On the significance of Surfactant Protein-A within the human lungs (original) (raw)
On the significance of Surfactant Protein-A within the human lungs
Torsten Goldmann*, Daniel Kähler, Holger Schultz, Mahdi Abdullah, Dagmar S Lang, Florian Stellmacher and Ekkehard Vollmer
Address: Division for Clinical and Experimental Pathology, Research Center Borstel, Borstel, Germany
Email: Torsten Goldmann* - tgoldmann@fz-borstel.de; Daniel Kähler - dkaehler@fz-borstel.de; Holger Schultz - hschultz@fz-borstel.de; Mahdi Abdullah - mabdull@fz-borstel.de; Dagmar S Lang - dlang@fz-borstel.de; Florian Stellmacher - fstellmacher@fz-borstel.de; Ekkehard Vollmer - evollmer@fz-borstel.de
- Corresponding author
Published: 12 March 2009
Received: 6 March 2009
Diagnostic Pathology 2009, 4:8 doi:10.1186/1746-1596-4-8
Accepted: 12 March 2009
This article is available from: http://www.diagnosticpathology.org/content/4/1/8
© 2009 Goldmann et al; licensee BioMed Central Ltd.
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0). which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Surfactant Protein-A (SP-A) is the most prominent among four proteins in the pulmonary surfactant-system. SP-A is expressed by alveolar epithelial cells type II as well as by a portion of non small cell lung carcinomas (NSCLC).
The expression of SP-A is complexly regulated on the transcriptional and the chromosomal level. SP-A is a major player in the pulmonary cytokine-network and moreover has been described to act in the pulmonary host defense.
By the use of cell culture or animal models the functional properties have been repeatedly shown in many aspects, often bearing surprising properties which strongly indicate the physiological importance of SP-A. To date SP-A is recognized as a molecule essential for pulmonary development, structure and function. An upcoming number of reports deals with the role of SP-A for pulmonary pathology. This article gives an overview about the state of knowledge on SP-A focused in applications for human pulmonary disorders and points out the importance for pathology-orientated research approaches using immunohistochemistry or in situ hybridization as promising methods to further elucidate the role of this molecule in adult lung diseases.
Review
Surfactant
The role of the surfactant system for the development of the human lung is known to be essential. Since it is synthesized by humans starting in the 28th 28^{\text {th }} week of pregnancy and reaching functional levels in the 34th 34^{\text {th }} week, surfactant-substitution-therapy is a fundamental part of the treatment of premature babies suffering from Infant Respiratory Distress Syndrome (IRDS)[1].
Pulmonary surfactant regulates dynamically the alveolar surface tension. The central role of the surfactant system
for maintaining pulmonary function has been repeatedly shown by the use of cell culture or animal models [2].
Surfactant is a complex mixture of lipids, carbohydrates and four proteins (SP-A, SP-B, SP-C, SP-D). The initial descriptions of surfactant lead back to the 1950s, but little attention was given to the surfactant proteins until the 1980s [3]. The genes coding for these proteins are located on different chromosomes. SP-B and SP-C are similarly structured hydrophobic proteins participating in the adsorption of phospholipids at the alveolar border, which leads to rapid reduction of the surface tension. The
hydrophilic proteins SP-A and SP-D are members of the collectins with C-type lectin domains. SP-D together with SP-A play a role in the pulmonary defense against Gramnegative bacteria [4].
