Implementing Optimal Team-Based Care to Reduce Clinician Burnout (original) (raw)
Abstract
AI
This research focuses on enhancing clinician well-being through optimal team-based care in healthcare settings. It identifies key characteristics of successful healthcare teams, discusses the significance of these teams in achieving shared healthcare goals, and reviews strategies to address barriers in establishing effective team dynamics. The paper emphasizes the importance of cultivating an enabling environment for teamwork, which positively impacts both clinician satisfaction and patient outcomes.
Figures (2)
Table 1 | Principles of High-Performing Teams SOURCE: Smith et al., “Implementing optimal team-based care to reduce clinician burnout,” National Academy of Medicine. NOTES: [a] Mitchell, P., M. Wynia, R. Golden, B. McNellis, S. Okun, C. E. Webb, V. Rohrbach, and I. V. Kohorn. 2012. Core principles and values of effective team-based health care. Discussion Paper, Institute of Medicine, Washington, DC; [b] So, T. T. C., M.A West, and J. F. Dawson. 2011. Team-based working and employee well-being: A crosscultural comparison of United Kingdorr and Hong Kong health services. European Journal of Work and Organizational Psychology 20(3):305-325; [c] Brunetto, Y., R. F Wharton, and K. Shacklock. 2011. Supervisor-nurse relationships, teamwork, role ambiguity and well-being: Public versus private sector nurses. Asia Pacific Journal of Human Resources 49(2):143-164; [d] Cheng, C., T. Bartram, L. Karimi, and S. G. Leggat. 2013 The role of team climate in the management of emotional labour: Implications for nurse retention. Journal of Advanced Nursing 69(12):2812-2825; [e] Estryn-Béhar, M., B. |. Van der Heijden, H. Oginska, D. Camerino, O. Le Nezet, P. M. Conway, C. Fry, H. M. Has: selhorn, and NEXT Study Group. 2007. The impact of social work environment, teamwork characteristics, burnout, and persona factors upon intent to leave among European nurses. Medical Care 45(10):939-950; [f] Bodenheimer, T., and R. Willard-Grace 2016. Teamlets in primary care: Enhancing the patient and clinician experience. Journal of the American Board of Family Medicine 29(1):135-138; [g] Helfrich, C. D., E. D. Dolan, J. Simonetti, R. J. Reid, S. Joos, B. J. Wakefield, G. Schectman, R. Stark, S. D. Fihn, H. B Harvey, and K. Nelson. 2014. Elements of team-based care in a patient-centered medical home are associated with lower burnout among VA primary care employees. Journal of General Internal Medicine 29(SUPPL. 2):S659-S666; [h] Catt, S., L. Fallowfield, V Jenkins, C. Langridge, and A. Cox. 2005. The informational roles and psychological health of members of 10 oncology multidisci plinary teams in the UK. British Journal of Cancer 93(10):1092-1097.
