complex accumulation of physical, psychological, and social factors that contribute to chronic pain.4 For example, there may be biological factors behind the sensation of pain, but the cognitive awareness of and the emotional response to the pain contribute to the overall experience of chronic pain.5 Given the complexities of pain management, and that the Centers for Disease Control and Prevention recommends nonopioid treatments, research on innovative nonpharmacological treatments to improve management of chronic pain is urgently needed.6,7
Because chronic pain involves multiple facets, the whole person is affected, and is likely why individuals with chronic pain are large consumers of complementary and integrative therapies (CIT).8 Therefore, a holistic mind-body intervention that is capable of simultaneously targeting multiple factors may be the most effective intervention for people with pain. Integrative therapies, such as yoga, address the whole person, connect the mind and body, and are holistic. Additionally, emotional or cognitive responses to the physical pain may lead to a disconnect between the mind and body, which may also be addressed via yoga.5,9 The sense of the mind and body reconnecting through yoga may be associated with improved awareness of afferent (sensory) feedback allowing for more effective efferent (motor) commands to muscles, reducing muscle tension, spasms, and associated pain.
Hatha yoga is considered gentle and is the foundation of other types of yoga most often found in the United States. As a result, Hatha yoga was used in this study, and the yoga components included in the intervention were physical postures, composed of stretching and strengthening (asanas)10,11; diaphragmatic breathing (pranayama)10; positive affirmations (mantras); and meditation (dhyana).11 Physical asana or postures simultaneously address flexibility and strengthening10,11 needs of the individual, often times cited as common issues for people with chronic pain.12 However, yoga may do more than heal the physical aspects of pain. For example, yoga may lead to changes in cognition13 or in emotional regulation.14 Yoga may also help people reduce pain interference,15 defined as the interference pain has on everyday life and functioning.
Authors of systematic reviews and meta-analyses tend to focus on specific locations of pain (low back pain, neck pain), but indicate that yoga decreases pain severity and pain-related interference on activities; however, authors note that additional research regarding yoga and pain is still needed.15–19 Furthermore, research has been completed in tightly controlled randomized controlled trials and most often only includes participants with one type or location of chronic pain (ie, back pain, low back pain, arthritis, migraines, fibromyalgia).15 Maintaining one type of pain in a study, such as low back pain, neck pain, or headaches, is an important and logical first step in the yoga and pain research trajectory. However, based on systematic reviews, yoga has been shown to work for many pain populations.15–19 Therefore, it is important to begin to translate the research that supports using yoga for pain into the real world (moving from research bench to bedside). Our local chronic pain clinic serves clients with any type of pain and were excited about the opportunity of adding yoga to the clinic. We therefore developed and tested a yoga intervention for participants with different types or locations of pain. Currently, there is no published research regarding the use of yoga in a community-based setting for individuals with any type or location of pain. Therefore, this study is unique in that the purpose of this study was to assess the feasibility and benefits of an 8-week yoga intervention delivered in a community-based pain clinic (Clinic) to people with any type or location of pain. All participants received usual care, including monthly self-management programming. Self-management is an interdisciplinary, multifaceted intervention shown to be effective to improve pain.4 Self-management allows participants to dynamically participate in their treatment, focusing on perceived problems and concerns.20
Methods
Design
This was an 8-week feasibility and pilot randomized controlled trial (RCT) comparing yoga to usual care. This study included a sample of individuals with various types of pain, reasons for pain, and location of pain. Feasibility and pre and post outcome measures were included to examine the use of a group yoga intervention with various types and locations of pain in a community setting.
Setting
The study was conducted at an outpatient pain Clinic that provides care for underserved and underinsured individuals.
Participants
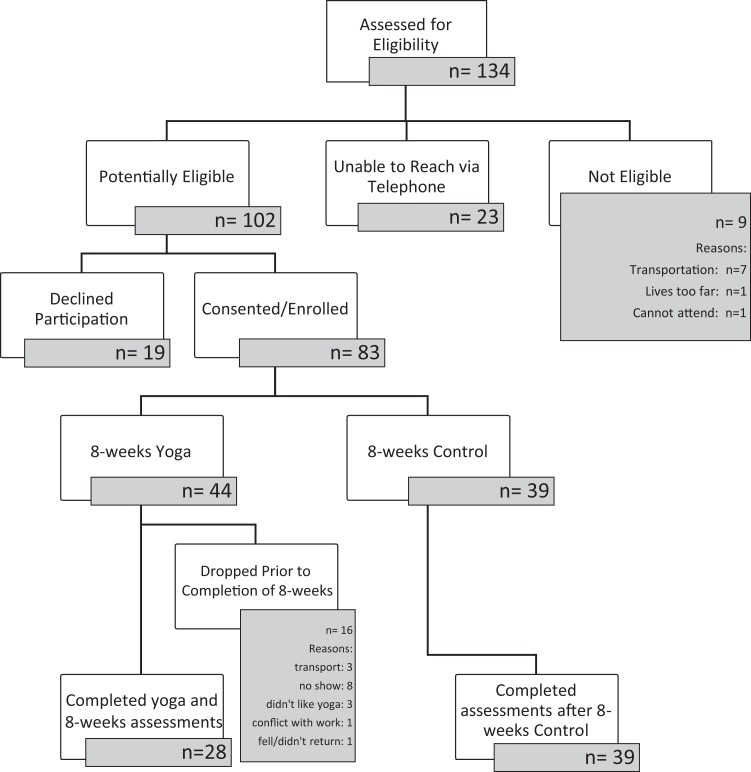
All participants were patients at the Clinic and were recruited for this study via telephone. To be included in the study, individuals had to meet the following criteria: self-report of chronic pain for at least 6 months (any type, reason, or location of pain was included); >18 years old; no self-report of exercise restrictions; no consistent (daily or weekly) yoga practice for the past year; no travel restrictions; and, able to and willing to consent to the study. The study was approved by the university institutional review board (IRB). See Figure 1 for the CONSORT (Consolidated Standards of Reporting Trials) diagram regarding recruitment and randomization.
Figure 1.
CONSORT (Consolidated Standards of Reporting Trials) diagram.