SP-A: biochemical properties and genetic organization
SP-A is the major surfactant apoprotein exhibiting complex interactions and participation in processes fundamental for pulmonary structure and function with its expression restricted to alveolar epithelial cells type II. Moreover expression of SP-A was also described for a portion of NSCLC facilitating a diagnostic marker for these carcinomas [5,6]. After characterization of the biochemical properties, a complex chromosomal organization of the genes coding for SP-A has been demonstrated [3]. The locus of the SP-A on the one hand consists of two functionally active genes and a pseudogene [7,8]. The two active genes SP-A1 and SP-A2 on the other hand display several different alleles and splicing variants, moreover different oligomeric states have been described [3,9]. During the development of the lung these two genes are regulated differentially, a process triggered by cAMP and glucocorticoids [10]. The SP-A1 and SP-A2 genes display a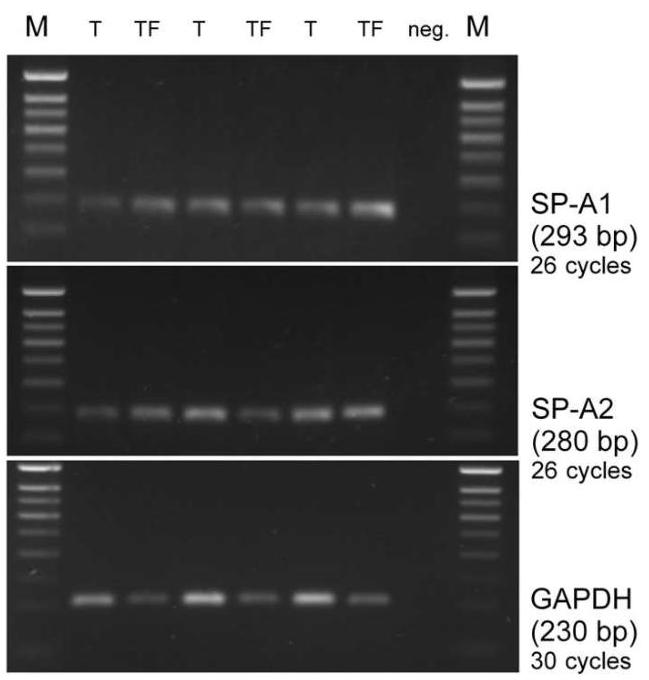
2%2 \% Agarose, Etb.
Figure I
RT-PCR: Transcription of SP-A1 and SP-A2 in NSCLC tumors (T) and corresponding tumor-free tissues (TF) from the same cases in comparison to GAPDH.
homology of 94%94 \% in their nucleotide sequences and even 96%96 \% homology in the amino acid sequences [11]. Fig. 1, as one example, shows the transcriptional activity of the SP-A1 and SP-A2 genes determined by RT-PCR in homogenates of biopsies from NSCLC and corresponding tumor-free samples. The importance of the differential transcription of SP-A1 and SP-A2 for maintaining pulmonary function has repeatedly been demonstrated [12]. Phylogenetic analyses revealed that an ancestor proto-SPA gene was diverged into SP-A1 and a second gene which subsequently emerged to SP-A2 and the SP-A pseudogene [3]. The high level of homology between SP-A1 and SP-A2 up to date prevents a differential analysis of the two gene products in situ. The expression of SP-A is also complexly regulated on the transcriptional level. Moreover the pro-tein-turnover and the release of SP-A into the serum represents a further point of regulation [12]. This sophisticated regulation of the genetic activity is recognized as a further hint for the functional importance of SP-A.
SP-A in pulmonary diseases
In recent years the role of defects in the expression of SPA in context with different pulmonary diseases has become an issue of scientific investigations. Initially numerous studies have been performed to elucidate the role of surfactant substitution in pediatrics [2].
As one major function SP-A displays a protective role of the molecule in pulmonary host defense by interacting with various infectious agents such as bacteria, fungi and viruses. SP-A deficient knock-out mice - compared to wild type animals - are susceptible to infections with Pseudomonas aeruginosa [13] and the clearance of group B streptococcus is slower [14]. In accordance the defense of SP-A deficient mice against Respiratory Syncytial Virus (RSV) has been shown to be reduced and may be restored by exogenous SP-A administration [15-17].
By mediating the attachment of Mycobacterium tuberculosis to alveolar macrophages and promoting the phagocytosis of these bacteria, SP-A is important in the pathogenesis of tuberculosis [18-21]. SP-A also functionally interacts with staphylococci [22,23], Haemophilus influenza Type A [24,25], Pneumocystis carinii [26,27], Influenza A Virus (less efficient than SP-D) [28], Candida tropicalis [29] and Aspergillus fumigatus [30].
Moreover, SP-A is involved in the complex pulmonary network of cytokines as a central player, for example interacting with TNF-alpha and several interleukins [31,12,14][31,12,14].
