Early psychological interventions to treat acute traumatic stress symptoms (original) (raw)
Abstract
Background
The amelioration of psychological distress following traumatic events is a major concern. Systematic reviews suggest that interventions targeted at all of those exposed to such events are not effective at preventing post traumatic stress disorder (PTSD). Recently other forms of intervention have been developed with the aim of treating acute traumatic stress problems.
Objectives
To perform a systematic review of randomised controlled trials of all psychological treatments and interventions commenced within three months of a traumatic event aimed at treating acute traumatic stress reactions. The review followed the guidelines of the Cochrane Collaboration.
Search methods
Systematic searches were performed of of CCDAN Registers up to August 2008. Editions of key journals were searched by hand over a period of two years; personal communication was undertaken with key experts in the field; online discussion fora were searched.
Selection criteria
Randomised controlled trials of any psychological intervention or treatment designed to reduce acute traumatic stress symptoms, with the exception of single session interventions.
Data collection and analysis
Data were entered and analysed for summary effects using Review Manager 5.0 software. Standardised mean differences were calculated for continuous variable outcome data. Relative risks were calculated for dichotomous outcome data. When statistical heterogeneity was present a random effects model was applied.
Main results
Fifteen studies (two with long term follow‐up studies) were identified examining a range of interventions.
In terms of main findings, twelve studies evaluated brief trauma focused cognitive behavioural interventions (TF‐CBT). TF‐CBT was more effective than a waiting list intervention (6 studies, 471 participants; SMD ‐0.64, 95% CI ‐1.06, ‐0.23) and supportive counselling (4 studies, 198 participants; SMD ‐0.67, 95% CI ‐1.12, ‐0.23). Effects against supportive counselling were still present at 6 month follow‐up (4 studies, 170 participants; SMD ‐0.64, 95% CI ‐1.02, ‐0.25). There was no evidence of the effectiveness of a structured writing intervention when compared against minimal intervention (2 studies, 149 participants; SMD ‐0.15, 95% CI ‐0.48, 0.17).
Authors' conclusions
There was evidence that individual TF‐CBT was effective for individuals with acute traumatic stress symptoms compared to both waiting list and supportive counselling interventions. The quality of trials included was variable and sample sizes were often small. There was considerable clinical heterogeneity in the included studies and unexplained statistical heterogeneity observed in some comparisons. This suggests the need for caution in interpreting the results of this review. Additional high quality trials with longer follow up periods are required to further test TF‐CBT and other forms of psychological intervention.
Keywords: Female; Humans; Male; Anxiety; Anxiety/therapy; Behavior Therapy; Behavior Therapy/methods; Cognitive Behavioral Therapy; Cognitive Behavioral Therapy/methods; Counseling; Counseling/methods; Depression; Depression/therapy; Randomized Controlled Trials as Topic; Stress Disorders, Post‐Traumatic; Stress Disorders, Post‐Traumatic/etiology; Stress Disorders, Post‐Traumatic/prevention & control; Stress Disorders, Post‐Traumatic/therapy; Stress Disorders, Traumatic, Acute; Stress Disorders, Traumatic, Acute/psychology; Stress Disorders, Traumatic, Acute/therapy; Writing
Plain language summary
Early psychological interventions to treat acute traumatic stress symptoms
Traumatic events can have a significant impact on individuals', families' and communities' abilities to cope. In the past, single session interventions such as psychological debriefing were widely used with the aim of preventing continuing psychological difficulties. However, previous reviews have found that single session individual interventions and interventions provided to all have not been effective at preventing PTSD. A range of other forms of intervention have been developed to try to reduce psychological distress for individuals exposed to trauma. This review evaluated the results of 15 studies that tested a diverse range of psychological interventions aimed at treating acute traumatic stress problems. There was evidence to support the use of trauma focused cognitive behavioural therapy with such individuals, although there were a number of potential biases in identified studies which means the results should be treated with some caution. Further research is required to evaluate longer terms effects of TF‐CBT, to explore potential benefits of other forms of intervention and to identify the most effective ways of providing psychological help in the early stages after a traumatic event.
Background
Description of the condition
There is now a large body of literature to show that traumatic experience can cause significant psychological difficulties for large numbers of people, through events such as natural disasters (e.g. McFarlane 1988; Goenjian 1993), man made disasters (e.g. Gleser 1981; Baum 1983; Green 1990), military combat (Kulka 1990), rape (Kilpatrick 1987; Crummier 1991), violent crime (e.g. Hough 1990; North 1994) and road traffic accidents (Ehlers 1998). Many individuals show great resilience in the face of such experiences and will manifest short‐lived or sub‐clinical stress reactions that diminish over time (Bonanno 2004) and most people recover without medical or psychological assistance (McNally 2003; North 2007 ). Nevertheless, a range of psychological difficulties may develop following trauma in some of those who have been exposed. These include depressive reactions, phobic reactions and other anxiety disorders, alcohol and other substance misuse and less frequently obsessive compulsive‐disorder, psychotic reactions and conversion symptoms (North 2007). Some individuals display symptoms consistent with Acute Stress Disorder (ASD) in the early phase after a traumatic event. Post‐traumatic stress disorder (PTSD) is one of the most common enduring mental health problems to occur and has probably received most attention in the research literature.
A diagnosis of ASD is limited to the four weeks immediately after a traumatic event, with disturbance lasting for at least two days. In the Diagnostic and Statistical Manual (DSM‐IV; APA 1994) ASD is defined in terms of four sets of symptoms. These are dissociative symptoms (e.g. a sense of numbing, derealisation, depersonalisation), persistent re‐experiencing of the traumatic event, marked avoidance of stimuli associated with the trauma which might cause distress, and symptoms of anxiety and heightened arousal. There is a large overlap between the diagnostic criteria for ASD and PTSD (Brewin 2003), with the key differences being the time period during which diagnosis can be made and the dissociative symptoms of ASD. Rates of ASD of 13% have been reported in motor vehicle accident survivors (Harvey 1998) and 19% in victims of violent crime (Brewin 1999). PTSD is defined by DSM‐IV (APA 1994) as a syndrome which is comprised of three clusters of symptoms: repeated re‐experiencing of the trauma; avoidance of reminders and symptoms of numbing; and symptoms of heightened arousal. For a diagnosis of acute PTSD to be made symptoms have to have been present for more than a month, with chronic PTSD being the presence of symptoms for three months or longer. Reported rates of acute PTSD have varied across different trauma populations from 23% in motor vehicle accident victims (Ehlers 1998) to 47% in rape victims (Rothbaum 1992). Epidemiological research suggests that a third of individuals who develop acute PTSD remain symptomatic for six years or longer (Kessler 1995). The impact on social, interpersonal and occupational functioning for those who develop chronic PTSD can be very significant across the life span (Litz 2004). Some attention has been given to the predictive relationship between ASD and subsequent PTSD, as ASD was first included in DSM‐IV because it was thought it would prove a good predictor of subsequent PTSD. In a review of 12 prospective studies (McNally 2003) it was observed that whilst ASD appears to predict subsequent PTSD fairly well, a large proportion of individuals with PTSD do not initially meet criteria for ASD.
Description of the intervention
Over the past 25 years or so clinicians have been increasingly involved in attempts to develop interventions that might mitigate against the effects of trauma and prevent the onset of chronic PTSD. For a number of years single session interventions such as Psychological Debriefing were a widely used and popular form of intervention. Debriefing came under increasing scrutiny in the 1990s and has been the subject of a Cochrane Review first published in 1998 and recently updated (Rose 2002). The lack of evidence for the efficacy of single session individual debriefing has led many experts in the field to caution against its use (e.g. NCCMH 2005). Increasingly the field has turned its attention to other models of intervention (Brewin 2003; Bisson 2003; Ehlers 2003a; Litz 2002; Litz 2004; Gray 2005). A common theme has been the suggestion that efforts should be focused on identifying those most at risk of developing ongoing problems in the aftermath of traumatic incidents and targeting resources and interventions mainly upon them (Brewin 2008). In addition to ASD, a range of other risk factors have been found to be predictive of PTSD. These include gender, intelligence, previous trauma history, previous psychiatric history, severity of trauma, perceived life threat, peri‐traumatic dissociation, impaired social support and post traumatic stressors (Brewin 2000; Ozer 2003).
Why it is important to do this review
A large number of RCTs have demonstrated the effectiveness of some psychological interventions in treating chronic PTSD (Foa 2008). Trauma focused cognitive behavioural therapy (see Bisson 2007, Bradley 2005) and eye movement desensitisation and reprocessing (EMDR) (NCCMH 2005) have the strongest evidence base. A number of studies have been conducted which have attempted to evaluate a range of multiple session early interventions with the aim of preventing PTSD. Interventions of this kind have recently been the subject of a parallel systematic review to this review (Roberts 2009), which found no evidence to support the use of psychological interventions provided to all individuals regardless of whether or not they were symptomatic when they were recruited to the study. However, Roberts 2009 deliberately excluded early intervention studies, focusing only on those individuals who were symptomatic. A number of forms of psychological intervention have been developed with various populations with acute traumatic stress reactions. These include several forms of Cognitive Behavioural Therapy (including TF‐CBT), hypnotherapy and supportive counselling.
A number of recent studies have been conducted to evaluate some of these forms of intervention. This review seeks to examine the effectiveness of psychological interventions aimed at preventing or reducing the symptoms of chronic PTSD in individuals who have developed acute traumatic stress symptoms. For this review the term "acute traumatic stress symptoms" refers to individuals with ASD or acute PTSD or sub‐threshold ASD or acute PTSD. As we have noted above there is a very large overlap between the symptoms of ASD and acute PTSD and, left untreated, a majority of people with ASD go on to meet diagnosis for PTSD (McNally 2003). From a clinical stand point, the 14 day to 3 month period is well recognised as an "intermediate phase" of early intervention response (Watson 2007). It is also clinically meaningful in that many clinicians would consider similar broadly similar intervention responses to the various traumatic stress reactions that they might meet at this time (NCCMH 2005). For these reasons we feel that it is sensible and appropriate to combine analysis of studies treating ASD, acute PTSD and sub‐threshold presentations of these conditions in one review. Studies of individuals with chronic PTSD have been excluded from the review.
Objectives
To assess the effects of psychological interventions for acute traumatic stress reactions in individuals who have been exposed to a traumatic event within the previous three months (acute traumatic stress reactions were considered to include presentation consistent with diagnosis of ASD or acute PTSD, sub‐diagnostic symptoms of ASD or acute PTSD or other indicators of significant acute distress) in comparison with control interventions (including usual care, waiting list interventions and no treatment) and other psychological treatments.
Methods
Criteria for considering studies for this review
Types of studies
Any randomised controlled trial was eligible. Sample size, language and publication status were not used to determine whether or not a study should be included. Cluster and cross‐over trials would have been included, although none were identified. Quasi‐randomised trials were not eligible for inclusion.
Types of participants
Any individual exposed to a traumatic event, beginning psychological intervention within three months of the incident. For the purposes of the review, an event was considered to be traumatic if it was likely to meet criterion A1 of DSM‐IV (APA 1994) for PTSD. Therefore, the majority of participants in included studies were considered to have experienced, witnessed, or been confronted with an event or events that involved actual or threatened death or serious injury, or a threat to the physical integrity of self or others. There was no restriction on the basis of severity of ASD or PTSD symptoms, type of traumatic event or co‐morbidity. The review considered studies involving adults only.
Types of interventions
This review considered any psychological intervention or treatment designed to treat or reduce symptoms of traumatic stress in individuals who were identified as being symptomatic at the time that they entered into a study. Single session interventions were excluded because they are the subject of a separate Cochrane review (Rose 2002).
For the purpose of the review a psychological intervention included any specified non‐pharmaceutical intervention aimed at reducing traumatic stress symptoms offered by one or more health professional or lay person, with contact between therapist and participant on at least two occasions. We decided a priori that eligible intervention categories would include forms of psychological therapy that were based on a specified theoretical model. Potential intervention categories were identified from previous PTSD based reviews (Bisson 2007; NCCMH 2005). These were:
1. Trauma focused cognitive behavioural therapy (TF‐CBT) ‐ Any psychological treatment that predominantly uses trauma focused cognitive, behavioural or cognitive‐behavioural techniques on an individual basis. This category includes exposure therapy. 2. TF‐CBT Group Therapy ‐ Any approach delivered in a group setting that predominantly uses trauma focused cognitive, behavioural or cognitive‐behavioural techniques. 3. Eye Movement Desensitisation and Reprocessing (EMDR) ‐ Any psychological treatment that predominantly uses EMDR on an individual basis. 4. Non‐trauma focused CBT therapy ‐ Any approach (such as stress management or relaxation) delivered in a group or on an individual basis that predominantly uses non‐trauma focused cognitive, behavioural or cognitive‐behavioural techniques. 5. Other psychological treatment ‐ Any psychological treatment, delivered on an individual basis, that predominantly uses non‐trauma focused techniques that would not be considered cognitive, behavioural or cognitive‐behavioural techniques. This category includes non‐directive counselling, psychodynamic therapy and hypnotherapy.
We also decided a priori that eligible interventions would include non‐pharmaceutical interventions that were not based or only partially based on a specified theoretical model but that nevertheless aim to reduce symptoms of traumatic stress, to include the following categories:
6. Education or information giving intervention ‐ Any group based or individual intervention which predominantly provides only education or information about possible future difficulties and/or offers advice about constructive means of coping. 7. Stepped care ‐ Any, individual based, a priori specified care plan which offers intervention in a stepped care manner based on the continuing needs of the included participants. 8. Interventions delivered on an individual basis aimed at enhancing positive coping skills and improving overall well being ‐ Any non‐pharmaceutical intervention which aims to improve well being such as an occupational therapy intervention, an exercise based intervention or a guided self help intervention.
The above list was not intended to provide an exhaustive list of the types of interventions that might potentially be included but was indicative of the types of intervention that we thought were most likely to have been subject to evaluation.
We decided a priori that the trials considered would include: 1. Psychological intervention vs wait list or usual care control. 2. Psychological intervention vs other psychological intervention.
We decided that each stage would be stratified by treatment type and that further analysis would include follow‐up data where these were available. Comparisons involving follow‐up data would only be made when outcome data were available for similar time points.
Types of outcome measures
Primary outcomes
We took the decision to make severity of clinician rated traumatic stress symptoms using a standardised measure (such as the Clinician Administered PTSD Scale (Blake 1995)) the primary outcome measure. Clinician rated measures are widely used as primary outcomes in evaluative studies in the traumatic stress field and are considered to provide the "gold standard" measure by many (e.g. Foa 1997).
Secondary outcomes
1. Severity of self‐reported traumatic stress symptoms using a standardised measure such as the Impact of Event Scale (Horowitz 1979), the Davidson Trauma Scale (Davidson 1997) or the Post‐traumatic Diagnostic Scale (Foa 1995) 2. Severity of self‐reported depressive symptoms using a standardised measure such as the Beck Depression Inventory (Beck 1961) 3. Severity of self‐reported anxiety symptoms using a standardised measure such as the Beck Anxiety Inventory (Beck 1988) or the Spielberger State‐Trait Anxiety Inventory (Spielberger 1970) 4. Drop‐out from treatment 5. Adverse effects 6. General functioning including quality of life measures such as the SF‐36 (Ware 1993) 7. Use of health related resources.
Search methods for identification of studies
See: Depression, Anxiety and Neurosis Group methods used in reviews. No language restrictions were applied.
Electronic searches
This review used a common search strategy with the Cochrane review of multiple session early interventions aimed at preventing PTSD (Roberts 2009).
The Cochrane Depression, Anxiety and Neurosis Group (CCDAN) Trials RegistersThe Cochrane Collaboration Depression Anxiety and Neurosis Group (CCDAN) maintain two clinical trials registers at their editorial base in Bristol, UK. A references register and a studies based register. The CCDANCTR‐References Register contains over 24,000 reports of trials in depression, anxiety and neurosis. Approximately 70% of these references have been coded and tagged to individual trials. These coded records are held in the CCDANCTR‐Studies Register.
References to trials for inclusion in the CCDAN registers are collated from routine (weekly), generic searches of MEDLINE, EMBASE and PsycINFO; quarterly searches of the Cochrane Central Register of Controlled Trials (CENTRAL); annual searches of PSYNDEX, LILACS, AMED and CINAHL and review specific searches of additional databases. Details of trials are also sourced from international trials registers, drug companies, the hand‐searching of key journals, conference proceedings and other (non‐Cochrane) systematic reviews and meta‐analyses. A list of CCDAN’s generic search strategies can be found in the ‘Specialized Register’ section of the Group’s module text.
The Cochrane Depression, Anxiety and Neurosis Group Trials Registers was searched using the following search strategies (date of search: August 2008).
CCDANCTR‐Studies Diagnosis = "stress disorder*" or PTSD and Intervention = therapy or intervention or counsel* or debriefing and Age‐group = adult or aged or "not stated" or unclear and notDuration of therapy = "1 session"
CCDANCTR‐References Keyword = "Stress Disorder*" or "Stress‐Disorder*" or Free‐text = PTSD and Free‐text = debrief* or *therap* or intervention* or counsel*
An internet search of known web sites and discussion for a was also made by the authors.
Searching other resources
Grey literature
Conference proceedings of the European Conference of Traumatic Stress 2007 and of the meeting of the International Society for Traumatic Stress Studies 2007 and 2008.
Hand searching
Journal of Traumatic Stress and the Journal of Consulting and Clinical Psychology January 2007 ‐ September 2008.
Reference lists
Reference lists of the National Institute for Clinical Excellence PTSD Guidelines (NCCMH 2005) and included studies identified in the search and of related review articles were searched.
Personal communication
The authors contacted key individuals in the field to identify ongoing or unpublished studies. These included: David Alexander, Chris Brewin, Richard Bryant, Carl Castro, David Clark, Mark Creamer, Enrique Echeburua, Anke Ehlers, Charles Engel, Edna Foa, Matthew Friedman, Berthold Gersons, Neil Greenberg, Terry Keane, Dean Kilpatrick, Brett Litz, Andreas Maercker, Sandy McFarlane, Meaghan O'Donnell, Miranda Olff, Lars‐Göran Öst, Roger Pitman, Sue Rose, Barbara Rothbaum, Joe Ruzek, Paula Schnurr, Arieh Shalev, Marit Sijbrandij, Ueli Schnyder, Zahava Solomon, Arnold van Emmerik, Patricia Watson, Simon Wessely, Doug Zatzick, and Lori Zoellner.
Other
Internet Search ‐ Of known web sites and discussion fora.
Data collection and analysis
Selection of studies
Abstracts of all potential trials were independently read by two review authors. If an abstract appeared to represent a relevant RCT, the full report was read by each review author independently to determine if the trial met the inclusion criteria. When agreement could not be reached about inclusion a third review author was consulted. The studies excluded on further reading are listed in the appendices and reasons given for their exclusion.
Data extraction and management
A data extraction sheet was designed to capture data that would then be entered into Review Manager (RevMan 2008) software. Information extracted included demographic details of participants, details of the traumatic event, the randomisation process, the interventions used, drop‐out rates and outcome data. Data were independently extracted by two review authors. When agreement could not be reached the issue was discussed with a third review author.
