Midterm Results of Primary Total Knee Arthroplasty Using a Dished Polyethylene Insert with a Recessed or Resected Posterior Cruciate Ligament (original) (raw)
Midterm Results of Primary Total Knee Arthroplasty Using a Dished Polyethylene Insert with a Recessed or Resected Posterior Cruciate Ligament
Sathappan S. Sathappan, MD, Bradley Wasserman, BS, William L. Jaffe, MD, Matthew Bong, MD, Michael Walsh, PhD, and Paul E. Di Cesare, MD
Abstract
Use of a dished polyethylene insert in 114 total knee arthroplasties, all with the posterior cruciate ligament resected or recessed, was retrospectively studied. Patients were evaluated at a mean follow-up of 8.3 years. Mean range of motion increased from 92∘92^{\circ} to 111∘111^{\circ}. Mean Knee Society pain and function scores increased from 35.2 and 39.7 to 91.3 and 74.7 , respectively. WOMAC scores improved significantly in each category evaluated, including pain, stiffness, and physical function. Kaplan-Meier survivorship was 95%95 \% at 10 years ( 95%95 \% confidence interval, 82%−99%82 \%-99 \% ). The use of a dished polyethylene insert in primary total knee arthroplasty provides good to excellent midterm results regardless of whether the posterior cruciate ligament is recessed or sacrificed. Key words: dished polyethylene insert, total knee arthroplasty, outcome.
© 2006 Elsevier Inc. All rights reserved.
The management of the posterior cruciate ligament (PCL) with respect to total knee arthroplasty (TKA) design is a subject of current controversy. Among the reasons cited for using a PCL-preserving TKA system are femoral rollback, superior knee kinematics, and improved stair-climbing ability [1]. Posterior cruciate ligament-preserving designs use minimally conforming components, and such flat-on-flat configurations have been shown to result in abnormal screw home motion, higher peak contact forces, eccentric loading, and premature polyethylene lining wear [2-5].
[1]Introducing articular geometric conformity to a PCL-preserving system has not been recommended; such a design would result in kinematic conflict and compromised mechanics [6]. The alternative, TKA systems with PCL-substituting components, are reported to result in increased range of motion (ROM) [7-9]; furthermore, their conforming articular surfaces minimize premature wear of the polyethylene component and avoid compromised knee kinematics. Among the disadvantages of PCL-substituting systems are the need for additional resection of femoral bone from the intercondylar notch, potential wear at the femoral cam-polyethylene post interface, and abnormal gait patterns [1,10−12][1,10-12].
A more recent solution uses a highly conforming dished polyethylene insert and involves either recessing or resecting the PCL, dispensing with the posterior stabilized component altogether [13-15]. Given the articular geometric congruity between the tibial component and femoral component, the risk of premature wear of the polyethylene
- From the Department of Orthopaedic Surgery, Musculoskeletal Research Center, NYU-Hospital for Joint Diseases, New York, NY. Submitted December 22, 2004; accepted June 9, 2005. No benefits or funds were received in support of the study. Reprint requests: Paul E. Di Cesare, MD, Musculoskeletal Research Center, 15th Floor, 301 East 17th Street, New York, NY 10003 .
© 2006 Elsevier Inc. All rights reserved.
0883-5403/06/1906-0004$32.00/0
doi:10.1016/j.arth.2005.06.018 ↩︎
insert is greatly reduced. The present study reviewed the authors’ midterm experience with such a system, the Osteonics Series 7000 Total Knee System with Deltafit Keel.
Materials and Methods
A retrospective study approved by the Investigational Review Board was conducted of 114 knees in 77 consecutive patients undergoing primary TKA at the authors’ institution using a TKA system with a dished, metal-backed polyethylene tibial component (Osteonics Series 7000, Allendale, NJ). The only exclusion was patients who had undergone a prior tibial or femoral osteotomy.
The Osteonics Series 7000 system includes a cobalt-chromium femoral component, a cobaltchromium microstructured modular tibial component, a resurfacing polyethylene patella, and a tibial insert consisting of a “dished” ultrahigh-molecular-weight polyethylene liner with anterior and posterior constraints and a single mediallateral radius.
