5 Ways State Governments Can Support Student Mental Health (original) (raw)
Media Contact
Government Affairs
In this article

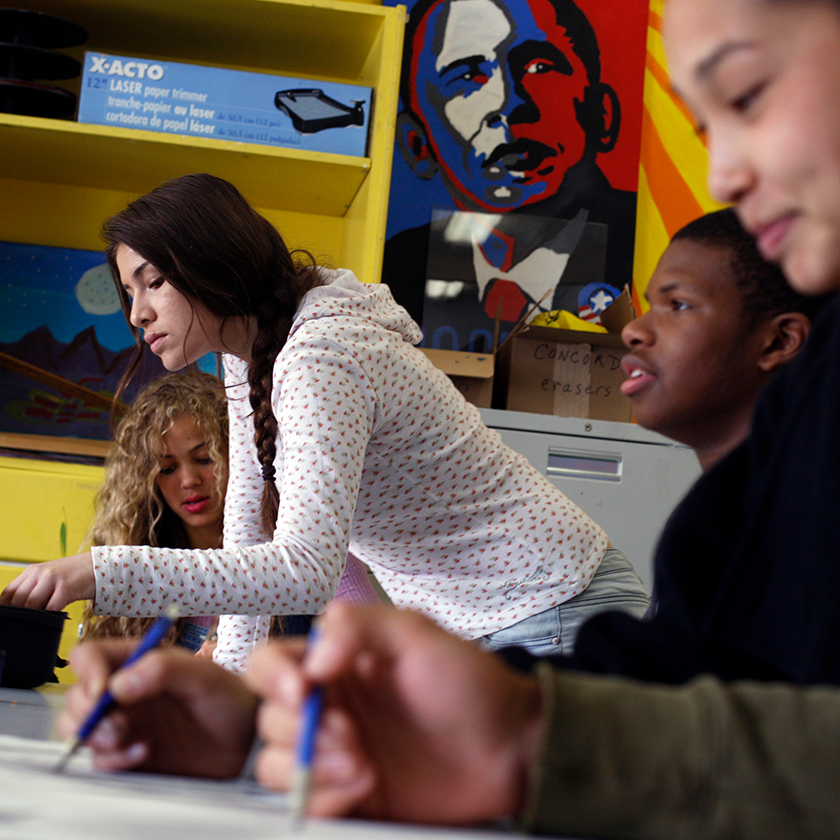
High school students in Chicago head down the stairs between classes, June 2023. (Getty/Antonio Perez/Chicago Tribune/Tribune News Service)
Across the country, students, parents, and teachers face the realities of a student mental health crisis. Many look to schools for solutions, yet on their own, schools often do not have the resources necessary to provide comprehensive mental health services. This issue brief outlines how state governments can support schools in best serving their students and addressing the student mental health crisis.
The student mental health crisis
Even prior to the COVID-19 pandemic, student mental health was an increasingly alarming issue. Rates of childhood mental health concerns and suicide rose steadily over the past decade, and by 2018, suicide became the second leading cause of death for youth ages 10–24.1 From 2016 to 2019, anxiety diagnoses among children ages 3–17 rose by 27 percent, and depression diagnoses among the same age group rose by 24 percent.2 The pandemic only intensified this crisis, as students faced isolation, uncertainty, and loss. Mental health-related visits to the emergency department increased by 24 percent for children ages 5–11 and 31 percent for children ages 12–17.3 In the face of this reality, educators are noting an unprecedented number of students with trauma,4 and parents across the nation are listing mental health concerns as their top worry for their children.5
State of school supports
K-12 public schools, given their daily interaction with children, can provide an optimal environment to screen for and provide mental health services. In fact, children are nearly just as likely to receive mental health services in an education setting as they are from a specialty mental health provider.6 However, in the 2019-20 school year, only 55 percent of public schools provided students with diagnostic mental health assessments, and only 42 percent offered mental health treatment.7
Even as student mental health needs have risen over the course of the COVID-19 pandemic,8 a majority of public schools reported that they “did not strongly believe” they are able to provide mental health services in an effective manner to students in need.9 When asked why, most schools shared that their limitations relate to the shortage of mental health providers in schools.10 In the first full year of the pandemic, almost 40 percent of school districts were without any school psychologists, and only 8 percent of districts met the National Association of School Psychologists’ (NASP) recommended ratio of 1 school psychologist to 500 students.11 Nationwide, current data estimate a ratio of 1 school psychologist to 1,211 students, a far cry from NASP’s recommendation.12 While some districts have turned to COVID-19 relief funds for support, relying on temporary funding to hire permanent staff is not financially sustainable, particularly for lower-income districts whose students are more often in need of mental health services.13
In the first full year of the pandemic, almost 40 percent of school districts were without any school psychologists, and only 8 percent of districts met the … NASP recommended ratio of 1 school psychologist to 500 students.