Assessment of risk of bias in included studies
Assessment of methodological quality
Two review authors was assessed on methodological and reporting items identified as especially relevant by the authors. A number of recent Cochrane reviews had used a 23 item scale developed by Moncrieff 2001 to assess study quality. However, the Moncrieff 2001 scale includes a number of items (e.g. blinding of participants) that are of limited relevance to a psychological intervention. A checklist with an additional 19 criteria was therefore developed for this review to focus on key methodological issues pertinent to psychological interventions research in the traumatic stress field. In developing this checklist consideration was initially given to recommendations (Foa 1997) for seven "gold standards" required in RCTs investigating interventions for PTSD. These standards relate to clearly defined target symptoms, use of reliable and valid outcome measures, use of blind and independent assessors, assessor reliability, manualised specific and replicable treatment, concealment of allocation and treatment adherence. Further criteria related to non‐confounded conditions, use of multi‐modal outcome measures, reported level of therapist training and use of a control or comparison group were drawn from Hertlein 2004. One criterion based on a clear definition of the population to receive intervention was based on recommendations made by Kenardy 1996, as used by Rose 2002. A further nine criteria addressing adequate follow‐up, report of side effects, report of exclusions and refusals, comparability, intent to treat analysis, presentation of results, power calculation, appropriate statistical analysis and justified conclusions were drawn from the Moncrieff 2001 scale. The tool used appears in Appendix 1
Cases of disagreement were initially discussed between the two rating review authors. In cases where disagreement persisted advice was sought from a third review author in order to make a final decision. In developing this scale it was not the study group's intention to report an overall quality assessment score, but rather to allow for reporting on and discussion of specific study quality and reporting issues. In future updates of the review, authors intend to use the Risk of Bias tool recommended in Chapter 8 of the Cochrane Handbook (Higgins 2008).
Measures of treatment effect
Continuous outcomes were analysed using weighted mean difference (WMD) when all trials had measured the outcome on the same scale. When some trials measured outcomes on different scales the standardised mean difference (SMD) was used. Relative risk (RR) was used as the main categorical outcome measure as this is more widely used than odds ratio (OR) in health related practice. All outcomes were presented using 95% confidence intervals.
Unit of analysis issues
It was planned that for trials which had a crossover design only results from the first randomisation period would be considered. If the trial was a three (or more) armed trial, consideration would be given to undertaking pair wise meta‐analysis with each arm, depending upon the nature of the intervention in each arm and the relevance to the review objectives. Management of cluster randomised trials was intended to follow guidance provided in the Cochrane Handbook.
We decided that we would pool the data of active intervention outcomes in cases where a study, with three or more treatment arms, had compared an intervention with that same intervention plus an augmentation intervention and these two arms had also been compared against a control intervention. For example, we would pool the two TF‐CBT arms in a study comparing TF‐CBT vs TF‐CBT plus anxiety management vs a waiting list intervention.
Dealing with missing data
When Intention to Treat data were available this was reported in the results. Attempts were made to access ITT data wherever possible. Completer only data were included when these were the only data source available. In cases where there was inadequate information within a particular paper to undertake analysis, attempts were made to compute missing data from other information available within the paper, using guidance provided in the Cochrane Handbook (Higgins 2008). For example, in a number of cases dichotomous ITT outcomes (PTSD diagnosis) were calculated by adding the number of treatment drop‐outs to the number of completers continuing to have the diagnosis. When imputation was not possible or when further clarification was required we attempted to contact the authors concerned with a request for additional information. In cases where no further useable data were available the study was not included in further analysis.
Some clinician administered and self report measures for PTSD provide sub‐scale scores which when added together provide a total score (for example the CAPS (Blake 1995) uses "frequency" and "intensity" sub‐scales). Some studies report total mean scores, other studies provide sub‐scale means and standard deviations. When such scores were provided separately a total score was derived by adding the two scores together. A combined standard deviation was estimated using the formula: SD(Z) = √[(SD(X))² + (SD(Y))² + 2rSD(X)SD(Y)]. The correlation r between frequency and intensity was estimated using data from Vick unpublished based on the assumption that this data would provide a reasonable approximation of the correlation between these sub‐scales in Bryant 2003b.
Assessment of heterogeneity
A visual inspection of the forest plots was initially used to explore for possible heterogeneity. Heterogeneity between studies was also examined by observing the I² and χ² measures (p < 0 .10). As suggested in the Cochrane Handbook (Higgins 2008), an I² of less than 30% was taken to indicate mild heterogeneity and a fixed‐effects model was used to synthesise the results. An I² of 30% to 60% was considered to indicate moderate heterogeneity. An I² of 50%‐90% was considered to indicate substantial heterogeneity. In cases where the I² measure was 30% or more a random‐effects model was used to summarise results. In cases where significant heterogeneity was found to be present we attempted to explain the variation.
Assessment of reporting biases
It was decided a priori that if sufficient studies were available, funnel plots would be prepared and examined for signs of asymmetry. Where asymmetry was identified, other possible reasons for this would be considered. To investigate within study reporting bias, outcomes listed in the methods section of an article were compared with the results that were reported.
Data synthesis
Data was pooled from more than one study using a fixed‐effect model, except where heterogeneity was considered to be present. In these cases a random effects model was used as described below.
Subgroup analysis and investigation of heterogeneity
It was decided a priori that the following possible causes of heterogeneity would be explored if there was sufficient information to permit this:
1. Diagnostic clarity (studies where participants met full diagnostic criterion for either ASD or acute PTSD vs studies where full diagnostic criteria was not necessarily met) 2. Number of treatment sessions taken (two to six versus seven or more) 3. Type of traumatic event (Combat related trauma versus rape and sexual assault versus other civilian trauma)
In practice there was insufficient data and numbers of appropriate studies to allow sub‐group analysis on the basis of type of traumatic event.
Sensitivity analysis
It was decided a priori that sensitivity analysis would explore possible causes of methodological heterogeneity. 1. Trials considered most susceptible to bias would be excluded based on the following quality assessment criteria: a) those with unclear allocation concealment b) high levels of post‐randomisation losses (more than 40%) or exclusions or c) unblinded outcome assessment or blinding of outcome assessment uncertain. 2. Use of intention‐to‐treat analysis versus completer outcomes would be undertaken depending on available data.
Results
Description of studies
Results of the search
Two hundred and fifty one titles and abstracts were identified as a result of the search process and 50 papers were reviewed in detail by two of the review authors independently to establish if they met the specified inclusion criteria.
Included studies
Fifteen studies were found to meet the inclusion criteria and another two papers (Bryant 2003b; Bryant 2006) reported long term follow‐up on three studies (Bryant 1998; Bryant 1999; Bryant 2005). All studies were reported in English. These studies are described in the included studies table.
Participants
Participants in most studies (Bisson 2004; Bryant 1998;Bryant 1999;Bryant 2003a;Bryant 2005;Bryant 2008;Bugg 2009; Ehlers 2003b; Öst unpublished; Sijbrandij 2007; van Emmerik 2008; Wagner 2007 and Zatzick 2004) had experienced civilian trauma such as road traffic accidents, non‐sexual assault, other forms of crime or occupational injury. Participants in Wagner 2007 and Zatzick 2004 began intervention as hospitalised inpatients. Participants in the study by Echeburua 1996 were all female victims of sexual assault or rape, as were the majority of the participants in Foa 2006. Participants in Bryant 2003a had also experienced a mild brain injury.
Sample size
The number of patients randomised to the trials ranged from 8 (Wagner 2007) to 152 (Bisson 2004). Five studies included sample sizes of over 100 (Bisson 2004 (152), Bugg 2009 (102), Sijbrandij 2007 (143), van Emmerik 2008 (125) and Zatzick 2004 (121)).
Cultural setting
Five studies were conducted by one research group in Australia (Bryant 1998;Bryant 1999;Bryant 2003a;Bryant 2005;Bryant 2008).Three studies (Foa 2006; Wagner 2007; Zatzick 2004) were conducted in the USA, three in the UK (Bisson 2004; Bugg 2009; Ehlers 2003b), two in the Netherlands (Sijbrandij 2007; van Emmerik 2008), one in Sweden (Öst unpublished) and one in Spain (Echeburua 1996).
Diagnostic status
Table 1 shows the diagnostic status of individuals from each of the included studies. Six studies evaluated interventions for individuals with Acute Stress Disorder (Bryant 1998;Bryant 1999;Bryant 2003a;Bryant 2005;Bryant 2008 and Bugg 2009). Bisson 2004 and Zatzick 2004 included participants experiencing clinically significant levels of symptoms of PTSD and/ or depression at initial evaluation. Foa 2006 and Sijbrandij 2007 included participants meeting diagnostic criteria for acute PTSD (excluding the one month cut off criterion). Sijbrandij 2007 included a number of participants who met full diagnostic criterion for acute PTSD and separate data were obtained for this sub‐group. Participants in Echeburua 1996; Öst unpublished and Wagner 2007 all met diagnostic criteria for acute PTSD. Of the 125 participants in van Emmerik 2008 four met the diagnostic criteria for ASD, 62 met diagnostic criteria for acute PTSD and 59 met diagnostic criteria for chronic PTSD prior to beginning treatment. Of the 85 participants in Ehlers 2003b 12 met the diagnostic criteria for acute PTSD and 73 met the diagnostic criteria for chronic PTSD. Data from Ehlers 2003b and van Emmerik 2008 included in this review excludes participants who met diagnostic criteria for chronic PTSD at the time intervention began. Data used was in the form of unpublished subgroup data provided by the lead authors.
1. Diagnostic status of participants included in the review.
| Study | Participants with ASD | Participants with acute PTSD | Participants with threshold and sub‐ threshold status for ASD or acute PTSD | Participants with chronic PTSD (not included in this review) | Total Participants in the study |
|---|---|---|---|---|---|
| Bisson 2004 | 152 | 152 | |||
| Bryant 1998 | 24 | 24 | |||
| Bryant 1999 | 52 | 4 | 56 | ||
| Bryant 2003a | 24 | 24 | |||
| Bryant 2005 | 87 | 87 | |||
| Bryant 2008 | 90 | 90 | |||
| Bugg 2009 | 102 | 102 | |||
| Echeburua 1996 | 20 | 20 | |||
| Ehlers 2003b | 12 | 73 | 85 | ||
| Foa 2006 | 90 | 90 | |||
| Sijbrandij 2007 | 95 | 48 | 143 | ||
| van Emmerik 2008 | 4 | 62 | 59 | 125 | |
| Wagner 2007 | 8 | 8 | |||
| Zatzick 2004 | 121 | 121 | |||
| Öst unpublished | 43 | 43 | |||
| Total | 383 | 240 | 415 | 132 | 1170 |
Intervention
Table 2 provides a summary of the interventions used. The majority of studies evaluated a trauma focused cognitive behavioural intervention (TF‐CBT) as the active treatment intervention. Bisson 2004; Bryant 2008; Ehlers 2003b; Foa 2006; Öst unpublished; Sijbrandij 2007 and van Emmerik 2008 compared TF‐CBT against a waiting list intervention. Ehlers 2003b also included a minimal self‐help intervention, Foa included a supportive counselling intervention and van Emmerik 2008 included a structured writing therapy intervention. Bryant 2008 also included an cognitive restructuring intervention that did not include exposure. Bryant 1998;Bryant 1999;Bryant 2003a and Bryant 2005 evaluated a five session exposure based cognitive behavioural intervention against a supportive counselling intervention. Bryant 1999 evaluated these two interventions against a further intervention that included TF‐CBT plus anxiety management. Bryant 2005evaluated these two interventions against a further intervention that included TF‐CBT plus hypnosis. Echeburua 1996 compared TF‐CBT to relaxation training. Bugg 2009 evaluated a three session writing and information intervention against an information only intervention. Wagner 2007 was a pilot study which compared behavioural activation against treatment as usual. Zatzick 2004 evaluated a stepped collaborative care model (including case management, psychopharmacological and psychotherapeutic treatments to target alcohol abuse and PTSD) against treatment as usual.
2. Summary of study intervention arms.
| Study | TF‐CBT | TF‐CBT plus augmentation | Other active intervention | Supportive counselling | Waiting list or treatment as usual control |
|---|---|---|---|---|---|
| Bisson 2004 | Yes | Yes | |||
| Bryant 1998 | Yes | Yes | |||
| Bryant 1999 | Yes | Yes TF‐CBT plus anx man | Yes | ||
| Bryant 2003a | Yes | Yes | |||
| Bryant 2005 | Yes | Yes TF‐CBT plus | Yes | ||
| Bryant 2008 | Yes | Cognitive intervention without exposure | Yes | ||
| Bugg 2009 | Structured writing intervention | Yes | |||
| Echeburua 1996 | Yes | Relaxation | |||
| Ehlers 2003b | Yes | Minimal self help | Yes | ||
| Foa 2006 | Yes | Yes | Yes | ||
| Sijbrandij 2007 | Yes | Yes | |||
| van Emmerik 2008 | Yes | Structured writing intervention | Yes | ||
| Wagner 2007 | Behavioural activation | Yes | |||
| Zatzick 2004 | Collaborative care | Yes | |||
| Öst unpublished | Yes | Yes |
The number of treatment sessions available in Ehlers 2003b and Öst unpublished were greater than those available in other studies with 12 plus three booster sessions and 16 sessions respectively.
Excluded studies
Studies were excluded if they did not satisfy the inclusion criteria. Single session interventions included in the Cochrane review: Psychological debriefing for preventing post traumatic stress disorder (Rose 2002) were excluded from this review. One study (Bordow 1979) reported in that review did include more complex psychological intervention. We decided to exclude this study from the current review as the study design was only partially randomised. Other studies evaluating single session interventions were also excluded (Resnick 2005; Rose 1999; Rothbaum submitted; Turpin 2005). Other studies that were reviewed by paper and excluded are described in the table of Excluded studies.
Risk of bias in included studies
See Table 3 and Table 4 for results of individual included studies on the quality assessment tool described above and appearing in Appendix 1.
3. Quality scores of included studies (A‐E).
| | Bisson 2004 | Bryant 1998 | Bryant 1999 | Bryant 2003 | Bryant 2005 | Bryant 2008 | Bugg 2009 | Echebarua 1996 | Ehlers 2003 | | | ----------------------------------------------------- | ----------- | ----------- | ----------- | ----------- | ----------- | --------- | -------------- | ----------- | - | | Clearly defined targets for inclusion | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | | Reliable and valid measures | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | | Criteria A1 & A2 | 0 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | | Assessor reliability | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 2 | | Manualised, replicable, specific treatment | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 1 | | Treatment Adherence | 1 | 1 | 1 | 2 | 2 | 1 | 0 | 0 | 0 | | None confounded conditions | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | | Use of multi‐modal measures | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | | Reported level of therapist training | 1 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 0 | | Use of control or comparison group | 0 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | | Clear definition of the population/ participant group | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | | Adequate follow‐up period | 2 | 2 | 2 | 1 | 1 | 1 | 1 | 2 | 2 | | Details on side effects | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | | Exclusion criteria | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | | Comparability and adjustment | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | | Presentation of results | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | | Power calculation | 2 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | | Appropriate statistical analysis | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | | Justified conclusions | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 1 | 2 | | Handbook Risk of Bias Ratings | | | | | | | | | | | Adequate randomisation? | A | B | B | A | A | A | A | B | A | | Allocation concealment? | A | B | B | B | A | A | A | B | A | | Were outcome assessors blind to treatment condition? | A | A | A | A | A | A | B | C | A | | Reporting of loss to follow‐up? | A | A | B | A | A | A | A | A | A |
4. Quality scores of included studies (F‐Z).
| | Foa 2006 | Öst unpublished | Van Emmerik 2008 | Sijbrandij 2007 | Wagner 2007 | Zatzick 2004 | | | ----------------------------------------------------- | --------------- | ---------------- | --------------- | ----------- | ------------ | - | | Clearly defined targets for inclusion | 2 | 2 | 2 | 2 | 2 | 2 | | Reliable and valid measures | 2 | 2 | 2 | 2 | 2 | 2 | | Criteria A1 & A2 | 2 | 2 | 2 | 2 | 2 | 0 | | Assessor reliability | 1 | 1 | 2 | 2 | 0 | 2 | | Manualised, replicable, specific treatment | 2 | 1 | 2 | 2 | 2 | 2 | | Treatment Adherence | 1 | 1 | 1 | 2 | 0 | 1 | | None confounded conditions | 2 | 2 | 1 | 2 | 0 | 1 | | Use of multi‐modal measures | 2 | 2 | 0 | 2 | 0 | 2 | | Reported level of therapist training | 2 | 2 | 2 | 1 | 0 | 2 | | Use of control or comparison group | 2 | 1 | 2 | 1 | 0 | 0 | | Clear definition of the population/ participant group | 2 | 2 | 2 | 2 | 2 | 2 | | Adequate follow‐up period | 2 | 2 | See review | 1 | 0 | 2 | | Details on side effects | 0 | 0 | 0 | 0 | 1 | 0 | | Exclusion criteria | 1 | 2 | 1 | 2 | 1 | 2 | | Comparability and adjustment | 2 | 2 | 1 | 2 | 0 | 1 | | Presentation of results | 2 | 2 | 2 | 2 | 2 | 1 | | Power calculation | 0 | 0 | 0 | 2 | 0 | 0 | | Appropriate statistical analysis | 2 | 2 | 2 | 2 | 1 | 2 | | Justified conclusions | 2 | 2 | 2 | 2 | 2 | 2 | | Handbook Risk of Bias Ratings | | | | | | | | Adequate randomisation? | B | B | A | A | B | A | | Allocation concealment? | B | B | B | B | B | B | | Were outcome assessors blind to treatment condition? | A | B | A | B | A | B | | Reporting of loss to follow‐up? | A | A | A | A | A | A |
Allocation
Sequence generationSome studies did not provide full details of the method of allocation and as a result some bias was believed to be possible from the descriptions in six studies. In nine studies the method of allocation was judged to be adequately described, with no bias possible (Bisson 2004; Bryant 2003a; Bryant 2005; Bryant 2008; Bugg 2009; Ehlers 2003b; Sijbrandij 2007; van Emmerik 2008; Zatzick 2004).
Allocation concealmentMany studies did not provide full details of the method of randomisation and therefore concealment was unclear or inadequate in nine studies. There was reporting of adequate concealment procedures in five studies (Bisson 2004; Bryant 2005; Bryant 2008; Bugg 2009 and Ehlers 2003b).
Blinding
A double blind methodology for studies of psychological treatment is impossible as it is clear to participants what treatment they are receiving. However, a well designed study should have ensured blinding of the assessor of outcome measures. This was clearly performed in ten studies (Bisson 2004; Bryant 1998; Bryant 1999; Bryant 2003a; Bryant 2005; Bryant 2008; Ehlers 2003b; Foa 2006; van Emmerik 2008; Zatzick 2004).
Incomplete outcome data
This was fully reported with reasons by group in 14 of the 15 studies; only in Bryant 1999 was the number of withdrawals not entirely clear.
Other potential sources of bias
The overall quality of the studies in relation to these factors was variable.
Clearly defined targets for inclusion: All of the studies included in the review were considered to have defined clear targets for inclusion.
Participants satisfy A1 and A2 criteria for DSM‐IV PTSD: All studies were included in the review on the basis that the majority of participants had been exposed to an event or events that involved actual or threatened death or serious injury, or a threat to the physical integrity of self or others. All participants in Bryant 1998; Bryant 1999; Bryant 2003a; Bryant 2005; Bryant 2008; Echeburua 1996; Ehlers 2003b; Foa 2006; Öst unpublished; Sijbrandij 2007; van Emmerik 2008 and Wagner 2007 satisfied the additional intervention that the their response involved intense fear, helplessness, or horror at the time of the traumatic event.
Use of reliable and valid measures for assessment purposes and use of multi‐modal measures: All of the studies included in the review were considered to have used at least one reliable and valid outcome measure to assess key outcome variables. Clinician administered and self report measures were used in Bisson 2004; Bryant 1998; Bryant 1999; Bryant 2003a; Bryant 2005; Bryant 2008; Echeburua 1996; Ehlers 2003b; Foa 2006; Öst unpublished; Sijbrandij 2007 and Zatzick 2004.