Feasibility Measures
Feasibility data were collected and included information regarding: recruitment; adverse events/safety; attendance; maintenance of blinding; study participants’ ability to complete the intervention; acceptability; and fidelity. The assessor was blinded to randomization and did not attend the yoga intervention. To assess acceptability, participants randomized to yoga completed an evaluation form after the completion of the eight-weeks of yoga. The form included 7 questions on a 1-to-7 Likert-type scale with a score of 7 being the best or the highest. Participants were also asked what was helpful or not helpful and for recommendations for future yoga classes. Fidelity, or the yoga teachers’ adherence to the yoga intervention protocol, was documented using a prepared check-off form, including specific components, such as specific planned yoga postures, breath work, poses paired with breath, eye movements, mantra, and meditation at the end of class. Both the yoga teacher and an observer completed the fidelity check-off form. If a part of the intervention was missed, the item was noted and the yoga teacher was reminded to include the item in the next session (as appropriate).
Randomization and Outcome Measures
Self-report assessments were completed by participants on their own time and were returned to the study personnel within 2 weeks of the intervention beginning or ending. An assessor who was blinded to randomization allocation assisted participants as needed to complete all assessments. Demographic information and data related to pain characteristics (eg, time since pain onset, reason for pain, limitations due to pain, medications) were included. Once participants returned their baseline assessment package to the study personnel, they were randomized to yoga or the usual care group. Randomization was completed at the individual level using a random number generator.
Pain severity and pain interference on daily activities was measured with the Brief Pain Inventory (BPI). The BPI is considered a reliable and valid assessment to understand pain related interference on everyday life and has been used in hundreds of studies.21 The BPI has 2 subscales, assessing both pain severity and pain interference. The pain severity subscale includes 4 items and each item is rated between a 0 (no pain) to 10 (pain as bad as you can imagine) to assess the intensity of pain now and during the past week. The 7 items that assess pain interference on daily activities address general activity, mood, mobility, work, relationships, sleep, and enjoyment in life. Scores for each item ranges from 0 (does not interfere) to 10 (interferes completely). Mean scores are included for the 2 subscales and the total score. Lower scores indicate less pain severity or less pain interference.21,22
We assessed quality of life (QoL) with the Rand 36-item Health Survey.23 The Rand-36 includes 36 items and is valid and reliable and has been used in individuals with chronic pain. There are 8 domains, including current physical and mental health, limitation of activities due to health, and functional items such as housework and mobility.23 As it is now common in the literature, we calculated a single total score by averaging the 8 domain scores and scores ranges between 0 to 100; higher scores indicate improved QoL.24
As all participants received monthly self-management programming as part of usual care, we included assessments regarding self-efficacy to manage chronic pain. We included the Chronic Pain Self-Efficacy Scale (CPSS) and the 6-item Stanford Self-Efficacy for Managing Chronic Disease (SSMCD-6) assessments. The CPSS has been used in people with chronic pain and is considered reliable and valid.25 The CPSS includes 3 domains and a total score, domains include items assessing self-efficacy for pain management (9 items), physical function (5 items), and coping with symptoms (8 items).25 Participants indicate the percent, from 0% to 100%, of their confidence to address each item. We included mean domain and total scores (each with a range from 0% to 100%), increased scoring indicates improved self-efficacy. The SSMCD-6 includes 6 items related to pain and chronic disease and how confident a person is, from 0% to 100%, to complete each item.26 Valid and reliable items address management of fatigue, physical discomfort, emotional distress, other health symptoms, daily activities, and medication use. Increased scoring indicates increased confidence and scores range from 0% to 100%. Finally, we assessed body responsiveness using the Body Responsiveness scale by Daubenmier.27 The scale includes 7 items and participant answers indicate if the statement is “not at all true about me” or “very true about me.” Items address the mind-body connection and includes items such as asking whether the participants “listen to their body,” if they “suppress bodily feelings,” and whether “my mind and my body often want to do different things.” Increased scoring indicates increased body responsiveness or enhanced mind-body connection.
Yoga Intervention and Usual Care Control Group
Yoga was offered twice a week for eight weeks (16 sessions); each session lasted 60 minutes and the program was standardized and progressive, moving from sitting postures, to then include standing and floor postures. To best accommodate the needs of participants with chronic pain, yoga was taught by a yoga teacher who was also an occupational or physical therapist. Yoga postures were modified as needed so that individuals could successfully complete each posture. Multiple props were used to enhanced modification of each pose, including chairs with or without arm rests, blocks, straps, bolsters, and wedges. As typical in yoga interventions, postures, breath work, mantras, and meditation were included in each session. The yoga protocol was based on our prior yoga for neuropathy study28,29 as both studies included people with pain; however, the current intervention was further adapted by the yoga teacher to meet the needs of people with chronic pain in the study. Importantly, yoga became progressively more challenging over the 8 weeks. Yoga postures included in the 8 weeks are presented in Table 1.
Table 1.
Eight-Week Yoga Intervention.
| Weeks | Position | Description of Yoga Postures, Breath Work, and Mudras |
|---|---|---|
| Weeks 1-8 | Seated | Slower, deeper, rhythmic breathing (yogic breathing, inhaling through the nose and exhaling through the nose) |
| Alternate nostril breathing—brain regulator | ||
| Various head and neck positions and movements with prolonged stretches | ||
| Scapular range of motion and arm movements (receptive gesture, Cactus arms) | ||
| Finger movements (mudras) | ||
| Seated spinal extension (mini back bands), flexion (forward fold), lateral flexion, and hand to opposite knee (spinal twist) | ||
| Inhale with exaggerated exhale while focusing both eyes toward the forehead (Lion’s breath) | ||
| Hip rotation and stretching with ankle, foot, and toes movements | ||
| Seated forward fold | ||
| Forward fold with one knee on opposite ankle (seated Pigeon) | ||
| Weeks 1-8 | Standing | Standing (Mountain pose) |
| Roll shoulders back and down | ||
| Knees bent, up and down on toes (Chair pose) | ||
| Dynamic balancing on one leg—one arm outstretched | ||
| Hip extension while standing (Locust pose) | ||
| Lunges (Warrior I and Warrior II pose) | ||
| Balance on 1 foot, with opposite sole placed on calf | ||
| Toe/ball of foot, small knee bends with feet flat on floor (Awkward pose) | ||
| Balance on one foot with opposite sole on calf (Tree pose) | ||
| Weeks 2-8 | Supine on the floor | Posterior leg stretches |
| Supine extensions: bridge lifts (Bridge pose) | ||
| Knees into chest: separately then both at once—Energy release (Apanasana) | ||
| Hip rotation and stretching with ankle, foot, and toes (supine Pigeon) | ||
| Bilateral eye movements and hold eyes steady (during Savasana) | ||
| Supine relaxation (Savasana or corpse pose with meditation) |
All study participants received monthly self-management as part of usual care. Usual care in the Clinic includes monthly visits with the medical provider, recording of vitals (ie, blood pressure, heart rate, pulse oxygen), pain medication management, goal setting, nutritional counseling as needed, a set number of visits to a massage therapist or acupuncturist, and monthly self-management programming. All individuals treated in the Clinic were expected to attend 1 monthly self-management education session. While attendance to the self-management sessions was tracked and recorded, visits to massage or acupuncture were not, as those visits were to professionals outside of the Pain Clinic network. Decisions about self-management educational topics were selected by an interdisciplinary team that included the physician, nurse, nutritionist, and psychologist. The monthly 1-hour self-management education sessions were led by the Clinic nurse as part of the standard of care for this clinic. Self-management education sessions included information regarding health and wellness, but not necessarily pain management. For example, participants received education on smoking cessation, which is not directly linked to pain management, but may be helpful to general improvements in health.