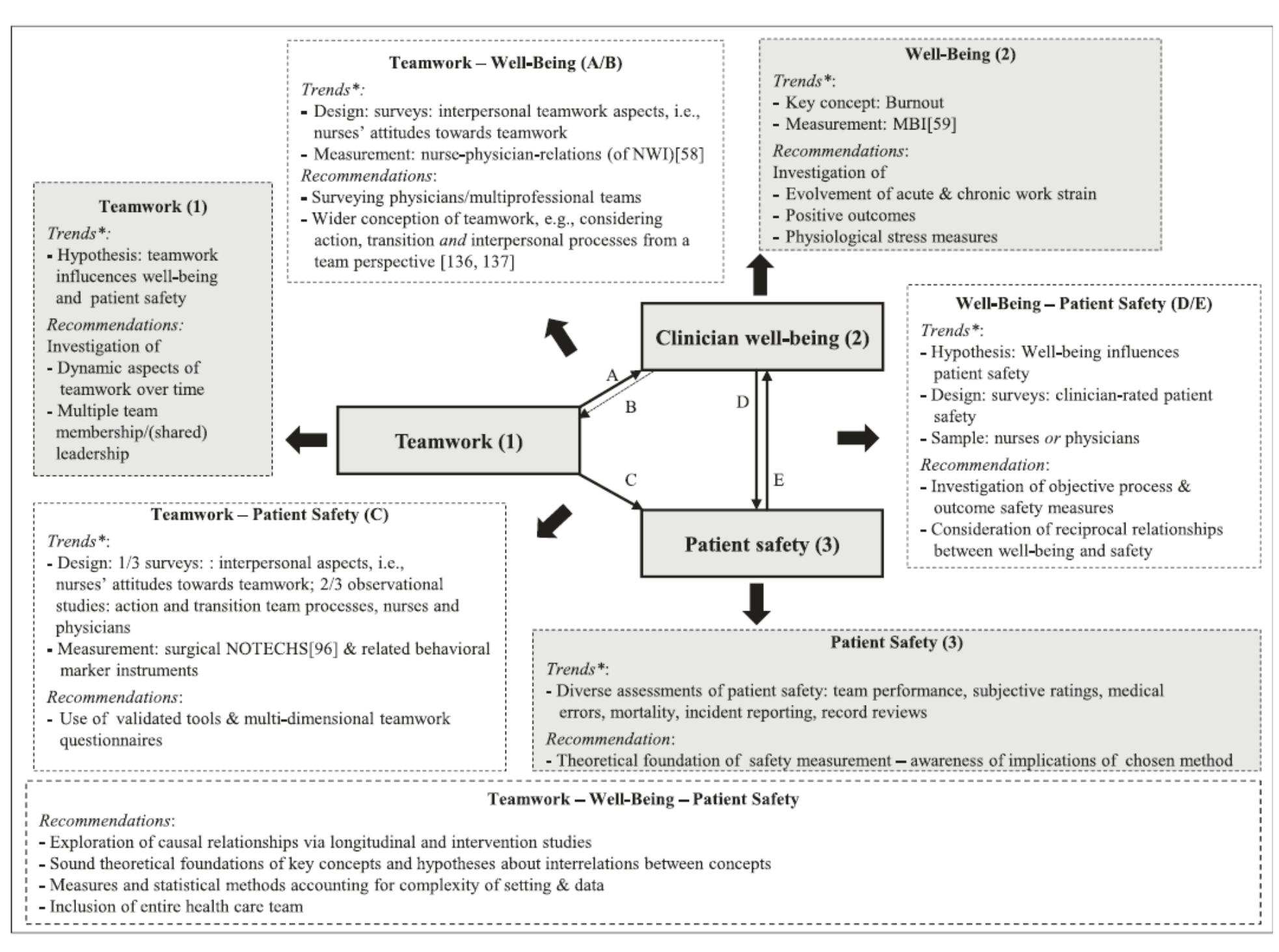
FIGURE 1 | Integrative Framework of Teamwork, Clinician Occupational Well-Being, and Patient Safety in Hospital Settings

Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
References (54)
- Welp, A., and T. Manser. 2016. Integrating team- work, clinician occupational well-being and patient safety-development of a conceptual framework based on a systematic review. BMC Health Services Research 16(1):281.
- Naylor, M. D., K. D. Coburn, E. T. Kurtzman, J. P. Bet- tger, H. G. Buck, J. V. Cleave, and C. A. Cott. 2010. Inter-professional team-based primary care for chroni- cally ill adults: State of the science. Unpublished white paper presented at the ABIM Foundation Meeting to Advance Team-Based Care for the Chronically Ill in Ambulatory Settings, Philadelphia, PA.
- Mitchell, P., M. Wynia, R. Golden, B. McNellis, S. Okun, C. E. Webb, V. Rohrbach, and I. V. Kohorn. 2012. Core principles and values of effective team-based health care. Discussion Paper, Institute of Medicine, Wash- ington, DC.