Assessor reliability: Few studies described whether training was offered to assessors and how performance, supervision or reliability checks of assessors were performed. Bryant 2005; Ehlers 2003b; Sijbrandij 2007 and Zatzick 2004 were the only studies that were considered to have explained this fully.
Manualised, replicable, specific treatment: Treatment was clearly described and considered to be replicable in Bisson 2004; Bryant 1998; Bryant 1999; Bryant 2003a; Bryant 2005; Bugg 2009; Foa 2006; Sijbrandij 2007; van Emmerik 2008; Wagner 2007 and Zatzick 2004.
Reported level of therapists' training and treatment adherence: Therapist qualification in the treatment and comparison group (where appropriate) was provided in Bryant 1998; Bryant 1999; Bryant 2003a; Bryant 2005; Bryant 2008; Echeburua 1996; Foa 2006; Öst unpublished; van Emmerik 2008; Zatzick 2004. Treatment fidelity was considered to have been independently checked and adequate in only a small number of studies (Bryant 2003a; Bryant 2005; Sijbrandij 2007. Other studies either did not report fidelity checks or relied on checks from a member of the research group (Bisson 2004; Bryant 1998; Bryant 1999; Bryant 2008; Foa 2006; Öst unpublished; van Emmerik 2008; Zatzick 2004).
Use of a control or comparison group: Minimum treatment or alternative treatment interventions were used by Bryant 1998; Bryant 1999; Bryant 2003a; Bryant 2005; Bryant 2008; Bugg 2009; Echeburua 1996; Ehlers 2003b; Foa 2006 and van Emmerik 2008. Waiting list controls were the only comparison used in Öst unpublished and van Emmerik 2008. Other studies used treatment as usual comparisons.
Clear description of the population/ participant group: Most studies made some description of participants. Participants were clearly described in Bisson 2004; Bryant 1999; Bryant 2008; Bugg 2009; Echeburua 1996; Ehlers 2003b; Foa 2006; Öst unpublished; Sijbrandij 2007; van Emmerik 2008; Wagner 2007 and Zatzick 2004.
Record of exclusion criteria and number of exclusions and refusals reported: Both exclusion criteria and number of exclusions and refusals were adequately reported in Bisson 2004; Bryant 1998; Bryant 1999; Bryant 2003a; Bryant 2005; Bryant 2008; Echeburua 1996; Ehlers 2003b; Öst unpublished; Sijbrandij 2007 and Zatzick 2004. Reasons for exclusion but not numbers excluded were reported in Bryant 1998; Foa 2006; van Emmerik 2008 and Wagner 2007 .
Non‐confounded conditions: Confounds were judged to be non‐existent (on the basis of information provided about each group) or adequately controlled for in Bisson 2004; Bryant 1998; Bryant 1999; Bryant 2003a; Bryant 2005; Bryant 2008; Bugg 2009; Echeburua 1996; Ehlers 2003b; Foa 2006; Öst unpublished; Sijbrandij 2007 and van Emmerik 2008.
Power calculation: Information about power calculation was reported for only three studies (Bisson 2004; Bugg 2009 and Sijbrandij 2007).
Adequate follow‐up period: Eight studies included follow‐up periods beyond six months (Bisson 2004; Bryant 1998; Bryant 1999; Bryant 2005; Echeburua 1996; Ehlers 2003b; Foa 2006 and Zatzick 2004. Long term follow‐up in van Emmerik 2008 was not conducted at a consistent time point. Öst unpublished report that they are undertaking twelve month follow‐up but this is not yet available.
Information on comparability and adjustment for differences in analysis: Sufficient information on comparability with appropriate adjustment was judged to be described in Bisson 2004; Bryant 1998; Bryant 1999; Bryant 2003a; Bryant 2005; Bryant 2008; Bugg 2009; Echeburua 1996; Ehlers 2003b; Öst unpublished and Sijbrandij 2007. Foa 2006 reported that the number of participants who had been exposed to non‐sexual (rather than sexual) assault was different in one of their intervention groups to that of the other two groups.
Details on side effects: Only Bryant 2008 gave information about whether or not any participants experienced side‐effects which might have been attributable to their intervention. One study (Wagner 2007) gave a narrative description of the process of therapy for each participant, which suggested that it was unlikely that any unwanted side‐effects were experienced.
Use of withdrawals in analysis: Four studies (Bryant 1998; Bryant 2003a; Echeburua 1996; Wagner 2007) fulfilled this criterion by virtue of the fact that no withdrawal or drop‐outs were experienced. Bryant 2005; Bryant 2008; Bugg 2009; Foa 2006; Sijbrandij 2007; van Emmerik 2008 and Zatzick 2004 included withdrawals in analysis by estimation of outcome. In most cases this was by the method of "last observation carried forward". Other studies provided data only for treatment completers.
Presentation of results: Most studies provided comprehensive presentation of results sufficient to allow re‐analysis of main outcomes. Zatzick 2004 provided graphic representation of key outcomes rather than tabular data. These graphs did not permit re‐analysis but the authors were able to provide outcome data for inclusion in this review.
Appropriate statistical analysis: Thirteen studies provided what was judged to be appropriate and comprehensive statistical analysis (Bisson 2004; Bryant 1998; Bryant 1999; Bryant 2005; Bryant 2008; Bugg 2009; Echeburua 1996; Ehlers 2003b; Foa 2006; Öst unpublished; Sijbrandij 2007; van Emmerik 2008 and Zatzick 2004).
Justified conclusions: Judgement was made on this item on the basis of accurate representation of results, acknowledgement of methodological limitations and possible sources of bias, and commentary on relevance of the study when compared against the existing literature. On this basis, Bisson 2004; Bryant 1998; Bryant 1999; Bryant 2005; Bryant 2008; Bugg 2009; Ehlers 2003b; Foa 2006; Öst unpublished; Sijbrandij 2007; van Emmerik 2008; Wagner 2007 and Zatzick 2004 were judged to have provided justified conclusions:
Effects of interventions
Results are reported for all available outcome measures specified in the methodology. Only one study (Bryant 2008) reported data on adverse effects. No studies reported data on use of health related resources.
For notation purposes "n" refers to the number of participants included in each piece of analysis, "k" refers to the number of studies contributing to the analysis. Analysis resulting from single studies only are reported in "Additional tables". Numbers in parentheses following each outcome heading indicate comparison tables.
COMPARISONS OF PSYCHOLOGICAL INTERVENTIONS WITH WAITINGLIST/ USUAL CARE INTERVENTIONS
Five types of intervention were compared against a waiting list or usual care condition. These were:
- TF‐CBT
- Supportive counselling
- Cognitive restructuring (without exposure)
- Behavioural activation
- Stepped collaborative care
Results for each intervention will be considered in turn.
Trauma focused CBT vs waiting listData was available from seven studies (Bisson 2004; Bryant 2008; Ehlers 2003b; Foa 2006; Öst unpublished; Sijbrandij 2007 and van Emmerik 2008) with a total of 515 participants. Long‐term follow‐up data were received for van Emmerik 2008. However this was not included in meta‐analysis because the follow‐up interval varied considerably across participants (91‐973 days).
Severity of PTSD (1.01‐ 1.07) Clinician administered (01.01‐ 01.07) There was strong evidence that the TF‐CBT intervention had an effect at initial outcome (random effects) (k=6, n=471; SMD ‐0.64, 95% CI ‐1.06, ‐0.23). A substantial level of statistical heterogeneity was indicated (I²=75%). To explore this we undertook separate sub‐group analysis to examine the effects of intervention on individuals who were identified as having met full criteria for diagnosis for ASD or acute PTSD. This analysis excluded data from Bisson 2004 and Foa 2006 and a sub‐set of individuals from Sijbrandij 2007 who did not meet full diagnostic criteria for either condition. The magnitude of the effect in favour of treatment increased (random effects)(k=4, n=208; SMD ‐0.96 95% CI ‐1.56, ‐0.36).
The length of the treatment intervention was another possible reasons for this heterogeneity. In two studies (Ehlers 2003b and Öst unpublished) the number of available treatment sessions was also greater than other studies (12 plus 3 and 16 sessions respectively). The number of treatment sessions available in the other studies was either 4 or 5. We therefore decided to conduct a sub‐group analysis excluding these two studies. The magnitude of the treatment effect was decreased and small (random effects) (k=4, n=416; SMD ‐0.40, 95% CI ‐0.75, ‐0.05) (random effects). A substantial level of statistical heterogeneity was still indicated (I²=66%). When Ehlers 2003b and Öst unpublished were subjected to analysis without the other studies the magnitude of the treatment effect increased (n=53; SMD ‐1.48, 95% CI ‐2.10, ‐0.85).
Long term follow‐up data were not collected at consistent time points across the studies identified. Three to five month follow‐up data were available from two studies (Foa 2006; Sijbrandij 2007). There was no strong evidence that the TF‐CBT intervention had an effect (fixed effects)(k=2, n=204; SMD ‐0.17, 95% CI ‐0.45, 0.11) (I² =0%). At 9‐11 months follow‐up data were available from two studies (Ehlers 2003band Foa 2006). There was no strong evidence that the TF‐CBT intervention had an effect (k=2, n=73; SMD ‐0.33, 95% CI ‐0.80, 0.15). A substantial level of statistical heterogeneity was indicated (I²=79%). Twelve to eighteen month follow‐up data were only available from Bisson 2004. There was no strong evidence that the TF‐CBT intervention had an effect (see Table 5 of the Additional Tables). Self report (1.05‐1.07) There was strong evidence that the TF‐CBT intervention had an effect at initial outcome (random effects) (k=6, n=370; SMD ‐0.83, 95% CI ‐1.43, ‐0.23). A substantial level of statistical heterogeneity was indicated in this analysis (I²=84%). As with clinician administered outcomes, separate sub‐group analysis was undertaken to examine the effects of intervention on individuals who were identified as having met full criteria for diagnosis for ASD or acute PTSD. This analysis excluded data from Bisson 2004 and Foa 2006 and a small number of participants from van Emmerik 2008 who met diagnosis for ASD. The magnitude of effect in favour of treatment increased (random effects)(k=4, n=158; SMD ‐1.16 95% CI ‐1.73, ‐0.58). A substantial level of statistical heterogeneity continued to be indicated (I²=57%).
5. Outcomes from single studies for trauma focused CBT vs waiting list.
| Study | Outcome | Participants | Statistical Method | Effect Estimate |
|---|---|---|---|---|
| Bisson 2004 | 12‐18 month follow‐up for clinician administered PTSD severity | 152 | Mean Difference (IV, Fixed, 95% CI) | ‐6.01, 95% CI ‐12.44, 0.42 |
| Foa 2006 | 3‐5 month follow‐up for self reported PTSD severity | 61 | Mean Difference (IV, Fixed, 95% CI) | ‐3.32, 95% CI ‐9.79, 3.15 |
| Bisson 2004 | 12‐18 month follow‐up for self report PTSD severity | 152 | Mean Difference (IV, Fixed, 95% CI) | ‐7.40, 95% CI ‐13.79, ‐1.01 |
| Bisson 2004 | 12‐18 month follow‐up for PTSD diagnosis | 115 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74, 95% CI 0.36, 1.51 |
| Bisson 2004 | 12‐18 month follow‐up for anxiety | 152 | Mean Difference (IV, Fixed, 95% CI) | ‐0.15, 95% CI ‐1.76, 1.46 |
| Bisson 2004 | 12‐18 month follow‐up for depression | 152 | Mean Difference (IV, Fixed, 95% CI) | ‐0.76, 95% CI ‐2.37, 0.85 |
| Öst unpublished | Quality of life ‐ initial outcomes | 41 | Mean Difference (IV, Fixed, 95% CI) | 1.65, 95% CI 0.91, 2.39 |
A post hoc sub‐group analysis excluding Ehlers 2003b and Öst unpublished was also conducted for the reasons outlined above. The magnitude of the effect in favour of treatment was decreased (random effects) (k=4, n=317; SMD ‐0.46, 95% CI ‐0.95, 0.03). A substantial level of statistical heterogeneity continued to be indicated (I²=76%).
Data from one study (Foa 2006) was available for follow‐up at 3‐5 months. There was no strong evidence that the TF‐CBT intervention had an effect (see Table 5 of the Additional Tables). At 9‐11 months follow‐up data were available from two studies (Ehlers 2003b and Foa 2006). There was no strong evidence that the TF‐CBT intervention had an effect (n=73; SMD ‐0.31, 95% CI ‐0.79, 0.17). A substantial level of statistical heterogeneity was indicated (I²=84%). Twelve to eighteen month follow‐up data were available from Bisson 2004. There was no strong evidence that the TF‐CBT intervention had an effect (see Table 5 of the Additional Tables).
**PTSD diagnosis (1.08‐1.11)**There was no strong evidence that the TF‐CBT intervention had an effect at initial follow‐up (random effects) (k=7, n=515; RR 0.72, 95% CI 0.50, 1.05). A substantial level of statistical heterogeneity was indicated (I²=71).
We undertook additional sub‐group analysis to examine the effects of intervention on individuals who were identified as having met full criteria for diagnosis for ASD or acute PTSD. This analysis excluded data from Bisson 2004 and Foa 2006 and some participants from Sijbrandij 2007 who did not meet full diagnostic criteria for either condition. The magnitude of the effect in favour of treatment increased (k=5, n=254; RR 0.54, 95% CI 0.31, 0.95). A substantial level of statistical heterogeneity was indicated (I²=67%).
There was strong evidence that the TF‐CBT intervention had an effect at 3‐5 month follow‐up (fixed effects) (k=2, n=141; RR 0.64, 95% CI 0.42, 0.99)(I²=0%). There was no strong evidence that the TF‐CBT intervention had an effect at 9‐11 months (fixed effects) (k=2, n=54; RR 0.61, 95% CI 0.27, 1.36). A substantial level of statistical heterogeneity was indicated (I²=70%). Neither study demonstrated a significant difference by itself. One study (Bisson 2004) provided completer data for follow‐up at 12‐18 months. There was no strong evidence that the TF‐CBT intervention had an effect (see Table 5 of the Additional Tables).
**Anxiety (1.12‐1.14)**All seven studies reported anxiety symptoms through self report at initial follow‐up. There was strong evidence that the TF‐CBT intervention had an effect at initial outcome (random effects) (k=7, n=513; SMD ‐0.53, 95% CI ‐0.91, ‐0.15). A substantial level of statistical heterogeneity was indicated (I²=73%).
Evidence for an effect was not strong at 3‐5 months follow‐up (fixed effects)(k=2, n=204; SMD ‐0.19, 95% CI ‐0.47, 0.08)(I²=0%). Evidence for an effect was not strong at 9‐11 months (fixed effects)(k=2, n=73; SMD ‐0.31, 95% CI ‐0.79, 0.16). A substantial level of statistical heterogeneity was indicated (I²=80%). There was a significant difference in favour of treatment for the subset from Ehlers 2003b but not for Foa 2006. One study (Bisson 2004) provided data for follow‐up at 12‐18 months. There was no strong evidence that the TF‐CBT intervention had an effect (see Table 5 of the Additional Tables).
**Depression (1.15‐ 1.17)**All seven studies reported depression symptoms through self report at initial follow‐up.There was strong evidence that the TF‐CBT intervention had an effect at initial outcome (random effects) (k=7, n=513; SMD ‐0.49, 95% CI ‐0.80, ‐0.18). A substantial level of statistical heterogeneity was indicated (I²=60%).
Evidence for an effect was not strong at 3‐5 months follow‐up (fixed effects)(k=2, n=204; SMD ‐0.12, 95% CI ‐0.39, 0.16) (I²=0%). Evidence for an effect was not strong at 9‐11 months (fixed effects)(k=2, n=73; SMD ‐0.21, 95% CI ‐0.67, 0.26). A moderate level of statistical heterogeneity was indicated (I²=57%). One study (Bisson 2004) provided data for follow‐up at 12‐18 months. There was no strong evidence that the TF‐CBT intervention had an effect (see Table 5 of the Additional Tables).
**Leaving the study early (1.18)**There was no evidence of an effect on drop‐out at initial follow‐up (k=7, n=515; RR 0.89, 95% CI 0.63, 1.26)(I² =0%).
Quality of lifeData was available from Öst unpublished. There was strong evidence that the TF‐CBT intervention had an effect on quality of life at initial outcome (n=41; WMD 1.65, 95% CI 0.91, 2.39).
Supportive counselling vs waiting listData was available from one study (Foa 2006) with 59 participants. Evidence for an effect was not strong at initial or at long‐term follow‐up on any of the outcome measures reported or in terms of leaving the study early. Weighted means and relative risk are reported by outcome in Table 6 of the Additional Tables.
6. Supportive counselling vs waiting list.
| Outcome | Studies | Participants | Statistical Method | Effect Estimate |
|---|---|---|---|---|
| Severity of PTSD (clinician administered) initial outcome | 1 | 59 | Mean Difference (IV, Fixed, 95% CI) | 1.17 [‐5.70, 8.04] |
| Severity of PTSD (self report) initial outcome | 1 | 59 | Mean Difference (IV, Fixed, 95% CI) | 3.36 [‐3.91, 10.63] |
| Severity of PTSD (clinician administered) 3‐5 month follow‐up | 1 | 59 | Mean Difference (IV, Fixed, 95% CI) | 0.79 [‐6.27, 7.85] |
| Severity of PTSD (self report) 3‐5 month follow‐up | 1 | 59 | Mean Difference (IV, Fixed, 95% CI) | ‐0.30 [‐7.00, 6.40] |
| Severity of PTSD (clinician administered) 9‐11 month follow‐up | 1 | 59 | Mean Difference (IV, Fixed, 95% CI) | ‐4.67 [‐11.93, 2.59] |
| Severity of PTSD (self report) 9‐11 month follow‐up | 1 | 59 | Mean Difference (IV, Fixed, 95% CI) | ‐1.98 [‐8.71, 4.75] |
| PTSD diagnosis after treatment: Initial outcome | 1 | 59 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.61, 1.39] |
| Anxiety: Initial outcome | 1 | 59 | Mean Difference (IV, Fixed, 95% CI) | 0.89 [‐5.88, 7.66] |
| Anxiety: 3‐5 months follow‐up | 1 | 59 | Mean Difference (IV, Fixed, 95% CI) | 0.99 [‐5.30, 7.28] |
| Anxiety: 9‐11 month follow‐up | 1 | 59 | Mean Difference (IV, Fixed, 95% CI) | ‐0.31 [‐7.10, 6.48] |
| Depression: Initial outcome | 1 | 59 | Mean Difference (IV, Fixed, 95% CI) | 0.51 [‐5.56, 6.58] |
| Depression: 3‐5 month follow‐up | 1 | 59 | Mean Difference (IV, Fixed, 95% CI) | ‐1.53 [‐6.94, 3.88] |
| Depression: 9‐11 month follow‐up | 1 | 59 | Mean Difference (IV, Fixed, 95% CI) | ‐1.47 [‐7.13, 4.19] |
| Leaving the study early due to any reason | 1 | 59 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.52 [0.20, 1.33] |
Cognitive restructuring (without exposure) vs waiting listData was available from one study (Bryant 2008) with 60 participants (see Table 7 of the Additional Tables). There was strong evidence that the cognitive restructuring had an effect on reducing the severity of PTSD on clinician administered assessment. Evidence for an effect was not strong for self reported PTSD, PTSD diagnosis, anxiety depression or in terms of drop‐out.