Data Analysis
Because this was a feasibility and pilot study, only participants who completed the study (at least 8 or more yoga sessions) and who completed the assessments were included in the study and data analyses. All data were analyzed using Statistical Package for the Social Sciences 23 (IBM Corp, Armonk, NY). Double data entry was completed on 10% of the total study sample to ensure quality of data entry. In the case of one measure, BPI severity, one individual with an outlying value was removed from the analysis. Descriptive statistics were used to describe data related to demographics, pain characteristics, and feasibility. As per the results of the Shapiro-Wilk test, the data were normally distributed. T tests or chi-square analyses were used to compare demographic variables between yoga and control groups.
To assess within group differences, paired t tests were used to compare outcome measure data between baseline and postintervention within each of the yoga and usual care control groups. We calculated the effect size (d Cohen) for each variable (using means, standard deviation, and the correlation).30 We used the following thresholds to interpret effect size: 0.20 for small, 0.50 for moderate, 0.80 for large, and 1.30 for very large.31,32 To study trends in the outcome data, the average percent change was calculated for each outcome measure (Average Time 2 – Average Time 1 divided by Average Time 1, multiplied by 100). Comparison of yoga and usual care groups 8-week outcome measure was conducted using analysis of covariance with group as a fixed effect adjusting for baseline outcome measure as a covariate.33 A significance level of .05 was used for all tests of significance.
Results
Feasibility
Recruitment and Participants
Overall, during a 5-month period, we attempted contact with 134 individuals who were patients at the Clinic. Of the 134 individuals, 102 individuals were contacted and 32 were never reached or were not eligible. Of the 102 individuals contacted, 83 (81%) consented and enrolled; 44 individuals were randomized to the yoga group and 39 to the usual care control group. Sixty-seven (81%) participants were maintained in the study and included in the analyses. Demographic data for the 67 participants who completed the study are presented in Table 2. Results from t tests or chi-square tests indicate no significant differences in demographics or pain-related characteristics between groups, except for race and education (Table 2).
Table 2.
Demographics and Pain-Related Characteristics.a
| Variable | All (N = 67) | Yoga (n = 28) | Control (n = 39) | P |
|---|---|---|---|---|
| Age, years | 50.78 ± 10.43 | 53.04 ± 9.6 | 49.15 ± 10.82 | .134 |
| Gender (female) | 46 (70%; n = 66) | 19 (68%) | 27 (71%; n = 38) | .780 |
| Race (Caucasian) | 45 (69%; n = 65) | 15 (56%; n = 27) | 30 (79%; n = 38) | .044 |
| Part of a couple (no) | 33 (50%; n = 66) | 15 (54%) | 18 (23%; n = 38) | .618 |
| Education (some college) | 39 (44%; n = 61) | 12 (46%; n = 26) | 27 (77%; n = 35) | .013 |
| Time since pain started, >10 years | 43 (66%; n = 65) | 20 (77%; n = 26) | 23 (59%) | .134 |
| Reasons for pain (trauma) | 34 (57%; n = 60) | 16 (57%) | 18 (56%; n = 32) | .944 |
| Are you limited in any activities due to pain? (yes)b | 51 (88%; n = 58) | 21 (84%; n = 25) | 30 (91%; n = 33) | .450 |
| Using opioids (yes)b | 66 (99%) | 28 (100%) | 38 (97%) | 1.00 |
| Number of medications | 9.87 ± 5.0 | 10.14 ± 5.70 | 9.67 ± 4.57 | .706 |
Time since the start of pain ranged widely and is presented as a dichotomous variable of less than or more than 10 years since the start of pain. In the sample, 43 (66%; n = 65) of the individuals reported their pain began over 10 years ago. As we included any chronic pain (not limiting to only back pain), the type or location of pain and reason for pain varied greatly. The majority of people reported that pain was located in more than one area or joint and 24 participants (36%) reported headaches or migraines. Participants were asked to identify the primary reason for their pain, 34 individuals (57%; n = 60) indicated that their pain was related to trauma (eg, automobile accident, work injury, fall). The other participants indicated that their pain was disease oriented (eg, arthritis, fibromyalgia, migraines, stroke). When asked if participants felt they had limitations related to their pain (yes or no), 51 participants (88%; n = 58) said yes, they sustained limitations secondary to chronic pain. Finally, all participants, except one, were using opioid medications for pain management and participants were taking an average of nearly 10 medications every day.
Adverse Events/Safety
While, in general, yoga is not associated with serious adverse events,34 we reported multiple adverse events to our IRB for the participants randomized to the yoga intervention. Adverse events reported, that the IRB deemed unrelated to the yoga intervention included the following: a participant came to yoga very ill, found to be related to an overdose of medications that led to nausea and dizziness, Clinic staff called for an ambulance and client was hospitalized; and a participant was found in her home deceased, related to her comorbidities. Nonserious adverse events reported that were likely related to yoga included dizziness (likely from forward folds for an individual with low blood pressure); increased muscle or joint pain, likely related to increased movement; a fall to the floor, without injury, for a participant who had impaired mobility and who used a walker, but who refused to use the walker when completing the standing postures (study staff were assigned to work with her; however, she still sustained a fall); and nausea and diarrhea for a client who came into yoga feeling ill but who did not report her symptoms, the twisting postures and forward folds in the yoga session likely exacerbated her symptoms making her sicker during the session.