- American College of Obstetricians and Gynecolo- gists. 2016. Collaboration in practice: Implementing team based care. Washington, DC.
- Hackman, R. 2014. What makes for a great team? Washington, DC: American Psychological Associa- tion.
- Gordon, S., D. L. Feldman, and M. Leonard. 2014. Col- laborative caring: Stories and reflections on teamwork in health care. Ithaca, NY: Cornell University Press.
- Bodenheimer, T., and R. Willard-Grace. 2016. Team- lets in primary care: Enhancing the patient and cli- nician experience. Journal of the American Board of Family Medicine 29(1):135-138.
- Agency for Healthcare Research and Quality. 2014. TeamSTEPPS long-term care implementation guide. https://www.ahrq.gov/teamstepps/longtermcare/ implement/implguide.html (accessed November 22, 2017).
- Pape, G. A., J. S. Hunt, K. L. Butler, J. Siemienczuk, B. H. LeBlanc, W. Gillanders, Y. Rozenfeld, and K. Bo- nin. 2011. Team-based care approach to cholesterol management in diabetes mellitus: Two-year cluster randomized controlled trial. Archives of Internal Med- icine 171(16):1480-1486.
- Groenestege-Kreb, D. T., O. Van Maarseveen, and L. Leenen. 2014. Trauma team. British Journal of Anaes- thesia 113(2):258-265.
- Roberts, M. S., J. A. Stokes, M. A. King, T. A. Lynne, D. M. Purdie, P. P. Glasziou, D. A. J. Wilson, S. T. Mc- Carthy, G. E. Brooks, F. J. de Looze, and C. B. Del Mar. 2001. Outcomes of a randomized controlled trial of a clinical pharmacy intervention in 52 nursing homes. British Journal of Clinical Pharmacology 51(3):257-265.
- Njie, G. J., K. K. Proia, A. B. Thota, R. K. C. Thota, D. P. Hopkins, S. M. Banks, D. B. Callahan, N. P. Pronk, K. J. Rask, D. T. Lackland, T. E. Kottke, and Community Preventive Services Task Force. 2015. Clinical deci- sion support systems and prevention: A commu- nity guide cardiovascular disease systematic review. American Journal of Preventive Medicine 49(5):784- 795.
- Panattoni, L., L. Hurlimann, C. Wilson, M. Durbin, and M. Tai-Seale. 2017. Workflow stan- dardization of a novel team care model to im- prove chronic care: A quasi-experimental study. BMC Health Services Research 17(1):286.
- Chang, H., Y. Liu, M. Lu, S. Jou, Y. Yang, D. Lin, K. H. Lin, K. Tzen, R. Yen, C. C. Lu, C. J. Liu, S. S. Peng, Y. Jeng, S. Huang, H. Lee, H. F. Juan, M. Huang, Y. Liao, Y. Lee, and W. Hsu. 2016. A multidisciplinary team care approach improves outcomes in high-risk pedi- atric neuroblastoma patients. Oncotarget 8(3):4360- 4372.
- Jacob, V., S. K. Chattopadhyay, A. B. Thota, K. K. Pro- ja, G. Njie, D. P. Hopkins, R. K. C. Finnie, N. P. Pronk, T. E. Kottke, and Community Preventive Services Task Force. 2015. Economics of team-based care in controlling blood pressure: A community guide sys- tematic review. American Journal of Preventive Medi- cine 49(5):772-783.
- Reiss-Brennan, B., K. D. Brunisholz, C. Dredge, P. Briot, K. Grazier, A. Wilcox, L. Savitz, and B. James. 2016. Association of integrated team-based care with health care quality, utilization, and cost. JAMA 316(8):826-834.
- Manser, T. 2009. Teamwork and patient safety in dynamic domains of healthcare: A review of the literature. Acta Anaesthesiologica Scandinavica 53(2):143-151.
- Wang, S. M., P. T. Kung, W. H. Wang, K. H. Huang, and W. C. Tsai. 2014. Effects of multidisciplinary team care on utilization of emergency care for pa- tients with lung cancer. American Journal of Managed Care 20(8):e353-364.