7. Cognitive restructuring (without exposure) vs waiting list.
| Outcome | Studies | Participants | Statistical Method | Effect Estimate |
|---|---|---|---|---|
| Severity of PTSD symptoms: Clinician administered: initial outcome: ITT | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐12.90 [‐25.78, ‐0.02] |
| Severity of PTSD symptoms: self report: initial outcome: ITT | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐9.90 [‐21.36, 1.56] |
| Severity of PTSD (clinician administered): initial outcome: completers | 1 | 44 | Mean Difference (IV, Fixed, 95% CI) | ‐14.30 [‐28.37, ‐0.23] |
| Severity of PTSD (self report): initial outcome: completers | 1 | 44 | Mean Difference (IV, Fixed, 95% CI) | ‐11.89 [‐25.93, 2.15] |
| PTSD diagnosis after treatment: initial outcome | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.59, 1.16] |
| Anxiety: Initial outcome | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 3.80 [‐3.26, 10.86] |
| Depression: Initial outcome | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐3.00 [‐9.86, 3.86] |
| Leaving the study early due to any reason | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.81, 1.49] |
Behavioural activation vs treatment as usual to treat acute PTSDData was available from one pilot study (Wagner 2007) with 8 participants. Evidence for an effect at follow‐up was not strong for self reported PTSD severity, depression or general functioning. There was no drop‐out from either intervention. Weighted means and relative risk are reported by outcome in Table 8 of the Additional Tables.
8. Behavioral activation vs treatment as usual.
| Outcome | Studies | Participants | Statistical Method | Effect Estimate |
|---|---|---|---|---|
| Severity of PTSD: initial outcomes (clinician administered) | 1 | 8 | Mean Difference (IV, Fixed, 95% CI) | ‐18.70 [‐43.41, 6.01] |
| Depression | 1 | 8 | Mean Difference (IV, Fixed, 95% CI) | ‐9.00 [‐31.74, 13.74] |
| Leaving the study early due to any reason | 1 | 8 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| General functioning | 1 | 8 | Mean Difference (IV, Fixed, 95% CI) | 12.61 [‐10.16, 35.38] |
Stepped collaborative care vs usual care for an inpatient service for symptomatic individualsData was available from one study (Zatzick 2004) with 121 participants. Evidence for an effect at initial follow‐up was not strong or at any subsequent time point in terms of PTSD diagnosis or in terms of leaving the study early. Weighted means and relative risk are reported by outcome in Table 9 of the Additional Tables.
9. Stepped Collaborative care vs usual care for an inpatient service.
| Outcome | Studies | Participants | Statistical Method | Effect Estimate |
|---|---|---|---|---|
| PTSD Diagnosis at one month | 1 | 106 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.42, 1.69] |
| PTSD Diagnosis at 3 months | 1 | 103 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.44, 1.85] |
| PTSD diagnosis at 6 months | 1 | 102 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.33, 1.23] |
| PTSD diagnosis at 12 months | 1 | 91 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.34, 1.60] |
| Leaving the study early due to any reason at one month | 1 | 121 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.52 [0.58, 4.02] |
| Leaving the study early due to any reason at 3 months | 1 | 121 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.34, 1.92] |
| Leaving the study early due to any reason at 6 months | 1 | 121 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.59 [0.25, 1.40] |
| Leaving the study early due to any reason at 12 months | 1 | 121 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.36, 1.28] |
COMPARISONS OF PSYCHOLOGICAL INTERVENTIONS WITH OTHER PSYCHOLOGICAL INTERVENTION
Seven comparisons were made of one psychological intervention against another psychological intervention. These were:
- Structured writing therapy vs minimal intervention
- TF‐CBT vs supportive counselling
- TF‐CBT vs structured writing therapy
- TF‐CBT vs cognitive restructuring (without exposure)
- TF‐CBT vs relaxation
- TF‐CBT vs TF‐CBT plus anxiety management
- TF‐CBT vs TF‐CBT plus hypnosis
Results for each intervention will be considered in turn.
Structured writing therapy vs minimal interventionData was available from two studies (Bugg 2009; van Emmerik 2008) with 149 participants in these two treatment interventions.
Severity of PTSD (2.01) Clinician administered
No clinician administered data were reported.
_Self report_Evidence for an effect was not strong at initial follow‐up (fixed effects) (k=2, n=149; SMD ‐0.15, 95% CI ‐0.48, 0.17) or 3 month follow‐up (see Table 10 of the Additional Tables). A substantial level of statistical heterogeneity was indicated in the initial follow‐up analysis (I²=89%). There were a number of differences in the methodologies of these two studies. Notably, some of the treatment sessions offered in Bugg 2009 were by telephone, whereas van Emmerik 2008 treatment sessions were face to face. There was evidence of a strong effect in favour of the active intervention in van Emmerik 2008.
10. Structured writing therapy vs minimal intervention.
| Outcome | Studies | Participants | Statistical Method | Effect Estimate |
|---|---|---|---|---|
| Severity of PTSD, self report, 3 month follow‐up | 1 | 104 | Mean Difference (IV, Fixed, 95% CI) | 1.10 95% CI ‐3.80, 6.00 |
| PTSD diagnosis at initial follow‐up | 1 | 45 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22, 95% CI 0.74, 2.02 |
| Anxiety, 3 month follow‐up | 1 | 104 | Mean Difference (IV, Fixed, 95% CI) | 0.47, 95% CI ‐1.25, 2.19 |
| Depression, 3 month follow‐up | 1 | 104 | Mean Difference (IV, Fixed, 95% CI) | 0.29, 95% CI ‐2.11, 1.53 |
PTSD diagnosisData was only available from van Emmerik 2008. Evidence for an effect at initial follow‐up was not strong (see Table 10 of the Additional Tables).
**Anxiety (2.02)**Evidence for an effect was not strong at initial follow‐up (fixed effects) (k=2, n=149; SMD ‐0.27, 95% CI ‐1.04, 0.50) or 3 month follow (see Table 10 of the Additional Tables) . A substantial level of statistical heterogeneity was indicated in the initial follow‐up analysis (I²=78%).
**Depression (2.03)**Evidence for an effect was not strong at initial follow‐up (fixed effects) (k=2, n=149; SMD ‐0.02 95% CI ‐0.34, 0.30) or 3 month follow (see Table 10 of the Additional Tables). No statistical heterogeneity was indicated in the initial follow‐up analysis (I²=0%).
**Leaving the study early (2.04)**There was no evidence of an effect on drop‐out at initial follow‐up (fixed effects) (k=2, n=149; RR 0.90, 95% CI 1.04, 1.66). No statistical heterogeneity was indicated (I²=0%).
Trauma focused CBT vs supportive counsellingFive studies (Bryant 1998; Bryant 1999; Bryant 2003a;Bryant 2005 and Foa 2006) contributed to analysis in this comparison with a total of 251 participants. Long‐term follow‐up data were provided for Bryant 1998; Bryant 1999 and Bryant 2005 in Bryant 2003b and Bryant 2006. These two papers provided clinician administered outcomes for PTSD severity for frequency and intensity separately. Bryant 2003b provided clinician administered outcomes for PTSD severity for frequency and intensity scores separately. This was addressed using the steps described in "dealing with missing data" above.
Severity of PTSD symptoms (3.01‐3.04) Clinician administered (3.01‐3.02) Data was available from Bryant 1999; Bryant 2003a; Bryant 2005 and Foa 2006. There was strong evidence that the TF‐CBT intervention had an effect at initial follow‐up (k=4, n=198; SMD ‐0.67, 95% CI ‐1.12, ‐0.23). A moderate level of statistical heterogeneity was indicated (I²=53%). The three studies conducted by Bryant and colleagues all included participants who met diagnostic criteria for Acute Stress Disorder. Some participants in Foa 2006 did not meet full diagnostic criteria for PTSD as recruitment normally occurred before one month post trauma (Zoellner personal communication). To investigate the effects of diagnostic clarity a sub‐group analysis was conducted excluding Foa 2006 from the analysis. The magnitude of the effect in favour of treatment was increased (k=3, n=138; SMD ‐0.92 95% CI ‐1.29, ‐0.55)(I²=0%). There was strong evidence that the TF‐CBT intervention had an effect at 6 months follow‐up (random effects) (k=4, n=194; SMD ‐0.60, 95% CI ‐1.03, ‐0.16). A moderate level of statistical heterogeneity was indicated (I²=50%). For reasons outlined above a sub‐group analysis was conducted excluding Foa 2006. Once again, the magnitude of the effect in favour of treatment was increased (k=3, n=134; SMD ‐0.77 95% CI ‐1.15, ‐0.39)(I²=4%). Foa 2006 provided further follow‐up data at 6‐9 months. Evidence for an effect was not strong. (see Table 9 of the Additional Tables). Long term follow‐up data for Bryant 1998; Bryant 1999 and Bryant 2005 was available in Bryant 2003b and Bryant 2006. However, there was evidence of a strong effect in favour of TF‐CBT at 3‐4 years for those available to follow‐up (k=3, n=94; WMD ‐14.52, 95% CI ‐23.20, ‐5.84).
Self report (3.03‐3.04) Data was available from all five studies. There was evidence of a strong effect in favour of TF‐CBTat initial follow‐up (random effects) (k=5, n=240; SMD ‐1.02, 95% CI ‐1.64, ‐0.41). A substantial level of statistical heterogeneity was indicated (I²=76%). For reasons outlined above a sub‐group analysis was undertaken excluding data from Foa 2006. The magnitude of the effect in favour of treatment was increased (k=4, n=170; SMD ‐1.26 95% CI ‐1.91, ‐0.60). The level of statistical heterogeneity remained substantial (I²=68%). There was also evidence of a strong effect in favour of TF‐CBT at 6 months follow‐up (fixed effects) (k=5, n=236; SMD ‐0.54, CI ‐0.82, ‐0.27). The level of heterogeneity in this analysis was low (I²=24%). Nine month follow‐up data were available for Foa 2006. Evidence for an effect was not strong. (see Table 9 of the Additional Tables).
**PTSD diagnosis (3.05‐3.06)**At initial follow‐up there was no evidence of a strong effect for either treatment (random effects) (k=5, n=251; RR 0.56, 95% CI 0.29, 1.06). A substantial level of heterogeneity was indicated (I²=74%). For reasons outlined above a sub‐group analysis was undertaken excluding data from Foa 2006. The magnitude of the effect increased in favour of TF‐CBT (k=4, n=191; RR 0.53, 95% CI 0.33, 0.85)(I²=54%). There was evidence of a strong effect at 6 months follow‐up (random effects) (k=5, n=200; RR 0.37, 95% CI 0.20, 0.67). The level of statistical heterogeneity was moderate (I²=44%). There was no evidence of a strong effect at 3‐4 years (fixed effects)(k=3, n= 137; RR 0.72, 95% CI 0.48, 1.07)(I²=1%). **Anxiety (3.07‐3.08)**There was evidence of a strong effect in favour of TF‐CBT at initial follow‐up (fixed effects) (k=5, n=240, SMD ‐0.40, 95% ‐0.67, ‐0.13) and at 6 months follow‐up (fixed effects)(k=5, n=236; SMD ‐0.49, 95% CI ‐0.76, ‐0.22). The level of statistical heterogeneity was low in both analyses (I²=6% and 0% respectively).
**Depression (3.09‐3.10)**There was evidence of a strong effect in favour of TF‐CBT at initial follow‐up (fixed effects) (k=5, n=240; WMD ‐3.84, 95%CI ‐6.50, ‐1.18) and at 6 months follow‐up (fixed effects)(k=5, n=236; SMD ‐3.94, 95% CI ‐6.50, ‐1.38). No statistical heterogeneity was indicated in either analysis (I²=0% and 0% respectively). Long term follow‐up data were available for Bryant 2005 through Bryant 2006 . There was evidence of a strong effect in favour of TF‐CBT at 3‐4 years for those available to follow‐up (see Table 11 in Additional Tables).
11. Trauma focused CBT vs supportive counselling.
| Study | Outcome | Participants | Statistical Method | Effect Estimate |
|---|---|---|---|---|
| Foa 2006 | 9 month follow‐up for clinician administered PTSD severity | 60 | Mean Difference (IV, Fixed, 95% CI) | 2.51 95% CI ‐4.79, 9.81 |
| Foa 2006 | 9 month follow‐up for self reported PTSD severity | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.45, 95% CI ‐6.63, 7.53 |
| Bryant 2005 in Bryant 2006 | 3‐4 year follow‐up for depression | 35 | Mean Difference (IV, Fixed, 95% CI) | ‐11.62, 95% CI ‐20.68, ‐2.56 |
03.11 Leaving the study earlyThere was no evidence of a strong effect in drop‐out rate between the two treatment groups (fixed effects) (k=5; n=251; RR 1.91, 95% CI 0.98, 3.72)(I²=0), although there was a trend in favour of more participants dropping out of the TF‐CBT group.
Trauma focused CBT vs structured writing therapy for acute PTSDData was available from one study (van Emmerik 2008) with 43 participants in these two treatment interventions. There was no evidence of a strong effect at initial or at long‐term follow‐up on any of the outcome measure reported or in terms of leaving the study early. Weighted means and relative risk are reported by outcome in Table 12 of Additional tables.
12. Trauma focused CBT vs structured writing therapy.
| Outcome | Studies | Participants | Statistical Method | Effect Estimate |
|---|---|---|---|---|
| Severity of PTSD symptoms:self report: Initial outcome | 1 | 43 | Mean Difference (IV, Fixed, 95% CI) | ‐2.47 [‐16.25, 11.31] |
| PTSD diagnosis after treatment: Initial outcome | 1 | 43 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.57 [0.68, 3.65] |
| Anxiety: Initial outcome | 1 | 44 | Mean Difference (IV, Fixed, 95% CI) | 3.19 [‐5.93, 12.31] |
| Depression: Initial outcome | 1 | 44 | Mean Difference (IV, Fixed, 95% CI) | ‐5.09 [‐12.28, 2.10] |
| Leaving the study early due to any reason | 1 | 43 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.40, 2.74] |
**Trauma focused CBT vs cognitive restructuring (without exposure)**Data was available from one study (Bryant 2008) with 60 participants (see Table 13 in Additional Tables).
13. Trauma focused CBT vs cognitive restructuring (without exposure).
| Outcome | Studies | Participants | Statistical Method | Effect Estimate |
|---|---|---|---|---|
| Severity of PTSD symptoms: Initial outcome: Clinician administered | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐11.50 [‐25.39, 2.39] |
| Severity of PTSD symptoms: Initial outcome: Self report | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐10.70 [‐23.28, 1.88] |
| Severity of PTSD (clinician administered): initial outcome: completers | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐11.40 [‐24.96, 2.16] |
| Severity of PTSD (self report): initial outcome: completers | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐12.60 [‐25.42, 0.22] |
| Severity of PTSD Symptoms: 6 Month follow‐up: Clinician administered | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐17.70 [‐32.50, ‐2.90] |
| Severity of PTSD Symptoms: 6 Month follow‐up: Self report | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐13.60 [‐26.00, ‐1.20] |
| PTSD diagnosis after treatment: initial outcome | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.30, 0.94] |
| PTSD diagnosis after treatment: 6 month follow‐up | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.34, 1.00] |
| Anxiety: Initial outcome | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐10.00 [‐17.47, ‐2.53] |
| Anxiety: 6 month follow‐up | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐10.50 [‐18.80, ‐2.20] |
| Depression: Initial outcome | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐6.80 [‐13.16, ‐0.44] |
| Depression: 6 month follow‐up | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐8.00 [‐14.63, ‐1.37] |
| Leaving the study early due to any reason | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.84, 1.40] |
Severity of PTSD symptoms _Clinician administered_There was no evidence of a strong effect at initial follow‐up. However, there was evidence of such an effect in favour of TF‐CBT at 6 month follow‐up (see Table 13 in Additional Tables). _Self report_There was no evidence of a strong effect at initial follow‐up. However, there was evidence of such an effect in favour of TF‐CBT at 6 month follow‐up (see Table 13 in Additional Tables).
PTSD diagnosisThere was evidence of a strong effect in favour of trauma focused CBT at initial follow‐up and at 6 month follow‐up (see Table 13 in Additional Tables).
AnxietyThere was evidence of a strong effect in favour of trauma focused CBT at initial follow‐up and at 6 month follow‐up (see Table 13 in Additional Tables).
DepressionThere was evidence of a strong effect in favour of trauma focused CBT at initial follow‐up and at 6 month follow‐up (see Table 13 in Additional Tables).
Leaving the study earlyThere was no evidence of a strong effect in terms of those leaving the study early (n=60; RR 1.09, 95% CI 0.84, 1.40).
Trauma focused CBT vs relaxation to treat acute PTSDData was available from one study (Echeburua 1996) with 20 participants. Evidence of a strong effect was only found for clinician administered severity of PTSD at 12 months follow‐up. This difference was in favour of trauma focused CBT. Weighted means and relative risk are reported by outcome in Table 14 of Additional tables.
14. Trauma focused CBT vs relaxation.
| Outcome | Studies | Participants | Statistical Method | Effect Estimate |
|---|---|---|---|---|
| Severity of PTSD: clinician administered: Initial outcome | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | ‐6.70 [‐13.84, 0.44] |
| Severity of PTSD: clinician administered: 6 month follow‐up | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | ‐4.30 [‐9.02, 0.42] |
| Severity of PTSD: clinician administered:12 month follow‐up | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | ‐5.50 [‐10.20, ‐0.80] |
| PTSD diagnosis after treatment: Initial outcome | 1 | 20 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.40 [0.10, 1.60] |
| PTSD diagnosis after treatment: 6 month follow‐up | 1 | 20 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.02, 7.32] |
| PTSD diagnosis after treatment: 12 month follow‐up | 1 | 20 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.20 [0.01, 3.70] |
| Anxiety: Initial outcome | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | ‐2.10 [‐12.96, 8.76] |
| Anxiety: 6 month follow‐up | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | ‐1.80 [‐9.74, 6.14] |
| Anxiety: 12 month follow‐up | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | ‐3.10 [‐11.34, 5.14] |
| Depression: Initial outcome | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | 0.90 [‐6.71, 8.51] |
| Depression: 6 month follow‐up | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | ‐1.00 [‐5.31, 3.31] |
| Depression: 12 month follow‐up | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | ‐0.50 [‐3.64, 2.64] |
| Leaving the study early due to any reason | 1 | 20 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
10. Trauma focused CBT vs trauma focused CBT plus anxiety managementData was available from one study (Bryant 1999) with 37 participant. There was no evidence of a strong effect at initial or at 6 months follow‐up on any of the outcome measure reported or in terms of leaving the study early. Weighted means and relative risk are reported by outcome in Table 15 of the Additional tables.