Attendance
In the yoga group, 28 individuals participated in 8 or more yoga sessions and had completed data and were therefore included in the data analysis. Attendance to yoga was tracked, and on average, for those participants included in these analyses, 12.11 ± 2.3 sessions were attended out of a possible 16 sessions. Missed yoga classes were related to lack of transportation, illness, new job, did not like yoga, worried that yoga would increase pain, worried that the medical doctor would alter or stop the opioid prescription if participant reported decreased pain due to yoga, or yoga increased pain. Attendance to usual care self-management monthly classes were tracked, all study participants were offered 2 sessions during the eight-week period. On average, participants in both groups attended 1.9 ± 0.28 self-management sessions, there were no differences in attendance between yoga or usual care groups (1.93 ± 0.26 vs 1.90 ± 0.31,P = .666).
Maintenance of Blinding
After the 8-week assessment was completed, the assessor recorded if they thought the individual was randomized to the yoga or control group, randomization allocation was then revealed. Of the 67 participants who completed the intervention and assessments, the assessor remained blinded (did not correctly guess) the randomization for 76% (n = 51) of the study participants.
Ability to Complete the Intervention
All individuals randomized to yoga and who completed the study were able to complete the planned yoga intervention. It was necessary, as expected, to modify postures, use props (bolsters, wedges), or provide verbal or physical cueing to facilitate completion of the yoga intervention. When a certain pose was not accessible to an individual participant, a modification was provided or the participant was reminded to just take a breath, perhaps imagining their body in the pose. It is common practice in yoga to ask participants to honor and listen to their body, making modifications or rest a normal part of a yoga practice. The yoga teachers were also an occupational or physical therapist, both adept at modifying poses.
Acceptability
Twenty-four (86%) of the 28 individuals who were randomized to yoga and who completed the intervention completed the acceptability evaluation form (7 items, score of 7 being the highest). Overall, participants found value in the yoga intervention to improve their pain (5.0 ± 1.4) and management of pain (5.3 ± 1.2). Participants indicated high scores for the instructors’ yoga knowledge (6.8 ± 0.4) and ability to teach yoga and facilitate movements (6.6 ± 0.7). In general, participants were satisfied with class format (6.5 ± 0.8), progression of yoga classes (5.8 ± 1.1), assistance in class (6.7 ± 0.5), and the physical environment (6.4 ± 0.8). Participants found the breathing, relaxation techniques, instructors, and stretching exercises particularly helpful. There were few recommendations for improvement. When asked what they would change about the intervention, participants concluded, “Nothing! Everything was great. The teacher was great!” or “Nothing, I learned a lot from yoga.” The only recommendations offered included the possibility of increasing each class session from 1 hour to 1.5 hours and conducting the class outside.
Fidelity
The fidelity form included yoga postures, breath work, poses paired with breath, eye movements, mantra, and the meditation at the end of class. Of the 80 sessions offered, 88% of the sessions were completed precisely to the protocol. There were 23 instances within 10 classes where a planned component was not offered.
Outcome Measures
For individuals randomized to the yoga group, results of the paired_t_-tests indicated significant improvement in BPI interference and total scores, but not in pain severity (Table 3). After yoga, BPI interference scores decreased from 7.15 ± 1.70 to 6.14 ± 2.21 (P = .007), a 14% decrease with an approximately moderate effect size (d = 0.493), and BPI total scores decreased from 7.05 ± 1.22 to 6.45 ± 1.61 (P = .027), a 9% decrease. Scores for BPI severity and interference subscore and total BPI scores were relatively maintained for participants randomized to the usual care control group. Average BPI subscores and average total BPI did not significantly differ between yoga and usual care control groups at 8 weeks, adjusting for baseline BPI score (Table 4).
Table 3.
Change in Outcome Measure Scores Over 8 Weeks for Yoga and Control Groups (Within-Group Comparison).
| Outcome Measures | Yoga | Control | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 8 Weeks | P | d Cohen | % Change | Baseline | 8 Weeks | P | d Cohen | % Change | |
| BPI total score | 7.05 ± 1.22 (n = 25) | 6.45 ± 1.61 | .027 | 0.387 | ↓9 | 6.39 ± 1.53 (n = 28) | 6.50 ± 1.50 | .743 | 0.066 | ↑2 |
| BPI, pain severity | 6.88 ± 0.71 (n = 27) | 6.98 ± 0.87 | .480 | 0.135 | ↑1 | 6.97 ± 1.13 (n = 29a) | 6.93 ± 1.01 | .436 | 0.069 | ↓1 |
| BPI, pain interference | 7.15 ± 1.70 (n = 25) | 6.14 ± 2.21 | .007 | 0.493 | ↓14 | 6.06 ± 2.03 (n = 28) | 6.19 ± 1.80 | .731 | 0.065 | ↑2 |
| Rand-36 QoL, total score | 82.04 ± 7.87 (n = 28) | 94.07 ± 8.60 | <.001 | 1.170 | ↑15 | 82.91 ± 7.30 (n = 32) | 94.63 ± 6.07 | <.001 | 1.404 | ↑14 |
| CPSS, total score | 49.07 ± 24.76 (n = 24) | 62.27 ± 22.44 | .008 | 0.646 | ↑27 | 54.78 ± 16.99 (n = 31) | 56.19 ± 18.30 | .611 | 0.092 | ↑3 |
| CPSS, management | 55.62 ± 27.54 (n = 27) | 69.13 ± 22.07 | .004 | 0.716 | ↑24 | 61.00 ± 24.33 (n = 31) | 62.49 ± 22.62 | .646 | .083 | ↑2 |
| CPSS, physical | 41.22 ± 26.31 (n = 26) | 58.81 ± 24.33 | .001 | 0.665 | ↑43 | 52.68 ± 21.19 (n = 31) | 52.34 ± 21.97 | .935 | 0.015 | ↓1 |
| CPSS, coping | 42.75 ± 29.69 (n = 25) | 60.73 ± 29.40 | .021 | 0.691 | ↑42 | 49.30 ± 18.35 (n = 32) | 51.62 ± 20.47 | .450 | 0.136 | ↑5 |
| SSMCD-6 | 30.11 ± 12.08 (n = 28) | 36.68 ± 12.27 | .006 | 0.526 | ↑22 | 33.75 ± 10.99 (n = 32) | 35.13 ± 10.96 | .495 | 0.123 | ↑4 |
| Body responsiveness | 26.46 ± 6.25 (n = 28) | 31.32 ± 6.28 | <.001 | 0.826 | ↑18 | 26.97 ± 6.76 (n = 32) | 26.97 ± 6.60 | 1.000 | 0.000 | 0 |
Table 4.