- Schubert, C. C., L. J. Myers, K. Allen, and S. R. Coun- sell. 2016. Implementing geriatric resources for as- sessment and care of elders team care in a Veterans Affairs medical center: Lessons learned and effects observed. Journal of the American Geriatrics Society 64(7):1503-1509.
- Mundt, M. T., V. J. Gilchrist, M. F. Fleming, L. I. Zak- letskia, W. Tuan, and J. W. Beasley. 2015. Effects of primary care team social networks on quality of care and costs for patients with cardiovascular disease. Annals of Family Medicine 13(2):139-148.
- Dyrbye, L. N., T. D. Shanafelt, C. A. Sinsky, P. F. Cipriano, J. Bhatt, A. Ommaya, C. P. West, and D. Meyers. 2017. Burnout among health care profes- sionals: A call to explore and address this under- recognized threat to safe, high-quality care. NAM Perspectives. Discussion Paper, National Acad- emy of Medicine, Washington, DC. https://nam. edu/Burnout-Among-Health-Care-Professionals.
- Dehn, R. W., D. M. Brock, A. O. Keller, R. S. Hooker, D. Mittman. 2015. Commentaries on health services research. Journal of the American Academy of Physi- cian Assistants 28(6):1-3.
- Willard-Grace, R., D. Hessler, E. Rogers, K. Dubé, E. Bodenheimer, and K. Grumbach. 2014. Team struc- ture and culture are associated with lower burnout in primary care. Journal of the American Board of Family Medicine 27:229-238.
- Day, A. L., A. Sibley, N. Scott, J. M. Tallon, and S. Ack- royd-Stolarz. 2009. Workplace risks and stressors as predictors of burnout: The moderating impact of job control and team efficacy. Canadian Journal of Administrative Sciences 26:7-22.
- Lin, Y., and Y. Huang. 2014. Team climate, emo- tional labor and burnout of physicians: A multilevel model. Journal of Taiwan Public Health 33(3):271-289.
- Mijakoski, D., J. Bislimovska, M. Milosevic, and J. Mi- nov. 2015. Differences in burnout, work demands and team work between Croatian and Macedonian hospital nurses. Cognition, Brain, Behavior 19(3):179- 200.
- So, T. T. C., M. A. West, and J. F. Dawson. 2011. Team-based working and employee well-being: A crosscultural comparison of United Kingdom and Hong Kong health services. European Journal of Work and Organizational Psychology 20(3):305-325.
- Stout, S., L. Zallman, L. Arsenault, A. Sayah, and K. Hacker. 2017. Developing high-functioning teams: Factors associated with operating as a "real team" and implications for patient-centered medical home development. Inquiry (54).
- Hooker, R. S., J. Cawley, C. Everett, and D. M. Brock. 2017. Commentaries on health services research. Journal of the American Academy of Physician Assis- tants 30(8):1-3.
- Hastings, S. E., E. Suter, J. Bloom, and K. Shar- ma. 2016. Introduction of a team-based care model in a general medical unit. BMC Health Services Re- search 16(1):245.
- Hunt, J. S., J. Siemienczuk, G. Pape, Y. Rozen- feld, J. MacKay, B. H. LeBlanc, and D. Touchette. 2008. A randomized controlled trial of team- based care: Impact of physician-pharmacist col- laboration on uncontrolled hypertension. Jour- nal of General Internal Medicine 23(12):1966-1972.
- Kawamoto, K., K. J. Anstrom, J. B. Anderson, H. B. Bosworth, D. F. Lobach, C. M. Marx, J. M. Ferranti, H. Shang, and K. S. H. Yarnall. 2016. Long-term impact of an electronic health record-enabled, team-based, and scalable population health strategy based on the chronic care model. AMIA Annual Symposium Pro- ceedings: 686-695.