15. Trauma focused CBT vs trauma focused CBT plus anxiety management.
| Outcome | Studies | Participants | Statistical Method | Effect Estimate |
|---|---|---|---|---|
| Severity of PTSD symptoms: Initial outcome: Clinician administered | 1 | 29 | Mean Difference (IV, Fixed, 95% CI) | ‐4.46 [‐19.28, 10.36] |
| Severity of PTSD symptoms: Initial outcome: Self Report | 1 | 29 | Mean Difference (IV, Fixed, 95% CI) | ‐7.00 [‐20.51, 6.51] |
| Severity of PTSD symptoms: 6 month follow‐up: Clinician administered | 1 | 26 | Mean Difference (IV, Fixed, 95% CI) | ‐4.77 [‐24.40, 14.86] |
| Severity of PTSD symptoms: 6 month follow‐up: self report | 1 | 26 | Mean Difference (IV, Fixed, 95% CI) | 0.60 [‐14.35, 15.55] |
| PTSD diagnosis after treatment: Initial outcome | 1 | 37 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.38, 2.18] |
| PTSD diagnosis after treatment: 6 month follow‐up | 1 | 26 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.13, 3.35] |
| Anxiety: Initial outcome | 1 | 29 | Mean Difference (IV, Fixed, 95% CI) | 1.61 [‐8.47, 11.69] |
| Anxiety: 6 month follow‐up | 1 | 26 | Mean Difference (IV, Fixed, 95% CI) | 1.62 [‐8.22, 11.46] |
| Depression: Initial outcome | 1 | 29 | Mean Difference (IV, Fixed, 95% CI) | ‐1.15 [‐7.23, 4.93] |
| Depression: 6 month follow‐up | 1 | 26 | Mean Difference (IV, Fixed, 95% CI) | ‐0.95 [‐7.40, 5.50] |
| Leaving the study early due to any reason | 1 | 37 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.31, 3.60] |
12. Trauma focused CBT vs trauma focused CBT plus hypnosisData was available from one study (Bryant 2005) with 63 participants. There was no evidence of a strong effect at initial follow‐up, at 6 months follow‐up or at long‐term follow‐up on any of the outcome measures reported or in terms of leaving the study early. Weighted means and relative risk are reported by outcome in Table 16 of Additional tables.
16. Trauma focused CBT vs trauma focused CBT plus hypnosis.
| Outcome | Studies | Participants | Statistical Method | Effect Estimate |
|---|---|---|---|---|
| Severity of PTSD symptoms: Initial outcome: Clinician administered | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | ‐0.22 [‐11.84, 11.40] |
| Severity of PTSD symptoms: Initial outcome Self Report | 1 | 63 | Mean Difference (IV, Fixed, 95% CI) | 1.31 [‐8.51, 11.13] |
| Severity of PTSD symptoms: 6 month follow‐up: Clinician administered | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | ‐0.42 [‐15.65, 14.81] |
| 13.4 Severity of PTSD symptoms: 6 month follow‐up: Self report | 1 | 63 | Mean Difference (IV, Fixed, 95% CI) | 1.40 [‐10.16, 12.96] |
| Severity of PTSD symptoms: 2‐4 year follow‐up: Clinician administered | 1 | 37 | Mean Difference (IV, Fixed, 95% CI) | ‐0.68 [‐16.40, 15.04] |
| PTSD diagnosis after treatment: Initial outcome | 1 | 63 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.21 [0.60, 2.46] |
| PTSD diagnosis after treatment: 6 month follow‐up | 1 | 63 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.52, 1.58] |
| PTSD diagnosis after treatment: 2‐4 year follow‐up: ITT data | 1 | 63 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.48, 1.49] |
| PTSD diagnosis after treatment: 2‐4 year follow‐up: Completer only data | 1 | 37 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.10, 2.28] |
| Anxiety: Initial outcome | 1 | 63 | Mean Difference (IV, Fixed, 95% CI) | ‐0.56 [‐7.03, 5.91] |
| Anxiety: 6 month follow‐up | 1 | 63 | Mean Difference (IV, Fixed, 95% CI) | ‐1.40 [‐7.81, 5.01] |
| Depression: Initial outcome | 1 | 63 | Mean Difference (IV, Fixed, 95% CI) | 1.87 [‐2.95, 6.69] |
| Depression: 6 month follow‐up | 1 | 63 | Mean Difference (IV, Fixed, 95% CI) | 1.04 [‐4.21, 6.29] |
| Depression: 2‐4 year follow‐up | 1 | 37 | Mean Difference (IV, Fixed, 95% CI) | 1.59 [‐5.73, 8.91] |
| Leaving the study early due to any reason | 1 | 63 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.50, 2.75] |
Publication biasFourteen of the 15 studies identified for this review have been published. There were insufficient numbers of studies in each comparison to allow for meaningful consideration of publication bias using funnel plots (Lau 2006).
Discussion
Main findings
We identified 15 RCTs of early psychological interventions starting within three months of a traumatic event that were designed to reduce traumatic stress symptoms in individuals who had become symptomatic with ASD, acute PTSD or sub‐threshold variants of these disorders. The studies included in this review evaluated a number of psychological interventions including TF‐CBT, cognitive restructuring, structured writing intervention, supportive counselling, stepped collaborative care, behavioural activation and relaxation training.
The evidence available showed that TF‐CBT had greater effect than waiting list/usual care and supportive counselling at reducing traumatic stress symptoms in individuals who were symptomatic at entry into the study. These effects were demonstrated across a number of outcome measures. The magnitude of effect varied and was largest for TF‐CBT when participants met full diagnosis for ASD/ acute PTSD. Evidence of the benefits of TF‐CBT for symptomatic individuals who did not meet diagnostic criteria for these interventions was weaker. The only evidence to support any other form of treatment was for cognitive restructuring, which was also demonstrated to have a greater effect than a waiting list intervention on the primary outcome measure but less effect than TF‐CBT. There was evidence of continuing benefits of TF‐CBT over supportive counselling across a number of measures at six month follow‐up and some positive outcomes at long term follow‐up. However, the numbers of individuals included in these analyses was small and need to be interpreted with particular caution. TF‐CBT delivered with an augmentation intervention of either anxiety management or hypnosis showed no greater effect than delivery of TF‐CBT alone. TF‐CBT performed better than supportive counselling, suggesting that active components of TF‐CBT are required as opposed to effectiveness being due to non‐specific factors such as attention or a supportive relationship. The absence of evidence for other treatments does not mean they are ineffective but that they may not have been appropriately evaluated to date.
Heterogeneity
There was evidence of both clinical and statistical heterogeneity in the included studies.
Clinical heterogeneity
Although all the trials attempted to reduce traumatic stress symptoms, the nature of the interventions was quite diverse. This was primarily dealt with by separating interventions into predetermined groups including TF‐CBT, supportive counselling and psycho‐education. There were more studies evaluating TF‐CBT than other interventions but the specific interventions in the TF‐CBT group were not identical. All were trauma focused, but some TF‐CBT interventions primarily used a prolonged exposure paradigm (e.g. Bisson 2004), whereas others (e.g. Ehlers 2003b) primarily used cognitive techniques with more limited exposure. In addition, the total number of hours of intervention provided varied from around four hours to around 16 hours.
There were also differences in the clinical populations, especially with regards to the severity of symptoms at entry to the studies. Some studies only included ASD or acute PTSD sufferers, some included all distressed individuals irrespective of them meeting the criteria for a specific diagnosis (e.g. Bisson 2004; Zatzick 2004) and others included only individuals with either ASD or acute PTSD (see Table 1 of the Additional Tables). We tried to address this by considering diagnostic status separately and by performing sub‐group analyses of the studies that included individuals who met full diagnostic criteria for either ASD and/ or acute PTSD only.
There were also difference in the type of trauma that study participants were exposed to. Two studies (Echeburua 1996 and Foa 2006) included only individuals who had experienced sexual assault or rape. Outcomes in these two studies were not as positive as those in other studies evaluating TF‐CBT interventions, although this might partly be as a result of sample size and other methodological issues. Other studies included participants who were exposed to a more heterogeneous range of single traumas, such as RTAs, industrial accidents and assaults. Findings from this review are most appropriately generalised to these groups. Participants in Wagner 2007 and Zatzick 2004 were also hospitalised.
Varying levels of co‐morbidity may also have been a source of clinical heterogeneity. There was insufficient data in the identified studies to allow us to consider this in analyses.
Statistical heterogeneity
The I² statistic demonstrated inconsistencies in the outcomes of some trials that were grouped together and substantial levels of statistical heterogeneity were indicated in a number of the analyses that were undertaken. When statistical heterogeneity was identified we used a random effects model as opposed to a fixed‐effect model to calculate more conservative confidence intervals. We concluded that all trials were essentially trying to measure the same thing and that it was worthwhile summarizing their combined results, but the variation means that caution should be applied when interpreting the results (Fletcher 2007).
Methodological quality
The overall quality of the studies was varied and is described above. Using the Cochrane quality criteria, 13 (87%) studies fully reported loss to follow‐up with reasons, ten (67%) described using appropriately blinded assessors to measure outcome, nine (60%) described appropriate sequence generation, with no bias possible and only six (40%) reported adequate allocation concealment. The small sample sizes of most of the studies are also an important limitation. However, the intervention and control groups in most studies appeared well matched at baseline reducing the risk of the reported unadjusted mean outcomes being influenced by baseline differences. Several studies, including those that provided more positive results, had strong methodological characteristics. Previous research (Moher 1998) has found an association between poorer methodology and more favourable results. The apparent opposite finding of this review may reflect the tendency for better studies to be more recent and therefore associated with improved techniques (cf Bisson 2007a), and to have focused on symptomatic individuals.
As with all psychological treatment trials there are issues with the control groups. This is particularly important in early intervention research where a reduction in symptoms over the duration of the trial would be expected given the natural course of traumatic stress reactions. The development of a psychological treatment placebo is very difficult, if not impossible, as is blinding of participants and therapists. Some of the wait list/usual care groups may have received some form of intervention by virtue of contact through symptom monitoring but this was not properly evaluated and it is not possible to determine what, if any, impact on outcomes this would have had.
Potential biases in the review process
This review adhered strictly to the Cochrane Collaboration guidelines. This will have reduced potential bias but there is likely to have been a bias towards published as opposed to unpublished studies and English language rather than other language manuscripts. Full data were not available for all studies although this potential bias was reduced by personal contact with authors of papers who supplied information that could not be extracted from the published manuscripts. The clear inclusion and exclusion criteria helped with correct identification as did the fact that study selection was performed independently by two of the review authors, with a third becoming involved if there were any disagreements.
Tolerability
Unfortunately only one study Bryant 2008 reported adverse effects and it is unclear whether or not any occurred. The dropout rates were no higher in the intervention than the control groups across the studies reviewed suggesting that the interventions did not cause major adverse effects. However, the absence of tolerability assessment is a key shortcoming in the RCTs identified and one that has previously been noted in psychological treatment studies of chronic PTSD (Bisson 2007a).
Authors' conclusions
Implications for practice.
This review supports the efficacy of trauma focused cognitive behavioural therapy as a treatment for individuals with acute traumatic stress symptoms. TF‐CBT was the only early psychological intervention with some evidence of efficacy (excepting the weaker evidence for cognitive restructuring without exposure). For those meeting full diagnostic criteria for ASD or acute PTSD the evidence was good, although this needs to be tempered by the fact there were a number of potential sources of bias from the studies included and it is noted that five of the trials came from the same research group. Nevertheless this evidence indicates that ASD and acute PTSD sufferers should be offered TF‐CBT.
Whilst the majority of symptomatic individuals are likely to gain some benefit from TF‐CBT between one and three months following a traumatic event, the magnitude may not be very large. Whether or not the magnitude of improvement is likely to be clinically significant enough to justify the routine provision of TF‐CBT to all symptomatic individuals is open to debate. The evidence suggests that TF‐CBT should be considered for those who experience ASD or acute PTSD as a result of a single trauma and that limiting it to this group may be justified, particularly when resources are limited. The limited availability of longer term follow‐up in the trials included in this review makes interpretation of the results difficult. The results from the limited numbers of studies that did include follow‐up suggested slightly reduced effectiveness over time. The results for non TF‐CBT interventions were disappointing but it remains possible that elements from some interventions are effective, particularly if used with more symptomatic individuals. For example, behavioural reactivation (Wagner 2007) has clearly not yet been evaluated with an adequately powered trial and would benefit from further evaluation.
The results of this review are in line with calls that have been made for a stepped or stratified care system whereby those with the most symptoms are offered more complex interventions (e.g. Brewin 2008). The fact that TF‐CBT appears to be an effective treatment suggests that more work should be done to determine if it could be delivered as part of a screening programme after major traumatic events. The results also suggest that not all ASD or acute PTSD sufferers will benefit from TF‐CBT. There is a lack of evidence regarding what to do next in such circumstances. Extending the number of sessions and re‐evaluation would seem appropriate depending on the clinical presentation, but there is currently no evidence for the effectiveness of any other form of intervention within three months of a traumatic event including pharmacological interventions (NCCMH 2005).
Implications for research.
Further well‐designed randomised controlled trials of TF‐CBT and other psychological treatments, including eye movement desensitization and reprocessing, within the first three months of traumatic events are required. There is a need for further comparison studies of one type of psychological treatment against another and the role, if any, of pharmacological treatments in combination with psychological treatment. Most of the studies included in this review have attempted to evaluate individual psychological therapy. Given the important role of social support as a predictor of outcome (Brewin 2000; Ozer 2003) it would be of interest to examine interventions aimed at couples and families to improve familial response. It would also be of interest to evaluate forms of community intervention and interventions aimed at improving coping skills and enhancing positive and helpful behaviours (Ruzek 2007).
All of the studies included in this review were with civilian populations exposed to single traumas. There is a particular need to evaluate the effectiveness of early interventions for those involved in combat and exposed to war and disasters. Future research should also explore the optimal time to intervene, how long treatment should last for and whether other techniques can be incorporated into existing treatments to improve their efficacy. There is also a need for larger effectiveness trials of TF‐CBT to determine if the results of the efficacy trials can be achieved in real practice. Future trials should consider adverse events and tolerability of treatment, and carefully control for additional intervention.
What's new
| Date | Event | Description |
|---|---|---|
| 6 December 2011 | Amended | Plain language title added |
History
Protocol first published: Issue 1, 2008 Review first published: Issue 3, 2010
| Date | Event | Description |
|---|---|---|
| 24 February 2010 | Amended | Slight amendments to contact details of three authors, including contact author |
| 28 October 2008 | Amended | Converted to new review format. |
| 29 February 2008 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
We wish to express our thanks to Jonathan Bisson, Richard Bryant, Alison Bugg, Anke Ehlers, Lars‐Göran Öst, Marit Sijbrandij, Arnold van Emmerik, Amy Wagner, Doug Zatzick and Lori Zoellner for providing additional unpublished data and to Barbara Rothbaum and Maryrose Geradi for allowing us to consider an unpublished study. We would like to express thanks to Robert Newcombe for statistical advice and Helen Davies for administrative support. We should also like to thank Hugh McGuire for his help with searches and Rachel Churchill, Jane Tuckerman, Vivien Hunot and Jane Dennis for their helpful comments and assistance in preparing this report. Finally thanks to those experts who responded with additional suggestions and contacts during the search process.
Appendices
Appendix 1. Quality assessment tool
| QUALITY ASSESSMENT TOOL FOR INCLUDED STUDIES 1. Clearly defined target symptoms for inclusionNo clear diagnosis or symptom definition 0Not all participants meet target symptom criteria 1All participants meet target symptom criteria 2 2. Reliable and valid measures of change with good psychometric propertiesDid not use reliable and valid measures 0Measures used inadequate to measure change 1Reliable valid and adequate measures used 2 3. Participants satisfy A1 & A2 criteriaStudy has not determined but majority likely to have satisfied A1 criterion 0A1 and/or A2 criteria assessed but not all participants satisfy them 1All participants satisfied A1 & A2 criteria 2 4. Assessor reliabilityNo training in administration of instruments used in the study 0Training in administration of instruments used in the study 1Training with performance supervision or reliability checks 2 5. Manualised, replicable, specific treatmentTreatment was not replicable or specific 0Treatment was partially described but not easily replicable 1Treatment was clearly described and replicable with manual available 2 6. Treatment adherenceTreatment fidelity poor 0Treatment fidelity variable or self monitored by therapist only 1Treatment fidelity independently checked and adequate 2 7. Non‐confounded conditions (eg concurrent psychotherapy orPsychopharmacology, violent household etc)Most participant exposed to confounds with no control for variables 0Few participants exposed to confounds with no control for variables 1Confounds non‐existent or controlled for (eg exclusion, matched assignment) 2 8. Use of multi‐modal measuresSelf‐report measures only 0Clinician administered structured interview only 1Clinician administered structured interview plus self report 2 9. Reported level of therapists trainingNo qualifications for treating clinicians provided 0Qualifications for treatment group, clinicians provided 1Qualifications for treatment group and comparative group, clinicians provided 2 10. Use of a control or comparison groupUse of a usual care group 0Use of a waiting list control group 1Use of a minimal treatment control group 2 11. Clear definition of the population/ participant group to receive intervention in termsof exposure, time since exposure, pre‐morbid vulnerability factors and otherDemographicsParticipant group inadequately described 0Participant group partially described 1Participants clearly described 2 12. Adequate follow‐up period Follow‐up of less than 3 months 0Follow‐up of 3 ‐ 6months 1Follow up period beyond 6 months 2 13. Details on side effectsInadequate detail 0Recorded by group but details inadequate 1Full side effect profiles by group 2 14. Record of exclusion criteria and number of exclusions and refusals reportedCriteria and number not reported 0Criteria or number of exclusions and refusals not reported 1Criteria and number of exclusions and refusals reported 2 15. Information on comparability and adjustment for differences in analysisNo information on comparability 0Some information on comparability with appropriate adjustment 1Sufficient comparability information with appropriate adjustment 2 16. Presentation of results with inclusion of data for re‐analysis of main outcomes(eg standard deviations)Inadequate presentation 0Adequate 1Comprehensive 2 17. Power calculationNot reported 0Mentioned without details 1Details of calculation provided 2 18. Statistical analysis appropriate for sample size (including correction for multiple test whereApplicable) Inadequate 0Adequate 1Appropriate and comprehensive 2 19. Conclusions justified (eg accurate representation of results, acknowledgement of methodological limitations)No 0Partially 1Yes 2 | Not reported |
|---|
Data and analyses
Comparison 1. Trauma focused CBT vs waiting list.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Severity of PTSD symptoms (clinician administered): Initial outcome | 6 | 469 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.64 [‐1.06, ‐0.23] |
| 2 Severity of PTSD symptoms for individuals meeting diagnosis for ASD or acute PTSD (clinician administered) | 4 | 208 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.96 [‐1.56, ‐0.36] |
| 3 Severity of PTSD symptoms (clinician administered): 3‐5 month follow‐up | 2 | 204 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.17 [‐0.45, 0.11] |
| 4 Severity of PTSD symptoms (clinician administered): 9‐11 month follow‐up | 2 | 73 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.33 [‐0.80, 0.15] |
| 5 Severity of PTSD symptoms (self report): Initial outcome | 6 | 370 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.83 [‐1.43, ‐0.23] |
| 6 Severity of PTSD symptoms for individuals meeting diagnosis for ASD or acute PTSD (self report) | 4 | 158 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.16 [‐1.73, ‐0.58] |
| 7 Severity of PTSD symptoms (self report): 9‐11 month follow‐up | 2 | 73 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.31 [‐0.79, 0.17] |
| 8 PTSD diagnosis after treatment: Initial outcome | 7 | 515 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.50, 1.05] |
| 9 PTSD diagnosis after treatment for individuals meeting diagnosis for ASD or acute PTSD: Initial outcome | 5 | 254 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.31, 0.95] |
| 10 PTSD diagnosis after treatment: 3‐5 month follow‐up | 2 | 141 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.42, 0.99] |
| 11 PTSD diagnosis after treatment: 9‐11 month follow‐up | 2 | 54 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.27, 1.36] |
| 12 Anxiety: Initial outcome | 7 | 513 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐0.91, ‐0.15] |
| 13 Anxiety 3‐5 month follow‐up | 2 | 204 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.19 [‐0.47, 0.08] |
| 14 Anxiety: 9‐11 month follow‐up | 2 | 73 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.31 [‐0.79, 0.16] |
| 15 Depression: Initial outcome | 7 | 513 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.49 [‐0.80, ‐0.18] |
| 16 Depression: 3‐5 month follow‐up | 2 | 204 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.12 [‐0.39, 0.16] |
| 17 Depression: 9‐11 month follow‐up | 2 | 73 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.21 [‐0.67, 0.26] |
| 18 Leaving the study early due to any reason | 7 | 515 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.63, 1.26] |
1.1. Analysis.
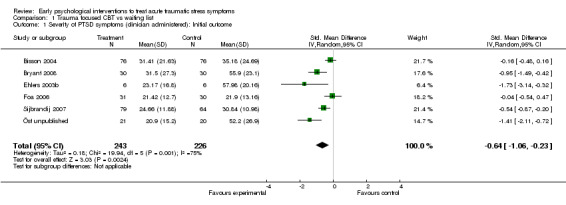
Comparison 1 Trauma focused CBT vs waiting list, Outcome 1 Severity of PTSD symptoms (clinician administered): Initial outcome.