Results of Analysis of Covariance (ANCOVA) With 8-Week Outcome Measure as the Dependent Variable, Group as Fixed Effect, and Baseline Outcome Measure as Covariate (Between Groups).
| Outcome Measures | Difference Between 8-Week Means (Yoga vs Control; 95% CI) | P |
|---|---|---|
| BPI total score | −0.37 (−1.09, 0.36) | .311 |
| BPI, pain severitya | 0.15 (−0.18, 0.49) | .364 |
| BPI, pain interference | −0.67 (−1.66, 0.32) | .179 |
| Rand-36 QoL, total score | −0.21 (−3.73, 3.31) | .906 |
| CPSS, total score | 9.34 (0.25, 18.44) | .044 |
| CPSS, management | 9.74 (0.82, 18.66) | .033 |
| CPSS, physical | 12.23 (1.28, 23.18) | .029 |
| CPSS, coping | 11.63 (−0.89, 24.16) | .068 |
| SSMCD-6 | 3.44 (−1.83, 8.70) | .197 |
| Body responsiveness | 4.62 (1.79, 7.46) | .002 |
Interestingly, QoL total scores increased significantly for both the yoga (15%) and the usual care control group (about 14%; Table 3). Average QoL total scores did not significantly differ between yoga and usual care control groups at 8 weeks, adjusting for baseline QoL score (_P_= .906; Table 4). All 3 domains and the total score for the CPSS significantly improved for the yoga group but not for the usual care control group. The total score for the CPSS improved by 27% from 49.08 ± 24.76 to 62.27 ± 22.44 (P = .008) for participants in the yoga group. This change in score indicates improved self-efficacy surrounding pain management, physical function, and coping with symptoms. A moderate effect size was found for the CPSS pain management, physical functioning, and coping domains (d ≥ 0.5). Average CPSS total, pain management, and physical function 8-week scores significantly differed between yoga and usual care control groups, adjusting for the baseline score, with participants in the yoga group having a higher average CPSS in these domains (Table 4). The 8-week average CPSS coping score did not significantly differ between yoga and usual care control groups, adjusting for baseline CPSS coping score (Table 4).
SSMCD-6 scores significantly improved for individuals randomized to the yoga group (30.11 ± 12.08 to 36.68 ± 12.27, P = .006). The 22% improvement in SSMCD-6 scores indicates improved confidence to address pain and chronic disease. There was not a significant difference between yoga and usual care control groups 8-week average SSMCD-6 scores, adjusting for baseline SSMCD-6 score (Table 4). Finally, Body Responsiveness Scale scores significantly improved by 18% in the yoga group (from 26.46 ± 6.25 to 31.32 ± 6.28,P < .001) with a moderate effect size (≥0.5). The average 8-week body responsiveness scores significantly differed between yoga and usual care control groups, adjusting for baseline body responsiveness, with yoga average body responsiveness higher than usual care control group body responsiveness (95% CI 1.79-7.46; Table 4). Other than the QoL scores, there were no significant differences between baseline and 8-week scores for the control group (Table 3).
Discussion
Through this feasibility and pilot RCT, we found that providing 8 weeks of yoga at a community pain clinic to people with different types and location of pain was both feasible and beneficial.
Feasibility
Within the pain clinic, where individuals already receive pain management, we recruited 83 people in only 5 months. This may indicate a great need for novel pain interventions, perhaps specifically nonpharmaceutical interventions. While there were not severe adverse events related to the study, it seems most events were related to study participants not listening to their bodies and trying to “push through” to be part of the yoga class. While participants were taught to honor and listen to their bodies, it was also clear that some of them came to yoga and participated in yoga when they should have maybe taken a rest or a break. For example, someone who was dizzy after forward folds was encouraged to take a break but instead continued her yoga practice but became dizzier.
On average, participants randomized to yoga attended 75% of the 16 sessions (12.11 ± 2.3). This is a similar attendance rate to our other 16-session/8-week interventions. We did have 16 participants drop out of the yoga group (16/44 = 36%). This dropout rate is higher than we have seen in our other studies, where it has been more likely to see 5% to 20% attrition rates.29,35,36 This dropout rate may be attributable to this study having limited resources through a small internal grant. The dropout rate perhaps was also related to us including individuals with any type of pain. Perhaps future trails should not include any type of pain, but instead limit to musculoskeletal pain. Musculoskeletal pain would still be more inclusive than studies that only included low back pain, but would not mix people with migraines or complex regional pain syndrome with people with musculoskeletal pain. It may be that migraine or complex regional pain syndrome pain is inherently different and requires a different yoga intervention. However, we must also question the feasibility of an 8-week yoga intervention for people with significant pain and who are also underresourced and underserved. Yoga class attendance was likely not a priority for people who were homeless or underemployed, thus the delivery of the intervention may need to be additionally flexible. We included evening classes, but to enhance attendance and decrease attrition it may be necessary to also include classes on the weekend or alter the “dose” of yoga and offering it weekly instead of twice a week. Further feasibility testing is likely necessary.
Additionally, while participants did not quite use these exact words, we also had the sense from participants who dropped out or who missed many sessions, that they were somewhat attached to their pain, and their pain medicines. It seems that some participants had their personal identify wrapped up with their chronic pain and were not sure how to handle a shift in this identity. For others, we heard concern that if their pain decreased, their prescription for their pain mediation might be changed and they were concerned about being able to manage their pain with less medications. These are important and complex issues to manage, likely requiring additional therapy or interventions.