Two fellowship-trained adult reconstructive surgeons performed all surgeries. The surgical approach consisted of a midline incision followed by a medial parapatellar arthrotomy. Patients received perioperative cephazolin or, if they were allergic to penicillin, vancomycin. Posterior cruciate ligament recession or resection was performed in all cases depending on PCL tightness as assessed intraoperatively during flexion-extension gap balancing [16,17][16,17]. All prostheses were implanted using hand-mixed cement fixation of the femoral, tibial, and patellar components (Simplex, Howmedica, Rutherford, NJ). All varus-valgus deformities were corrected using appropriate soft tissue releases.
Postoperative rehabilitation protocol allowed all patients immediate weight bearing as tolerated on postoperative day 1. Low-molecular-weight heparin or coumadin was used for deep vein thrombosis prophylaxis.
Preoperative and latest follow-up Knee Society clinical scores, Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) [18], and radiographic assessments were used to evaluate patient outcomes [19]. Weight-bearing anteroposterior, lateral, and patellofemoral radiographs were obtained preoperatively and at each postoperative follow-up visit. All radiographs were evaluated by a single experienced surgeon not involved in the preoperative, operative, or postoperative clinical evaluation and were assessed using the Knee Society roentgenographic scoring system [20].
The prosthesis-bone interface was evaluated for the presence and/or progression of radiolucent lines. Progression of a radiolucent line was defined as an increase in length and/or width of 2 mm or greater on sequential radiographs. Component alignment and position were compared with previous radiographs to determine whether subsidence or loosening had occurred. Joint spaces, as evaluated on anteroposterior weight-bearing radiographs, were evaluated for asymmetry or changes in thickness (as measured with a magnification ruler) suggestive of polyethylene insert wear.
Statistical analysis was performed using paired Student tt tests (with significance set at P<.05P<.05 ). Survivorship was determined using Kaplan-Meier survivorship curves, with clinical or radiographic failure (defined as a revision of the tibial, femoral, or patellar components or any subsequent procedure that altered knee components) taken as the end point.
Results
The study cohort comprised 54 females and 23 males. Mean age at the time of operation was 68.4 years (range, 25-87 years); mean weight was 183 lb (range, 105-265 lb). Mean time from index surgery to most recent follow-up was 8.3 years (range, 5.0-12.4 years). There were 62 right and 52 left TKAs, 37 cases were performed as bilateral procedures. Preoperative diagnoses were osteoarthritis ( 93.9%93.9 \% ), rheumatoid arthritis ( 3.5%3.5 \% ), and avascular necrosis (2.6%)(2.6 \%).
Of the original 77 patients (114 knees), 10 patients ( 12 knees) died of causes unrelated to the surgery and 2 patients ( 3 knees) were unable to return for reevaluation; none of these knees had been revised and were therefore included in survivorship analysis only. Four knees in 3 patients (4%)(4 \%) were lost to follow-up.
At a mean follow-up of 8.3 years (range, 5.0−12.45.0-12.4 years), ROM had increased from a preoperative mean of 92∘92^{\circ} (range, 25∘−120∘25^{\circ}-120^{\circ} ) to 111∘111^{\circ} (range, 75∘−130∘75^{\circ}-130^{\circ} ) ( P<.001P<.001 ). Knee Society pain and function scores increased from means of 35.2 (range, 4-69) and 39.7 (range, 0-80) to 91.3 (range, 51-100) and 74.7 (range, 30-100), respectively (both P<.001P<.001 ). Results were good or excellent in 94%94 \% of knees ( 80 excellent, 9 good); 5 patients reported fair results and 1 patient had a poor outcome due to comorbid diseases. WOMAC analysis, graded on a scale of 0 to 4 , with 4 representing severe impairment, improved from mean normalized scores of 3.1 for pain (range, 1-4), 2.9 for stiffness (range, 0-4),
and 3.2 for physical function (range, 0.18−40.18-4 ) preoperatively to 0.5 (range, 0−30-3 ), 0.5 (range, 0−3.50-3.5 ), and 0.8 (range, 0−3.350-3.35 ), respectively (all P<.01P<.01 ), at most recent follow-up.