Therefore it is likely that defects in the expression of SP-A may be important in the course of non infectious pulmo-
nary diseases of adult patients. In the case of idiopathic pulmonary fibrosis, for example, low levels of SP-A (measured by ELISA) have been reported in broncho alveolar lavages (BAL), but elevated levels were found in the sera [32-34]. Immunohistochemical examinations of the expression of SP-A in pulmonary fibrosis demonstrated evident defects by using specimens from different diseases displaying fibrotic changes in the lungs. In good agreement with the results in BAL reduced levels of SP-A have been observed in fibrotic lungs. This reduced SP-A-expression in fibrotic lungs may be caused by two reasons: a limited number of the SP-A producing type II pneumocytes and by a clearly reduced SP-A expression of the remaining cells [35].
Reduced levels of SP-A have been demonstrated also in other pulmonary diseases such as the Adult Respiratory Distress Syndrome (ARDS) and in pneumonia [36].
Keeping in mind that surfactant substitutes are widely available due to their application in pediatrics, a growing number of therapeutic possibilities may result from these findings.
In sarcoidosis elevated levels of SP-A have been described [37] using BAL; the same applies for the sera from patients with alveolar proteinosis [38].
Since SP-A represents a central molecule in pulmonary immunoregulation as well as in host-defense it is obvious that defects in the surfactant system may have functional influence in the course of these pulmonary disorders.
Another point of research concerning SP-A is the diagnostic value of this molecule, the expression of which is restricted to the lungs. It has been reported that SP-A levels in BAL or serum from patients suffering from idiopathic pulmonary fibrosis correlate with the progression of the disease and can be used to predict survival [34,38]. In samples from airway secretions SP-A measurements are described to be useful also for the diagnostics of pulmonary edema where elevated levels have been found compared to healthy volunteers and ARDS patients [39]. By utilizing highly sensitive RT-PCR techniques the amplification of SP-A transcripts can be used for the detection of occult metastases in non small cell lung cancer patients [5,40]. Comparative studies of different malignomas with pulmonary localization have shown the diagnostic properties of immunohistochemically determined SP-A [6,41,42][6,41,42]. In carcinomas of occult origin localized in the lungs the diagnosis has a crucial influence on the therapy. A positive detection of SP-A represents a clear hint for a primary location in the lung [43]. Fig. 2 as an example shows the immunohistochemical detection of SP-A in a moderately differentiated adenocarcinoma of the lung
Figure 2
Immunohistochemical detection of SP-A using the monoclonal antibody PE-10 (LSAB, amonoethylcarbazole, 400×400 \times ).
using the primary monoclonal antibody PE-10 and LSAB (AEC-substrate, ×100\times 100 ). The positive staining in the tumor cells (reddish) in this certain case helped to manifest the diagnosis as a primary carcinoma of the lung.
However, the choice of a suitable SP-A antibody is highly important since approaches using polyclonals display cross reactions with other tumors [44]. This procedure has already become a part of pathological routine diagnosis, and - along with other markers such as the Thyroid-transcription-factor-1 (TTF-1) - the detection of SP-A (by PE10) is a useful part of the immunohistochemical panel in pulmonary pathology.
Immunohistochemical detection of SP-A even might be utilized for forensic purposes helping to distinguish between fatal drowning and postmortem immersion [45].
Conclusion
It is evident that SP-A is a molecule which already proves to be an interesting subject for medical research. However, the studies concerning the possible role of surfactantdefects in pulmonary diseases of adults have been performed mainly in different cell culture or animal models hardly analyzing adult human lung tissue. For these reasons SP-A is a promising target for histomorphological approaches using pathological specimens which exactly represent the scenarios of various diseases with all the different cell types involved which are difficult to simulate in models. With the modern tools of molecular pathology, the genetic activities of genes can be analyzed in situ, which provides evidence of the cellular activities in the context of a human native tissue. One example is shown
in Fig. 3: a lung section hybridized with a digoxigeninlabeled SP-A probe to analyze the transcriptional activity in situ; the reddish signals of the transcripts are visible in the cytoplasm of type II pneumocytes. When analyzing the expression of SP-A in histological sections in context with other molecules of the pulmonary cytokine network one can expect further clues for the scenarios taking place in the course of interstitial lung diseases.