- Hackman, J. R. 1990. Teams that work (and those that don't): Creating conditions for effective teamwork. Somerset, NJ: Jossey-Bass.
- Salas, E., S. Zajac, and S. L. Marlow. 2018. Trans- forming health care one team at a time: Ten obser- vations and the trail ahead. Group & Organization Management 43(3): 357-381.
- Ommaya, A. K., P. F. Cipriano, D. B. Hoyt, K. A. Hor- vath, P. Tang, H. L. Paz, M. S. DeFrancesco, S. T. Hin- gle, S. Butler, and C. A. Sinsky. 2018. Care-centered clinical documentation in the digital environment: Solutions to alleviate burnout. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://nam.edu/care-centered- clinical-documentation-digital-environment-solu- tions-alleviate-burnout.
- Drawz, P. E., P. Archdeacon, C. J. McDonald, N. R. Powe, K. A. Smith, J. Norton, D. E. Williams, U. D. Pa- tel, and A. Narva. 2015. CKD as a model for improv- ing chronic disease care through electronic health records. Clinical Journal of the American Society of Ne- phrology 10(8):1488-1499.
- Clark, C. 2016. 10 ways EHRs lead to burnout. Fam- ily Practice News Digital Network, March 28.
- Baldwin J. L., H. Singh, D. F. Sittig, and T. D. Giar- dina. 2017. Patient portals and health apps: Pitfalls, promises, and what one might learn from the other symptoms. Healthcare 5:81-85.
- O'Leary, K. J., D. B. Wayne, C. Haviley, M. E. Slade, J. Lee, and M. V. Williams. 2010. Improving teamwork: Impact of structured interdisciplinary rounds on a medical teaching unit. Journal of General Internal Medicine 25(8):826-832.
- Weller, J., M. Boyd, and D. Cumin. 2014. Teams, tribes and patient safety: Overcoming barriers to ef- fective teamwork in healthcare. Postgraduate Medi- cal Journal 90(1061):149-154.
- Accreditation Council for Pharmacy Education. 2016. Accreditation standards and key elements for the professional program in pharmacy lead- ing to the doctor of pharmacy degree. Chicago.
- Network for Regional Healthcare Improvement. 2016. Accelerating the implementation of value-based care and payment: Recommendations from the 2016 National Payment Reform Summit. Portland, ME: http://www.nrhi.org/uploads/2016\_nationalpay- mentreformsummit.pdf.
- Wohler, D. M., and W. Liaw. 2016. Team-based pri- mary care: Opportunities and challenges. https:// www.graham-center.org/content/dam/rgc/docu- ments/publications-reports/reports/StarfieldSum- mit_Report_TeamBasedPrimaryCare.pdf.
- Centers for Medicare and Medicaid Services (CMS). 2017. MACRA. https://www.cms.gov/Medicare/ Quality-Initiatives-Patient-Assessment-Instruments/ Value-Based-Programs/MACRA-MIPS-and-APMs/ MACRA-MIPS-and-APMs.html (accessed November 30, 2017).
- CMS. Alternative payment model (APM) design toolkit. Washington, DC. https://www.cms.gov/Medicare/ Quality-Payment-Program/Resource-Library/Alter- native-Payment-Model-APM-Design-Toolkit.pdf.
- Milken Institute. A closer look at alternative payment models. Santa Monica, CA. http://www.fastercures. org/assets/Uploads/PDF/VC-Brief-AlternativePay- mentModels.pdf.
- Bodenheimer, T., and C. Sinsky. 2014. From triple to Quadruple Aim: Care of the patient requires care of the provider. Annals of Family Medicine 12(6):573- 576.
- Dehmer, S. P., M. M. Baker-Goering, M. V. Maci- osek, Y. Hong, T. E. Kottke, K. L. Margolis, J. C. Will, T. J. Flottemesch, A. B. LaFrance, B. C. Martinson, A. J. Thomas, and K. Roy. 2016. Modeled health and eco- nomic impact of team-based care for hypertension. American Journal of Preventive Medicine 50(5):S34- S44.