Radiographically, there were no instances of changes in prosthetic alignment or position. There was no gross evidence of thinning or asymmetry consistent with wear or failure of the tibial or femoral components with the exception of one patient, both of whose knees exhibited wear of the medial aspect of the polyethylene component and subsequently underwent revision. On anteroposterior radiographs, 4 knees ( 3.9%3.9 \% ) exhibited radiolucent lines in Knee Society zone 1 of the tibial component-bone interface; 1 radiolucent line (1.0%)(1.0 \%) was observed in zone 4 . On lateral radiographs, 2 knees ( 2.0%2.0 \% ) exhibited radiolucent lines in zone 1 of the tibial component-bone interface. All observed radiolucencies were less than 2 mm and were nonprogressive in subsequent films.
In 93 patients, the PCL was resected, and in 21 patients, it was recessed. On all measures (ROM, Knee Society scores, and WOMAC scores), there was no statistically significant difference between the two treatments (power 89%89 \%; see Table 1).
Three patients ( 4 knees) underwent revision. One patient, who suffered a fall 1 year after surgery, sustained a periprosthetic fracture of the lateral femoral condyle and underwent a successful femoral component revision with a long femoral stem and wedge augmentation to the lateral femoral condyle. This patient was functioning well for 8 years before her death from a stroke. A second revision followed a fall in which the patient sustained a tibial plateau fracture 38 months after the index TKA. This patient had failed 4 months of conservative treatment after the accident; subsequently, serial radiographs revealed medial subsidence and loosening of the tibial component. This patient underwent successful tibial component revision with a long-stem implant and wedge augmentation; 71/271 / 2 years later, the patient had
Table 1. Patient Outcome Scores, PCL Recession vs PCL Resection
| Recessed PCL (n=21)(\mathbf{n}=\mathbf{2 1}) | Resected PCL (n=93)(\mathbf{n}=\mathbf{9 3}) | PP | |
|---|---|---|---|
| ROM | 114 | 111 | .42 |
| Knee Society | 95 | 91 | .24 |
| \quad score (pain) | 80 | 74 | .25 |
| Knee Society | |||
| \quad score (function) | 11 | 19 | .13 |
| WOMAC score |
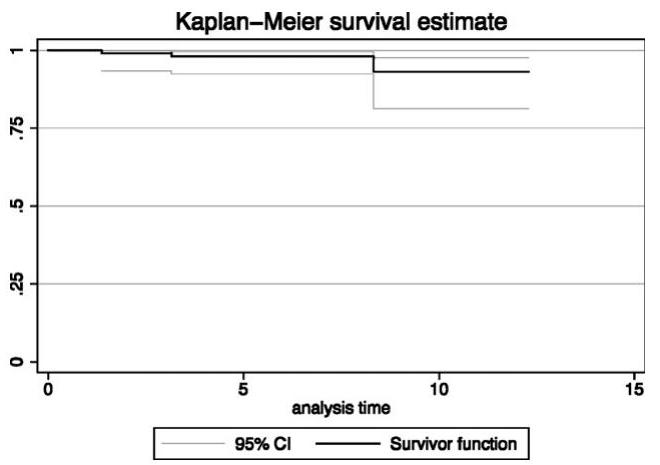
Fig. 1. Kaplan-Meier survivorship curve of TKA with dished polyethylene insert at 10 years.
no complaints of pain (Knee Society score 93) but ambulated with a cane due to severe osteoarthritis of the contralateral knee. A third patient with a body mass index of 45 had both knees revised 8 years after bilateral TKA due to a 1-year history of progressive bilateral knee pain and radiographic findings consistent with bilateral polyethylene wear of the medial aspect of the components. Intraoperatively, the femoral, tibial, and patellar components were found to be well fixed without evidence of loosening, although wear was observed on the medial aspects of both polyethylene components, which were exchanged without complication. At last follow-up, the patient was pain-free and ambulating without an assistive device.
Survivorship analysis using Kaplan-Meier survivorship curves yielded a clinical and radiographic survivorship of 95%95 \% ( 95%95 \% confidence interval, 82%−99%82 \%-99 \% ) at 10 years (Fig. 1).