Figure 3
In situ hybridization targeting using a 663 bp digoxigenated DNA-probe complementary to SP-A
mRNA. Detection was achieved by Anti-digoxigenin antibody conjugated to alkaline phosphatase with NBT/BCIP as a chromogen (400×).
Taken together, SP-A is a complexly regulated molecule with surprising properties and essential importance for pulmonary development, structure and function which is getting more and more into focus concerning various diseases of the adult lung. Thus, as an outlook, it will become an issue of pulmonary pathology which might provide promising perspectives for applications in research, diagnosis and therapy.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
TG, DK and EV conceived the study. HS, MA, DSL and FS took part in the conception and writing of the manuscript. All authors read and approved the final manuscript.
Acknowledgements
The authors thank J. Tiebach and M. Lammers for excellent technical assistance.
References
I. Gibson AT: Surfactant and the neonatal lung. Br J Hosp Med 1997, 58:381-384.
2. Katswinkel J: 2Surfactant. Evolving issues. Clin Pedinatol 1998, 25(1):17-32.
3. Floros J, Karinch AM: Human SP-A: then and now. Am J Physiol 1995, 268:L162-L165.
4. Hoppe HJ, Reid KBM: Collectins - soluble proteins containing collagenous regions and lectin domains - and their roles in innate immunity. Prot Sci 1994, 3:I143-I158.
5. Betz C, Papadopoulos Th, Buchwald J, Dämmrich J, Müller-Hermelink HK: Surfactant protein gene expresssion in metastatic and micrometastatic pulmonary adenocarcinomas and other non-small cell lung carcinomas: detection by reverse transcriptase-polymerase chain reaction. Cancer Res 1995, 55:4283-4286.
6. Dempo K, Satoh M, Tsuji S, Mori M, Kuroki Y, Akino T: Immunohistochemical studies on the expression of pulmonary surfactant apoproteins in human lung carcinomas using monoclonal antibodies. Pathol Res Pract 1987, 182:669-675.
7. White RT, Damm D, Miller J, Spratt K, Schilling J, Hawgood S, Benson B, Cordell B: Isolation and characterization of the human pulmonary surfactant apoprotein gene. Nature 1985, 317:361-363.
8. Korfhagen TR, Glasser SW, Bruno MD, McMahan MJ, Whitsett JA: A portion of the human surfactant protein A (SP-A) gene locus consists of a pseudogene. Am J Respir Cell Mol Biol 1991, 4:463-469.
9. Hickling TP, Malhorta R, Sim RB: Human lung surfactant protein A exsits in several different oligomeric states: oligomer size distribution varies between patient groups. Molecular Medicine 1998, 4:266-275.
10. McCormick SM, Mendelson CR: Human SP-AI and SP-A2 genes are differentially regulated during development and by cAMP and glucocorticoids. Am J Physiol 1994, 266:L367-L374. (Lung Cell Mol Physiol 10)
II. McCormick SM, Boggaram V, Mendelson CR: Characterization of mRNA transcripts and organization of human SP-AI and SP-A2 genes. Am J Physiol 1994, 266:L354-366. (Lung Cell Mol Physiol 10)
12. Korfhagen TR, Glasser SW, Stripp BR: Regulation of gene expression in the lung. Curr Opin Pediatr 1994, 6:255-261.
13. LeVine AM, Kurak KE, Bruno MD, Stark JM, Whitsett JA, Korfhagen TR: Surfactant protein-A-deficient mice are susceptible to Pseudomonas aeruginosa infection. Am J Respir Cell Mol Biol 1998, 19:700-708.
14. LeVine AM, Kurak KE, Wright JR, Watford WT, Bruno MD, Ross GF, Whitsett JA, Korfhagen TR: Surfactant protein-A binds group B streptococcus enhancing phagocytosis and clearance from lungs of surfactant protein-A-deficient mice. Am J Respir Cell Mol Biol 1999, 20:279-286.
15. Kerr MH, Paton JY: Surfactant protein levels in severe respiratory syncytial virus infection. Am J Respir Crit Care Med 1999, 159:I115-I118.