It appears the study and intervention were completed as planned. For example, the assessor remained blinded for 76% of the assessments. This was a challenge, as while individuals randomized to yoga were asked to not talk about yoga or changes they attributed the yoga, some participants were very enthusiastic about the yoga programming and their improvements. Therefore, some participants “slipped” and disclosed that they were randomized to yoga. In our future studies we will provide an active control group, rather than a usual care control group, which should alleviate some issues related to blinding. Through modification of the yoga practice, all individuals were able to complete the yoga intervention. Additionally, participants determined the yoga teachers and the yoga sessions were acceptable. For example, on a scale of 1 to 7 with a 7 being the highest score, scores for all 7 items on the acceptability form were a 5 or greater. Finally, the yoga teacher and an observer completed the fidelity check-off form. Of the 80 classed offered, 88% of the classes were completed precisely to the protocol. There were only 10 yoga sessions (with 23 instances) where a component of yoga being missed. Most often, poses where omitted in order to complete the class on time.
Outcome Measures
Participants with chronic pain who were randomized to receive 8 weeks of yoga significantly improved in all outcome measures, except for BPI pain severity. Effect sizes were small to moderate for the BPI pain-related interference score (0.493) and moderate to large for the QoL Rand-36 total scores, CPSS pain management and physical functioning scores, and body responsiveness scores (Cohen’s d ≥ .50).31,32 In the usual care control, only the QoL Rand-36 scores increased significantly and had an effect size of 1.20, nearly the same as changes demonstrated by individuals randomized to the yoga intervention. This is perhaps secondary to the high level of care received as part of usual care, including monthly self-management programming. Treatment in the Clinic likely includes more time with a clinician and resources than typical pain management settings. The Clinic has not studied their outcomes related to their programming, but it is possible that usual care received in the Clinic is enough to improve QoL scores, but not other constructs measured as part of this study.
To our knowledge, this is the first yoga study to include people with any type or location of chronic pain (ie, back pain, low back pain, arthritis, migraines) and to be embedded into a community-based clinic, not completed in a research laboratory. In studies or in reviews that include people with only one type or location of pain, pain severity has improved.15–19 This is in contrast to the results from the current study, where BPI pain severity scores worsened by 1% (not clinically significant). However, after yoga, BPI pain interference scores, or how pain interferes with day to day life, significantly decreased (P = .007) by 14% with an effect size of 0.493. This indicates that the physical pain severity did not change for individuals, perhaps due to the different types of pain sustained in the group. A review of the literature indicates that different types of yoga or different yoga protocols are included for different types of pain. For example, we used Hatha yoga in this study; Hatha yoga is a common and gentle type of yoga and has been used to improve pain for individuals with low back pain,37,38 irritable bowel syndrome,39 pain after stroke,40 muscle soreness,41 arthritis,42 and even individuals on hemodialysis.43 Other researchers found positive impacts on pain using Iyengar yoga in people with carpal tunnel pain44 or low back pain.45 Still, in a large randomized trial, Sherman et al46 used Viniyoga style yoga for individuals with low back pain.
Some participants in our study had low back pain, but others had migraines, cancer related pain, stroke related pain, trauma or arthritis in other parts of the body, cervical neck pain, fibromyalgia, or neuropathies. As we included individuals with many types of pain in differing locations and stemming from many different causes, we were not able to target certain body parts or needs. We therefore delivered a more generalized yoga protocol that addressed the whole body and included breath work and meditation. We included language about listening to the body and not pushing through pain. The yoga teacher also included “letting go” of the pain during the practice and the meditation, and stated that sometimes the pain would not decrease or change, but that participants could change their relationship (interference) with the pain. This may have led to the significant improvements found in BPI interference and body response for the people in the yoga group (moderate effect size).
As this was a pilot study, we did not expect to see differences between yoga and usual care control groups, there was however a difference in body responsiveness and 2 of the CPSS domain scores at 8 weeks. CPSS scores were improved in pain management and physical functioning for individuals randomized to yoga. Perhaps, as yoga improves neural connectivity, executive functioning, and memory,47,48 participating in yoga may have enhanced comprehension of self-management education. Using yoga to change the internal conversation about pain may have allowed for the improvements in body responsiveness scores (or listening to your body), as well as pain-related interference, and self-efficacy. Additionally, yoga may be used as a coping tool, and may thereby enhance the ability to cope with pain.49 The delivery of our yoga protocol in this manner may have allowed for the improvement we found in pain interference in daily activities. Importantly, using the same yoga protocol for all participants, regardless of type or location of pain, increases the generalizability of the yoga program and allows participants to more easily transition to local beginner yoga classes that may be offered in the community.
In the yoga group, there were significant improvements in CPSS domain and total scores and SSMCD-6 scores. Improved scores indicate improved self-efficacy surrounding pain and chronic disease management. A moderate effect size was demonstrated for CPSS management and physical function. Participants in the yoga group and usual care control group both received self-management education, but there were no improvements found for people in the usual care control group. Additionally, self-management is effective with people with chronic pain and improves the ability to manage pain on a daily basis.50 Self-management interventions often include education regarding the importance of physical activity, however do not include guided activity. Also, individuals with pain are often fearful of movement or that exercise may elicit increased pain.51 We addressed the need of guided physical activity by adding yoga to ongoing self-management and provided a low intensity activity that was easily modified with less risk of increasing pain.
Limitations
This was a pilot RCT and therefore had limitations. We were not powered to detect differences between groups, instead, the sample size was simply based on the number of individuals who could be recruited in a short recruitment period. An additional limitation, is that on average, only about 75% of the yoga classes were attended. As common in smaller studies, results cannot be generalized because of the size of the study and also because the Clinic is in a smaller city in the Southwest United States. As this was a complex sample (ie, pain >10 years, high opioid use, high activity limitations due to pain), it may have been warranted to have a longer treatment duration to have greater treatment effects. Additionally, the Clinic is a safety net facility caring for people who are underserved and have less resources (ie, homelessness, poverty, low education rates). When basic needs are not met there are other challenges related to pain management and self-management that cannot be addressed with yoga. Most participants were not able to financially afford to continue with yoga outside of the Clinic, thus limiting sustainability of their improvements. However, the administrators at the Clinic witnessed the results of the study, and began to offer free weekly yoga classes. Finally, there was variance seen in multiple outcome measures at both baseline and follow up. These issues were controlled for and may be eliminated with a larger study, but may have affected results in our smaller pilot study.