Discussion
To avoid kinematic conflict, initial PCL-retaining designs used a flat-on-flat total condylar system that resulted in both abnormal kinematics and wear patterns. Stiehl et al [5] demonstrated that flat-on-flat condylar systems can give rise to femoral-tibial subluxation, posteroanterior sliding, lateral condyle liftoff, and erratic screw home motion. This would explain the abnormal wear characteristics of the polyethylene insert reported in studies of implants that use flat or minimally conforming articular surfaces, especially if the PCL is not properly balanced or later ruptures [2,3,5]. Hirakawa et al [21] noted in their studies of failed
TKAs that the flat tibial articular surfaces were associated with significantly larger and more numerous wear particles. Wear studies on 33 flat designed tibial insert revealed that 75%75 \% of cases had a rotationally asymmetric wear pattern [22].
The question therefore remains whether these concerns about PCL retention with flat-on-flat design apply if the tibial insert is highly congruent (ie, dished) and the PCL is recessed or resected. There is, however, little evidence to date to indicate whether it is necessary to substitute for the PCL with a boxed femoral component and a polyethylene post when the articulating geometry is conforming (ie, dished).
The case for using dished tibial polyethylene inserts is supported by the results of studies using normal cadaveric knees [23]. During axial loading, dishing of the menisci, especially at the medial and lateral edges, results in a “wedging” effect that produces increased stability between the femoral and tibial surfaces [23,24]. A search of the literature yielded only three articles on the outcomes of TKAs using highly congruent/dished polyethylene tibial inserts [13-15]. Laskin et al [14] compared a posterior stabilized tibial polyethylene insert with a dished polyethylene tibial insert and reported no statistically significant differences in ROM, ability to ascend and descend stairs, or knee scores. Scott and Thornhill [15] concluded that in cases with a retained, but balanced, PCL, dished tibial polyethylene inserts do not adversely affect ROM or tibial radiolucencies as compared with flat tibial polyethylene inserts. Font-Rodriguez et al [13], analyzing the long-term results of 215 total condylar prostheses with an all-polyethylene dished tibia, reported an average annual failure rate of 0.46%0.46 \% and a 21-year success rate of 90.77%90.77 \%. These studies suggest that the theoretical drawbacks of using a dished component when retaining the PCL-kinematic conflict or instability-do not apply clinically in the situation where the PCL is rendered incompetent by either resection or recession.
The current study assessed the midterm results of TKA performed with either a retained (but recessed) or sacrificed PCL with a dished polyethylene insert and no PCL substitution. There were no statistically significant differences (P<.05)(P<.05) between PCL recession and resection cases with regard to ROM, Knee Society scores, or WOMAC scores. In all cases, meticulous soft tissue balancing was performed [25].
These results are not unexpected: Bartel et al [26], who performed stress and strain analyses on several knee designs, cited the reduction in interlace stresses and polyethylene wear in systems with
conforming articulating surfaces and concluded on this basis that they were superior to the other articulations they studied. The present study revealed that both PCL-preserving and PCL-sacrificing techniques with a dished polyethylene insert resulted in excellent survivorship and functional outcomes. No cases of femorotibial instability were observed even when the PCL was sacrificed and not substituted for, indicating that the dished tibial polyethylene insert is sufficient for anteroposterior knee stability when the knee is properly balanced in flexion and extension and the mechanical axis of the knee restored. Furthermore, survivorship and clinical outcome results ( 94%94 \% of knees had good or excellent results with no evidence of radiographic loosening) are comparable with those of other TKA systems [13,27,28]. In conclusion, primary TKA using a dished polyethylene component yields good or excellent midterm outcomes when the PCL is recessed or resected.
Acknowledgment
The authors thank Samuel Park, MD, for his assistance on this project.
References
Andriacchi TP, Galante JO, Fermier RW. The influence of total knee-replacement design on walking and stair-climbing. J Bone Joint Surg Am 1982; 64:1328.
Feng EL, Stulberg SD, Wixson RL. Progressive subluxation and polyethylene wear in total knee replacements with flat articular surfaces. Clin Orthop 1994;60.
Lewis P, Rorabeck CH, Bourne RB, et al. Posteromedial tibial polyethylene failure in total knee replacements. Clin Orthop 1994;11.