- Brunetto, Y., R. F. Wharton, and K. Shacklock. 2011. Supervisor-nurse relationships, teamwork, role am- biguity and well-being: Public versus private sec- tor nurses. Asia Pacific Journal of Human Resources 49(2):143-164.
- Hopkins, K. D., and C. A. Sinsky. 2014. Physicians can maximize their time -and their practice's in- come -by delegating more documentation tasks to well-trained staff. Family Practice Management 21(6):23-29.
- Berry, L. L., and D. Beckham. 2014. Team-based care at Mayo Clinic: A model for ACOs. Journal of Healthcare Management 59(1):9-13.
- Cromp, D., C. Hsu, K. Coleman, P. A. Fishman, D. T. Liss, K. Ehrlich, E. Johnson, T. R. Ross, C. Trescott, B. Trehearne, and R. J. Reid. 2015. Barriers and facilita- tors to team-based care in the context of primary care transformation. Journal of Ambulatory Care Management 38(2):125-133.
- DOI 10.31478/201809c
- Suggested Citation Smith, C. D., C. Balatbat, S. Corbridge, A. L. Dopp, J. Fried, R. Harter, S. Landefeld, C. Martin, F. Opelka, L. Sandy, L. Sato, and C. Sinsky. 2018. Implementing optimal team-based care to reduce clinician burnout. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://nam.edu/ implementing-optimal-team-based-care-to-reduce- clinician-burnout. doi: 10.31478/201809c
![Table 1 | Principles of High-Performing Teams SOURCE: Smith et al., “Implementing optimal team-based care to reduce clinician burnout,” National Academy of Medicine. NOTES: [a] Mitchell, P., M. Wynia, R. Golden, B. McNellis, S. Okun, C. E. Webb, V. Rohrbach, and I. V. Kohorn. 2012. Core principles and values of effective team-based health care. Discussion Paper, Institute of Medicine, Washington, DC; [b] So, T. T. C., M.A West, and J. F. Dawson. 2011. Team-based working and employee well-being: A crosscultural comparison of United Kingdorr and Hong Kong health services. European Journal of Work and Organizational Psychology 20(3):305-325; [c] Brunetto, Y., R. F Wharton, and K. Shacklock. 2011. Supervisor-nurse relationships, teamwork, role ambiguity and well-being: Public versus private sector nurses. Asia Pacific Journal of Human Resources 49(2):143-164; [d] Cheng, C., T. Bartram, L. Karimi, and S. G. Leggat. 2013 The role of team climate in the management of emotional labour: Implications for nurse retention. Journal of Advanced Nursing 69(12):2812-2825; [e] Estryn-Béhar, M., B. |. Van der Heijden, H. Oginska, D. Camerino, O. Le Nezet, P. M. Conway, C. Fry, H. M. Has: selhorn, and NEXT Study Group. 2007. The impact of social work environment, teamwork characteristics, burnout, and persona factors upon intent to leave among European nurses. Medical Care 45(10):939-950; [f] Bodenheimer, T., and R. Willard-Grace 2016. Teamlets in primary care: Enhancing the patient and clinician experience. Journal of the American Board of Family Medicine 29(1):135-138; [g] Helfrich, C. D., E. D. Dolan, J. Simonetti, R. J. Reid, S. Joos, B. J. Wakefield, G. Schectman, R. Stark, S. D. Fihn, H. B Harvey, and K. Nelson. 2014. Elements of team-based care in a patient-centered medical home are associated with lower burnout among VA primary care employees. Journal of General Internal Medicine 29(SUPPL. 2):S659-S666; [h] Catt, S., L. Fallowfield, V Jenkins, C. Langridge, and A. Cox. 2005. The informational roles and psychological health of members of 10 oncology multidisci plinary teams in the UK. British Journal of Cancer 93(10):1092-1097.](https://figures.academia-assets.com/76544772/table_001.jpg) ](
](