Future Directions and Conclusion
In future studies, yoga should be compared with active exercise control groups but may also be added to pain specific self-management. Protocols that combine yoga and self-management education may also be helpful for other populations who suffer from chronic pain or who have other needs commonly addressed with self-management. Additionally, there may be a possibility to continue to transition yoga further into the community by taking yoga out of the clinic and making yoga more adaptable and affordable in the community. Our general yoga protocol appears to have worked for people with different types and location of pain and would therefore allow for use by increased number of people to improve pain related outcomes.
Acknowledgments
We thank Carol Chop, OTR, and Jodie Higgns, PTA, for teaching yoga in this study. We also thank all of the Colorado State University occupational therapy and social work students who assisted with the study. Finally, we thank Drs David Marchant and Tasha Marchant and Kathy Randall, along with other staff at the Family Medical Center where the study was completed.
Footnotes
Author Contributions: All authors were co-investigators on the grant and study and were therefore part of the study design. AAS and JDP were co–principal investigators. AAS and MVP developed the yoga intervention. AAS, CAF, and MVP were involved in managing day-to-day aspects of the study, including but not limited to recruitment, attending sessions, collecting data, analyzing data, and writing the paper. JLS managed all data analyses. MJB is an expert in pain and medications and worked with the team to review all medications and discuss medical adverse events. All authors were involved in data analysis, data interpretation, and paper review and revisions.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval: Institutional review board approval was received and all participants consented to being in the study.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Colorado State University Prevention Research Center; JDP is funded by a NIA career development award (K76AG059934).
References
- 1.Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain. 2012;13:715–724. [DOI] [PubMed] [Google Scholar]
- 2.Manchikanti L, Helm S, 2nd, Fellows B. et al. Opioid epidemic in the United States. Pain Physician. 2012;15(3 suppl):ES9–ES38. [PubMed] [Google Scholar]
- 3.Dart RC, Surratt HL, Cicero TJ. et al. Trends in opioid analgesic abuse and mortality in the United States. N Engl J Med. 2015;372:241–248. [DOI] [PubMed] [Google Scholar]
- 4.Bair MJ, Ang D, Wu J. et al. Evaluation of stepped care for chronic pain (ESCAPE) in veterans of the Iraq and Afghanistan conflicts: a randomized clinical trial. JAMA Intern Med. 2015;175:682–689. [DOI] [PubMed] [Google Scholar]
- 5.McCaffrey R, Frock TL, Garguilo H. Understanding chronic pain and the mind-body connection. Holist Nurs Pract. 2003;17:281–289. [DOI] [PubMed] [Google Scholar]
- 6.McCracken LM, Eccleston C. Coping or acceptance: what to do about chronic pain? Pain. 2003;105:197–204. [DOI] [PubMed] [Google Scholar]
- 7.National Institutes of Health. National pain strategy: a comprehensive population health-level strategy for pain. https://www.iprcc.nih.gov/sites/default/files/HHSNational_Pain_Strategy_508C.pdf. Accessed June 27, 2019.
- 8.Okoro CA, Zhao G, Li C, Balluz LS. Use of complementary and alternative medicine among USA adults with functional limitations: for treatment or general use? Complement Ther Med. 2011;19:208–215. [DOI] [PubMed] [Google Scholar]
- 9.Tul Y, Unruh A, Dick BD. Yoga for chronic pain management: a qualitative exploration. Scand J Caring Sci. 2011;25:435–443. [DOI] [PubMed] [Google Scholar]
- 10.Nayak NN, Shankar K. Yoga: a therapeutic approach. Phys Med Rehabil Clin N Am. 2004;15:783–789. [DOI] [PubMed] [Google Scholar]
- 11.Smith AJ, Greer T, Sheets T, Watson S. Is there more to yoga than exercise? Altern Ther Health Med. 2011;17:22–29. [PubMed] [Google Scholar]
- 12.Ott MJ. Yoga as a clinical intervention: pain control and stress reduction may be just a breath away. Adv Nurse Pract. 2002;10:81–90. [PubMed] [Google Scholar]
- 13.Dauwan M, Begemann MJ, Heringa SM, Sommer IE. Exercise improves clinical symptoms, quality of life, global functioning, and depression in schizophrenia: a systematic review and meta-analysis. Schizophr Bull. 2016;42:588–599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Menezes CB, Dalpiaz NR, Kiesow LG, Sperb W, Hertzberg J, Oliveira AA. Yoga and emotion regulation: A review of primary psychological outcomes and their physiological correlates. Psychol Neurosci. 2015;8:82–101. [Google Scholar]
- 15.Büssing A, Ostermann T, Lüdtke R, Michalsen A. Effects of yoga interventions on pain and pain-associated disability: a meta-analysis. J Pain. 2012;13:1–9. [DOI] [PubMed] [Google Scholar]
- 16.Posadzki P, Ernst E. Yoga for low back pain: a systematic review of randomized clinical trials. Clin Rheumatol. 2011;30:1257–1262. [DOI] [PubMed] [Google Scholar]
- 17.Posadzki P, Ernst E, Terry R, Lee MS. Is yoga effective for pain? A systematic review of randomized clinical trials. Complement Ther Med. 2011;19:281–287. [DOI] [PubMed] [Google Scholar]
- 18.Cramer H, Klose P, Brinkhaus B, Michalsen A, Dobos G. Effects of yoga on chronic neck pain: a systematic review and meta-analysis. Clin Rehabil. 2017;31:1457–1465. [DOI] [PubMed] [Google Scholar]
- 19.Chang DG, Holt JA, Sklar M, Groessl EJ. Yoga as a treatment for chronic low back pain: a systematic review of the literature. J Orthop Rheumatol. 2016;3:1–8. [PMC free article] [PubMed] [Google Scholar]
- 20.Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26:1–7. [DOI] [PubMed] [Google Scholar]
- 21.Cleeland CS. Measurement of pain by subjective report In: Chapman CR, Loeser JD, eds. Advances in Pain Research and Therapy. Vol 12 New York, NY: Raven Press; 1989:391–403. [Google Scholar]