State recommendations
To effectively address the student mental health crisis, states must act swiftly and should consider these five options to best support schools, students, and their families.
1. Establish a statewide student mental health task force
As schools struggle to develop comprehensive student mental health systems, some states are turning to task forces to evaluate and recommend policies that promote student mental health. Task forces have the unique capability of pooling experts from various fields to examine issues and discuss solutions. They give states the opportunity to properly analyze the current state of student mental health through targeted data collection and provide expert evidence-based recommendations.
Take, for example, North Carolina’s School Health Advisory Council.14 Implemented in 2017, the advisory group comprises both health and education experts, who provide advice to the school system on aspects of the school health programs, including mental health services. In 2020, based on the recommendations from the advisory council, North Carolina enacted a law that requires the state Board of Education to adopt a school-based mental health policy and to require K-12 schools to adopt and implement a school-based mental health plan that includes a mental health training program and a suicide risk referral protocol. These kinds of clearly defined policies can support comprehensive systems that more consistently address students’ mental health needs.
2. Organize state-level interagency coordination
The student mental health crisis stretches across multiple areas of expertise and therefore demands cross-agency collaboration. State governments need to establish systems that ensure collaboration between their state department of health and human services and their state department of education in order to be most effective.
The Maryland School-Based Health Center Program was developed in coordination between the state Department of Health and state Department of Education.15 With 95 centers across the state, this program provides health services to students, families, and communities in clinics on school campuses—including primary care, sick visits, and mental health services. The centers not only enhance health outcomes but are also shown to have a measurable impact on school performance, grade promotion, and high school completion.16 This type of cross-agency collaboration maximizes the efficiency of programs and can assist states in reaching a larger population.
3. Expand access to Medicaid-covered school-based mental health services
Nearly 4 in 10 children nationwide are covered by Medicaid, the government program providing health insurance for low-income people and those with disabilities.17 While states administer Medicaid, it is funded jointly with the federal government, which provides matching dollars for qualified services.
In December 2014, the Centers for Medicare and Medicaid Services (CMS) clarified Medicaid reimbursement in school-based settings, opening the door to more funding.18 Previously, states could only obtain federal reimbursement for services provided to Medicaid-enrolled students who had an individualized educational plan (IEP), but the policy clarification allows reimbursements for eligible services delivered to all Medicaid-enrolled students, including those without an IEP. While this federal rule change allows billing for more school-based services under Medicaid, states must update their Medicaid plans and state-level policies to enable schools to take advantage of this resource. Since 2014, fewer than half of states have extended their Medicaid programs to cover more school-based services.19 Most notably, Colorado passed Senate Bill 174 this year, which requires Medicaid to cover mental health services for Medicaid-enrolled youth up to age 21, regardless of a formal mental health diagnosis.20 These services include access to family, group, and individual therapy, as well as prevention and evaluation services and case management. Allowing these services to be billed to Medicaid prior to a formal diagnosis will enable children to access early help and eliminates unnecessary barriers to seeking mental health services.
To assist states and schools in this process, the Bipartisan Safer Communities Act (BSCA) required the CMS to update a technical assistance guide for schools and provided $50 million in grants for states to implement or expand school-based Medicaid programs.21 In May 2023, the CMS issued new guidance on Medicaid services in school-based settings to assist states and districts in increasing access to school-based services by decreasing administrative burden.22 The guide offers flexibility to reduce administrative burden, making it easier for schools to bill Medicaid and receive payment for delivering Medicaid-covered services. This ease in process can encourage schools to participate in school-based health services and provide access to more students. The BSCA also created a technical assistance center launched by the CMS and the U.S. Department of Education to help states and schools find ways to pay for services.23 While pandemic relief funds have helped cover the costs of mental health services, these one-time funds are not sustainable. By expanding Medicaid services, states can generate a more sustainable stream of funding that will strengthen comprehensive mental health programs in the long term.
4. Increase access to school-based mental health providers
For most students in the United States, school-based mental health providers are not easily accessible, with only 8 percent of districts nationwide meeting NASP’s recommended ratio of 1 school psychologist to 500 students.24 At a time when children need more help than ever, it is essential that states work to close this gap and increase access to school-based mental health providers. School-based providers allow students to access health care where they are and eliminate barriers families may face in finding appropriate care. With children spending most of their waking hours in schools, bringing care directly to them and hiring staff trained to assess students and catch early signs of struggle can greatly reduce mental health concerns.