Soudry M, Walker PS, Reilly DT, et al. Effects of total knee replacement design on femoral-tibial contact conditions. J Arthroplasty 1986;1:35.
Stiehl JB, Komistek RD, Dennis DA. Detrimental kinematics of a flat on flat total condylar knee arthroplasty. Clin Orthop 1999;139.
Vince KG. Principles of condylar knee arthroplasty: issues evolving. Instr Course Lect 1993;42:315.
Dennis DA, Komistek RD, Stiehl JB, et al. Range of motion after total knee arthroplasty: the effect of implant design and weight-bearing conditions. J Arthroplasty 1998;13:748.
Hirsch HS, Lotke PA, Morrison LD. The posterior cruciate ligament in total knee surgery. Save, sacrifice, or substitute? Clin Orthop 1994;64.
Tanzer M, Smith K, Burnett S. Posterior-stabilized versus cruciate-retaining total knee arthroplasty: balancing the gap. J Arthroplasty 2002;17:813.
Dorr LD, Ochsner JL, Gronley J, et al. Functional comparison of posterior cruciate-retained versus cruciate-sacrificed total knee arthroplasty. Clin Orthop 1988;36.
Mikulak SA, Mahoney OM, dela Rosa MA, et al. Loosening and osteolysis with the press-fit condylar posterior-cruciate-substituting total knee replacement. J Bone Joint Surg Am 2001;83-A:398.
Puloski SK, McCalden RW, MacDonald SJ, et al. Tibial post wear in posterior stabilized total knee arthroplasty. An unrecognized source of polyethylene debris. J Bone Joint Surg Am 2001;83-A:390.
Font-Rodriguez DE, Scuderi GR, Insall JN. Survivorship of cemented total knee arthroplasty. Clin Orthop 1997;79.
Laskin RS, Maruyama Y, Villaneuva M, et al. Deepdish congruent tibial component use in total knee arthroplasty: a randomized prospective study. Clin Orthop 2000;36.
Scott RD, Thornhill TS. Posterior cruciate supplementing total knee replacement using conforming inserts and cruciate recession. Effect on range of motion and radiolucent lines. Clin Orthop 1994;146.
Arima J, Whiteside LA, Martin JW, et al. Effect of partial release of the posterior cruciate ligament in total knee arthroplasty. Clin Orthop 1998;194.
Ritter MA, Faris PM, Keating EM. Posterior cruciate ligament balancing during total knee arthroplasty. J Arthroplasty 1988;3:323.
Bellamy N, Buchanan WW, Goldsmith CH, et al. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 1988;15:1833.
Insall JN, Dorr LD, Scott RD, et al. Rationale of the Knee Society clinical rating system. Clin Orthop 1989;13.
Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop 1989:9.
Hirakawa K, Bauer TW, Yamaguchi M, et al. Relationship between wear debris particles and polyethylene surface damage in primary total knee arthroplasty. J Arthroplasty 1999;14:165.
Benjamin J, Szivek J, Dersam G, et al. Linear and volumetric wear of tibial inserts in posterior cruciateretaining knee arthroplasties. Clin Orthop Relat Res 2001;131.
Hsieh HH, Walker PS. Stabilizing mechanisms of the loaded and unloaded knee joint. J Bone Joint Surg Am 1976;58:87.
Markolf KL, Bargar WL, Shoemaker SC, et al. The role of joint load in knee stability. J Bone Joint Surg Am 1981;63:570.
Scott RD, Volatile TB. Twelve years’ experience with posterior cruciate-retaining total knee arthroplasty. Clin Orthop 1986;100.
Bartel DL, Rawlinson JJ, Burstein AH, et al. Stresses in polyethylene components of contemporary total knee replacements. Clin Orthop 1995;76.
Rand JA, Ilstrup DM. Survivorship analysis of total knee arthroplasty. Cumulative rates of survival of 9200 total knee arthroplasties. J Bone Joint Surg Am 1991;73:397.
Scuderi GR, Insall JN, Windsor RE, et al. Survivorship of cemented knee replacements. J Bone Joint Surg Br 1989;71:798.