1.2. Analysis.
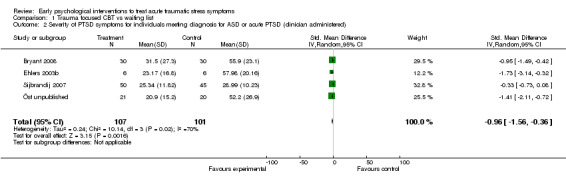
Comparison 1 Trauma focused CBT vs waiting list, Outcome 2 Severity of PTSD symptoms for individuals meeting diagnosis for ASD or acute PTSD (clinician administered).
1.3. Analysis.
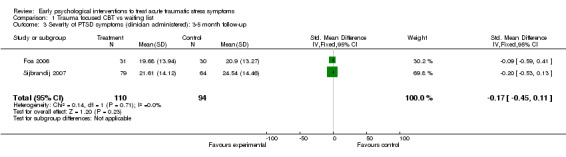
Comparison 1 Trauma focused CBT vs waiting list, Outcome 3 Severity of PTSD symptoms (clinician administered): 3‐5 month follow‐up.
1.4. Analysis.
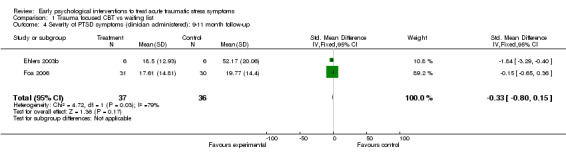
Comparison 1 Trauma focused CBT vs waiting list, Outcome 4 Severity of PTSD symptoms (clinician administered): 9‐11 month follow‐up.
1.5. Analysis.
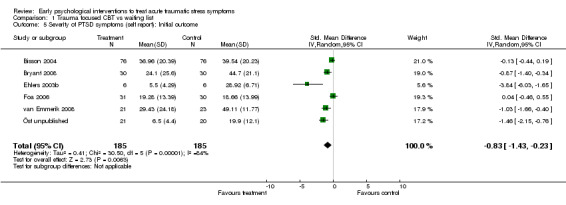
Comparison 1 Trauma focused CBT vs waiting list, Outcome 5 Severity of PTSD symptoms (self report): Initial outcome.
1.6. Analysis.
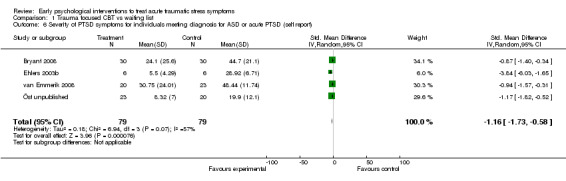
Comparison 1 Trauma focused CBT vs waiting list, Outcome 6 Severity of PTSD symptoms for individuals meeting diagnosis for ASD or acute PTSD (self report).
1.7. Analysis.
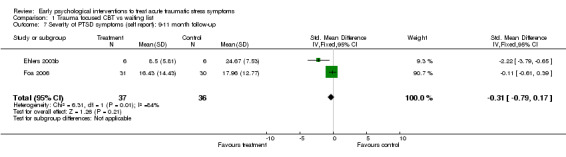
Comparison 1 Trauma focused CBT vs waiting list, Outcome 7 Severity of PTSD symptoms (self report): 9‐11 month follow‐up.
1.8. Analysis.
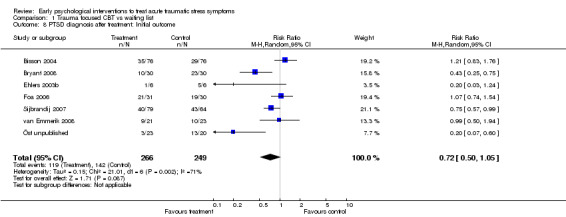
Comparison 1 Trauma focused CBT vs waiting list, Outcome 8 PTSD diagnosis after treatment: Initial outcome.
1.9. Analysis.
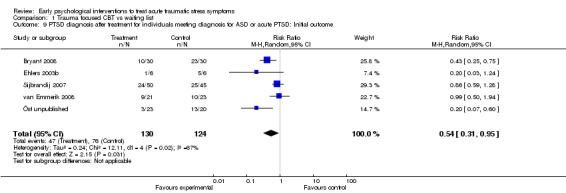
Comparison 1 Trauma focused CBT vs waiting list, Outcome 9 PTSD diagnosis after treatment for individuals meeting diagnosis for ASD or acute PTSD: Initial outcome.
1.10. Analysis.
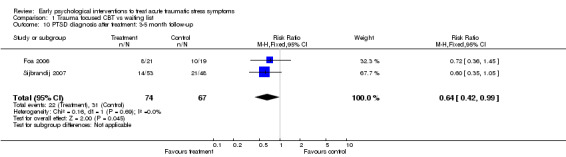
Comparison 1 Trauma focused CBT vs waiting list, Outcome 10 PTSD diagnosis after treatment: 3‐5 month follow‐up.
1.11. Analysis.
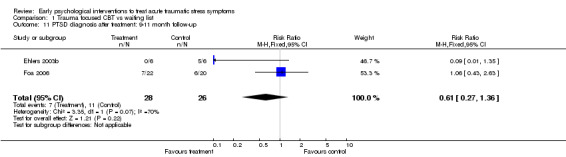
Comparison 1 Trauma focused CBT vs waiting list, Outcome 11 PTSD diagnosis after treatment: 9‐11 month follow‐up.
1.12. Analysis.
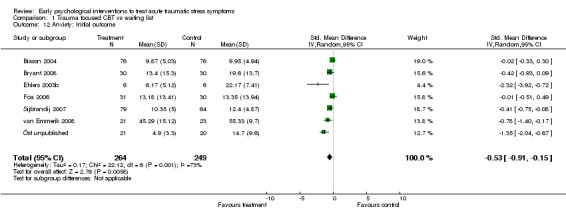
Comparison 1 Trauma focused CBT vs waiting list, Outcome 12 Anxiety: Initial outcome.
1.13. Analysis.
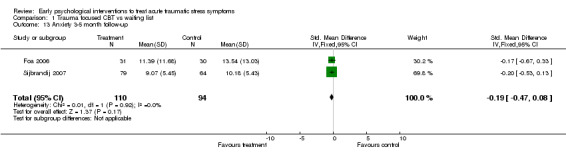
Comparison 1 Trauma focused CBT vs waiting list, Outcome 13 Anxiety 3‐5 month follow‐up.
1.14. Analysis.
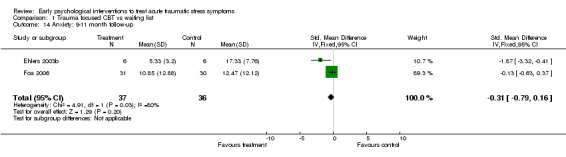
Comparison 1 Trauma focused CBT vs waiting list, Outcome 14 Anxiety: 9‐11 month follow‐up.
1.15. Analysis.
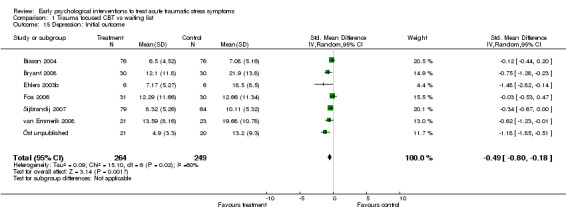
Comparison 1 Trauma focused CBT vs waiting list, Outcome 15 Depression: Initial outcome.
1.16. Analysis.
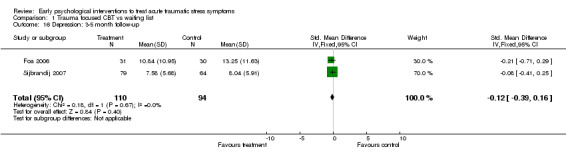
Comparison 1 Trauma focused CBT vs waiting list, Outcome 16 Depression: 3‐5 month follow‐up.
1.17. Analysis.
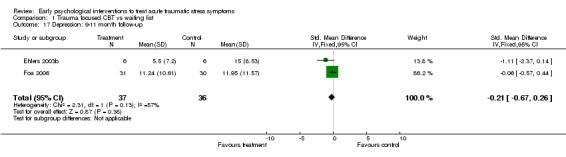
Comparison 1 Trauma focused CBT vs waiting list, Outcome 17 Depression: 9‐11 month follow‐up.
1.18. Analysis.
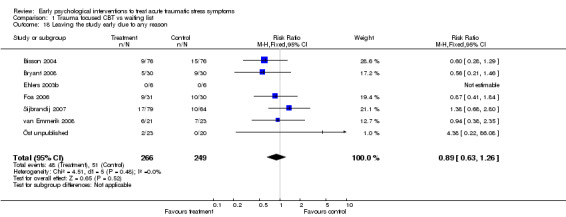
Comparison 1 Trauma focused CBT vs waiting list, Outcome 18 Leaving the study early due to any reason.
Comparison 2. Structured writing intervention vs minimal intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Severity of PTSD symptoms: self report: initial outcome | 2 | 149 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.15 [‐0.48, 0.17] |
| 2 Anxiety | 2 | 149 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.14 [‐0.46, 0.19] |
| 3 Depression | 2 | 149 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.34, 0.30] |
| 4 Leaving the study early due to any reason | 2 | 149 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.65, 1.66] |
2.1. Analysis.
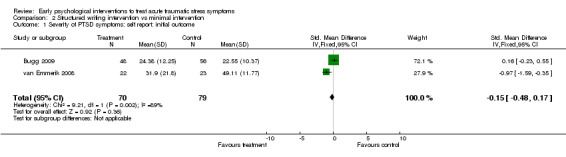
Comparison 2 Structured writing intervention vs minimal intervention, Outcome 1 Severity of PTSD symptoms: self report: initial outcome.
2.2. Analysis.
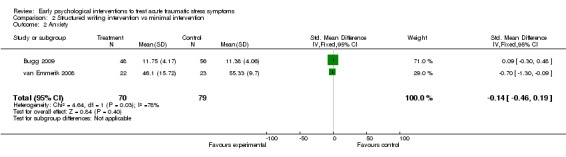
Comparison 2 Structured writing intervention vs minimal intervention, Outcome 2 Anxiety.
2.3. Analysis.
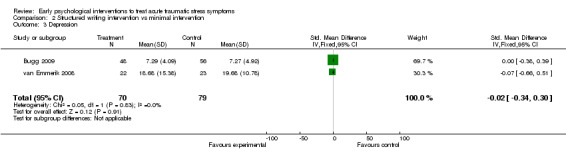
Comparison 2 Structured writing intervention vs minimal intervention, Outcome 3 Depression.
2.4. Analysis.
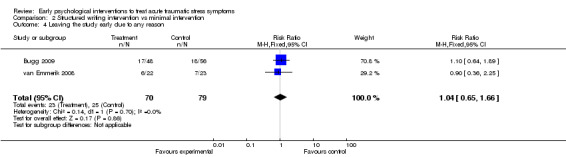
Comparison 2 Structured writing intervention vs minimal intervention, Outcome 4 Leaving the study early due to any reason.
Comparison 3. Trauma focused CBT vs supportive counselling.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Severity of PTSD symptoms (clinician administered): Initial outcome | 4 | 198 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.67 [‐1.12, ‐0.23] |
| 2 Severity of PTSD symptoms (clinician administered): 3‐6 month follow‐up | 4 | 194 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐1.03, ‐0.16] |
| 3 Severity of PTSD symptoms (self report): Initial outcomes | 5 | 240 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.02 [‐1.64, ‐0.41] |
| 4 Severity of PTSD symptoms (self report): 3‐6 Month follow‐up | 5 | 236 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.54 [‐0.82, ‐0.27] |
| 5 PTSD diagnosis: initial outcomes | 5 | 251 | Risk Ratio (M‐H, Random, 95% CI) | 0.56 [0.29, 1.06] |
| 6 PTSD diagnosis: 3‐6 month follow‐up | 5 | 200 | Risk Ratio (M‐H, Random, 95% CI) | 0.37 [0.20, 0.67] |
| 7 Anxiety: initial outcome | 5 | 240 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.40 [‐0.67, ‐0.13] |
| 8 Anxiety: 3‐6 month follow‐up | 5 | 236 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.49 [‐0.76, ‐0.22] |
| 9 Depression: Initial outcome | 5 | 240 | Mean Difference (IV, Fixed, 95% CI) | ‐3.84 [‐6.50, ‐1.18] |
| 10 Depression: 3‐6 month follow‐up | 5 | 236 | Mean Difference (IV, Fixed, 95% CI) | ‐3.94 [‐6.50, ‐1.38] |
| 11 Leaving the study early due to any reason | 5 | 251 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.91 [0.98, 3.72] |
3.1. Analysis.
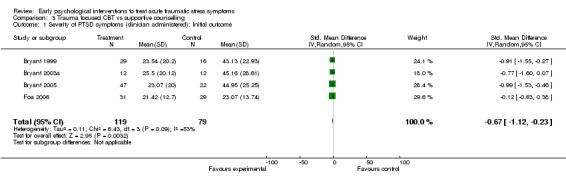
Comparison 3 Trauma focused CBT vs supportive counselling, Outcome 1 Severity of PTSD symptoms (clinician administered): Initial outcome.
3.2. Analysis.
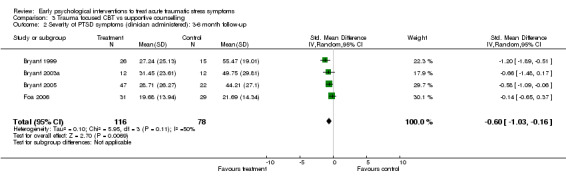
Comparison 3 Trauma focused CBT vs supportive counselling, Outcome 2 Severity of PTSD symptoms (clinician administered): 3‐6 month follow‐up.
3.3. Analysis.
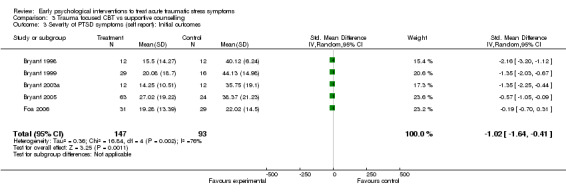
Comparison 3 Trauma focused CBT vs supportive counselling, Outcome 3 Severity of PTSD symptoms (self report): Initial outcomes.
3.4. Analysis.
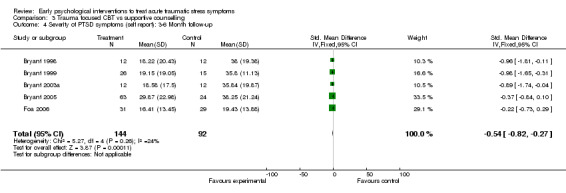
Comparison 3 Trauma focused CBT vs supportive counselling, Outcome 4 Severity of PTSD symptoms (self report): 3‐6 Month follow‐up.
3.5. Analysis.
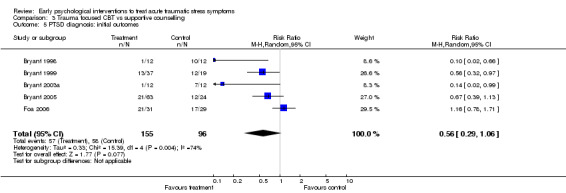
Comparison 3 Trauma focused CBT vs supportive counselling, Outcome 5 PTSD diagnosis: initial outcomes.
3.6. Analysis.
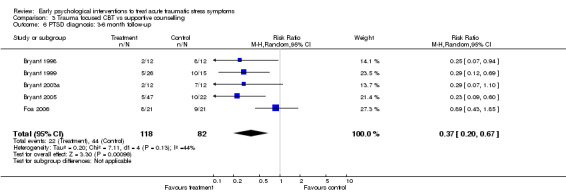
Comparison 3 Trauma focused CBT vs supportive counselling, Outcome 6 PTSD diagnosis: 3‐6 month follow‐up.
3.7. Analysis.
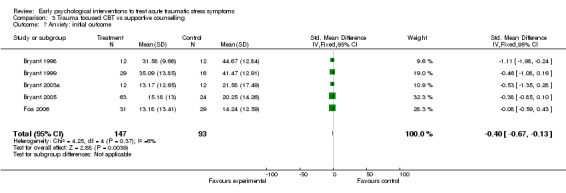
Comparison 3 Trauma focused CBT vs supportive counselling, Outcome 7 Anxiety: initial outcome.
3.8. Analysis.
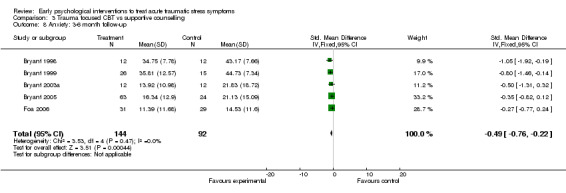
Comparison 3 Trauma focused CBT vs supportive counselling, Outcome 8 Anxiety: 3‐6 month follow‐up.
3.9. Analysis.
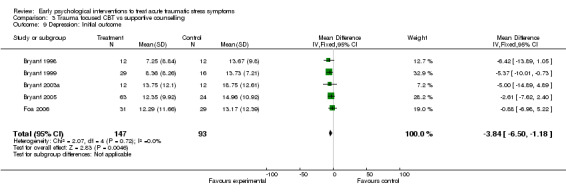
Comparison 3 Trauma focused CBT vs supportive counselling, Outcome 9 Depression: Initial outcome.
3.10. Analysis.
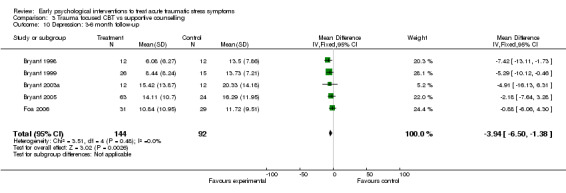
Comparison 3 Trauma focused CBT vs supportive counselling, Outcome 10 Depression: 3‐6 month follow‐up.