- 22.Turk DC, Dworkin RH, Burke LB. et al. Developing patient-reported outcome measures for pain clinical trials: IMMPACT recommendations. Pain. 2006;125:208–215. [DOI] [PubMed] [Google Scholar]
- 23.Hays RD, Morales LS. The RAND-36 measure of health-related quality of life. Ann Med. 2001;33:350–357. [DOI] [PubMed] [Google Scholar]
- 24.Lins L, Carvalho FM. SF-36 total score as a single measure of health-related quality of life: scoping review. SAGE Open Med. 2016;4:2050312116671725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Anderson KO, Dowds BN, Pelletz RE, Edwards WT, Peeters-Asdourian C. Development and initial validation of a scale to measure self-efficacy beliefs in patients with chronic pain. Pain. 1995;63:77–83. [DOI] [PubMed] [Google Scholar]
- 26.Lorig K, Sobel D, Ritter P, Laurent D, Hobbs M. Effect of a self-management program on patients with chronic disease. Effect Clin Pract. 2001;4:256–262. [PubMed] [Google Scholar]
- 27.Daubenmier JJ. The relationship of yoga, body awareness, and body responsiveness to self-objectification and disordered eating. Psychol Women Q. 2005;29:207–219. [Google Scholar]
- 28.Phillips CE, Willis LA, Van Puymbroeck M, Tracy BL, Sample PL, Schmid AA. Yoga improves functional gait and quality of life for adults with diabetic peripheral neuropathy: a pilot study. Jacobs J Yoga Nat Med. 2016;1:002,1–8. [Google Scholar]
- 29.Boslego LW, Phillips CM, Atler EK, Tracy BL, Van Puymbroeck M, Schmid AA. Impact of yoga on balance, balance confidence and occupational performance for adults with diabetic peripheral neuropathy: a pilot study. Br J Occup Ther. 2017;80:155–162. [Google Scholar]
- 30.Kelley K, Preacher KJ. On effect size. Psychol Methods. 2012;17:137–152. [DOI] [PubMed] [Google Scholar]
- 31.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2d ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 32.Rosenthal JA. Qualitative descriptors of strength of association and effect size. J Soc Serv Res. 1996;21:37–59. [Google Scholar]
- 33.Vickers AJ, Altman DG. Statistics notes: analysing controlled trials with baseline and follow up measurements. BMJ. 2001;323:1123–1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wieland LS, Skoetz N, Pilkington K, Vempati R, D’Adamo CR, Berman BM. Yoga treatment for chronic non-specific low back pain. Cochrane Database Syst Rev. 2017;(1):CD010671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schmid AA, Van Puymbroeck M, Altenburger P. et al. Poststroke balance improves with yoga. Stroke. 2012;43:2402–2407. [DOI] [PubMed] [Google Scholar]
- 36.Schmid AA, Van Puymbroeck M, Portz JD, Atler KE, Fruhauf CA. Merging yoga and occupational therapy (MY-OT): a feasibility and pilot study. Complement Ther Med. 2016;28:44–49. [DOI] [PubMed] [Google Scholar]
- 37.Attanayake AP, Somarathna K, Vyas G, Dash S. Clinical evaluation of selected yogic procedures in individuals with low back pain. Ayu. 2010;31:245–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Saper RB, Sherman KJ, Cullum-Dugan D, Davis RB, Phillips RS, Culpepper L. Yoga for chronic low back pain in a predominantly minority population: a pilot randomized controlled trial. Altern Ther Health Med. 2009;15:18–27. [PMC free article] [PubMed] [Google Scholar]
- 39.Kuttner L, Chambers CT, Hardial J, Israel DM, Jacobson K, Evans K. A randomized trial of yoga for adolescents with irritable bowel syndrome. Pain Res Manag. 2006;11:217–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schmid AA, Miller KK, Van Puymbroeck M, DeBaun-Sprague E. Yoga leads to multiple physical improvements after stroke, a pilot study. Complement Ther Med. 2014;22:994–1000. [DOI] [PubMed] [Google Scholar]
- 41.Boyle CA, Sayers SP, Jensen BE, Headley SA, Manos TM. The effects of yoga training and a single bout of yoga on delayed onset muscle soreness in the lower extremity. J Strength Cond Res. 2004;18:723–729. [DOI] [PubMed] [Google Scholar]
- 42.Bosch PR, Traustadottir T, Howard P, Matt KS. Functional and physiological effects of yoga in women with rheumatoid arthritis: a pilot study. Altern Ther Health Med. 2009;15:24–31. [PubMed] [Google Scholar]
- 43.Yurtkuran M, Alp A, Yurtkuran M, Dilek K. A modified yoga-based exercise program in hemodialysis patients: a randomized controlled study. Complement Ther Med. 2007;15:164–171. [DOI] [PubMed] [Google Scholar]
- 44.Garfinkel MS, Singhal A, Katz WA, Allan DA, Reshetar R, Schumacher HR., Jr Yoga-based intervention for carpal tunnel syndrome: a randomized trial. JAMA. 1998;280:1601–1603. [DOI] [PubMed] [Google Scholar]
- 45.Williams K, Abildso C, Steinberg L. et al. Evaluation of the effectiveness and efficacy of Iyengar yoga therapy on chronic low back pain. Spine (Phila Pa 1976). 2009;34:2066–2076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sherman KJ, Cherkin DC, Erro J, Miglioretti DL, Deyo RA. Comparing yoga, exercise, and a self-care book for chronic low back pain: a randomized, controlled trial. Ann Intern Med. 2005;143:849–856. [DOI] [PubMed] [Google Scholar]
- 47.Gothe NP, Kramer AF, McAuley E. The effects of an 8-week Hatha yoga intervention on executive function in older adults. J Gerontol A Biol Sci Med Sci. 2014;69:1109–1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Eyre HA, Acevedo B, Yang HY. et al. Changes in neural connectivity and memory following a yoga intervention for older adults: a pilot study. J Alzheimers Dis. 2016;52:673–684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Crowe BM, Van Puymbroeck M, Schmid AA. Yoga as coping: a conceptual framework for meaningful participation in yoga. Int J Yoga Therap. 2016;26:123–129. [DOI] [PubMed] [Google Scholar]
- 50.Mann EG, LeFort S, VandenKerkhof EG. Self-management interventions for chronic pain. Pain Manag. 2013;3:211–222. [DOI] [PubMed] [Google Scholar]
- 51.Vlaeyen JW, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85:317–332. [DOI] [PubMed] [Google Scholar]