16. LeVine AM, Gwozdz J, Stark J, Bruno M, Whitsett J, Korfhagen T: Surfactant protein-A enhances respiratory syncytial virus clearance in vivo. J Clin Invest 1999, 103:I015-I021.
17. Van Schaik SM, Vargas I, Welliver RC, Enhorning G: Surfactant dysfunction develops BAB/c mice infected with respiratory syncytial virus. Pediatr Res 1997, 42:I69-I73.
18. Downing JF, Pasula R, Wright JR, Twigg HL 3rd, Martin WJ 2nd: Surfactant protein a promotes attachment of Mycobacterium tuberculosis to alveolar macrophages during infection with human immunodeficiency virus. Proc Natl Acad Sci USA 1995, 92:4848-4852.
19. Gaynor CD, McCormack FX, Voelker DR, McGowan SE, Schlesinger LS: Pulmonary surfactant protein A mediates enhanced phagocytosis of Mycobacterium tuberculosis by a direct interaction with human macrophages. J Immunol 1995, 155:5343-5351.
20. Martin WJ 2nd, Downing JF, Williams MD, Pasula R, Twigg HL 3rd, Wright JR: Role of surfactant protein A in the pathogenesis of tuberculosis in subjects with human immunodeficiency virus infection. Proc Assoc Am Physicians 1995, 107:340-345.
21. Pasula R, Downing JF, Wright JR, Kachel DL, Davis TE Jr, Martin WJ 2nd: Surfactant protein A (SP-A) mediates attachment of Mycobacterium tuberculosis to murine alveolar macrophages. Am J Respir Cell Mol Biol 1997, 17:209-217.
22. Manz-Keinke H, Plattner H, Schlepper-Schafer J: Lung surfactant protein A (SP-A) enhances serum-independent phagocytosis
of bacteria by alveolar macrophages. Eur J Cell Biol 1992, 57:95-100.
23. Van Iwaarden F, Welmers B, Verhoef J, Haagsman HP, van Golde LM: Pulmonary surfactant protein A enhances the host-defense mechanism of rat alveolar macrophages. Am J Respir Cell Mol Biol 1990, 2:91-98.
24. McNeely TB, Coonrod JD: Aggregation and opsonization of type A but not type B Hemophilus influenzae by surfactant protein A. Am J Respir Cell Mol Biol 1994, 11:114-122.
25. Tino MJ, Wright JR: Surfactant protein A stimulates phagocytosis of specific pulmonary pathogens by alveolar macrophages. Am J Physiol 1996, 270:L677-L688.
26. Koziel H, Phelps DS, Fishman JA, Armstrong MY, Richards FF, Rose RM: Surfactant protein-A reduces binding and phagocytosis of pneumocystis carinii by human alveolar macrophages in vitro. Am J Respir Cell Mol Biol 1998, 18:834-843.
27. Zimmerman PE, Voelker DR, McCormack FX, Paulsrud JR, Martin WJ 2nd: 120-kD surface glycoprotein of Pneumocystis carinii is a ligand for surfactant protein A. J Clin Invest 1992, 89:143-9.
28. Harshorn KL, White MR, Shepherd V, Reid K, Jensenius JC, Crouch EC: Mechanisms of anti-influenza activity of surfactant proteins A and D: comparison with serum collectins. Am J Physiol 1997, 273:L1156-1166.
29. Pison U, Max M, Neuendank A, Weissbach S, Pietschmann S: Host defence capacities of pulmonary surfactant: evidence for ‘non-surfactant’ functions of the surfactant system. Eur J Clin Invest 1994, 24:586-99.
30. Madan T, Eggleton P, Kishore U, Strong P, Aggrawal SS: Binding of pulmonary surfactant proteins A and D to Aspergillus fumigatus conidia enhances phagocytosis and killing by human neutrophils and alveolar macrophages. Infect Immun 1997, 65:3171-3179.
31. Arias-Diaz J, Vara E, Garcia C, Gomez M, Balibrea JL: Tumor necrosis factor-alpha inhibits synthesis of surfactant by isolated human type II pneumocytes. Eur J Surg 1993, 159:541-549.