3.11. Analysis.
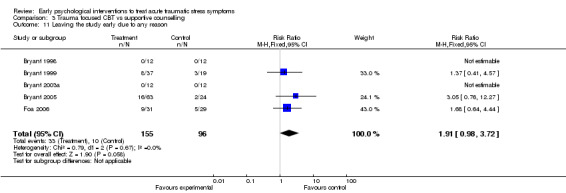
Comparison 3 Trauma focused CBT vs supportive counselling, Outcome 11 Leaving the study early due to any reason.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bisson 2004.
| Methods | RCT ‐ bias unlikely | |
|---|---|---|
| Participants | 152 outpatients with acute psychological distress who had physical injury from civilian trauma | |
| Interventions | Four 60 min. sessions of exposure based CBT vs. standard care | |
| Outcomes | CAPS, IES, HAD | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
Bryant 1998.
| Methods | RCT ‐ bias possible | |
|---|---|---|
| Participants | 24 outpatients with Acute Stress Disorder resulting from MVA or industrial accident | |
| Interventions | Five 90 min. weekly sessions of exposure based CBT vs supportive counselling | |
| Outcomes | IES, BDI, STAI, CIDI PTSD module | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
Bryant 1999.
| Methods | RCT ‐ bias possible | |
|---|---|---|
| Participants | 56 outpatients with Acute Stress Disorder resulting from MVA or non‐ sexual assault | |
| Interventions | Five 90 min. weekly sessions of prolonged exposure or prolonged exposure plus anxiety management vs. supportive counselling | |
| Outcomes | IES, BDI, CAPS, STAI | |
| Notes | We have assumed that there is a typographical error in this paper in that 66 participants are reported to have been recruited initially. We assume that this should be 56, otherwise figures reported do not add up. We have not been able to clarify this with the authors. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
Bryant 2003a.
| Methods | RCT ‐ bias possible | |
|---|---|---|
| Participants | 24 outpatients with mild traumatic brain injury and Acute Stress Disorder resulting from MVA or non‐sexual assault | |
| Interventions | Five 90 min. weekly sessions of exposure based CBT vs. supportive counselling | |
| Outcomes | IES, BAI, BDI, CAPS | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
Bryant 2005.
| Methods | RCT ‐ bias unlikely | |
|---|---|---|
| Participants | 87 outpatients with Acute Stress Disorder as a result of MVA or non‐sexual assault | |
| Interventions | Six 90 min. sessions of exposure based CBT or CBT plus hypnosis vs. supportive counselling | |
| Outcomes | CAPS‐2, IES, BAI, BDI | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
Bryant 2008.
| Methods | RCT‐ bias unlikely | |
|---|---|---|
| Participants | 90 outpatient victims of civilian trauma with Acute Stress Disorder | |
| Interventions | Five 90 min sessions of exposure therapy or cognitive restructuring vs. waiting list | |
| Outcomes | CAPS‐2, IES, BAI, BDI, PTCI | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
Bugg 2009.
| Methods | RCT‐ bias unlikely | |
|---|---|---|
| Participants | 148 outpatients with symptoms of ASD who were victims of MVA occupational injury or assault | |
| Interventions | One face to face and two telephone sessions with a writing task and information intervention vs information only | |
| Outcomes | PDS, HADS, WHO QoL‐BREF | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
Echeburua 1996.
| Methods | RCT ‐ bias possible | |
|---|---|---|
| Participants | 20 female victims of rape or sexual assault | |
| Interventions | Five 60 min. session of exposure based CBT vs. relaxation | |
| Outcomes | Scale of Severity of PTSD Symptoms, Modified fear survey, Scale of Adaptation, BDI, STAI | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
Ehlers 2003b.
| Methods | RCT‐ bias unlikely | |
|---|---|---|
| Participants | 85 outpatient victims of MVA with acute or chronic PTSD | |
| Interventions | Twelve plus three 90 min. sessions of trauma focused CBT or self help booklet vs. waiting list | |
| Outcomes | CAPS,BAI, BDI, PDS, Sheehan Disability Scale | |
| Notes | A sub‐sample of 12 participants with acute PTSD were included in this review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
Foa 2006.
| Methods | RCT ‐ bias possible | |
|---|---|---|
| Participants | 90 female victims of sexual and non‐sexual assault meeting diagnosis for PTSD (apart from duration) | |
| Interventions | Four 2 hour sessions of exposure based CBT or supportive counselling vs. continuous assessment. | |
| Outcomes | SCID‐PTSD, SAI. PSSI, BDI, BAI, ETO, UTI | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
Sijbrandij 2007.
| Methods | RCT ‐ bias possible | |
|---|---|---|
| Participants | 143 outpatient victims of various civilian traumatic events with ASD or acute PTSD | |
| Interventions | Four 2 hour weekly sessions of exposure based CBT vs. waiting list | |
| Outcomes | SI‐PTSD, SCID‐I, HADS | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
van Emmerik 2008.
| Methods | RCT‐bias unlikely | |
|---|---|---|
| Participants | 125 outpatients, with ASD, acute PTSD or chronic PTSD who had experienced civilian trauma | |
| Interventions | Five 90 minute sessions of exposure based CBT, or a writing intervention vs. waiting list intervention. | |
| Outcomes | IES, BDI, STAI, DES | |
| Notes | A sub‐sample of 66 participants with ASD or acute PTSD were included in this review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
Wagner 2007.
| Methods | RCT ‐ bias possible | |
|---|---|---|
| Participants | 8 inpatients with acute PTSD who had experienced civilian trauma | |
| Interventions | Up to six 90 min. sessions of behavioural activation and treatment as usual vs. treatment as usual. | |
| Outcomes | PCL, CESD, SF 12 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
Zatzick 2004.
| Methods | RCT ‐ bias unlikely | |
|---|---|---|
| Participants | 121 physically injured hospitalised MVA & assault victims with significant symptoms of PTSD and/or depression | |
| Interventions | Multifaceted collaborative care for PTSD and alcohol abuse | |
| Outcomes | PCL, CIDI alcohol module | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
Öst unpublished.
| Methods | RCT ‐ bias possible | |
|---|---|---|
| Participants | 43 outpatient victims of violent crime with acute PTSD | |
| Interventions | Sixteen 60 min. sessions of exposure based CBT vs. waiting list | |
| Outcomes | CAPS, Hamilton Anx. & Depr. scales, IES‐R, BAI, STAI, BDI, QOL, SAS‐SR, PSS‐SR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Andre 1997 | Preventative study |
| Backman 1997 | Not a true RCT and not a clear early intervention |
| Bordow 1979 | Not a true RCT and does not include outcome measures aimed at assessing symptoms of PTSD |
| Brom 1993 | Preventative study |
| Collie in press | Not an RCT and does not appear to be an early intervention |
| Devilly 1999 | Not an early intervention study |
| Difede 2007 | Not an early intervention study |
| Falsetti 2001 | Not an early intervention study |
| Fecteau 1999 | Not an early intervention study |
| Foa 2004 | Not an early intervention study |
| Gamble 2005 | Preventative study |
| Gidron 2001 | Preventative study |
| Gidron 2007 | Preventative study |
| Hirai 2005 | Not an early intervention study |
| Hollifield 2007 | Not an early intervention study |
| Holmes 2007 | Preventative study |
| Kazak 2005 | Preventative study |
| Lange 2001 | Not an early intervention study |
| Lee 2002 | Not an early intervention study |
| Levine 2005 | Not an early intervention study |
| Marchand 2006 | Preventative study |
| Marcus 1997 | Not an early intervention study |
| Power 2002 | Not an early intervention study |
| Resnick 2005 | Single session intervention |
| Rose 1999 | Single session intervention |
| Rosser 1991 | Not an RCT |
| Rothbaum 1997 | Not an early intervention study |
| Rothbaum submitted | Single session intervention |
| Ryding 1998 | Preventative study |
| Ryding 2004 | Preventative study |
| Scheck 1998 | Not an early intervention study |
| Schoutrop 2002 | Not an early intervention study and it was not clear that participants had experienced a traumatic event consistent with the A1 criteria for diagnosis of PTSD using DSM‐IV. |
| Sloan 2004 | Not an early intervention study |
| Steffgen 2002 | Not an RCT |
| Taylor 2003 | Not an early intervention study |
| Turpin 2005 | Single session intervention |
| Wilson 1995 | Not an early intervention study |
| Zatzick 2001 | Preventative study |
Differences between protocol and review
The title of this review has been changed from 'Multiple session early interventions to treat acute traumatic stress symptoms' to 'Early psychological interventions to treat acute traumatic stress symptoms' for clarity.
Contributions of authors
NR: Writing of the protocol and review. Underook quality assessment and data entry. NJK: Commentary on the protocol and review. Underook quality assessment and recording of data. JK: Commentary on the protocol and review. Underook quality assessment. JIB: Offered supervision of the protocol development and commentary on the protocol and review. Writing of the discussion section of the review.
Sources of support
Internal sources
- Professor Robert Newcombe, Department Primary Care and Public Health, Cardiff University, UK.
Statistical support
External sources
- No sources of support supplied
Declarations of interest
JIB has published one RCT that was included in the review.
Edited (no change to conclusions)
References
References to studies included in this review
Bisson 2004 {published and unpublished data}
- Bisson JI, Shepherd JP, Joy D, Probert R, Newcombe RG. Early cognitive‐behavioural therapy for post‐traumatic stress symptoms after physical injury. British Journal of Psychiatry 2004;184:63‐9. [DOI] [PubMed] [Google Scholar]
Bryant 1998 {published and unpublished data}
- Bryant RA, Harvey AG, Basten C, Dang ST, Sackville T. Treatment of Acute Stress Disorder: A comparison of cognitive‐behavioral therapy and supportive counseling. Journal of Consulting & Clinical Psychology 1998;66(5):862‐6. [DOI] [PubMed] [Google Scholar]
- Bryant RA, Moulds ML, Nixon RVD. Cognitive behaviour therapy of acute stress disorder: a four‐year follow‐up. Behaviour Research & Therapy 2003;41:489‐94. [DOI] [PubMed] [Google Scholar]
Bryant 1999 {published and unpublished data}
- Bryant RA, Moulds ML, Nixon RVD. Cognitive behaviour therapy of acute stress disorder: a four‐year follow‐up. Behaviour Research & Therapy 2003;41:489‐94. [DOI] [PubMed] [Google Scholar]
- Bryant RA, Sackville T, Dang ST, Moulds M, Guthrie R. Treating acute stress disorder: An evaluation of cognitive behavior therapy and supportive counseling techniques. American Journal of Psychiatry 1999;156(11):1780‐6. [DOI] [PubMed] [Google Scholar]
Bryant 2003a {published and unpublished data}
- Bryant RA, Moulds M, Guthrie R, Nixon RDV. Treating acute stress disorder following mild traumatic brain injury. American Journal of Psychiatry 2003;160:585‐7. [DOI] [PubMed] [Google Scholar]
Bryant 2005 {published and unpublished data}
- Bryant RA, Moulds ML, Guthrie RM, Nixon RDV. The additive benefits of hypnosis and cognitive‐behavioral therapy in treating acute stress disorder. Journal of Consulting & Clinical Psychology 2005;73(2):334‐40. [DOI] [PubMed] [Google Scholar]
- Bryant RA, Moulds ML, Nixon RDV, Mastrodomenico J, Felmingham K, Hopwood S. Hypnotherapy and cognitive behaviour therapy of acute stress disorder: A 3‐year follow‐up. Behaviour Research & Therapy 2006;44:1331‐5. [DOI] [PubMed] [Google Scholar]
Bryant 2008 {published and unpublished data}
- Bryant RA, Mastrodomenico J, Felmingham KL, Hopwood S, Kenny L, Kandris E, Cahill C, Creamer M. Treatment of Acute Stress Disorder: A randomized controlled trial. Archives of General Psychiatry 2008;65(6):659‐667. [DOI] [PubMed] [Google Scholar]
Bugg 2009 {published and unpublished data}
- Bugg A, Turpin G, Mason S, Scholes C. A randomised controlled trial of the effectiveness of writing as a self‐help intervention for traumatic injury patients at risk of developing post‐traumatic stress disorder. Behaviour Research and Therapy 2009;47:6‐12. [DOI] [PubMed] [Google Scholar]
Echeburua 1996 {published data only}
- Echeburua E, Corral P, Sarasua B, Zubizarreta I. Treatment of acute posttraumatic stress disorder in rape victims: An experimental study. Journal of Anxiety Disorders 1996;10(3):185‐99. [Google Scholar]
Ehlers 2003b {published and unpublished data}
- Ehlers A, Clark DM, Hackmann A, McManus F, Fennell M, Herbert C, Mayou R. A randomized controled trial of cognitive therapy, a self help booklet, and repeated assessments as early interventions for posttraumatic stress disorder. Archives of General Psychiatry 2003;60:1024‐32. [DOI] [PubMed] [Google Scholar]
Foa 2006 {published and unpublished data}
- Foa EB, Zoellner LA, Feeny NC. An evaluation of three brief programs for facilitating recovery after assault. Journal of Traumatic Stress 2006;19(1):29‐43. [DOI] [PubMed] [Google Scholar]
Sijbrandij 2007 {published and unpublished data}
- Sijbrandij M, Olff M, Reitsma JB, Carlier IVE, Vries MH, Gersons BPR. Treatment of acute posttraumatic stress disorder with brief cognitive behavioural therapy: A randomised controlled trial. American Journal of Psychiatry 2007;164:82‐90. [DOI] [PubMed] [Google Scholar]
van Emmerik 2008 {published and unpublished data}
- Emmerik AAP, Kamphuis JH, Emmelkamp PMG. Treating acute stress disorder and posttraumatic stress disorder with cognitive behavioural therapy or structured writing therapy: A randomised controlled trial. Psychotherapy and Psychosomatics 2008;77(2):93‐100. [DOI] [PubMed] [Google Scholar]
Wagner 2007 {published and unpublished data}
- Wagner AW, Zatzick DF, Ghesquiere A, Jurkovoich GJ. Behavioral activation as an early intervention for posttraumatic stress disorder and depression. Cognitive and Behavioral Practice 2007;4:341‐9. [Google Scholar]
Zatzick 2004 {published and unpublished data}
- Zatzick D, Roy‐Byrne P, Russo J, Rivara F, Droesch R, Wagner A, Dunn C, Jurkovich G, Uehara E, Katon W. A randomized effectiveness trial of stepped collaborative care for acutely injured trauma survivors. Archives of General Psychiatry 2004;61:498‐506. [DOI] [PubMed] [Google Scholar]
Öst unpublished {unpublished data only}
- Öst LG, Paunovic N, Gillow AM. Cognitive‐behavior therapy in the prevention of chronic PTSD in crime victims. Unpublished manuscript.