States should allocate additional funding for districts to hire more providers and move closer to NASP’s recommended ratio. States have taken various routes to do so, including encouraging districts to partner with local mental health providers. Washington, D.C., has increased funding over time for schools to develop partnerships with community-based mental health services,25 expanding services to 119 public and public charter schools.26 With this funding, the district aims to make behavioral health services available to all public and public charter school students. In addition to state funds, there are multiple opportunities for states to receive federal funding for these initiatives.
For example, the federal Mental Health Service Professional Demonstration Grant Program aims to increase the number and diversity of high-quality, trained providers by supporting and demonstrating innovative partnerships to prepare school-based mental health services providers.27 Through this grant, Minnesota established Project LIME, which leverages an innovative partnership between the University of Minnesota School Psychology program and one of Minnesota’s largest high-need school districts.28 This partnership uses a workforce development model to place graduate assistants in high-need schools to provide mental health services.
Likewise, the federal School-Based Mental Health Services Grant Program provides competitive grants to state and local education agencies to “increase the number of credentialed mental health services providers providing school-based mental health services to students in LEAs [local education agencies] with demonstrated need.”29 The New Jersey Department of Education was granted $2.7 million through the program to increase the number and diversity of credentialed school-based mental health services providers.30 The department intends to award 10 to 25 subgrants to local education agencies with demonstrated need and provide additional training opportunities for local education agency leadership and mental health providers. With this training and technical assistance, New Jersey aims to increase local education agencies’ capacity to build comprehensive systems of mental health supports, create a sustainable pipeline of school-based mental health providers, and establish communities of practice.
5. Invest in programs that improve school culture
A positive school culture leads to better student outcomes and promotes student mental health. While many actions that cultivate a positive school culture happen at the local level, states can encourage local education agencies to take specific steps through funding and state-sponsored opportunities. These may include training school staff in trauma-informed practices, building mental health into curricula, and administering school climate surveys to detect school policies and practices that threaten student mental well-being.
These investments can be as simple as steps Ohio has recently taken: The state Department of Education guided local education agencies on ways to spend COVID-19 relief funds to support a positive school climate.31 This includes access to needs assessments, a template for a planning process to address concerns, and various strategies for funding. Investments can also involve more in-depth programming, such as Pennsylvania’s Senate Bill 144, which mandates training administrators, staff, and school board directors to identify the signs and symptoms of trauma.32 These policies lead to higher identification rates of mental health needs in students, the first step in providing support.
In addition to state funding, states can also access federal funding to support these programs. The U.S. Department of Education’s School Climate Transformation Grant – Local Educational Agency Program provides funding to develop and adopt multitiered support systems33 such as positive behavioral interventions and supports, a schoolwide systems approach rethinking behavior and discipline.34 The Substance Abuse and Mental Health Services Administration (SAMHSA) offers grants to raise awareness about youth mental health issues and train school personnel and programs that coordinate treatment for young people with mental health disorders. SAMHSA’s Project Advancing Wellness and Resiliency in Education (AWARE) provides funding to raise awareness about mental health issues among school-age children and to train school personnel to detect mental health issues and connect students who need help to services.35 Through Project AWARE, nearly 800 policy changes have occurred at the state and local levels to improve mental health-related programs and services; more than 800,000 mental health professionals, first responders, teachers, school staff, families, and community members have participated in mental health-related trainings; and more than 200,000 students have been referred for mental health or related services.36 Through these types of funding, as well as state-generated funding, state governments can encourage local education agencies to implement comprehensive practices that better promote a positive school culture and reduce mental health concerns.
Conclusion
At a time when students need more support than ever, state governments must invest in programs that will support schools, students, and families. With statewide task forces, cross-agency collaboration, expansion of Medicaid services to include school-based services, increased investment in school-based mental health providers, and promotion of programs that improve school culture, states can begin to make positive changes that resolve this crisis. These investments can create lasting impacts that not only address student mental health, but also reduce violence in schools, increase student academic achievement, and create better working environments for school staff.
Acknowledgments
The author would like to thank the Health Policy team and Emma Lofgren from the Government Affairs team at the Center for American Progress for their valuable contributions to this brief.
The positions of American Progress, and our policy experts, are independent, and the findings and conclusions presented are those of American Progress alone. A full list of supporters is available here. American Progress would like to acknowledge the many generous supporters who make our work possible.
K-12 Education Policy
The K-12 Education Policy team is committed to developing policies for a new education agenda rooted in principles of opportunity for all and equity in access.