32. Honda Y, Kuroki Y, Shijubo N, Fujishima T, Takahashi H, Hosoda K, Akino T, Abe S: Aberrant appearance of lung surfactant protein A in sera of patients with idiopathic pulmonary fibrosis and its clinical significance. Respiration 1995, 62(2):64-69.
33. Kuroki Y, Tsutahara S, Shijubo N, Takahashi H, Shiratori M, Hattori A, Honda Y, Abe S, Akino T: Elevated levels of lung surfactant protein A in sera from patients with idiopathic pulmonary fibrosis and pulmonary alveolar proteinosis. Am Rev Respir Dis 1993, 147:723-729.
34. McCormack FX, King TE Jr, Bucher BL, Nielsen L, Mason RJ: Surfactant protein A predicts survival in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 1995, 152(2):751-759.
35. Deutschbein ME, Goldmann T, Galle J, Vollmer E: Patterns of Surfactant Aporotein-A (SP-A) Expression in Pulmonary Fibrosis. E J Pathol 1999, 5:99-101.
36. Gunther A, Siebert C, Schmidt R, Ziegler S, Grimminger F, Yabut M, Temmesfeld B, Walmrath D, Morr H, Seeger W: Surfactant alterations in severe pneumonia, acute respiratory distress syndrome, and cardiogenic lung edema. Am J Respir Crit Care Med 1996, 153:176-184.
37. Hamm H, Luhrs J, Guzman y Rotaeche J, Costabel U, Fabel H, Bartsch W: Elevated surfactant protein A in bronchoalveolar lavage fluids from sarcoidosis and hypersensitivity pneumonitis patients. Chest 1994, 106(6):1766-1770.
38. Kinder BW, Brown KK, McCormack FX, le JH, Kervitsky A, Schwarz MI, King TE: Serum Surfactant Protein-A Is a Strong Predictor of Early Mortality in Idiopathic Pulmonary Fibrosis. Chest 2009 in press.
39. Shimura S, Masuda T, Takishima T, Shirato K: Surfactant ProteinA concentration in airway secretions for the detection of pulmonary oedema. Eur Respir J 1996, 9:2525-2530.
40. Papadopoulos T: Detection of surfactant protein gene expression by reverse transcriptase-polymerase chain reaction (RT-PCR) identifies metastases and occult tumor spread of pulmonary adenocarcinomas. Verh Dtsch Ges Pathol 1996, 80:LVII-LXI.
41. Sugiyama K, Kawai T, Nakanishi K, Suzuki M: Histochemical reactivities of lectins and surfactant apoprotein in pulmonary adenocarcinomas and their metastases. Mod Pathol 1992, 5:273-276.
42. Nicholson AG, McCormick CJ, Shimosato Y, Butcher DN, Sheppard MN: The value of PE-10, a monoclonal antibody against pulmonary surfactant, in distinguishing primary and metastatic lung tumors. Histopathol 1995, 25:57-60.
43. Goldmann T, Vollmer E: Immunohistochemical detection of SPA is of diagnostik support in a patient suffering froma metastatic adenocarcinoma of the lungs. EJ Pathol 1999, 5:993-998.
44. Bejarano PA, Baughman RP, Biddinger PW, Miller MA, Fenoglio-Preiser C, Al-Kafaji B, Di Lauro R, Whitsett JA: Surfactant Proteins and Thyroid Transcription Factor-I in Pulmonary and Breast Carcinomas. Mod Pathol 1996, 9:445-452.
45. Stemberga V, Stifter S, Cuculiæ D, Coklo M, Bosnar A: Immunohistochemical surfactant protein-A expression: Fatal drowning vs. postmortem immersion. Med Hypotheses 2009, 72:413-415. Epub 2009
Publish with Bio Med Central and every
sientist can read your work free of charge
“BioMed Central will be the most significant development for disseminating the results of biomedical research in our lifetime.”
Sir Paul Nurse, Cancer Research UK
Your research papers will be:
- available free of charge to the entire biomedical community
- peer reviewed and published immediately upon acceptance
- cited in PubMed and archived on PubMed Central
- yours - you keep the copyright
Submit your manuscript here:
http://www.biomedcentral.com/info/publishing\_adv.asp
BioMedcentral