References to studies excluded from this review
Andre 1997 {published data only}
- Andre C, Lelord F, Legeron P, Reignier A, Delattre A. Effectiveness of early intervention on 132 bus drivers victims of aggressions: a controlled trial [Etude controlee sur l'efficacite a 6 mois d'une prise en charge precoce de 132 conducteurs d'autobus victimes d'agression]. L'Encephale 1997;23:65‐71. [PubMed] [Google Scholar]
Backman 1997 {published data only}
- Backman L, Arnetz BB, Levin D, Lublin A. Psychphysiological effects of mental imaging training for police trainees. Stress Medicine 1997;13:43‐8. [Google Scholar]
Bordow 1979 {published data only}
- Bordow S, Porritt D. An experimental evaluation of crisis intervention. Social Science & Medicine 1979;13A:251‐256. [PubMed] [Google Scholar]
Brom 1993 {published data only}
- Brom D, Kleber RJ, Hofman M. Victims of traffic accidents: Incidence and prevention of post‐traumatic stress disorder. Journal of Clinical Psychology 1993;49(2):131‐40. [DOI] [PubMed] [Google Scholar]
Collie in press {unpublished data only}
- Collie K, Kreshka MA, Ferrier S, Parsons R, Graddy K, Avram S, Mannell P, Chen X, Perkins J, Koopman C. Videoconferencing for delivery of breast cancer support groups to women living in rural communities: A pilot study. Psycho‐Oncology In press. [DOI] [PubMed]
Devilly 1999 {published data only}
- Devilly GJ, Spence SH. The relative efficacy and treatment distress of EMDR and a cognitive‐ behavior trauma treatment protocol in the amelioration of posttraumatic stress disorder. Journal of Anxiety Disorders 1999;13(1‐2):131‐57. [DOI] [PubMed] [Google Scholar]
Difede 2007 {published data only}
- Difede J, Malta LS, Best S, Henn‐Haase C, Metzler T, Bryant R, Marmar C. A randomized controlled clinical treatment trial for World Trade Center attack‐related PTSD in disaster workers. Journal of Nervous and Mental Disease 2007;195(10):861‐5. [DOI] [PubMed] [Google Scholar]
Falsetti 2001 {published data only}
- Falsetti SA, Resnick HS, Davis J, Gallagher NG. Treatment of posttraumatic stress disorder with comorbid panic attacks: Combining cognitive processing therapy with panic control treatment techniques. Group Dynamics 2001;5(4):252‐60. [Google Scholar]
Fecteau 1999 {published data only}
- Fecteau G, Nicki R. Cognitive behavioural treatment of post traumatic stress disorder after motor vehicle accident. Behavioural & Cognitive Psychotherapy 1999;27(3):201‐14. [Google Scholar]
Foa 2004 {published data only}
- Foa EB, Rauch SA. Cognitive changes during prolonged exposure versus prolonged exposure plus cognitive restructuring in female assault survivors with posttraumatic stress disorder. Journal of Consulting and Clinical Psychology 2004;72(5):879‐84. [DOI] [PubMed] [Google Scholar]
Gamble 2005 {published data only}
- Gamble J, Creedy D, Moyle W, Webster J, McAllister M, Dickson P. Effectiveness of a counseling intervention after a traumatic childbirth: A randomized controlled trial. Birth 2005;32(1):11‐19. [DOI] [PubMed] [Google Scholar]
Gidron 2001 {published data only}
- Gidron Y, Gal R, Freedman S, Twiser I, Lauden A, Snir Y, Benjamin J. Translating research findings to PTSD prevention: Results of a randomized‐controlled pilot study. Journal of Traumatic Stress 2001;14(4):773‐80. [DOI] [PubMed] [Google Scholar]
Gidron 2007 {published data only}
- Gidron Y, Gal R, Givati G, Lauden A, Snir Y, Binjamin J. Interactive effects of Memory Structuring and gender in preventing posttraumatic stress symptoms. The Journal of Nervous and mental Disease 2007;195(2):1‐4. [DOI] [PubMed] [Google Scholar]
Hirai 2005 {published data only}
- Hirai M, Clum G. An Internet‐Based Self‐Change Program for Traumatic Event Related Fear, Distress, and Maladaptive Coping. Journal of Traumatic Stress 2005;18(6):631‐6. [DOI] [PubMed] [Google Scholar]
Hollifield 2007 {published data only}
- Hollifield M, Sinclair‐Lian N, Warner TD, Hammerschlag TD. Acupuncture for post traumatic stress disorder. Journal of Nervous and Mental Disease 2007;195:504‐13. [DOI] [PubMed] [Google Scholar]
Holmes 2007 {published data only}
- Holmes A, Hodgins G, Adey S, Menzel S, Danne P, Kossmann T, Judd F. Trial of interpersonal counselling after major physical trauma. Australian and New Zealand Journal of Psychiatry 2007;41:926‐33. [DOI] [PubMed] [Google Scholar]
Kazak 2005 {published data only}
- Kazak AE, Simms S, Alderfer MA, Rourke MT, Crump T, McClure K, Jones P, Rodriguez A, Boeving A, Hwang WT, Reilly A. Feasibility and preliminary outcomes from a pilot study of a brief psychological intervention for families of children newly diagnosed with cancer. Journal of Pediatric Psychology 2005;30(8):644‐55. [DOI] [PubMed] [Google Scholar]
Lange 2001 {published data only}
- Lange A, Ven JP, Schrieken B, Emmelkamp PM. Interapy. Treatment of posttraumatic stress through the Internet: a controlled trial. Journal of Behavior Therapy & Experimental Psychiatry 2001;32(2):73‐90. [DOI] [PubMed] [Google Scholar]
Lee 2002 {published data only}
- Lee C, Gavriel H, Drummond P, Richards J, Greenwald R. Treatment of PTSD: stress inoculation training with prolonged exposure compared to EMDR. Journal of Clinical Psychology 2002;58(9):1071‐89. [DOI] [PubMed] [Google Scholar]
Levine 2005 {published data only}
- Levine EG, Eckhardt J, Targ E. Change in post‐traumatic stress symptoms following psychological treatment for breast cancer. Psycho‐Oncology 2005;14(8):618‐35. [DOI] [PubMed] [Google Scholar]
Marchand 2006 {published data only}
- Marchand A, Guay S, Boyer R, Iucci S, Martin A, St‐Hilaire M. A randomized controlled trial of an adapted form of individual critical incident stress debriefing for victims of an armed robbery. Brief Treatment and Crisis Intervention 2006;6:122‐9. [Google Scholar]
Marcus 1997 {published data only}
- Marcus SV, Marquis P, Sakai C. Controlled study of treatment of PTSD using EMDR in an HMO setting. Psychotherapy 1997;34(3):307‐15. [Google Scholar]
Power 2002 {published data only}
- Power K, McGoldrick T, Brown K, Buchanan R, Sharp D, Swanson V, & Karatzias A. A controlled comparison of eye movement desensitisation and reprocessing versus exposure plus cognitive restructuring versus waiting list in the treatment of post‐traumatic stress disorder. Clinical Psychology and Psychotherapy 2002;9(5):299‐318. [Google Scholar]
Resnick 2005 {published data only}
- Resnick H, Acierno R, Kilpatrick DG, Holmes M. Description of an early intervention to prevent substance abuse and psychopathology in recent rape victims. Behavior Modification 2005;29(1):156‐188. [DOI] [PubMed] [Google Scholar]
Rose 1999 {published data only}
- Rose S, Brewin CR, Andrews B, Kirk M. A randomized controlled trial of individual psychological debriefing for victims of violent crime. Psychological Medicine 1999;29:793‐799. [DOI] [PubMed] [Google Scholar]
Rosser 1991 {published data only}
- Rosser R, Dewar S, Thompson J. Psychological aftermath of the King's Cross fire. Journal of the Royal Society of Medicine 1991;84:4‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rothbaum 1997 {published data only}
- Rothbaum BO. A controlled study of eye movement desensitization and reprocessing in the treatment of posttraumatic stress disorder sexual assault victims. Bulletin of the Meninger Clinic 1997;61:317‐34. [PubMed] [Google Scholar]
Rothbaum submitted {unpublished data only}
- Rothbaum BA, Houry D, Heekin M, Leiner AS, Daugherty J, Smith LS, Gerardi M. A pilot study of an exposure‐based intervention in the emergency department designed to prevent posttraumatic stress disorder A Pilot Study of an Exposure‐Based Intervention in the Emergency Department Designed to Prevent Posttraumatic Stress Disorder. Submitted for publication. [DOI] [PubMed]
Ryding 1998 {published data only}
- Ryding EL, Wijma K, Wijma B. Postpartum counselling after an emergency cesarean. Clinical Psychology and Psychotherapy 1998;5:231‐7. [Google Scholar]
Ryding 2004 {published and unpublished data}
- Ryding EL, Wiren E, Johansson G, Ceder B, Dahlstrom A. Group counselling for mothers after emergency cesarean section: A randomized controlled trial of intervention. Birth 2004;31(4):247‐53. [DOI] [PubMed] [Google Scholar]
Scheck 1998 {published data only}
- Scheck MM, Schaeffer JA, Gillette C. Brief psychological intervention with traumatized young women: the efficacy of eye movement desensitization and reprocessing. Journal of Traumatic Stress 1998;11(1):25‐44. [DOI] [PubMed] [Google Scholar]
Schoutrop 2002 {published data only}
- Schoutop MJA, Lange A, Hanewald G, Davidovich U. Structured writing and processing major stressful events: A controlled trial. Psychotherapy and Psychosomatics 2002;71:151‐7. [DOI] [PubMed] [Google Scholar]
Sloan 2004 {published data only}
- Sloan DM, Marx BP. A closer examination of the structured written disclosure procedure. Journal of Consulting and Clinical Psychology 2004;72(2):165‐75. [DOI] [PubMed] [Google Scholar]
Steffgen 2002 {published data only}
- Steffgen G, Boer C, Bollendorff C. Prevention of post‐traumatic stress disorder in bank clerks after a bank robbery [Prävention der Posttraumatischen Belastungsstörung bei Bankangestellten nach einem Überfall]. Arbeitsmedizin Sozialmedizin Umweltmedizin 2002;37(8):369‐72. [Google Scholar]
Taylor 2003 {published data only}
- Taylor S, Thordarson DS, Maxfield L, Fedoroff IC, Lovell K, Ogrodniczuk J. Comparative efficacy, speed, and adverse effects of three PTSD treatments: exposure therapy, EMDR, and relaxation training. Journal of Consulting and Clinical Psychology 2003;71(2):330‐8. [DOI] [PubMed] [Google Scholar]
Turpin 2005 {published data only}
- Turpin G, Downs M, Mason S. Psychological debriefing for preventing post traumatic stress disorder (PTSD). British Journal of Psychiatry 2005;187(1):76‐82. [Google Scholar]
Wilson 1995 {published data only}
- Wilson SA, Becker LA, Tinker RH. Eye movement desensitization and reprocessing (EMDR) treatment for psychologically traumatized individuals. Journal of Consulting and Clinical Psychology 1995;63(6):928‐37. [DOI] [PubMed] [Google Scholar]
Zatzick 2001 {published and unpublished data}
- Zatzick DF, Roy‐Byrne P, Russo JE, Rivara FP, Koike A, Jurkovich GJ, Katon W. Collaborative interventions for physically injured trauma survivors: A pilot randomized effectiveness trial. General Hospital Psychiatry 2001;23:114‐23. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Kilpatrick 1984 {published data only}
- Kilpatrick DG, Veronen LJ. Treatment of rape‐related problems: Crisis intervention is not enough. In: Cohen L, Claiborn W, Specter G editor(s). Crisis Intervention: Community‐Clinical Psychology Series. Second Edition. New York: Human Services Press, 1984. [Google Scholar]
References to ongoing studies
Koopman {unpublished data only}
- Koopman C, Kreshka MA, Bodai BI, Chen XH, Angell KL, Nakata T, Wolf H, Graddy K, Donnelly P. The effects of a workbook‐journal in reducing depression and posttraumatic stress disorder in rural/socially isolated women newly diagnosed with breast cancer. 63rd Annual Meeting of the American Psychosomatic Society, 2005 March 2‐5, Vancouver, Canada. 2005.
Nixon {unpublished data only}
- Nixon RD. Using cognitive processing therapy for assault victims with acute stress disorder. 29th Australian Association for Cognitive and Behaviour Therapy Annual Conference; 2006 October 18 ‐ 23; Manly. 2006:30.
Shalev {unpublished data only}
- Shalev A, Freedman S, Adessky R, & Watson P. Early interventions for PTSD: What works, and for whom?. 22nd Annual Meeting, International Society for Traumatic Stress Studies, November 4 ‐ 7 2006, Hollywood, CA. 2006:62.
Additional references
APA 1994
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Washington DC: American Psychiatric Association, 1994. [Google Scholar]
Baum 1983
- Baum A, Gatchel RJ, Schaeffer MA. Emotional , behavioral and physiological effects of chronic stress at Three Mile Island. Journal of Consulting and Clinical Psychology 1983;51:565‐72. [DOI] [PubMed] [Google Scholar]
Beck 1961
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry 1961;4:561‐71. [DOI] [PubMed] [Google Scholar]
Beck 1988
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology 1988;56:893‐7. [DOI] [PubMed] [Google Scholar]
Bisson 2003
- Bisson JI, Roberts N, Macho G. Service innovations: The Cardiff traumatic stress initiative: An evidence‐based approach to early psychological intervention following traumatic events. Psychiatric Bulletin 2003;27(4):145‐7. [Google Scholar]
Bisson 2007
- Bisson JI, Andrews M. Psychological treatment of post‐traumatic stress disorder (PTSD). Cochrane Database of Systematic Reviews 2007, Issue 3. [DOI: 10.1002/14651858.CD003388.pub3] [DOI] [PubMed] [Google Scholar]
Bisson 2007a
- Bisson JI, Ehlers A, Matthews R, Pilling S, Richards D, Turner S. Psychological treatments for chronic post‐traumatic stress disorder: Systematic review and meta‐analysis. British Journal of Psychiatry 2007;190(2):97‐104. [DOI] [PubMed] [Google Scholar]
Blake 1995
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney, D.S, et al. The development of a clinician administered PTSD scale dDevelopment of a clinician administered PTSD scale. Journal of Traumatic Stress 1995;8:75‐90. [DOI] [PubMed] [Google Scholar]
Bonanno 2004
- Bonanno GA. Loss, trauma and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events?. American Psychologist 2004;59(1):20‐8. [DOI] [PubMed] [Google Scholar]
Bradley 2005
- Bradley R, Greene J, Russ E, Dutra L, Westen D. A Multidimensional Meta‐Analysis of Psychotherapy for PTSD. American Journal of Psychiatry 2005;162(2):214‐27. [DOI] [PubMed] [Google Scholar]
Brewin 1999
- Brewin CR, Andrews B, Rose S, Kirk M. Acute stress disorder and posttraumatic stress disorder in victims of violent crime. American Journal of Psychiatry 1999;156(3):360‐6. [DOI] [PubMed] [Google Scholar]
Brewin 2000
- Brewin CR, Andrew B, Valentine JD. Meta‐analysis of risk factors for posttraumatic stress disorder in trauma‐exposed adults. Journal of Consulting & Clinical Psychology 2000;68:748‐66. [DOI] [PubMed] [Google Scholar]
Brewin 2003
- Brewin CR. Posttraumatic Stress Disorder: Malady or Myth. New Haven: Yale University Press, 2003. [Google Scholar]
Brewin 2008
- Brewin CR, Scragg P, Robertson M, Thompson M, d'Ardenne P, Ehlers A. Promoting mental healthfollowing the London bombings: a screen and treat approach. Journal of Traumatic Stress 2008;21(1):3‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bryant 2003b
- Bryant RA, Moulds ML, Nixon RVD. Cognitive behaviour therapy of acute stress disorder: a four‐year follow‐up. Behaviour Research & Therapy 2003;41:489‐94. [DOI] [PubMed] [Google Scholar]
Bryant 2006
- Bryant RA, Moulds ML, Nixon RDV, Mastrodomenico J, Felmingham K, Hopwood S. Hypnotherapy and cognitive behaviour therapy of acute stress disorder: A 3‐year follow‐up. Behaviour Research & Therapy 2006;44:1331‐5. [DOI] [PubMed] [Google Scholar]
Crummier 1991
- Crummier TL, Green BL. Posttraumatic stress disorder as an early response to sexual assault. Journal of Interpersonal Violence 1991;6:160‐73. [Google Scholar]
Davidson 1997
- Davidson JR, Book SW, Colket L, Tupler LA, Roth S, David D, et al. Assessment of a new self‐rating scale for posttraumatic stress disorder. Psychological Medicine 1997;27:153‐60. [DOI] [PubMed] [Google Scholar]
Ehlers 1998
- Ehlers A, Mayou RA, Bryant B. Psychological predictors of chronic posttraumatic stress disorder after motor vehicle accidents. Journal of Abnormal Psychology 1998;107(3):508‐19. [DOI] [PubMed] [Google Scholar]
Ehlers 2003a
- Ehlers A, Clark DM. Early psychological interventions for adult survivors of trauma: A review. Biological Psychiatry 2003;53:817‐26. [DOI] [PubMed] [Google Scholar]
Fletcher 2007
- Fletcher J. What is heterogeneity and is it important?. British Medical Journal 2007;334:94‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Foa 1995
- Foa EB. Posttraumatic Stress Diagnostic Scale Manual. United States of America: National Computer Systems, Inc, 1995. [Google Scholar]
Foa 1997
- Foa EB, Meadows EA. Psychosocial treatments for posttraumatic stress disorder: A critical review. Annual Review of Psychology 1997;48:449‐80. [DOI] [PubMed] [Google Scholar]
Foa 2008
- Foa EB, Keane TM, Friedman MJ, Cohen JA. Effective Treatments for PTSD: Practice Guidelines from the International Society for Traumatic Stress Studies. Second Edition. New York: Guildford Press, 2008. [Google Scholar]
Gleser 1981
- Gleser CG, Green BL, Winget CN. Prolonged psychological effects of disaster. New York: Academic Press, 1981. [Google Scholar]
Goenjian 1993
- Goenjian A. A mental health relief programme in Armenia after the 1988 Earthquake: Implementation and clinical observations. British Journal of Psychiatry 1993;163:230‐9. [DOI] [PubMed] [Google Scholar]
Gray 2005
- Gray MJ, Litz BT. Behavioral interventions for recent trauma. Behavior Modification 2005;29(1):189‐215. [DOI] [PubMed] [Google Scholar]
Green 1990
- Green BL, Grace MC, Lindy JD, Gleser GC, Leonard AC, Crummier TL. Buffalo Creek survivors in the second decade: comparison with unexposed and nonlitigant groups. Journal of Applied Social Psychology 1990;20:1033‐50. [Google Scholar]
Harvey 1998
- Harvey AG, Bryant RA. The relationship between acute stress disorder and posttraumatic stress disorder: A prospective evaluation of motor vehicle accident survivors. Journal of Consulting & Clinical Psychology 1998;66(3):507‐12. [DOI] [PubMed] [Google Scholar]
Hertlein 2004
- Hertlein KM, Ricci RJ. A systematic research synthesis of EMDR studies: Implementation of the platinum standard. Trauma, Violence and Abuse 2004;5(3):285‐300. [DOI] [PubMed] [Google Scholar]
Higgins 2008
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.1 [updated September 2008]. Cochrane Collaboration, 2008. [Google Scholar]
Horowitz 1979
- Horowitz MJ, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosomatic Medicine 1979;41:209‐18. [DOI] [PubMed] [Google Scholar]
Hough 1990
- Hough RL, Vega WA, Valle R, Kolody B, Griswald del Castillo R, Tarke H. Mental health consequences of the San Ysidro McDonald's massacre: A community study. Journal of Traumatic Stress 1990;3:71‐92. [Google Scholar]
Kenardy 1996
- Kenardy J, Carr V. Imbalance in the debriefing debate: what we don't know outweighs what we do. Bulletin of the Australian Psychological Society 1996;17(1):4‐6. [Google Scholar]
Kessler 1995
- Kessler R, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry 1995;52:1048‐60. [DOI] [PubMed] [Google Scholar]
Kilpatrick 1987
- Kilpatrick DG, Saunders BE, Veronen LJ, Best CL, Von JM. Criminal victimization: Lifetime prevalence reporting to police, and psychological impact. Crime and Delinquency 1987;33:479‐89. [Google Scholar]
Kulka 1990
- Kulka RA, Schlenger WE, Fairbank JA, Jordan BK, Hough RL, Marmar CR, Weiss DS. Trauma and the Vietnam war generation: Report of findings form the Vietnam Veterans Study. New York: Bruner/Mazel, 1990. [Google Scholar]
Lau 2006
- Lau J, Ioannidis JPA, Terrin N, Schmid CH, Olkin I. The case of the misleading funnel plot. British Medical Journal 2006;333:597‐600. [DOI] [PMC free article] [PubMed] [Google Scholar]
Litz 2002
- Litz BT, Gray MJ, Bryant RA, Adler AB. Early intervention for trauma: Current status and future directions. Clinical Psychology: Science and Practice 2002;9(2):112‐34. [Google Scholar]
Litz 2004
- Litz BT, Gray MJ. Early intervention for trauma in adults: A framework for first aid and secondary prevention. In: Litz BT editor(s). Early Intervention for Trauma and Traumatic Loss. New York: Guilford Press, 2004. [Google Scholar]
McFarlane 1988
- McFarlane AC. The longitudinal course of posttraumatic morbidity: The range of outcomes and their predictors. Journal of Nervous and Mental Disease 1988;176:22‐9. [DOI] [PubMed] [Google Scholar]
McNally 2003
- McNally RJ, Bryant RA, Ehlers A. Does early psychological intervention promote recovery from posttraumatic stress disorder?. Psychological Science in the Public Interest 2003;4(2):45‐79. [DOI] [PubMed] [Google Scholar]
Moher 1998
- Moher D, Pham B, Jones A, Cook DJ, Jadad AR, Moher M, Tugwell P, Klassen TP. Does quality of reports of randomised trials affect estimates of intervention efficacy in meta‐analyses?. The Lancet 1998;352:609‐13. [DOI] [PubMed] [Google Scholar]
Moncrieff 2001
- Moncrieff J, Churchill R, Drummond C. Development of a quality assessment for trials of treatment for depression and neurosis. International Journal of Methods in Psychiatric Research 2001;10(3):126‐33. [Google Scholar]
NCCMH 2005
- National Institute for Clinical Excellence. Post‐traumatic Stress Disorder (PTSD): The Management of PTSD in Adults and Children in Primary and Secondary Care. London: National Collaborating Centre for Mental Health, 2005. [Google Scholar]
North 1994
- North CS, Smith EM, Spitzangel EL. Postraumatic stress disorder in survivors of a mass shooting. American Journal of Psychiatry 1994;151:82‐8. [DOI] [PubMed] [Google Scholar]
North 2007
- North CS. Epidemiology of Disaster Mental Health. In: Ursano RJ, Fullerton CS, Weisaeth L, Raphael B editor(s). Textbook of Disaster Psychiatry. Cambridge: Cambridge University Press, 2007. [Google Scholar]
Ozer 2003
- Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: A meta‐analysis. Psychological Bulletin 2003;129(1):52‐73. [DOI] [PubMed] [Google Scholar]
RevMan 2008 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version Version 5.0. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2008.
Roberts 2009
- Roberts NP, Kitchiner NJ, Kenardy J, Bisson J. Multiple session early psychological interventions for the prevention of post traumatic stress disorder. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD006869.pub2] [DOI] [PubMed] [Google Scholar]
Rose 2002
- Rose S, Bisson J, Churchill R, Wessely S. Psychological debriefing for preventing post traumatic stress disorder (PTSD). Cochrane Database of Systematic Reviews 2002, Issue 2. [DOI: 10.1002/14651858.CD000560] [DOI] [PubMed] [Google Scholar]
Rothbaum 1992
- Rothbaum BO, Foa EB, Riggs DS, Murdock T, Walsh W. A prospective examination of post‐traumatic stress disorder in rape victims. Journal of Traumatic Stress 1992;5:455‐75. [Google Scholar]
Ruzek 2007
- Ruzek JI. Wanted: A Theory of Post‐Trauma Information Delivery. Paper presented at the European Conference on Traumatic Stress, Opatija, Croatia. 2007.
Spielberger 1970
- Spielberger CD, Gorsuch RL, Lushene RE. Manual for the Stait‐Trait Anxiety Inventory. Consulting Psychologists Press, Palo Alto, California, 1970. [Google Scholar]
Vick unpublished
- Vick T. A prospective study to determine the prevalence of traumatic stress symptoms after critical illness. . Unpublished PhD.
Ware 1993
- Ware JE, Snow KK, Kosinski M, Gandek B. SF‐36® Health Survey Manual and Interpretation Guide. Boston, MA: New England Medical Center, The Health Institute, 1993. [Google Scholar]
Watson 2007
- Watson PJ. Early intervention for trauma‐related problems following mass trauma. In: Ursano RJ, Fullerton CS, Weisaeth L, Raphael B editor(s). Textbook of Disaster Psychiatry. Cambridge: Cambridge University Press, 2007. [Google Scholar]
Zoellner personal communication
- Zoellner LA. Email to Neil Roberts concerning diagnosis of participants and duration of condition 2007 (26 November).